Serious Reportable Events in 2015 Acute Care Hospitals
Serious Reportable Events in 2015 Acute Care Hospitals, Non-Acute Care Hospitals and Ambulatory Surgical Centers Katherine T. Fillo, Ph. D, RN-BC Quality Improvement Manager Bureau of Health Care Safety and Quality Lauren B. Nelson, JD Director of Policy and Quality Improvement Bureau of Health Care Safety and Quality Public Health Council August 23, 2016 Slide 1
Overview • Purpose • Background • Serious Reportable Event Category Definitions • Outcomes • Quality Improvement Activities Slide 2
Purpose This presentation is given for the following purposes: • To provide an update of the Serious Reportable Event program and related quality improvement activities at the Bureau of Health Care Safety and Quality; and • To share the trends in the types and volume of Serious Reportable Events reported in 2015 and previous years. Slide 3
Background • Adverse events that occur in the health care setting are a patient safety concern and public health issue. • It is estimated that 10% of Medicare patients nationally experience an adverse event during a rehabilitation hospital stay (OIG, 2016). • Recent multiple hospital studies showed that as many as 1/3 of patients nationally were harmed during their hospitalization (Landrigan, et. al. , 2010). • Section 51 H of chapter 111 of the Massachusetts General Laws authorizes the Department to collect adverse medical event data and disseminate the information publicly to encourage quality improvement. Slide 4
Background • The National Quality Forum (NQF) has operationalized a group of adverse events into measurable, evidence-based outcomes called Serious Reportable Events (SRE). • MA adopted SREs as its adverse event reporting framework in 2008. • 27 other states have state-based adverse event reporting programs and over half use the SRE framework including Connecticut, Minnesota and New Hampshire. Slide 5
SREs Defined • Section 51 H of Chapter 111 of the General Laws: “Serious reportable event”, an event that results in a serious adverse patient outcome that is clearly identifiable and measurable, reasonably preventable, and that meets any other criteria established by the department in regulations. • 105 CMR 130. 332 and 105 CMR 140. 308: Serious Reportable Event (SRE) means an event that occurs on premises covered by a hospital's license that results in an adverse patient outcome, is clearly identifiable and measurable, has been identified to be in a class of events that are usually or reasonably preventable, and of a nature such that the risk of occurrence is significantly influenced by the policies and procedures of the hospital. The Department issued a list of SREs based on those events included on the NQF table of reportable events to which 105 CMR 130. 332 and 105 CMR 14. 308 apply in guidance. Slide 6
Reporting • Hospitals and ambulatory surgical centers (ASCs) are required to report SREs to the patient/family, third party payer, and the Bureau of Health Care Safety and Quality (BHCSQ) within seven days of the incident. • An updated report to all three parties is required within 30 days of the incident, including documentation of the root cause analysis findings and determination of preventability as required by 105 CMR 130. 332(c) & 105 CMR 140. 308(c). • In June 2009, the Department implemented regulations prohibiting health care facilities from charging for services provided as a result of preventable SREs. Slide 7
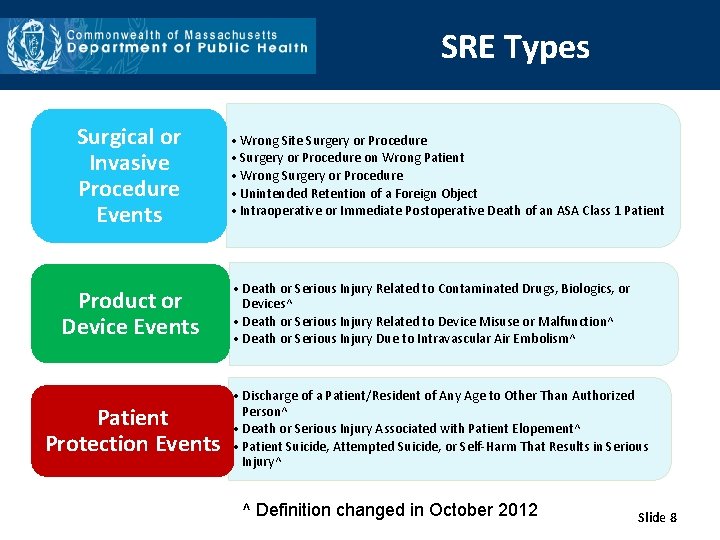
SRE Types Surgical or Invasive Procedure Events Product or Device Events Patient Protection Events • Wrong Site Surgery or Procedure • Surgery or Procedure on Wrong Patient • Wrong Surgery or Procedure • Unintended Retention of a Foreign Object • Intraoperative or Immediate Postoperative Death of an ASA Class 1 Patient • Death or Serious Injury Related to Contaminated Drugs, Biologics, or Devices^ • Death or Serious Injury Related to Device Misuse or Malfunction^ • Death or Serious Injury Due to Intravascular Air Embolism^ • Discharge of a Patient/Resident of Any Age to Other Than Authorized Person^ • Death or Serious Injury Associated with Patient Elopement^ • Patient Suicide, Attempted Suicide, or Self-Harm That Results in Serious Injury^ ^ Definition changed in October 2012 Slide 8
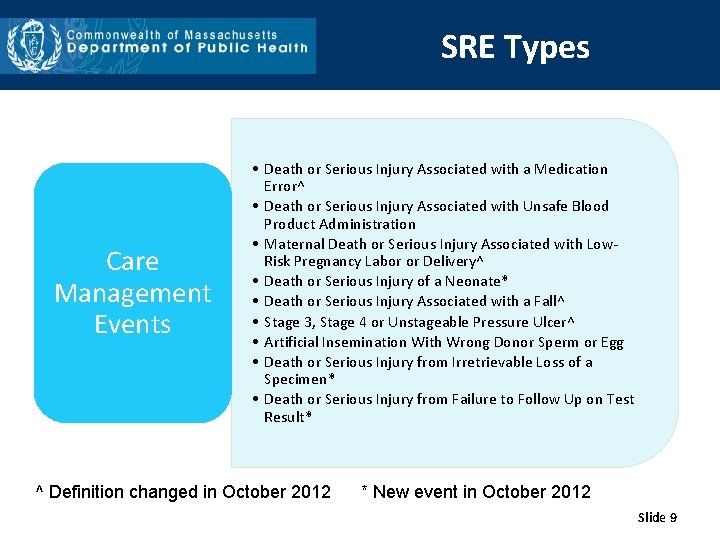
SRE Types Care Management Events • Death or Serious Injury Associated with a Medication Error^ • Death or Serious Injury Associated with Unsafe Blood Product Administration • Maternal Death or Serious Injury Associated with Low. Risk Pregnancy Labor or Delivery^ • Death or Serious Injury of a Neonate* • Death or Serious Injury Associated with a Fall^ • Stage 3, Stage 4 or Unstageable Pressure Ulcer^ • Artificial Insemination With Wrong Donor Sperm or Egg • Death or Serious Injury from Irretrievable Loss of a Specimen* • Death or Serious Injury from Failure to Follow Up on Test Result* ^ Definition changed in October 2012 * New event in October 2012 Slide 9
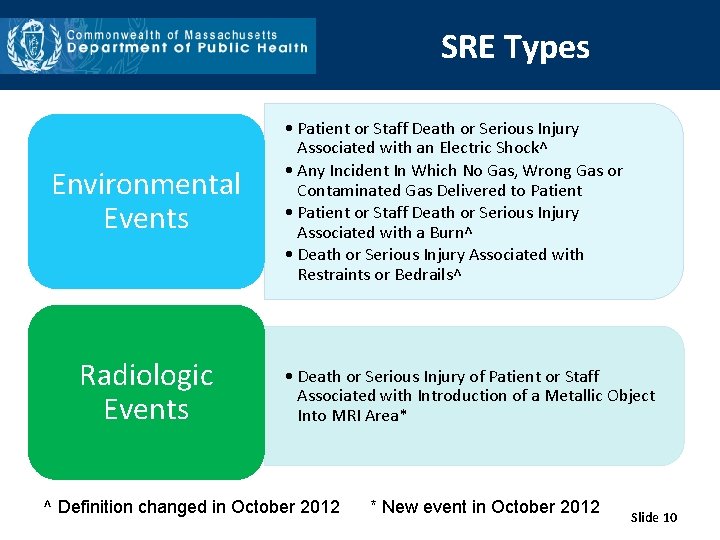
SRE Types Environmental Events Radiologic Events • Patient or Staff Death or Serious Injury Associated with an Electric Shock^ • Any Incident In Which No Gas, Wrong Gas or Contaminated Gas Delivered to Patient • Patient or Staff Death or Serious Injury Associated with a Burn^ • Death or Serious Injury Associated with Restraints or Bedrails^ • Death or Serious Injury of Patient or Staff Associated with Introduction of a Metallic Object Into MRI Area* ^ Definition changed in October 2012 * New event in October 2012 Slide 10
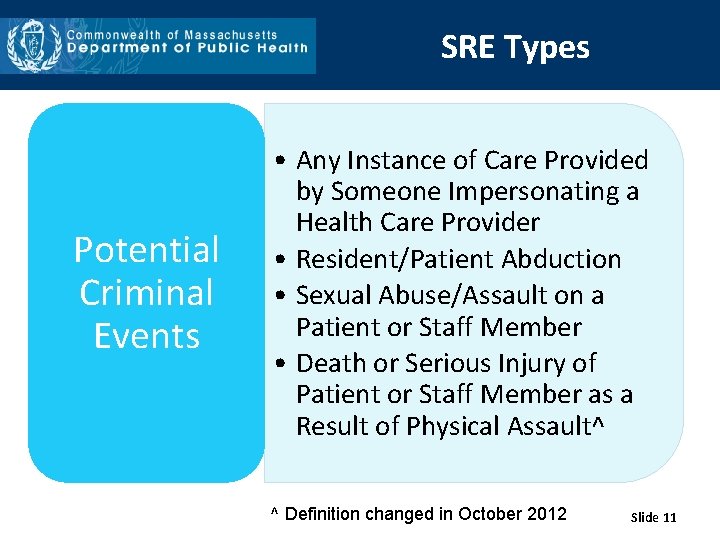
SRE Types Potential Criminal Events • Any Instance of Care Provided by Someone Impersonating a Health Care Provider • Resident/Patient Abduction • Sexual Abuse/Assault on a Patient or Staff Member • Death or Serious Injury of Patient or Staff Member as a Result of Physical Assault^ ^ Definition changed in October 2012 Slide 11
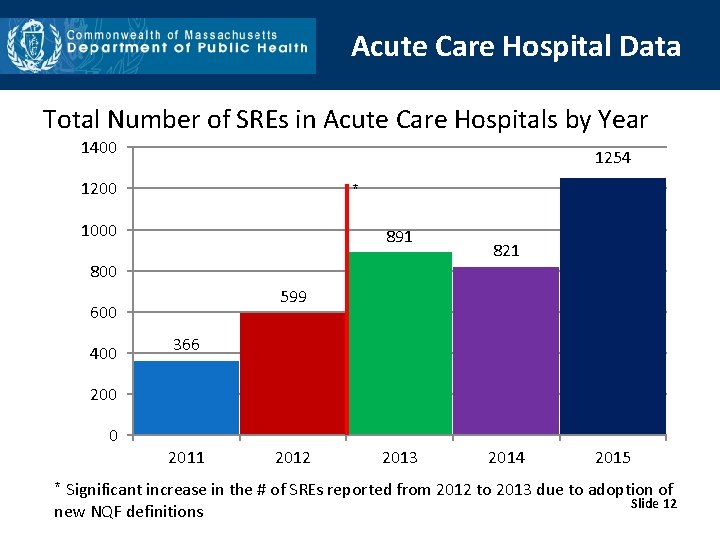
Acute Care Hospital Data Total Number of SREs in Acute Care Hospitals by Year 1400 1254 1200 * 1000 891 800 599 600 400 821 366 200 0 2011 2012 2013 2014 2015 * Significant increase in the # of SREs reported from 2012 to 2013 due to adoption of Slide 12 new NQF definitions
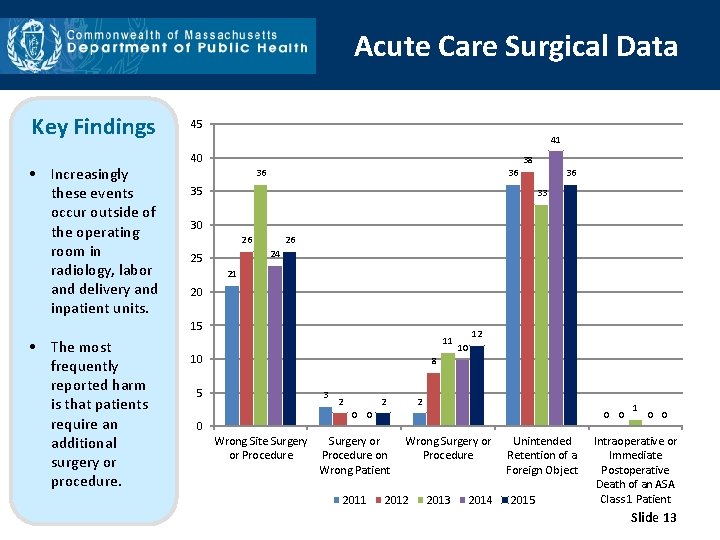
Acute Care Surgical Data Key Findings • Increasingly these events occur outside of the operating room in radiology, labor and delivery and inpatient units. 45 41 40 38 36 36 35 33 30 26 26 24 25 21 20 15 • The most frequently reported harm is that patients require an additional surgery or procedure. 36 11 10 12 10 8 5 3 2 2 2 0 0 0 Wrong Site Surgery or Procedure 0 0 Surgery or Procedure on Wrong Patient 2011 Wrong Surgery or Procedure 2012 2013 2014 Unintended Retention of a Foreign Object 2015 1 0 0 Intraoperative or Immediate Postoperative Death of an ASA Class 1 Patient Slide 13
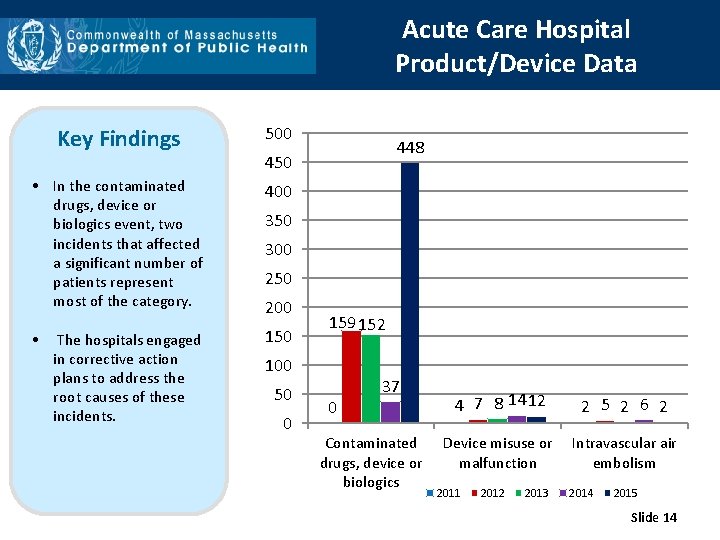
Acute Care Hospital Product/Device Data Key Findings 500 • In the contaminated drugs, device or biologics event, two incidents that affected a significant number of patients represent most of the category. 400 • 150 The hospitals engaged in corrective action plans to address the root causes of these incidents. 448 450 300 250 200 159 152 100 50 0 0 37 Contaminated drugs, device or biologics 4 7 8 14 12 2 5 2 6 2 Device misuse or malfunction Intravascular air embolism 2011 2012 2013 2014 2015 Slide 14
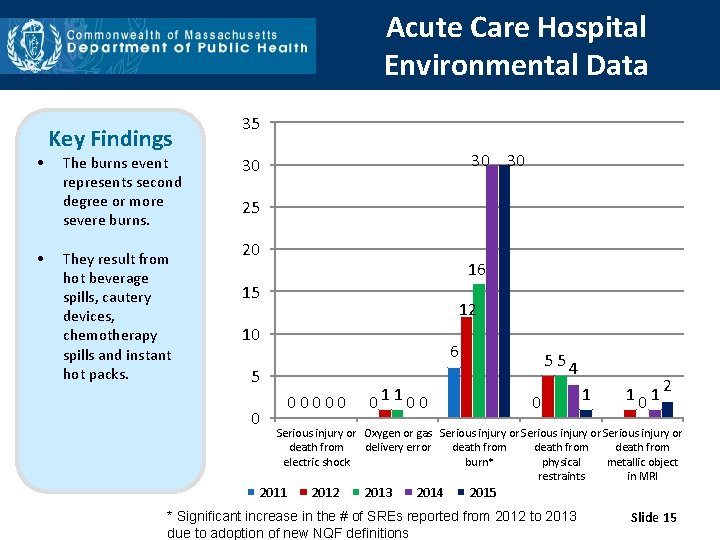
Acute Care Hospital Environmental Data • • Key Findings The burns event represents second degree or more severe burns. They result from hot beverage spills, cautery devices, chemotherapy spills and instant hot packs. 35 30 30 30 25 20 16 15 12 10 6 5 0 00000 554 01100 0 1 1012 Serious injury or Oxygen or gas Serious injury or death from delivery error death from electric shock burn* physical metallic object restraints in MRI 2011 2012 2013 2014 2015 * Significant increase in the # of SREs reported from 2012 to 2013 due to adoption of new NQF definitions Slide 15
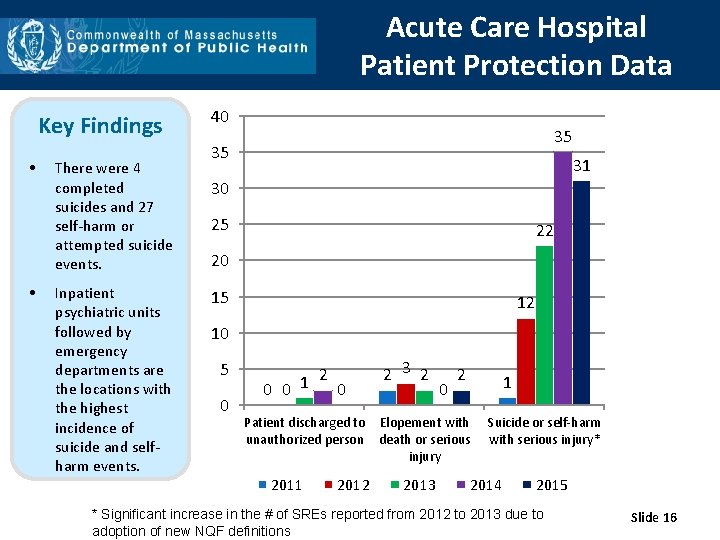
Acute Care Hospital Patient Protection Data Key Findings • • There were 4 completed suicides and 27 self-harm or attempted suicide events. Inpatient psychiatric units followed by emergency departments are the locations with the highest incidence of suicide and selfharm events. 40 35 35 31 30 25 22 20 15 12 10 5 0 2 0 0 1 0 2 3 2 0 2 1 Patient discharged to Elopement with unauthorized person death or serious injury 2011 2012 2013 Suicide or self-harm with serious injury* 2014 2015 * Significant increase in the # of SREs reported from 2012 to 2013 due to adoption of new NQF definitions Slide 16
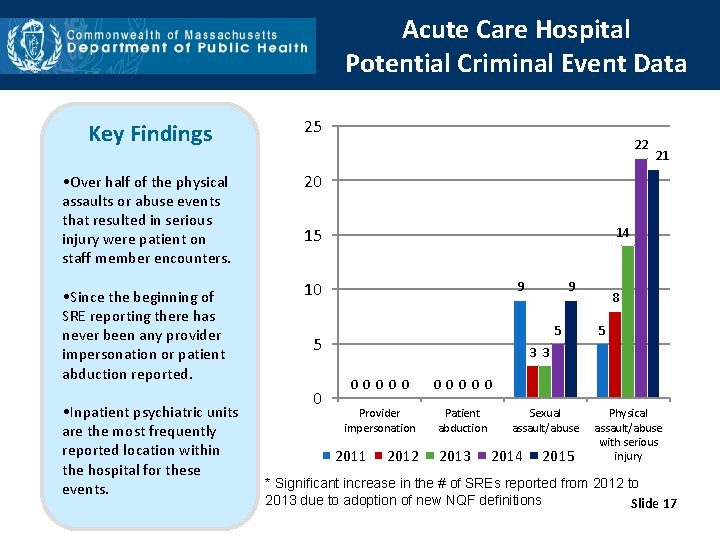
Acute Care Hospital Potential Criminal Event Data Key Findings 25 • Over half of the physical assaults or abuse events that resulted in serious injury were patient on staff member encounters. 20 • Since the beginning of SRE reporting there has never been any provider impersonation or patient abduction reported. 10 • Inpatient psychiatric units are the most frequently reported location within the hospital for these events. 22 14 15 9 9 5 5 0 21 8 5 3 3 0 0 0 0 0 Provider impersonation Patient abduction 2011 2012 2013 Sexual assault/abuse 2014 2015 Physical assault/abuse with serious injury * Significant increase in the # of SREs reported from 2012 to 2013 due to adoption of new NQF definitions Slide 17
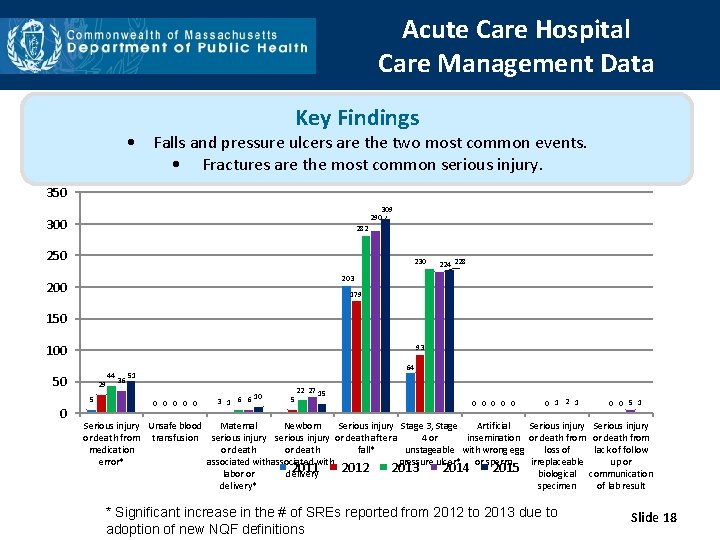
Acute Care Hospital Care Management Data Key Findings • Falls and pressure ulcers are the two most common events. • Fractures are the most common serious injury. 350 309 290 300 282 250 230 224 228 203 200 179 150 100 93 50 0 29 5 44 36 64 51 0 0 0 10 3 1 6 6 5 22 27 15 0 0 0 1 2 1 0 0 5 1 Serious injury Unsafe blood Maternal Newborn Serious injury Stage 3, Stage Artificial Serious injury or death from transfusion serious injury or death after a 4 or insemination or death from medication or death fall* unstageable with wrong egg loss of lack of follow error* associated with pressure ulcer* or sperm irreplaceable up or 2011 2012 2013 2014 2015 biological communication labor or delivery* specimen of lab result * Significant increase in the # of SREs reported from 2012 to 2013 due to adoption of new NQF definitions Slide 18
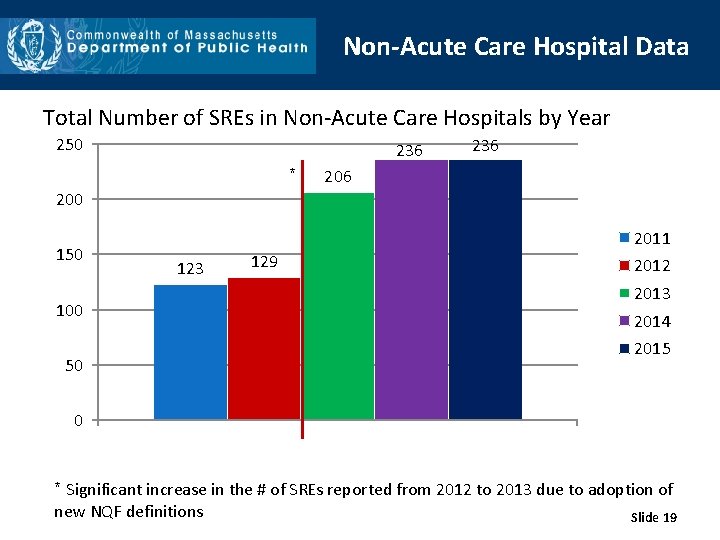
Non-Acute Care Hospital Data Total Number of SREs in Non-Acute Care Hospitals by Year 250 236 * 236 200 150 100 50 2011 123 129 2012 2013 2014 2015 0 * Significant increase in the # of SREs reported from 2012 to 2013 due to adoption of new NQF definitions Slide 19
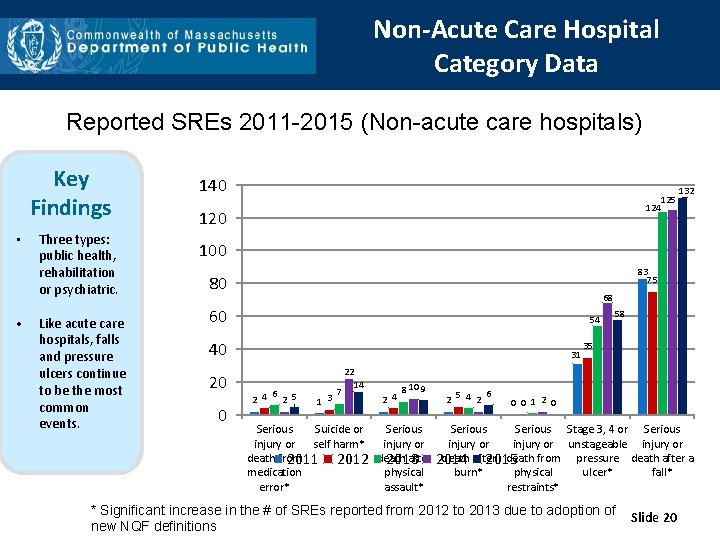
Non-Acute Care Hospital Category Data Reported SREs 2011 -2015 (Non-acute care hospitals) Key Findings • • Three types: public health, rehabilitation or psychiatric. Like acute care hospitals, falls and pressure ulcers continue to be the most common events. 140 124 120 125 132 100 83 75 80 68 60 54 40 20 0 31 6 2 4 2 5 1 3 7 22 14 2 4 8 10 9 6 2 5 4 2 58 35 0 0 1 2 0 Serious Suicide or Serious Stage 3, 4 or Serious injury or self harm* injury or unstageable injury or death from after 2014 death after death from pressure death after a 2011 2012 death 2013 2015 medication physical burn* physical ulcer* fall* error* assault* restraints* * Significant increase in the # of SREs reported from 2012 to 2013 due to adoption of new NQF definitions Slide 20
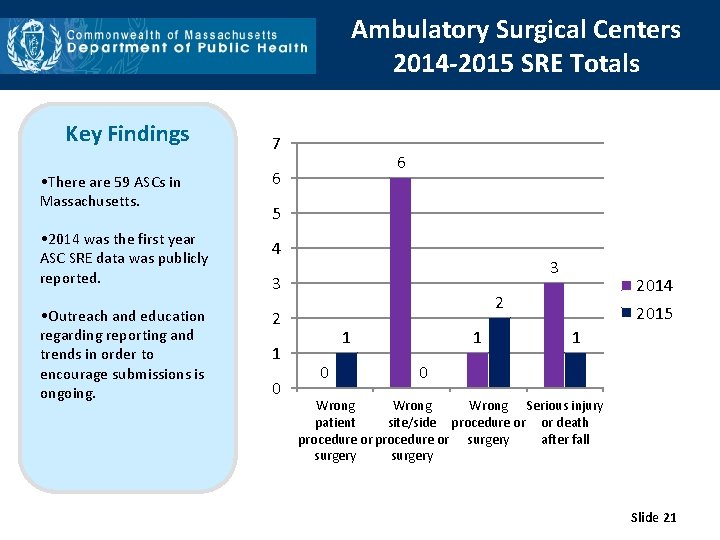
Ambulatory Surgical Centers 2014 -2015 SRE Totals Key Findings 7 • There are 59 ASCs in Massachusetts. 6 • 2014 was the first year ASC SRE data was publicly reported. 4 • Outreach and education regarding reporting and trends in order to encourage submissions is ongoing. 6 5 3 3 2 2 1 0 2014 1 0 1 2015 1 0 Wrong Serious injury patient site/side procedure or or death procedure or surgery after fall surgery Slide 21
Quality Improvement Activities • Partnering with Betsy Lehman Center to address the following: • Wrong site, wrong patient and wrong procedure cataract surgeries; and • Maintain an Interagency Service Agreement to allow for more seamless data sharing, as intended by the 2012 cost containment act. • Collaborated with the Department of Mental Health and DPH’s Suicide Prevention Program to develop and disseminate best practices for reducing suicide and self-harm in the inpatient setting ; • Actively participating in MA Coalition for the Prevention of Medical Errors; and • Working with individual facilities after a SRE occurs to develop corrective action plans and prevent an event of a similar type from happening in the future; and • Utilize DPH list serves for widespread education and to share Slide 22 appropriate guidance.
Contact Information Thank you for the opportunity to present this information today. Please direct any questions to: Katherine T. Fillo Ph. D, RN-BC Quality Improvement Manager Bureau of Health Care Safety and Quality katherine. fillo@state. ma. us Slide 23
- Slides: 23