Sexually transmitted diseases 2 Lianjun Chen Huashan Hospital




























- Slides: 55
Sexually transmitted diseases (2) Lianjun Chen Huashan Hospital

Genital Herpes
Definition & Etiology l l Genital herpes , or Herpes progenitalis, is a sexually transmitted disease (STD) which is mainly caused by the herpes simplex viruses type 2 (HSV-2). HSV can cause blister、erosion and sores, which appear in and around the skin or mucous membranes of the genital area. The pathogen is herpes simplex viruses (HSV) – HSV- type 2, 90%。 – HSV- type 1,10%。
Transmission & Epidemiology l l l way of infection: the sex contact infection is the main path of the GH source of infection:the patients and nonsymptomatic virus carrier of GH mode of infection: HSV-1 is often transmitted by droplet and saliva, HSV-2 is chiefly transmitted by sex contact Genital herpes is one of the most common sexuallytransmitted viral diseases in Euro-American The incidence of GH is higher in the HIV patients.
Clinical menifestation l Primary genital herpes – The latency is averagely 3~5 days. – The eruption starts with erythema and papules that develop rapidly into crops of vesicles, produce erosion or ulcer after vesicles rupture. – The lesions are often extensive and bilateral inguinal lymph nodes can be enlarged with tenderness. – Flu-like symptoms, such as fever, headache and systemic malaise may be also be present. Patients often complain about incandescence and pain in the involved area, together with dysuria. – Sometimes neurologic involvement. – The disorder lasts between 2-3 weeks
Clinical manifestation l Recurrent genital herpes – It recurs for 5~8 times in the first year and less frequently in the years that follow. – Patients infected by HSV-1 less frequently suffer from recurrence than those by HSV-2. – The duration may be 7 days. – The signs and symptoms of recurrent lesions are mild. – The recurrences of GH are triggered by trauma, fatigue, infection, menstrual or cold onset, and so on.


HSV & Carcinomas cervicis l Researches of recent years report that HSV-Ⅱ is associated with the development of carcinoma cervicis, here are the evidences: – Women with GH correlate with a higher incidence of cervical cancer. – women with GH have higher sero-positive for HSV-Ⅱ antibody – HSV-Ⅱ antigen found in the carcinoma cervicis cells. – The DNA of HSV-Ⅱ cultured in histiocyte can transform the hamster cells into cancer cells.
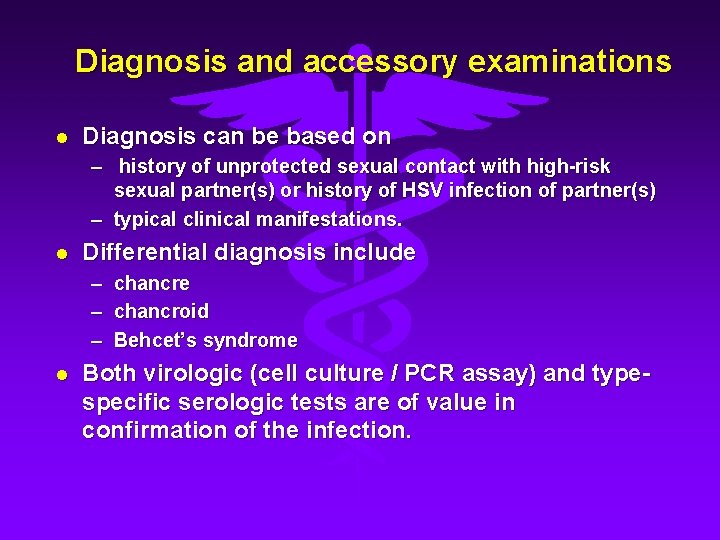
Diagnosis and accessory examinations l Diagnosis can be based on – history of unprotected sexual contact with high-risk sexual partner(s) or history of HSV infection of partner(s) – typical clinical manifestations. l Differential diagnosis include – chancroid – Behcet’s syndrome l Both virologic (cell culture / PCR assay) and typespecific serologic tests are of value in confirmation of the infection.

Treatment l Systemic antiviral drugs can partially control the signs and symptoms of herpes episodes when used to treat first clinical and recurrent episodes, or when used as daily suppressive therapy. l Systemic antiviral drugs neither eradicate latent virus nor affect the risk, frequency, or severity of recurrences after the drug is discontinued.
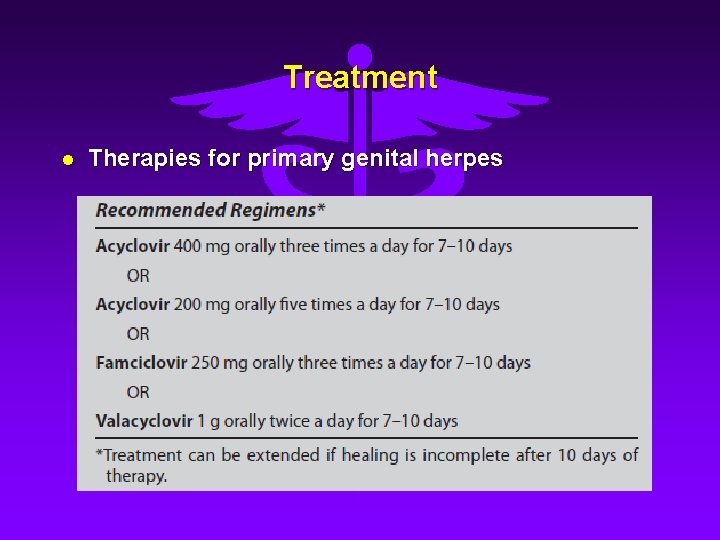
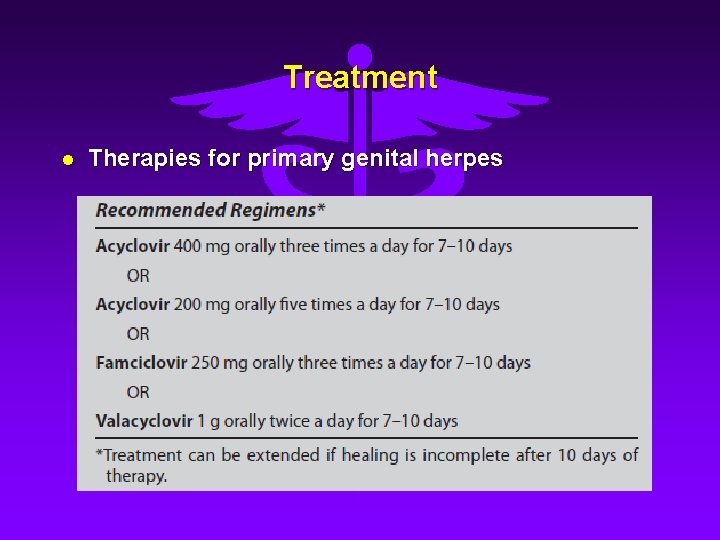
Treatment l Therapies for primary genital herpes
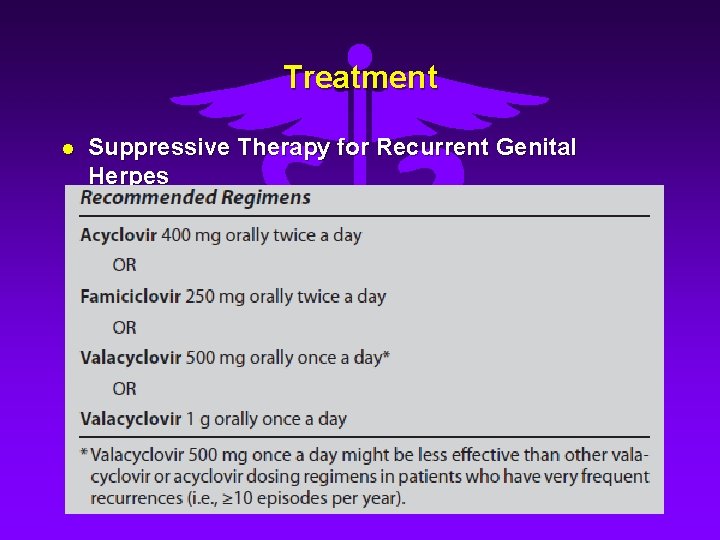
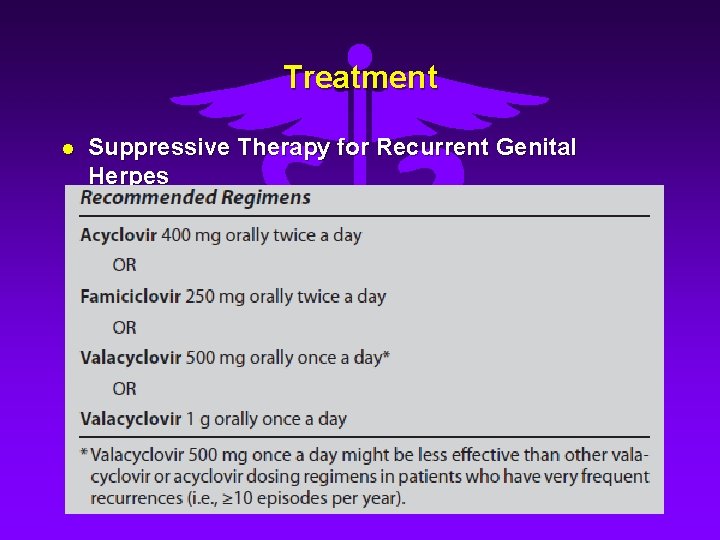
Treatment l Suppressive Therapy for Recurrent Genital Herpes
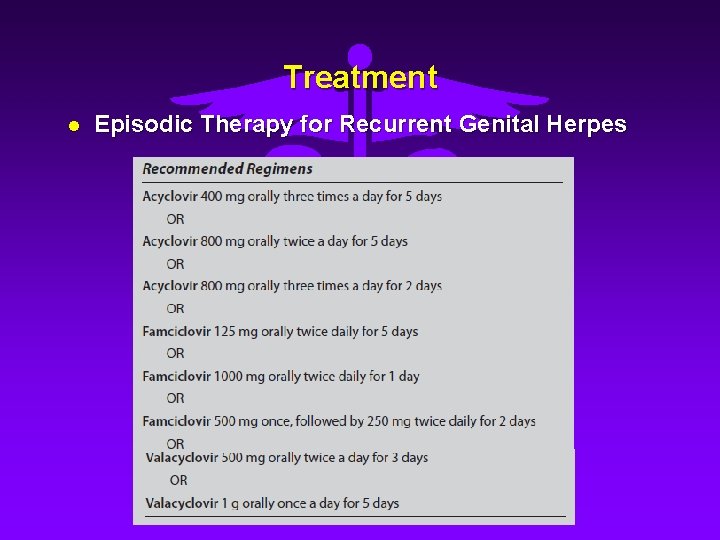
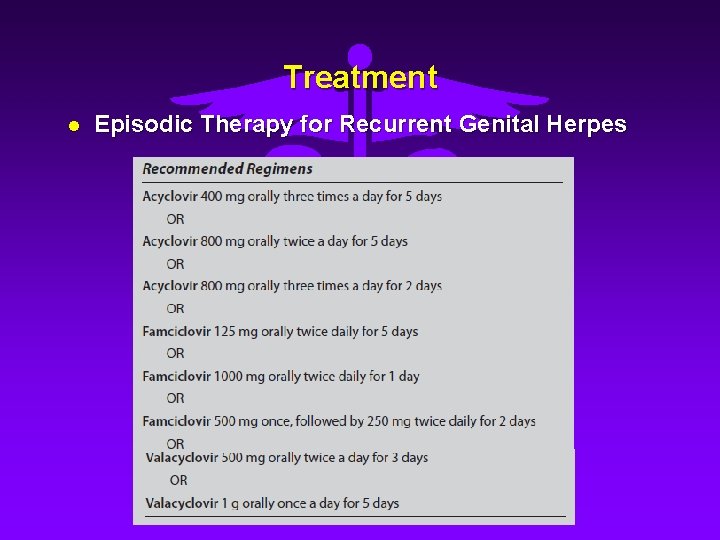
Treatment l Episodic Therapy for Recurrent Genital Herpes

Treatment l Pregnant women with genital herpes – All women with active lesions at delivery are delivered by cesarean section, ideally within 4 hours of rupture of the membrane. – Acyclovir suppression can be used in women with their initial outbreak during pregnancy, to reduce recurrence during late phase of gestation and therefore prevent the necessity of cesarean section. l Other: topical agents, interferon, transfer factor, chinese medicine, etc.

Syphilis

Definition l Syphilis is a chronic sexually transmitted disease due to infection of Treponema pallidum, which may involve multiple systems, including skin and mucosa as well as cardiovascular system and neural system, and present with various clinical manifestations.
Etiology l l Syphilis is caused by infection of Treponema pallidum. By dark-field microscopy, the characteristic motility of the pathogen can be observed, which consists of three movements: – – – l a projection in the direction of the long axis a rotation on its long axis a twisting from side to side. Treponema is not easy to survive in vitro. Boil, dry, soapsuds or common antiseptic can kill the pathogen.
Transmission & Epidemiology l The primary mode of transmission: sexual contact. l The next most common is transfer across the placenta. l l Blood transfusion. Others:kissing , suckling, or contacting the blood, secretion, dunnage (clothes, towel, razor, table dinner service, cigarette holder, et)of the patients.
Course and stage of disease l early syphilis(<2 years):primary syphilis, secondary syphilis l secondary syphilis(>2 years)or tertiary syphilis: tertiary cutaneous syphilis , late osseous syphilis , cardiovascular syphilis, neurosyphilis and others l latent syphilis :early latent syphilis (<2 years), latent syphilis (>2 years)
Clinical manifestation l Primary stage (chancre) – Presents as the first lesion, usually 18 to 21 days after infection. – Often occur at the external genitalia, others on the mouth, tongue, anus or finger. – Typically a single, painless, round or oval, borderline clear, indurated, slightly elevated papule, with erosion but no ulceration. – A cartilage-like consistency on palpation. – Heal spontaneously within three to six weeks, even in the absence of treatment. – Regional lymph nodes are often enlarged, usually beginning 1~2 weeks after the appearance of chancre. – Darkfield microscopy:early often TP (+) ; late may (-) – RPR or VDRL:eraly(-) , late(+).



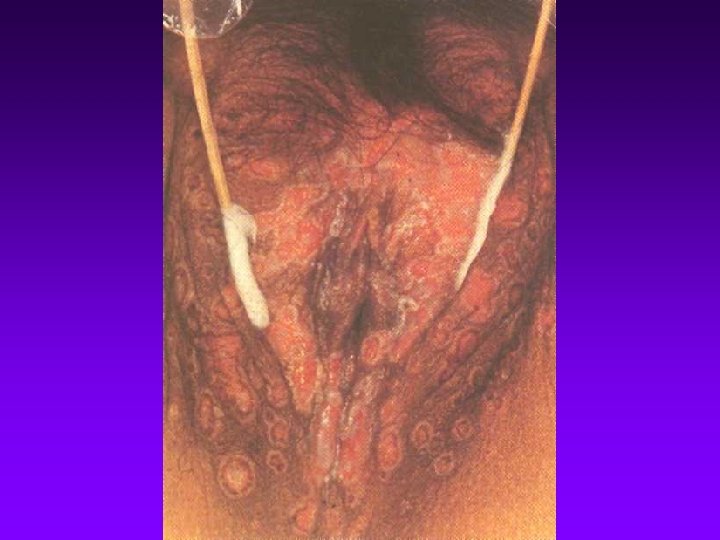
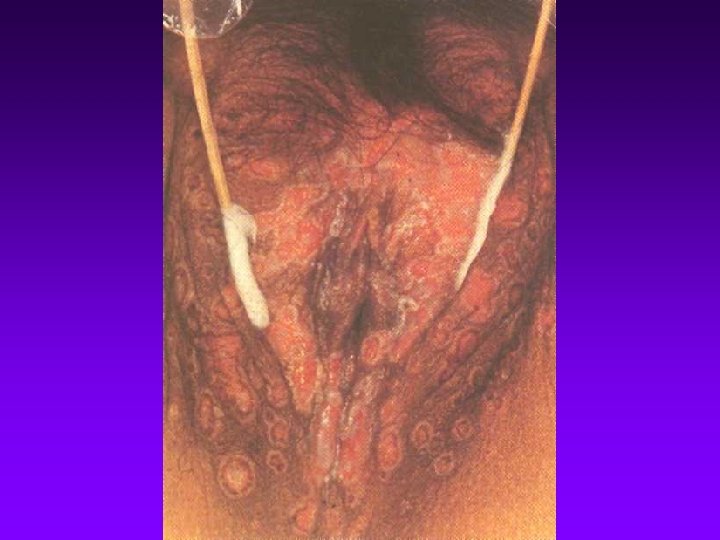
Clinical manifestation l Secondary stage – Cutaneous and mucosal lesions (syphilids) l l l Appear about 10 weeks(8~ 12 weeks)after infection. Prodrome: fever, acratia, headache, arthralgia, myosalgia, anorexia. Eruption : macule, papule, follicular papule or pustule; symmetrical, generalized and dense, round or oval, red copper. Without pain or itch. RPR or VDRL(+). – Syphilids on palms or soles: ham-colored macules with more or less scales, but without fusion, symmetrically scattering on palms or soles. – Condylomata lata: usually located in folds of moist skin, such as vulvae and about anus, which are characterized by broad and flat moist papules. – Other typical cutaneous lesions : moth-eaten alopecia and depigmentized macules. – Syphilitic mucosal patches : the most characteristic mucosal lesion of secondary syphilisfeatured by macerated, flat, grayish, rounded
Clinical manifestation l Secondary stage – Systemic involvement l l multiple lymph nodes involved: frequently inguinal, posterior cervical, postauricular, and epitrochlear, and are often shotty, firm, nontender and discrete. osteal lesion, often presenting as osteomyoelitis, periostitis or polyarthritis. ophthalmic lesions, presenting as iritis, iridocyclitis, choroiditis, retinitis, optic neuritis, or retinitis neural lesions, presenting as acute meningitis, sensorineural hearng loss, Bell’s palsy, or asymptomatic neural lesion with abnormality of CSF. – Relapsing secondary syphilis l l Appear after early syphilid, most within 1 -2 year Lesions may appear on the same site as before, however, the lesions on skin may present more congregated and usually asymmetrical.









Clinical manifestation l Tertiary syphilis or late syphilis Late syphilis is defined as infection of Treponema pallitum with duration of more than 2 years. – Tertiary cutaneous and mucosal syphilis l l l isolated, localized, invasive plaques or nodules, usually asymmetric and destructive, with slow progression, but healing with scars. Nodular syphilid: often present as reddish brown firm nodules, which tend to form rings or serpentine patterns; may be ulcerated with a rough base and a raised edge Gummas : often beginning as small nodules, then gradually enlarged, followed by central necrosis, leaving a steep edge and a gummy base.
Clinical manifestation l Tertiary syphilis or late syphilis – Tertiary osseous syphilis l periostitis, osteomyelitis, ostetis, gummatous osteroarthits syphilitic arthropathy. – Tertiary ophthalmic syphilis l iritis, iridocyclitis, choroiditis, retinitis or optic neuritis. – Late cardiovascular syphilis l l may occur in about 40% untreated patients, often 10~30 years after infection. Aortitis(most common), aortic aneurysm, aortic insufficiency , coronary artery diseases, gumma of cardiac muscles. – Late neurosyphilis l l l asymtomatic neurosyphilis with positive CSF examinations meningovascular neurosyphilis parenchymatous syphilis: often appear as late as over 10 years after infection, the most common patterns include general paralysis of insane, tabes dorsalis and optic atrophy.



Latent Syphilis l Early latent syphilis – < 2 years after infection. – Without clinical symptom or sign. – Blood RPR or VDRL(+). – CSF(-). l Late latent syphilis – – – > 2 years after infection. Without clinical symptom ,but has left scar of tertiary syphilis. Blood RPR or VDRL(+). CSF(-)(if CSF abnormal, called Asymptomatic neurosyphilis). Chest fluoroscopy negtive to exclude syphilitic aortitis.
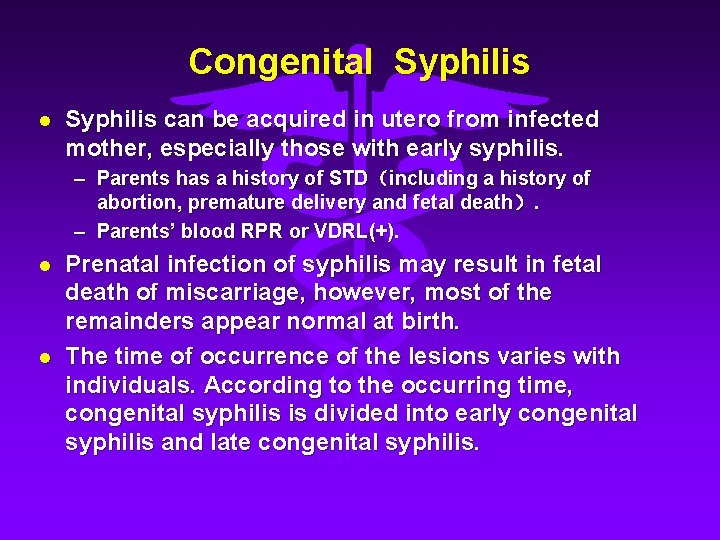
Congenital Syphilis can be acquired in utero from infected mother, especially those with early syphilis. – Parents has a history of STD(including a history of abortion, premature delivery and fetal death). – Parents’ blood RPR or VDRL(+). l l Prenatal infection of syphilis may result in fetal death of miscarriage, however, most of the remainders appear normal at birth. The time of occurrence of the lesions varies with individuals. According to the occurring time, congenital syphilis is divided into early congenital syphilis and late congenital syphilis.
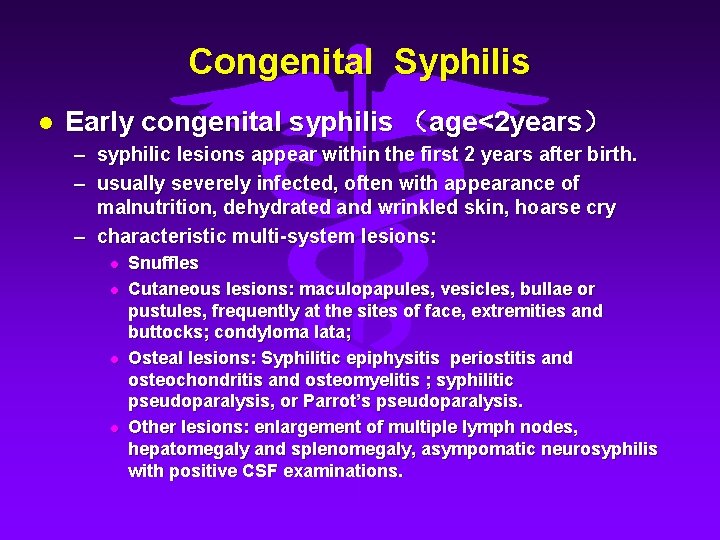
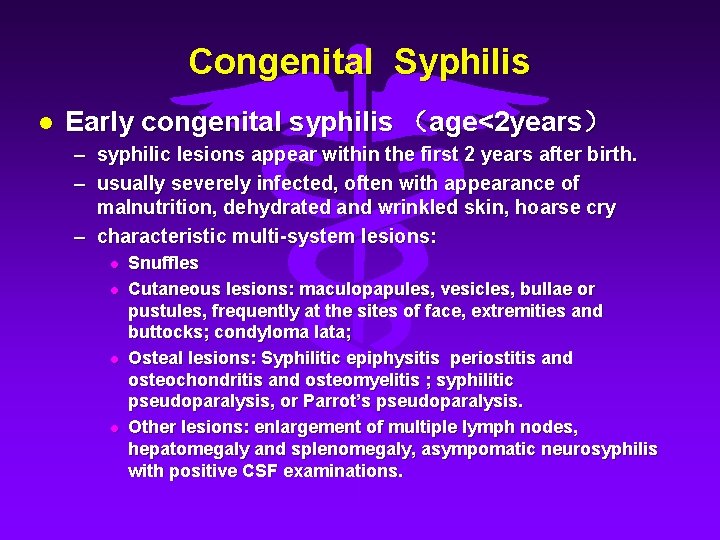
Congenital Syphilis l Early congenital syphilis (age<2 years) – syphilic lesions appear within the first 2 years after birth. – usually severely infected, often with appearance of malnutrition, dehydrated and wrinkled skin, hoarse cry – characteristic multi-system lesions: l l Snuffles Cutaneous lesions: maculopapules, vesicles, bullae or pustules, frequently at the sites of face, extremities and buttocks; condyloma lata; Osteal lesions: Syphilitic epiphysitis periostitis and osteochondritis and osteomyelitis ; syphilitic pseudoparalysis, or Parrot’s pseudoparalysis. Other lesions: enlargement of multiple lymph nodes, hepatomegaly and splenomegaly, asympomatic neurosyphilis with positive CSF examinations.


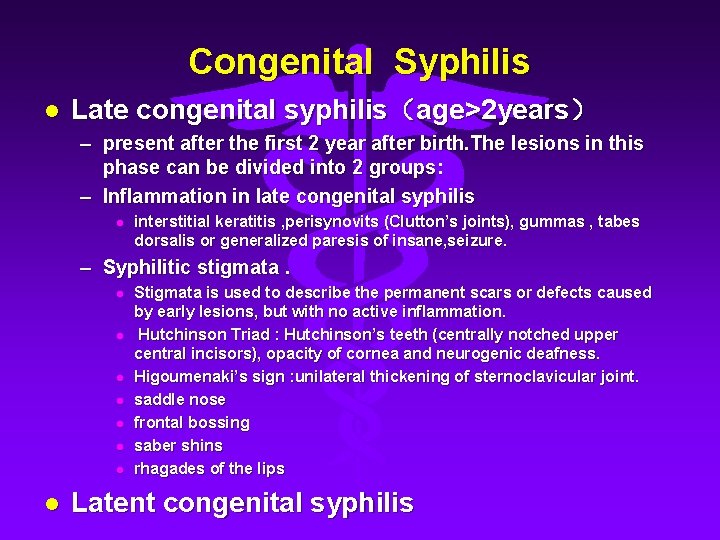
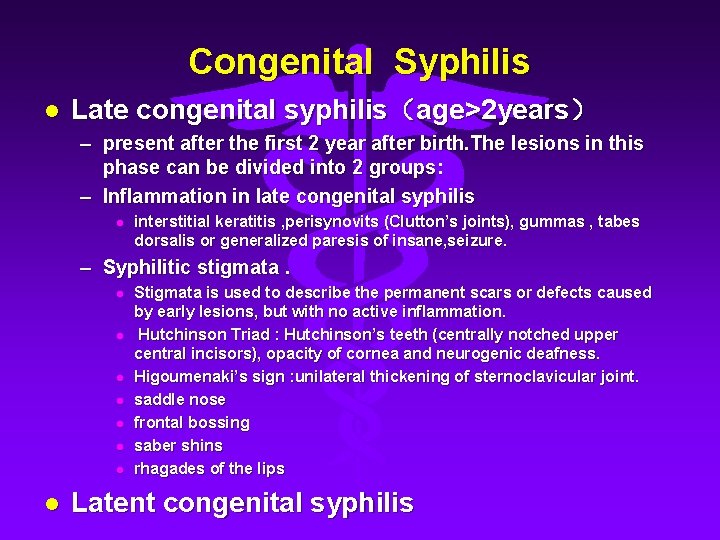
Congenital Syphilis l Late congenital syphilis(age>2 years) – present after the first 2 year after birth. The lesions in this phase can be divided into 2 groups: – Inflammation in late congenital syphilis l interstitial keratitis , perisynovits (Clutton’s joints), gummas , tabes dorsalis or generalized paresis of insane, seizure. – Syphilitic stigmata. l l l l Stigmata is used to describe the permanent scars or defects caused by early lesions, but with no active inflammation. Hutchinson Triad : Hutchinson’s teeth (centrally notched upper central incisors), opacity of cornea and neurogenic deafness. Higoumenaki’s sign : unilateral thickening of sternoclavicular joint. saddle nose frontal bossing saber shins rhagades of the lips Latent congenital syphilis
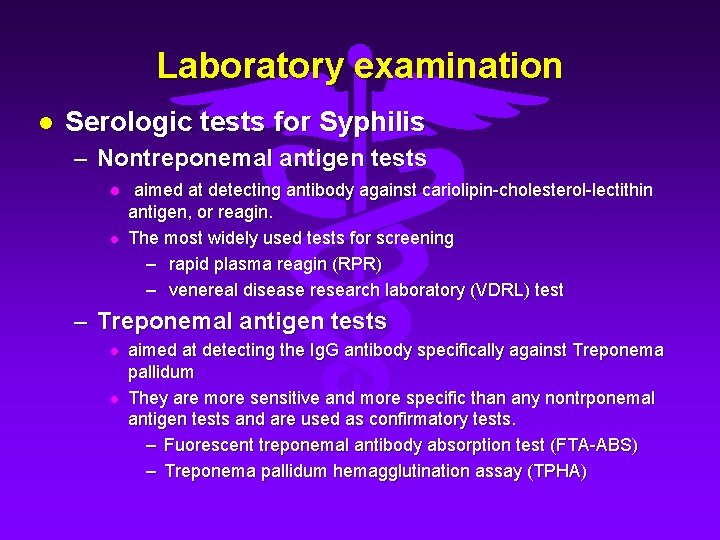
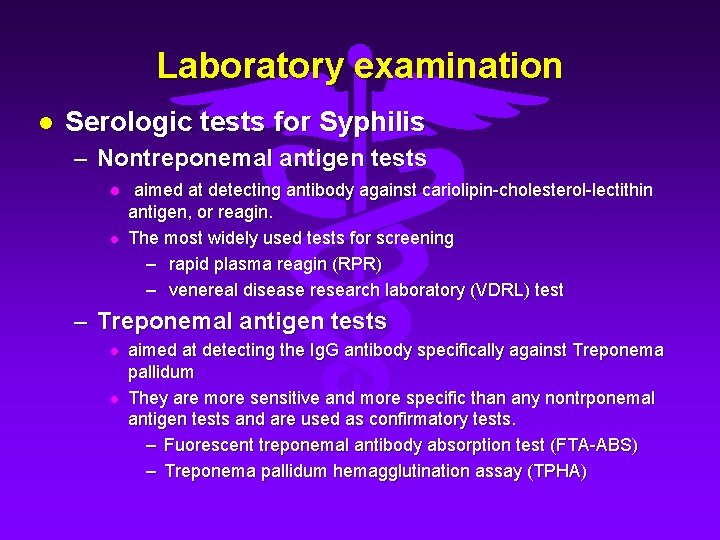
Laboratory examination l Serologic tests for Syphilis – Nontreponemal antigen tests l l aimed at detecting antibody against cariolipin-cholesterol-lectithin antigen, or reagin. The most widely used tests for screening – rapid plasma reagin (RPR) – venereal disease research laboratory (VDRL) test – Treponemal antigen tests l l aimed at detecting the Ig. G antibody specifically against Treponema pallidum They are more sensitive and more specific than any nontrponemal antigen tests and are used as confirmatory tests. – Fuorescent treponemal antibody absorption test (FTA-ABS) – Treponema pallidum hemagglutination assay (TPHA)
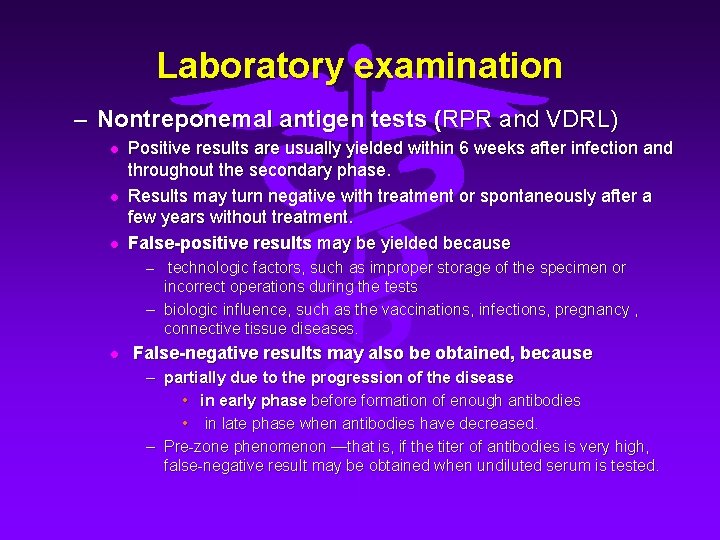
Laboratory examination – Nontreponemal antigen tests (RPR and VDRL) l l l Positive results are usually yielded within 6 weeks after infection and throughout the secondary phase. Results may turn negative with treatment or spontaneously after a few years without treatment. False-positive results may be yielded because – technologic factors, such as improper storage of the specimen or incorrect operations during the tests – biologic influence, such as the vaccinations, infections, pregnancy , connective tissue diseases. l False-negative results may also be obtained, because – partially due to the progression of the disease • in early phase before formation of enough antibodies • in late phase when antibodies have decreased. – Pre-zone phenomenon —that is, if the titer of antibodies is very high, false-negative result may be obtained when undiluted serum is tested.
Laboratory examination l Dark-field examination – Treponema pallidum can be detected by dark-field microscopy in the specimen collected from chancre, condylomata lata, or mucosal lesions, according to its characteristic motility mentioned above. l Examinations of cerebral-spinal fluid (CSF) l Chest X-ray – The result can provide evidence for the diagnosis of cardiovascular syphilis.
Diagnosis l History of unprotected sexual contact with high-risk partner(s) or partner(s) with syphilis. l Clinical manifestation of various phases. l Preliminary nontreponemal antigen serologic tests and confirmatory treponema-specific tests.
Treatment l l Penicillin G, administered parenterally, is the preferred drug for treating all stages of syphilis. The preparation used, the dosage, and the length of treatment depend on the stage and clinical manifestations of the disease. Selection of the appropriate penicillin preparation is important, because T. pallidum can reside in sequestered sites (e. g. , the CNS and aqueous humor) that are poorly accessed by some forms of penicillin. Combinations of benzathine penicillin, procaine penicillin, and oral penicillin preparations are not considered appropriate for the treatment of syphilis.
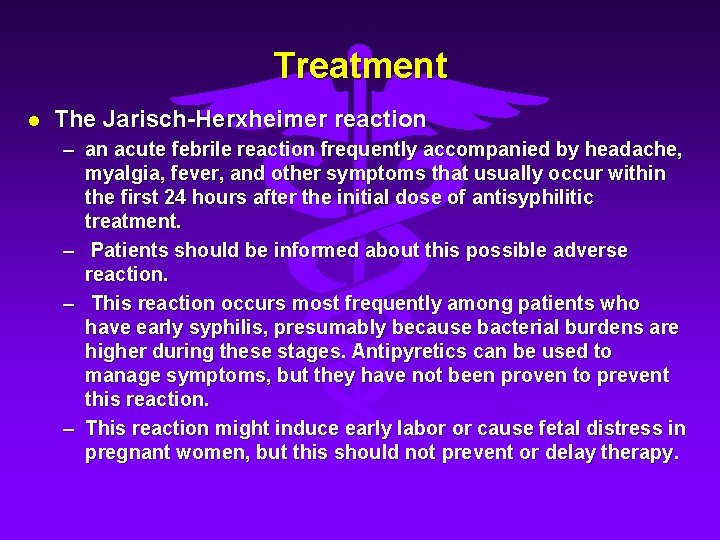
Treatment l The Jarisch-Herxheimer reaction – an acute febrile reaction frequently accompanied by headache, myalgia, fever, and other symptoms that usually occur within the first 24 hours after the initial dose of antisyphilitic treatment. – Patients should be informed about this possible adverse reaction. – This reaction occurs most frequently among patients who have early syphilis, presumably because bacterial burdens are higher during these stages. Antipyretics can be used to manage symptoms, but they have not been proven to prevent this reaction. – This reaction might induce early labor or cause fetal distress in pregnant women, but this should not prevent or delay therapy.
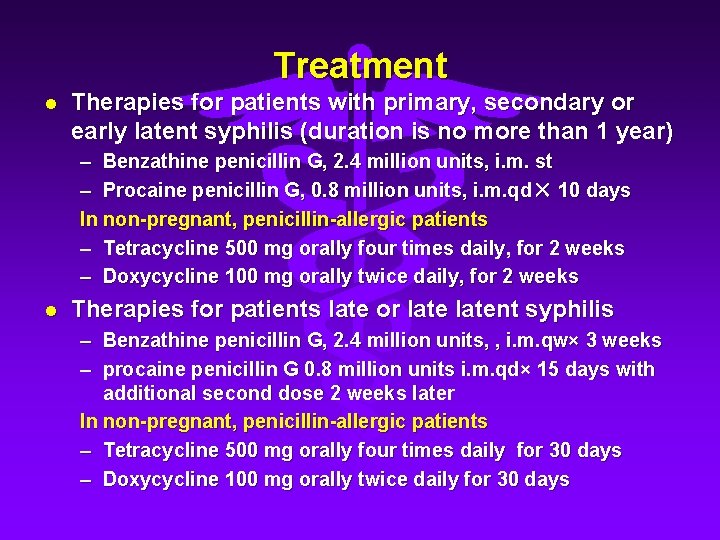
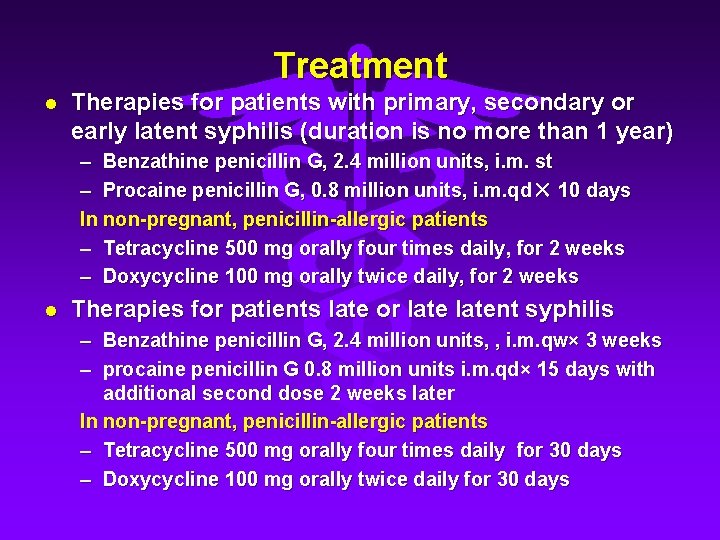
Treatment l Therapies for patients with primary, secondary or early latent syphilis (duration is no more than 1 year) – Benzathine penicillin G, 2. 4 million units, i. m. st – Procaine penicillin G, 0. 8 million units, i. m. qd × 10 days In non-pregnant, penicillin-allergic patients – Tetracycline 500 mg orally four times daily, for 2 weeks – Doxycycline 100 mg orally twice daily, for 2 weeks l Therapies for patients late or latent syphilis – Benzathine penicillin G, 2. 4 million units, , i. m. qw× 3 weeks – procaine penicillin G 0. 8 million units i. m. qd× 15 days with additional second dose 2 weeks later In non-pregnant, penicillin-allergic patients – Tetracycline 500 mg orally four times daily for 30 days – Doxycycline 100 mg orally twice daily for 30 days

Treatment l Therapies for late neurosyphilis – Aqueous crystalline penicillin G 18– 24 million units per day, administered as 3– 4 million units IV every 4 hours or continuous infusion, for 10 to 14 days – Procaine penicillin G, 2. 4 million units , i. m. qd, together with probenecid 500 mg orally four times daily, for 10 to 14 days – both of therapies are followed by benzathine penicillin G, 2. 4 million units, , i. m. qw× 3 weeks. – In penicillin-allergic patients, desensitization and use of penicillin is recommended. – In order to avoid Jarisch-Herxheimer reaction, orally taken corticosteroid before the beginning of anti-syphilitic treatment alleviate the reaction.
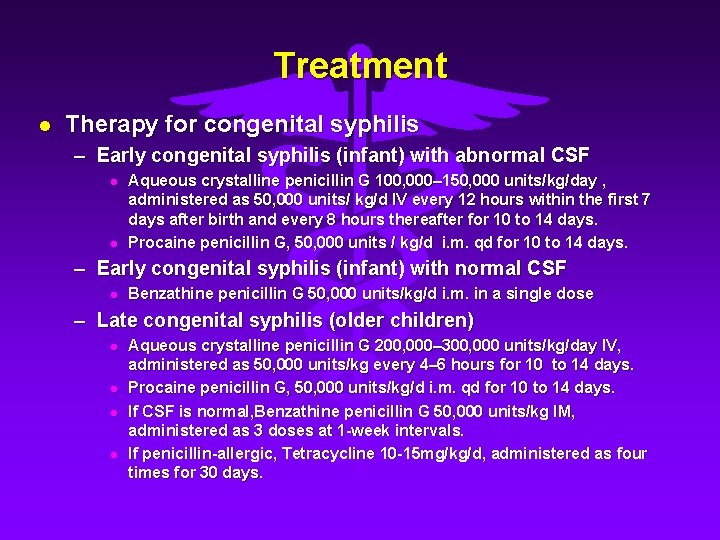
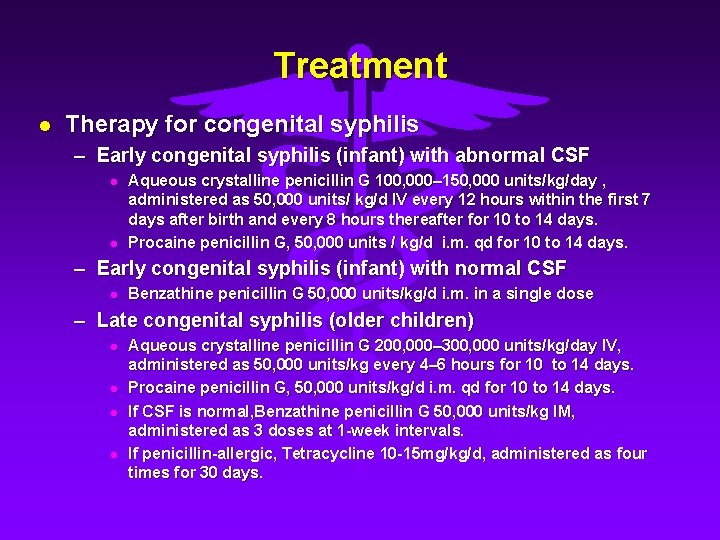
Treatment l Therapy for congenital syphilis – Early congenital syphilis (infant) with abnormal CSF l l Aqueous crystalline penicillin G 100, 000– 150, 000 units/kg/day , administered as 50, 000 units/ kg/d IV every 12 hours within the first 7 days after birth and every 8 hours thereafter for 10 to 14 days. Procaine penicillin G, 50, 000 units / kg/d i. m. qd for 10 to 14 days. – Early congenital syphilis (infant) with normal CSF l Benzathine penicillin G 50, 000 units/kg/d i. m. in a single dose – Late congenital syphilis (older children) l l Aqueous crystalline penicillin G 200, 000– 300, 000 units/kg/day IV, administered as 50, 000 units/kg every 4– 6 hours for 10 to 14 days. Procaine penicillin G, 50, 000 units/kg/d i. m. qd for 10 to 14 days. If CSF is normal, Benzathine penicillin G 50, 000 units/kg IM, administered as 3 doses at 1 -week intervals. If penicillin-allergic, Tetracycline 10 -15 mg/kg/d, administered as four times for 30 days.

Treatment l Therapies for pregnant women with syphilis – The therapy should be restricted to application of penicillin, the dose should be the same as non-pregnant women according to particular stages. – In penicillin-allergic patients, desensitization and use of penicillin is recommended. – Besides, follow-up quantitative serologic tests monthly until delivery are necessary.

Treatment l Management of Sex Partners – Sexual partners of infected patients should be considered at risk and provided treatment if they have had sexual contact with the patient within l l l 3 months plus the duration of symptoms for patients diagnosed with primary syphilis 6 months plus duration of symptoms for those with secondary syphilis 1 year for patients with early latent syphilis. – Persons who were exposed within the 90 days preceding the diagnosis of primary, secondary, or early latent syphilis in a sex partner should be treated – Persons who were exposed >90 days before the diagnosis of primary, secondary, or early latent syphilis in a sex partner should be treated presumptively if serologic test results are not available immediately and the opportunity for follow-up is uncertain. – For purposes of partner notification and presumptive treatment of exposed sex partners, patients with syphilis of unknown duration who have high RPR titers (i. e. , >1: 32) can be assumed to have early syphilis. – Long-term sex partners of patients who have latent syphilis should be evaluated clinically and serologically for syphilis and treated on the basis of the evaluation findings.

Follow-ups l l Treated patients should follow up every 3 months within the first year after treatment, and every 6 months thereafter, for totally 2~3 years. The follow-ups should include clinical examinations as well as non-specific serologic tests. For patients with recurrence of syphilis, according to clinical manifestations or serologic test results (become positive again after turning negative), antisyphilitic therapies should be repeated. However, in patients with congenital or late syphilis, if the serologic tests continue to yield strong positive result, in spite of sufficient treatment, repeated treatment is not recommended.
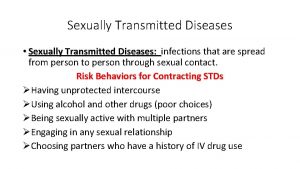
 Chapter 24 lesson 1 sexually transmitted diseases
Chapter 24 lesson 1 sexually transmitted diseases Chapter 24 sexually transmitted diseases and hiv/aids
Chapter 24 sexually transmitted diseases and hiv/aids Sti std
Sti std Nursing management of reproductive tract infection
Nursing management of reproductive tract infection Syphalitis
Syphalitis A bacterial std that usually affects mucous membranes
A bacterial std that usually affects mucous membranes Std
Std Chen chen berlin
Chen chen berlin Abuse prevention training quiz answers
Abuse prevention training quiz answers Dimorphism meaning
Dimorphism meaning Sexual harassment true or false quiz
Sexual harassment true or false quiz Run away selection
Run away selection Cargo
Cargo Is phytoplankton a protist
Is phytoplankton a protist Sex offender evaluation illinois
Sex offender evaluation illinois How do whales reproduce sexually
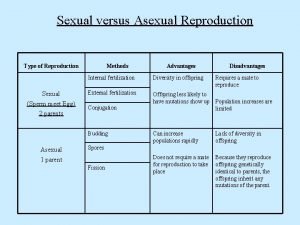
How do whales reproduce sexually Atis sexually or asexually
Atis sexually or asexually What is sexually coercive behavior
What is sexually coercive behavior Body structure of porifera
Body structure of porifera Ad sex
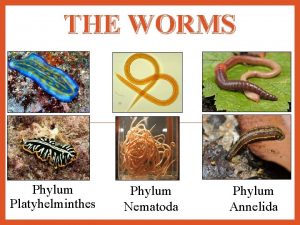
Ad sex Is flatworm asexual reproduction
Is flatworm asexual reproduction Cnidaria class
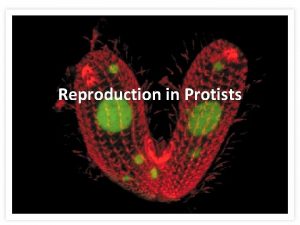
Cnidaria class Asexual reproduction in protists
Asexual reproduction in protists How birds reproduce sexually
How birds reproduce sexually Do worms reproduce sexually or asexually
Do worms reproduce sexually or asexually Parasitism phylum
Parasitism phylum Do jellyfish reproduce sexually
Do jellyfish reproduce sexually Starfish aboral view
Starfish aboral view Functions of hospital pharmacist
Functions of hospital pharmacist The totality of learned socially transmitted behavior
The totality of learned socially transmitted behavior A song transmitted orally which tells a story
A song transmitted orally which tells a story In case of pivot bearing the rate of wear is
In case of pivot bearing the rate of wear is Oblique light examination in questioned document
Oblique light examination in questioned document Electronically transmitted postal ballot system
Electronically transmitted postal ballot system Protein deficiency diseases
Protein deficiency diseases Capnia suffix
Capnia suffix Diseases caused by bacteria
Diseases caused by bacteria Chapter 23 lesson 1 understanding communicable diseases
Chapter 23 lesson 1 understanding communicable diseases In what situation should a nail service not be performed?
In what situation should a nail service not be performed? Whats a sex linked trait
Whats a sex linked trait Nutritional diseases
Nutritional diseases Myth and fallacies about non-communicable diseases
Myth and fallacies about non-communicable diseases Chapter 22 genetics and genetically linked diseases
Chapter 22 genetics and genetically linked diseases Public health entomology certificate
Public health entomology certificate Albugo eye
Albugo eye Mycoplasma
Mycoplasma Consestence
Consestence Examples of communicable diseases
Examples of communicable diseases Non communicable diseases
Non communicable diseases Gingival diseases
Gingival diseases What are periradicular tissues?
What are periradicular tissues? Le mone
Le mone Milady chapter 10 nail disorders and diseases
Milady chapter 10 nail disorders and diseases Female reproductive system diseases
Female reproductive system diseases Periradicular tissues
Periradicular tissues Chapter 6 musculoskeletal system diseases and disorders
Chapter 6 musculoskeletal system diseases and disorders