Sepsis Management National Clinical Guideline No 6 1
- Slides: 25
Sepsis Management National Clinical Guideline No. 6 1
Sepsis Management Guideline 2 National Clinical • The aim of the guideline is to facilitate the early recognition and appropriate treatment of sepsis in Ireland in order to maximise survival and minimise the burden of chronic sequelae. • All information regarding the guideline is available on QPulse • The summary document is available at: www. health. gov. ie/patient-safety/ncec www. hse. ie/sepsis • The guideline adapts the Surviving Sepsis Campaign guidelines 2013 and Sepsis Six to the Irish context.
3 Sepsis Management Guideline National Clinical “Sepsis is a life threatening condition that arises when the body’s response to an infection injures its own tissues and organs. Sepsis leads to shock, multiple organ failure and death especially if not recognised early and treated promptly. Sepsis remains the primary cause of death from infection despite advances in modern medicine, including vaccines, antibiotics and acute care. Millions of people die of sepsis every year worldwide. ” Merinoff Symposium 2010: Sepsis
4 International context • Approximately 300 cases per 100, 000 population per annum. As comparators, myocardial infarction affects 208 and stroke 223 patients per 100, 000 per year. • Mortality from sepsis is currently as high as mortality from acute myocardial infarction was in the 1960 s. • In the U. K. sepsis is estimated to claim 37, 000 lives annually and cost the NHS approximately £ 2. 5 billion. Sepsis incidence is predicted to grow at a rate of 1. 5% annually due to: - aging population - increased numbers of invasive procedures - increasing number of people living with co-morbidities - increasing number of people long-term immunosuppressive therapies. •
5 Irish Context • Up to 60% of all hospital deaths have a sepsis or infection diagnosis (HIPE data) • Irish Intensive Care Units Mortality rates of patients with a diagnosis of sepsis is 28. 8% Mortality rates reduced by 17. 7% and average length of stay is decreasing every year with increased awareness. (National Clinical Effectiveness Committee, 2014; Dellinger et al 2013) • • Each hour of delay in antimicrobial administration associated with an average decrease in survival of 7. 6% (Kumar et al, 2006)
6 UK report from the Health Service Ombudsman • • • Lack of timely history and examination on presentation Lack of necessary investigations Failure to recognise the severity of the illness Inadequate first-line treatment with fluids and antibiotics Delay in administering first-line treatment Inadequate physiological monitoring of vital signs Delay in source control of infection Delay in senior medical input Lack of timely referral to critical care
7 Sepsis Management Program is aimed at early identification and treatment of patients with sepsis lead to reduced mortality timely ICU admission decrease ICU length of stay
DEFINITIONS KNOW IMPORTANT TO 8 Infection is defined as a pathological process caused by invasion of normally sterile tissue or fluid or body cavity by pathogenic or potentially pathogenic micro-organisms. Sepsis is the clinical syndrome defined by the presence of both infection and the systemic inflammatory response syndrome (SIRS). Severe sepsis refers to sepsis complicated by organ dysfunction. Septic shock is defined as severe sepsis with circulatory shock with signs of organ dysfunction or hypoperfusion. Australian Modification of ICD-10 incorporating the Australian Classification of Health Interventions and the Australian Coding
PATHOPHYSIOLOGY OF SEPSIS • • • Pathogenic features of the microorganism Patient’s immune response to these features Failure of the immune system to control an initially localised infection Exaggerated immune and inflammatory response Cellular dysfunction Vasodilation and leaky capillaries
PATHOPHYSIOLOGY OF SEPSIS • • Distributive shock Myocardial depression Bone marrow suppression Activation of clotting cascade � DIC (Disseminatedd Intrtavascular Caogulation) • • • Organ dysfunction MODS (Multiple Organ Dysfunction Syndrome) Death
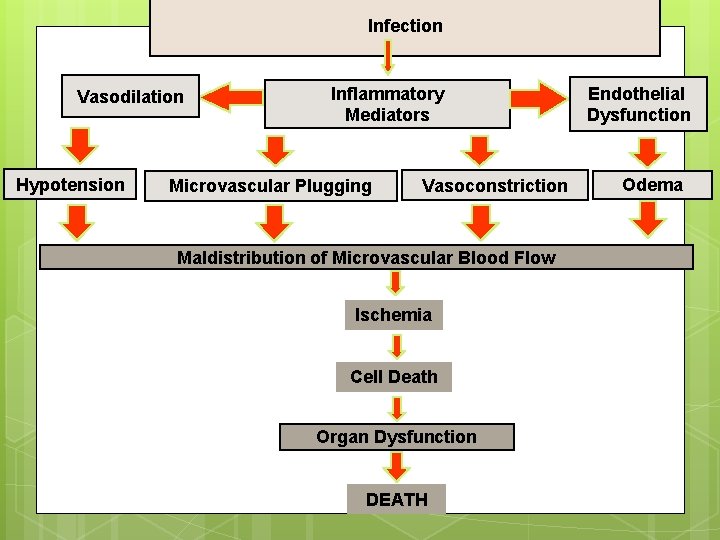
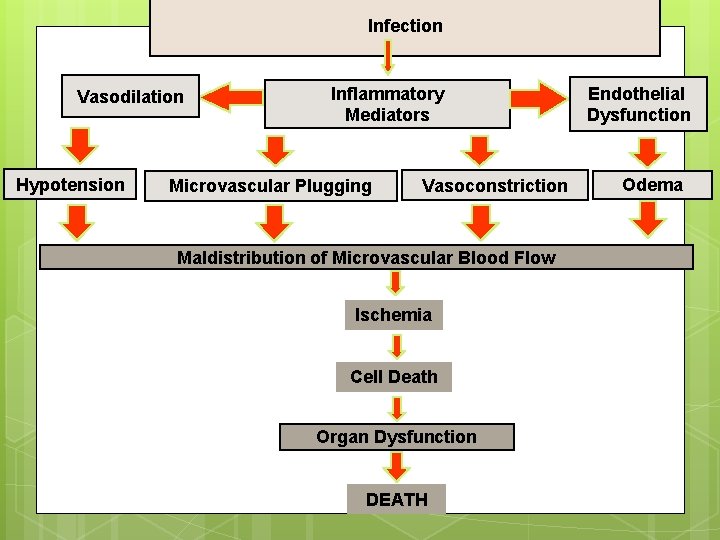
Infection Vasodilation Hypotension Inflammatory Mediators Microvascular Plugging Vasoconstriction Maldistribution of Microvascular Blood Flow Ischemia Cell Death Organ Dysfunction DEATH Endothelial Dysfunction Odema
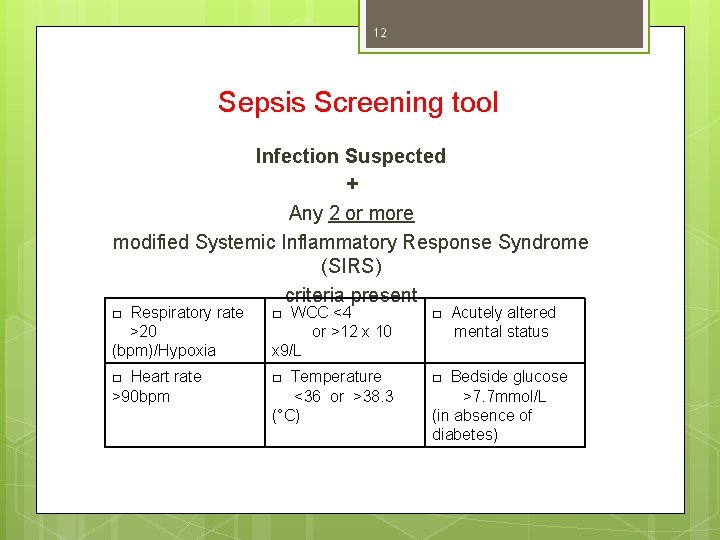
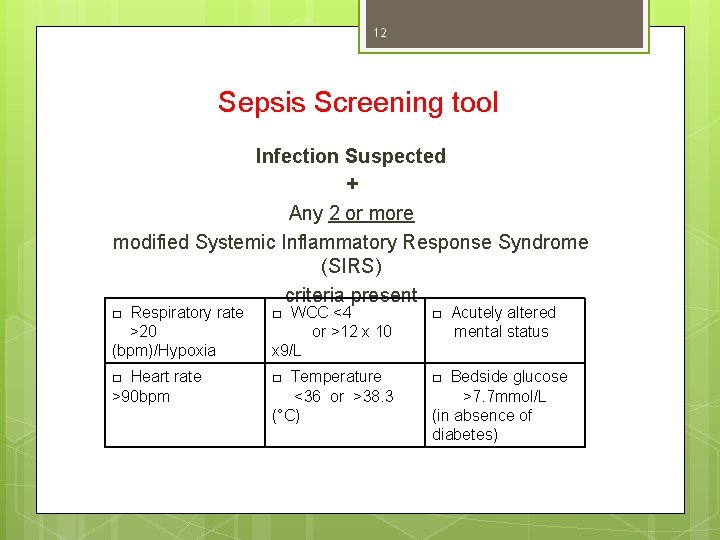
12 Sepsis Screening tool Infection Suspected + Any 2 or more modified Systemic Inflammatory Response Syndrome (SIRS) criteria present □ Respiratory rate >20 (bpm)/Hypoxia □ WCC <4 or >12 x 10 x 9/L □ Acutely altered mental status □ Heart rate >90 bpm □ Temperature <36 or >38. 3 (°C) □ Bedside glucose >7. 7 mmol/L (in absence of diabetes)
13 Presenting complaints to consider • • • Cough / flu-like symptoms UTI / flank pain Fever Pleuritic chest pain / SOB Abdominal pain Generally unwell with co-morbidities /caution with elderly patients Confusion Headache (signs of meningism) Abcess / local infections Limb problems (intra-articular infections / septic arthritis) Wounds
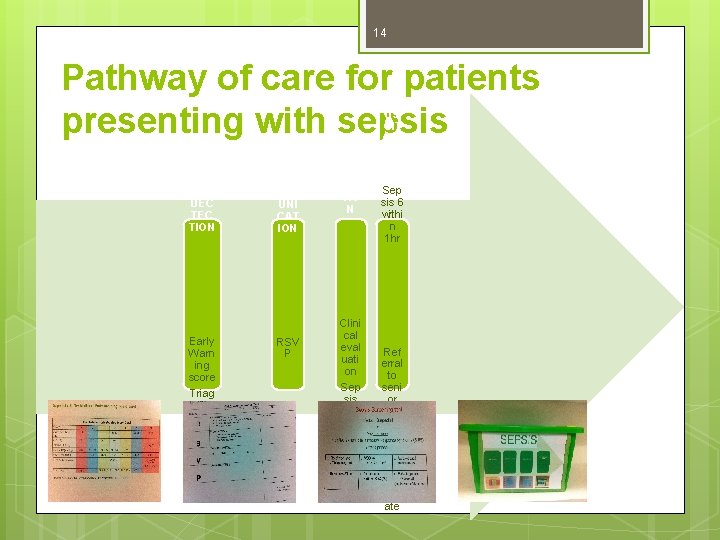
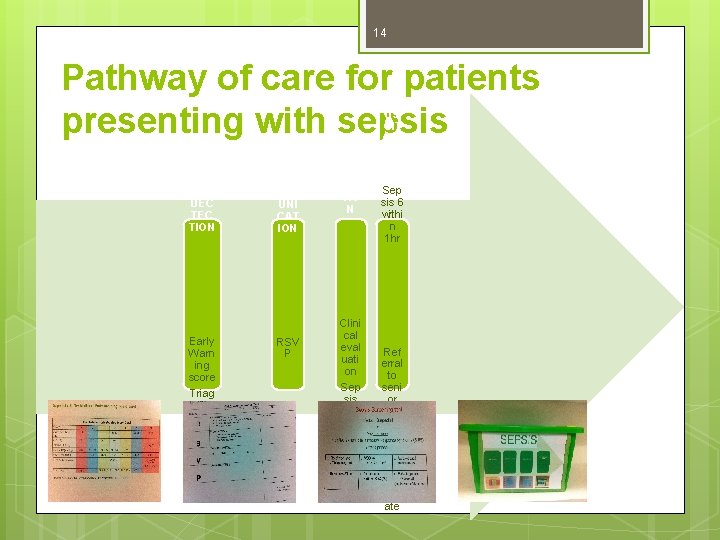
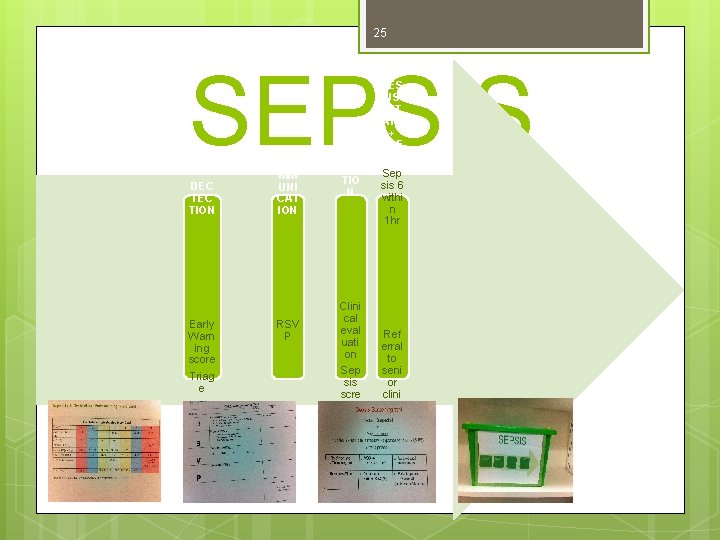
14 Pathway of care for patients presenting with sepsis DEC TION Early Warn ing score Triag e CO MM UNI CAT ION RSV P RE CO GNI TIO N Clini cal eval uati on Sep sis scre enin g tool RES US CIT ATE + REF ER Sep sis 6 withi n 1 hr Ref erral to seni or clini cian s and ICU if appr opri ate
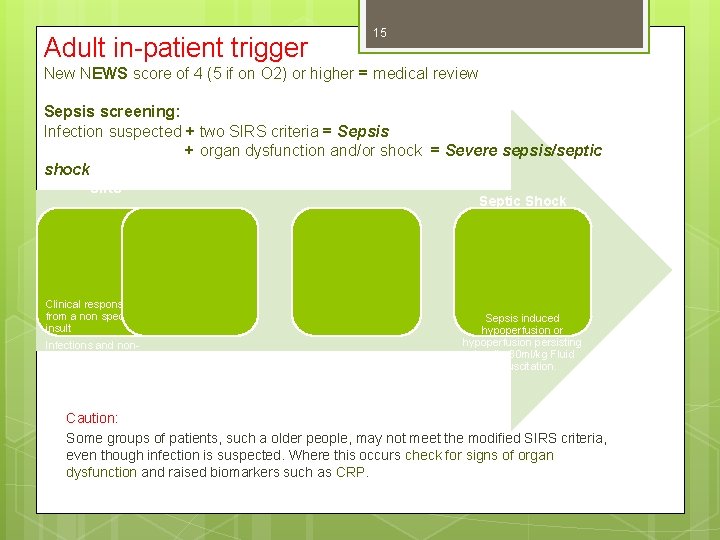
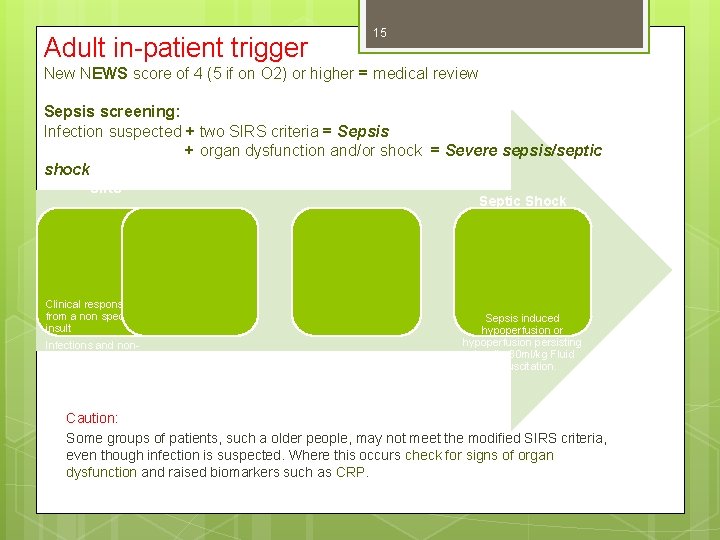
Adult in-patient trigger 15 New NEWS score of 4 (5 if on O 2) or higher = medical review Sepsis screening: Infection suspected + two SIRS criteria = Sepsis + organ dysfunction and/or shock = Severe sepsis/septic Severe Sepsis shock SIRS Septic Shock Clinical response arising from a non specific insult Infections and noninfectious causes SIRS + a presumed or confirmed infection Sepsis + sepsisinduced organ dysfunction or tissue hypoperfusion Sepsis induced hypoperfusion or hypoperfusion persisting despite 30 ml/kg Fluid Resuscitation. Caution: Some groups of patients, such a older people, may not meet the modified SIRS criteria, even though infection is suspected. Where this occurs check for signs of organ dysfunction and raised biomarkers such as CRP.
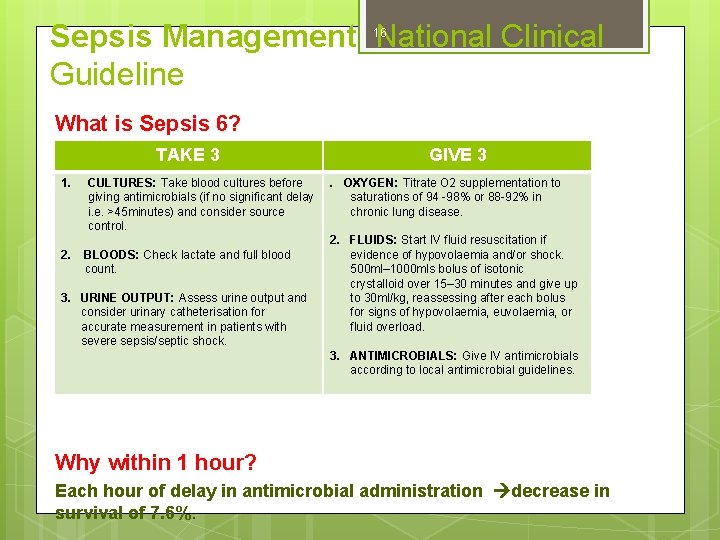
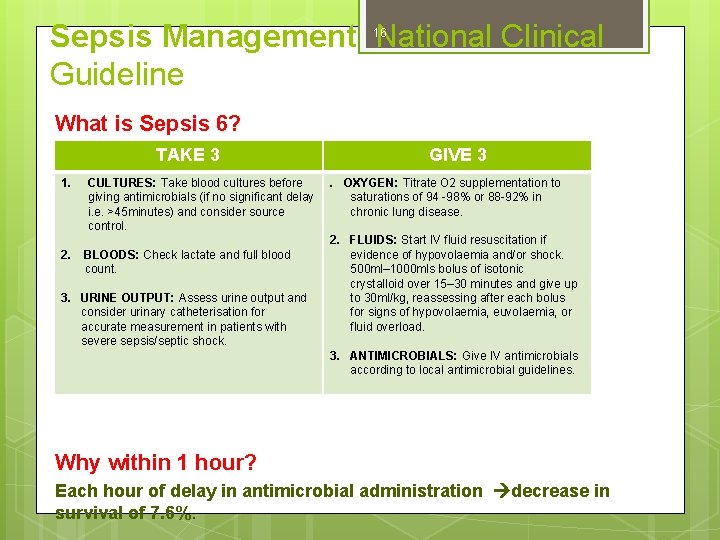
Sepsis Management National Clinical Guideline 16 What is Sepsis 6? TAKE 3 1. 2. CULTURES: Take blood cultures before giving antimicrobials (if no significant delay i. e. >45 minutes) and consider source control. BLOODS: Check lactate and full blood count. 3. URINE OUTPUT: Assess urine output and consider urinary catheterisation for accurate measurement in patients with severe sepsis/septic shock. GIVE 3. OXYGEN: Titrate O 2 supplementation to saturations of 94 -98% or 88 -92% in chronic lung disease. 2. FLUIDS: Start IV fluid resuscitation if evidence of hypovolaemia and/or shock. 500 ml– 1000 mls bolus of isotonic crystalloid over 15– 30 minutes and give up to 30 ml/kg, reassessing after each bolus for signs of hypovolaemia, euvolaemia, or fluid overload. 3. ANTIMICROBIALS: Give IV antimicrobials according to local antimicrobial guidelines. Why within 1 hour? Each hour of delay in antimicrobial administration decrease in survival of 7. 6%.
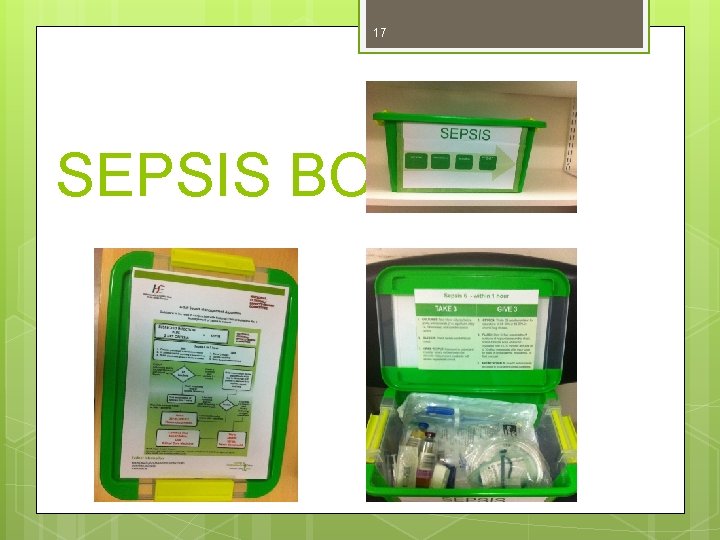
17 SEPSIS BOX
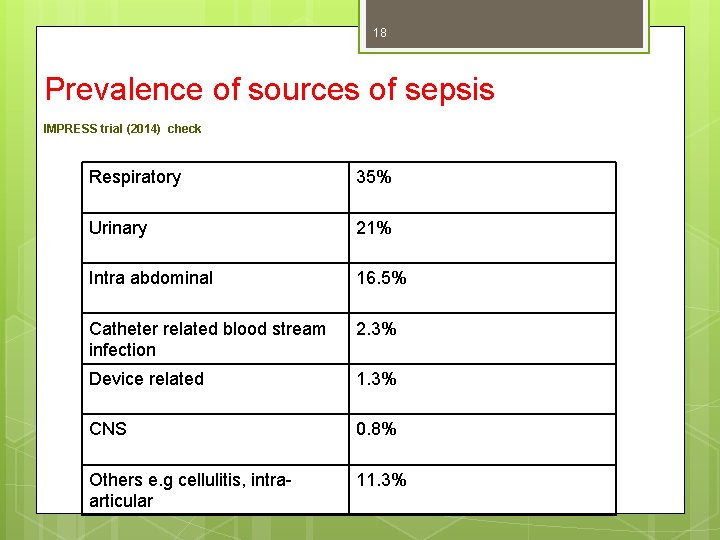
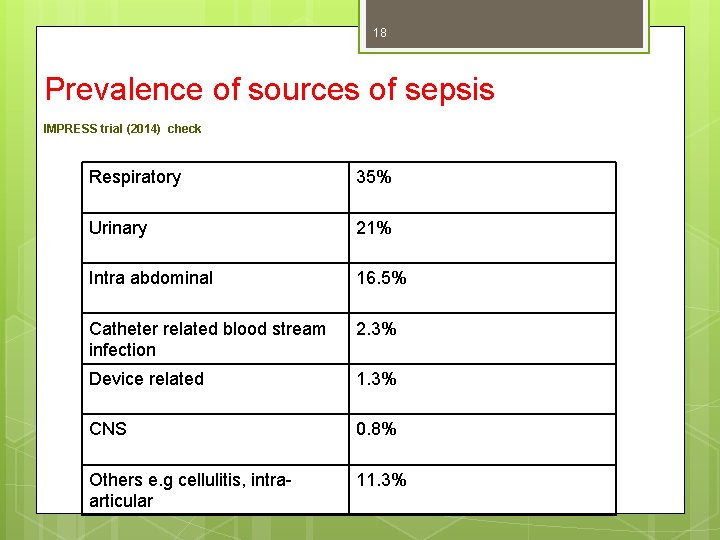
18 Prevalence of sources of sepsis IMPRESS trial (2014) check Respiratory 35% Urinary 21% Intra abdominal 16. 5% Catheter related blood stream infection 2. 3% Device related 1. 3% CNS 0. 8% Others e. g cellulitis, intraarticular 11. 3%
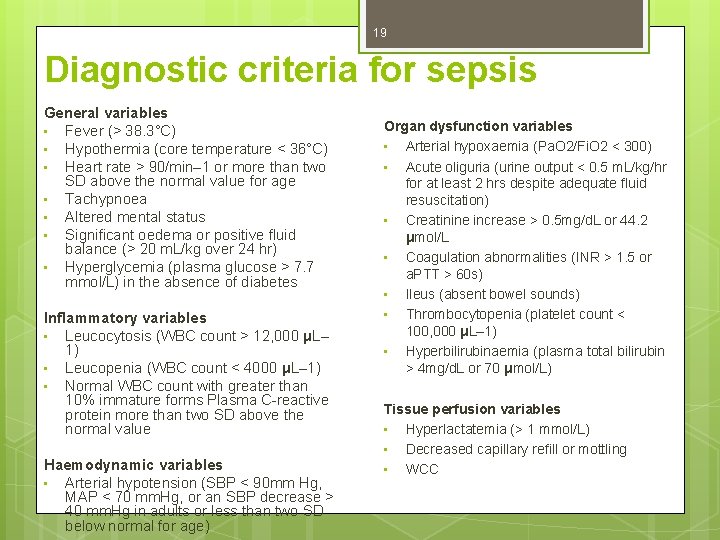
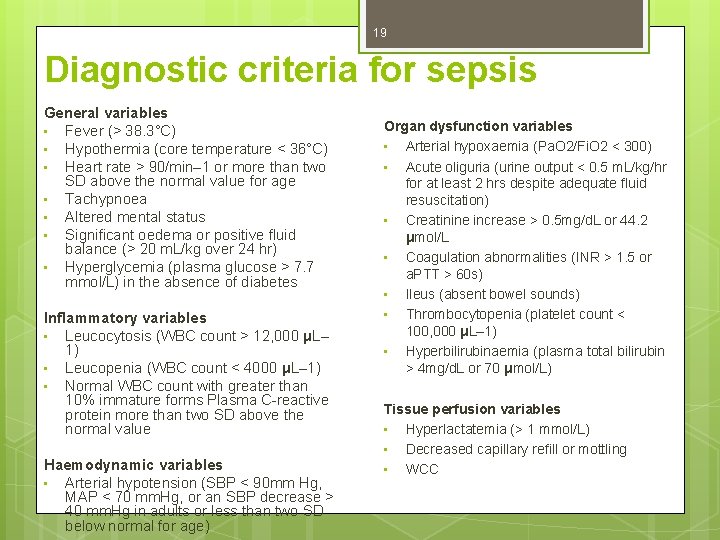
19 Diagnostic criteria for sepsis General variables • Fever (> 38. 3°C) • Hypothermia (core temperature < 36°C) • Heart rate > 90/min– 1 or more than two SD above the normal value for age • Tachypnoea • Altered mental status • Significant oedema or positive fluid balance (> 20 m. L/kg over 24 hr) • Hyperglycemia (plasma glucose > 7. 7 mmol/L) in the absence of diabetes Inflammatory variables • Leucocytosis (WBC count > 12, 000 μL– 1) • Leucopenia (WBC count < 4000 μL– 1) • Normal WBC count with greater than 10% immature forms Plasma C-reactive protein more than two SD above the normal value Haemodynamic variables • Arterial hypotension (SBP < 90 mm Hg, MAP < 70 mm. Hg, or an SBP decrease > 40 mm. Hg in adults or less than two SD below normal for age) Organ dysfunction variables • Arterial hypoxaemia (Pa. O 2/Fi. O 2 < 300) • Acute oliguria (urine output < 0. 5 m. L/kg/hr for at least 2 hrs despite adequate fluid resuscitation) • Creatinine increase > 0. 5 mg/d. L or 44. 2 μmol/L • Coagulation abnormalities (INR > 1. 5 or a. PTT > 60 s) • Ileus (absent bowel sounds) • Thrombocytopenia (platelet count < 100, 000 μL– 1) • Hyperbilirubinaemia (plasma total bilirubin > 4 mg/d. L or 70 μmol/L) Tissue perfusion variables • Hyperlactatemia (> 1 mmol/L) • Decreased capillary refill or mottling • WCC
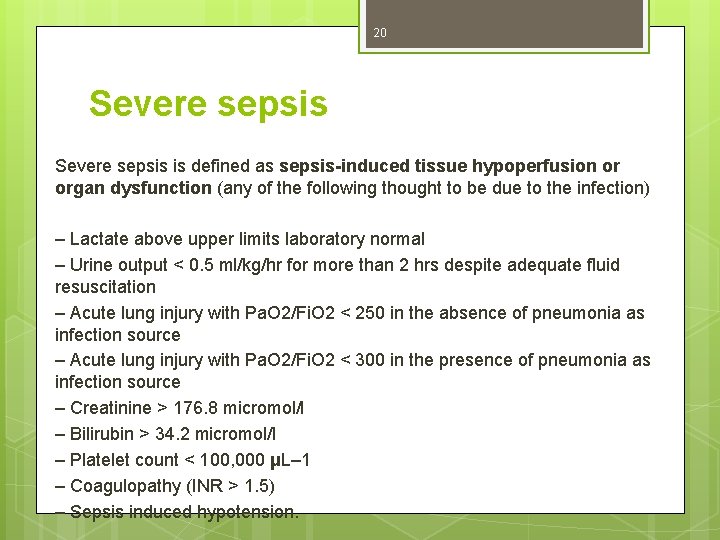
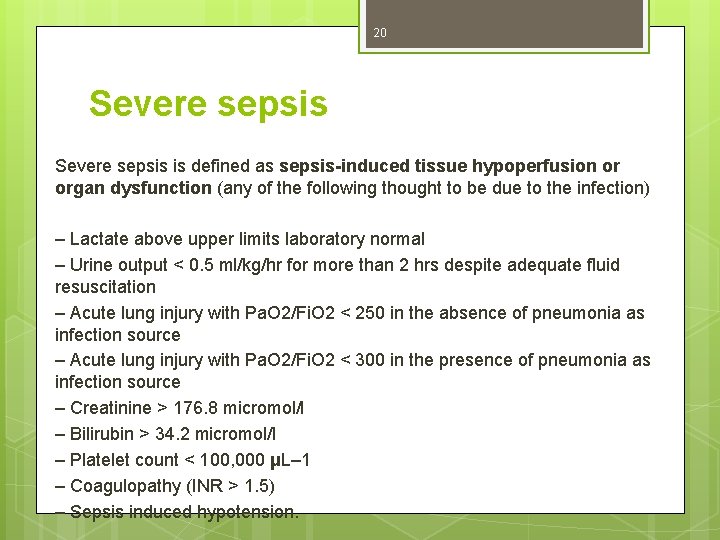
20 Severe sepsis is defined as sepsis-induced tissue hypoperfusion or organ dysfunction (any of the following thought to be due to the infection) – Lactate above upper limits laboratory normal – Urine output < 0. 5 ml/kg/hr for more than 2 hrs despite adequate fluid resuscitation – Acute lung injury with Pa. O 2/Fi. O 2 < 250 in the absence of pneumonia as infection source – Acute lung injury with Pa. O 2/Fi. O 2 < 300 in the presence of pneumonia as infection source – Creatinine > 176. 8 micromol/l – Bilirubin > 34. 2 micromol/l – Platelet count < 100, 000 μL– 1 – Coagulopathy (INR > 1. 5) – Sepsis induced hypotension.
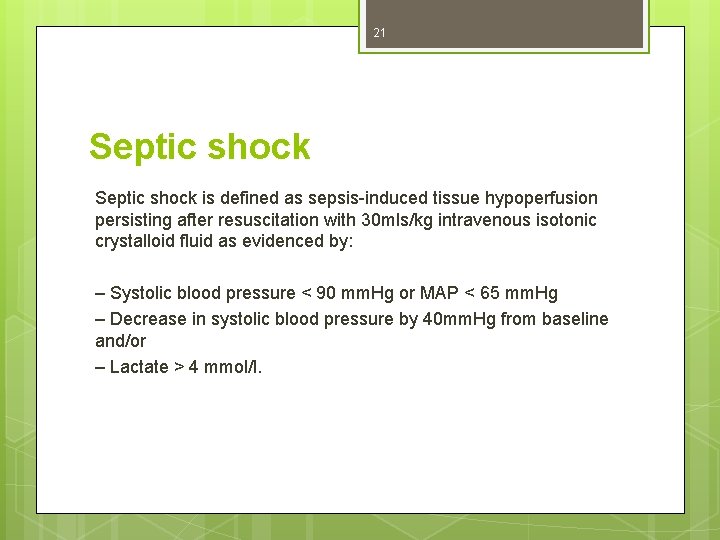
21 Septic shock is defined as sepsis-induced tissue hypoperfusion persisting after resuscitation with 30 mls/kg intravenous isotonic crystalloid fluid as evidenced by: – Systolic blood pressure < 90 mm. Hg or MAP < 65 mm. Hg – Decrease in systolic blood pressure by 40 mm. Hg from baseline and/or – Lactate > 4 mmol/l.
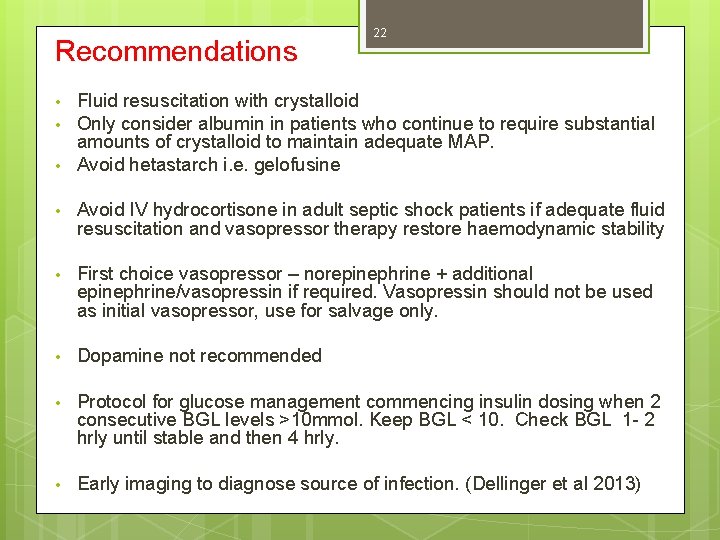
Recommendations • • • 22 Fluid resuscitation with crystalloid Only consider albumin in patients who continue to require substantial amounts of crystalloid to maintain adequate MAP. Avoid hetastarch i. e. gelofusine • Avoid IV hydrocortisone in adult septic shock patients if adequate fluid resuscitation and vasopressor therapy restore haemodynamic stability • First choice vasopressor – norepinephrine + additional epinephrine/vasopressin if required. Vasopressin should not be used as initial vasopressor, use for salvage only. • Dopamine not recommended • Protocol for glucose management commencing insulin dosing when 2 consecutive BGL levels >10 mmol. Keep BGL < 10. Check BGL 1 - 2 hrly until stable and then 4 hrly. • Early imaging to diagnose source of infection. (Dellinger et al 2013)
23 References Dellinger R. P. et al. (2013) Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock: 2012. Critical Care Medicine 41 (2), 580 -621. Kumar A. et al (2006) Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Critical Care Medicine 34, 1589 -1596. National Clinical Effectiveness Committee, Health Service Executive (2014) Sepsis Management: National Clinical Guideline No. 6 www. hse. ie/eng/about/Who/clinical. natclinprog/sepsis%20 management. pd f Australian Modification of ICD-10 incorporating the Australian Classification of Health Interventions and the Australian Coding
24 Thank you Any Questions?
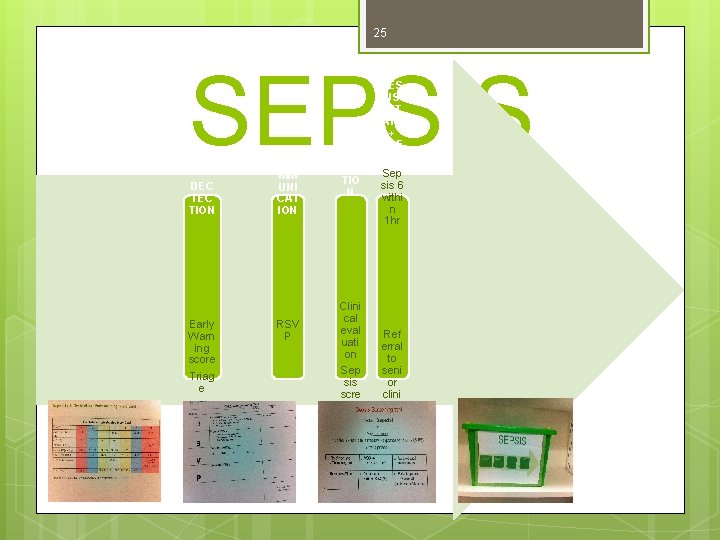
25 SEPSIS DEC TION Early Warn ing score Triag e CO MM UNI CAT ION RSV P RE CO GNI TIO N Clini cal eval uati on Sep sis scre enin g tool RES US CIT ATE + REF ER Sep sis 6 withi n 1 hr Ref erral to seni or clini cian s and ICU if appr opri ate