Session 1 Definition and Diagnosis of Asthma Quality
- Slides: 27
Session 1 Definition and Diagnosis of Asthma Quality Education for a Healthier Scotland
Learning Outcomes 1: Theoretical demonstration at Scottish Credit Qualifications Framework (2017) Level 9/10 • Describe asthma including diagnostic criteria • Perform clinical assessment including pharmacological, nonpharmacological treatments and trigger avoidance strategies • Demonstrate correct inhaler technique (Baverstock et al 2010) • Conduct asthma annual reviews (SIGN 2016; GINA 2017; NICE 2017) • Recognise sub-optimal asthma control and appropriate referral Quality Education for a Healthier Scotland
Learning Outcomes 2: • Identify current asthma control, interpreting objective measurements e. g. peak expiratory flow rate (PEFR), Royal College of Physicians (RCP) 3 questions, asthma control test (ACT) • Adopt an inclusive team approach with appropriate referral back to the clinical lead in the surgery for asthma (NMC Code 2015) • Write a Personal Asthma Action Plan (PAAP) for selfmanagement in collaboration with the patient to improve asthma care (NRAD 2014; SIGN 2016) • Practice person centred care: respect, holism, choice, empathy, autonomy and compassion (RCN 2015). Quality Education for a Healthier Scotland
Definition of Asthma • Inflammatory condition of airways, resulting in smooth muscle contraction, oedema of airway wall and increase in production and secretion of mucus • A response of smooth muscle in respiratory tree to external allergens and irritants resulting in muscle contraction and obstruction to normal breathing • SIGN (2016) description of asthma includes hyperresponsiveness and inflammation as elements of disease Quality Education for a Healthier Scotland
Diagnosis of Asthma • Combination of clinical signs and symptoms are more helpful and increase probability: Ø Wheeze Ø Breathlessness Ø Chest tightness Ø Cough • Confirmation hinges on demonstrating airway variability Quality Education for a Healthier Scotland
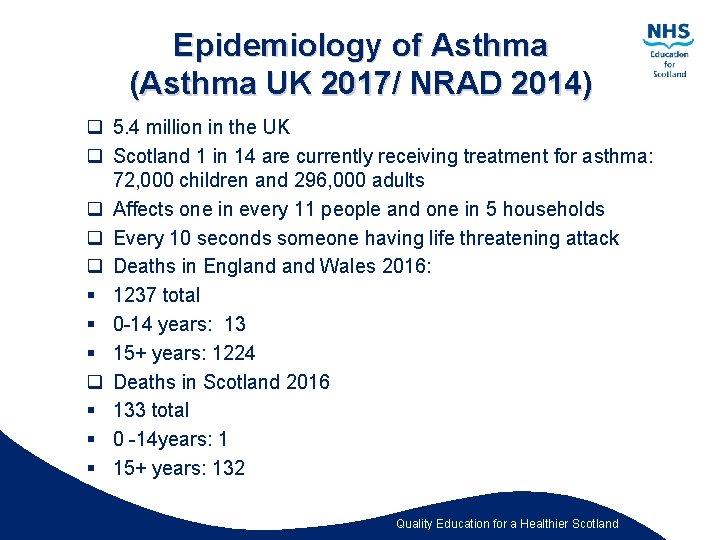
Epidemiology of Asthma (Asthma UK 2017/ NRAD 2014) q 5. 4 million in the UK q Scotland 1 in 14 are currently receiving treatment for asthma: 72, 000 children and 296, 000 adults q Affects one in every 11 people and one in 5 households q Every 10 seconds someone having life threatening attack q Deaths in England Wales 2016: § 1237 total § 0 -14 years: 13 § 15+ years: 1224 q Deaths in Scotland 2016 § 133 total § 0 -14 years: 1 § 15+ years: 132 Quality Education for a Healthier Scotland
Why Asthma Still Kills THE NATIONAL REVIEW OF ASTHMA DEATHS (NRAD) (2014) Quality Education for a Healthier Scotland
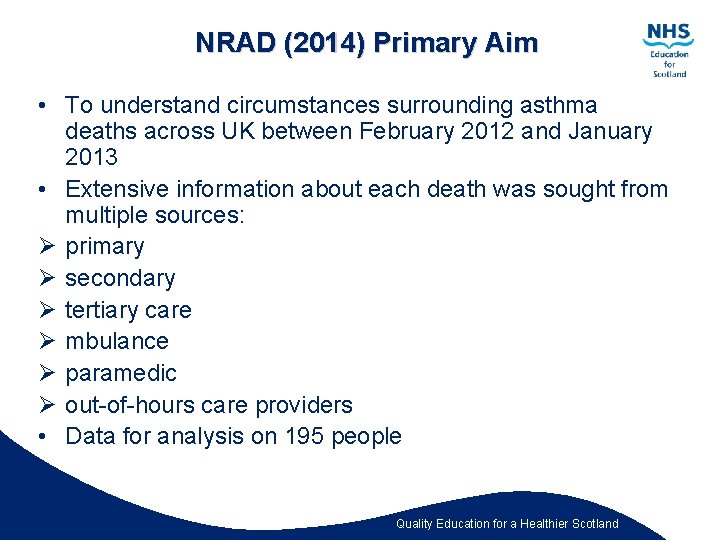
NRAD (2014) Primary Aim • To understand circumstances surrounding asthma deaths across UK between February 2012 and January 2013 • Extensive information about each death was sought from multiple sources: Ø primary Ø secondary Ø tertiary care Ø mbulance Ø paramedic Ø out-of-hours care providers • Data for analysis on 195 people Quality Education for a Healthier Scotland
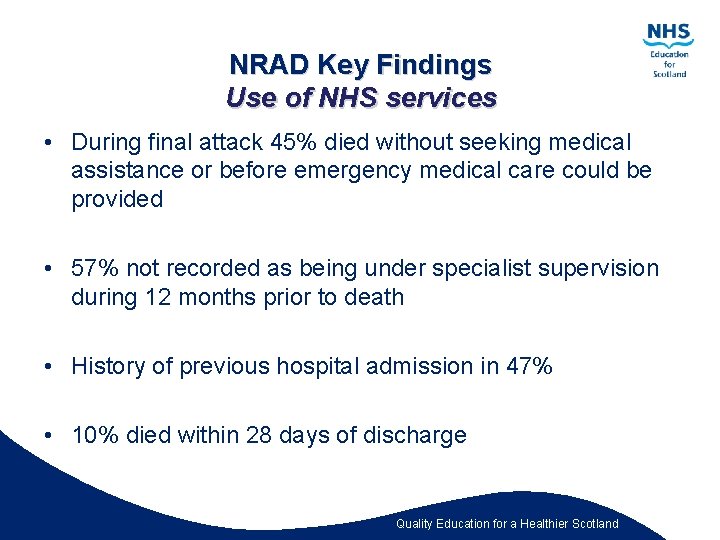
NRAD Key Findings Use of NHS services • During final attack 45% died without seeking medical assistance or before emergency medical care could be provided • 57% not recorded as being under specialist supervision during 12 months prior to death • History of previous hospital admission in 47% • 10% died within 28 days of discharge Quality Education for a Healthier Scotland
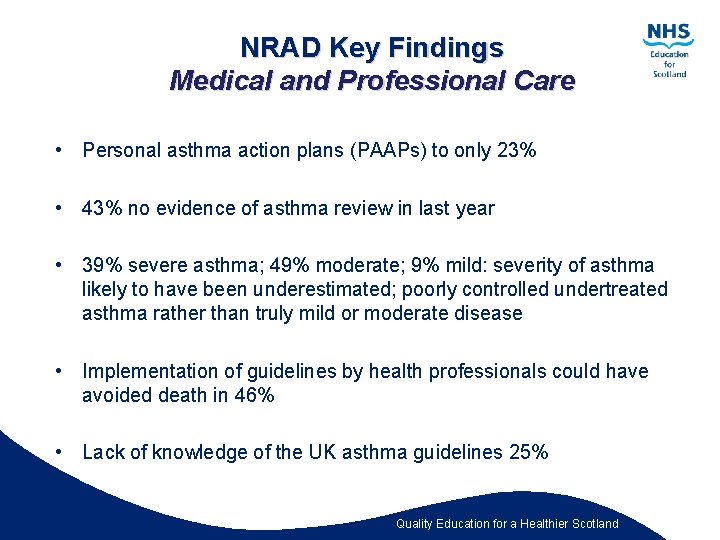
NRAD Key Findings Medical and Professional Care • Personal asthma action plans (PAAPs) to only 23% • 43% no evidence of asthma review in last year • 39% severe asthma; 49% moderate; 9% mild: severity of asthma likely to have been underestimated; poorly controlled undertreated asthma rather than truly mild or moderate disease • Implementation of guidelines by health professionals could have avoided death in 46% • Lack of knowledge of the UK asthma guidelines 25% Quality Education for a Healthier Scotland
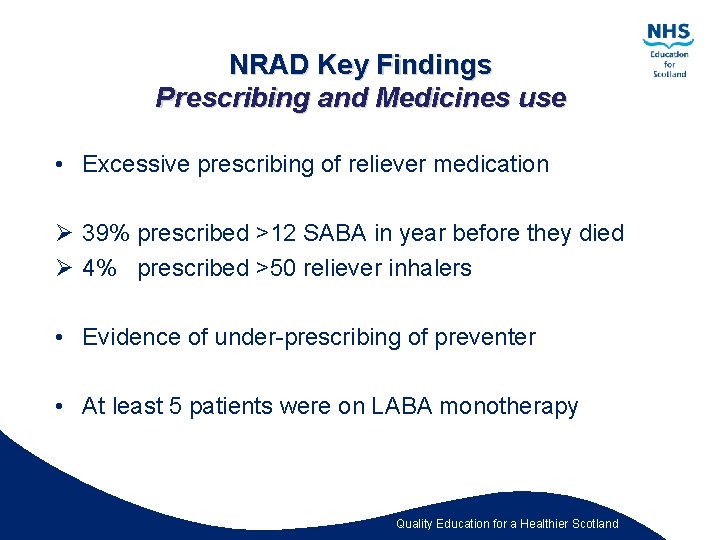
NRAD Key Findings Prescribing and Medicines use • Excessive prescribing of reliever medication Ø 39% prescribed >12 SABA in year before they died Ø 4% prescribed >50 reliever inhalers • Evidence of under-prescribing of preventer • At least 5 patients were on LABA monotherapy Quality Education for a Healthier Scotland
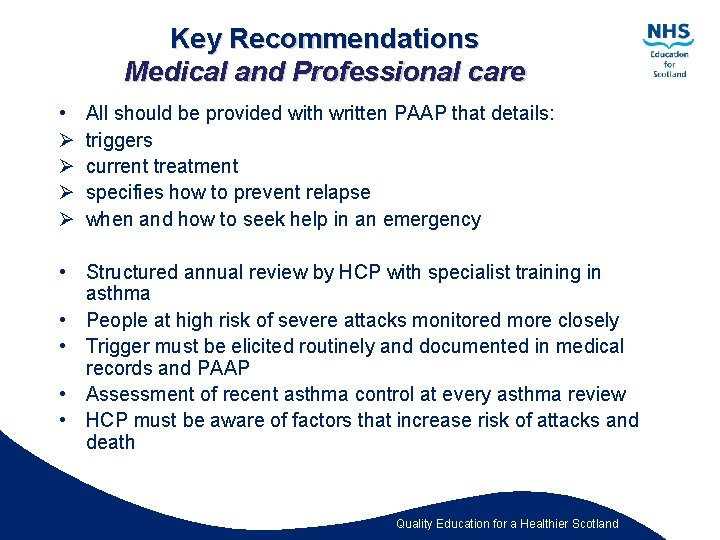
Key Recommendations Medical and Professional care • Ø Ø All should be provided with written PAAP that details: triggers current treatment specifies how to prevent relapse when and how to seek help in an emergency • Structured annual review by HCP with specialist training in asthma • People at high risk of severe attacks monitored more closely • Trigger must be elicited routinely and documented in medical records and PAAP • Assessment of recent asthma control at every asthma review • HCP must be aware of factors that increase risk of attacks and death Quality Education for a Healthier Scotland
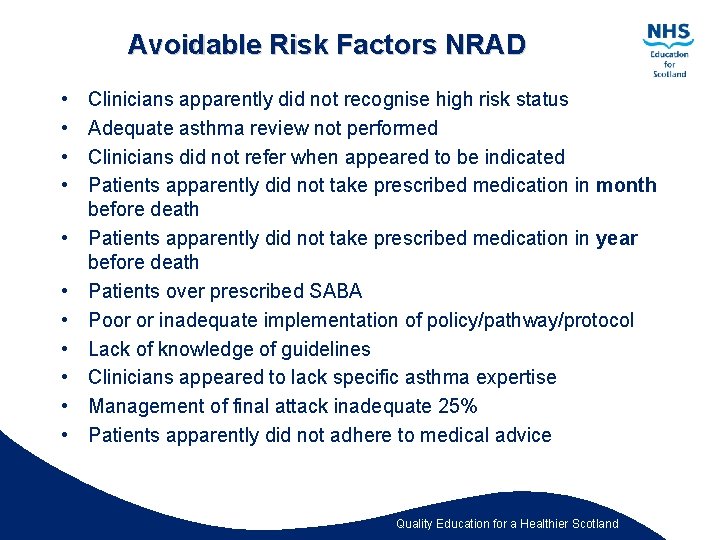
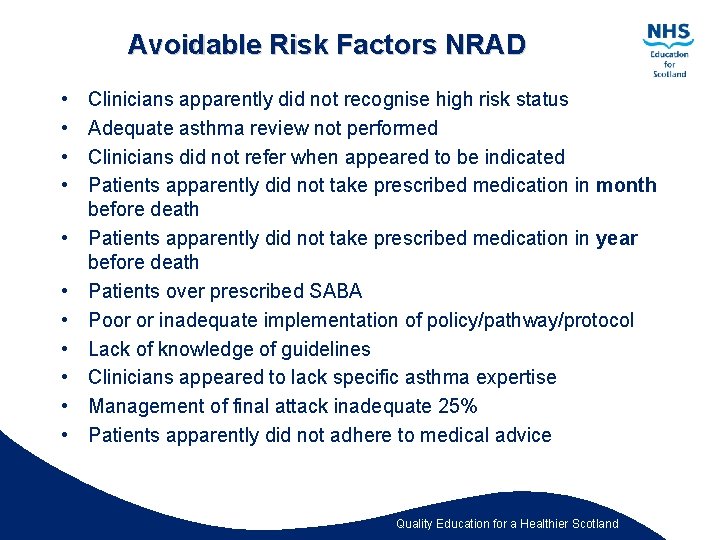
Avoidable Risk Factors NRAD • • • Clinicians apparently did not recognise high risk status Adequate asthma review not performed Clinicians did not refer when appeared to be indicated Patients apparently did not take prescribed medication in month before death Patients apparently did not take prescribed medication in year before death Patients over prescribed SABA Poor or inadequate implementation of policy/pathway/protocol Lack of knowledge of guidelines Clinicians appeared to lack specific asthma expertise Management of final attack inadequate 25% Patients apparently did not adhere to medical advice Quality Education for a Healthier Scotland
Avoidable Factors related to Patient, Family or Environment • Poor adherence to medical advice: i. e. DNA, failure to respond to symptoms • Psychosocial factors: i. e. substance abuse • Smoker or exposed to 2 nd hand smoke • Allergies: i. e. animals, food, seasonal, drug Quality Education for a Healthier Scotland
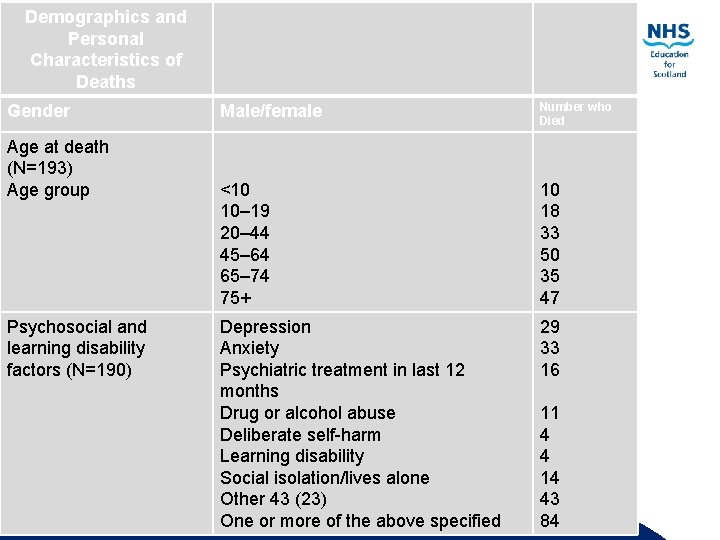
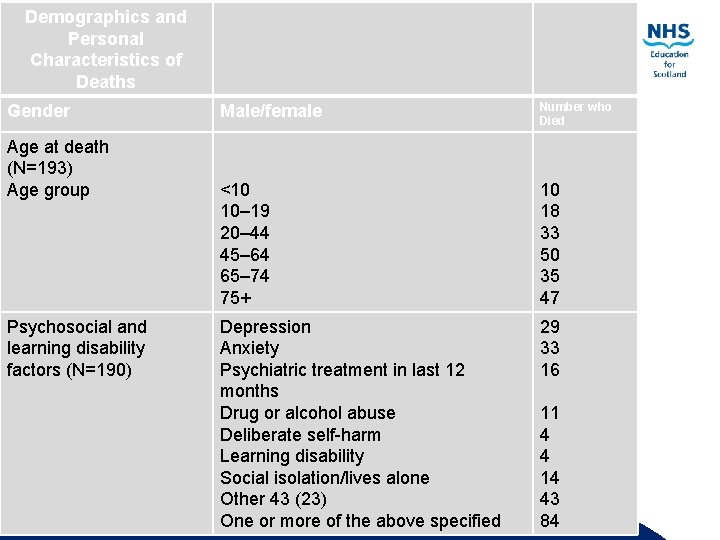
Demographics and Personal Characteristics of Deaths Gender Age at death (N=193) Age group Psychosocial and learning disability factors (N=190) Male/female Number who Died <10 10– 19 20– 44 45– 64 65– 74 75+ 10 18 33 50 35 47 Depression 29 Anxiety 33 Psychiatric treatment in last 12 16 months Drug or alcohol abuse 11 Deliberate self-harm 4 Learning disability 4 Social isolation/lives alone 14 Other 43 (23) 43 One or more of the above 84 Scotland Qualityspecified Education for a Healthier
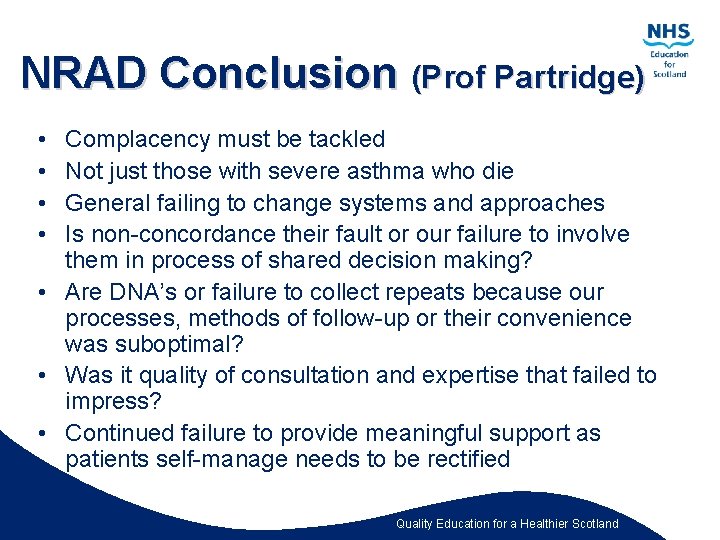
NRAD Conclusion (Prof Partridge) • • Complacency must be tackled Not just those with severe asthma who die General failing to change systems and approaches Is non-concordance their fault or our failure to involve them in process of shared decision making? • Are DNA’s or failure to collect repeats because our processes, methods of follow-up or their convenience was suboptimal? • Was it quality of consultation and expertise that failed to impress? • Continued failure to provide meaningful support as patients self-manage needs to be rectified Quality Education for a Healthier Scotland
Why Accurate Diagnosis is Important • Differentiating asthma from COPD and Asthma COPD Overlap (ACO) can be problematic, particularly in smokers and older adults • Differentiating is important because of marked differences in treatment, disease progression, and outcomes between the 3 conditions Quality Education for a Healthier Scotland
Asthma COPD Overlap (GINA 2017): 1 • Some patients may have clinical features of both asthma and COPD • Asthma-COPD overlap is useful to maintain awareness by clinicians of the needs of these patients • Asthma-COPD overlap does NOT describe a single disease; like asthma and COPD it likely includes different phenotypes caused by a range of underlying mechanisms. Quality Education for a Healthier Scotland
Asthma COPD Overlap (GINA 2017): 2 • • Stepwise approach to diagnosis Referral for confirmatory investigations encouraged Initial treatment: See GINA (2017) guidelines for management options Quality Education for a Healthier Scotland
COPD / Asthma differences • The differences in disease distribution may partly reflect distribution of main inhaled inciting agents • Asthma = allergens • COPD = tobacco smoke and environmental Quality Education for a Healthier Scotland
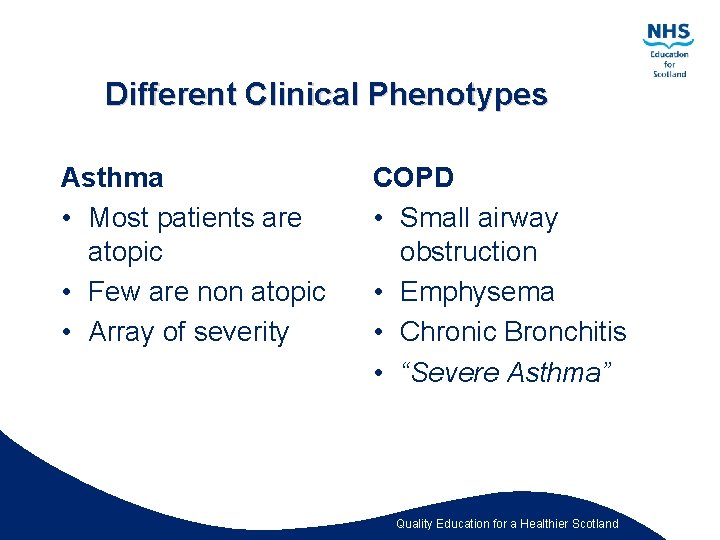
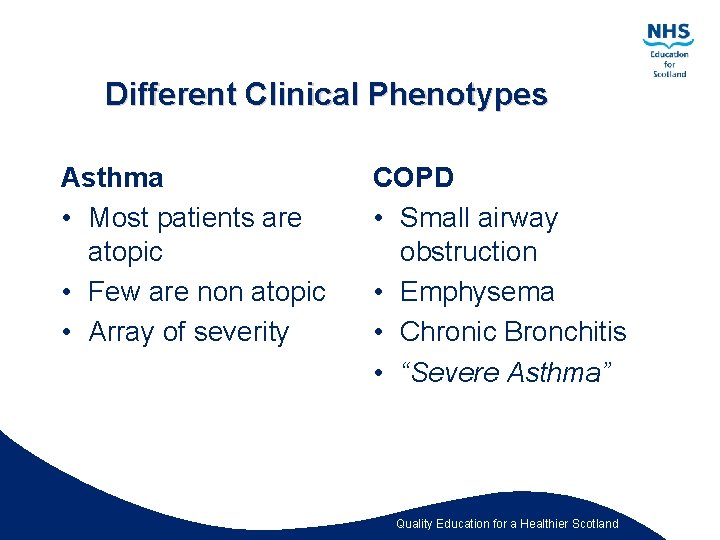
Different Clinical Phenotypes Asthma • Most patients are atopic • Few are non atopic • Array of severity COPD • Small airway obstruction • Emphysema • Chronic Bronchitis • “Severe Asthma” Quality Education for a Healthier Scotland
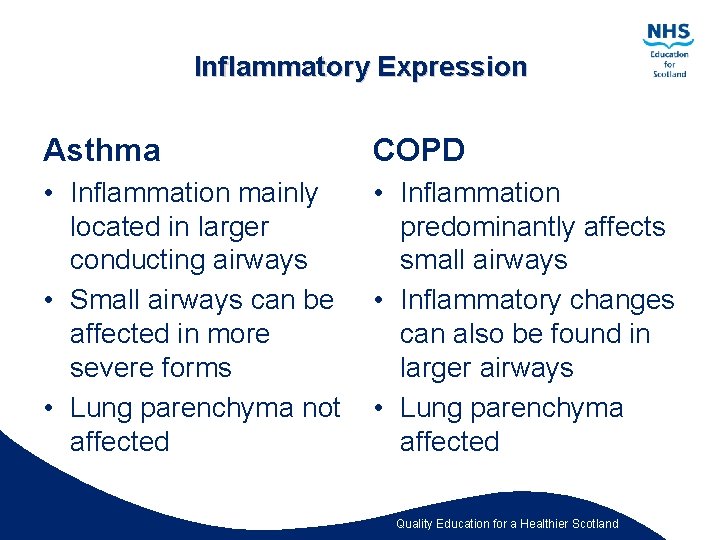
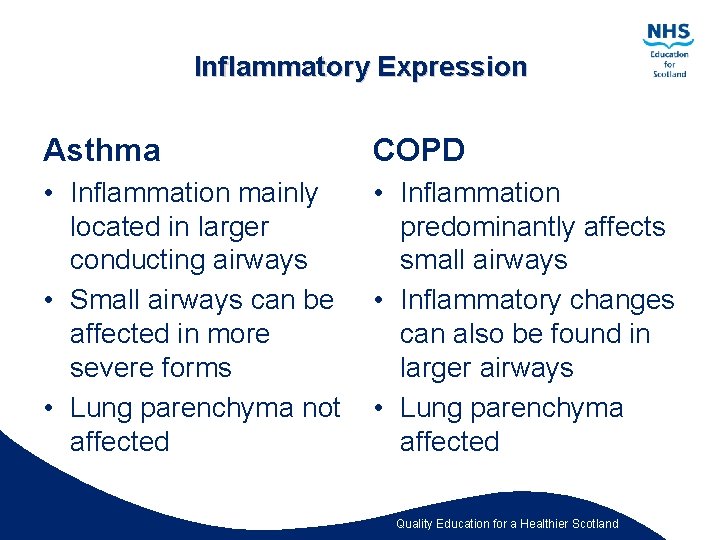
Inflammatory Expression Asthma COPD • Inflammation mainly located in larger conducting airways • Small airways can be affected in more severe forms • Lung parenchyma not affected • Inflammation predominantly affects small airways • Inflammatory changes can also be found in larger airways • Lung parenchyma affected Quality Education for a Healthier Scotland
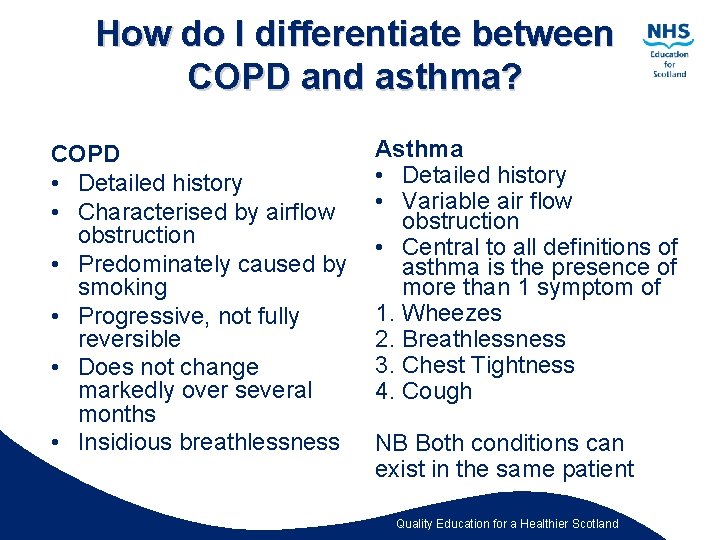
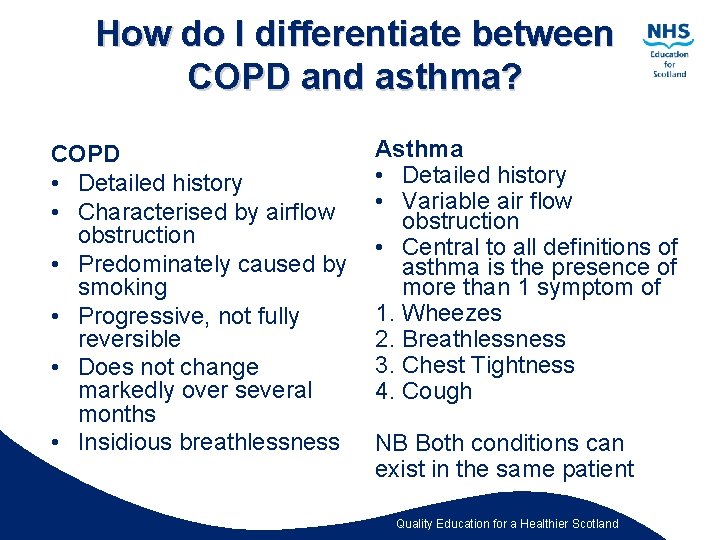
How do I differentiate between COPD and asthma? COPD • Detailed history • Characterised by airflow obstruction • Predominately caused by smoking • Progressive, not fully reversible • Does not change markedly over several months • Insidious breathlessness Asthma • Detailed history • Variable air flow obstruction • Central to all definitions of asthma is the presence of more than 1 symptom of 1. Wheezes 2. Breathlessness 3. Chest Tightness 4. Cough NB Both conditions can exist in the same patient Quality Education for a Healthier Scotland
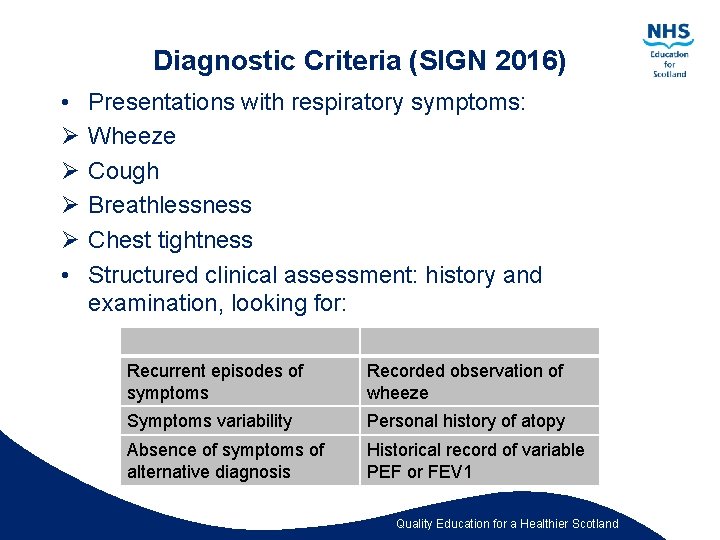
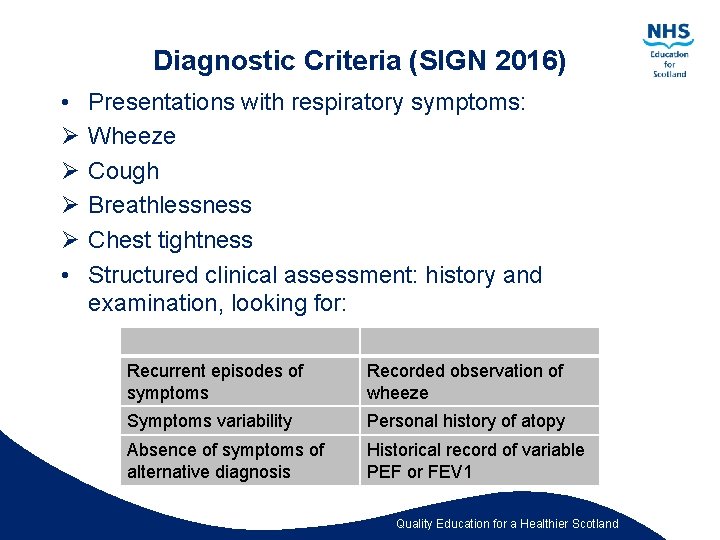
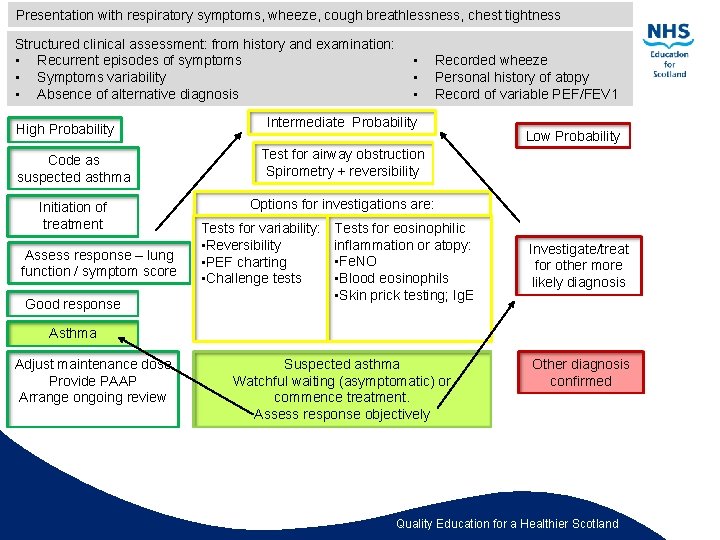
Diagnostic Criteria (SIGN 2016) • Ø Ø • Presentations with respiratory symptoms: Wheeze Cough Breathlessness Chest tightness Structured clinical assessment: history and examination, looking for: Recurrent episodes of symptoms Recorded observation of wheeze Symptoms variability Personal history of atopy Absence of symptoms of alternative diagnosis Historical record of variable PEF or FEV 1 Quality Education for a Healthier Scotland
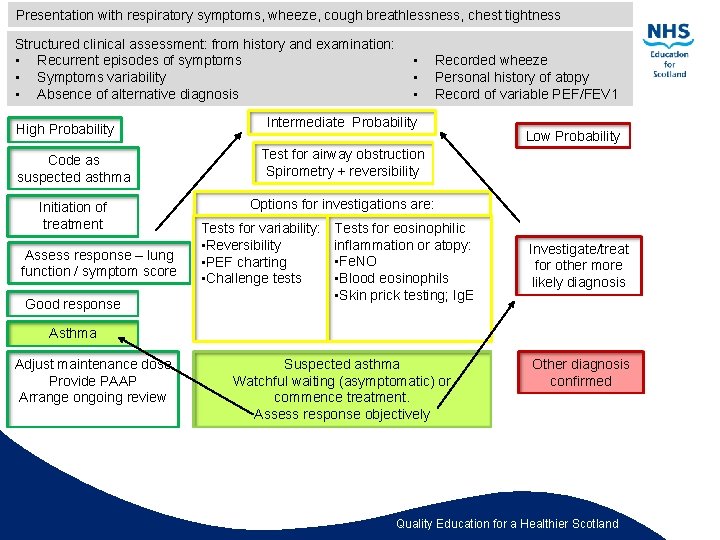
Presentation with respiratory symptoms, wheeze, cough breathlessness, chest tightness Structured clinical assessment: from history and examination: • Recurrent episodes of symptoms • Symptoms variability • Absence of alternative diagnosis High Probability • • • Intermediate Probability Code as suspected asthma Test for airway obstruction Spirometry + reversibility Initiation of treatment Options for investigations are: Assess response – lung function / symptom score Good response Recorded wheeze Personal history of atopy Record of variable PEF/FEV 1 Tests for variability: • Reversibility • PEF charting • Challenge tests Tests for eosinophilic inflammation or atopy: • Fe. NO • Blood eosinophils • Skin prick testing; Ig. E Low Probability Investigate/treat for other more likely diagnosis Asthma Adjust maintenance dose Provide PAAP Arrange ongoing review Suspected asthma Watchful waiting (asymptomatic) or commence treatment. Assess response objectively Other diagnosis confirmed Quality Education for a Healthier Scotland
Spirometry in Asthma • Spirometry recommended objective test to identify abnormalities in lung volumes and air flow (PCC 2013) • Use at clinic visits for diagnosis, alternatively domiciliary PEF • Spirometry with reversibility as appropriate preferred initial test • Used in conjunction with physical assessment, history taking, blood tests and x-rays, to exclude or confirm particular types of lung disease, enabling timely diagnosis and treatment • Should only be performed by people trained and assessed to ARTP or equivalent standards by recognised training bodies (PCC 2013) • All health professionals involved in the care of people with COPD should have access to spirometry and be able to interpret results (NICE 2010) Quality Education for a Healthier Scotland
Conclusion • Failure to accurately diagnose matters, prognoses for patients with the 3 disorders differ • Incorrect diagnosis can lead to inappropriate management • Patients with well-controlled asthma should have normal activity levels and life expectancy Quality Education for a Healthier Scotland