Shared Decision Making Patient Empowerment in Family Medicine

- Slides: 29
Shared Decision Making &Patient Empowerment in Family Medicine Introduction to Primary Care: a course of the Center of Post Graduate Studies in FM PO Box 27121 – Riyadh 11417 Tel: 4912326 – Fax: 4970847 1
Objectives – Discuss the definition of patient empowerment – Discuss the status of patient empowerment in FP – Explain the need for patient empowerment – Discuss the reasons of powerless patients – Explain how to empower patients 2
Contents • • Shared decision making Patient Empowerment The old model vs. the new Common problems that can lead to poor decisions • Model for Clinical Problem Solving & ISDM • What is a "good" health care decision? 3
What is Patient Empowerment? 4
Patient Empowerment • Empowerment is a concept that has recently emerged in the health scene. It embraces the idea that everyone has the right to make their own choices about their health care • because patients are the ones who experience the consequences of both having and treating their illnesses, they have the right to be the primary decision makers regarding their medical conditions 5
Patient Empowerment • A key part of empowerment is that the patient, personally, must actively search out sufficient information to fully understand their health conditions and their treatment plans • Although their physician should be involved in the decision-making process, the final determination of what is best for the patient is both the right and responsibility of the individual patient. 6
Why Patient Empowerment? Remember the “patient centered clinical method” • Evaluating both the disease and the illness experience • Understanding the whole person • Finding common ground with the patient about the problem and its management • Incorporating prevention and health promotion • Enhancing the doctor-patient relationship • Being realistic 7
Why Patient Empowerment? • Only 9% of consultations with surgeons and primary care physicians meet full criteria for informed decision making. Braddock JAMA 1999 • Distinguishing elements of shared decision making occurred in 0 -11% of audio taped patient interviews with general practitioners. Elwyn 2001 • “. . Checking of understanding, and the involving of patients in decision making. . are rarely demonstrated” [in video taped consultations submitted for MRCGP examination]. Campion BMJ 2002 8
What is shared decision making? 9
• Two definitions of shared decision making: • The process of interaction of patients with their health care providers in making health care decisions • Involvement of patients with their providers in making health care decisions that are informed by the best available evidence about treatment / screening / illness management options, potential benefits, and harms, and that consider patient preferences. 10
What is it? • an individual being an active member of his/her disease management team Laura E. Santurri. Patient Empowerment: Improving the Outcomes of Chronic Diseases Through Self-Management Education. http: //www. case. edu/med/epidbio/mphp 439/Patient_Empowerment. htm 11
Shared decision making combines the measurement of patient preferences with evidencebased practice. 12
Why is shared decision making important? 13
• Interventions have different benefits/ risks that patients value differently • There is no single right answer for everyone • Ethical principle of patient autonomy and legal requirement of informed consent • Evidence-based practice movement • Increasing realization that an important piece of evidence is missing without the patient’s perspective 14
• Patients cannot be forced to follow a lifestyle dictated by others. • Preventive medicine requires patient empowerment for it to be effective. • Patients as consumers have the right to make their own choices and the ability to act on them 15
Why is the concentration of power in this relationship with physician? • Patient is sick, weak, vulnerable, not feeling fully oneself… • Patient may be afraid • Patient in a state of dependency • Lack of medical knowledge • Lack of knowledge on the “system” and how it works • Unfamiliar environment 16
Why is the concentration of power in this relationship with physician? • • Education Professional status/authority Knowledge Skills Expertise Experience On familiar territory GATEKEEPER TO HEALTHCARE SYSTEM 17
Why Patient Empowerment? “People whose lives are affected by a decision must be a part of the process of arriving at that decision. ” –John Naisbitt, Megatrends 18
How to empower patients • • Education supporting self care and self-management Offering a choice of providers Sharing treatment decisions 19
Benefits of Patient Empowerment • Learning from our patients • Taking a proactive role • Providing a support & information service to our patients and staff • Complaint Resolution • Negotiation & Mediation • Building trust 20
The old model vs. the new 21
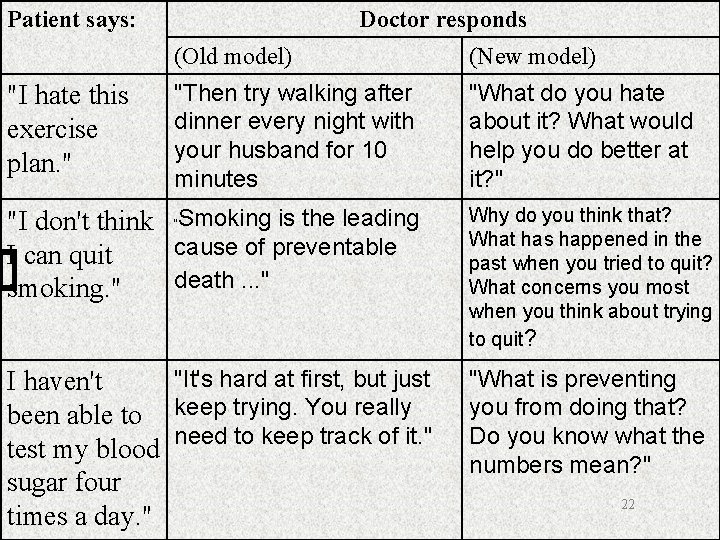
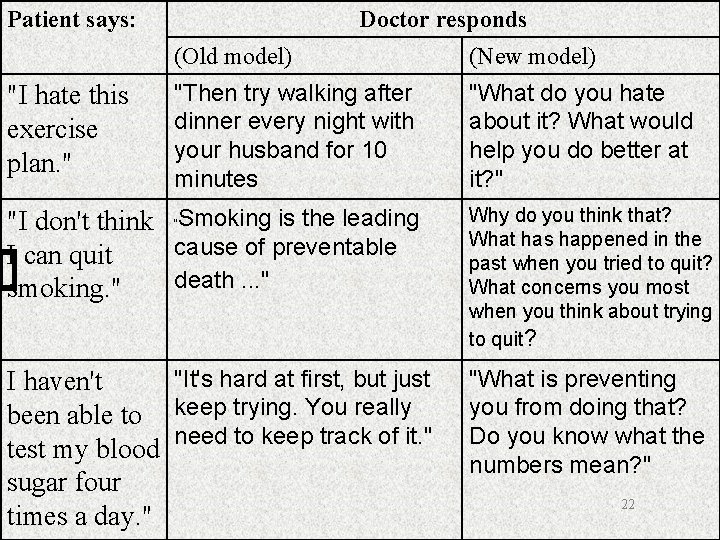
Patient says: "I hate this exercise plan. " Doctor responds (Old model) (New model) "Then try walking after dinner every night with your husband for 10 minutes "What do you hate about it? What would help you do better at it? " "I don't think Smoking is the leading cause of preventable I can quit death. . . " smoking. " Why do you think that? What has happened in the past when you tried to quit? What concerns you most when you think about trying to quit? "It's hard at first, but just I haven't been able to keep trying. You really test my blood need to keep track of it. " sugar four times a day. " "What is preventing you from doing that? Do you know what the numbers mean? " " 22
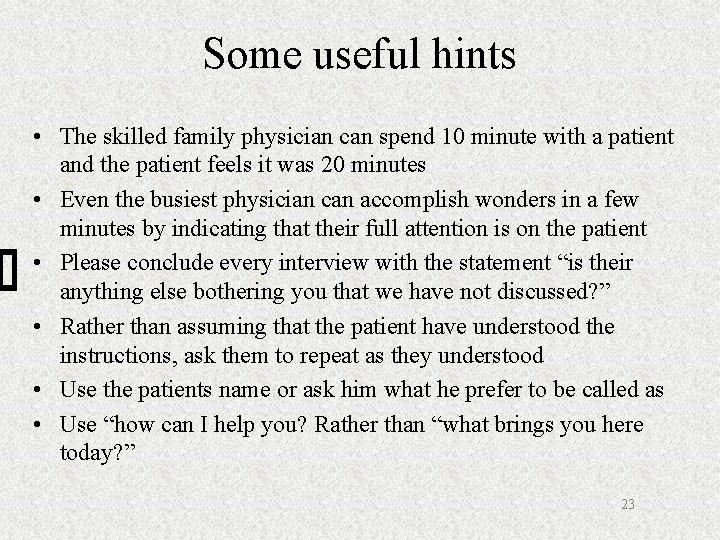
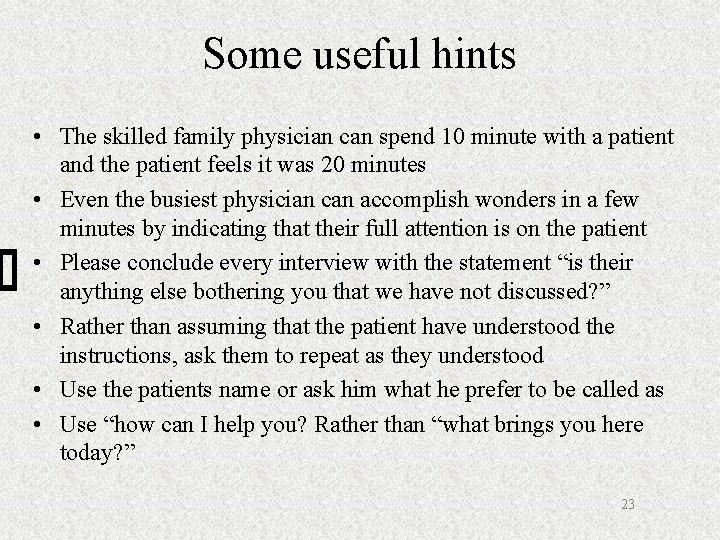
Some useful hints • The skilled family physician can spend 10 minute with a patient and the patient feels it was 20 minutes • Even the busiest physician can accomplish wonders in a few minutes by indicating that their full attention is on the patient • Please conclude every interview with the statement “is their anything else bothering you that we have not discussed? ” • Rather than assuming that the patient have understood the instructions, ask them to repeat as they understood • Use the patients name or ask him what he prefer to be called as • Use “how can I help you? Rather than “what brings you here today? ” 23
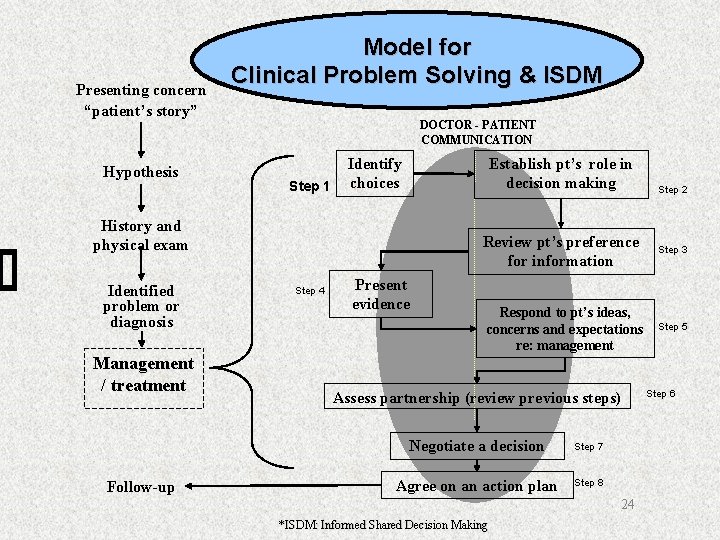
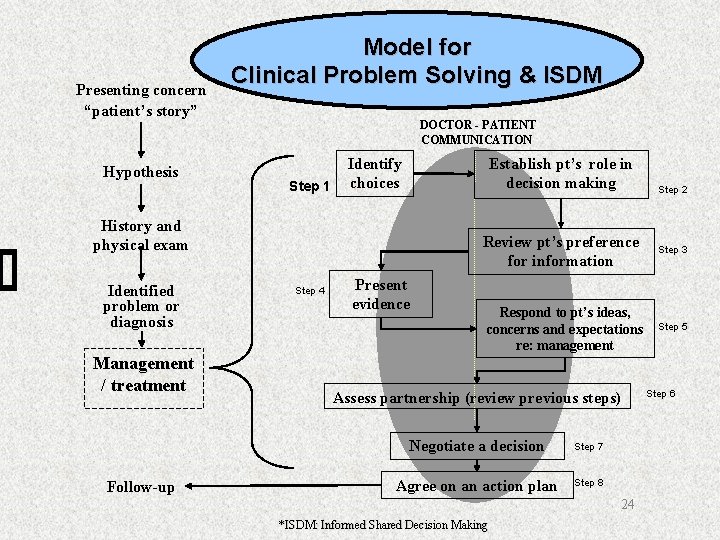
Presenting concern “patient’s story” Hypothesis Model for Clinical Problem Solving & ISDM DOCTOR - PATIENT COMMUNICATION Step 1 Identify choices Establish pt’s role in decision making History and physical exam Identified problem or diagnosis Management / treatment Follow-up Review pt’s preference for information Step 4 Present evidence Respond to pt’s ideas, concerns and expectations re: management Assess partnership (review previous steps) Negotiate a decision Step 7 Agree on an action plan Step 8 24 *ISDM: Informed Shared Decision Making Step 2 Step 3 Step 5 Step 6
Common problems that can lead to poor decisions: • Relationships and roles are unclear • Objective data are inadequate • Values, interests and assumptions are unexplored • Too few options have been considered • Alternatives are unclear • Communication is poor 25
What is a "good" health care decision? o Well informed, supported by the best available evidence, weighs pros and cons, compatible with patient's values and practical (Dow, 1999). 26

Disempowered Not involved No dialogue No Voice in the System Feeling vulnerable No Partnership 27
Empowerment allows our relationships to grow in strength 28
“Coming together is a beginning; keeping together is progress; working together is success. ” Henry Ford 29