Session 4 Standard and Transmission Based Precautions and
Session 4: Standard and Transmission Based Precautions and Novel Approaches to Controlling the Spread of MDROs Session 4
Approaches to Controlling the Spread of MDROs Our primary objectives in this session are as follows 1. Describe HICPAC/CDC precautions for preventing transmission 2. Understand literature on adherence to precaution measures We would like to hear from you about your facility’s efforts to monitor and evaluate precaution measures and spread of infection Session 4 2
Approaches to Controlling the Spread of MDROs In this session, we are going to discuss • Standard and Transmission (including Contact) precaution guidelines • Literature on effectiveness of contact precautions, including Universal Glove and Gown • Other techniques such as Red Box Entry • Local efforts to control C. difficile or other MDROs Session 4 3
Precautions to Prevent Transmission of Infectious Agents • HICPAC/CDC has two tiers of precautions for preventing transmission – Standard Precautions • Intended for all patients in all healthcare settings, regardless of suspected infection – Transmission-based Precautions • Intended for patients who are known or suspected to be infected or colonized with infectious agents Session 4 4
Precautions to Prevent Transmission of Infectious Agents • Standard Precautions – Assume that every person is potentially infected or colonized Hand Hygiene – Avoid unnecessary touching of surfaces in close proximity to patient – When hands are visibly dirty, contaminated with proteinaceous material, or visibly soiled with blood or body fluids, wash hands with either a nonantimicrobial soap and water or an antimicrobial soap and water Session 4 5
Precautions to Prevent Transmission of Infectious Agents • Standard Precautions Hand Hygiene – If hands are not visibly soiled, or after removing visible material with non-antimicrobial soap and water, decontaminate hands • The preferred method of hand decontamination is with an alcohol - based hand rub • Alternatively, hands may be washed with an antimicrobial soap and water. • Frequent use of alcohol - based hand rub immediately following hand-washing with nonantimicrobial soap may increase the frequency of dermatitis Session 4 6
Precautions to Prevent Transmission of Infectious Agents • Standard Precautions – Perform hand hygiene: • Before having direct contact with patients • After contact with blood, body fluids or excretions, mucous membranes, non-intact skin, or wound dressings • After contact with a patient’s intact skin (e. g. , when taking a pulse or blood pressure or lifting a patient) • If hands will be moving from a contaminated - body site to a clean – body site during patient care. • After contact with inanimate objects (including medical equipment) in the immediate vicinity of the patient • After removing gloves Session 4 7
Precautions to Prevent Transmission of Infectious Agents • Standard Precautions – Wash hands with non-antimicrobial soap and water or with antimicrobial soap and water if contact with spores (e. g. , C. difficile or Bacillus anthracis) is likely to have occurred • The physical action of washing and rinsing hands under such circumstances is recommended because alcohols, chlorhexidine, iodophors, and other antiseptic agents have poor activity against spores Session 4 8
Precautions to Prevent Transmission of Infectious Agents • Standard Precautions – Do not wear artificial fingernails or extenders if duties include direct contact with patients at high risk for infection and associated adverse outcomes (e. g. , those in ICUs or operating rooms) • Develop an organizational policy on the wearing of non – natural nails by healthcare personnel who have direct contact with certain patients Summer décor? Session 4 9
Precautions to Prevent Transmission of Infectious Agents Personal Protection Equipment • When close to, or are handling, blood, body fluid, body tissues, mucous membranes, or areas of open skin, HCWs must use personal protective equipment, depending on the anticipated exposure, such as: – Gloves – Mask and goggles – Apron, gown, and shoe covers Session 4 10
Precautions to Prevent Transmission of Infectious Agents • Transmission-based Precautions – Three categories • Contact Precautions • Airborne Precautions • Droplet Precautions Session 4 11
Precautions to Prevent Transmission of Infectious Agents Transmission-based Precautions • Should be initiated when illness is first suspected, and discontinued only when the illness has been treated or ruled-out and the room has been cleaned – Contact precautions may be needed • Wear a gown and gloves • CRE, MDR-Ab, C. difficile and norovirus, and respiratory syncytial virus (RSV) Session 4 12
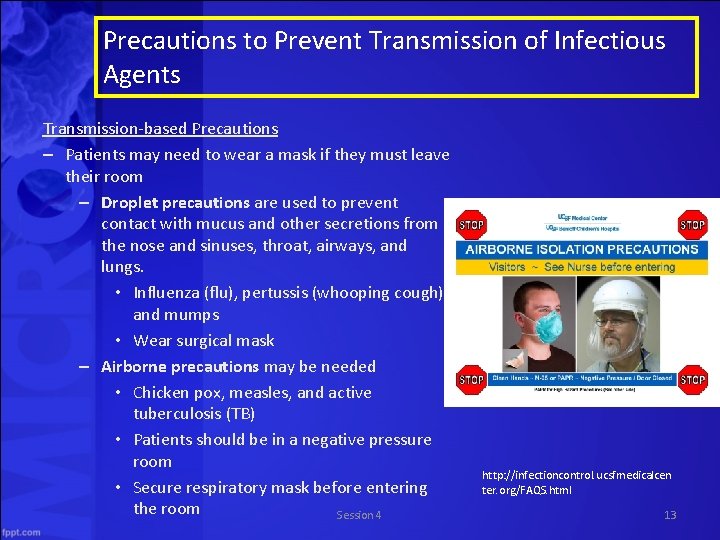
Precautions to Prevent Transmission of Infectious Agents Transmission-based Precautions – Patients may need to wear a mask if they must leave their room – Droplet precautions are used to prevent contact with mucus and other secretions from the nose and sinuses, throat, airways, and lungs. • Influenza (flu), pertussis (whooping cough), and mumps • Wear surgical mask – Airborne precautions may be needed • Chicken pox, measles, and active tuberculosis (TB) • Patients should be in a negative pressure room • Secure respiratory mask before entering the room Session 4 http: //infectioncontrol. ucsfmedicalcen ter. org/FAQS. html 13
Discontinuation of Contact Precautions Per HICPAC 2006 guidelines: Unresolved “In general, it seems reasonable to discontinue Contact Precautions when three or more surveillance cultures for the target MDRO are repeatedly negative over the course of a week or two in a patient who has not received antimicrobial therapy for several weeks, especially in the absence of a draining wound, profuse respiratory secretions, or evidence implicating the specific patient in ongoing transmission of the MDRO within the facility. ” Session 4 14
Time for a movie quiz!
How well do we adhere to contact precautions? Session 4 16
Contact Precautions for Multidrug Resistant Organisms (MDROs): Current Recommendations and Actual Practice This study by Clock et al. was conducted in a network of three hospitals in New York City and sought to assess availability of contact precautions equipment and adherence to protocol by staff and visitors Clock SA et al. Am J Infect Control 2010; 38(2): 105 -111 Session 4 17
Contact Precautions for Multidrug Resistant Organisms (MDROs) Results • January – June 2008, 424 patients observed – 67% positive MDRO cultures for one organism – 33% positive for 2 to 6 organisms – Most common VRE and MRSA • Provision of supplies – 85. 4% of room observations in the 60 day study period indicated contact precautions with a sign display – Approximately 95% of rooms with sign display had isolation carts Clock SA et al. Am J Infect Control 2010; 38(2): 105 -111 Session 4 18
Contact Precautions for Multidrug Resistant Organisms (MDROs) Patient Care Staff had higher adherence rates for all contact precautions behavior, compared with other staff (52 to 70%) Visitors wore a gown 43 to 64% of the time Clock SA et al. Am J Infect Control 2010; 38(2): 105 -111 Session 4 19
Contact Precautions for Multidrug Resistant Organisms (MDROs) Overall adherence rates on room entry and exit, respectively, were • 19. 4% (entry) and 48. 4% (exit) for hand hygiene • 67. 5% and 63. 5% for gloves • 67. 9% and 77. 1% for gowns Conclusions: Findings support the recommendation that methods to monitor contact precautions and identify and correct non-adherent practices should be a standard component of infection prevention and control programs Clock SA et al. Am J Infect Control 2010; 38(2): 105 -111 Session 4 20
Contact Isolation Precautions: More is not Necessarily Better • Kaye et al found a negative relationship between contact isolation precautions and compliance • Conclusions: Compliance with CIP was low across multiple hospitals. Increased indications for CIP and burden of MDROs were associated with decreased HCW compliance. Hospitals should weigh the . implications of decreased HCW compliance when implementing widespread CIP, and consider targeting CIP practices towards MDROs that pose particular threats to their patient populations. Kaye, et. al. , Oral abstract presentation Decennial Saturday, March 20, 2010 Session 4
Why might HCWs not be adherent to precautions? Session 4
Adverse outcomes associated with contact precautions: A review of the literature • • Four main adverse outcomes related to Contact Precautions Less patient-health care worker contact Delays and more noninfectious adverse events Increased symptoms of depression and anxiety Decreased patient satisfaction with care Morgan, et al. American Journal of Infection Control - March 2009 (Vol. 37, Issue 2, Pages 85 -93) Session 4
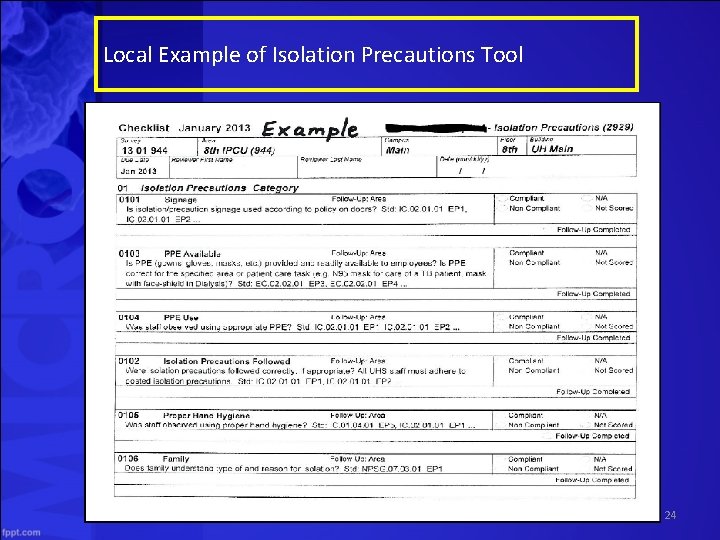
Local Example of Isolation Precautions Tool Session 4 24
Novel Approaches to Transmission Prevention Session 4
Taking Off the Gloves: Toward a Less Dogmatic Approach to the Use of Contact Isolation Conclusion: …. . Most importantly, there is good evidence that a less restrictive alternative exists that has the advantage of being universally applicable and acting at multiple sites in the chain of events leading to HAI For this reason, efforts to improve hand hygiene should be prioritized by all hospitals. If those efforts are successful, the role for contact isolation will be limited. Kirkland; Clin Infect Dis. (2009) 48 (6): 766 -771. Session 4
New Rules for Contact Precautions will be instituted for patients who have: 1. Diarrhea known or suspected to be infectious or toxin-mediated (e. g. C-diff), or diarrhea in a patient who is incontinent of stool, as detailed below: a. Known infectious cause of diarrhea, even if patient is continent of stool or stool is contained in a diaper or device. b. Patient is being tested for C. difficile or other form of infectious diarrhea c. Patient is incontinent of stool regardless of cause unless the stool is effectively contained in an incontinence brief or fecal collection device. 2. Draining wound that is not, or cannot be completely covered with a sealed dressing that contains the drainage (regardless of organism or infection) 3. Uncontrolled uncontained respiratory secretions (most commonly in trached patients, regardless of organism) 4. Selected specific infectious diseases (See “Isolation Guidelines 2007 for Specific Diseases” on the Infection Prevention Intranet Site) 5. Emerging MDROs that are defined by IP and ID Session 4
Contact Precautions require all of the elements of Standard Precautions, and in addition require the following: Patient must be in a private room (door may be left open) Gloves must be worn by staff whenever they enter the room. Gowns must be worn by staff when they enter the room unless there will be NO contact with the patient or the patient’s environment. Dedicated patient care equipment must be used when available. If dedicated equipment is not available, equipment must be disinfected between patients. Limit transport and movement of patients outside of the room to medically necessary purposes. ***Contact Precautions may be discontinued when signs and symptoms have resolved for at least 24 hours or according to disease-specific recommendations, whichever is later. Note: According to Standard Precautions gloves and gown are required for any contact with stool or items contaminated with stool. Session 4
New Rules for Contact Precautions • No increase in MDR HAIs • 3623 Nursing hours saved in one year • $291, 316 saved (if compliance was perfect before) Session 4 29
Red Box Entry A hospital in Illinois created a 3 foot square area, marked by red duct tape at the entrance to patient rooms placed on contact precaution due to risk of infection spread. Referred to as ‘safe zone’ where healthcare workers can interact with patients without donning personal protective equipment • Saves time donning clothing • Improved patient satisfaction • Increased staff productivity • No negative impact on HAI rate Source: www. innovations. ahrq. gov. Accessed June 30, 2014 Webinar available at : http: //webinars. apic. org/session. php? id=7272 Session 4 30
Universal Glove and Gown Use and Acquisition of Antibiotic Resistant Bacteria in the ICU: A randomized trial This study by Harris et al. sought to determine whether wearing gloves and gowns for all patient contact in the ICU decreased MRSA or VRE compared to usual care • 20 medical and surgical ICUs in 20 hospitals were randomized – In the intervention group, all healthcare workers were required to glove and gown for all patient contact and when entering any patient room – Primary Outcome: • Acquisition of MRSA or VRE based on surveillance cultures collected on admission and discharge from ICU Harris AD et al. JAMA 2013; 310(15): 1571 -1580 Session 4 31
Universal Glove and Gown Use and Acquisition of Antibiotic Resistant Bacteria in the ICU: A randomized trial Results • No differences in MRSA/VRE acquisition rates were seen between universal glove and gown and ‘usual care’ – There were fewer MRSA acquisitions: 40. 2% relative reduction in intervention vs. 15% reduction in control • Universal glove and gown – Decreased HCW room entry – Increased room-exit hand hygiene compliance – Had no effect on rates of adverse events • Adverse events were randomly sampled using the IHI Global trigger tool Harris AD et al. JAMA 2013; 310(15): 1571 -1580 Griffin F, Ressar R. IHI global trigger tool for measuring adverse events. 2009 IHI Innovation Series White Session 4 Paper (second ed) 32
Session 4 33
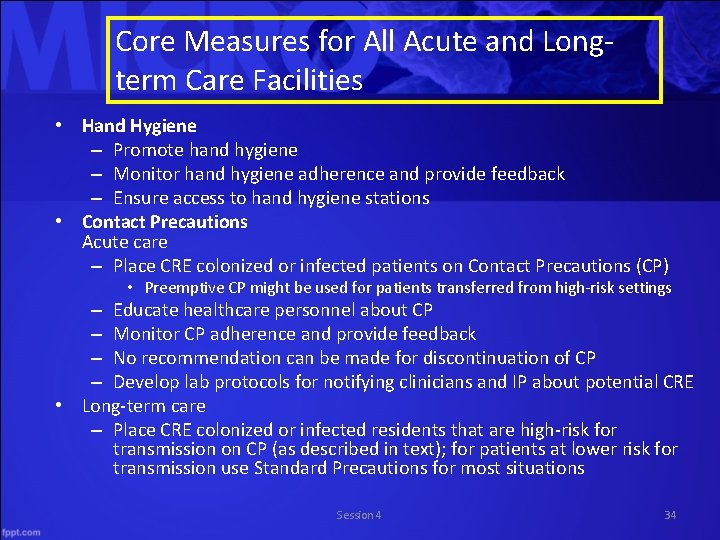
Core Measures for All Acute and Longterm Care Facilities • Hand Hygiene – Promote hand hygiene – Monitor hand hygiene adherence and provide feedback – Ensure access to hand hygiene stations • Contact Precautions Acute care – Place CRE colonized or infected patients on Contact Precautions (CP) • Preemptive CP might be used for patients transferred from high-risk settings – Educate healthcare personnel about CP – Monitor CP adherence and provide feedback – No recommendation can be made for discontinuation of CP – Develop lab protocols for notifying clinicians and IP about potential CRE • Long-term care – Place CRE colonized or infected residents that are high-risk for transmission on CP (as described in text); for patients at lower risk for transmission use Standard Precautions for most situations Session 4 34
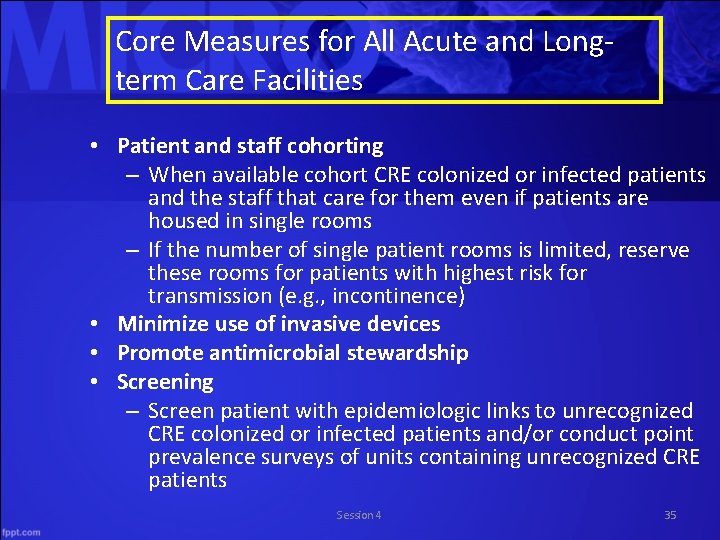
Core Measures for All Acute and Longterm Care Facilities • Patient and staff cohorting – When available cohort CRE colonized or infected patients and the staff that care for them even if patients are housed in single rooms – If the number of single patient rooms is limited, reserve these rooms for patients with highest risk for transmission (e. g. , incontinence) • Minimize use of invasive devices • Promote antimicrobial stewardship • Screening – Screen patient with epidemiologic links to unrecognized CRE colonized or infected patients and/or conduct point prevalence surveys of units containing unrecognized CRE patients Session 4 35
Supplemental Measures for Healthcare Facilities with CRE Transmission • Conduct active surveillance testing – Screen high-risk patients at admission or at admission and periodically during their facility stay for CRE. Preemptive CP can be used while results of admission surveillance testing are pending – Consider screening patients transferred from facilities known to have CRE at admission • Chlorhexidine bathing – Bathe patients with 2% chlorhexidine Session 4 36
Dealing with an Outbreak of C. difficile in a Children’s Hospital • Increase noted in high-risk frequent visit population • Cases mapped throughout affected patients' stays and clinic visits • Some common locations noted • Remedial education for care-givers and staff regarding proper hand hygiene, isolation, cleaning, etc. • One physician reported not knowing he was supposed to use soap and water for hand-hygiene • EVS reminded to use bleach for cleaning of isolation rooms • Took an estimated 2 months to see significant drop, but levels returned to baseline and remain Session 4 37
Questions and Discussion Session 4
What novel approaches to prevention have you implemented in your facility? Session 4 39
- Slides: 39