Severe trauma Trauma management Primary survey Secondary survey

- Slides: 42
Severe trauma
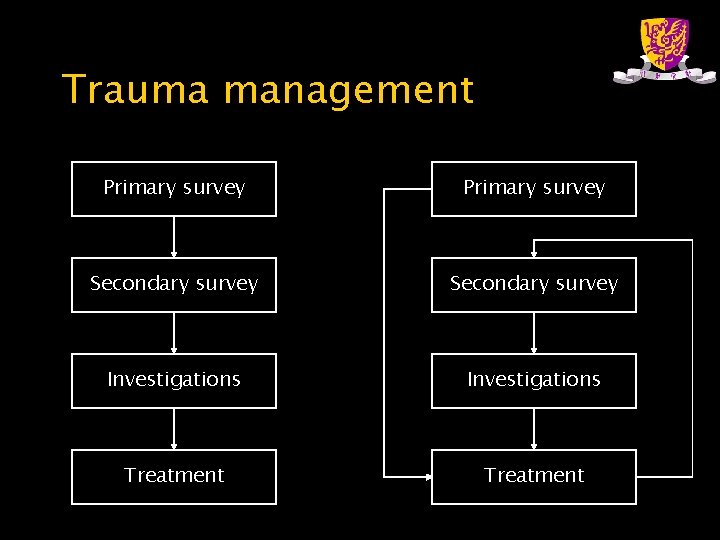
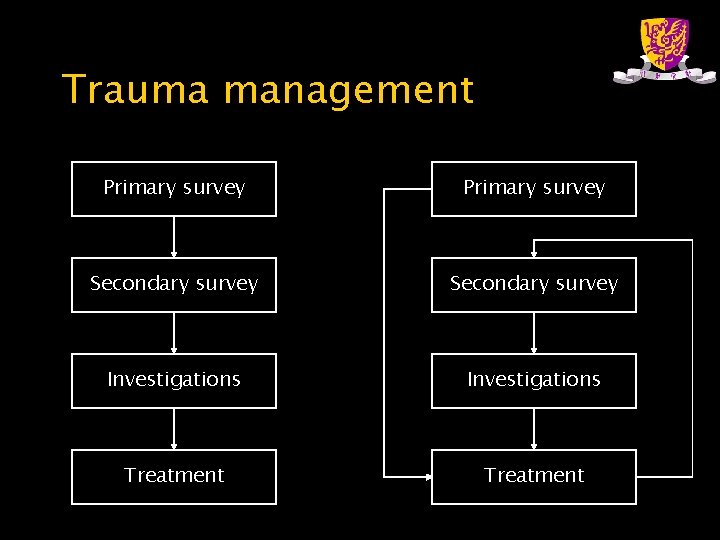
Trauma management Primary survey Secondary survey Investigations Treatment
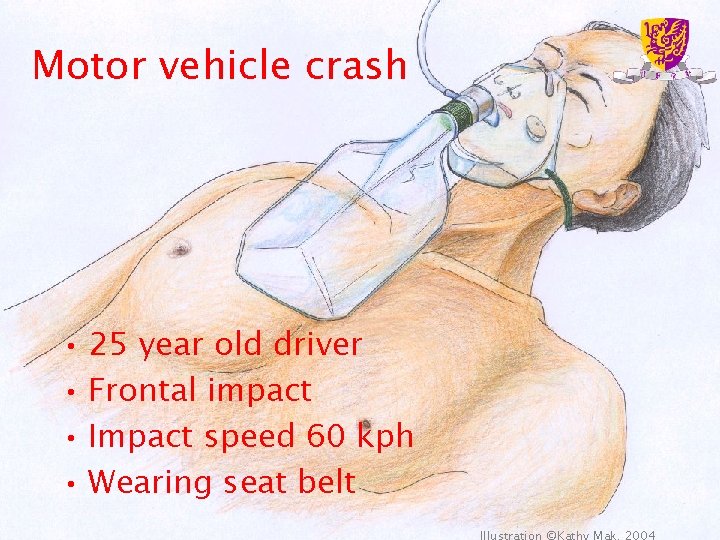
Motor vehicle crash • 25 year old driver • Frontal impact • Impact speed 60 kph • Wearing seat belt
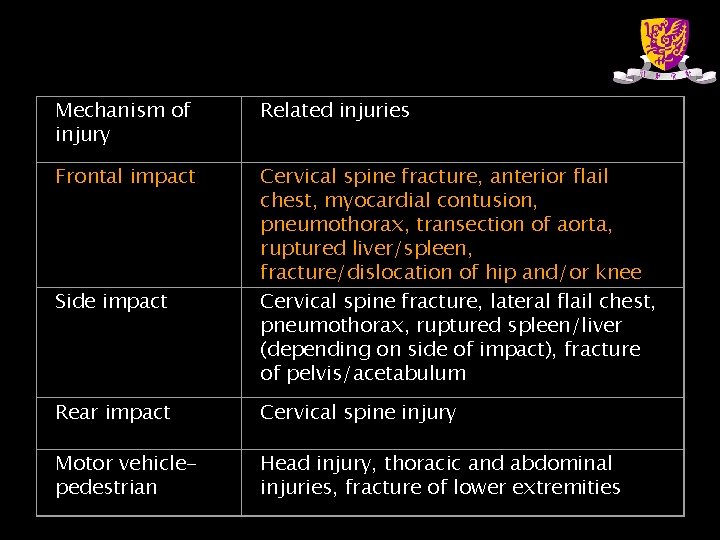
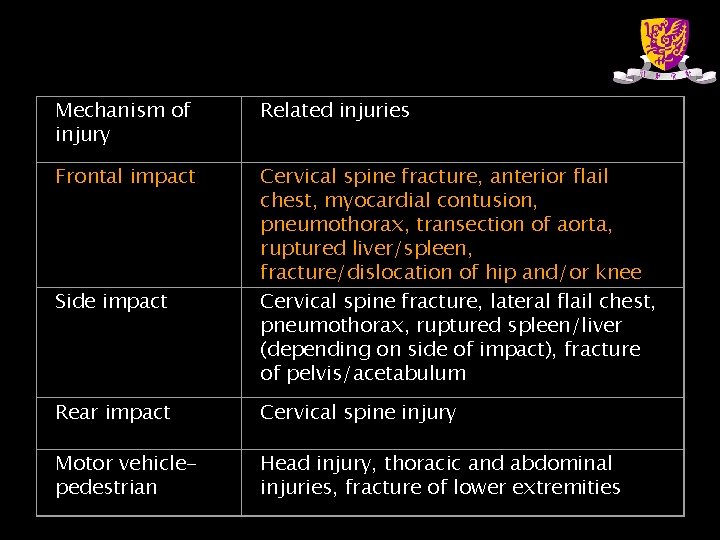
Mechanism of injury Related injuries Frontal impact Cervical spine fracture, anterior flail chest, myocardial contusion, pneumothorax, transection of aorta, ruptured liver/spleen, fracture/dislocation of hip and/or knee Cervical spine fracture, lateral flail chest, pneumothorax, ruptured spleen/liver (depending on side of impact), fracture of pelvis/acetabulum Side impact Rear impact Cervical spine injury Motor vehiclepedestrian Head injury, thoracic and abdominal injuries, fracture of lower extremities
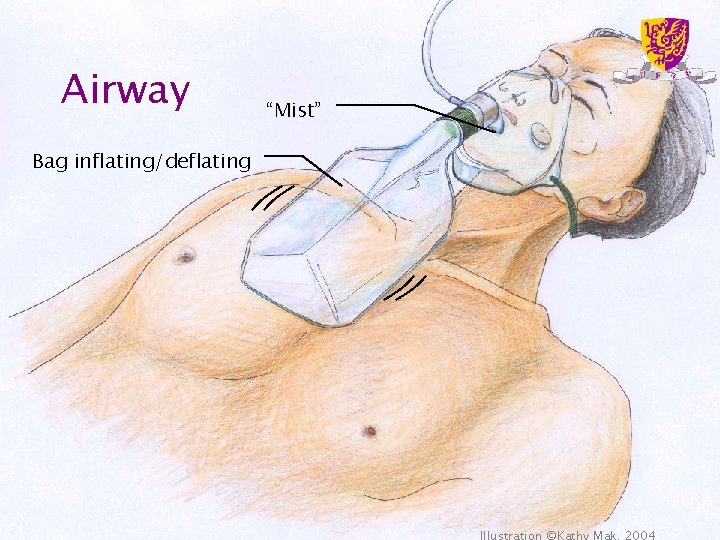
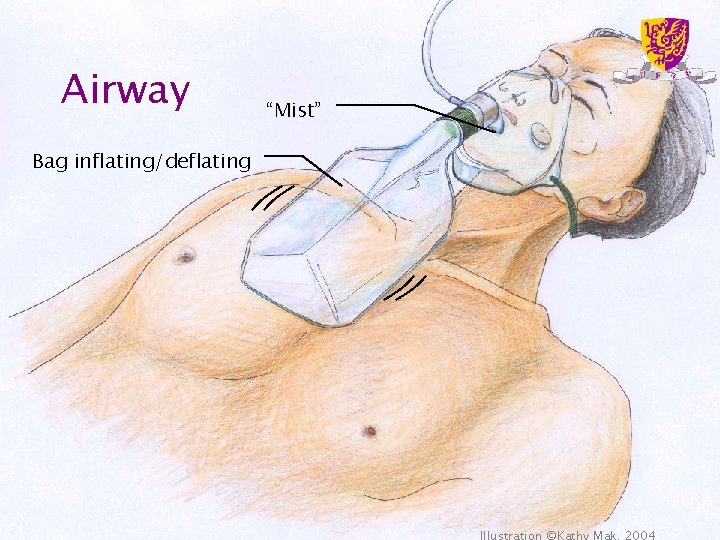
Airway Bag inflating/deflating “Mist”
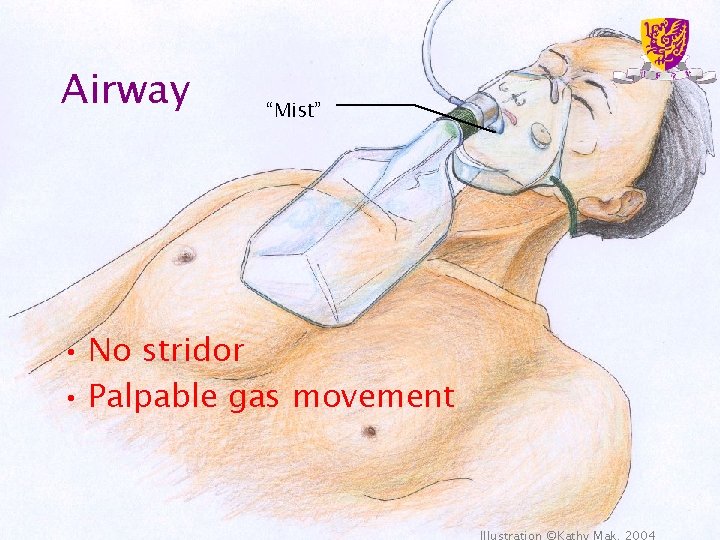
Airway “Mist” • No stridor • Palpable gas movement
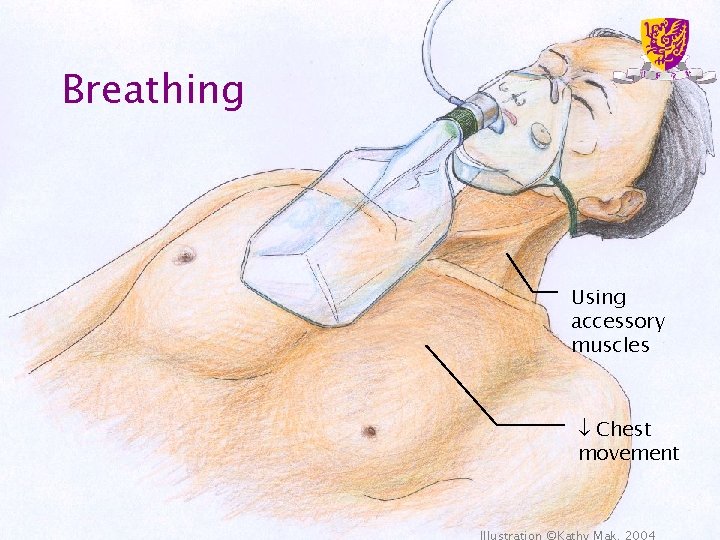
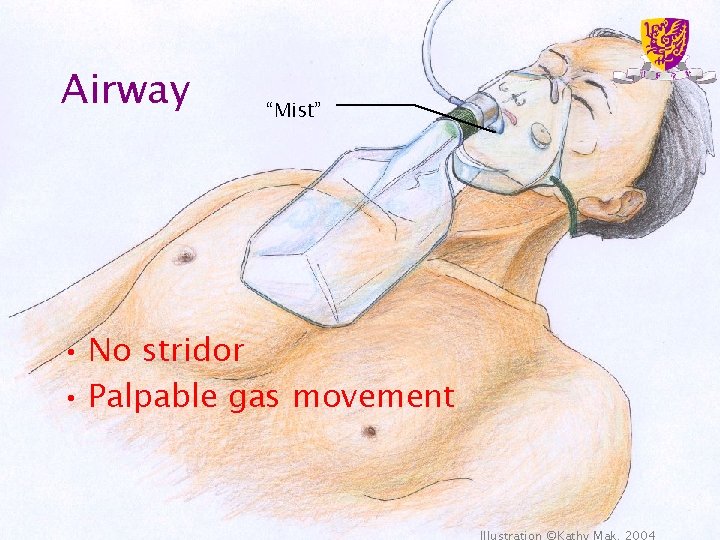
Breathing Using accessory muscles Chest movement
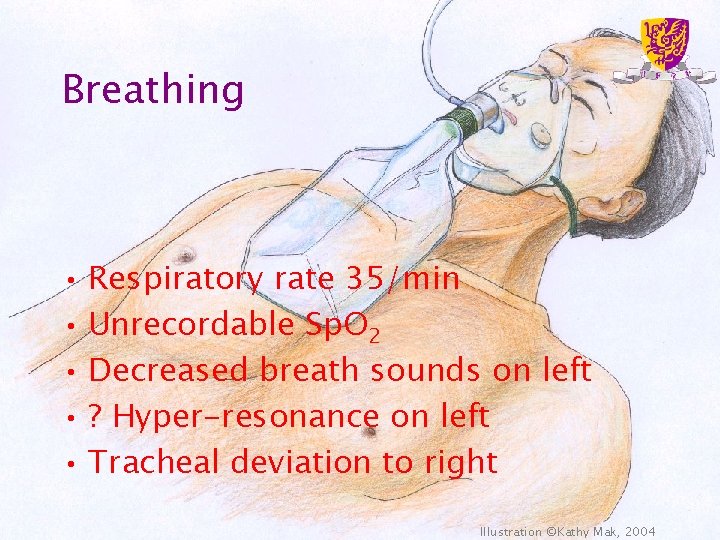
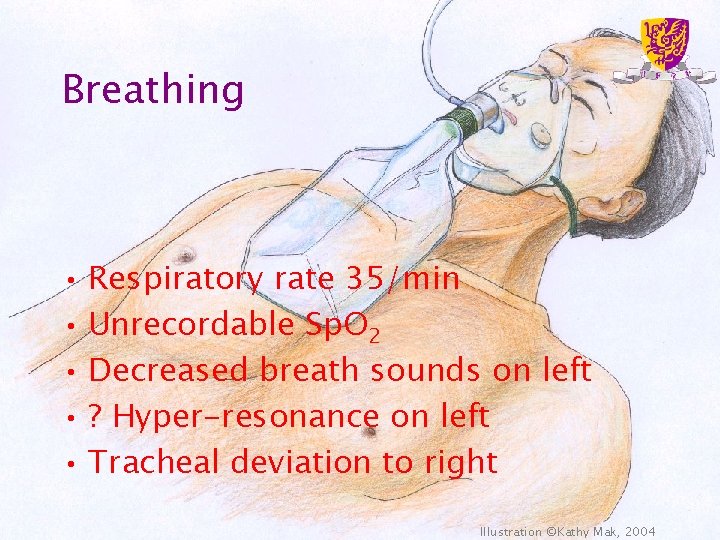
Breathing • Respiratory rate 35/min • Unrecordable Sp. O 2 • Decreased breath sounds on left • ? Hyper-resonance on left • Tracheal deviation to right Illustration ©Kathy Mak, 2004
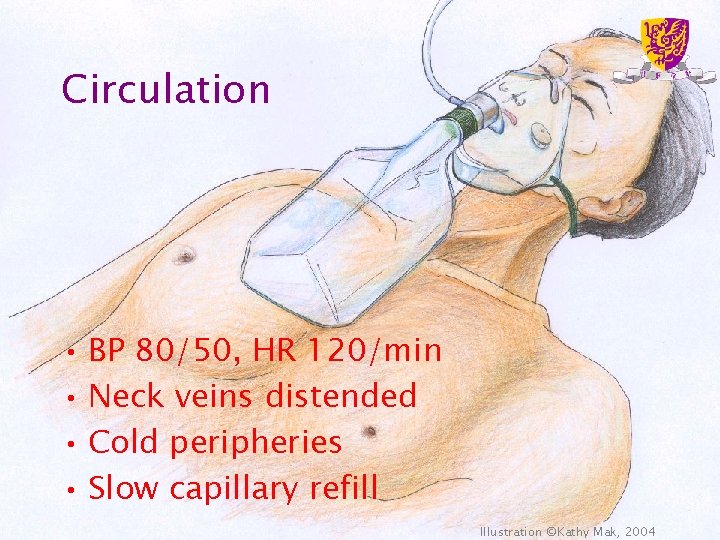
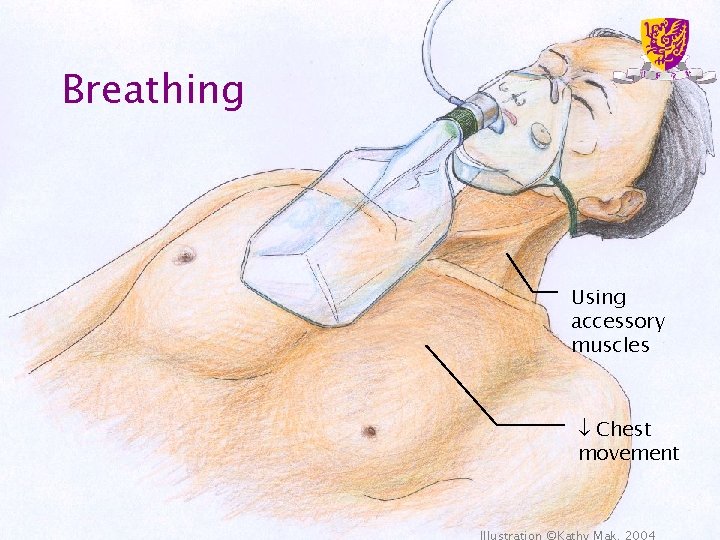
Circulation • BP 80/50, HR 120/min • Neck veins distended • Cold peripheries • Slow capillary refill Illustration ©Kathy Mak, 2004
Shock • Usually due to hypovolaemia • Consider – Tension pneumothorax – Cardiac tamponade – Myocardial contusion – Myocardial infarction
Tension pneumothorax • Clinical features – Respiratory distress – HR, shock – Tracheal deviation (late sign) – Unilateral absence of breath sounds and hyper-resonance (subtle sign) – Distended neck veins • often absent if there is concomitant hypovolaemia – ΔΔ cardiac tamponade
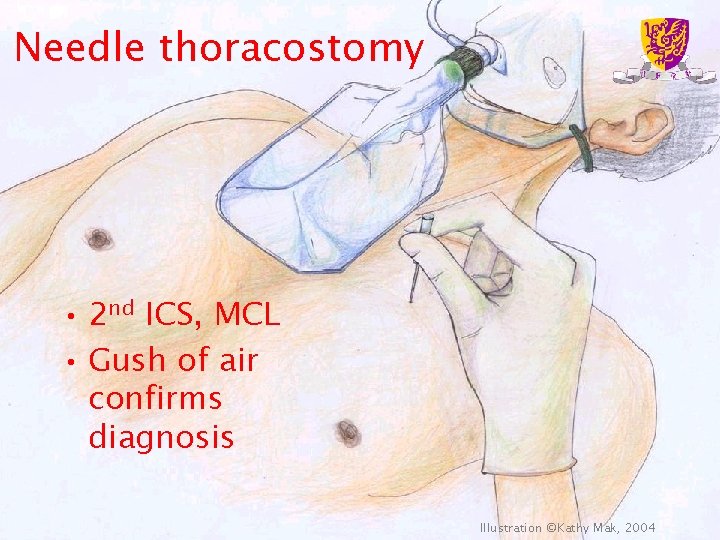
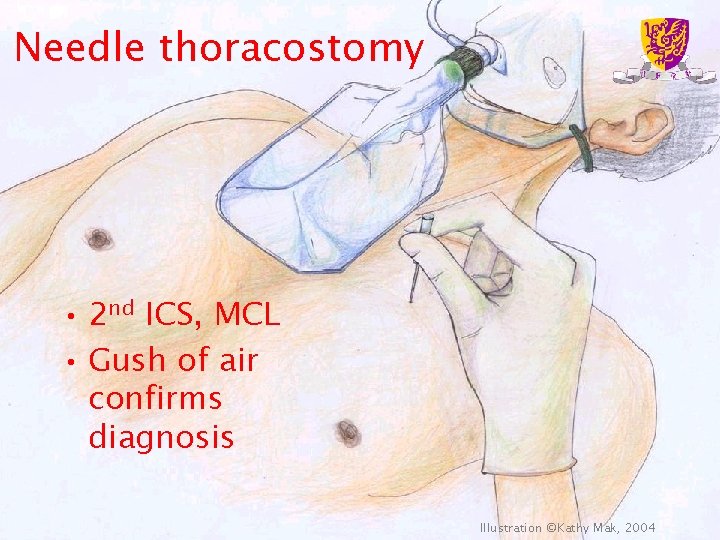
Needle thoracostomy • 2 nd ICS, MCL • Gush of air confirms diagnosis Illustration ©Kathy Mak, 2004
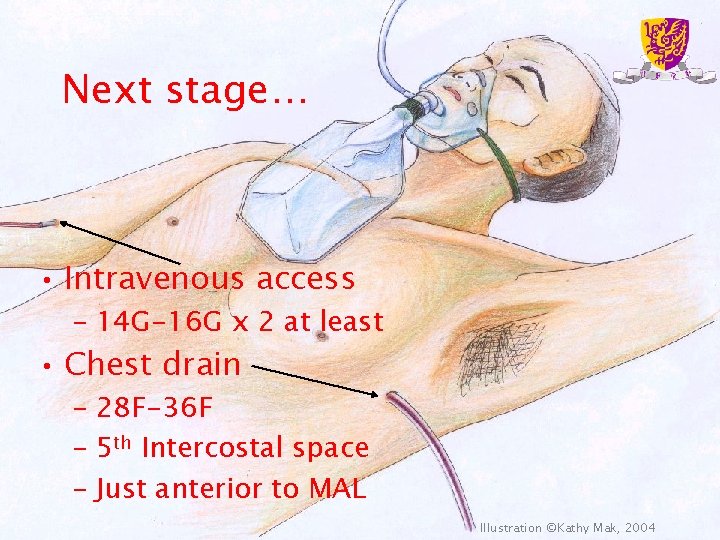
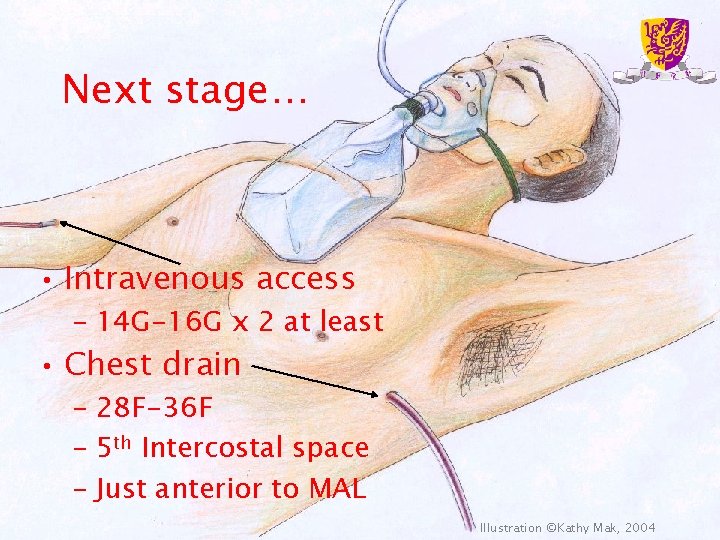
Next stage… • Intravenous access – 14 G-16 G x 2 at least • Chest drain – 28 F-36 F – 5 th Intercostal space – Just anterior to MAL Illustration ©Kathy Mak, 2004
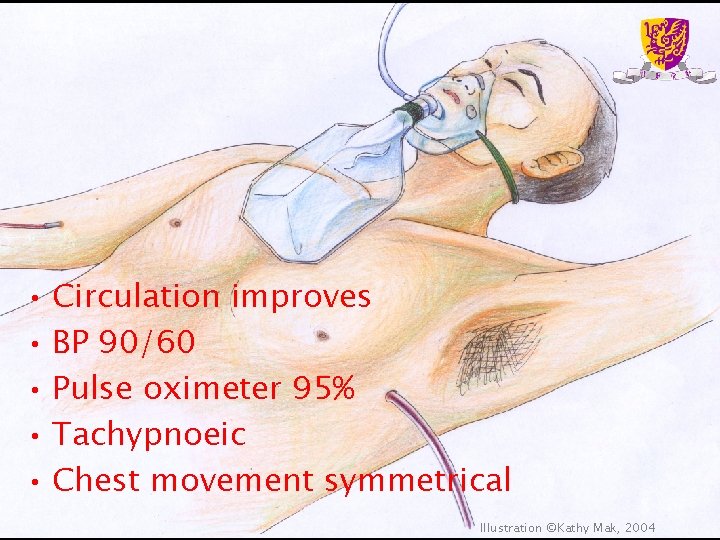
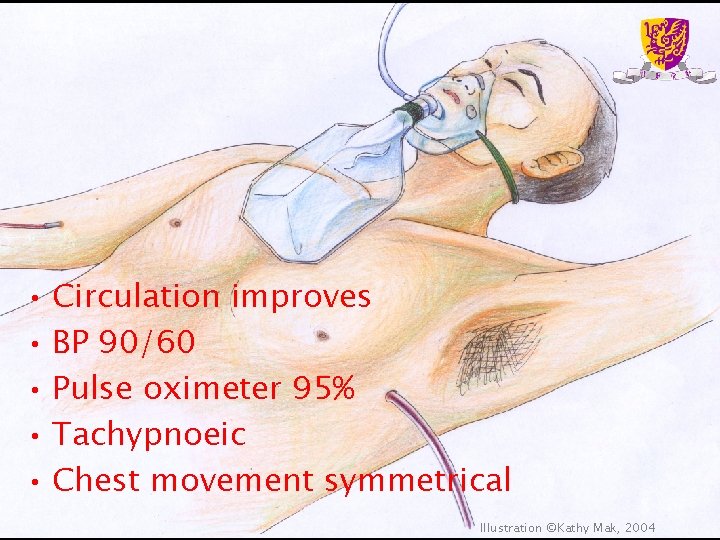
• Circulation improves • BP 90/60 • Pulse oximeter 95% • Tachypnoeic • Chest movement symmetrical Illustration ©Kathy Mak, 2004
Haemodynamic resuscitation • Aim for systolic BP 80 -100 mm. Hg in patients who have not suffered head or spinal injuries
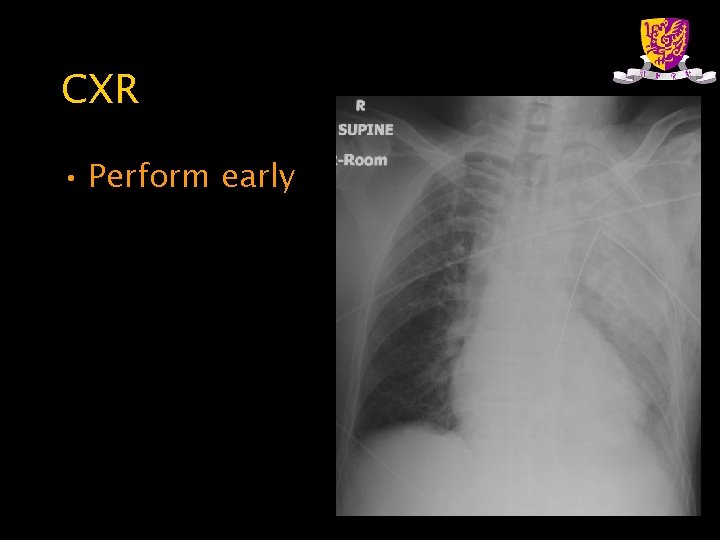
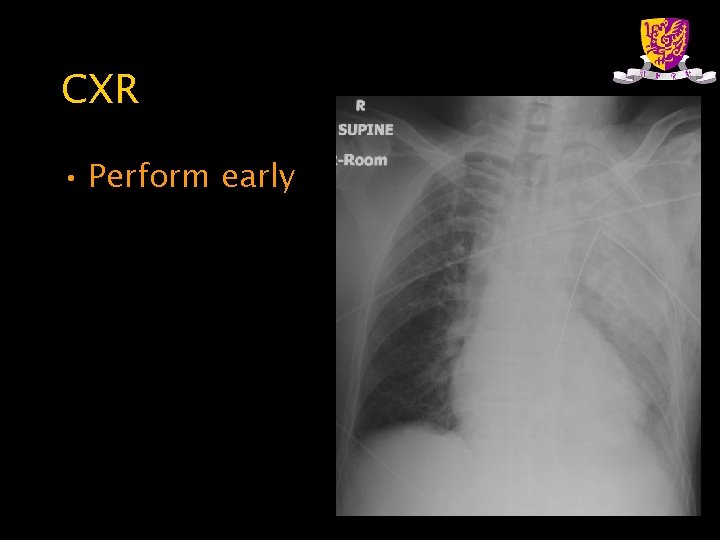
CXR • Perform early
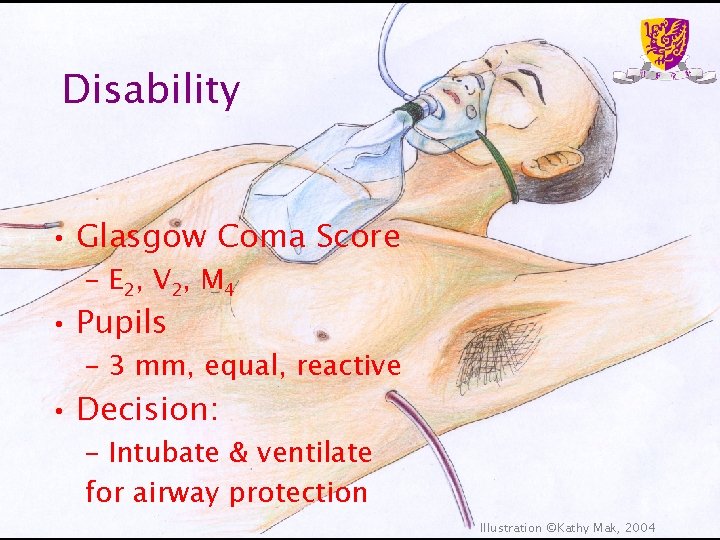
Disability • Glasgow Coma Score – E 2, V 2, M 4 • Pupils – 3 mm, equal, reactive • Decision: – Intubate & ventilate for airway protection Illustration ©Kathy Mak, 2004
Cervical spine injury • Cannot be excluded on clinical grounds in patients with multiple trauma – Distracting injuries – Decreased consciousness • Optimal method of intubation – Controversial – Dependent on skills of operator
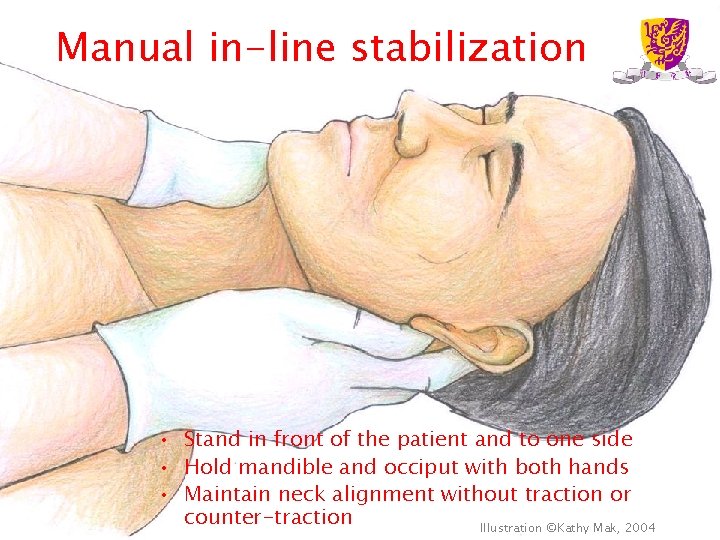
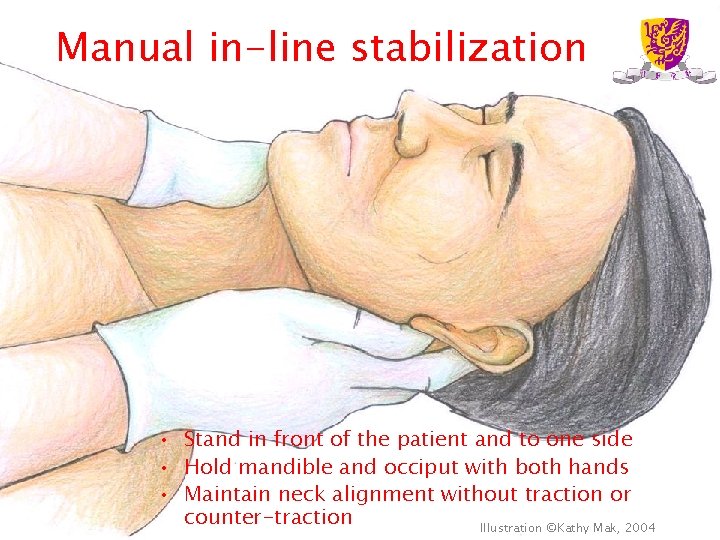
Manual in-line stabilization • Stand in front of the patient and to one side • Hold mandible and occiput with both hands • Maintain neck alignment without traction or counter-traction Illustration ©Kathy Mak, 2004
Intubation • Rapid sequence induction – Pre-oxygenate with tight fitting face mask and 100% O 2 for 3 -5 minutes – Cricoid pressure – Use gum elastic bougie routinely
Intubation • Failed intubation – You MUST have a back-up plan – LMA / Combitube / surgical airway
• Failed intubation • Anaesthetist arrives – Decides to attempt direct laryngoscopy & intubation again after bag-mask ventilation
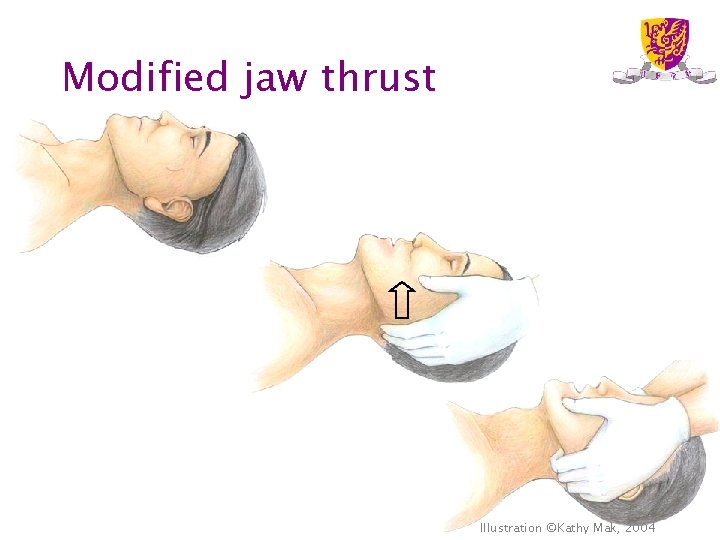
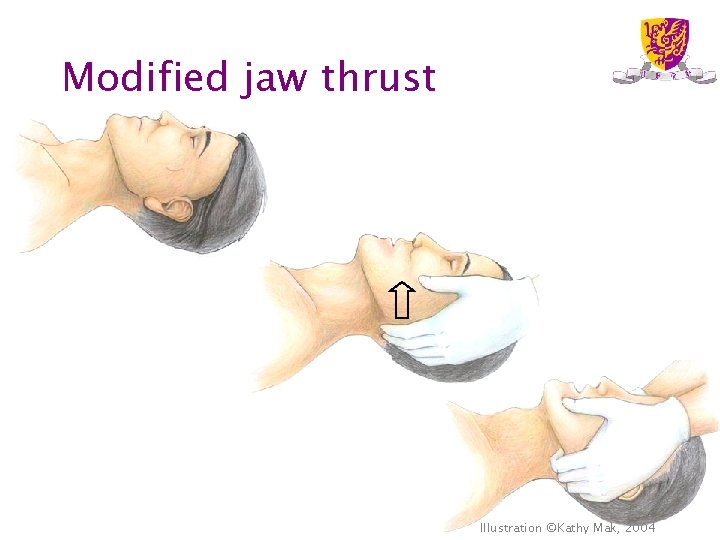
Modified jaw thrust Illustration ©Kathy Mak, 2004
Intubation • Trauma patients are more difficult to intubate • Do not intubate unless – you are skilled in intubation – dire emergency • Get expert help early
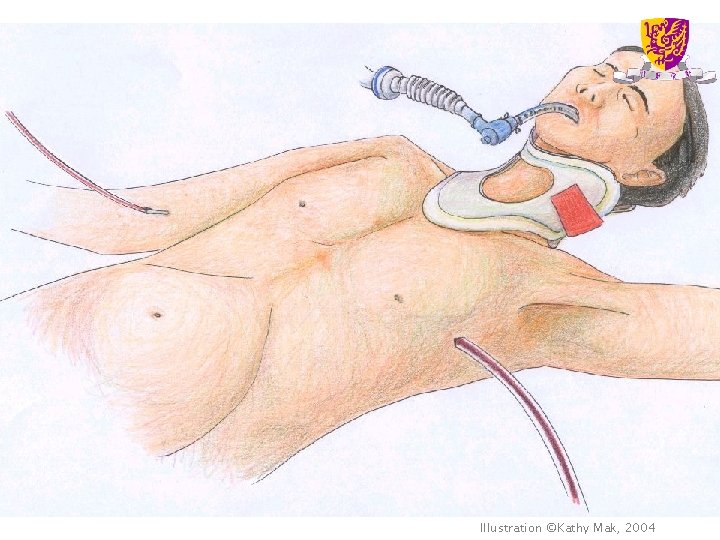
Illustration ©Kathy Mak, 2004
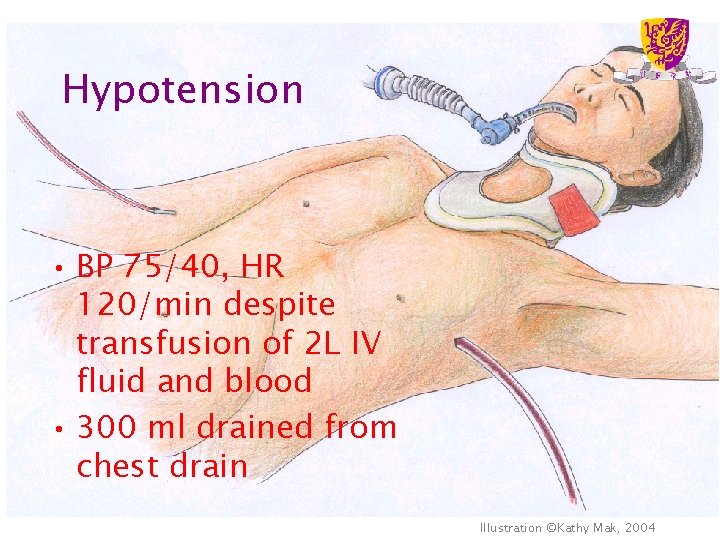
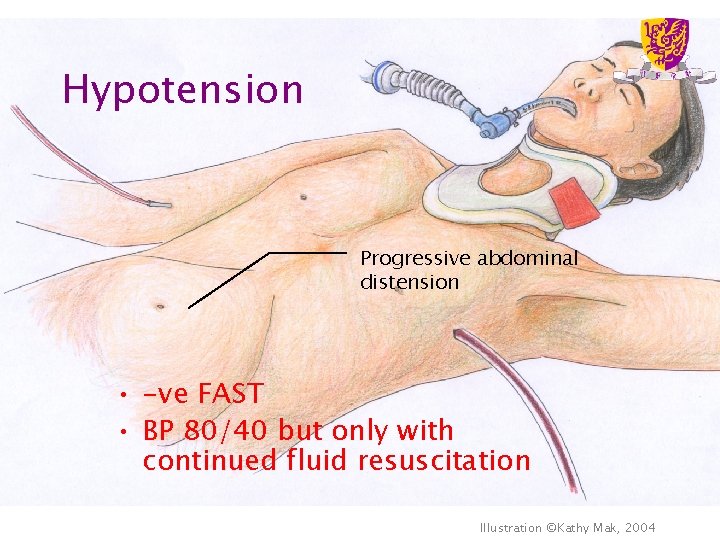
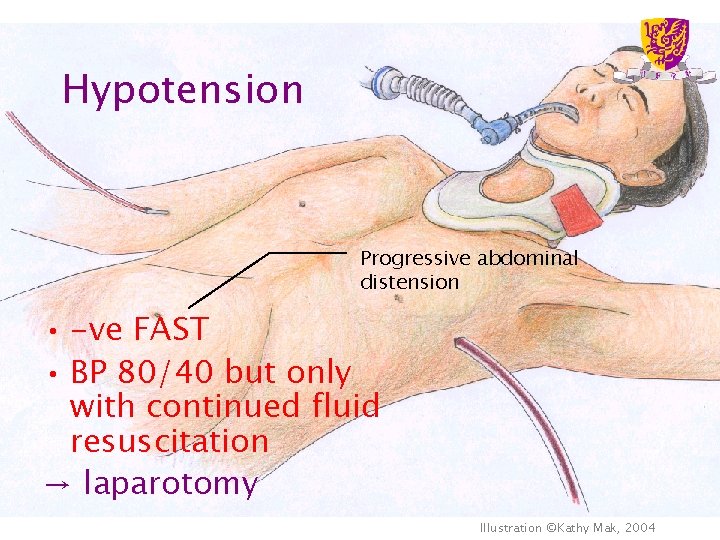
Hypotension • BP 75/40, HR 120/min despite transfusion of 2 L IV fluid and blood • 300 ml drained from chest drain Illustration ©Kathy Mak, 2004
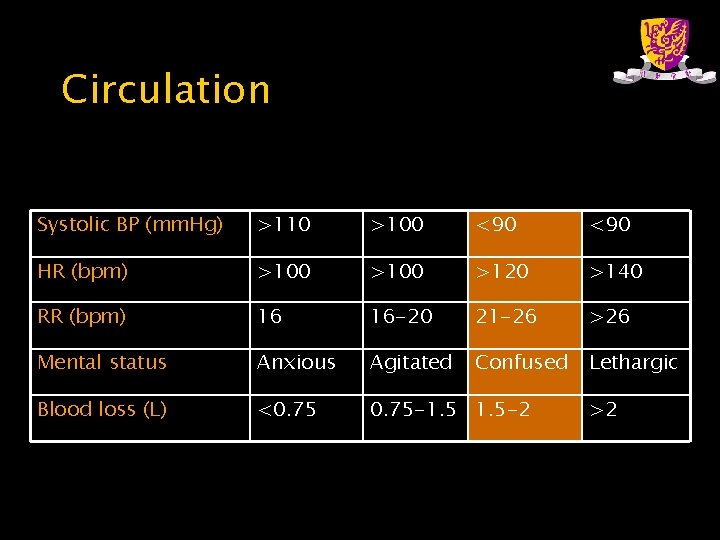
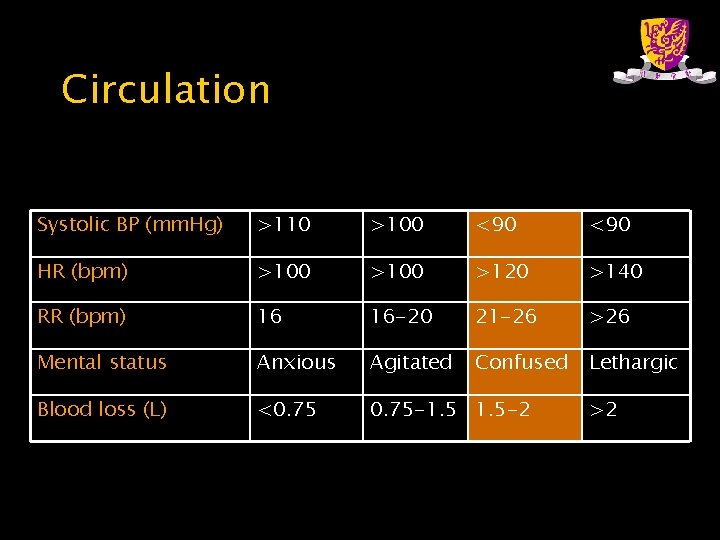
Circulation Systolic BP (mm. Hg) >110 >100 <90 HR (bpm) >100 >120 >140 RR (bpm) 16 16 -20 21 -26 >26 Mental status Anxious Agitated Confused Lethargic Blood loss (L) <0. 75 -1. 5 -2 >2
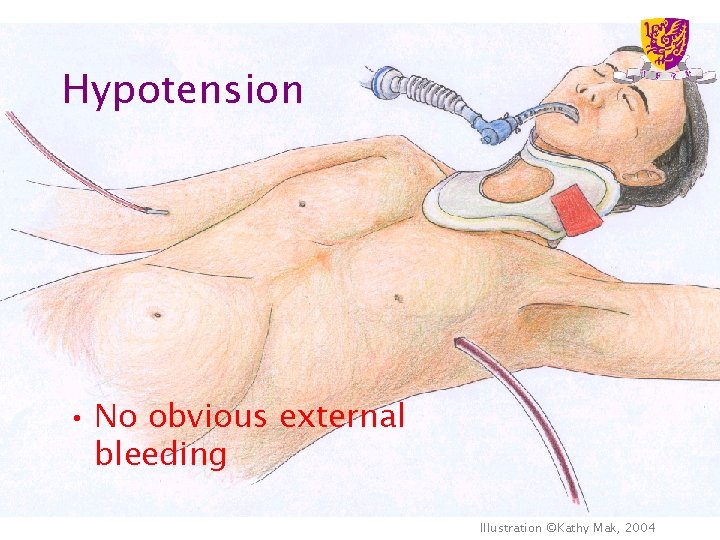
Hypotension • No obvious external bleeding Illustration ©Kathy Mak, 2004
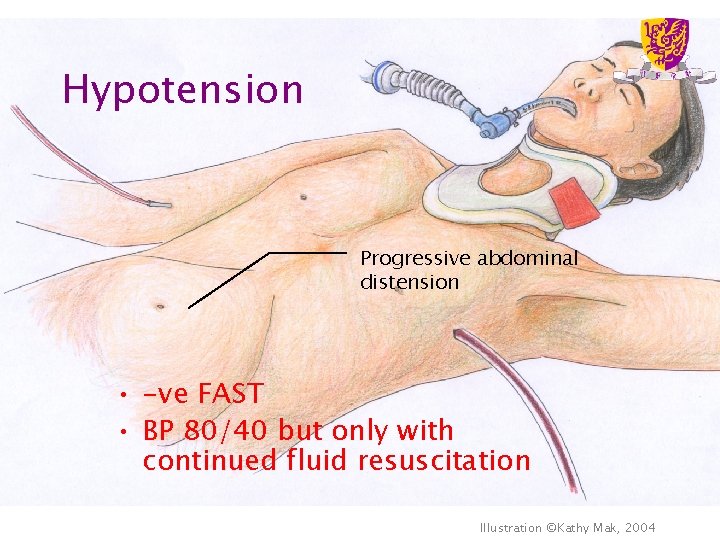
Hypotension Progressive abdominal distension • -ve FAST • BP 80/40 but only with continued fluid resuscitation Illustration ©Kathy Mak, 2004
Investigations • CT abdomen – Contraindicated in haemodynamically unstable patients • Diagnostic peritoneal lavage – Limited utility in developed countries • Laparotomy
Diagnostic peritoneal lavage • Indications – Abdominal examination is equivocal (eg lower rib, lumbar spine or pelvic fractures causing abdominal tenderness and guarding) and CT is not available (e. g. , developing countries) – Repeated abdominal examination impractical because of anticipated lengthy x-ray studies or GA for extra- abdominal injuries
Diagnostic peritoneal lavage • Contraindications – Absolute: existing indication for laparotomy, including haemodynamic instability – Relative: • Pregnancy • Significant obesity • Previous abdominal surgery • In these situations (or with pelvic fractures) supraumbilical open method should be used
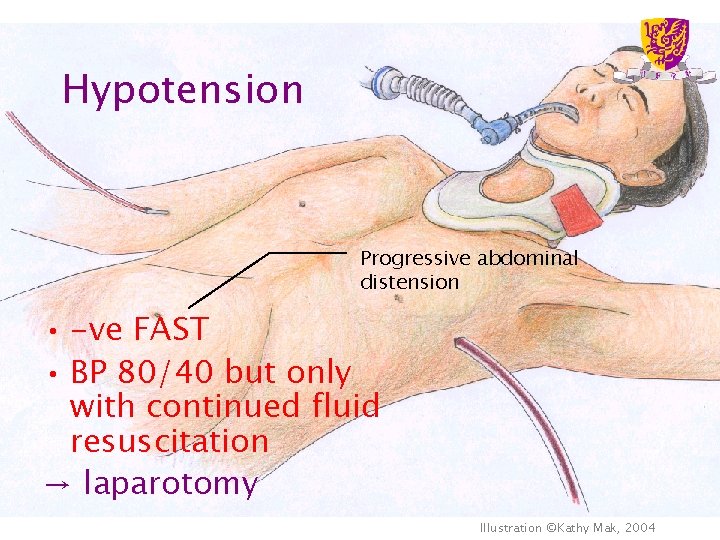
Hypotension Progressive abdominal distension • -ve FAST • BP 80/40 but only with continued fluid resuscitation → laparotomy Illustration ©Kathy Mak, 2004
Post-op intensive care • History – – – – Mechanism of trauma Identified injuries Injuries that have been excluded Operative findings Supportive and definitive treatment Blood loss & blood/fluid transfused Laboratory results Past medical history, drug allergies etc
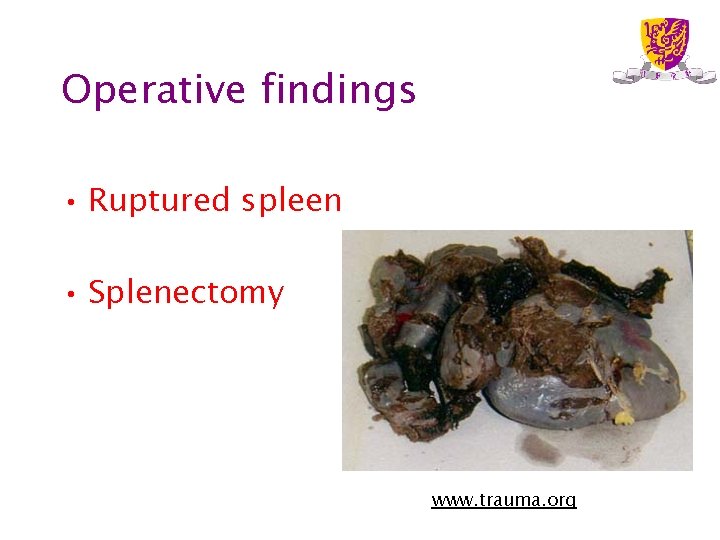
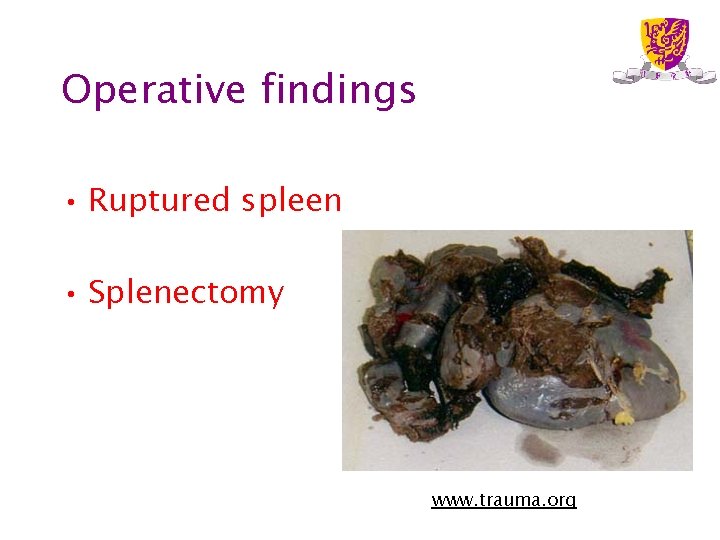
Operative findings • Ruptured spleen • Splenectomy www. trauma. org

ABCD Illustration ©Kathy Mak, 2004
ABCDE • Breathing – Symmetrical chest movement & breath sounds – Sp. O 2, ABG • Circulation – IV access – Appropriate monitoring – BP, HR, CVP • Disability – Level of consciousness – Limb movements – Cervical spine immobilization & logroll • Exposure and environment control – Look for other injuries and prevent hypothermia
Secondary survey • Fill in the gaps • Look for problems that have become apparent with time
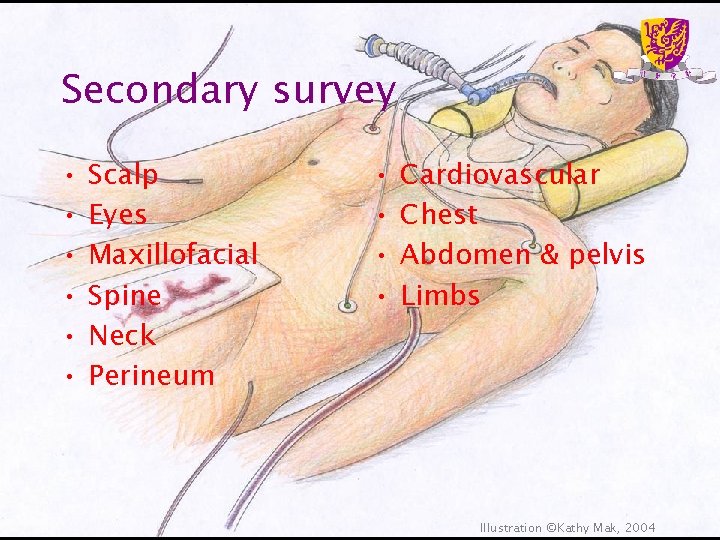
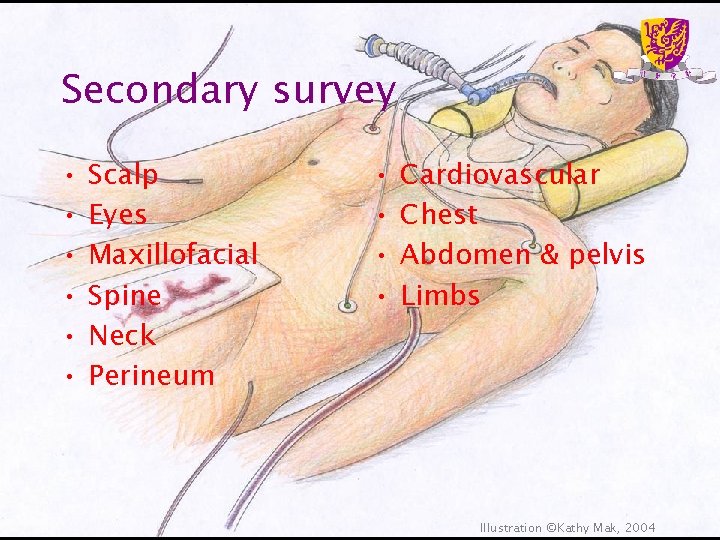
Secondary survey • • • Scalp Eyes Maxillofacial Spine Neck Perineum • • Cardiovascular Chest Abdomen & pelvis Limbs Illustration ©Kathy Mak, 2004
Investigations • Routine bloods • Radiology – CT brain – Cervical spine lateral & AP, cervical CT – Pelvis XR – CXR • ECG
Management • Continued resuscitation – Target higher BP if haemostasis achieved • Seek for and exclude other injuries • Correct coagulopathy, acidosis, hypothermia • Treat complications – Organ failure – Distributive shock
Summary • Methodical ABCDE approach • Primary survey • Resuscitation simultaneously • Emergency surgery if required • Secondary survey • Imaging • Definitive care (OT and ICU)