Setting Expectations on Professionalism in Residency Orientation Workshop


- Slides: 12
Setting Expectations on Professionalism in Residency: Orientation Workshop on Common Professionalism Issues Jayne M. Peterson, MD Banner Good Samaritan Medical Center
Professionalism in Residency l l l One of 6 Core Competencies required for board certification by the ABIM Traditionally difficult to define, to “measure” and to teach “Unwritten rules” only “discovered when you make a mistake” References Medical Professionalism. Chicago: ACGME, 2006 (Accessed Jan. 8, 2007 at http: //www. acgme. org/outcome/implement/Profm_resource. pdf) Stern, D, Papadakis, M. The Developing Physician – Becoming a Professional. NEJM 2006; 355: 1794 -9.
Setting Expectations in Our Residency l l l Resident Manual Orientation for PGY 1 prior to starting residency Workshop for PGY 2’s prior to moving to supervisory role with follow up workshop in early PGY 3 year Monthly orientation to each new rotation Advisor Meetings twice per year
Definitions of Professionalism l l l Prokos = Trust Respect - for patients & families, peers, other healthcare team members Appropriate behavior – polite, dedicated, compassionate, hardworking, timely, well groomed, honest, maintain confidentiality
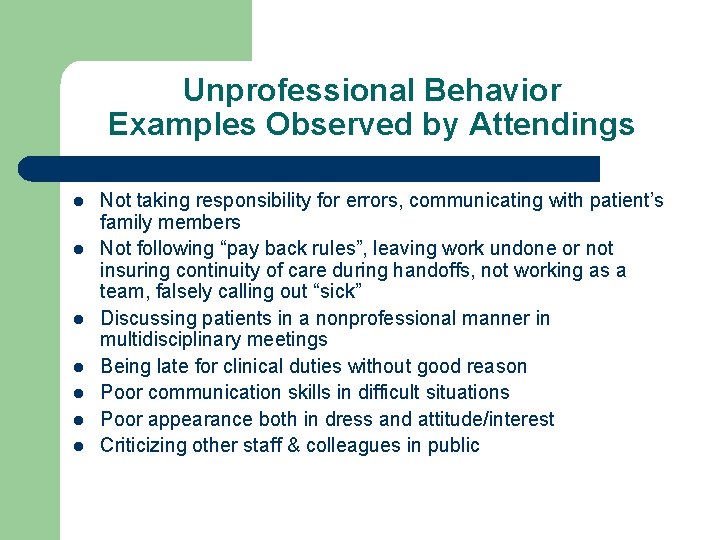
Unprofessional Behavior Examples Observed by Attendings l l l l Not taking responsibility for errors, communicating with patient’s family members Not following “pay back rules”, leaving work undone or not insuring continuity of care during handoffs, not working as a team, falsely calling out “sick” Discussing patients in a nonprofessional manner in multidisciplinary meetings Being late for clinical duties without good reason Poor communication skills in difficult situations Poor appearance both in dress and attitude/interest Criticizing other staff & colleagues in public
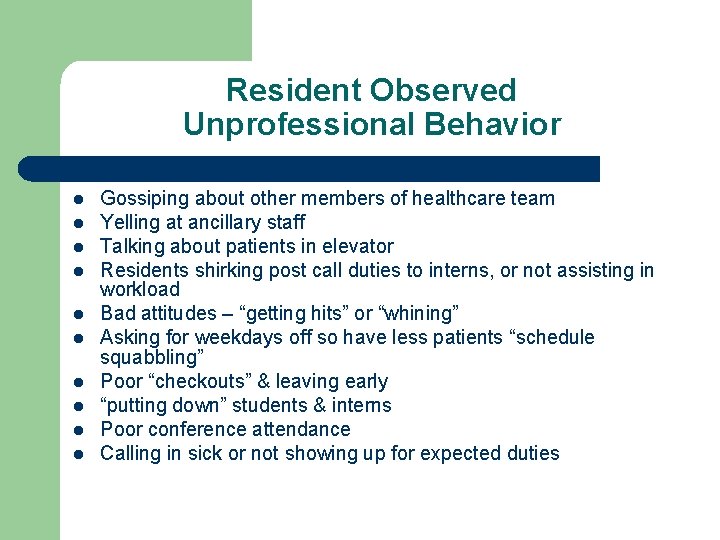
Resident Observed Unprofessional Behavior l l l l l Gossiping about other members of healthcare team Yelling at ancillary staff Talking about patients in elevator Residents shirking post call duties to interns, or not assisting in workload Bad attitudes – “getting hits” or “whining” Asking for weekdays off so have less patients “schedule squabbling” Poor “checkouts” & leaving early “putting down” students & interns Poor conference attendance Calling in sick or not showing up for expected duties
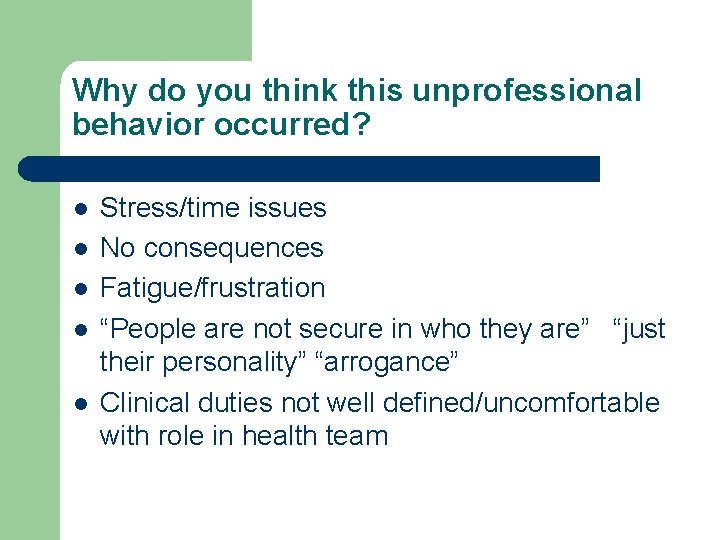
Why do you think this unprofessional behavior occurred? l l l Stress/time issues No consequences Fatigue/frustration “People are not secure in who they are” “just their personality” “arrogance” Clinical duties not well defined/uncomfortable with role in health team
Personal Professionalism Plans l l l Open your envelope from 2007 Did you do what you said you would do? Do you have a way to measure your change?
Professionalism Quality Improvement Identify Something you want to change: l Plan – What are your opportunities & barriers to change? How will I know that the change was effective? l Do – Try it l Study – Measure the change l Act – See if you can incorporate the change in your life. Start the cycle over again.

Summary of PDSA Cycle Act Plan Study Do
Example – Jayne Peterson Opportunity: Time Management – I waste too much time looking for things on my desk Plan – Organize my desk & then deal with each item only once – toss it, file it, or complete it. Do – schedule clean up date, get a new on-desk file system Study – In one month – is my desk still clean and can I find what I need? Act – If in one month it is working – I will keep this system and move on to my book shelf.

Resident Small Group Discussion l l How can we improve professionalism in our residency program? What do you think should be the consequence of unprofessional behavior? Does it matter what the behavior is? Share a personal professional plan for 20082009 with your group and how you plan to measure it.