Sepsis SIRS Wade Woelfle MD FAAEM UW ECC

- Slides: 44
Sepsis & SIRS Wade Woelfle, MD, FAAEM UW ECC 2016 June 21, 2016
Sepsis Objectives Definition Why and how it happens Identification Similar problems Monitoring Treatments New and revisited developments
Sepsis Inflammatory syndrome from severe infection Vasodilatation Increased WBCs Leakage of fluid from capillary beds Remote from the site of infection Infection = invasion of normally sterile tissue by organisms Bacteremia – Presence of viable bacteria in blood
SIRS Systemic Inflammatory Response Syndrome Identical to sepsis but without infection Noninfectious process as a cause Pancreatitis Autoimmune disease Vasculitis Thromboembolism Burns Surgery/trauma Pulmonary contusion
Definition of SIRS 2 or more of the following abnormalities Temp HR RR WBC count Note the lack of specificity Example: Patients with pulmonary edema
Basic Pathophysiology Poor regulation of inflammatory mediators Chain of events causing tissue injury Causes multiple organ dysfunction syndrome MODS High mortality
More Detailed Pathophysiology Bacterial components from site of infection Host immune response chemical signals from site of infection Both enter the bloodstream Vasodilatation and changes in vascular autoregulation Direct cellular toxicity BP drops and perfusion decreases Organ injury and dysfunction at sites away from the infection Heart, lungs, kidneys, liver, brain, coagulation cascade, etc.
Sepsis - Diagnostic Criteria Infection and some of these General variables Temp >38. 3 or < 36 HR > 90 RR >20 Altered Mental Status Edema/positive fluid balance (>20 ml/kg/24 hrs) Hyperglycemia
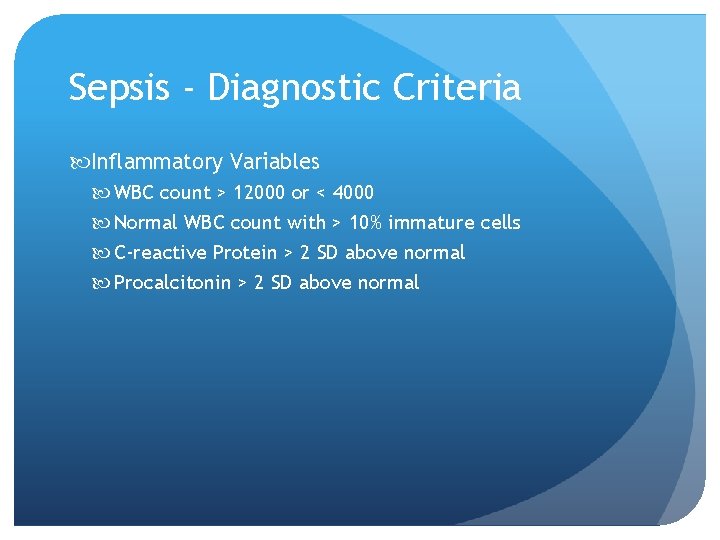
Sepsis - Diagnostic Criteria Inflammatory Variables WBC count > 12000 or < 4000 Normal WBC count with > 10% immature cells C-reactive Protein > 2 SD above normal Procalcitonin > 2 SD above normal
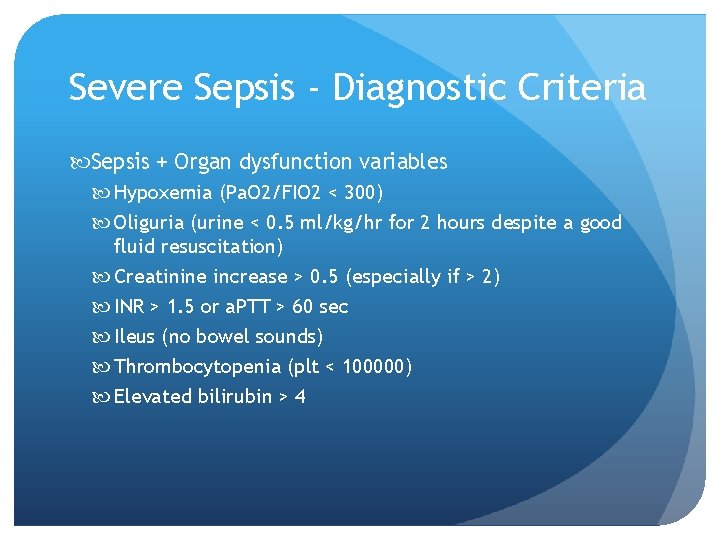
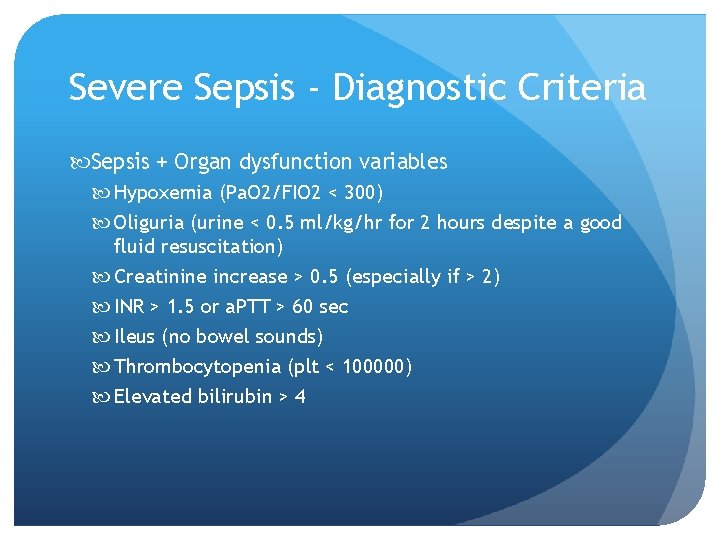
Severe Sepsis - Diagnostic Criteria Sepsis + Organ dysfunction variables Hypoxemia (Pa. O 2/FIO 2 < 300) Oliguria (urine < 0. 5 ml/kg/hr for 2 hours despite a good fluid resuscitation) Creatinine increase > 0. 5 (especially if > 2) INR > 1. 5 or a. PTT > 60 sec Ileus (no bowel sounds) Thrombocytopenia (plt < 100000) Elevated bilirubin > 4
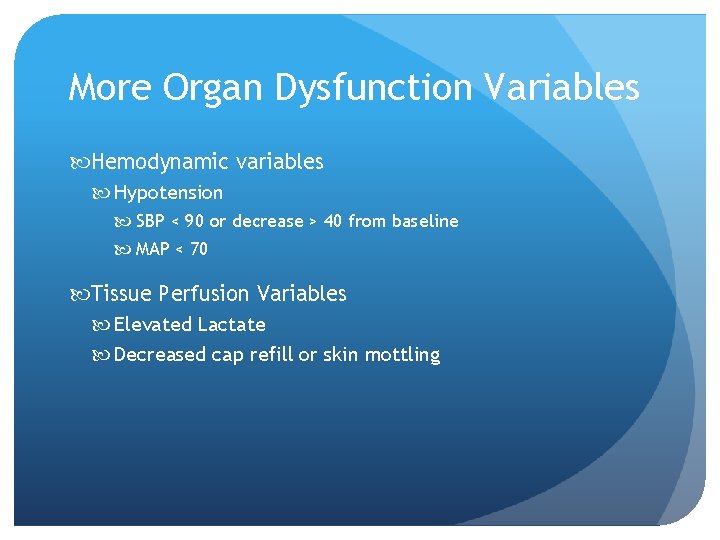
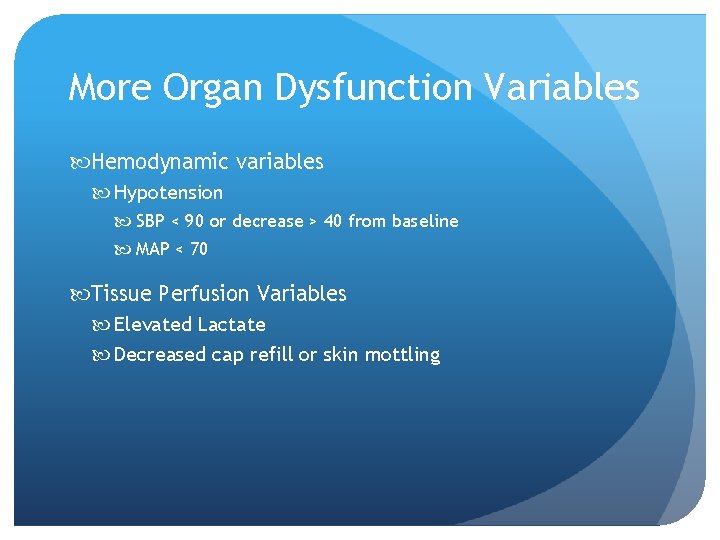
More Organ Dysfunction Variables Hemodynamic variables Hypotension SBP < 90 or decrease > 40 from baseline MAP < 70 Tissue Perfusion Variables Elevated Lactate Decreased cap refill or skin mottling
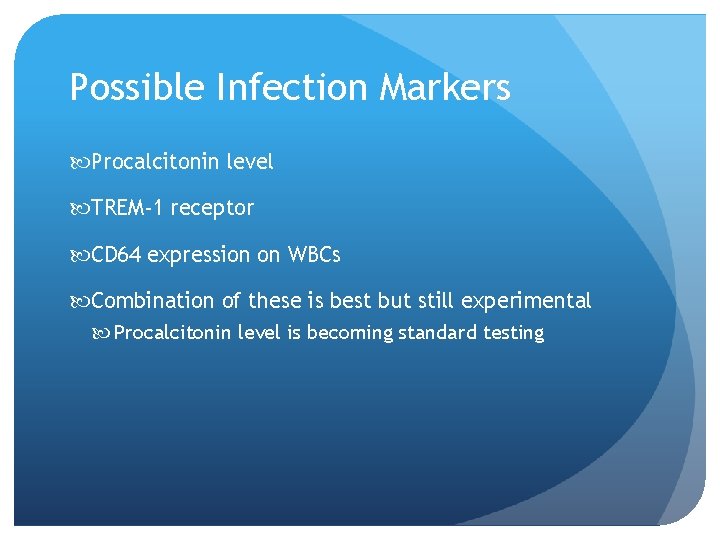
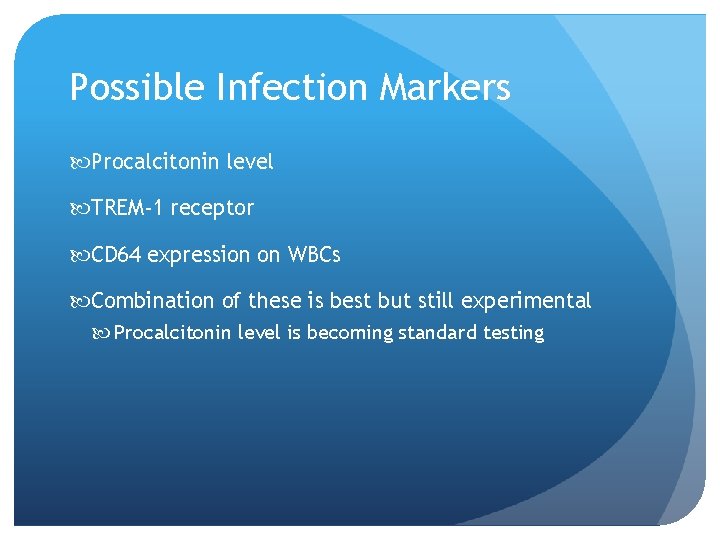
Possible Infection Markers Procalcitonin level TREM-1 receptor CD 64 expression on WBCs Combination of these is best but still experimental Procalcitonin level is becoming standard testing
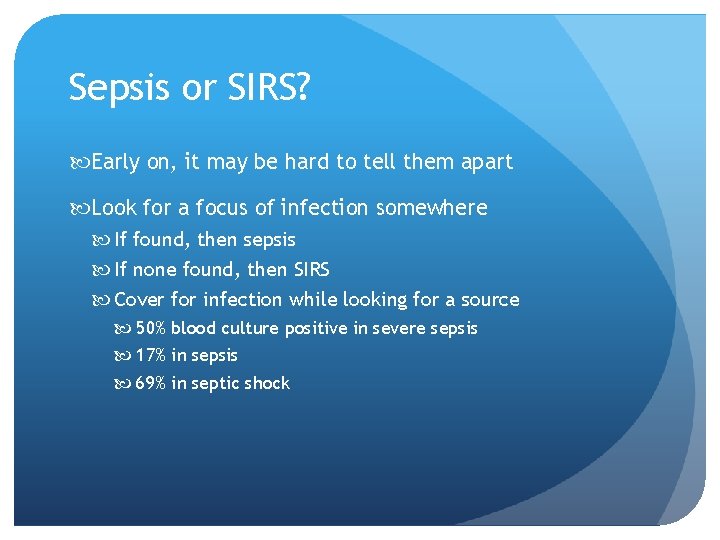
Sepsis or SIRS? Early on, it may be hard to tell them apart Look for a focus of infection somewhere If found, then sepsis If none found, then SIRS Cover for infection while looking for a source 50% blood culture positive in severe sepsis 17% in sepsis 69% in septic shock
Septic Shock Sepsis with hypotension Despite 30 ml/kg IV fluid MODS Multiple abnormalities listed above Labs BP Mental Status Urine Output
Sepsis Risk Factors Nosocomial infection (antibiotics or ICU stay) Bacteremia (positive blood cultures) Age 65 or greater Immunosuppression Cancer, renal/liver failure, AIDS, medications, splenectomy Diabetes Community Acquired Pneumonia Genetics
Sepsis Epidemiology US estimate 1. 665 million cases per year (and increasing) Older population (60 -85% of cases) More immunosuppressive meds More antibiotic resistance Maybe better detection Highest incidence is African American Males Highest in winter (Respiratory infections/flu)
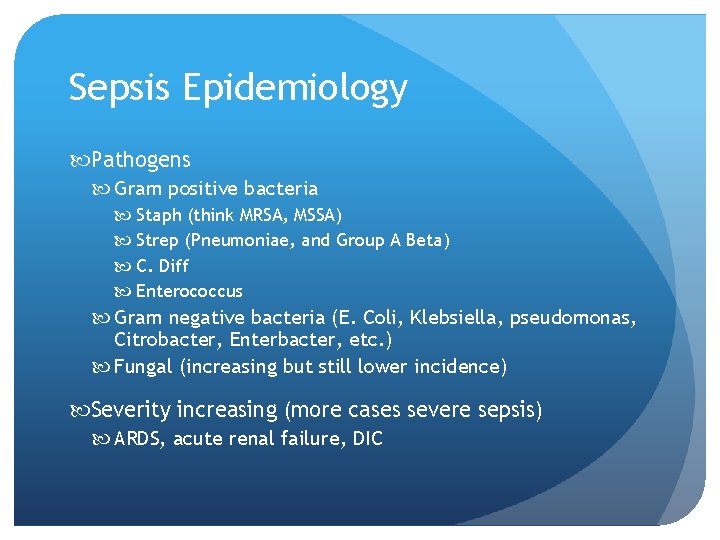
Sepsis Epidemiology Pathogens Gram positive bacteria Staph (think MRSA, MSSA) Strep (Pneumoniae, and Group A Beta) C. Diff Enterococcus Gram negative bacteria (E. Coli, Klebsiella, pseudomonas, Citrobacter, Enterbacter, etc. ) Fungal (increasing but still lower incidence) Severity increasing (more cases severe sepsis) ARDS, acute renal failure, DIC
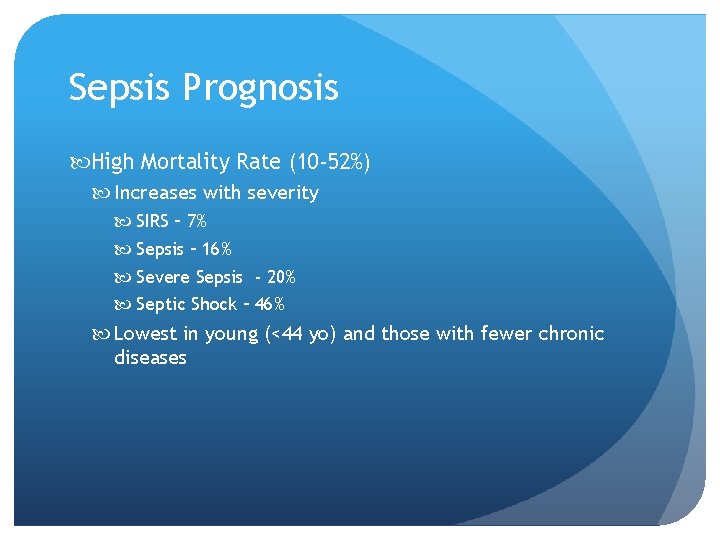
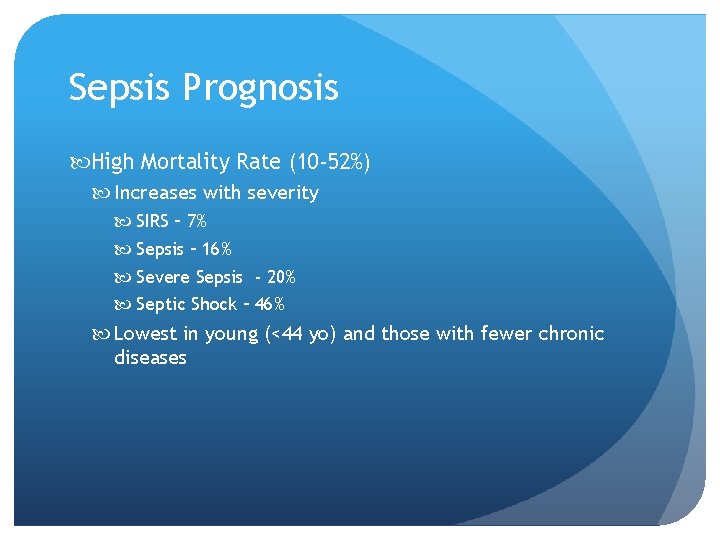
Sepsis Prognosis High Mortality Rate (10 -52%) Increases with severity SIRS – 7% Sepsis – 16% Severe Sepsis - 20% Septic Shock – 46% Lowest in young (<44 yo) and those with fewer chronic diseases
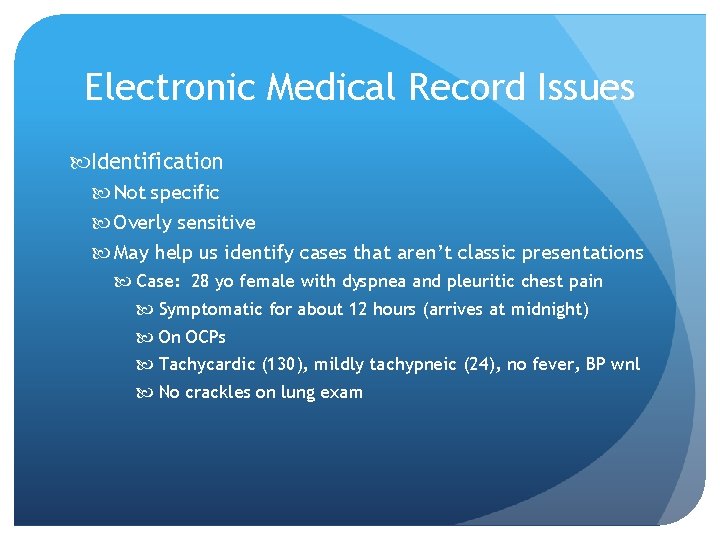
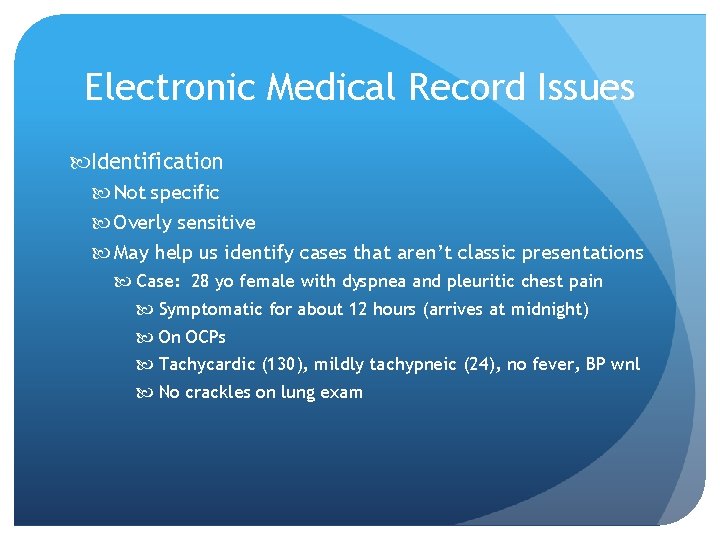
Electronic Medical Record Issues Identification Not specific Overly sensitive May help us identify cases that aren’t classic presentations Case: 28 yo female with dyspnea and pleuritic chest pain Symptomatic for about 12 hours (arrives at midnight) On OCPs Tachycardic (130), mildly tachypneic (24), no fever, BP wnl No crackles on lung exam
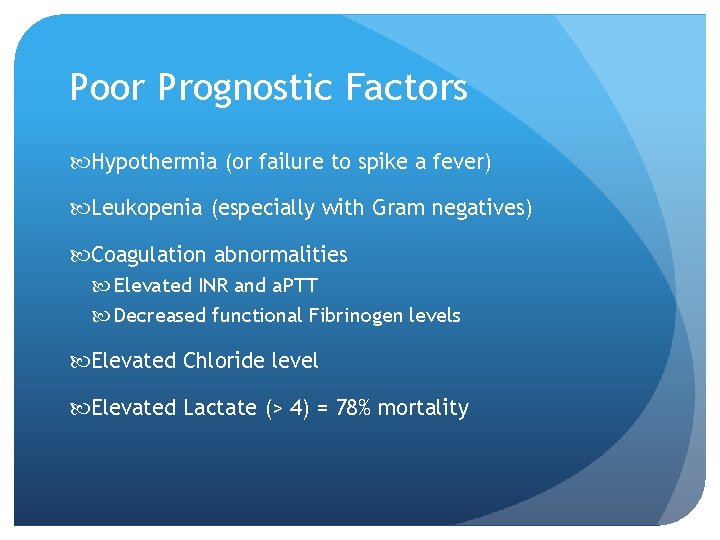
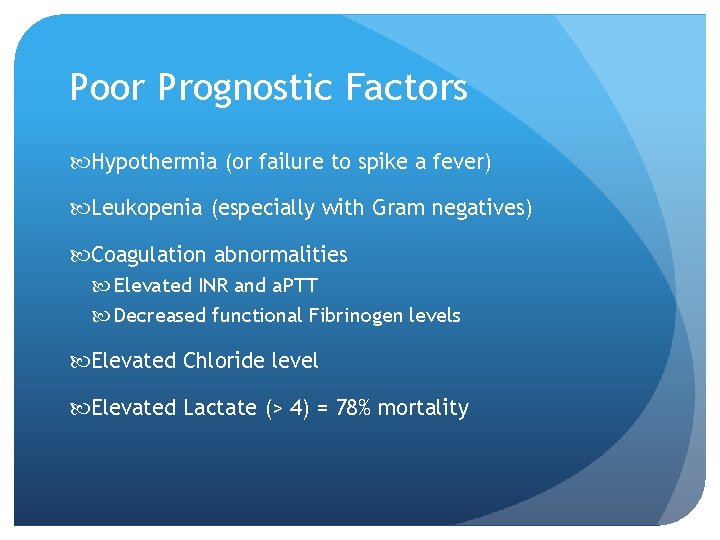
Poor Prognostic Factors Hypothermia (or failure to spike a fever) Leukopenia (especially with Gram negatives) Coagulation abnormalities Elevated INR and a. PTT Decreased functional Fibrinogen levels Elevated Chloride level Elevated Lactate (> 4) = 78% mortality
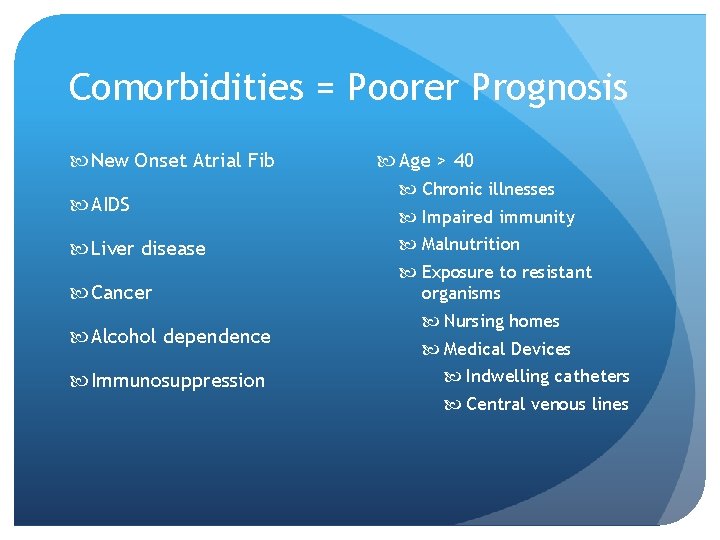
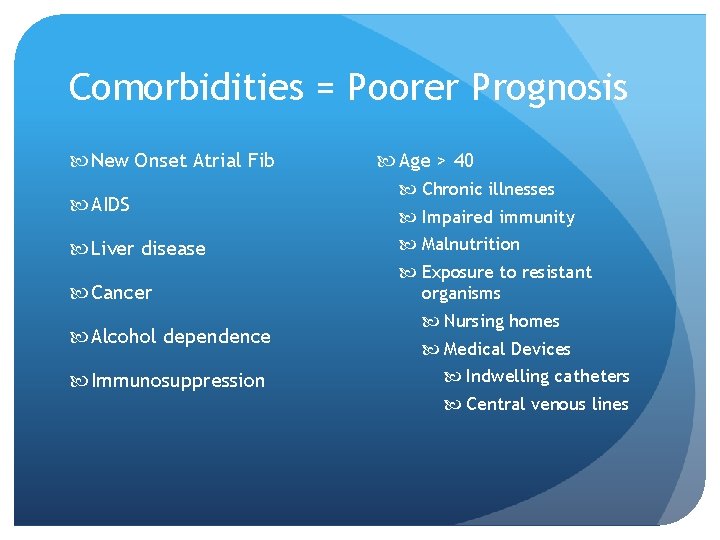
Comorbidities = Poorer Prognosis New Onset Atrial Fib AIDS Liver disease Cancer Alcohol dependence Immunosuppression Age > 40 Chronic illnesses Impaired immunity Malnutrition Exposure to resistant organisms Nursing homes Medical Devices Indwelling catheters Central venous lines
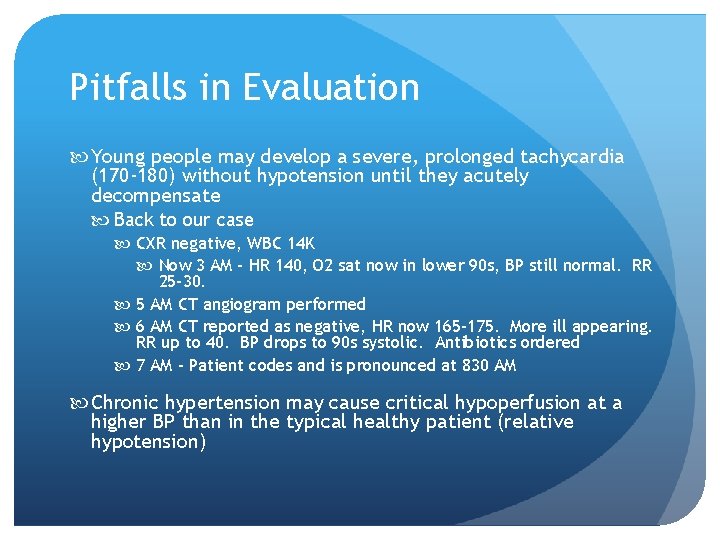
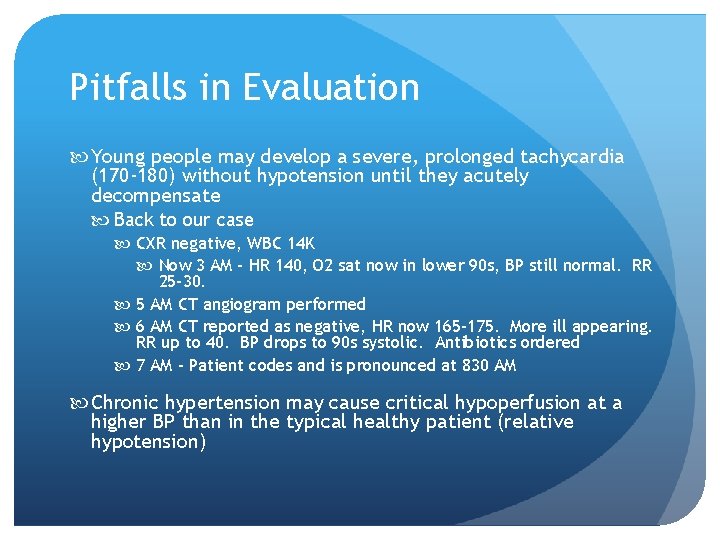
Pitfalls in Evaluation Young people may develop a severe, prolonged tachycardia (170 -180) without hypotension until they acutely decompensate Back to our case CXR negative, WBC 14 K Now 3 AM - HR 140, O 2 sat now in lower 90 s, BP still normal. RR 25 -30. 5 AM CT angiogram performed 6 AM CT reported as negative, HR now 165 -175. More ill appearing. RR up to 40. BP drops to 90 s systolic. Antibiotics ordered 7 AM – Patient codes and is pronounced at 830 AM Chronic hypertension may cause critical hypoperfusion at a higher BP than in the typical healthy patient (relative hypotension)
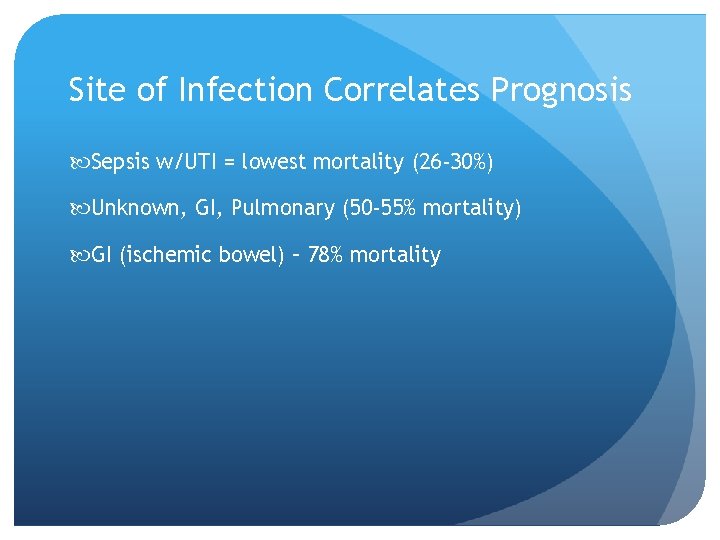
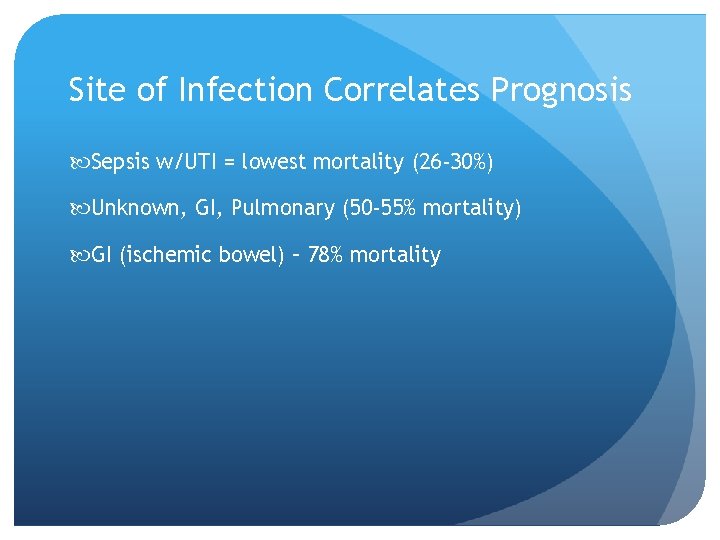
Site of Infection Correlates Prognosis Sepsis w/UTI = lowest mortality (26 -30%) Unknown, GI, Pulmonary (50 -55% mortality) GI (ischemic bowel) – 78% mortality
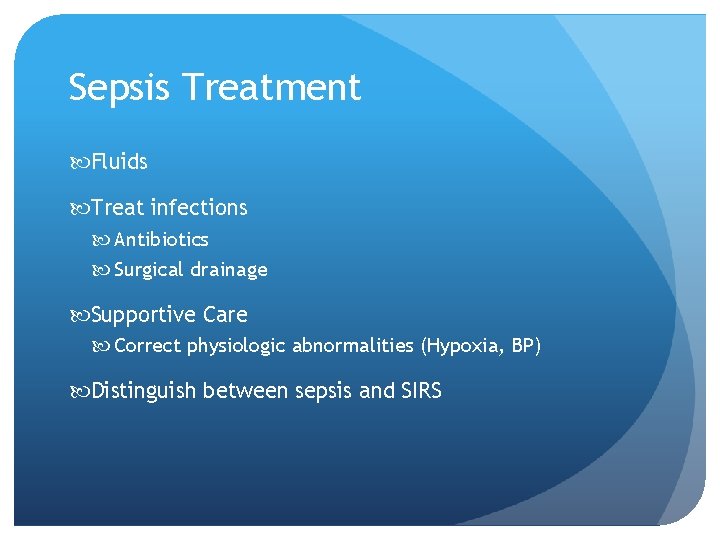
Sepsis Treatment Fluids Treat infections Antibiotics Surgical drainage Supportive Care Correct physiologic abnormalities (Hypoxia, BP) Distinguish between sepsis and SIRS
Early Management ABCs Oxygen Monitor pulse ox Consider intubation and mechanical ventilation Decrease work of breathing Airway protection for decreased mental status Diagnostics ABG CXR Labs including cultures
Early Management Correct decreased tissue perfusion Monitor BP (frequently) Consider arterial line monitoring, if BP unstable Hypotension is most common sign Other signs include tachycardia, decreased capillary refill, decreased mental status/restlessness, decreased urine output Modified by preexisting conditions or meds i. e. Beta blockers Follow Lactate levels
Fluid Management Venous Access ASAP May need a central line Fluids, pressors, blood products Blood draws Central venous pressure (? ) Central venous Oxygen saturation (? ) Pulmonary artery catheter (Swan-Ganz) No longer routinely used Cv. P and Scv. O 2 give similar findings More Complications
Fluid Management IVFs (crystalloids) May need 2 -5 L over 6 hours (500 ml boluses) Careful if history of CHF Assess volume status, perfusion, BP, and signs of pulmonary edema or ARDS Fluid overload is common Monitor fluid responsiveness/perfusion and don’t continue once improvement stops
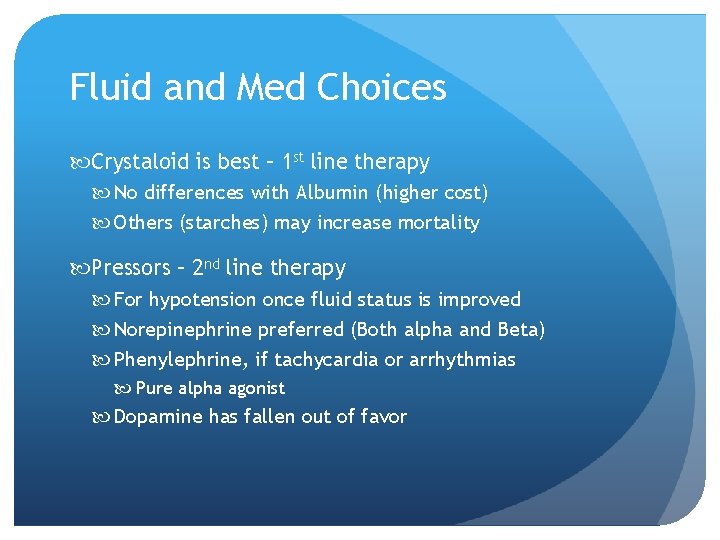
Fluid and Med Choices Crystaloid is best – 1 st line therapy No differences with Albumin (higher cost) Others (starches) may increase mortality Pressors – 2 nd line therapy For hypotension once fluid status is improved Norepinephrine preferred (Both alpha and Beta) Phenylephrine, if tachycardia or arrhythmias Pure alpha agonist Dopamine has fallen out of favor
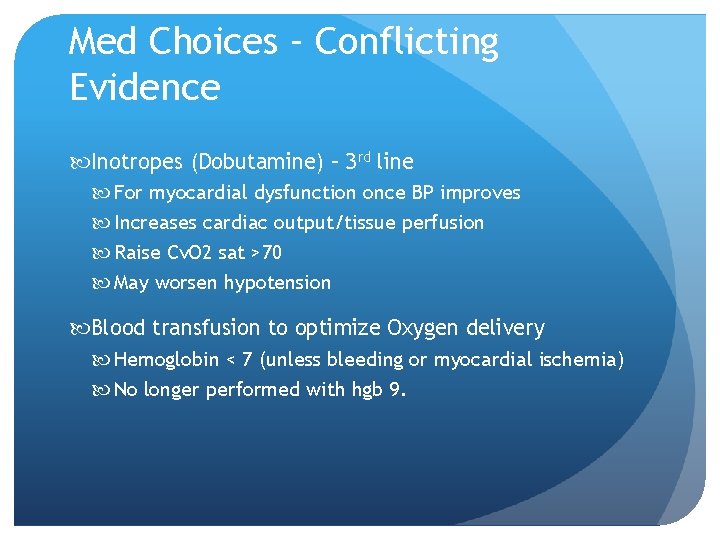
Med Choices – Conflicting Evidence Inotropes (Dobutamine) – 3 rd line For myocardial dysfunction once BP improves Increases cardiac output/tissue perfusion Raise Cv. O 2 sat >70 May worsen hypotension Blood transfusion to optimize Oxygen delivery Hemoglobin < 7 (unless bleeding or myocardial ischemia) No longer performed with hgb 9.
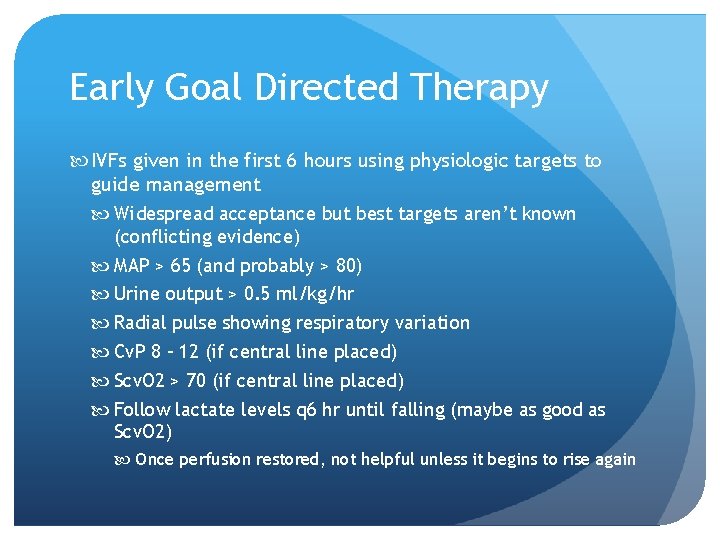
Early Goal Directed Therapy IVFs given in the first 6 hours using physiologic targets to guide management Widespread acceptance but best targets aren’t known (conflicting evidence) MAP > 65 (and probably > 80) Urine output > 0. 5 ml/kg/hr Radial pulse showing respiratory variation Cv. P 8 – 12 (if central line placed) Scv. O 2 > 70 (if central line placed) Follow lactate levels q 6 hr until falling (maybe as good as Scv. O 2) Once perfusion restored, not helpful unless it begins to rise again
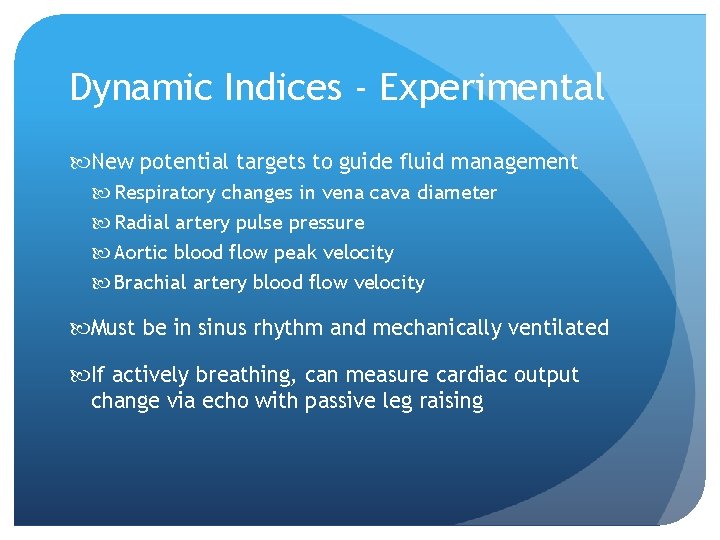
Dynamic Indices - Experimental New potential targets to guide fluid management Respiratory changes in vena cava diameter Radial artery pulse pressure Aortic blood flow peak velocity Brachial artery blood flow velocity Must be in sinus rhythm and mechanically ventilated If actively breathing, can measure cardiac output change via echo with passive leg raising
Protocol Directed Therapy (EGDT) Scv. O 2, CVP, MAP, urine output, and lactate Guide fluid resuscitation Early administration of antibiotics Guide first 6 hours of presentation Conflicting evidence Central lines originally required (complications) Original study funded by company making central lines Some studies show no difference from normal care
Bottom Line Whether protocols, early goal directly therapy, or usual care is given Fluid resuscitation should begin within 6 hours Stopped or reduced when perfusion restored Antibiotics given expeditiously when it appears that infection is present/worked up If perfusion deficit/organ failure progresses Reassess adequacy of fluids, antibiotics, need for surgical care, accuracy of diagnosis, complications When patient responds, back off of support but monitor the markers for sepsis (BP, UO, labs, etc. ) Reevaluate if worsening or not continuing to improve
Dealing with the Focus of Infection Identify site of infection Info from History and Physical Blood culture 2 sites, aerobic and anaerobic Urine cultures, sputum culture and Gram stain ? CSF CXR Infected line, indwelling catheter, site of injury in trauma patient
Treating Site of Infection Early, appropriate antibiotics after cultures Started within 6 hours (prefer 1 hour) Consider recent antibiotics, comorbidities, and possibility of hospital/health care acquired infection Late/Inadequate/inappropriate antibiotic = poor outcome
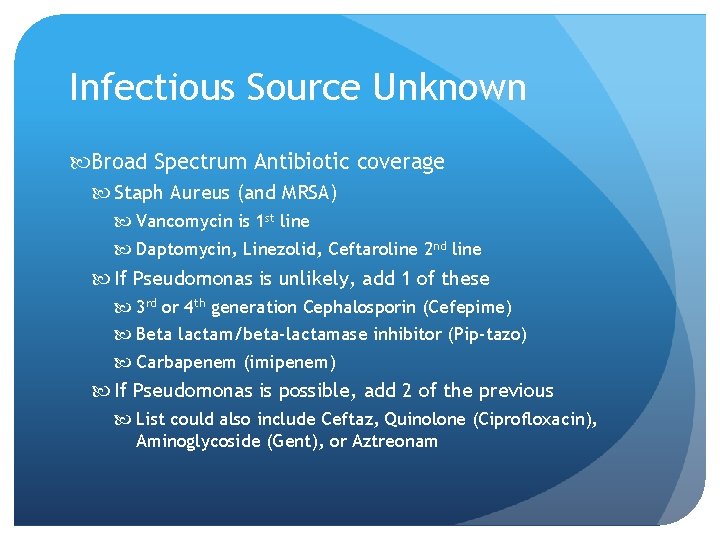
Infectious Source Unknown Broad Spectrum Antibiotic coverage Staph Aureus (and MRSA) Vancomycin is 1 st line Daptomycin, Linezolid, Ceftaroline 2 nd line If Pseudomonas is unlikely, add 1 of these 3 rd or 4 th generation Cephalosporin (Cefepime) Beta lactam/beta-lactamase inhibitor (Pip-tazo) Carbapenem (imipenem) If Pseudomonas is possible, add 2 of the previous List could also include Ceftaz, Quinolone (Ciprofloxacin), Aminoglycoside (Gent), or Aztreonam
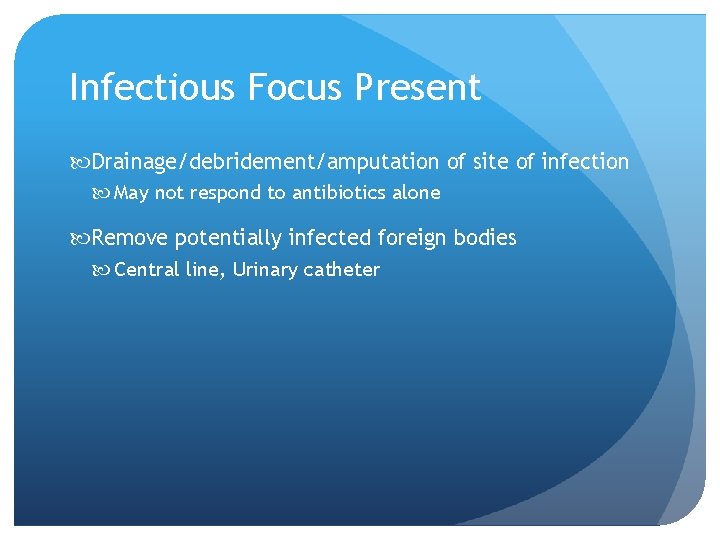
Infectious Focus Present Drainage/debridement/amputation of site of infection May not respond to antibiotics alone Remove potentially infected foreign bodies Central line, Urinary catheter
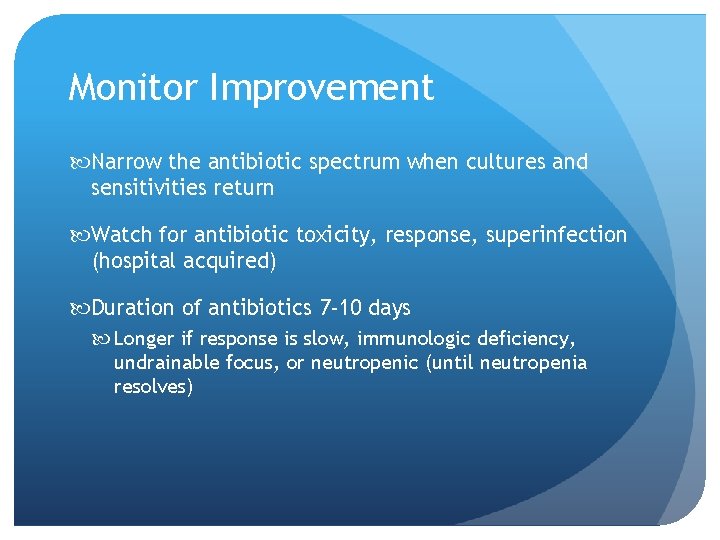
Monitor Improvement Narrow the antibiotic spectrum when cultures and sensitivities return Watch for antibiotic toxicity, response, superinfection (hospital acquired) Duration of antibiotics 7 -10 days Longer if response is slow, immunologic deficiency, undrainable focus, or neutropenic (until neutropenia resolves)

Additional Therapies Steroids (glucocorticoids) Treat host inflammatory response Most likely to help hypotensive septic shock unresponsive to fluids and pressors Nutrition Helps conserve body weight and muscle mass May not change clinical outcomes Venous thromboembolus prophylaxis Reduces risk of DVT/PE
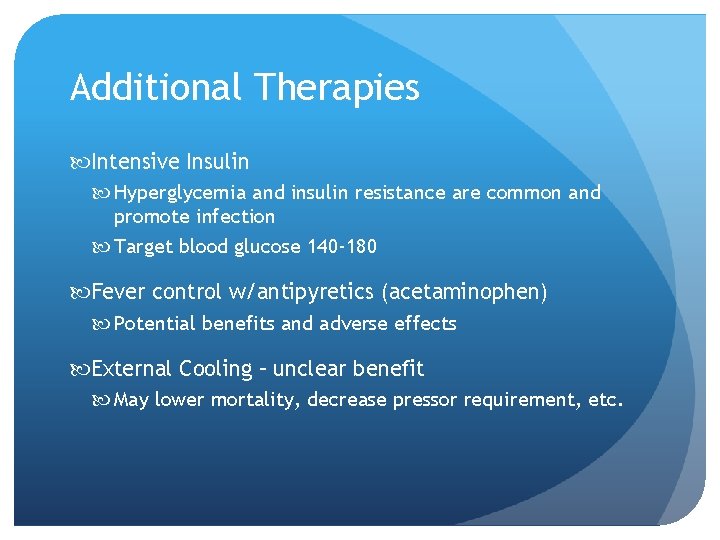
Additional Therapies Intensive Insulin Hyperglycemia and insulin resistance are common and promote infection Target blood glucose 140 -180 Fever control w/antipyretics (acetaminophen) Potential benefits and adverse effects External Cooling – unclear benefit May lower mortality, decrease pressor requirement, etc.
Effect of Improving Sepsis Treatment Some studies now show decreasing mortality 50% risk reduction Possibly due to better therapeutic strategy Appropriate antibiotics Restoration of perfusion Questionable if sepsis bundles/Goal-Directed Therapy make any difference Risk remains post-survival Death rate increased at 1 year Recurrent sepsis/hospital admission Resistant bacteria (especially Gram negatives) Long-term care facility admission Decreased quality of life
Readmission Diagnoses After Sepsis CHF Pneumonia COPD exacerbation UTI C. Diff
References Up. To. Date search was used with “sepsis” as a search term. The following Up. To. Date articles were used as references Sepsis syndromes in adults: Epidemiology, definitions, clinical presentation, diagnosis, and prognosis Evaluation and management of suspected sepsis and septic shock in adults Pathophysiology of sepsis