SHAHZAD AHMAD M D F A C E




































- Slides: 120
SHAHZAD AHMAD M. D F. A. C. E DIPLOMATE AMERICAN BOARD OF INTERNAL MEDICINE DIPLOMATE AMERICAN BOARD OF ENDOCRINOLOGY/DIABETES AND METABOLISM THYROID INSTITUTE OF UTAH
Thyroid nodule • discrete lesion in the thyroid gland radiologically distinct from the surrounding Thyroid Nonpalpable nodules are called “incidentilomas”
How Common are nodules? • 19 -67 % if ultrasound is done
How common is Thyroid Cancer • 5 -15% depending on risk factors
• Incidence of thyroid cancer has increased more than threefold. • nearly 50% of the increased incidence is from tumors >2 cm, suggesting that a significant number of patients have clinically important tumors.
So you feel a nodule, now what
• Nonpalpable nodules have the same risk of malignancy as palpable nodules with the same size
Who should you send for an ultrasound ? • All patients with a suspected thyroid nodule, nodular goiter, a nodule found incidentally • On (CT) or MRI or on PET scan. Anyone with a first degree relative with thyroid cancer
• Generally, only nodules >1 cm should be evaluated • Any thyroid lesion seen on PET scan should be evaluated by an Endocrinologist
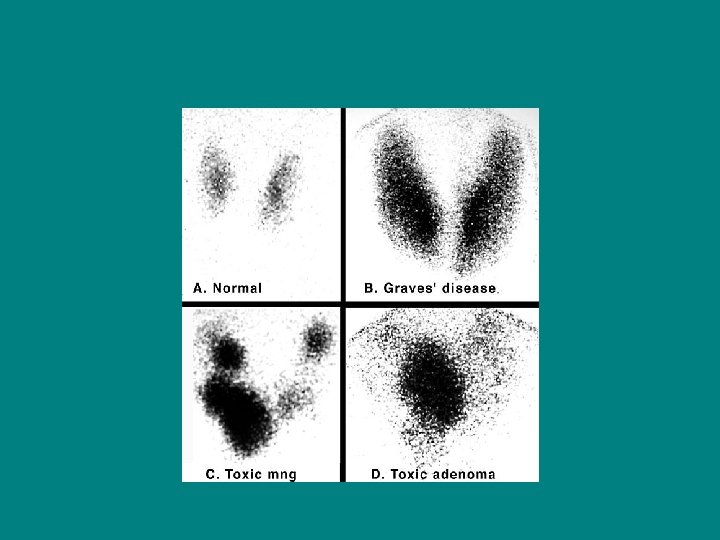
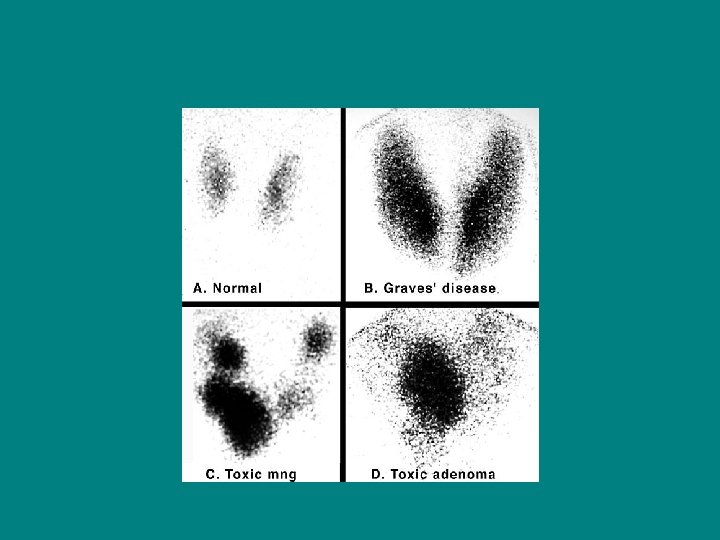
appropriate evaluation of clinically or incidentally discovered thyroid nodule(s) • Measure TSH • If serum TSH is subnormal, radionuclide thyroid I-123 scan

Right Left
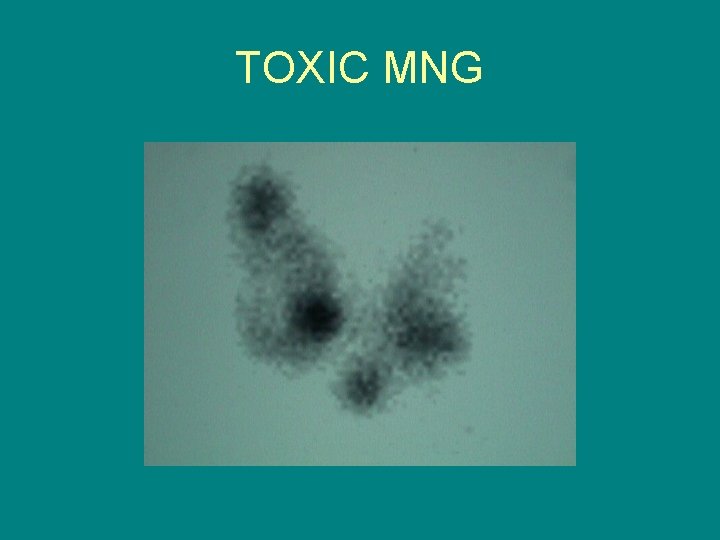
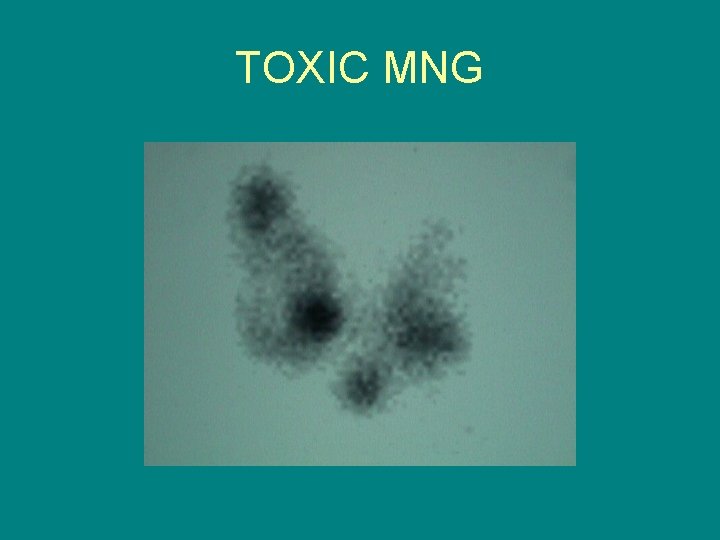
TOXIC MNG
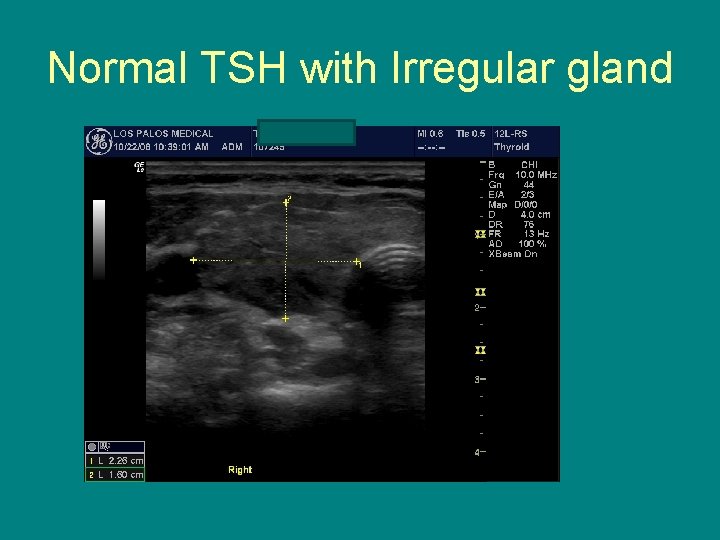
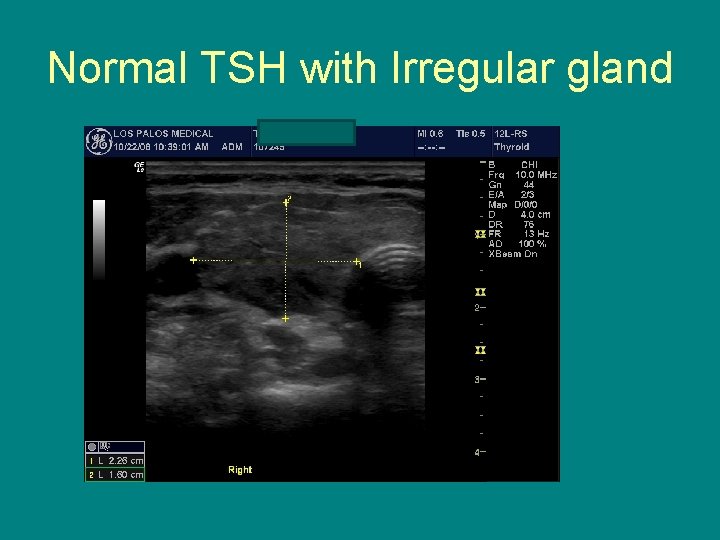
Normal TSH with Irregular gland
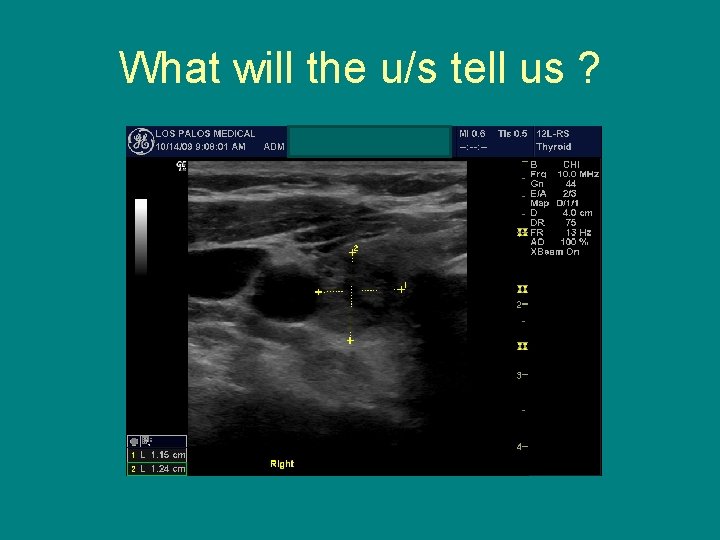
What will the u/s tell us ?

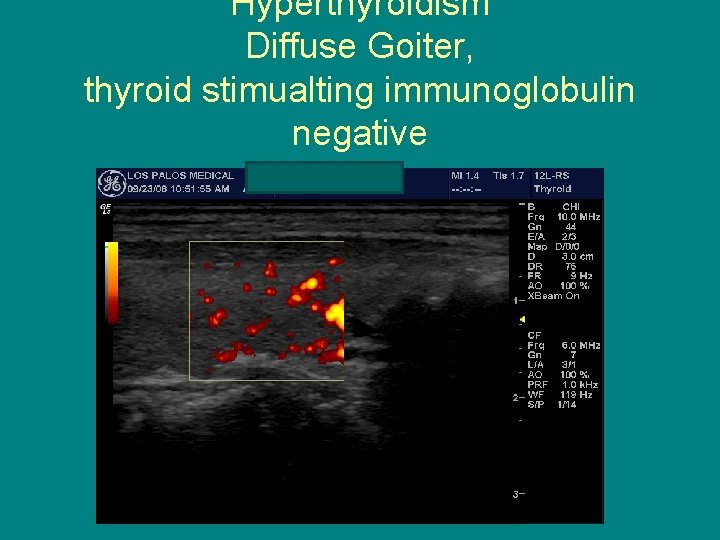
Hyperthyroidism Diffuse Goiter, thyroid stimualting immunoglobulin negative
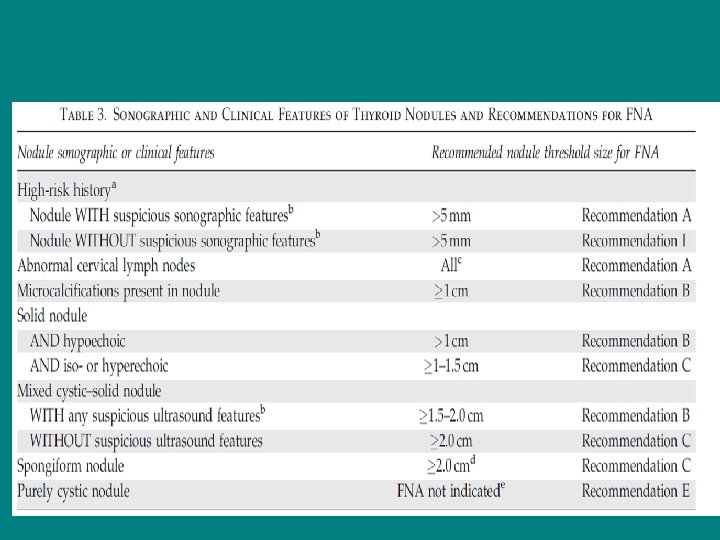
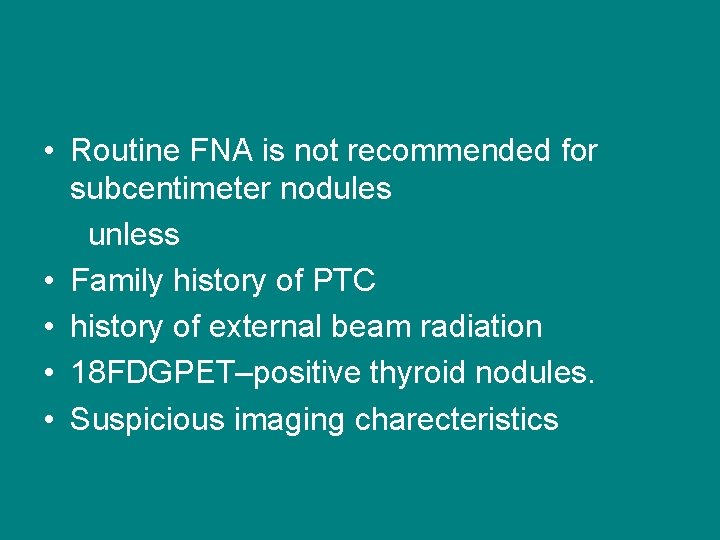
• Routine FNA is not recommended for subcentimeter nodules unless • Family history of PTC • history of external beam radiation • 18 FDGPET–positive thyroid nodules. • Suspicious imaging charecteristics
long-term follow-up of patients with thyroid nodules? • benign nodules require follow-up As there is a 5 % fasle negative rate its actually only 0. 6% for u/s guided ! • which may be even higher with • nodules >4 cm
• reasonable definition of growth is a 20% increase in nodule diameter • serial US examinations 6– 18 months after the initial FNA.

Cytology interpretation • 6 follicular cell groups , 10 -15 cells each • 7% of biopsies can be non diagnostic
Follicular neoplam • Can be seen in 15 -30% of biopsies • If the cytology reading reports a follicular neoplasm, a 123 I • thyroid scan may be considered, if not already done, especially • if the serum TSH is in the low-normal range

Indeterminate cytology/neoplasm • Indeterminate cytology, reported as ‘‘follicular neoplasm’’ or ‘Hurthle cell neoplasm’’ can be found in 15– 30% FNA’s • carries a 10– 30% risk of malignancy

• If the cytology reading reports a follicular neoplasm, • a 123 I thyroid scan may be considered
• The use of molecular markers (e. g. , BRAF, RAS, RET=PTC, or galectin-3) may be considered for patients with indeterminate cytology Recommendation rating: C
Brief Discussion Of molecular markers • BRAF V-600 E, associated with PTC, predicts aggressive course and lymph node mets • Not associated with Radiation! Enviromental toxins?

FOLLICULAR CANCERS • RAS MUTATION seen in approximately 40 percent of follicular cancers • PAX 8 -PPAR gamma 1, seen in 10 percent of Follicular cancers
MOLECULAR ANALYSIS OF INDETERMINATE CYTOLOGY • 1056 indeterminate FNA samples • Assessed for- BRAF V 600 E, RAS, RET/PTC, PAX/PPAR False negative rate at surgery was 5. 9% Finding of RAS mutation increased risk of Thyroid cancer to 80% • J Clin Endocrinol Metab 2011; 96: 3390 -7.
Cystic nodules Recurrent cystic thyroid nodules with benign cytology should be considered for surgical removal or PEI Recommendation B
What is the role of medical therapy for benign thyroid nodules? • Old time Endocrinologists are still using Thyroid hormone to “shrink” thyroid nodules

• 30 YEAR OLD FEMALE WITH MULTI NODULAR GOITER DISCOVERED SEPT 2006 ANTI-TPO 154, ANTI TG AB-368 TSH 7. 36 • FNA CONSISTENT WITH WELL DIFFERENTIATED PAPILARY THYROID CANCER ON THE RIGHT • LEFT INDETERMINATE
Next step(s) ?
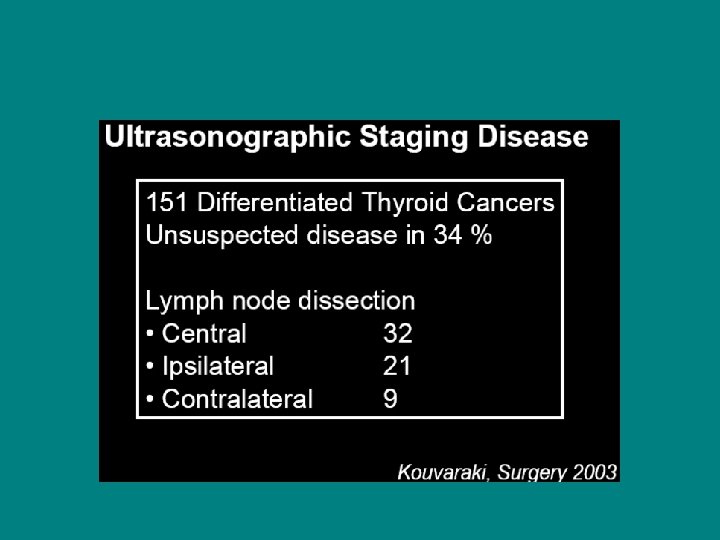
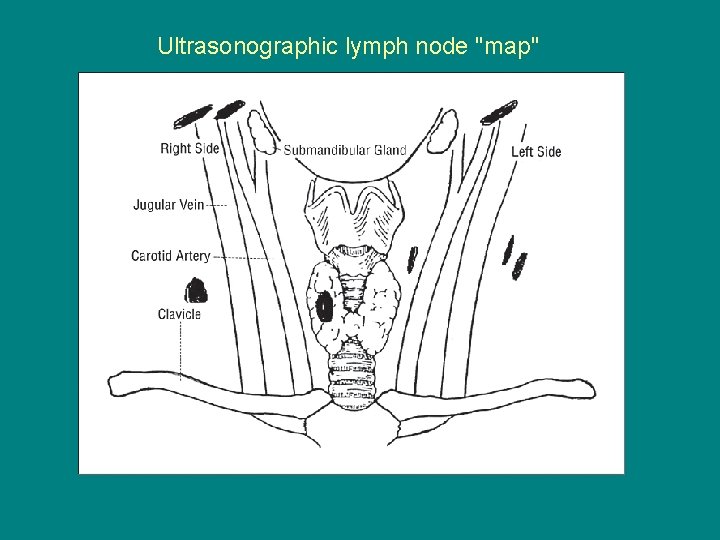
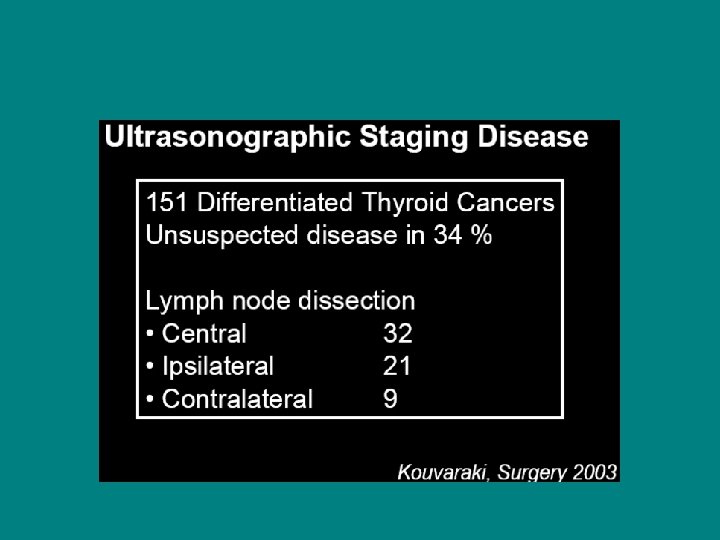
Preoperative Ultrasound ? • Preoperative neck ultrasound for cervical lymph nodes is recommended for all patients undergoing thyroidectomy • Use of CT/MRI/PET not recommended by the American Thyroid Association • Cooper , D. S thyroid 16(2) 109 -141 2006


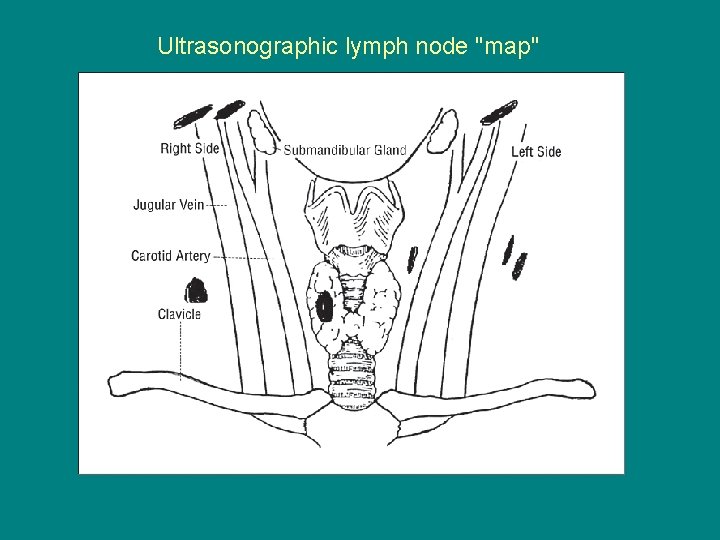
Ultrasonographic lymph node "map"
WHY TOTAL THYROIDECTOMY? • Multiple Foci of PTC are found in thyroid lobes in up to 80 percent of patients • Upto 40 % can be bilateral The only predictor of contra lateral cancer is multifocality in ipsilateral lobe Katoh R, sasaki , cancer 1992 15; 70

What does the A. T. A recommend? • • NTT for bilateral nodules NTT if metastatic lymph nodes seen Age more than 45 Nodule more than 1 cm
• Cervical recurrence occurs in up to 25% of patients with papillary thyroid carcinoma (PTC) • The use of total thyroidectomy for most patients with thyroid carcinoma is supported by the following arguments:
NODE DISSECTION • should be performed if there is clinical evidence of cervical or mediastinal node metastases due to the increased risk of neck recurrence and mortality Am J Med 1994 Nov; 97(5): 418 -28 MAZAFFERI
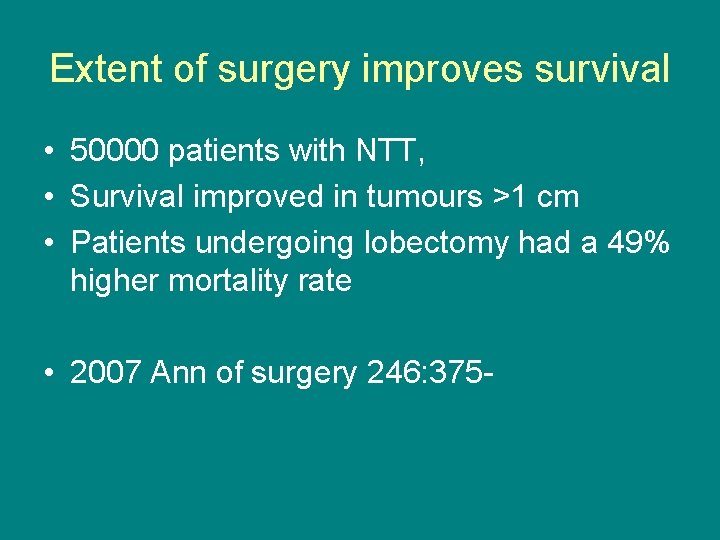
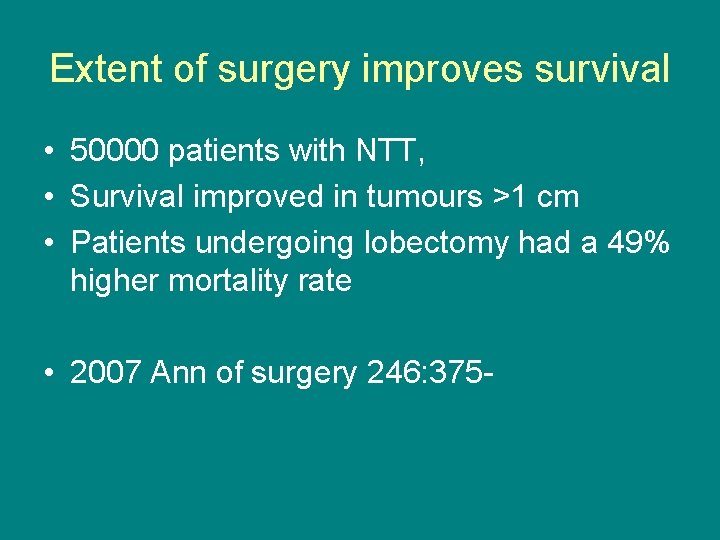
Extent of surgery improves survival • 50000 patients with NTT, • Survival improved in tumours >1 cm • Patients undergoing lobectomy had a 49% higher mortality rate • 2007 Ann of surgery 246: 375 -

Threshold size for lymph node metastases • 5 mm for Pappilary thyroid cancer • 20 mm for Follicular thyroid cancer • Machens et al Cancer 103(11) 2269 -2273



Radioactive iodine • • Indications Benefits Risks Dose?
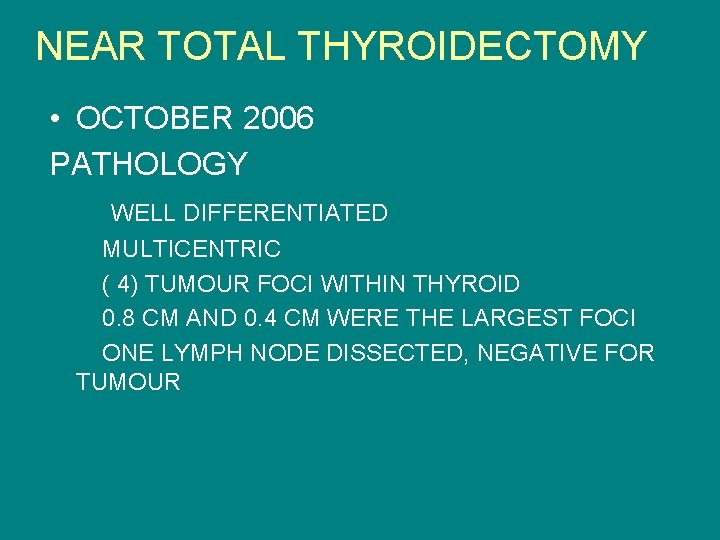
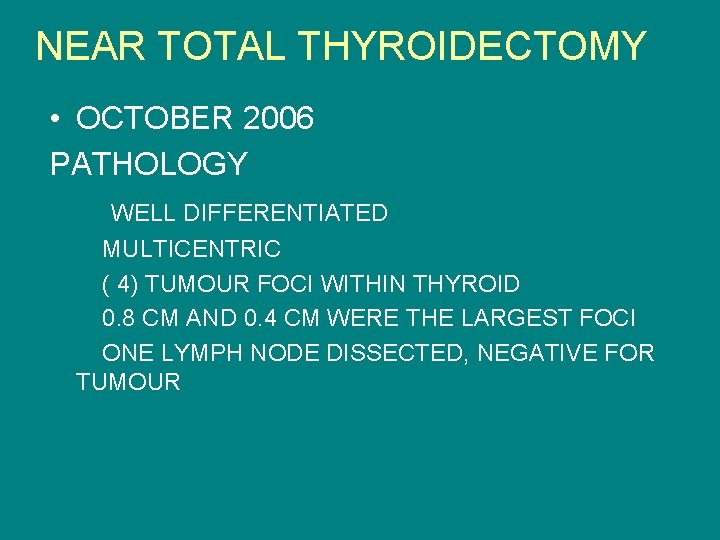
NEAR TOTAL THYROIDECTOMY • OCTOBER 2006 PATHOLOGY WELL DIFFERENTIATED MULTICENTRIC ( 4) TUMOUR FOCI WITHIN THYROID 0. 8 CM AND 0. 4 CM WERE THE LARGEST FOCI ONE LYMPH NODE DISSECTED, NEGATIVE FOR TUMOUR
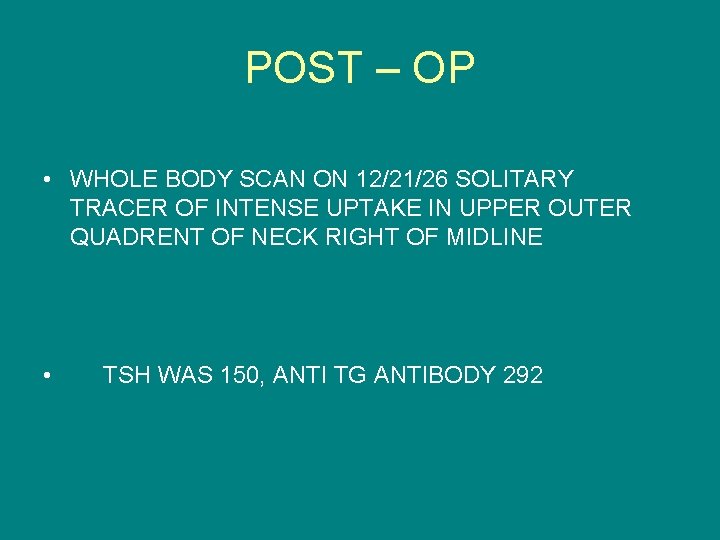
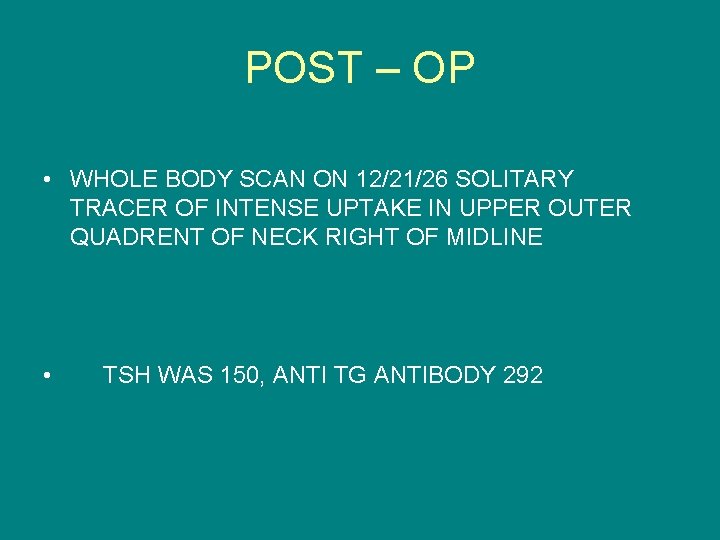
POST – OP • WHOLE BODY SCAN ON 12/21/26 SOLITARY TRACER OF INTENSE UPTAKE IN UPPER OUTER QUADRENT OF NECK RIGHT OF MIDLINE • TSH WAS 150, ANTI TG ANTIBODY 292

REMNANT ABLATION • 12/29/06 WITH 49. 8 MILLICURIE • POST TREATMENT SCAN 1/9/07 • RIGHT NECK UPTAKE WORRISOME FOR METASTATIC FOCUS !!

• HOW DO WE LOOK FOR RESIDUAL/RECURRENT DISEASE ?
• C. T scan neck looking for recurrence/ persistent mass • NEGATIVE !
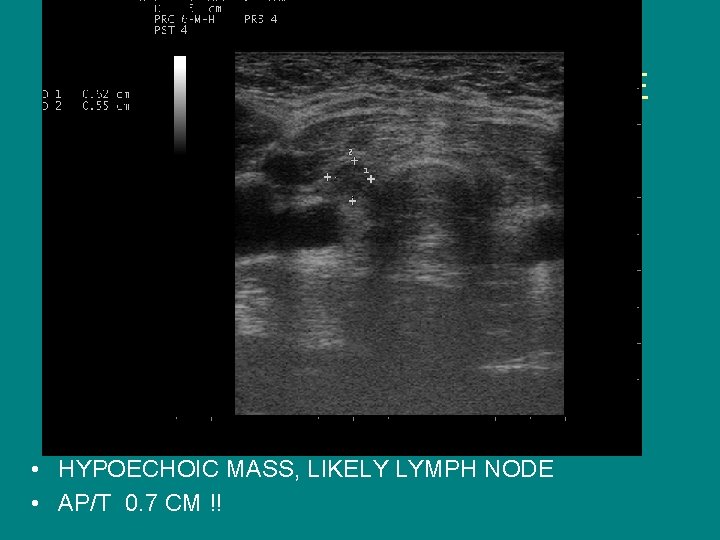
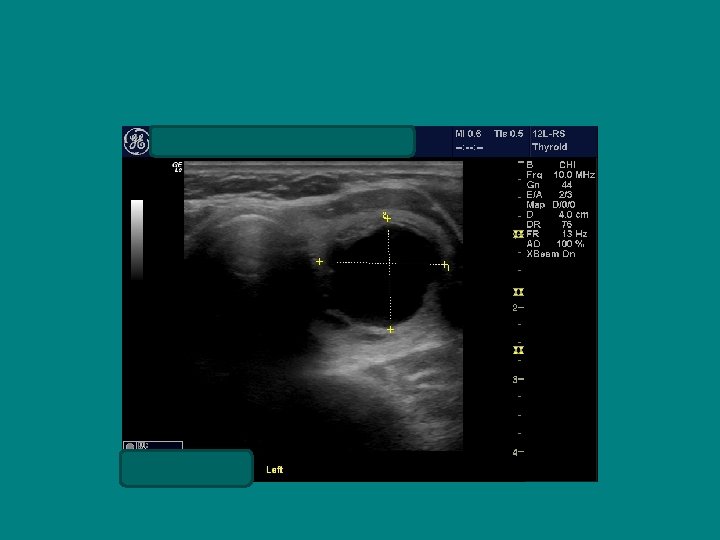
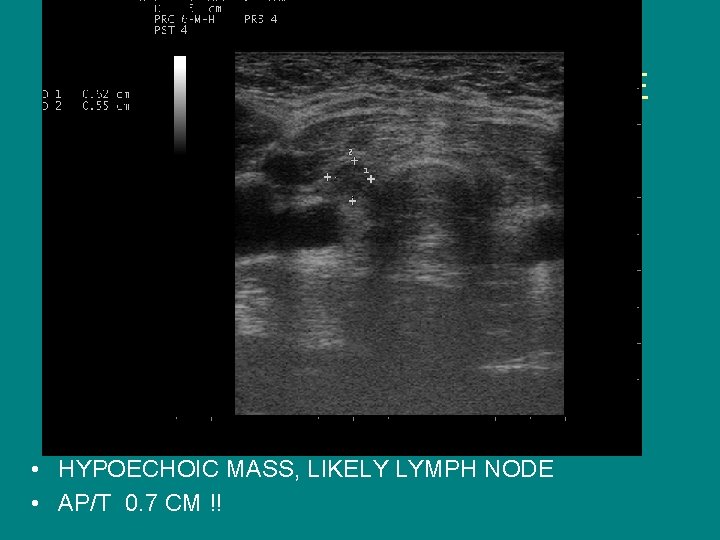
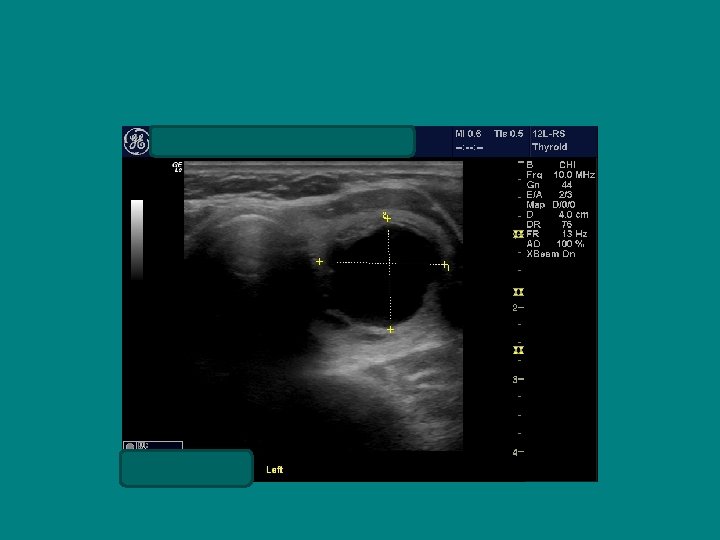
SEARCH FOR RECURRENT/RESIDUAL DISEASE • HYPOECHOIC MASS, LIKELY LYMPH NODE • AP/T 0. 7 CM !!


Now to evaluate this lymph node! • What are my options? a) should we have this resected ? b) check a whole body scan at 6 months c) Biopsy it
Ultrasound characteristics of a benign lymph node Ø Flattened or oval ( AP/T < 0. 5 Ø Echogenic Hilus Ø Hilar Flow on Doppler
Best ultrasound criteria for malignancy • Short to long axis diameter ratio of more than 0. 5 • It has 75 % sensitivity, 81 % specificity • 79 % accuracy

Does size help predict a malignant lymph node? • NO ! • Size doesn’t matter, • Border doesn’t help either
What's the Best Way to Detect Cancer Recurrence After a Thyroidectomy?
• Cervical ultrasonography is the best way to detect early recurrent disease • Albert B. Lowenfels, MD, Professor of Surgery Medscape General Surgery. 2007;
How sensitive is ultrasonography? • Operator dependent • Frasoldati et al reported cytology to be 84% sensitive and if combined with TG washout 95. 6 % sensitive
Cervical Ultrasonography, A. T. A recommends cervical ultrasound at 6 and 12 months after surgery and then annually
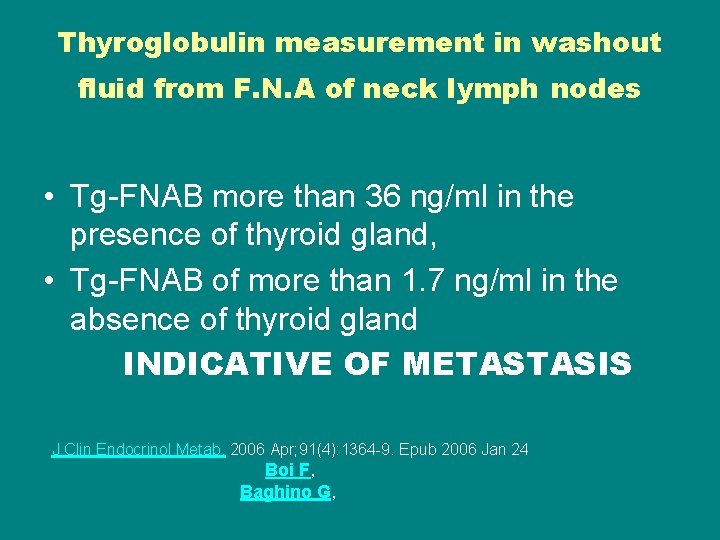
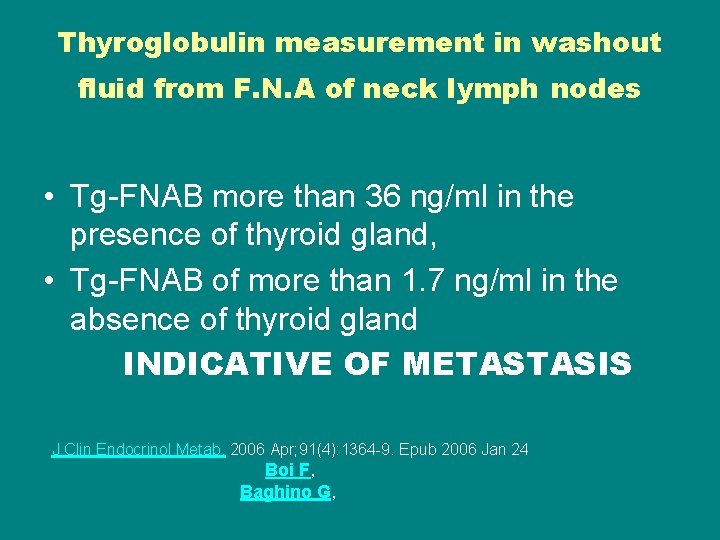
Thyroglobulin measurement in washout fluid from F. N. A of neck lymph nodes • Tg-FNAB more than 36 ng/ml in the presence of thyroid gland, • Tg-FNAB of more than 1. 7 ng/ml in the absence of thyroid gland INDICATIVE OF METASTASIS J Clin Endocrinol Metab. 2006 Apr; 91(4): 1364 -9. Epub 2006 Jan 24 Boi F, Baghino G,
• Clinical performance of Tg-FNAB appears to be not substantially affected by Tg. Ab J Clin Endocrinol Metab. 2006 Apr; 91(4): 1364 -9. Epub 2006 Jan 24 Boi F, Baghino G,
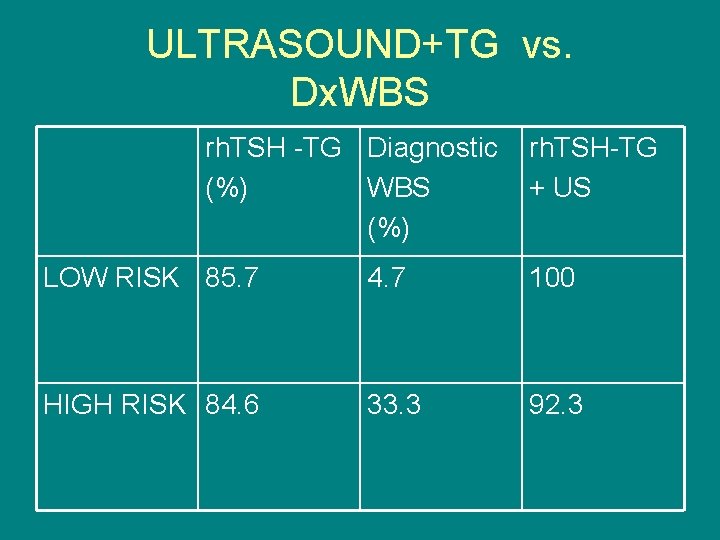
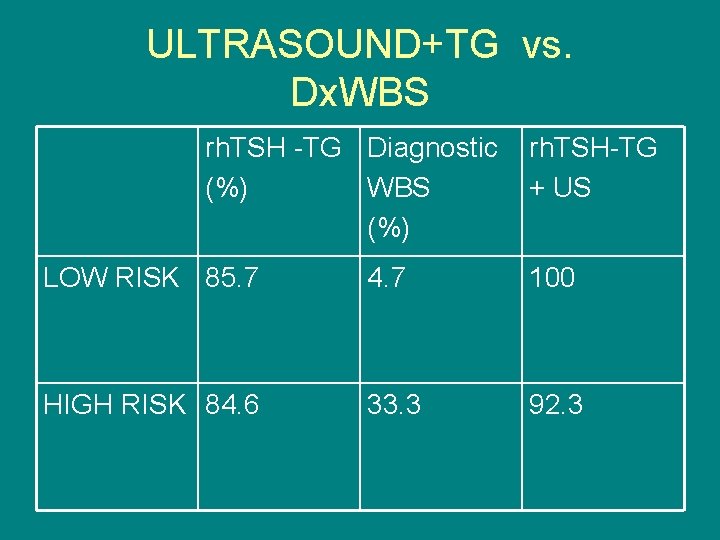
ULTRASOUND+TG vs. Dx. WBS rh. TSH -TG Diagnostic (%) WBS (%) rh. TSH-TG + US LOW RISK 85. 7 4. 7 100 HIGH RISK 84. 6 33. 3 92. 3

rh. TSH TG with neck ultrasonography has the highest sensitivity in monitoring differentiated thyroid cancer ! • Pacini, F J clin Endocrinol, Met 2003
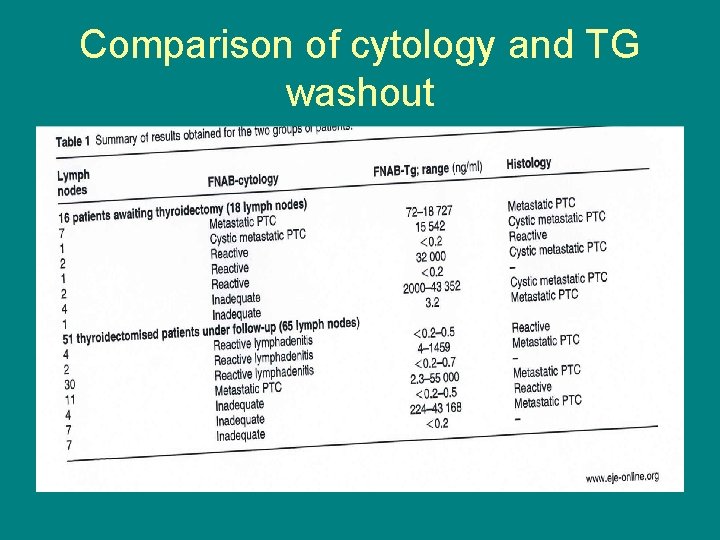
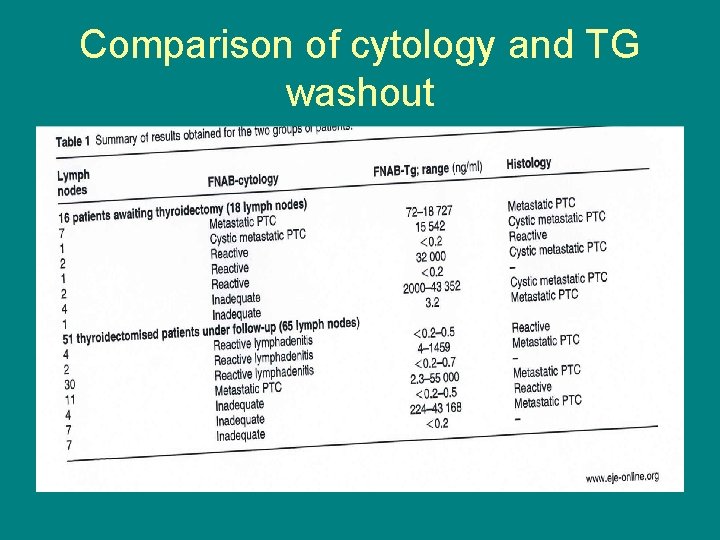
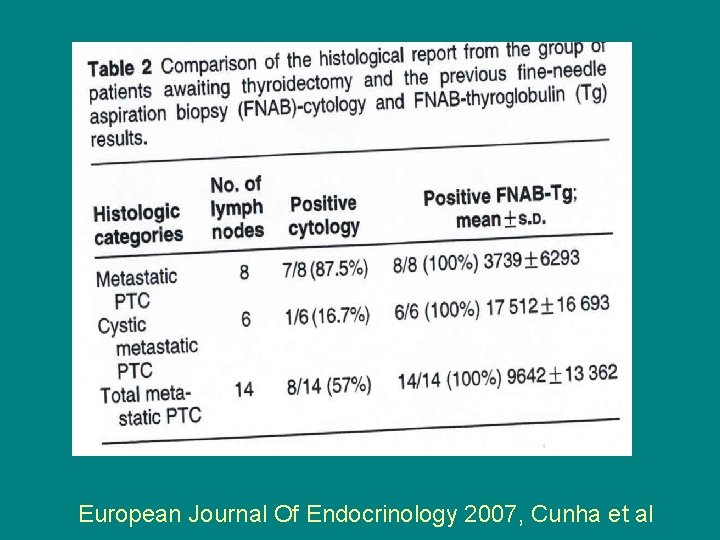
Comparison of cytology and TG washout
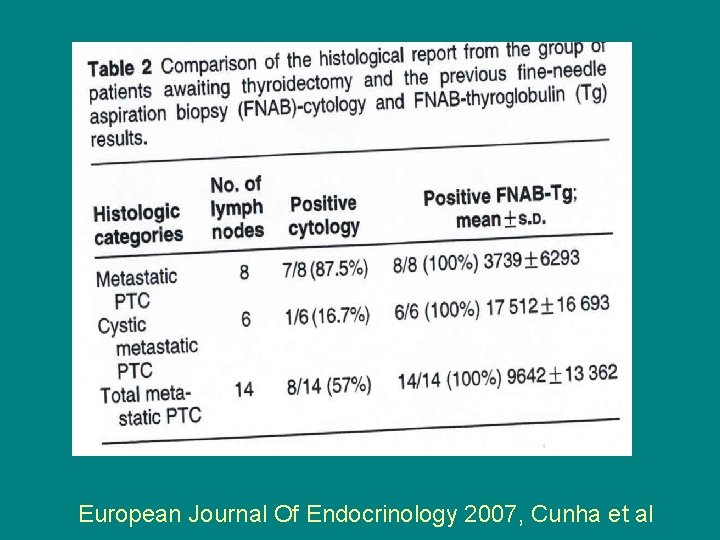
European Journal Of Endocrinology 2007, Cunha et al

“The data will be tortured untill they confess”

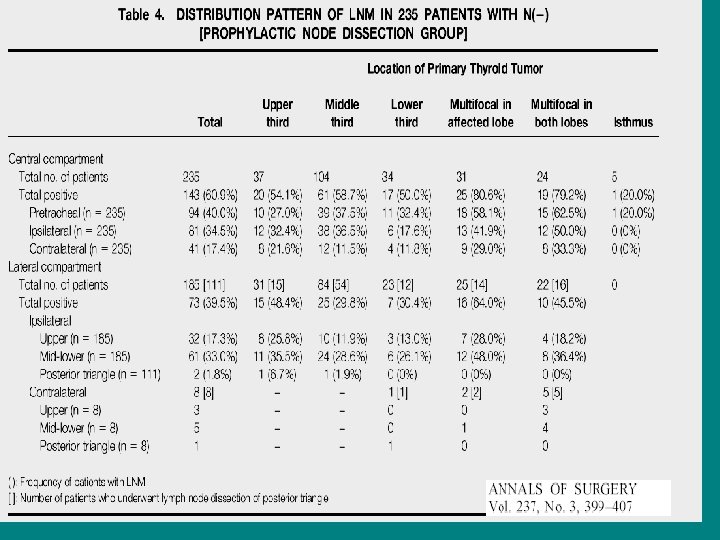
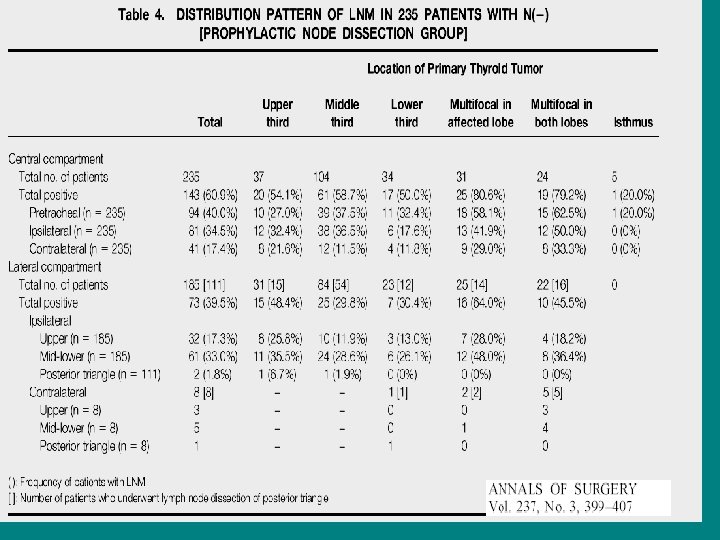
WHAT DOES THE DATA REALLY SAY • Both Central and ipsilateral Lymph Nodes are affected commonly even with small PTCs • Skip lesions ( involvement of lateral lymph nodes without central involvement) is RARE

• PATIENTS WITH MULTIFOCAL TUMOURS MUCH MORE LIKELY TO HAVE LYMPH NODE METASTASIS • MORTALITY HIGHER IN PATIENTS WITH MULTIFOCAL INTRATHYROIDAL TUMOUR • AMERICAN JOURNAL OF MEDICINE 1997 VOL 97 MAZZAFERI ET AL
CONCLUSIONS (OPINION) • PRE-OP NECK ULTRASOUND TO EVAULATE COTRALATERAL LOBE AND LYMPH NODES (AACE RECOMMENDATION LEVEL B) • BIOPSY SUSPICIOUS LYMPH NODES (CYTOLOGY AND TG-WASHOUT) BASED ON MORPHOLOGY TO HELP SURGEONS DECIDE ABOUT NECK DISSECTION
• MULTIFOCAL MICRO PTC MORE LIKELY TO HAVE LYMPH NODE METS • PROBABLY SHOULD HAVE CENTRAL COMPARTMENT DISSECTION • THIS WILL IMPACT RECURRENCE • NO LONG TERM OUTCOMES DATA AVAILABLE

• We should concentrate on mid-lower central compartment to avoid recurrence IN HIGHER RISK PATIENTS
DID ALL THIS SURGERY AFFECT LONG TERM OUTCOME? • Recurrence was followed for 53 months in a japanese study • One group of patients had prophylactic lymph node resection, the other only therapeutic • Recurrence rate was 16. 7 % lower in the group with therapeutic lymp node resection • Patients with no palpable lymph nodes who had prophylactic dissection had a much lower recurrence rate- 0. 4 %
Case 2 Ø 32 y/o male with Papillary thyroid cancer 1999 ØNTT pathology showed 4. 5 x 2. 6 x 2. 0 cm mass ØMulti focal ØMultiple lymph nodes positive, bilaterally ØT 3 N 1 B MX
Remnant Ablation • 152 m. Ci dose of I-131 given 12/1999 • Lost to follow up until 2006 • Repeat WBS and PET negative
2007 • On synthroid 225 mcg • TSH 0. 30 • Thyroglobulin AB 0. 7 IU/ML (range 0 to 14. 4) • Thyroglobulin 5. 4 ng/ml
Looking for disease • Repeat Surveillance WBS scan negative

NOW WHAT ? • Role of ultrasound
WHERE AND WHEN DOES RECURRECE OCCUR • 79 % RECURRENCE OCCURS IN THE NECK • 74 % OF RECURRENCE IS IN THE LYMPH NODES • TIME TO RECURRENCE USUALLY VARIES, SOME CASES RECUR AT 7 -10 YEARS AMERICAN JOURNAL OF MEDICINE 1997 VOL 97 MAZZAFERI ET AL

HIGH SERUM THYROGLOBULIN NEGATIVE IMAGING ! LIKELY DUE TO A) CERVICAL LYMPH NODE METASTASIS B) METASTASIS TOO SMALL TO BE SEEN ON Dx. WBS OR Rx. WBS

• Higher Thyroglobulin level means a higher chance of detection of mets/mass • In patients with TG > 5 after rh. TSH ultrasound picked up neck masses/mets in 67 % patients
Cystic metastatic lymph nodes • 20 % of patients with Thyroid Cancer present with the sole finding of an abnormal lymph node • Cystic metastasis cause most of the nondiagnostic lymph node biopsies • Use a THYROGLUBULIN washout to prevent this from happening !
POST THYROIDECTOMY NECK Ø MEDIAL MOVEMENT OF CAROTID AND JUGULAR Ø Thyroid bed is filled with HYPER echoic connective tissue Ø This demarcates it from recurrence or metastatic lymph nodes which will be HYPO echoic



AP/T 0. 79/1. 45= 0. 54 !




PET/CT IN TG +ve, SCAN NEGATIVE PATIENTS • which is better, PET scan OR PET/CT Palmedo et al Journal of Nuclear Medicine Vol. 47 No. 4 616 -624
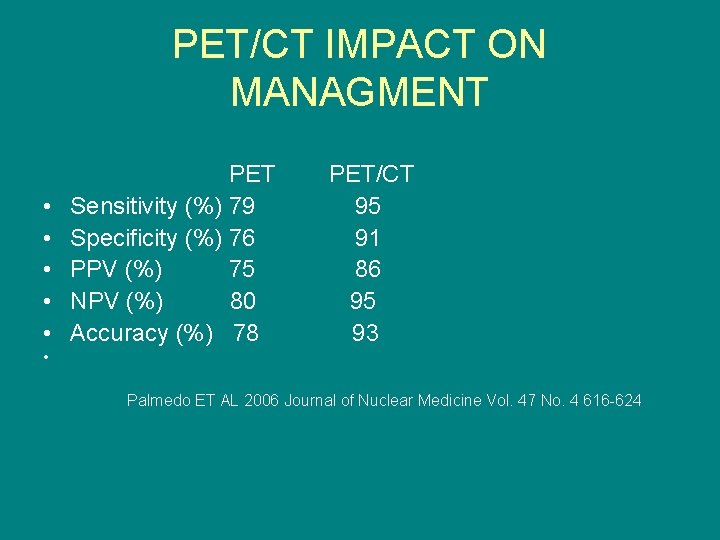
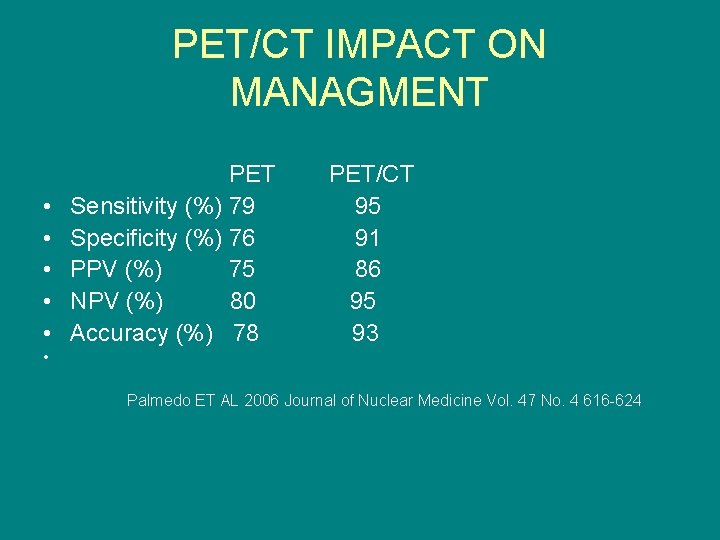
PET/CT IMPACT ON MANAGMENT • • • PET Sensitivity (%) 79 Specificity (%) 76 PPV (%) 75 NPV (%) 80 Accuracy (%) 78 PET/CT 95 91 86 95 93 • Palmedo ET AL 2006 Journal of Nuclear Medicine Vol. 47 No. 4 616 -624
Limitations • PET/C. T will miss small lymph nodes which might be malignant
PET/CT with a suppressed TSH vs. rh. TSH stimulated PET/CT • Which is better?
• Higher Thyroglobulin level means a higher chance of detection of mets/mass • In patients with TG > 5 after rh. TSH ultrasound picked up neck masses/mets in 67 % patients

Elastography ! • Imaging Modality to map elastic properties of tissue • Compression is done and strain distributed is checked on ultrasound • Results are displayed on an elastogram Lyschick et al, Radiology april 2007
• Stiff objects appear dark and flexible objects are bright ! Neck lymph nodes are in a great position for this technique to be applied Lyschick et al, Radiology april 2007

How accurate is it ? Elastography • 98 % specificity 92% accuracy Other ultrasound criteria • AP/ T ratio, vascularity, calcification 81 % specific 79% Lyschick et al, Radiology April 2007
Metastatic lymph nodes why they matter
PYTHIAN LYMPH NODES • Pythia was the priestess of Delphi , whose utterence was ambiguous and interpretable in different ways what happens to these lymph nodes • some may grow and become significant • Some may metastasize • Some may remain dormant and surgery not needed
AFTER thyroidectomy and RAI ablation how often do patients have residual disease?
• 20 - 25 % have disease 1 or more years after thyroidectomy and RAI ! • Rate of clinical lymph node recurrence is 13 %
• Given a 20 -25 % rate of PERSISTENT DISEASE And a 13 % risk of gross lymph node recurrence, THIS IMPLIES that one out of every 2 patients with Pythian Lymph nodes will eventually have a gross clinical recurrence
• CUMULTATIVE RISK OF death due to papillary thyroid cancer after diagnosis of neck nodal metastasis was 10 %
Can adverse outcomes from Malignant lymph nodes be prevented? • Because of a high rate of recurrent LN mets despite initial surgery and RAI its thought that pre op u/s might detect lymph node mets that wouldn’t be addressed otherwise • ATA recommends pre op u/s for all thyroid cancer patients
How often can patients with neck lymph node mets be rendered disease free ? • It ranges between 19 to 46 % • Probably around 20% of patients can be rendered disease free with re-operation for PYTHIAN LYMPH NODES with a low but possible risks of operative complications
• NOT CLEAR HOW MANY CLINICAL RECURRENCES THIS APPROACH OF RESECTING CANCEROUS LYMPH NODES PREVENTS • SURVIVAL BENEFIT ALSO ISNT CLEAR
TAKE HOME POINTS • Pre-operative ultrasound is essential because it guides surgery and decision to use remnant ablation even in “low risk” patients • We don’t need a WBS for low risk patients if stimulated TG is negative and ultrasound is normal
• TG positive scan negative patients should be evaluated with an ultrasound • Ultrasound and needle biopsy TG washout is the most sensitive modality to evaluate recurrence
QUESTIONS/COMMENTS?