SEXUALLY TRANSMITTED DISEASES Lynne D Feldman MD MPH


















- Slides: 70

SEXUALLY TRANSMITTED DISEASES Lynne D. Feldman, MD, MPH – District Health Director Elsie Napier, RN, FNP – District Program Manager Brenda Mims, RN – Infectious Disease Coordinator
South Health District, 8 -1 STD Presentation to Valdosta State University / Student Health Brenda Mims, RN – Infectious Disease Coodinator
DCH Mission ACCES S Access to affordable, quality health care in our communitie s RESPONSIB LE Responsible health planning and use of health care resources HEALTH Y Healthy behaviors and improved health outcomes
DCH Initiatives FY 2009 and FY 2010 FY 2009 FY 2010 Medicaid Transformation Health Care Consumerism Financial & Program Integrity Health Improvement Solutions for the Uninsured Workforce Development Customer Service Peach. Care for Kids. TM Program Stability Emergency Preparedness Customer Service
Disclosure Statements • To obtain nursing contact hours for this session, you must be present for the entire hour and complete an evaluation. • Neither the planners of this session nor I have any financial relationship with pharmaceutical companies, biomedical device manufacturers, or corporations whose products and services are related to the vaccines we discuss. • There is no commercial support being received for this event. • The mention of specific brands of vaccines in this presentation is for the purpose of providing education and does not constitute endorsement. • The GA Immunization Program utilizes ACIP recommendations as the basis for this presentation and for our guidelines, policies, and recommendations. • For certain vaccines this may represent a slight departure from or off-label use of the vaccine package insert guidelines.
Goal • To promote Sexually Transmitted Disease awareness, prevention and education.
Objectives • After the completion of this presentation participants should be able to: 1. 2. 3. 4. 5. 6. 7. Define Sexually Transmitted Diseases (STDs); Describe how STDs are transmitted; Name at least three of the most commonly diagnosed STDs; Identify signs and symptoms of STDs; Understand the effects of STDs on pregnancy; Describe recommended CDC treatments for STDs; Understand the STD reporting and follow-up process.
Sexually Transmitted Diseases (STDs) • Definition – An infection passed during sex by means of sexual contact, including vaginal intercourse, oral sex, and anal sex. • Until the 1990’s these illnesses/diseases were commonly known as venereal diseases. Veneris – the Latin name for Venus, who is considered the Roman goddess of love. • Can have no symptoms • Infect the following areas: – Mouth – Rectum – Sex organs ( vagina, vulva, penis, testes)
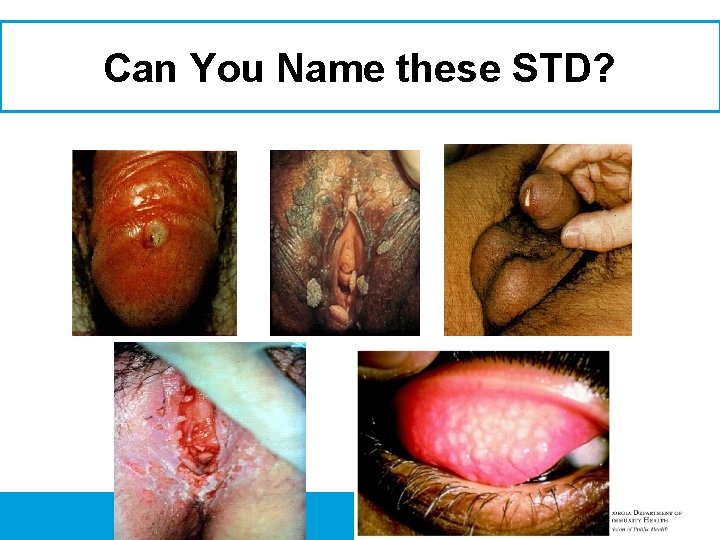
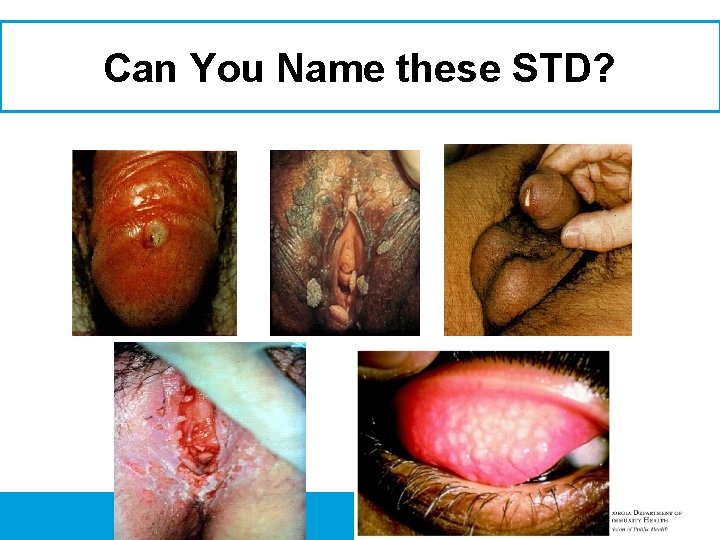
Can You Name these STD?

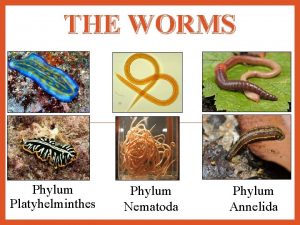
STDs • • CHLAMYDIA GONORRHEA Genital Warts HEPATITIS A, B. & C Bacterial Vaginosis Scabies Epididymitis Nongonococcal Urethritis • Pediculosis Pubis • • • GENITAL HERPES/HPV HIV/AIDS SYPHILIS Trichomoniasis “Trich” Genital & Perianal Warts Lymphogranuloma Venereum • Vulvovaginal Candidiasis • Pelvic Inflammatory Disease

Chlamydia • What is Chlamydia? – Sexually transmitted infection – A common STD caused by the bacterium Chlamydia Trachomatis – Can be transmitted through vaginal, anal or oral sex as well as to a child from the mother during birth – Can cause sterility • Mode of transmission – Spread during vaginal, anal or oral sex with someone who has Chlamydia • Symptoms – May present as non-gonococcal urethritis (NGU) syndrome in males or mucopurulent cervicitis syndrome in females – Known as the “silent” disease – Abnormal vaginal bleeding (between menstrual periods) – Burning sensation during urination – Back pain and/or pain during intercourse • Treatment – Antibiotic (Usually Azithromycin or Doxyclycline) – Partner should also be treated to prevent re-infection • Prevention – Abstinence – Condoms – Monogomy
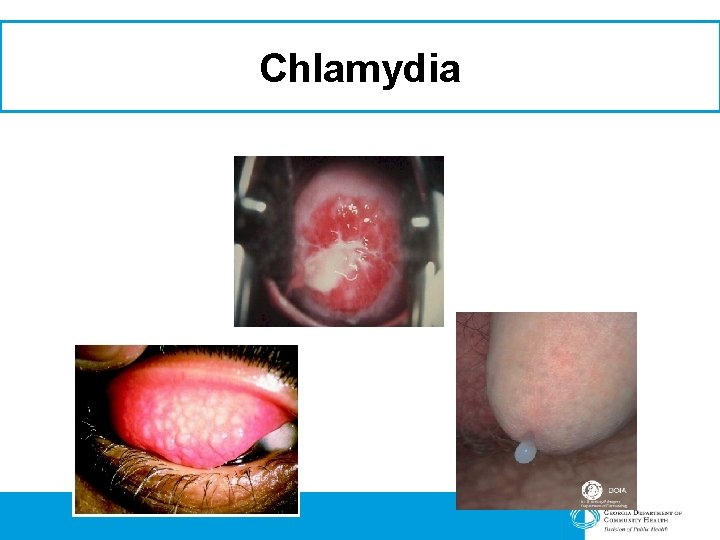
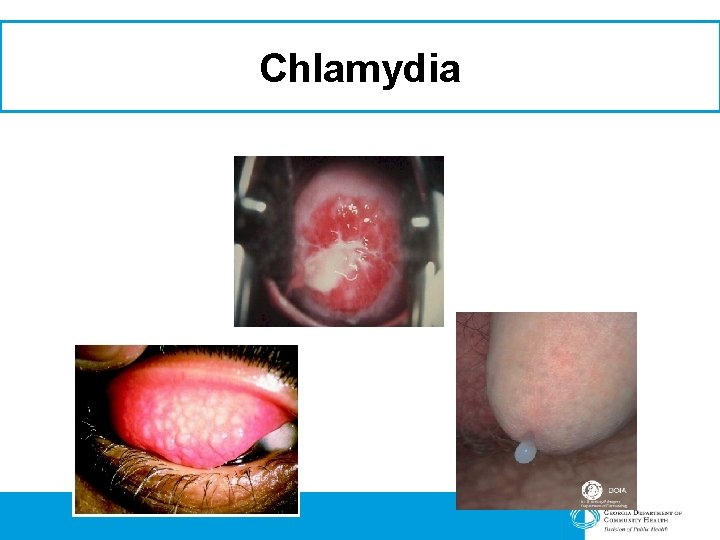
Chlamydia

Chlamydia
Treatment For Chlamydia • Chlamydia can be treated with the following medications: – Azithromycin – Doxyclycline – Amoxicillin – Erythromycin

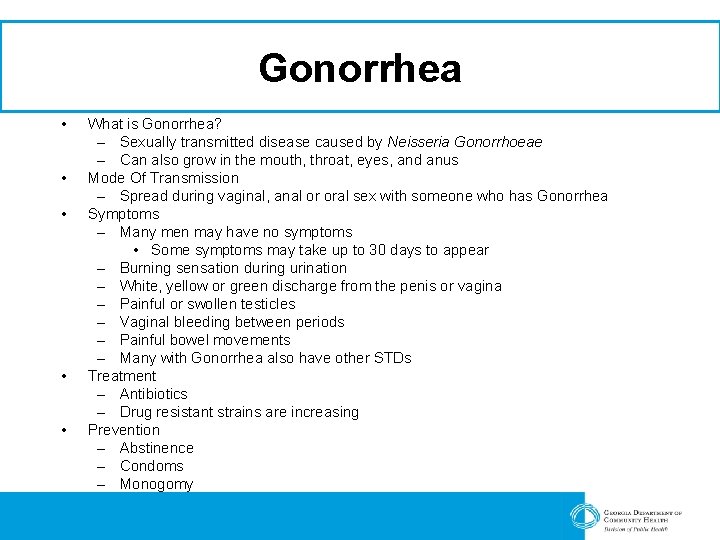
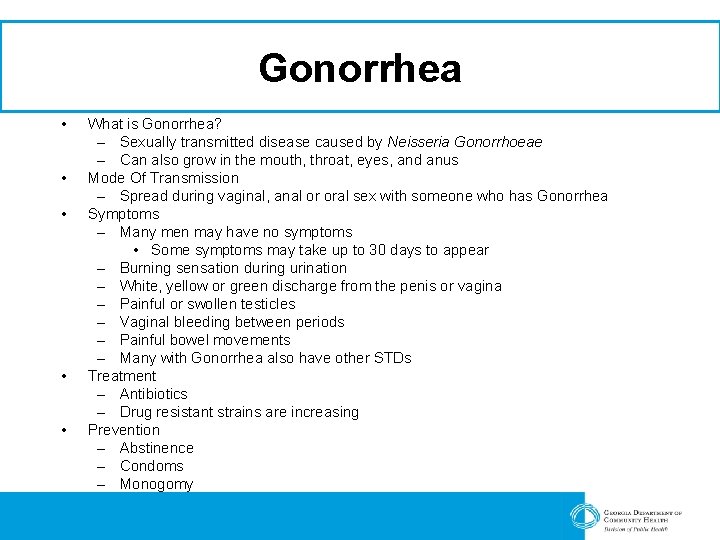
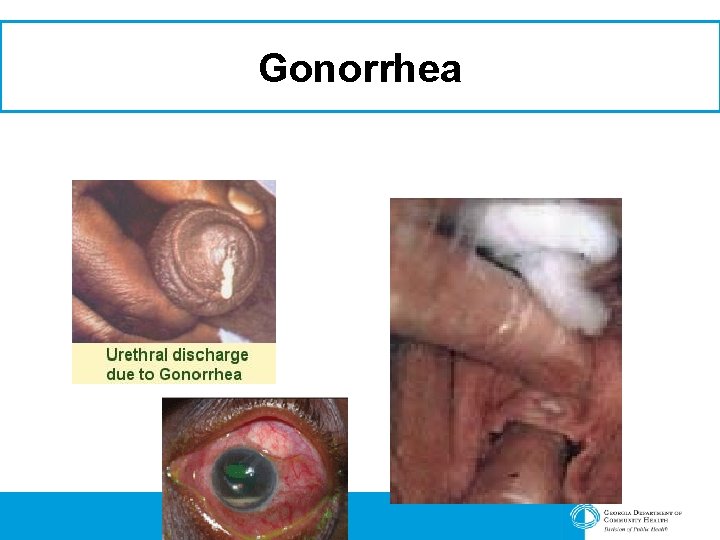
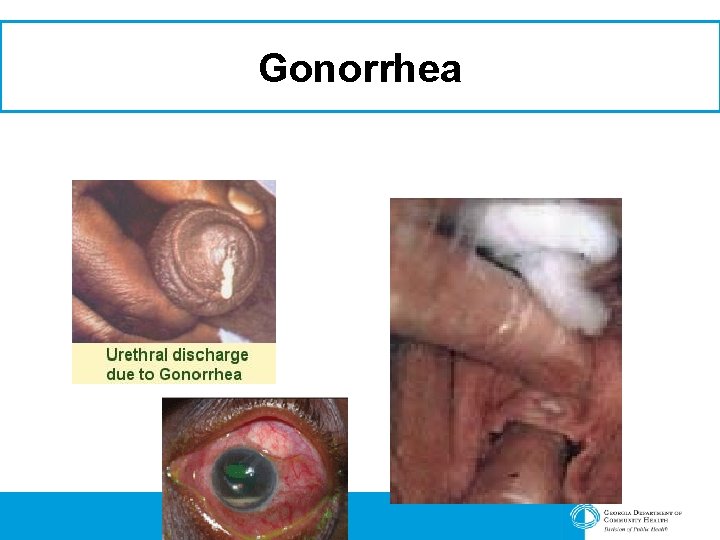
Gonorrhea • • • What is Gonorrhea? – Sexually transmitted disease caused by Neisseria Gonorrhoeae – Can also grow in the mouth, throat, eyes, and anus Mode Of Transmission – Spread during vaginal, anal or oral sex with someone who has Gonorrhea Symptoms – Many men may have no symptoms • Some symptoms may take up to 30 days to appear – Burning sensation during urination – White, yellow or green discharge from the penis or vagina – Painful or swollen testicles – Vaginal bleeding between periods – Painful bowel movements – Many with Gonorrhea also have other STDs Treatment – Antibiotics – Drug resistant strains are increasing Prevention – Abstinence – Condoms – Monogomy
Gonorrhea
Treatment For Gonorrhea • Gonorrhea can be treated with the following medications: – Ceftriaxone (Rocephin) – Cefixime – Azithromycin – Doxycycline – Erythromycin

Genital Warts • What is Genital Warts – Small, sexually transmitted growths that is caused by Human Papillona Virus – Flesh-colored (look like miniature cauliflower florets) – Can be visible in the vagina, urethra, cervix, vulva, penis, anus • Mode of Transmission – Spread during vaginal, anal or oral sex, and sometimes by genital touching, with someone who has genital warts • Symptoms – The virus lives in the skin or mucous membranes – Can cause no symptoms • Treatment – Can be removed – No Cure (will have the virus for the rest of your life) • Prevention – Condoms – Monogamy

Genital Warts
Treatment For Genital Warts • Genital Warts can be treated but not cured: – Podofilox – Imiquimod – Trichloroacetic Acid – Podophyllin – Gardasil (HPV Vaccine)

Hepatitis • What is Hepatitis? – A disease that damages the liver – Caused by a virus – Hepatitis A, B, C are most common • Hepatitis A – Passed in human feces, food and water – Symptoms: Jaundice, Fatigue, Abdominal Pain, Diarrhea, Nausea • Hepatitis B – Passed through blood, saliva, semen, or vaginal fluids (anal or oral sex), from mother to baby during birth, sharing needles to inject drugs or for any other reason – Symptoms: Persistent flu-like feelings, tiredness, jaundice, dark urine, light-colored bowel movements • Hepatitis C – Passed through blood, from mother to baby during birth, during sex (not common) • Hepatitis B & C can become chronic – Can cause cirrhosis (scarring) of the liver – Liver cancer • Prevention – Hepatitis A & B vaccine available – Hepatitis C – No Vaccine but medication available to prevent further liver damage

Hepatitis • Picture of a healthy liver • Effects of hepatitis on the liver
Treatment For Hepatitis A, B & C • Hepatitis A – No treatment – There is a vaccine to prevent Hepatitis A – Goes away by itself in 2 -6 months • Hepatitis B – Yes / Treatment isn’t always successful – There is a vaccine that should be started at birth – all ages 0 -18 should be vaccinated • Hepatitis C – Treatment with antivirals (interferon – most common) to manage and slow disease progression – There is no vaccine for Hepatitis C
Perinatal Hepatitis B
Perinatal Hepatitis B Prevention Program • Program Goals – Ensure all pregnant women are screened for HBs. Ag at their initial prenatal screening panel as standard of care – Be sure Public Health conducts case investigations on all positive HBs. Ag pregnant women – Confirm 90% of all infants born to HBs. Ag positive women receive HBIG and the first dose of Hep B vaccine within 12 hours of birth – Ensure that 90% of all infants born to HBs. Ag positive women receive the second dose of vaccine at 1 -2 months of age – Ensure that 80% of all infants born in Georgia to HBs. Ag positive women are tested at 9 months to 18 months of age for HBs. Ag and Hepatitis B surface antibodies (Anti-HBs)

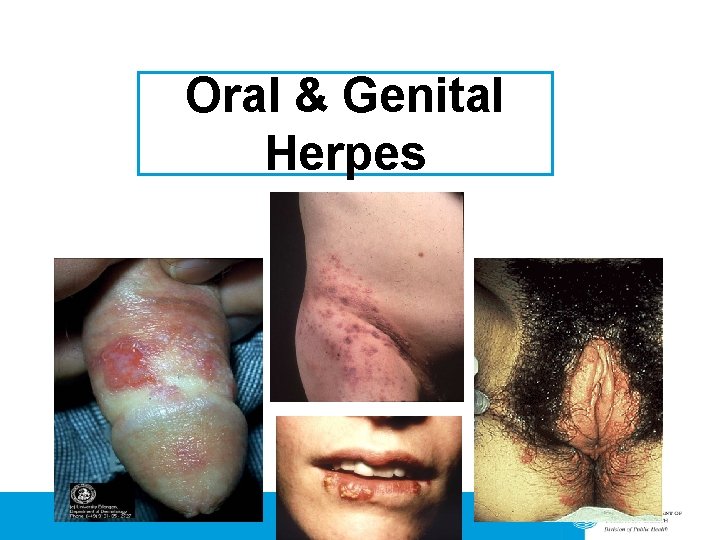
Genital Herpes • • What is herpes? – A viral infection characterized by recurring vesicular and ulcerative lesions on the genitals or adjacent areas that heal spontaneously without scarring. – Some severe cases of first episode infection last an average of 12 days and aseptic meningitis or generalized symptoms due to viremia may occur. Mode of transmission – Spread through vaginal, anal and oral sex – sometimes by genital touching with someone who has herpes Symptoms – Oral Herpes • Cold sores or “fever blisters” – Genital Herpes • Most have no symptoms • Most common symptoms – cluster of blistery sores – usually on the vagina, vulva, cervix, penis, buttocks or anus • May last several weeks – may return in weeks, months or years • Fever, blisters, burning feelings if urine flows over sores, itching, open sores Prevention – Abstinence – Do not have sexual contact during outbreaks – Use condoms between outbreaks
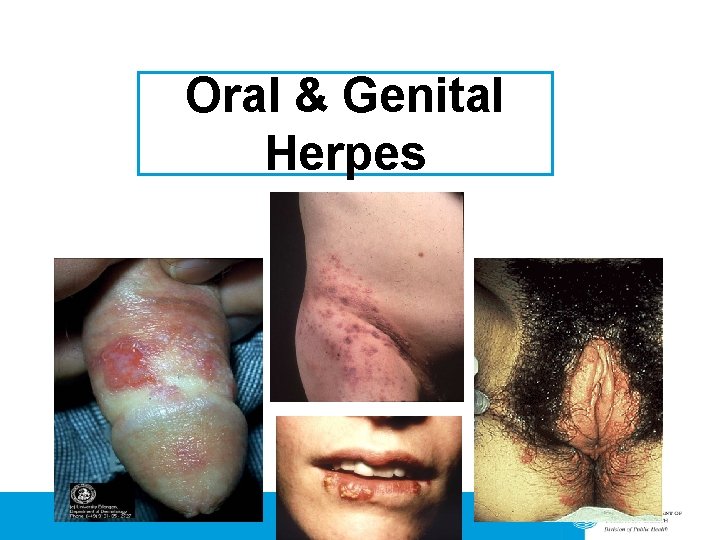
Oral & Genital Herpes
Treatment For Genital Herpes • There is no cure for Genital Herpes • Treatment may include: – – – Acyclovir Famciclovir Valacyclovir Valtrex Acetominophen or Ibuprofen (Oral Analgesic)

Syphilis • What is Syphilis? – – – An STD caused by the bacterium Treponema Pallidum Called the “great intimidator” because many of the signs and symptoms are indistinguishable from those of other diseases Stages of Syphilis • • • Mode of Transmission – • Spread during vaginal, anal or oral sex, and sometimes by genital touching, with someone who has Syphilis Symptoms – – • Primary Secondary Late Congenital Primary: Appearance of a sore (chancre) at the spot where syphilis entered the body – could be one or more Secondary: Skin rash and mucous membrane lesions, fever, swollen lymph glands, sore throat, patchy hair loss, headaches, weight loss, muscle aches and fatigue Late: Difficulty coordinating muscle movements, paralysis, numbness, gradual blindness, dementia Congenital: rash, thinning of the skin Prevention – – – Abstinence Condoms Monogamy
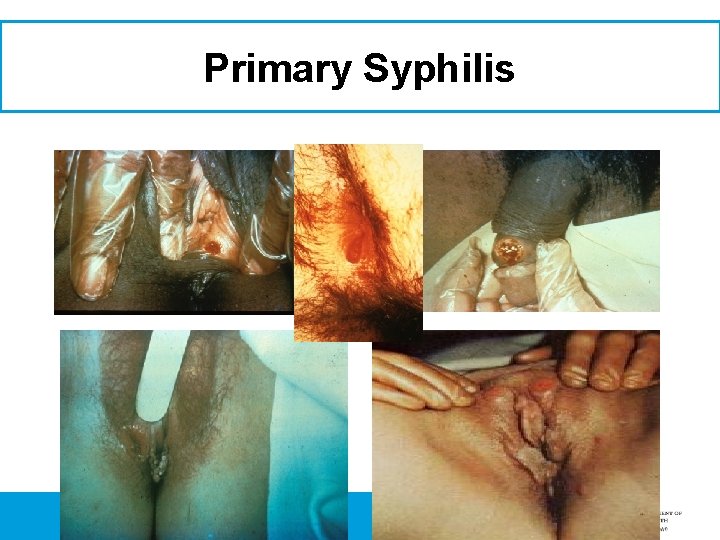
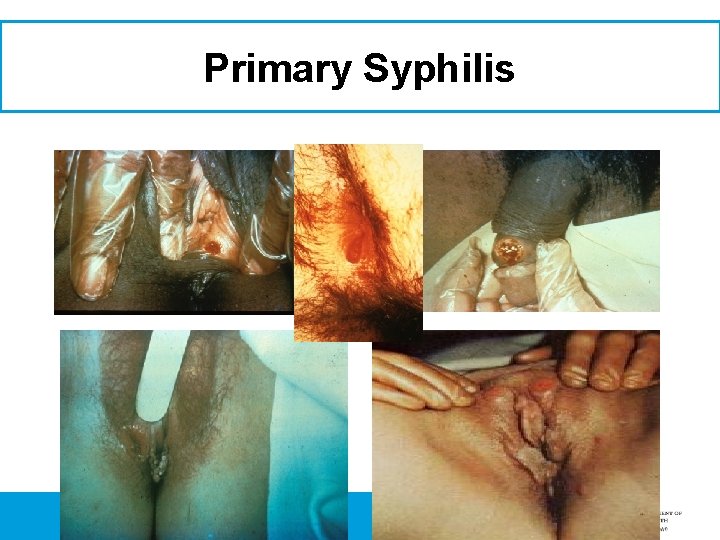
Primary Syphilis
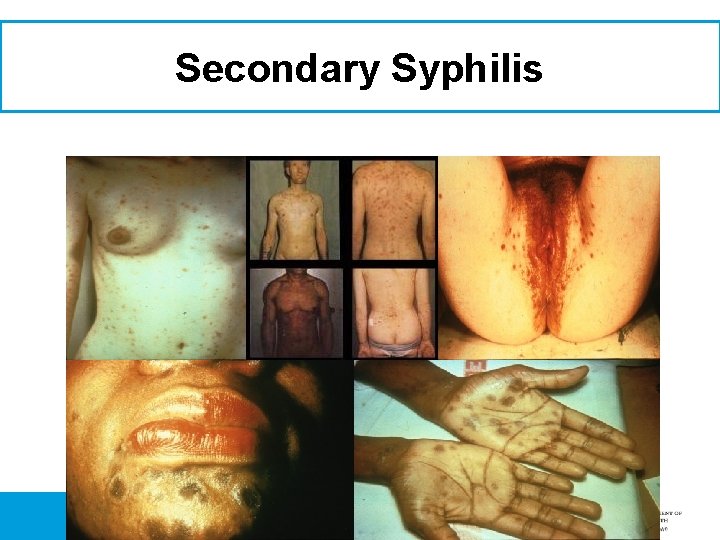
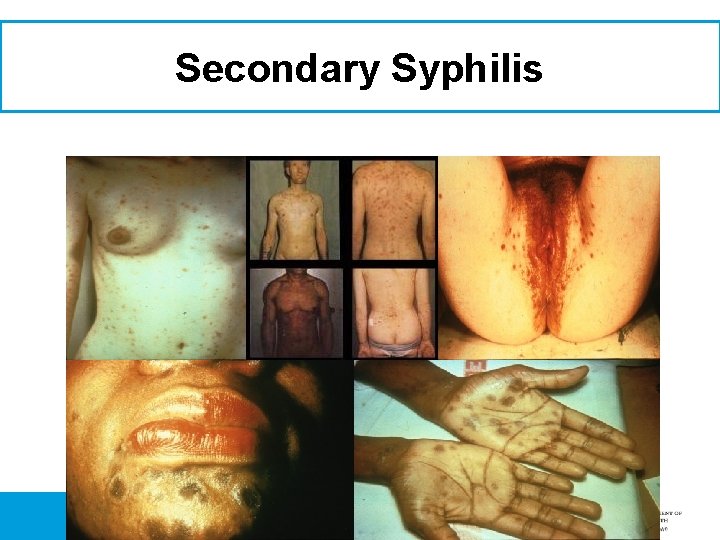
Secondary Syphilis
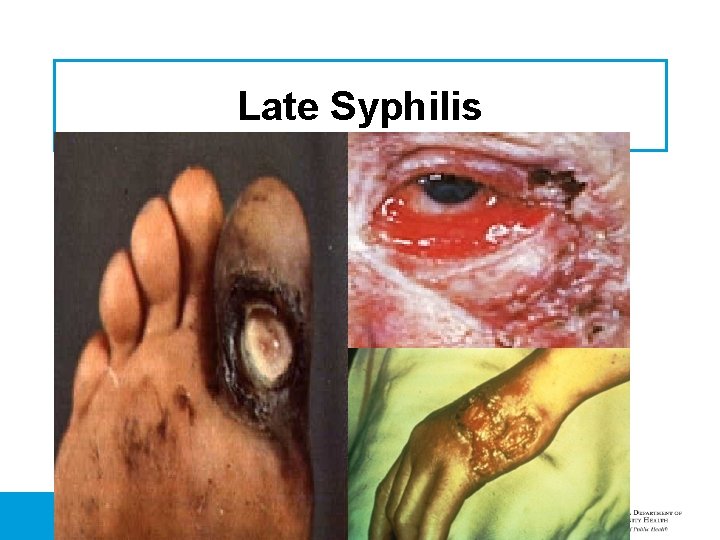
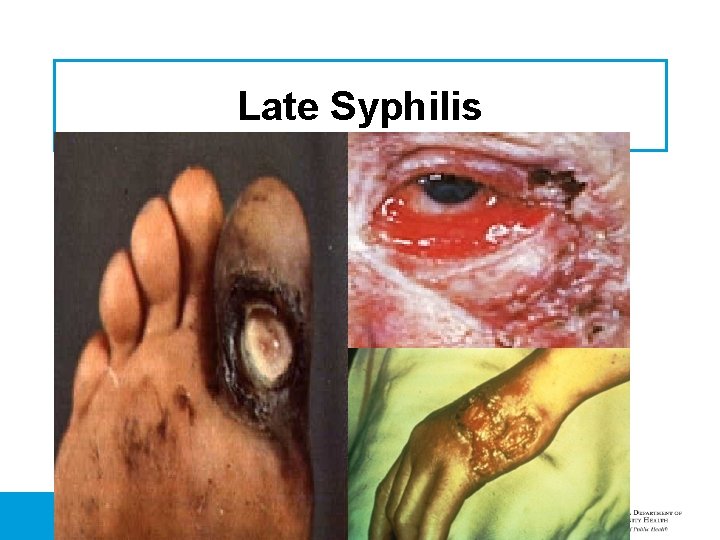
Late Syphilis
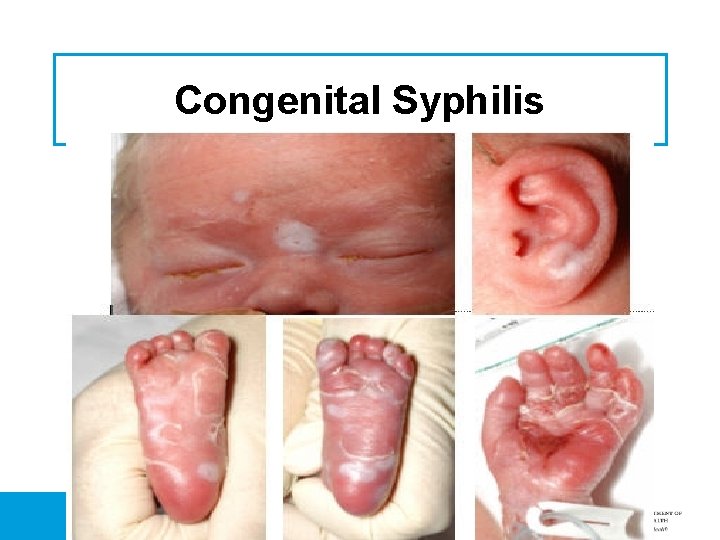
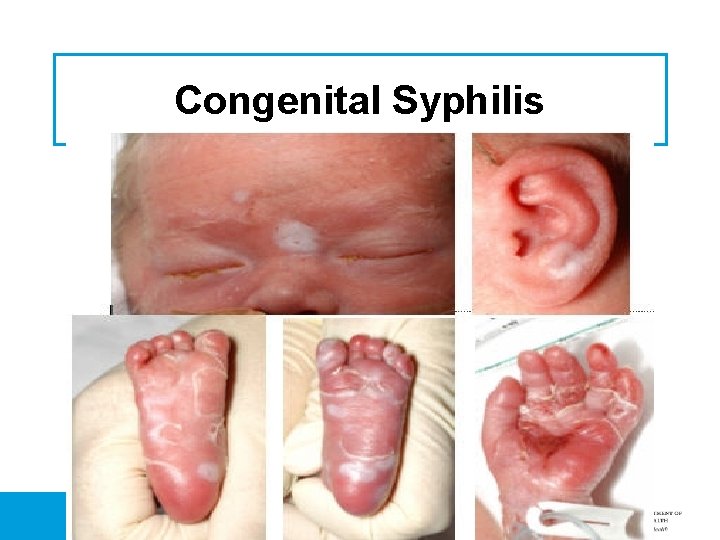
Congenital Syphilis
Treatment of Syphilis • Syphilis can be treated; however, a person will usually have a “titer” after treatment – Titer, def. the concentration of antibodies present in the highest dilution of a serum sample at which visible clumps with an appropriate antigen are formed. The concentration of antibodies present in the highest dilution of a serum sample at which visible clumps with an appropriate antigen are formed. • Benzathine Penicillin G • Doxyclycline (Cannot be used on lactating clients)

Can You Tell Who Has HIV?
HIV • Human Immunodeficiency Virus • The virus that causes AIDS • Damages the body’s immune system which protects the body from diseases • Can have for many years without signs or symptoms
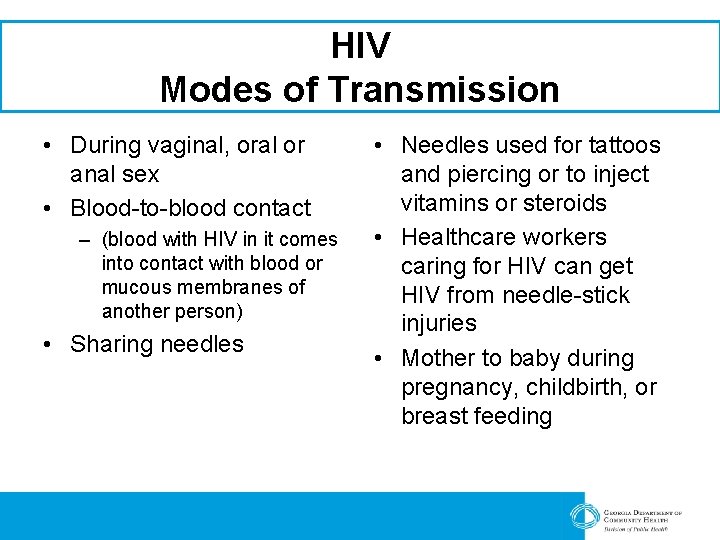
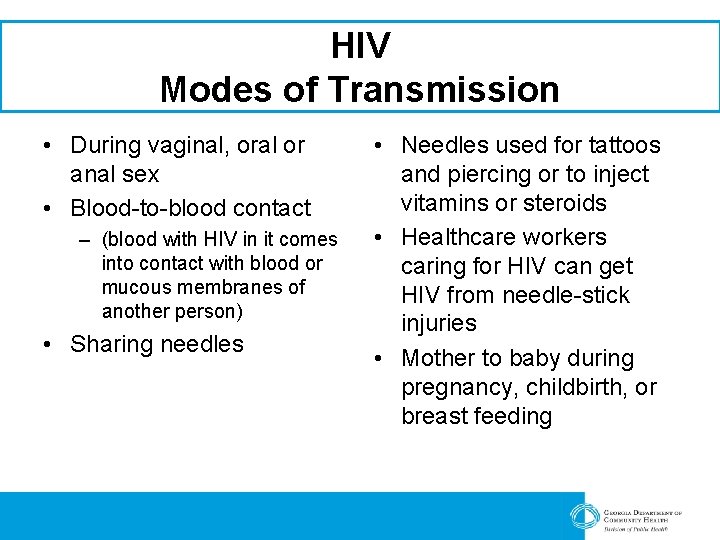
HIV Modes of Transmission • During vaginal, oral or anal sex • Blood-to-blood contact – (blood with HIV in it comes into contact with blood or mucous membranes of another person) • Sharing needles • Needles used for tattoos and piercing or to inject vitamins or steroids • Healthcare workers caring for HIV can get HIV from needle-stick injuries • Mother to baby during pregnancy, childbirth, or breast feeding
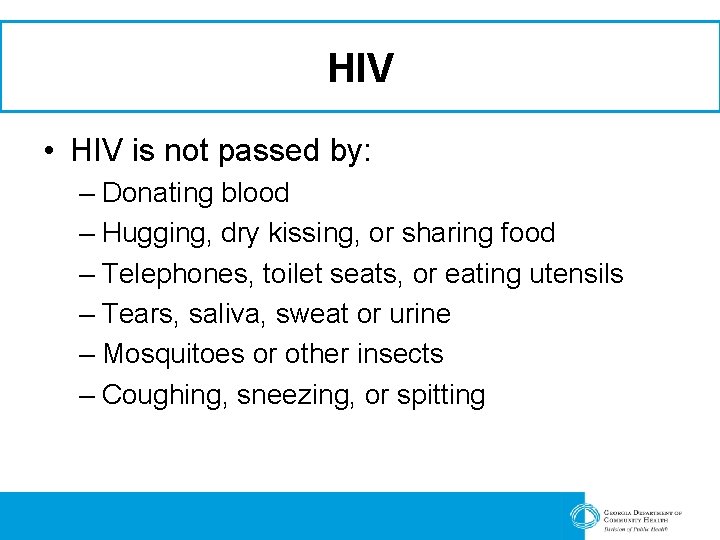
HIV • HIV is not passed by: – Donating blood – Hugging, dry kissing, or sharing food – Telephones, toilet seats, or eating utensils – Tears, saliva, sweat or urine – Mosquitoes or other insects – Coughing, sneezing, or spitting
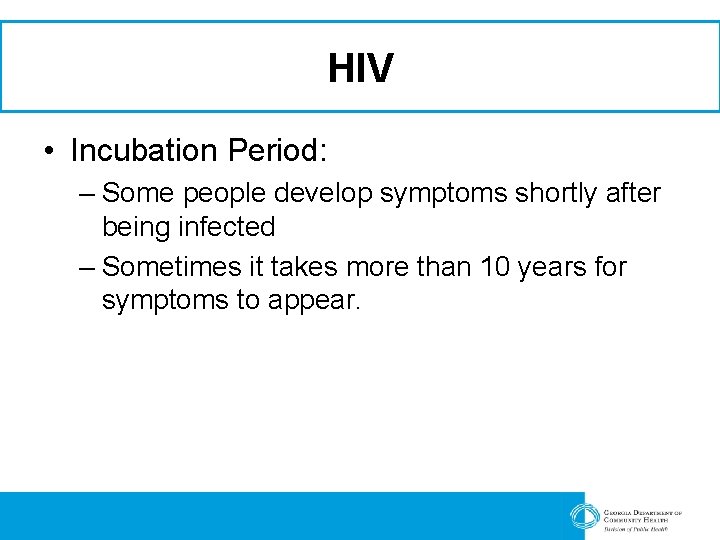
HIV • Incubation Period: – Some people develop symptoms shortly after being infected – Sometimes it takes more than 10 years for symptoms to appear.
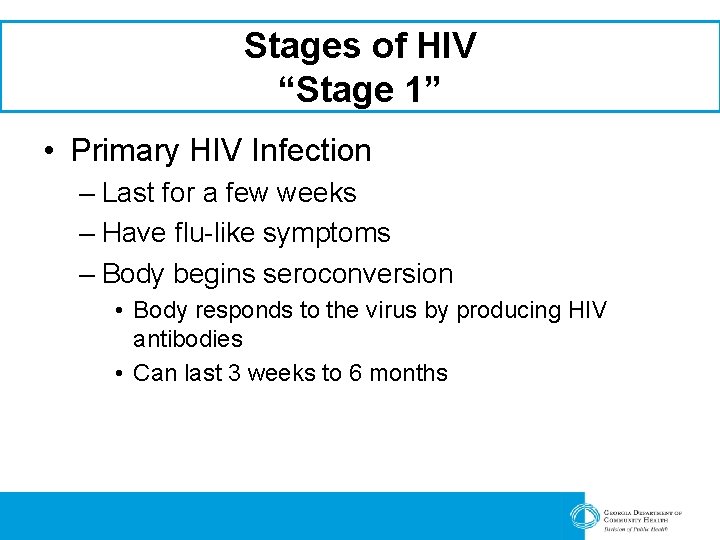
Stages of HIV “Stage 1” • Primary HIV Infection – Last for a few weeks – Have flu-like symptoms – Body begins seroconversion • Body responds to the virus by producing HIV antibodies • Can last 3 weeks to 6 months
Stages of HIV “Stage 2” • Asymptomatic Stage – Having no obvious signs of symptoms • Immune system still strong enough to prevent symptoms – Last for an average of 10 years – People continue to look and feel healthy • The virus can still be passed to other people – Unprotected sex, needle sharing – HIV virus continues to weaken the immune system
Stages of HIV “Stage 2” Continue • Symptoms: – Moderate unexplained weight loss – Recurrent respiratory infections – Fungal nail infections – Herpes zoster
Stages of HIV “Stage 3” • Symptomatic HIV Infection – The virus has become more active in the body and the immune system is weakened. – Symptoms: • • Skin Rashes Fatigue Night Sweats Slight weight loss Mouth ulcers Thrush (yeast infection) Fungal skin and nail infections
Stages of HIV “Stage 3” Continue – Symptoms • • • Unexplained sever weight loss Chronic diarrhea Persistent fever Oral candidiasis Oral hairy leukoplakia Bacterial infections – Pneumonia
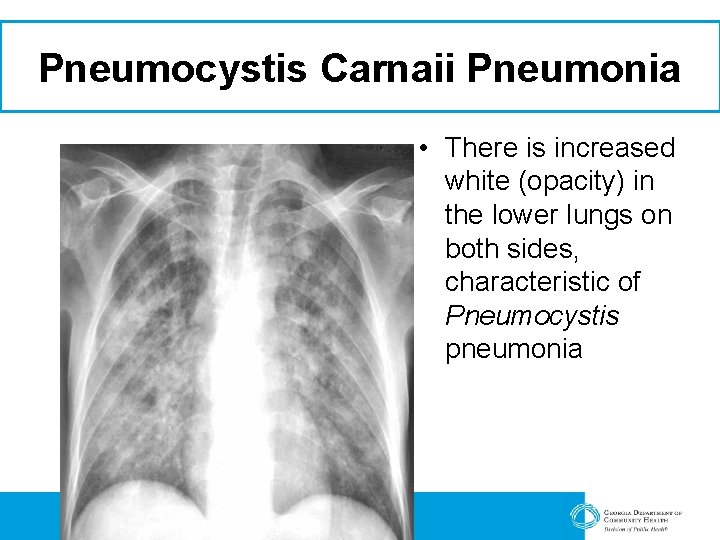
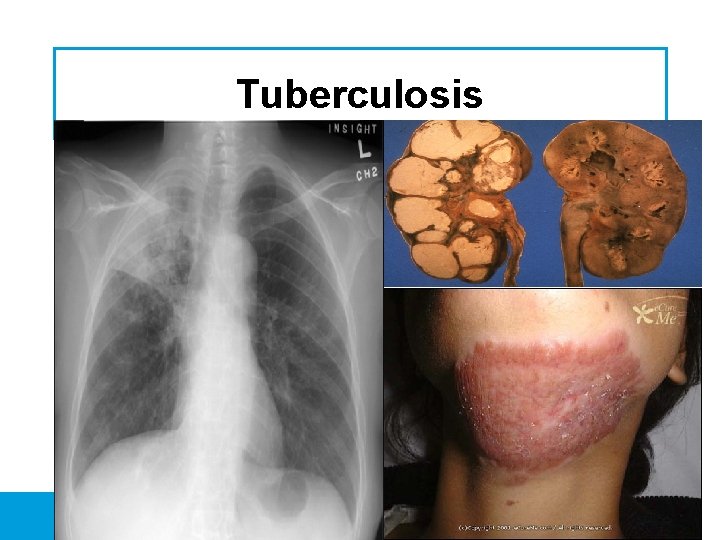
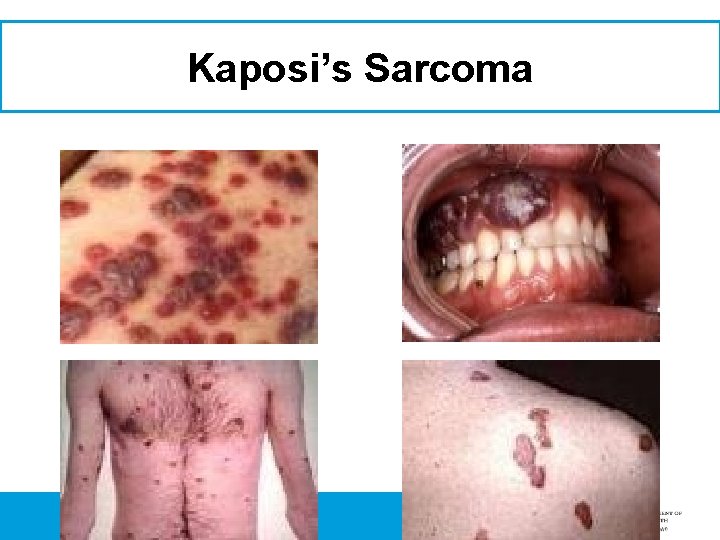
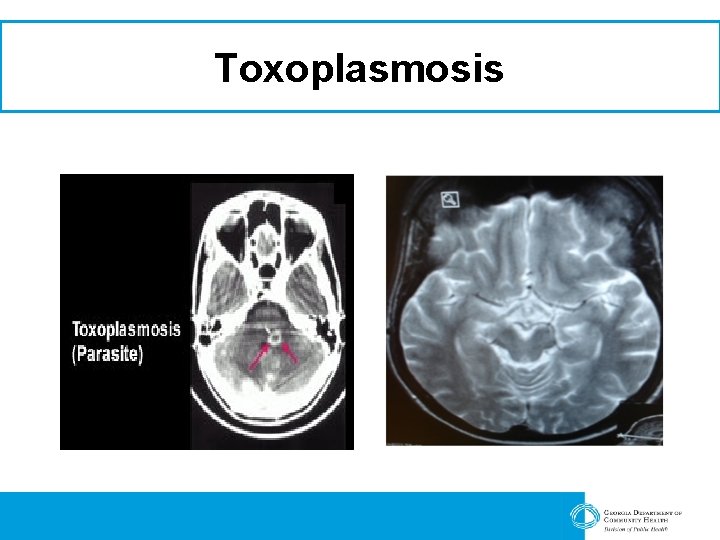
• Stages of HIV “Stage 4” AIDS – CD 4 count is less than 200 – Or has a history of an AIDS defining illness • Opportunistic Infections – Infections that the immune system would normally prevent. » Examples: – Pneumocystis Carinii Pneumonia (PCP) » A fungal infection of the lungs – Tuberculosis (TB) » A bacterial infection often found in the lungs but can spread to other parts of the body – Kaposi’s Sarcoma (KS) » A rare cancer that causes patches of abnormal tissue to grow under the skin, in the lining of the mouth, nose, and throat or in other organs – Cytomegalovirus (CMV) » A common virus that infects most people at some time during their lives but rarely causes obvious illness. It is a member of the herpes virus family » Can cause blindness – Toxoplasmosis » A disease caused by a single-celled parasite called Toxoplasma gondii
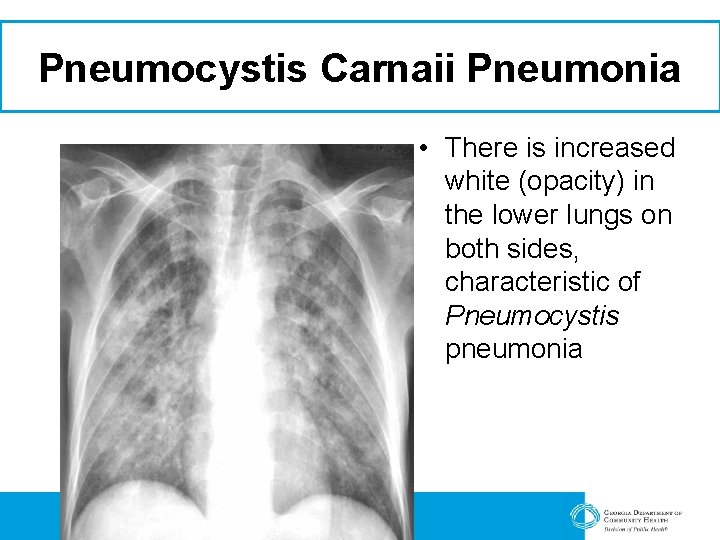
Pneumocystis Carnaii Pneumonia • There is increased white (opacity) in the lower lungs on both sides, characteristic of Pneumocystis pneumonia
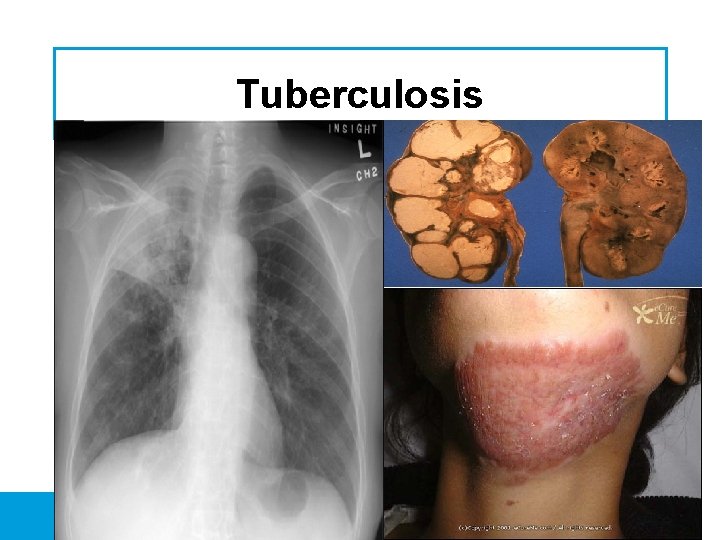
Tuberculosis
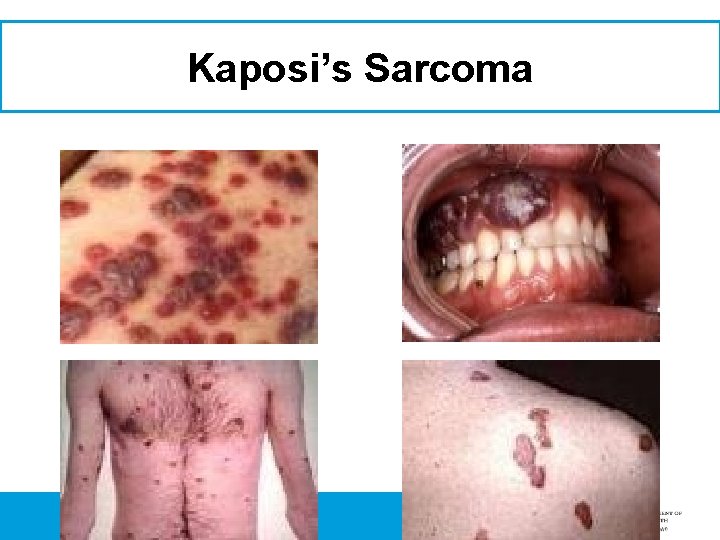
Kaposi’s Sarcoma

CMV Normal Retinas With CMV
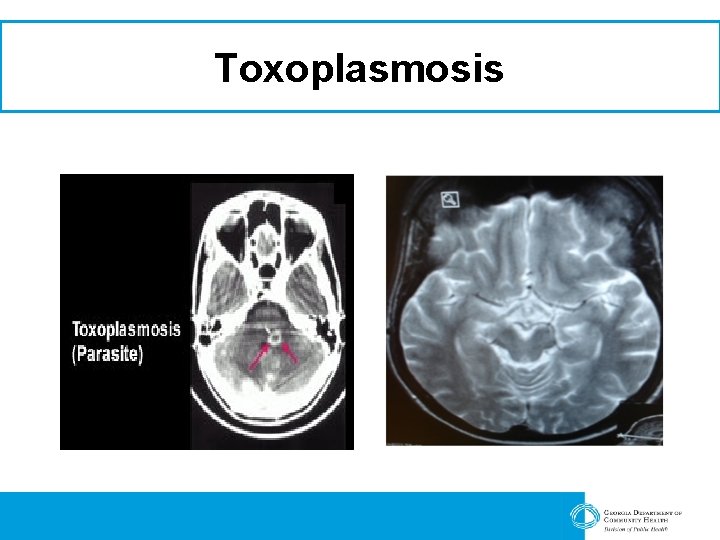
Toxoplasmosis
How Does A Person Find Out Whether Or Not They Are HIV+? • Taking the HIV Antibody test – Giving A Blood Sample • Blood is drawn and sent to the lab for processing • Results back in about two weeks – Taking the Ora. Sure Test • A swab is taken from the cheek (an additive on the swab pulls blood from the capillaries inside the cheek) • Results back in 2 -3 days – Taking the Ora. Quick test • A needlestick test • Results usually back in about 30 minutes • If a positive is revealed a confirmatory test is performed
HIV Testing • Test for HIV antibodies – Immune system makes these to fight HIV – Does not tell if you have AIDS • If you have antibodies – Test results are positive – Have HIV • If you don’t have HIV antibodies – Test results negative – You don’t have HIV
HIV Testing Continued • The Window Period – Usually takes up to 3 months after infection for the body to make HIV antibodies – In rare cases, it can take up to 6 months
STDs & Pregnancy
Additional Resources




Q Q U U E E S S T T I I O O N N S S
Contact Information Brenda Mims, RN, BSN Infectious Disease Coordinator South Health District, Unit 8 -1 (229) 245 -8711; Ext. 237 bcmims@dhr. state. ga. us

 Chapter 24 lesson 1 sexually transmitted diseases
Chapter 24 lesson 1 sexually transmitted diseases Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Std
Std Sexually transmitted diseases
Sexually transmitted diseases Chapter 25 sexually transmitted infections and hiv/aids
Chapter 25 sexually transmitted infections and hiv/aids Std
Std Pixel. com
Pixel. com Lynne hillenbrand
Lynne hillenbrand Lynne russell
Lynne russell Lynne abruzzo
Lynne abruzzo Nathan tinning
Nathan tinning Birthday present by lynne reid banks
Birthday present by lynne reid banks The great kapok tree vocabulary
The great kapok tree vocabulary Lynne finley
Lynne finley Lynne hybels
Lynne hybels Waylon jennings tomi lynne
Waylon jennings tomi lynne Lynne barasch
Lynne barasch Lynne korte
Lynne korte Dr lynne drummond
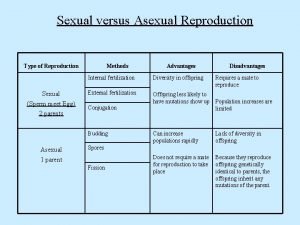
Dr lynne drummond How do birds reproduce
How do birds reproduce Concentricycloidea
Concentricycloidea Whale phylum
Whale phylum Class scyphozoa
Class scyphozoa Sexual coercion definition
Sexual coercion definition Dimorphism meaning
Dimorphism meaning Sexual harassment true or false quiz
Sexual harassment true or false quiz Protists habitat
Protists habitat Segmentation of nematoda
Segmentation of nematoda Freightment unpathetic
Freightment unpathetic Reproduction of protista
Reproduction of protista Sex offender evaluation illinois
Sex offender evaluation illinois Atis sexually or asexually
Atis sexually or asexually Male orgasm anatomy
Male orgasm anatomy Parasitism phylum
Parasitism phylum How do sponges reproduce sexually and asexually
How do sponges reproduce sexually and asexually Was i sexually abused as a child quiz
Was i sexually abused as a child quiz Class aves
Class aves How do annelids reproduce
How do annelids reproduce What is sexually dimorphic mean
What is sexually dimorphic mean Dr anna feldman
Dr anna feldman How does art criticism differ from art appreciation?
How does art criticism differ from art appreciation? Dr robert feldman
Dr robert feldman Production techniques
Production techniques Dr michael feldman
Dr michael feldman Dr robert feldman
Dr robert feldman Vitaly feldman
Vitaly feldman Dena feldman
Dena feldman Dr robert feldman
Dr robert feldman Feldman's model of organizational socialization
Feldman's model of organizational socialization Serial vs disjunctive
Serial vs disjunctive Grading for equity joe feldman
Grading for equity joe feldman Dr robert feldman
Dr robert feldman Feldman & gracon 1996
Feldman & gracon 1996 Paul feldman’s bagel test
Paul feldman’s bagel test Dr robert feldman
Dr robert feldman Chantal feldman
Chantal feldman Amiadarone
Amiadarone Dr robert feldman
Dr robert feldman Yehuda feldman
Yehuda feldman A song transmitted orally which tells a story
A song transmitted orally which tells a story Flat pivot bearing rate of wearing
Flat pivot bearing rate of wearing Transmitted light examination in questioned document
Transmitted light examination in questioned document Electronically transmitted postal ballot system
Electronically transmitted postal ballot system The totality of learned socially transmitted behavior
The totality of learned socially transmitted behavior 75 miles per hour to km
75 miles per hour to km Mph drug
Mph drug Monash public health
Monash public health Mudr. tomáš kampe mph
Mudr. tomáš kampe mph Melody hou md mph
Melody hou md mph Wait 1 h
Wait 1 h Lyme disease
Lyme disease