Shield and Sword strategy Concept Sword Shield Early
- Slides: 18
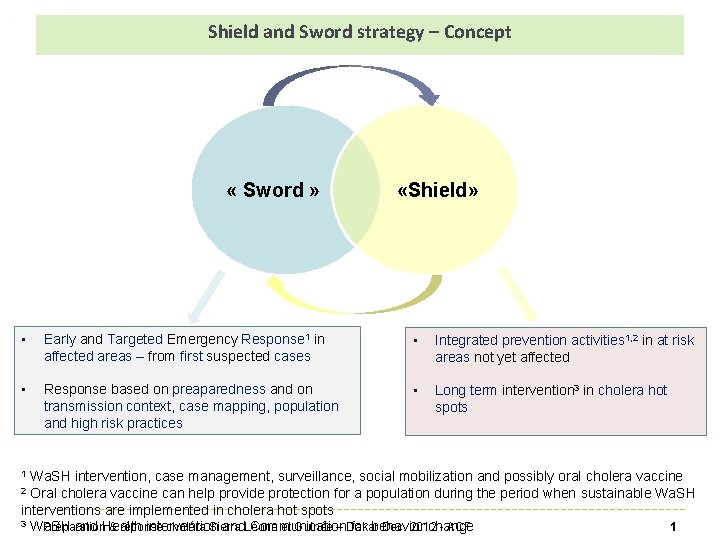
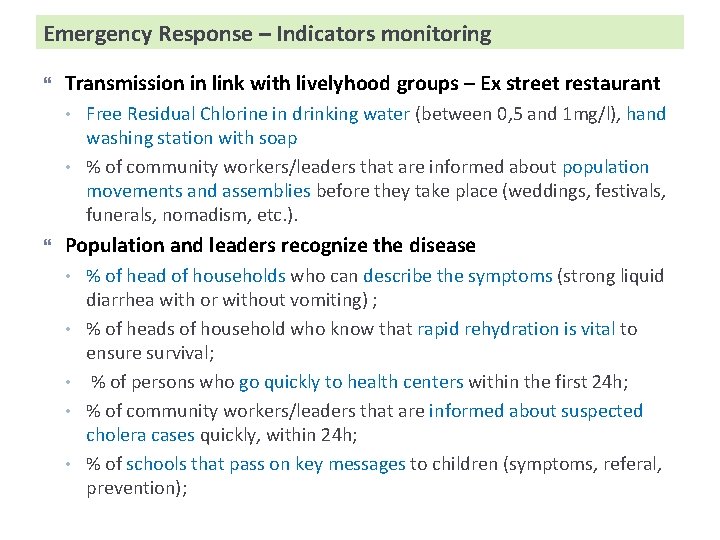
Shield and Sword strategy – Concept « Sword » «Shield» • Early and Targeted Emergency Response 1 in affected areas – from first suspected cases • Integrated prevention activities 1, 2 in at risk areas not yet affected • Response based on preaparedness and on transmission context, case mapping, population and high risk practices • Long term intervention 3 in cholera hot spots Wa. SH intervention, case management, surveillance, social mobilization and possibly oral cholera vaccine Oral cholera vaccine can help provide protection for a population during the period when sustainable Wa. SH interventions are implemented in cholera hot spots 3 Wa. SH Préparation & réponse choléra Sierra et Guinée – Dakar Dec. 2012 - ACF 1 and Health intervention and. Léone Communication for behavior change 1 2
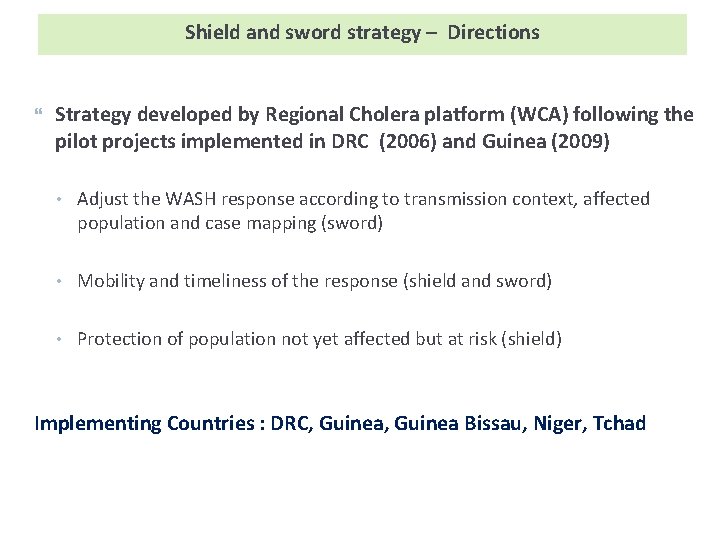
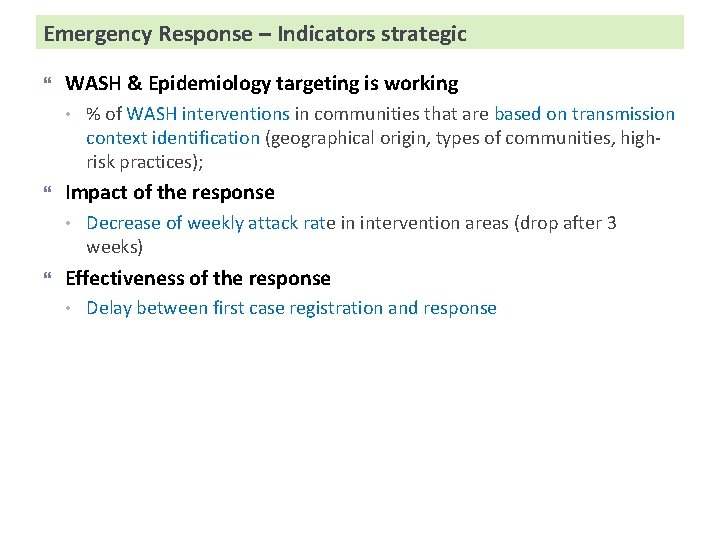
Shield and sword strategy – Directions Strategy developed by Regional Cholera platform (WCA) following the pilot projects implemented in DRC (2006) and Guinea (2009) • Adjust the WASH response according to transmission context, affected population and case mapping (sword) • Mobility and timeliness of the response (shield and sword) • Protection of population not yet affected but at risk (shield) Implementing Countries : DRC, Guinea Bissau, Niger, Tchad
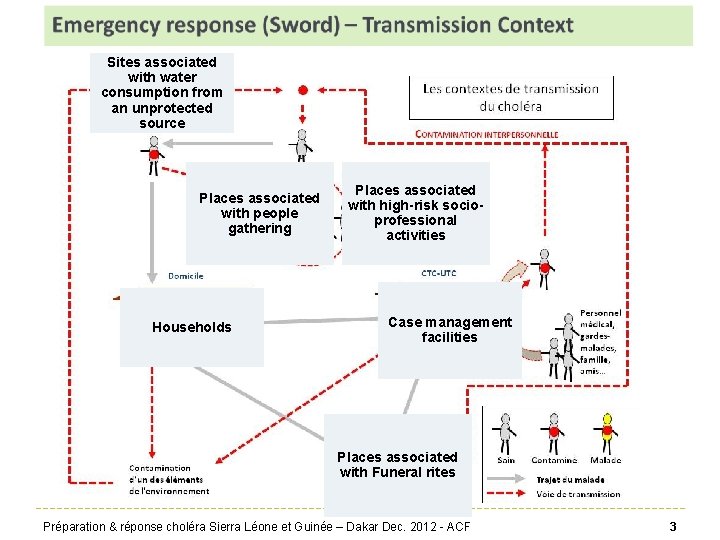
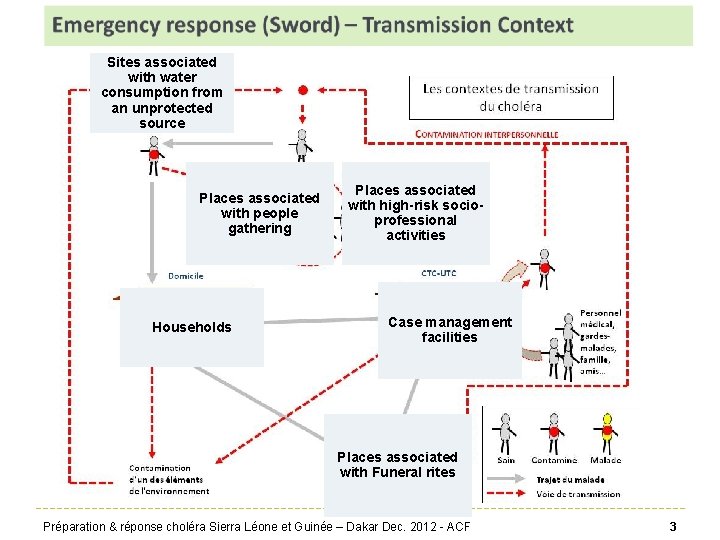
Sites associated with water consumption from an unprotected source Places associated with people gathering Households Places associated with high-risk socioprofessional activities Case management facilities Places associated with Funeral rites Préparation & réponse choléra Sierra Léone et Guinée – Dakar Dec. 2012 - ACF 3
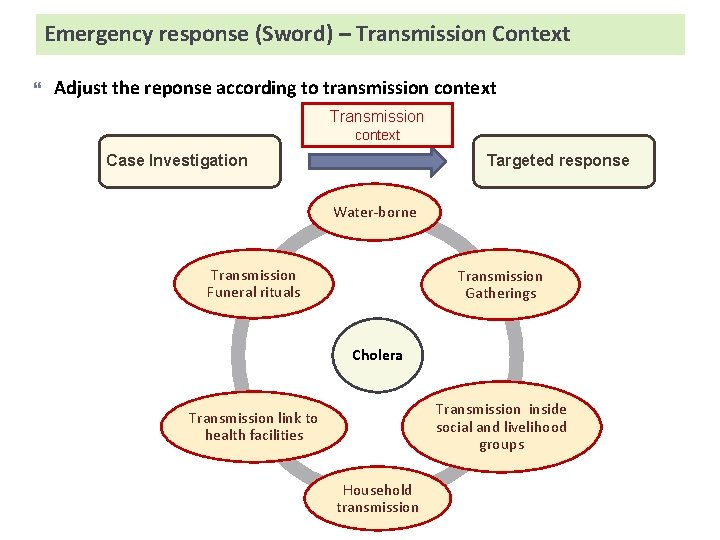
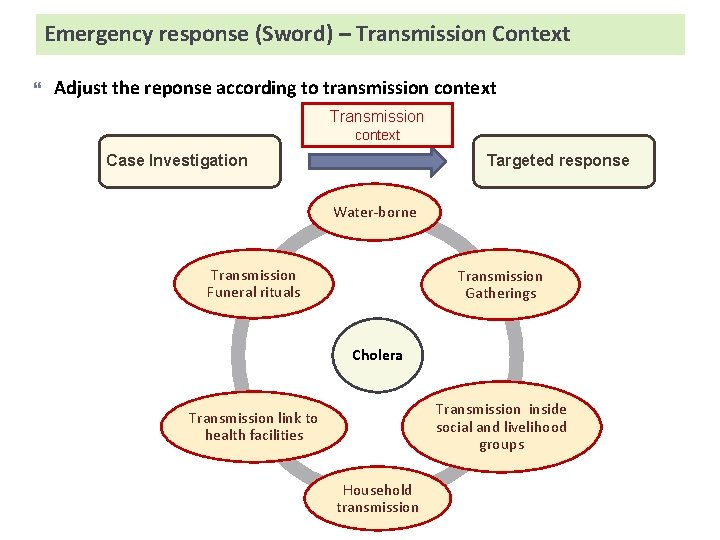
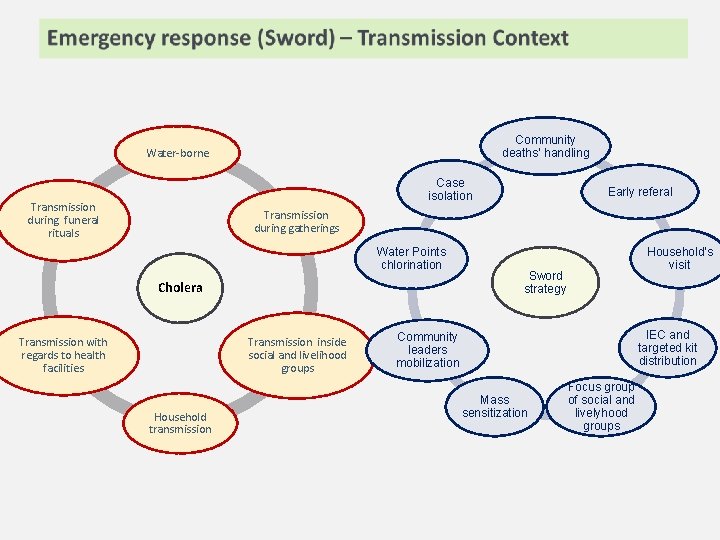
Emergency response (Sword) – Transmission Context Adjust the reponse according to transmission context Targeted response Case Investigation Water-borne Transmission Funeral rituals Transmission Gatherings Cholera Transmission inside social and livelihood groups Transmission link to health facilities Household transmission
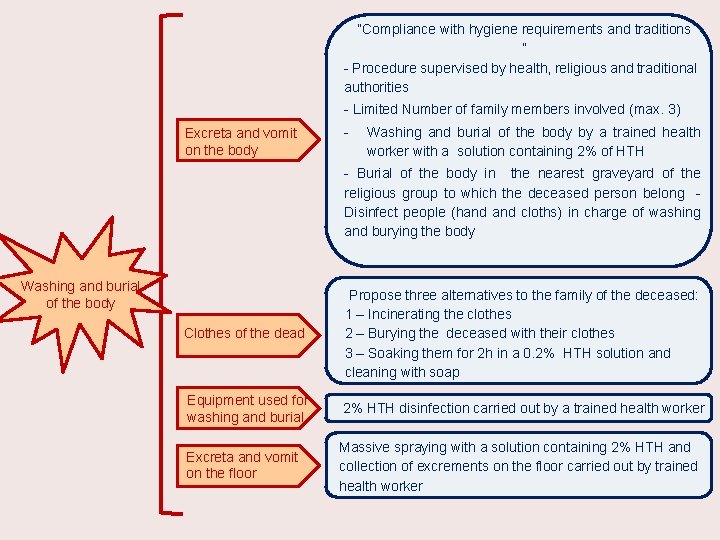
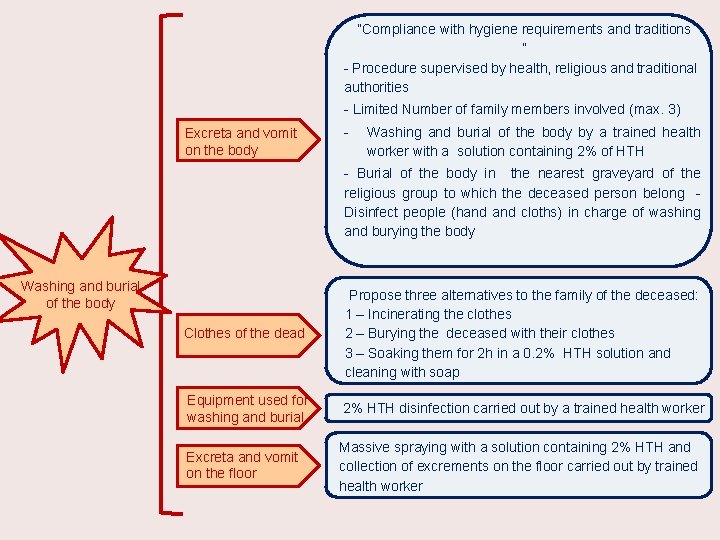
“Compliance with hygiene requirements and traditions ” - Procedure supervised by health, religious and traditional authorities - Limited Number of family members involved (max. 3) Excreta and vomit on the body - Washing and burial of the body by a trained health worker with a solution containing 2% of HTH - Burial of the body in the nearest graveyard of the religious group to which the deceased person belong Disinfect people (hand cloths) in charge of washing and burying the body Washing and burial of the body Clothes of the dead Propose three alternatives to the family of the deceased: 1 – Incinerating the clothes 2 – Burying the deceased with their clothes 3 – Soaking them for 2 h in a 0. 2% HTH solution and cleaning with soap Equipment used for washing and burial 2% HTH disinfection carried out by a trained health worker Excreta and vomit on the floor Massive spraying with a solution containing 2% HTH and collection of excrements on the floor carried out by trained health worker
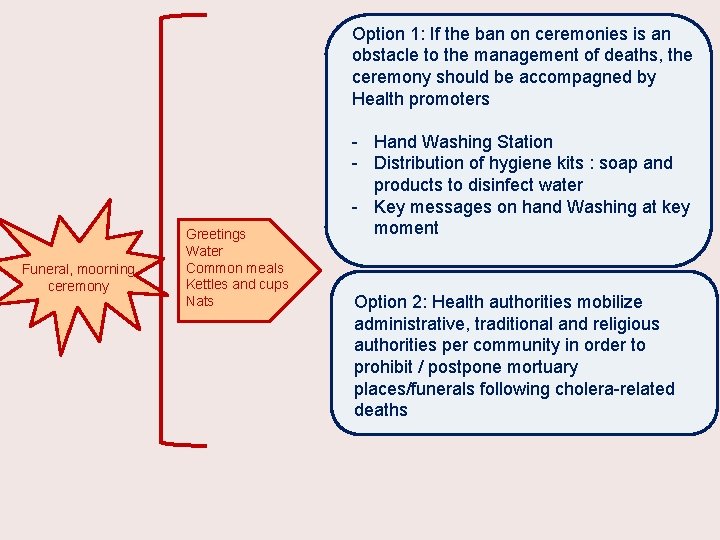
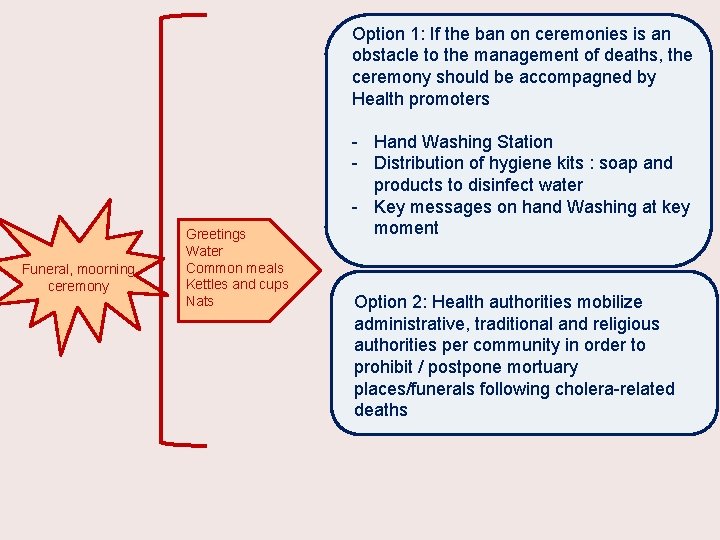
Option 1: If the ban on ceremonies is an obstacle to the management of deaths, the ceremony should be accompagned by Health promoters Funeral, moorning ceremony Greetings Water Common meals Kettles and cups Nats - Hand Washing Station - Distribution of hygiene kits : soap and products to disinfect water - Key messages on hand Washing at key moment Option 2: Health authorities mobilize administrative, traditional and religious authorities per community in order to prohibit / postpone mortuary places/funerals following cholera-related deaths
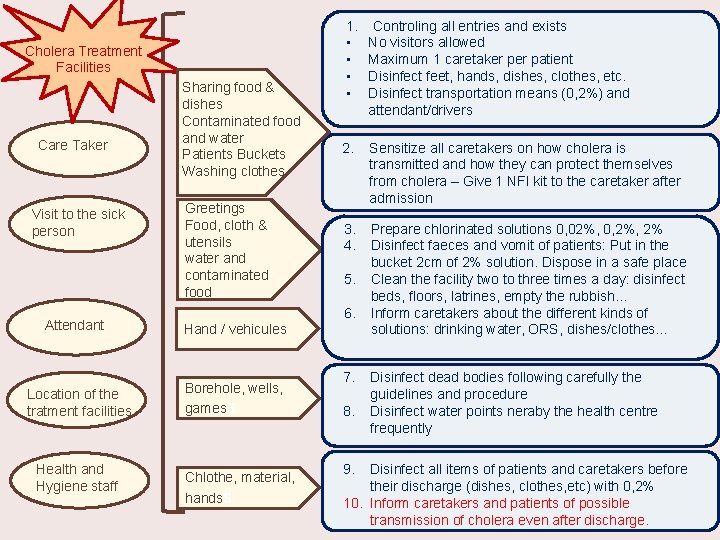
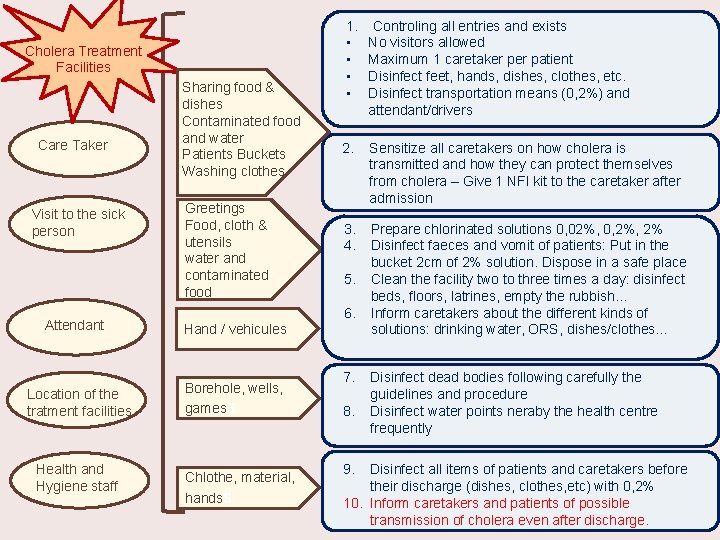
Cholera Treatment Facilities Care Taker Visit to the sick person Attendant Location of the tratment facilities Health and Hygiene staff Sharing food & dishes Contaminated food and water Patients Buckets Washing clothes Greetings Food, cloth & utensils water and contaminated food 1. • • Controling all entries and exists No visitors allowed Maximum 1 caretaker patient Disinfect feet, hands, dishes, clothes, etc. Disinfect transportation means (0, 2%) and attendant/drivers 2. Sensitize all caretakers on how cholera is transmitted and how they can protect themselves from cholera – Give 1 NFI kit to the caretaker after admission 3. 4. Prepare chlorinated solutions 0, 02%, 0, 2% Disinfect faeces and vomit of patients: Put in the bucket 2 cm of 2% solution. Dispose in a safe place Clean the facility two to three times a day: disinfect beds, floors, latrines, empty the rubbish… Inform caretakers about the different kinds of solutions: drinking water, ORS, dishes/clothes… 5. 6. Hand / vehicules Borehole, wells, gamess Chlothe, material, handss 7. 8. 9. Disinfect dead bodies following carefully the guidelines and procedure Disinfect water points neraby the health centre frequently Disinfect all items of patients and caretakers before their discharge (dishes, clothes, etc) with 0, 2% 10. Inform caretakers and patients of possible transmission of cholera even after discharge.
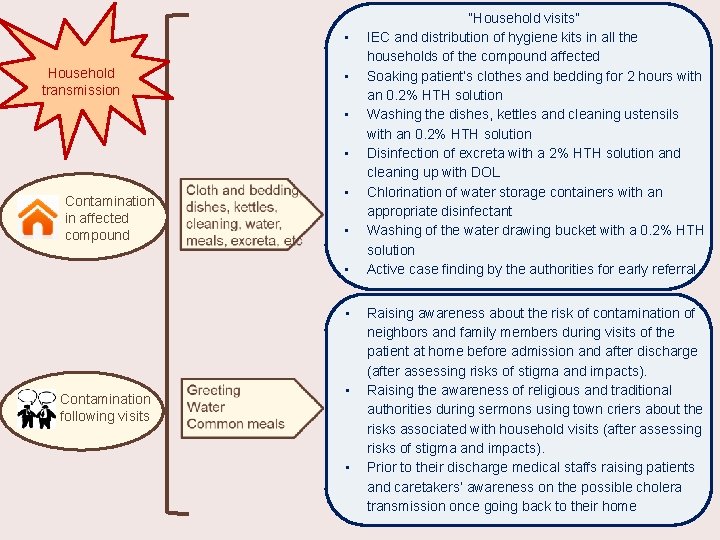
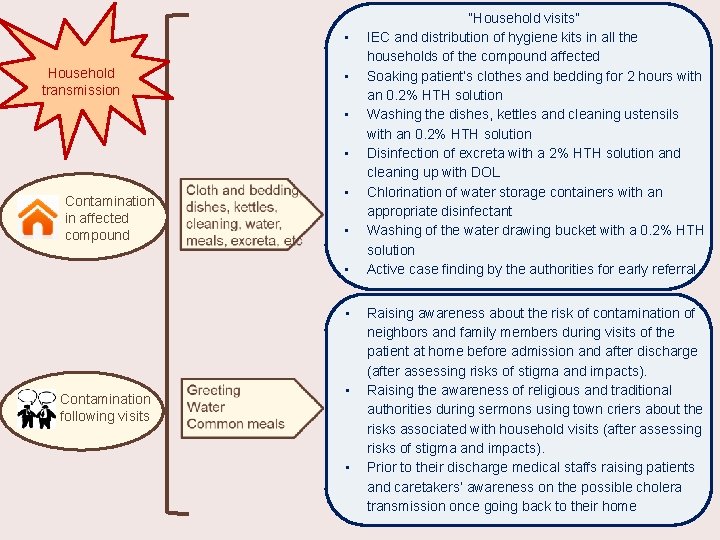
• Household transmission • • • Contamination in affected compound • • Contamination following visits • • “Household visits” IEC and distribution of hygiene kits in all the households of the compound affected Soaking patient’s clothes and bedding for 2 hours with an 0. 2% HTH solution Washing the dishes, kettles and cleaning ustensils with an 0. 2% HTH solution Disinfection of excreta with a 2% HTH solution and cleaning up with DOL Chlorination of water storage containers with an appropriate disinfectant Washing of the water drawing bucket with a 0. 2% HTH solution Active case finding by the authorities for early referral Raising awareness about the risk of contamination of neighbors and family members during visits of the patient at home before admission and after discharge (after assessing risks of stigma and impacts). Raising the awareness of religious and traditional authorities during sermons using town criers about the risks associated with household visits (after assessing risks of stigma and impacts). Prior to their discharge medical staffs raising patients and caretakers’ awareness on the possible cholera transmission once going back to their home
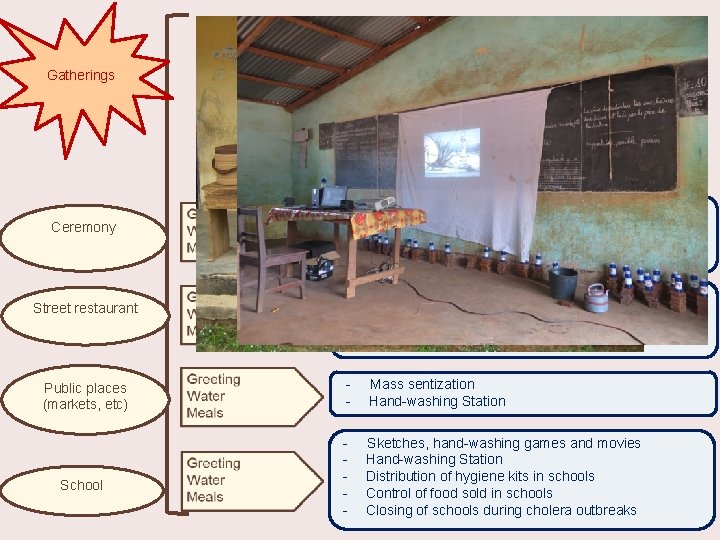
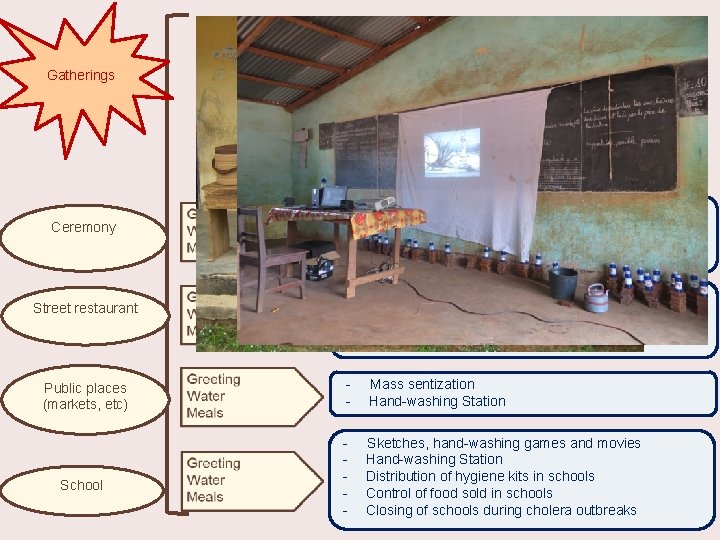
Gatherings - Ceremony - Hand Washing Station Distribution of hygiene kits : soap and products to disinfect water Key messages on food preparation - Mass sentization Hand-washing Station - Sketches, hand-washing games and movies Hand-washing Station Distribution of hygiene kits in schools Control of food sold in schools Closing of schools during cholera outbreaks Street restaurant Public places (markets, etc) School Hand Washing Station Distribution of hygiene kits : soap and products to disinfect water Key messages on hand Washing at key moment
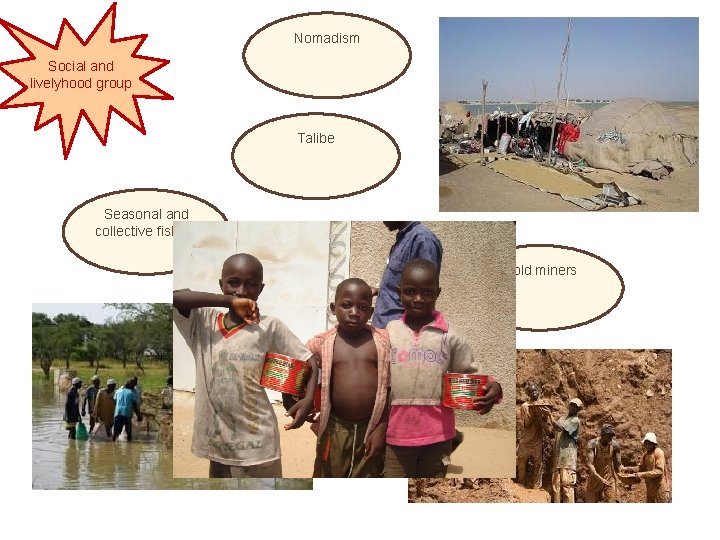
Nomadism Social and livelyhood group Talibe Seasonal and collective fishing Gold miners
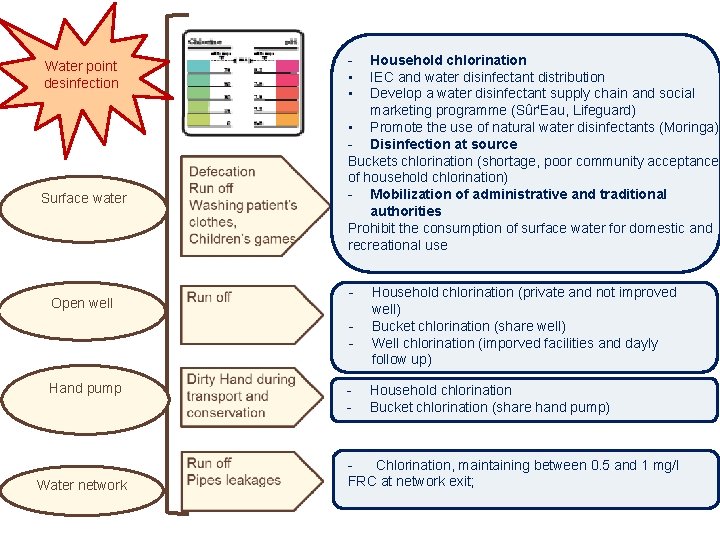
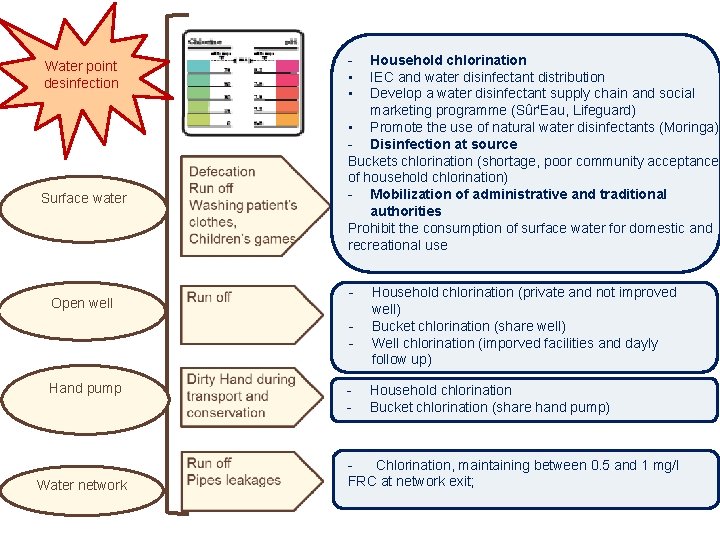
Water point desinfection Surface water Open well • • Household chlorination IEC and water disinfectant distribution Develop a water disinfectant supply chain and social marketing programme (Sûr'Eau, Lifeguard) • Promote the use of natural water disinfectants (Moringa) - Disinfection at source Buckets chlorination (shortage, poor community acceptance of household chlorination) - Mobilization of administrative and traditional authorities Prohibit the consumption of surface water for domestic and recreational use - Hand pump Water network - Household chlorination (private and not improved well) Bucket chlorination (share well) Well chlorination (imporved facilities and dayly follow up) Household chlorination Bucket chlorination (share hand pump) Chlorination, maintaining between 0. 5 and 1 mg/l FRC at network exit;
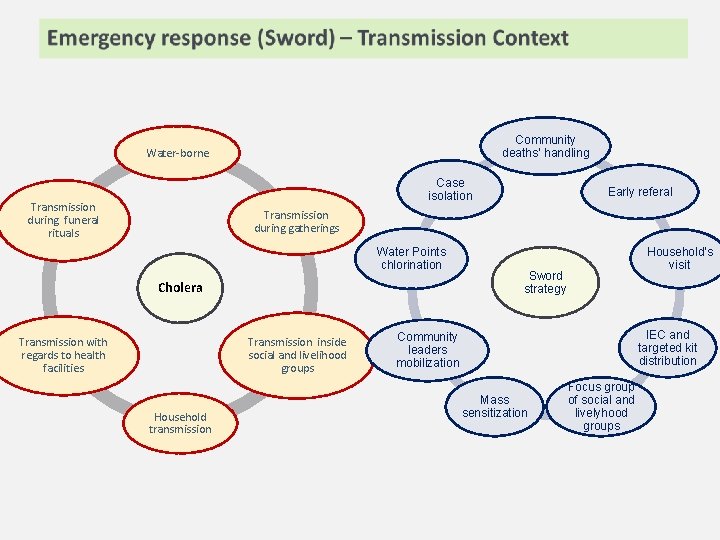
Community deaths’ handling Water-borne Case isolation Transmission during funeral rituals Early referal Transmission during gatherings Water Points chlorination Cholera Transmission inside social and livelihood groups Transmission with regards to health facilities Household transmission Household’s visit Sword strategy IEC and targeted kit distribution Community leaders mobilization Mass sensitization Focus group of social and livelyhood groups
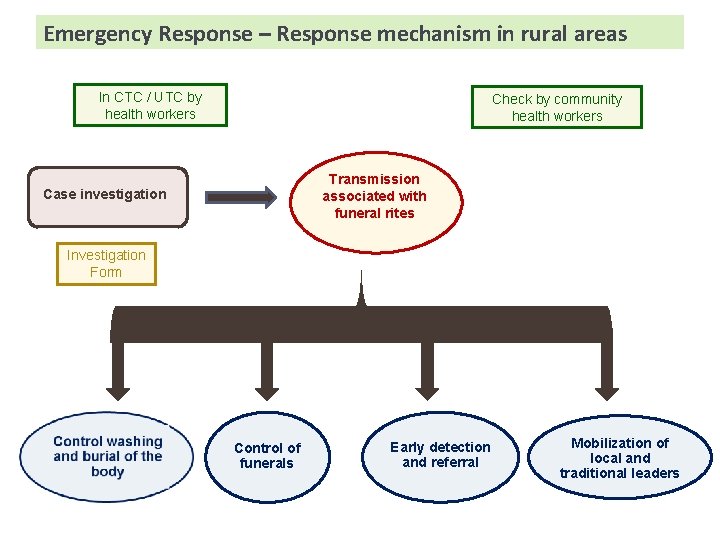
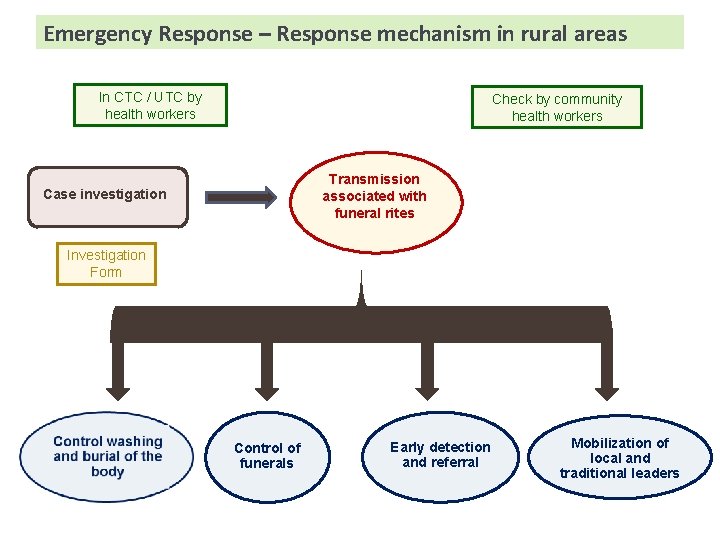
Emergency Response – Response mechanism in rural areas In CTC / UTC by health workers Check by community health workers Transmission associated with funeral rites Case investigation Investigation Form Control of funerals Early detection and referral Mobilization of local and traditional leaders
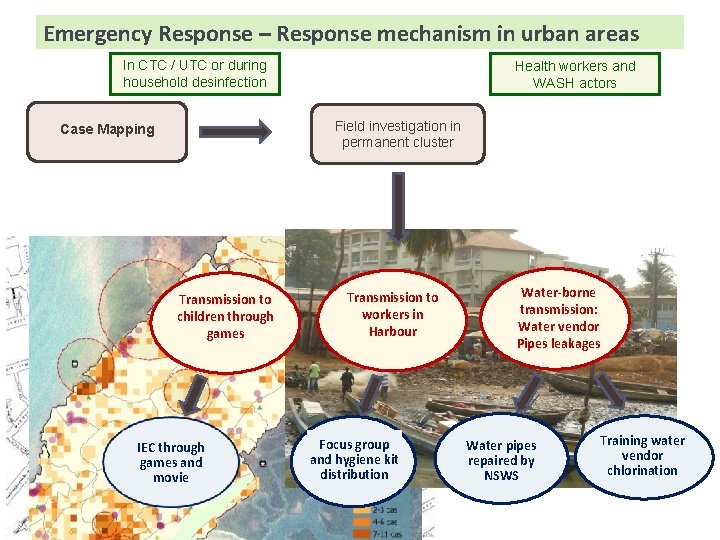
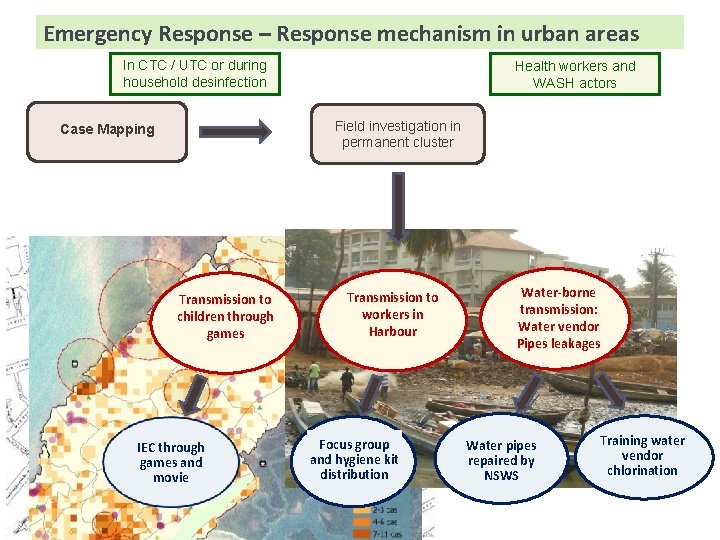
Emergency Response – Response mechanism in urban areas In CTC / UTC or during household desinfection Health workers and WASH actors Field investigation in permanent cluster Case Mapping Transmission to children through games IEC through games and movie Transmission to workers in Harbour Focus group and hygiene kit distribution Water-borne transmission: Water vendor Pipes leakages Water pipes repaired by NSWS Training water vendor chlorination
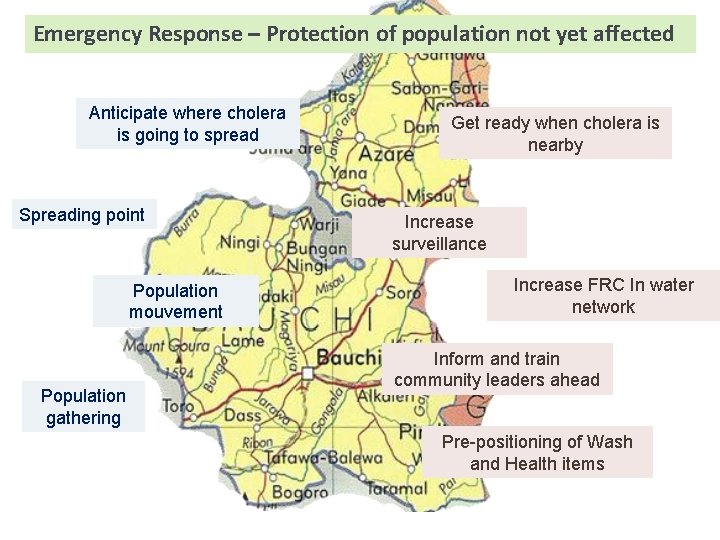
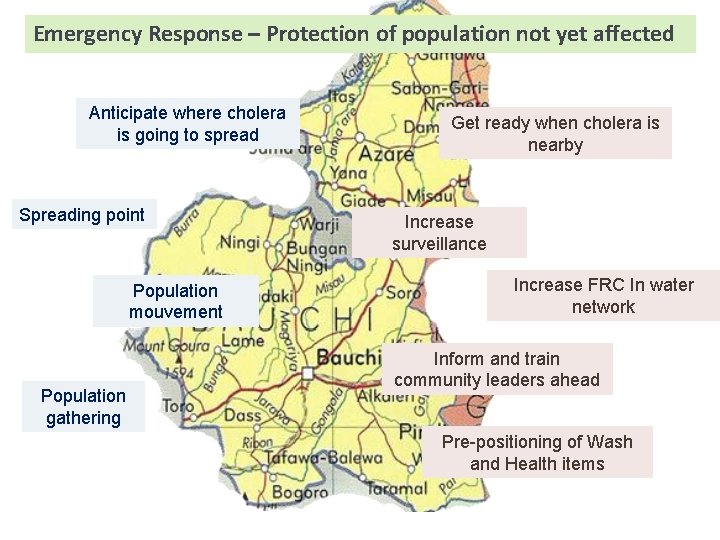
Emergency Response – Protection of population not yet affected Anticipate where cholera is going to spread Spreading point Population mouvement Population gathering Get ready when cholera is nearby Increase surveillance Increase FRC In water network Inform and train community leaders ahead Pre-positioning of Wash and Health items
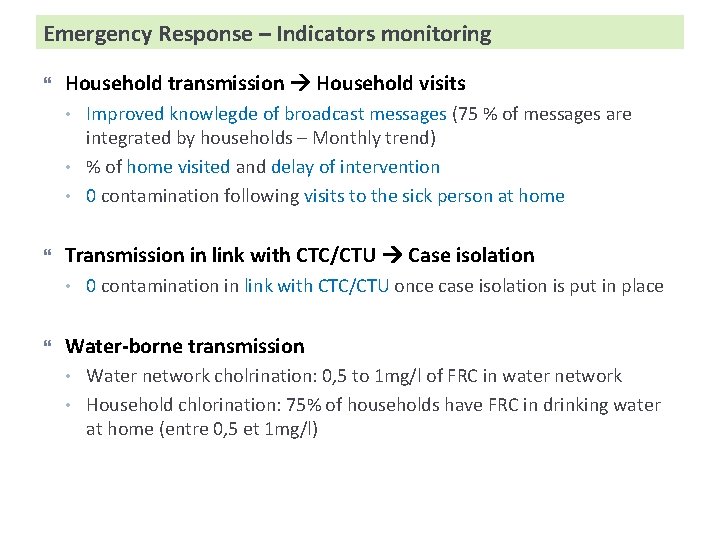
Emergency Response – Indicators monitoring Household transmission Household visits • • • Transmission in link with CTC/CTU Case isolation • Improved knowlegde of broadcast messages (75 % of messages are integrated by households – Monthly trend) % of home visited and delay of intervention 0 contamination following visits to the sick person at home 0 contamination in link with CTC/CTU once case isolation is put in place Water-borne transmission • • Water network cholrination: 0, 5 to 1 mg/l of FRC in water network Household chlorination: 75% of households have FRC in drinking water at home (entre 0, 5 et 1 mg/l)
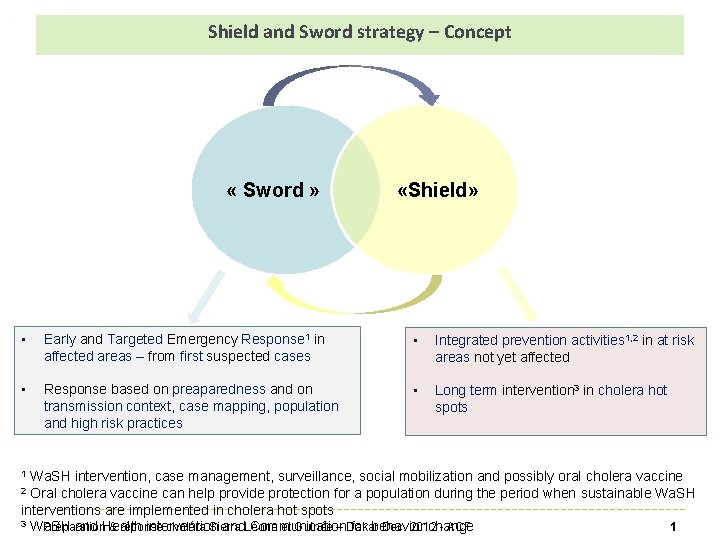
Emergency Response – Indicators monitoring Transmission in link with livelyhood groups – Ex street restaurant • • Free Residual Chlorine in drinking water (between 0, 5 and 1 mg/l), hand washing station with soap % of community workers/leaders that are informed about population movements and assemblies before they take place (weddings, festivals, funerals, nomadism, etc. ). Population and leaders recognize the disease • • • % of head of households who can describe the symptoms (strong liquid diarrhea with or without vomiting) ; % of heads of household who know that rapid rehydration is vital to ensure survival; % of persons who go quickly to health centers within the first 24 h; % of community workers/leaders that are informed about suspected cholera cases quickly, within 24 h; % of schools that pass on key messages to children (symptoms, referal, prevention);
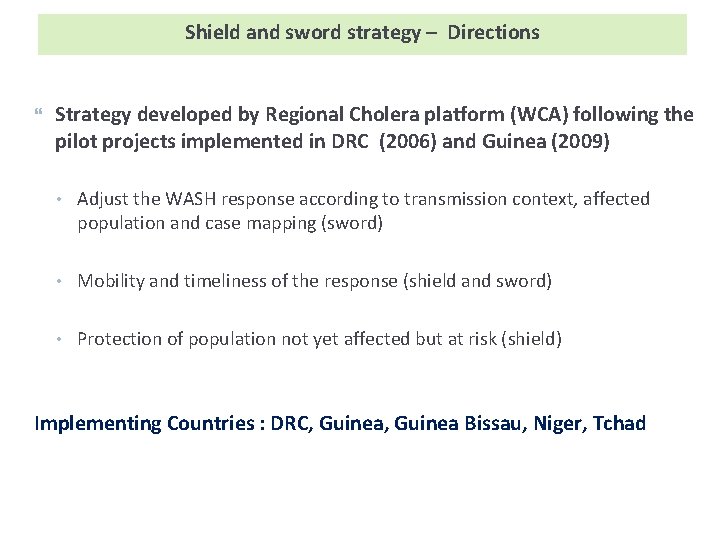
Emergency Response – Indicators strategic WASH & Epidemiology targeting is working • Impact of the response • % of WASH interventions in communities that are based on transmission context identification (geographical origin, types of communities, highrisk practices); Decrease of weekly attack rate in intervention areas (drop after 3 weeks) Effectiveness of the response • Delay between first case registration and response