SEVERE SEPSIS MULTIORGAN DYSFUNCTION SYNDROME MODS Michelle Liz






- Slides: 22
SEVERE SEPSIS & MULTI-ORGAN DYSFUNCTION SYNDROME (MODS) Michelle Liz LIU Post Dietetic Intern 5/5/14
Background Sepsis, severe sepsis and septic shock refer to an inflammatory state resulting from the systemic response to a bacterial infection. In most cases, septic shock is caused by hospital-acquired gram -positive cocci or gram-negative bacilli and often occurs in immunocompromised patients with chronic and debilitating diseases. Common sites of infection that lead to severe sepsis or septic shock include the lungs, and the biliary, urinary, and gastrointestinal (GI) tracts. In 2002, there were 400, 000 cases of sepsis, 300, 000 cases of severe sepsis and 200, 000 cases of septic shock in the United States. Today, it is estimated that there are more than 1, 000 cases of sepsis in the United states among hospitalized patients each year.
Severe sepsis & Septic shock Severe Sepsis Severe sepsis is accompanied by the failure of at least one organ The most common signs of severe sepsis include cardiovascular failure, renal failure, respiratory failure and hematologic failure Cardiovascular→ Hypotension Renal failure → Oliguria Respiratory failure → Hypoxemia Hematologic failure→ Septic Shock Septic shock is defined as severe sepsis with organ hypoperfusion and hypotension that respond poorly to fluid resuscitation. Septic shock occurs most often in patients >35 years of age, pregnant women and neonates
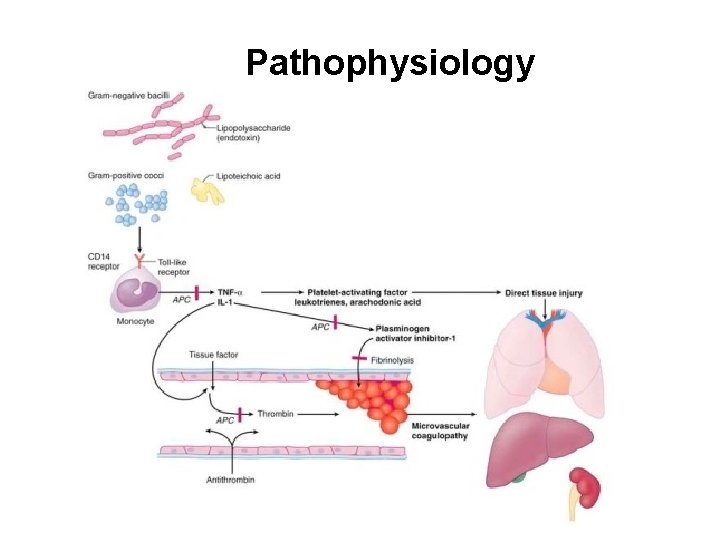
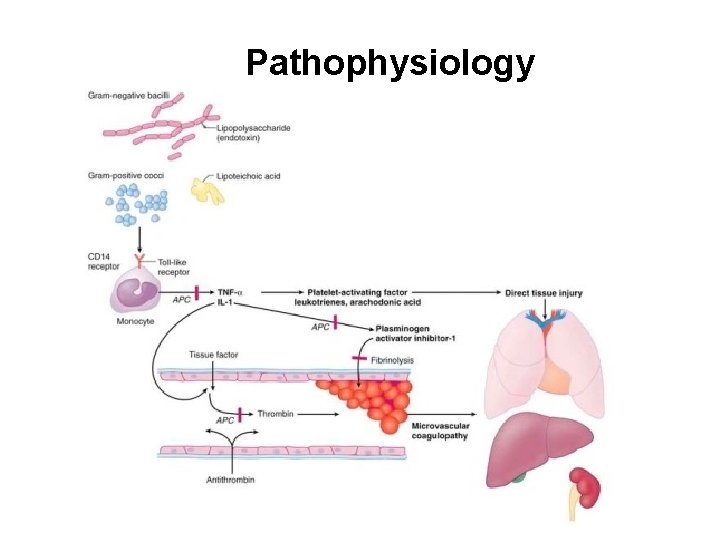
Pathophysiology

Diagnosis & Treatment The diagnosis for sepsis is clinical and based on analyzing: Complete blood count (CBC ) Arterial blood gases (ABGs) --- Pa. CO 2, HCO 3 Chest x –Ray Sublingual PCO 2 Lactate levels Liver function Treatment Fluid resuscitation with 0. 9% Saline: ↑ CVP Dopamine: to ↑ BP Oxygen- by mechanical ventilation or tracheal intubation Parenteral antibiotics

Nutritional Implications Septic shock may lead to gut hypoperfusion (decreased blood flow through an organ). Therefore, early enteral feedings are initiated to restore gut function. Stimulation by enteral nutrients decreases bacterial translocation and results in a decreased length of hospital stay. EN should be initiated within 48 hrs of admission and provide at least 60 -70% of the patients estimated energy needs. Protein needs are increased to 1. 5 -2. 0 g/kg of actual body weight (ABW), and energy needs are increased at 3035 kcal/kg. When patients are able to consume a po diet, a soft diet that
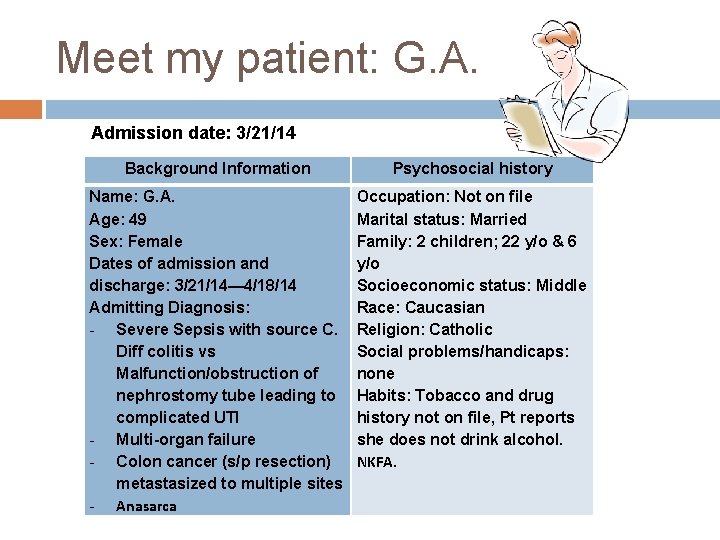
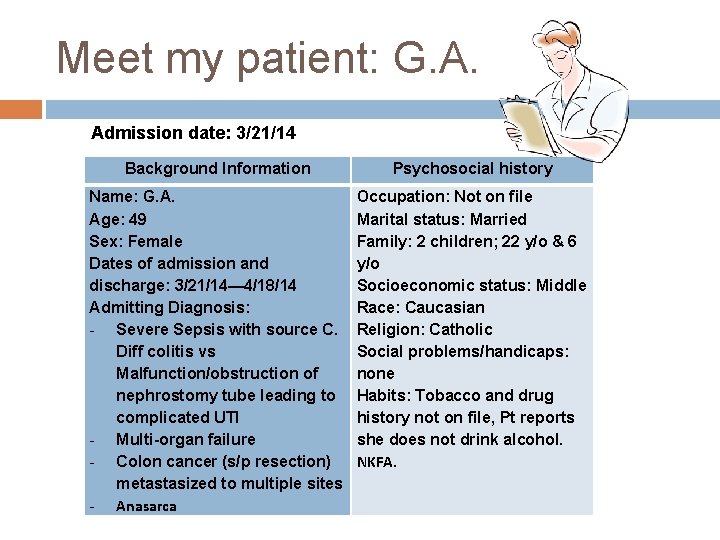
Meet my patient: G. A. Admission date: 3/21/14 Background Information Psychosocial history Name: G. A. Age: 49 Sex: Female Dates of admission and discharge: 3/21/14— 4/18/14 Admitting Diagnosis: - Severe Sepsis with source C. Diff colitis vs Malfunction/obstruction of nephrostomy tube leading to complicated UTI - Multi-organ failure - Colon cancer (s/p resection) metastasized to multiple sites - Anasarca Occupation: Not on file Marital status: Married Family: 2 children; 22 y/o & 6 y/o Socioeconomic status: Middle Race: Caucasian Religion: Catholic Social problems/handicaps: none Habits: Tobacco and drug history not on file, Pt reports she does not drink alcohol. NKFA.
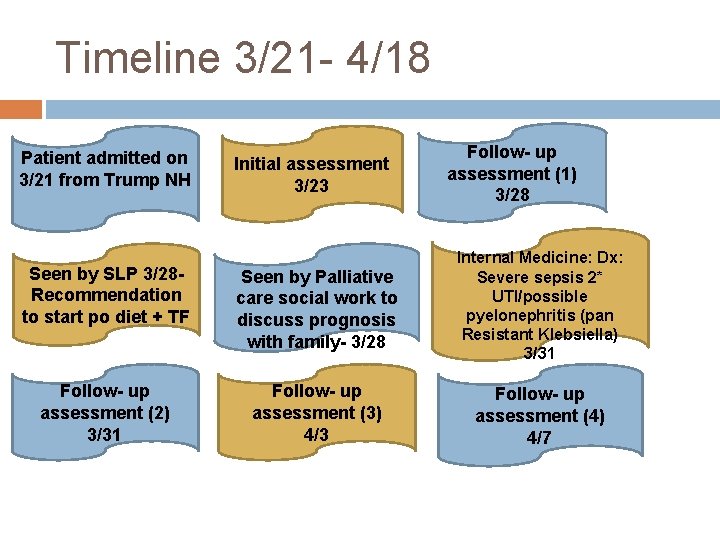
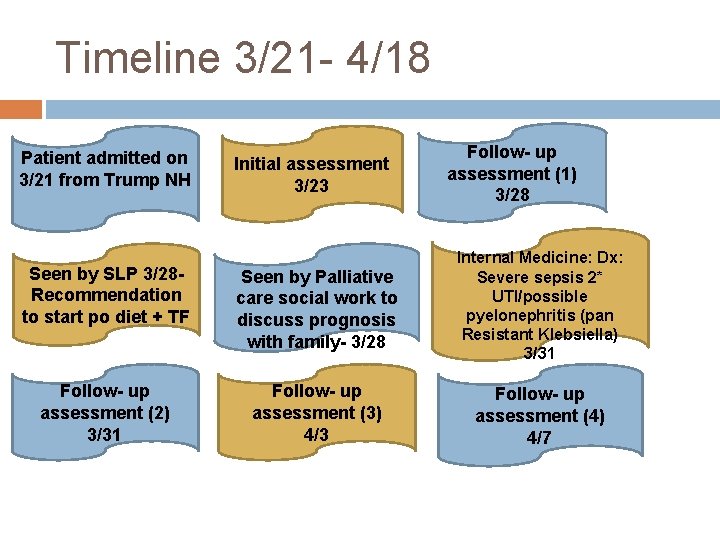
Timeline 3/21 - 4/18 Patient admitted on 3/21 from Trump NH Initial assessment 3/23 Follow- up assessment (1) 3/28 Seen by SLP 3/28 Recommendation to start po diet + TF Seen by Palliative care social work to discuss prognosis with family- 3/28 Internal Medicine: Dx: Severe sepsis 2* UTI/possible pyelonephritis (pan Resistant Klebsiella) 3/31 Follow- up assessment (2) 3/31 Follow- up assessment (3) 4/3 Follow- up assessment (4) 4/7
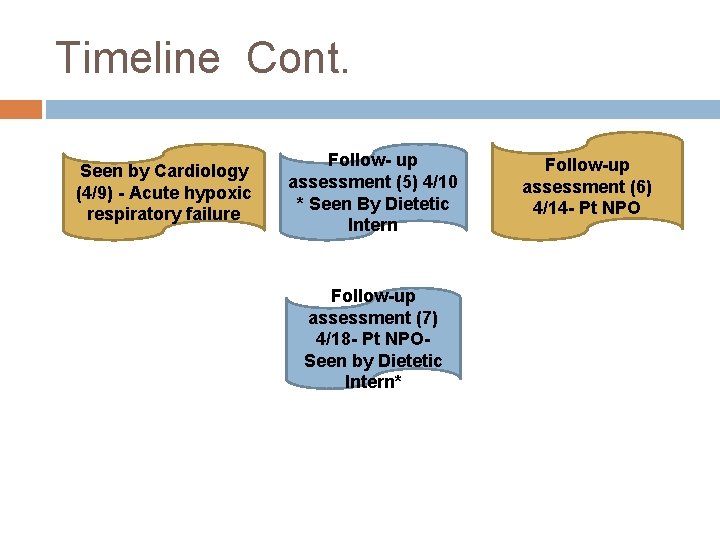
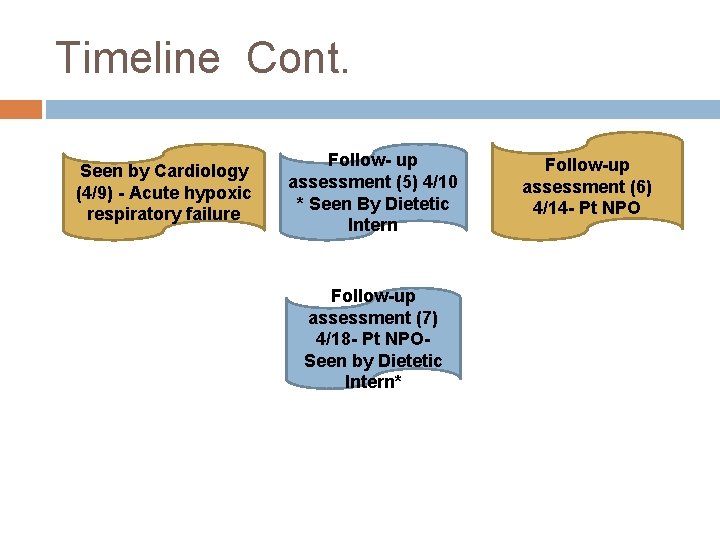
Timeline Cont. Seen by Cardiology (4/9) - Acute hypoxic respiratory failure Follow- up assessment (5) 4/10 * Seen By Dietetic Intern Follow-up assessment (7) 4/18 - Pt NPOSeen by Dietetic Intern* Follow-up assessment (6) 4/14 - Pt NPO
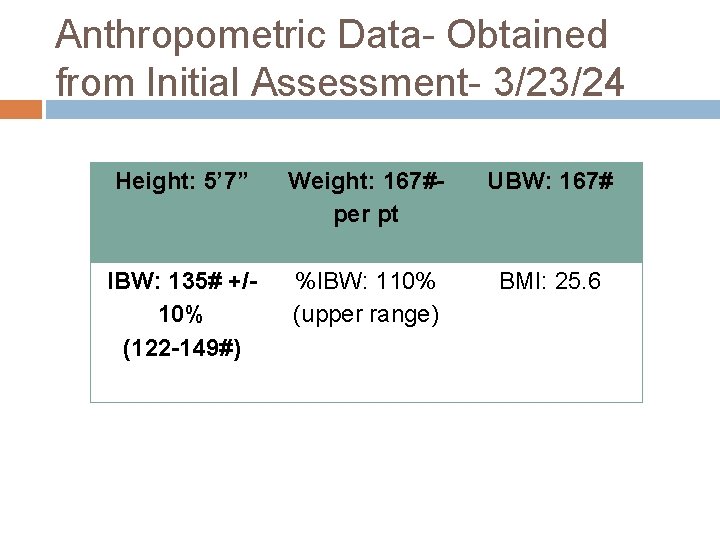
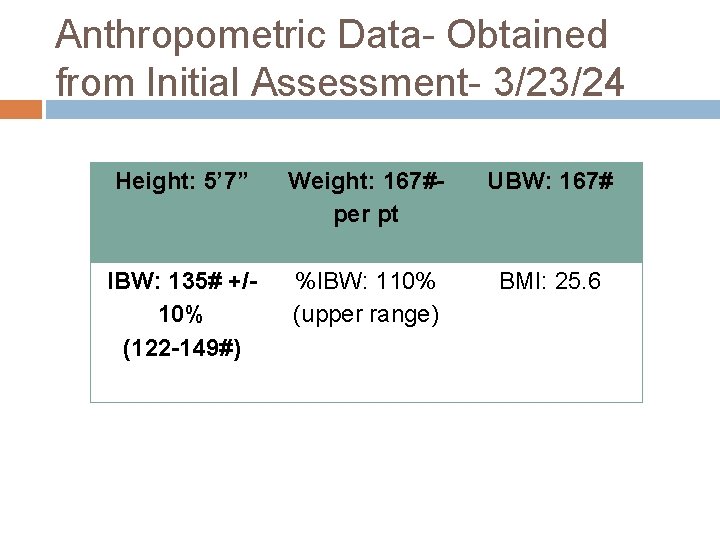
Anthropometric Data- Obtained from Initial Assessment- 3/23/24 Height: 5’ 7” Weight: 167#per pt UBW: 167# IBW: 135# +/10% (122 -149#) %IBW: 110% (upper range) BMI: 25. 6

Pertinent Medications throughout G. A. ’s hospital stay Protonix: Anti. Gerd; May ↓ absorption of Fe, ↓ Vit B 12. ↓Gastric acid secretion, ↑gastric p. H, may cause nausea, abdominal pain and diarrhea (Pronsky& Crowe, 2010, p. 260). Bacid: Biotherapeutic agent, Antidiarrheal; Take separately from antibiotics by ≥ 2 hrs. May cause burping, vomiting, diarrhea and transient flatulence (Pronsky & Crowe, 2010, p. 178). Levothyroxine: Thyroid hormone (T 4); May cause appetite changes, ↓wt. May also cause nausea and diarrhea (Pronsky & Crowe, 2010, p. 303). Duragesic: Analgesic, narcotic, Opoid- May cause anorexia, dry mouth, dyspepsia, N/V, abdominal pain, constipation, flatulence and diarrhea. Caution with ↓ renal function and ↓ pulmonary function. May also cause respiratory depression, weakness, ↑ or ↓ BP, and edema (Pronsky & Crowe, 2010, p. 133). Polymyxin B: Antibiotic; May cause anorexia, interferes with Fol absorption. May also ↑ BUN, ↑Creat, ↑K and ↓Na (Pronsky & Crowe, 2010, p. 314). Flagyl: Antibiotic- May cause anorexia, dry mouth, N/V, diarrhea and constipation (Pronsky & Crowe, 2010, p. 207). Oxycodone: Analgesic, narcotic; May cause anorexia, dry mouth, dyspepsia, gastritis, N/V, diarrhea and constipation. May ↓ Na. May also cause fatigue, weakness and hypotension (may be severe) (Pronsky & Crowe, 2010, p. 233). Dopamine: Pressure agent; improves blood flow to the kidneys. May cause chest pain, uneven heartbeats, and shallow breathing (http: //www. ncbi. nlm. nih. gov/pubmedhealth/PMHT 0010016/? report=details#side_effects) Linezolid: Antibiotic- May cause N/V, diarrhea and bleeding. May also cause headache, dyspnea and may ↑ BUN (Pronsky & Crowe, 2010, p. 187). Merrem: Antibiotic- May cause N/V, diarrhea, constipation, headache and apnea. May also ↑ BUN and Creatinine (Pronsky & Crowe, 2010, p. 199).

Evaluation of Labs throughout G. A. ’s hospital stay Glucose mg/d. L (3/28 -4/18) 65↓, 83, 82, 59↓, 65↓, 80, 98 ↓ with insulin overdose, islet-cell carcinoma, bacterial sepsis, hypothyroidism, Addison’s disease, extensive liver disease, glycogen storage disease, alcohol abuse, starvation, vigorous exercise, pancreatitis and oral hypoglycemic drugs (Pronksy & Crowe, 2010, p. 345). BUN mg/d. L (3/28 -4/18) 62↑, 64↑, 65↑, 66↑, 62↑, 60↑, 56↑ ↑ with renal failure, shock, dehydration, infection, DM, chronic gout, excessive pro intake/catabolism, and MI (Pronsky & Crowe, 2010, p. 342). Creatinine mg/d. L (3/28 -4/18) 1. 9↑, 1. 7↑, 1. 5↑, 1. 4↑, 1. 3↑, 1. 4↑, 1. 1↑ ↑ with acute & chronic renal disease, muscle damage, hyperthyroidism, muscle mass, starvation, diabetic acidosis, high meat intake, gigantism and acromegaly (Pronsky & Crowe, 2010, p. 344). Na m. Eq/L (3/28 -4/18) 134↓, 138, 137, 138, 136↓, 137, 130↓ ↓ with edema, severe burns, severe diarrhea/vomiting, Addison’s disease, severe nephritis, starvation, hyperglycemia, malabsorption and AIDS (Pronsky & Crowe, 2010, p. 352). K m. Eq/L (3/28 -4/18) 5. 3↑, 3. 6, 3. 8, 4. 1, 4. 8 ↑renal failure, tissue damage, acidosis, Addison’s, uncontrolled DM, internal hemorrhage, overuse of K supplements and acute AIDS. GFR (4/10*) 40↓ Moderate decrease in kidney function (Wilkens, Juneja & Shanaman, 2012, p. 811).
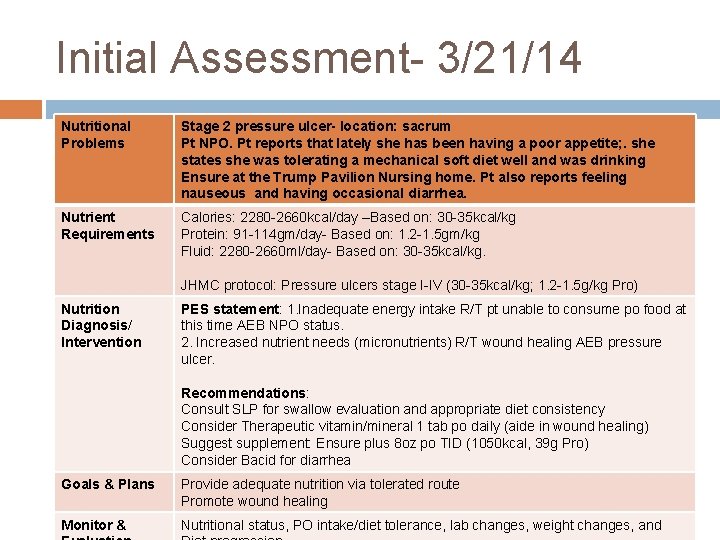
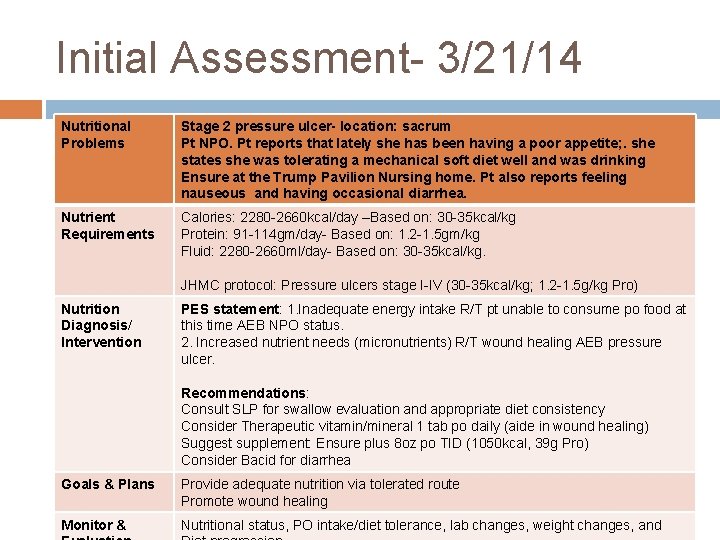
Initial Assessment- 3/21/14 Nutritional Problems Stage 2 pressure ulcer- location: sacrum Pt NPO. Pt reports that lately she has been having a poor appetite; . she states she was tolerating a mechanical soft diet well and was drinking Ensure at the Trump Pavilion Nursing home. Pt also reports feeling nauseous and having occasional diarrhea. Nutrient Requirements Calories: 2280 -2660 kcal/day –Based on: 30 -35 kcal/kg Protein: 91 -114 gm/day- Based on: 1. 2 -1. 5 gm/kg Fluid: 2280 -2660 ml/day- Based on: 30 -35 kcal/kg. JHMC protocol: Pressure ulcers stage I-IV (30 -35 kcal/kg; 1. 2 -1. 5 g/kg Pro) Nutrition Diagnosis/ Intervention PES statement: 1. Inadequate energy intake R/T pt unable to consume po food at this time AEB NPO status. 2. Increased nutrient needs (micronutrients) R/T wound healing AEB pressure ulcer. Recommendations: Consult SLP for swallow evaluation and appropriate diet consistency Consider Therapeutic vitamin/mineral 1 tab po daily (aide in wound healing) Suggest supplement: Ensure plus 8 oz po TID (1050 kcal, 39 g Pro) Consider Bacid for diarrhea Goals & Plans Provide adequate nutrition via tolerated route Promote wound healing Monitor & Nutritional status, PO intake/diet tolerance, lab changes, weight changes, and

Follow- up Assessment 3/28/14 Nutritional Problems Stage 2 pressure ulcer-location: sacrum SLP saw pt on 3/24 and recommended a pureed diet with honey thick liquids. Recommended biotene due to decreased saliva. Family informed RD that patient likes chocolate Ensure shakes; however pt had not been able to drink any Ensure due to NGT being placed. SLP recommends today to initiate puree solids + honey thick liquids + Enteral feedings. Nutrient Requirements Nutrient requirements (previously estimated) based on Patients UBW: 167#76 kg. Calories: 2280 -2660 kcal/day –Based on: 30 -35 kcal/kg Protein: 91 -114 gm/day- Based on: 1. 2 -1. 5 gm/kg Fluid: 2280 -2660 ml/day- Based on: 30 -35 kcal/kg. Nutrition Diagnosis/ Intervention *No new nutritional problems identified at this time. Recommendations: Change diet to TF with tray: Jevity 1. 2 @ 40 ml/hr x 24 hrs (1152 kcal, 53 g pro) + Puree solids/honey thick liquids (1900 -2200 kcal, 83 g Pro). Continue Therapeutic MVI, Prostat 30 ml BID (202 kcal, 30 gm Pro), and Ensure plus 8 oz TID (1050 kcal, 39 g Pro) Consider 48 hr calorie count to ensure pt meeting needs PO prior to D/C TF. Goals & Plans Provide adequate nutrition via tolerated route Promote wound healing Monitor & Evaluation Nutritional status, PO intake/diet tolerance, lab changes, weight changes, and Diet progression.

Follow-Up Assessment 3/31/14 Nutritional Problems Stage 2 Pressure ulcer-location sacrum Po diet ordered recently, po intake needs further observation. Nutrient Requirements Nutrient requirements (previously estimated) based on Patients UBW: 167#76 kg. Calories: 2280 -2660 kcal/day –Based on: 30 -35 kcal/kg Protein: 91 -114 gm/day- Based on: 1. 2 -1. 5 gm/kg Fluid: 2280 -2660 ml/day- Based on: 30 -35 kcal/kg. Nutrition Diagnosis/ Intervention *No new nutritional problems identified at this time. Continue current nutrition order: Jevity 1. 2 @ 50 ml/hr x 24 hrs via NGT (1440 kcal, 67 g Pro) Continue po diet per SLP recommendation: Pureed solids + honey thick liquids (1900 -2200 kcal, 83 g Pro) Continue Ensure plus 8 oz TID (1050 kcal, 39 g Pro) >>May recommend increasing TF at follow-up if appetite is poor and PO intake is <50%. Goals & Plans Provide adequate nutrition via tolerated route Promote wound healing Monitor & Nutritional status, PO intake/diet tolerance, lab changes, weight changes
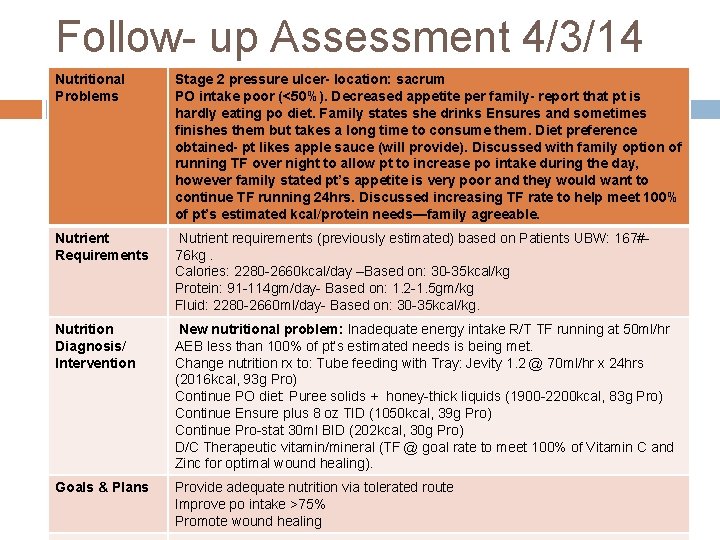
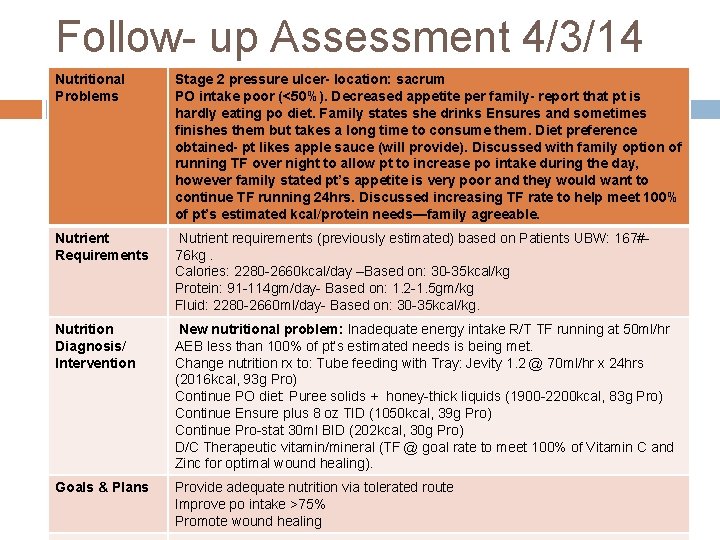
Follow- up Assessment 4/3/14 Nutritional Problems Stage 2 pressure ulcer- location: sacrum PO intake poor (<50%). Decreased appetite per family- report that pt is hardly eating po diet. Family states she drinks Ensures and sometimes finishes them but takes a long time to consume them. Diet preference obtained- pt likes apple sauce (will provide). Discussed with family option of running TF over night to allow pt to increase po intake during the day, however family stated pt’s appetite is very poor and they would want to continue TF running 24 hrs. Discussed increasing TF rate to help meet 100% of pt’s estimated kcal/protein needs—family agreeable. Nutrient Requirements Nutrient requirements (previously estimated) based on Patients UBW: 167#76 kg. Calories: 2280 -2660 kcal/day –Based on: 30 -35 kcal/kg Protein: 91 -114 gm/day- Based on: 1. 2 -1. 5 gm/kg Fluid: 2280 -2660 ml/day- Based on: 30 -35 kcal/kg. Nutrition Diagnosis/ Intervention New nutritional problem: Inadequate energy intake R/T TF running at 50 ml/hr AEB less than 100% of pt’s estimated needs is being met. Change nutrition rx to: Tube feeding with Tray: Jevity 1. 2 @ 70 ml/hr x 24 hrs (2016 kcal, 93 g Pro) Continue PO diet: Puree solids + honey-thick liquids (1900 -2200 kcal, 83 g Pro) Continue Ensure plus 8 oz TID (1050 kcal, 39 g Pro) Continue Pro-stat 30 ml BID (202 kcal, 30 g Pro) D/C Therapeutic vitamin/mineral (TF @ goal rate to meet 100% of Vitamin C and Zinc for optimal wound healing). Goals & Plans Provide adequate nutrition via tolerated route Improve po intake >75% Promote wound healing
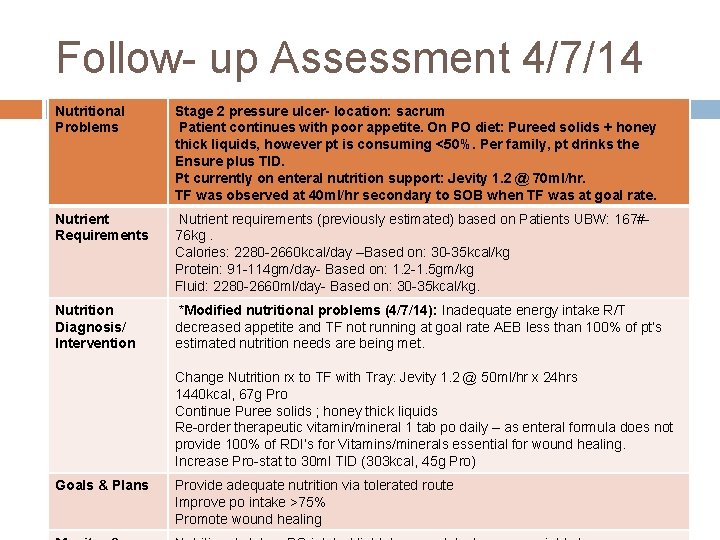
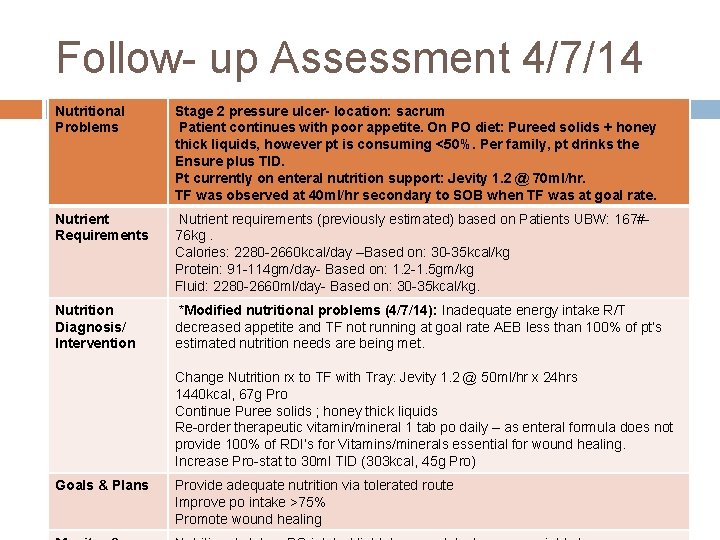
Follow- up Assessment 4/7/14 Nutritional Problems Stage 2 pressure ulcer- location: sacrum Patient continues with poor appetite. On PO diet: Pureed solids + honey thick liquids, however pt is consuming <50%. Per family, pt drinks the Ensure plus TID. Pt currently on enteral nutrition support: Jevity 1. 2 @ 70 ml/hr. TF was observed at 40 ml/hr secondary to SOB when TF was at goal rate. Nutrient Requirements Nutrient requirements (previously estimated) based on Patients UBW: 167#76 kg. Calories: 2280 -2660 kcal/day –Based on: 30 -35 kcal/kg Protein: 91 -114 gm/day- Based on: 1. 2 -1. 5 gm/kg Fluid: 2280 -2660 ml/day- Based on: 30 -35 kcal/kg. Nutrition Diagnosis/ Intervention *Modified nutritional problems (4/7/14): Inadequate energy intake R/T decreased appetite and TF not running at goal rate AEB less than 100% of pt’s estimated nutrition needs are being met. Change Nutrition rx to TF with Tray: Jevity 1. 2 @ 50 ml/hr x 24 hrs 1440 kcal, 67 g Pro Continue Puree solids ; honey thick liquids Re-order therapeutic vitamin/mineral 1 tab po daily – as enteral formula does not provide 100% of RDI’s for Vitamins/minerals essential for wound healing. Increase Pro-stat to 30 ml TID (303 kcal, 45 g Pro) Goals & Plans Provide adequate nutrition via tolerated route Improve po intake >75% Promote wound healing
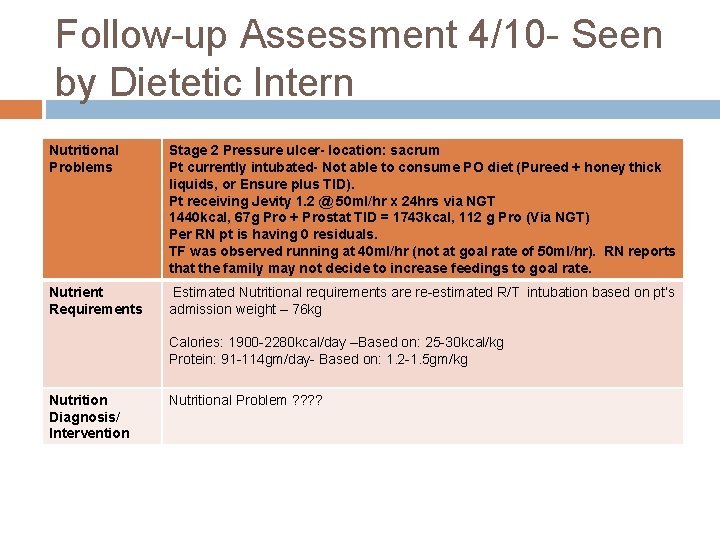
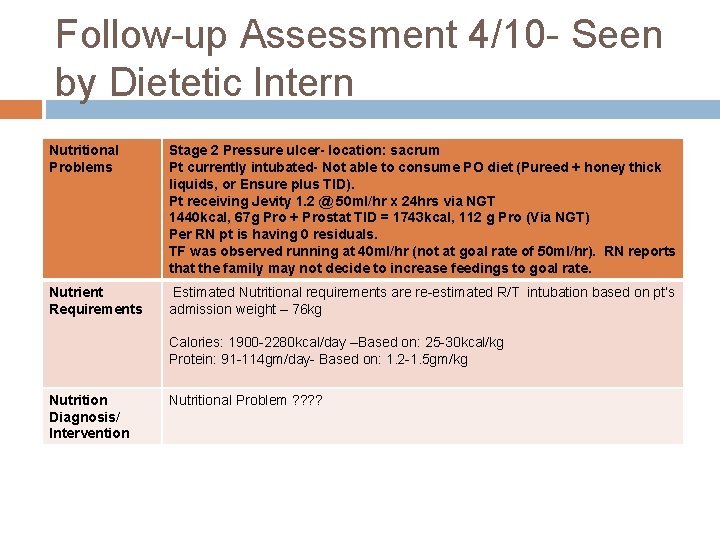
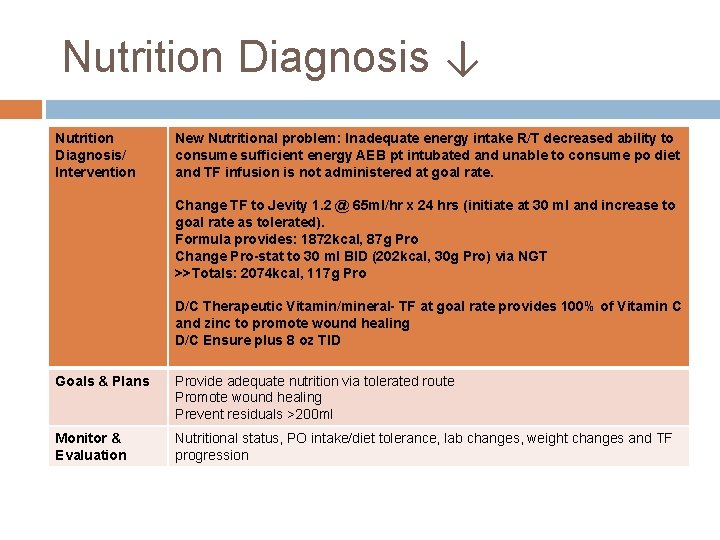
Follow-up Assessment 4/10 - Seen by Dietetic Intern Nutritional Problems Stage 2 Pressure ulcer- location: sacrum Pt currently intubated- Not able to consume PO diet (Pureed + honey thick liquids, or Ensure plus TID). Pt receiving Jevity 1. 2 @ 50 ml/hr x 24 hrs via NGT 1440 kcal, 67 g Pro + Prostat TID = 1743 kcal, 112 g Pro (Via NGT) Per RN pt is having 0 residuals. TF was observed running at 40 ml/hr (not at goal rate of 50 ml/hr). RN reports that the family may not decide to increase feedings to goal rate. Nutrient Requirements Estimated Nutritional requirements are re-estimated R/T intubation based on pt’s admission weight – 76 kg Calories: 1900 -2280 kcal/day –Based on: 25 -30 kcal/kg Protein: 91 -114 gm/day- Based on: 1. 2 -1. 5 gm/kg Nutrition Diagnosis/ Intervention Nutritional Problem ? ?
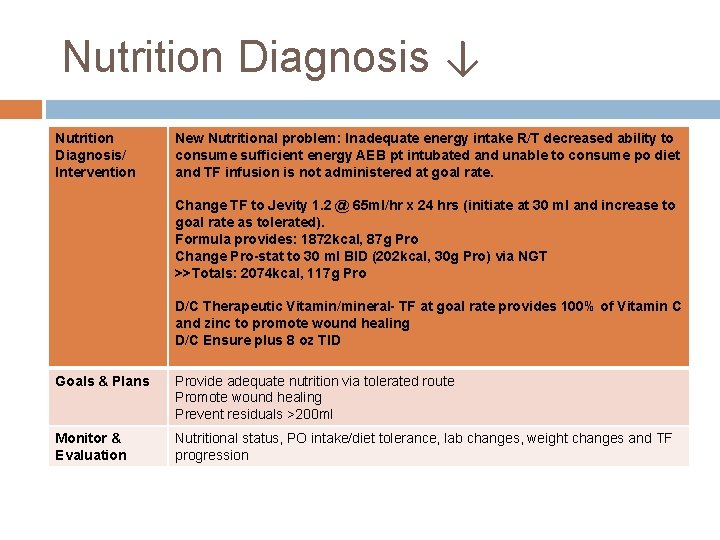
Nutrition Diagnosis ↓ Nutrition Diagnosis/ Intervention New Nutritional problem: Inadequate energy intake R/T decreased ability to consume sufficient energy AEB pt intubated and unable to consume po diet and TF infusion is not administered at goal rate. Change TF to Jevity 1. 2 @ 65 ml/hr x 24 hrs (initiate at 30 ml and increase to goal rate as tolerated). Formula provides: 1872 kcal, 87 g Pro Change Pro-stat to 30 ml BID (202 kcal, 30 g Pro) via NGT >>Totals: 2074 kcal, 117 g Pro D/C Therapeutic Vitamin/mineral- TF at goal rate provides 100% of Vitamin C and zinc to promote wound healing D/C Ensure plus 8 oz TID Goals & Plans Provide adequate nutrition via tolerated route Promote wound healing Prevent residuals >200 ml Monitor & Evaluation Nutritional status, PO intake/diet tolerance, lab changes, weight changes and TF progression
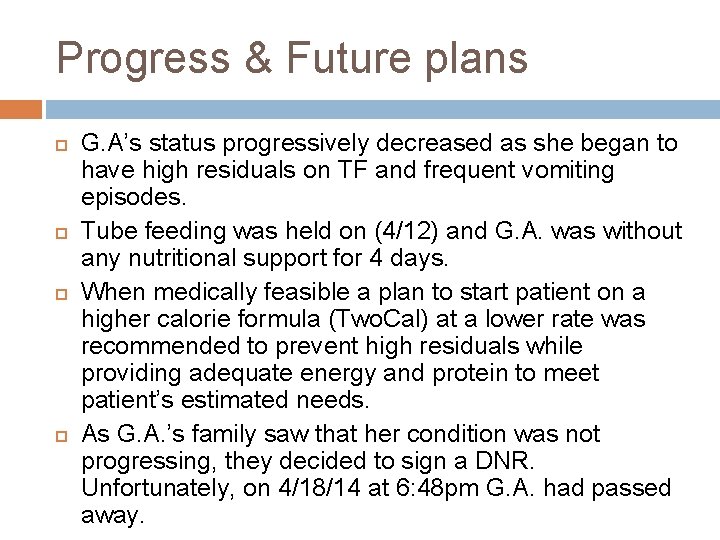
Progress & Future plans G. A’s status progressively decreased as she began to have high residuals on TF and frequent vomiting episodes. Tube feeding was held on (4/12) and G. A. was without any nutritional support for 4 days. When medically feasible a plan to start patient on a higher calorie formula (Two. Cal) at a lower rate was recommended to prevent high residuals while providing adequate energy and protein to meet patient’s estimated needs. As G. A. ’s family saw that her condition was not progressing, they decided to sign a DNR. Unfortunately, on 4/18/14 at 6: 48 pm G. A. had passed away.
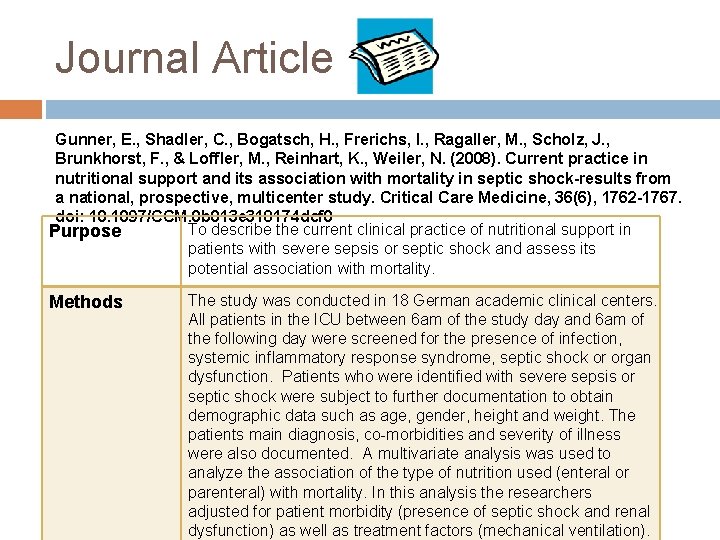
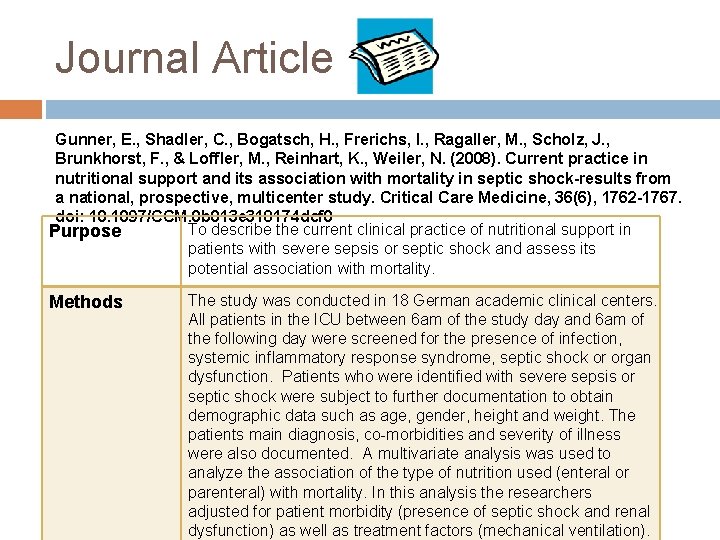
Journal Article Gunner, E. , Shadler, C. , Bogatsch, H. , Frerichs, I. , Ragaller, M. , Scholz, J. , Brunkhorst, F. , & Loffler, M. , Reinhart, K. , Weiler, N. (2008). Current practice in nutritional support and its association with mortality in septic shock-results from a national, prospective, multicenter study. Critical Care Medicine, 36(6), 1762 -1767. doi: 10. 1097/CCM. 0 b 013 e 318174 dcf 0 To describe the current clinical practice of nutritional support in Purpose patients with severe sepsis or septic shock and assess its potential association with mortality. Methods The study was conducted in 18 German academic clinical centers. All patients in the ICU between 6 am of the study day and 6 am of the following day were screened for the presence of infection, systemic inflammatory response syndrome, septic shock or organ dysfunction. Patients who were identified with severe sepsis or septic shock were subject to further documentation to obtain demographic data such as age, gender, height and weight. The patients main diagnosis, co-morbidities and severity of illness were also documented. A multivariate analysis was used to analyze the association of the type of nutrition used (enteral or parenteral) with mortality. In this analysis the researchers adjusted for patient morbidity (presence of septic shock and renal dysfunction) as well as treatment factors (mechanical ventilation).
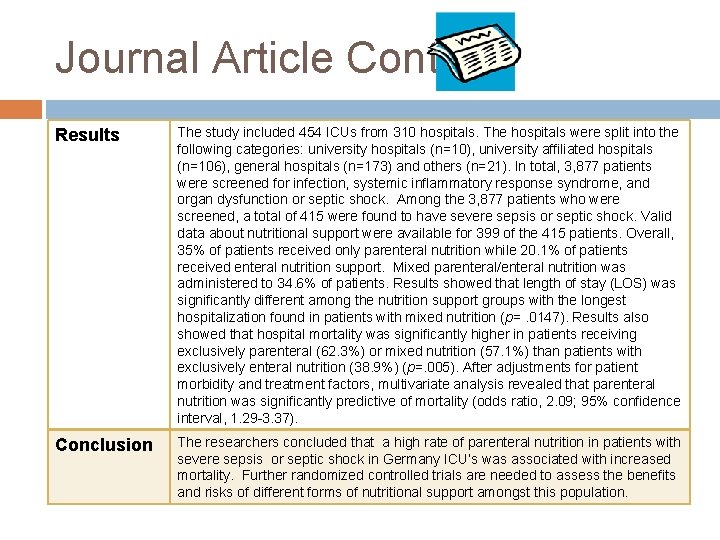
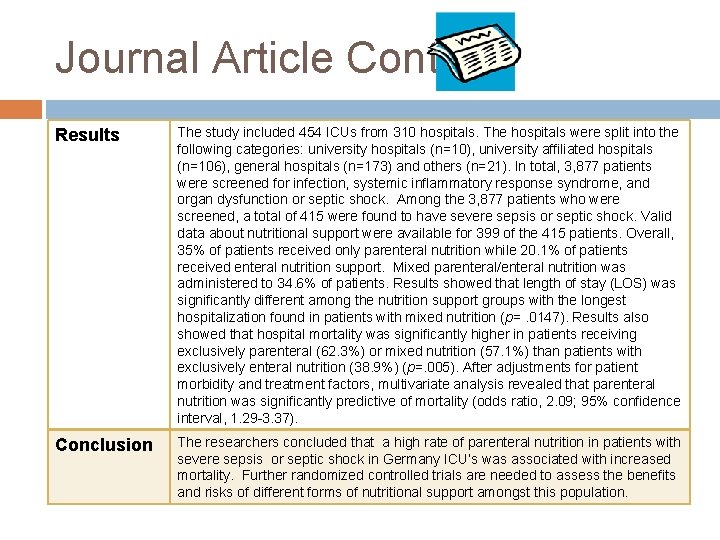
Journal Article Cont. Results The study included 454 ICUs from 310 hospitals. The hospitals were split into the following categories: university hospitals (n=10), university affiliated hospitals (n=106), general hospitals (n=173) and others (n=21). In total, 3, 877 patients were screened for infection, systemic inflammatory response syndrome, and organ dysfunction or septic shock. Among the 3, 877 patients who were screened, a total of 415 were found to have severe sepsis or septic shock. Valid data about nutritional support were available for 399 of the 415 patients. Overall, 35% of patients received only parenteral nutrition while 20. 1% of patients received enteral nutrition support. Mixed parenteral/enteral nutrition was administered to 34. 6% of patients. Results showed that length of stay (LOS) was significantly different among the nutrition support groups with the longest hospitalization found in patients with mixed nutrition (p=. 0147). Results also showed that hospital mortality was significantly higher in patients receiving exclusively parenteral (62. 3%) or mixed nutrition (57. 1%) than patients with exclusively enteral nutrition (38. 9%) (p=. 005). After adjustments for patient morbidity and treatment factors, multivariate analysis revealed that parenteral nutrition was significantly predictive of mortality (odds ratio, 2. 09; 95% confidence interval, 1. 29 -3. 37). Conclusion The researchers concluded that a high rate of parenteral nutrition in patients with severe sepsis or septic shock in Germany ICU’s was associated with increased mortality. Further randomized controlled trials are needed to assess the benefits and risks of different forms of nutritional support amongst this population.