Sepsis Care and the New Core Measures Daniel
- Slides: 60
Sepsis Care and the New Core Measures Daniel S. Hagg, MD January 15, 2016
Outline �What is sepsis? �A brief history of sepsis care �How should we take care of septic patients now? �Core measures �What strategies work? �Advice for small hospitals
Sepsis IS Sepsis is NOT The inflammatory response to infection Bacteria in the Blood
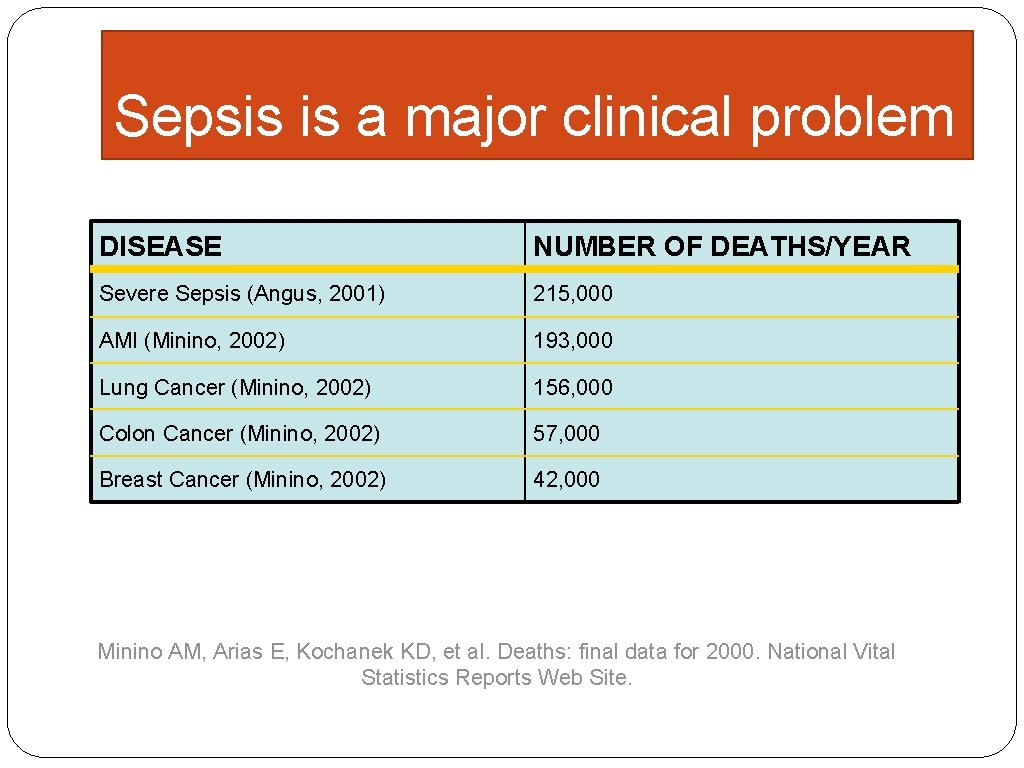
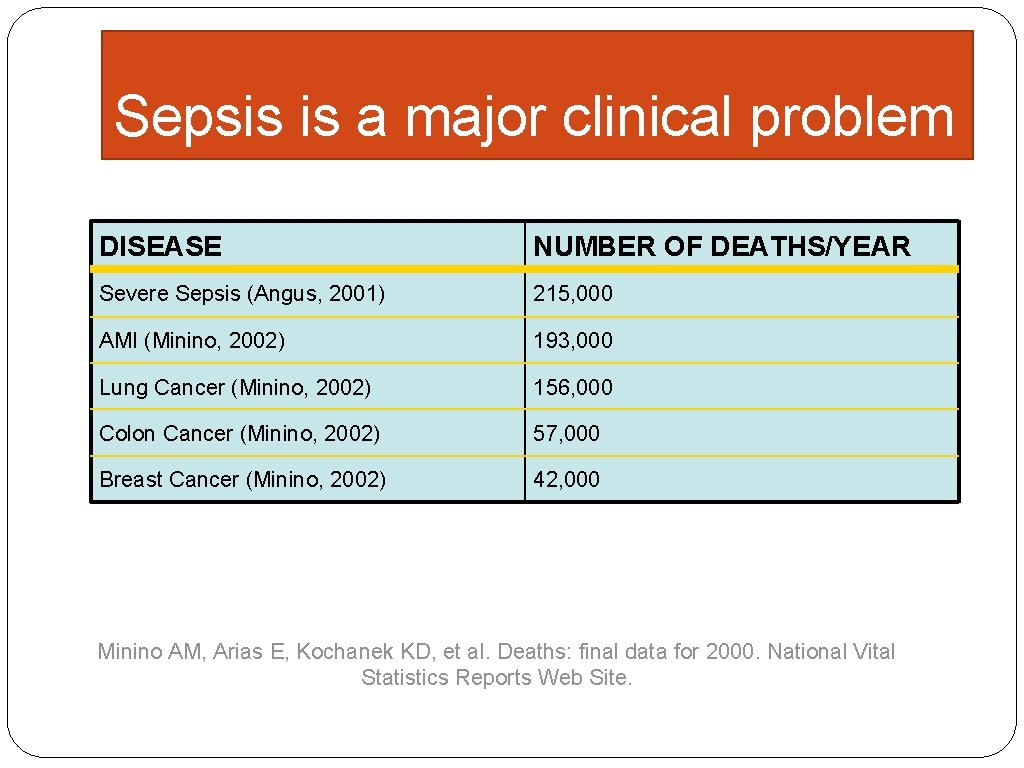
Sepsis is a major clinical problem DISEASE NUMBER OF DEATHS/YEAR Severe Sepsis (Angus, 2001) 215, 000 AMI (Minino, 2002) 193, 000 Lung Cancer (Minino, 2002) 156, 000 Colon Cancer (Minino, 2002) 57, 000 Breast Cancer (Minino, 2002) 42, 000 Minino AM, Arias E, Kochanek KD, et al. Deaths: final data for 2000. National Vital Statistics Reports Web Site.
�A patient presenting with severe sepsis has a mortality risk � 6 -10 times greater than AMI � 4 -5 times greater than stroke
Diagnosis � Terms to foster common dialogue
Diagnosis � Sepsis = Systemic Inflammatory Response Syndrome (SIRS) plus suspected infection � Sepsis ≠ hypotension
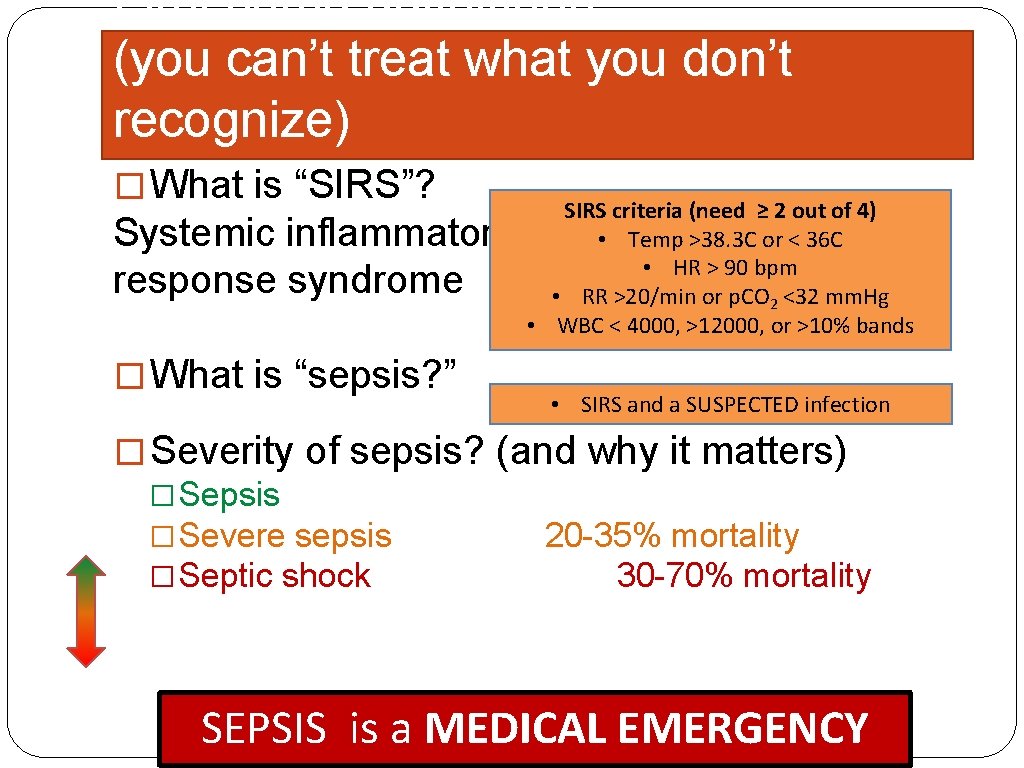
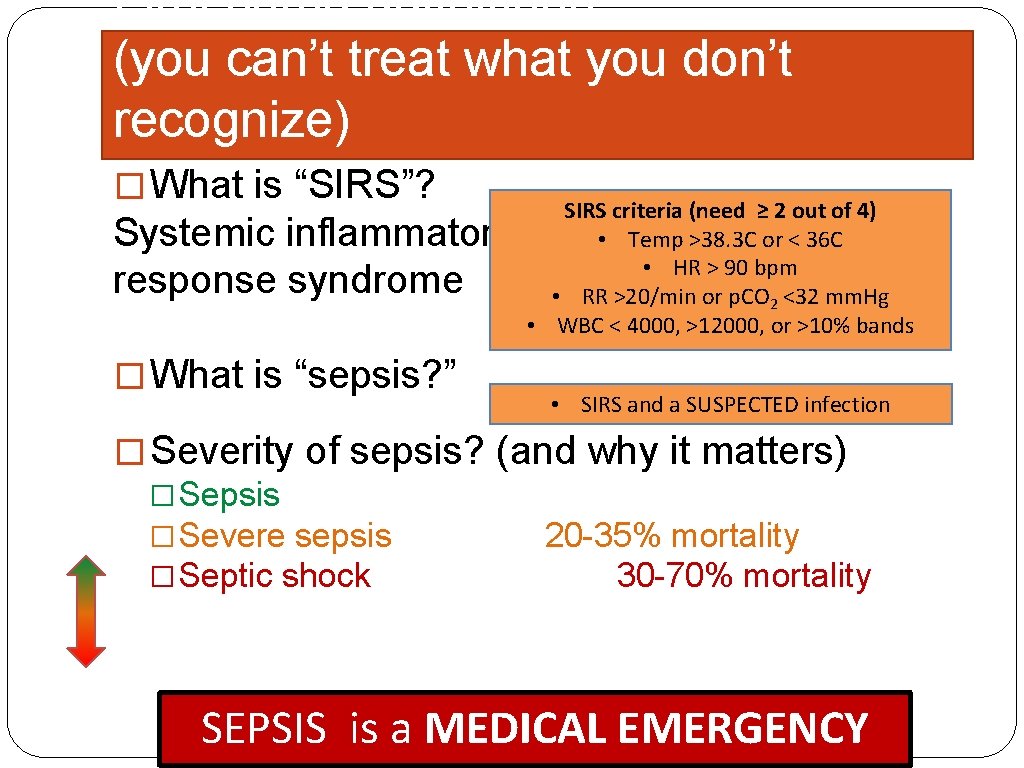
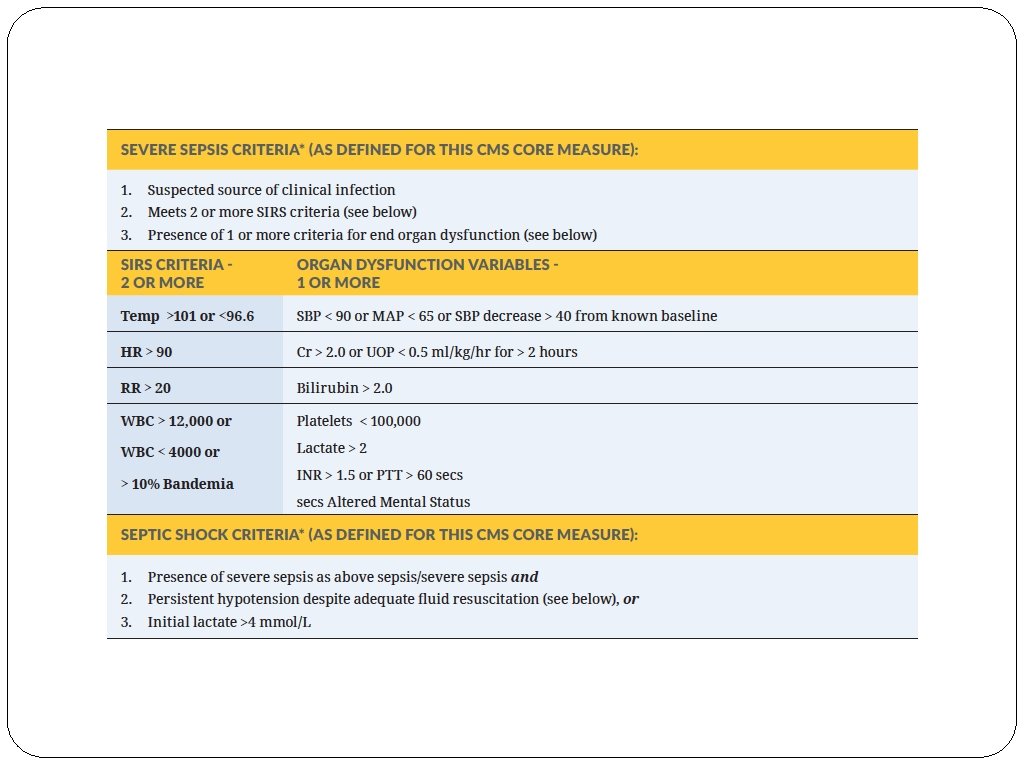
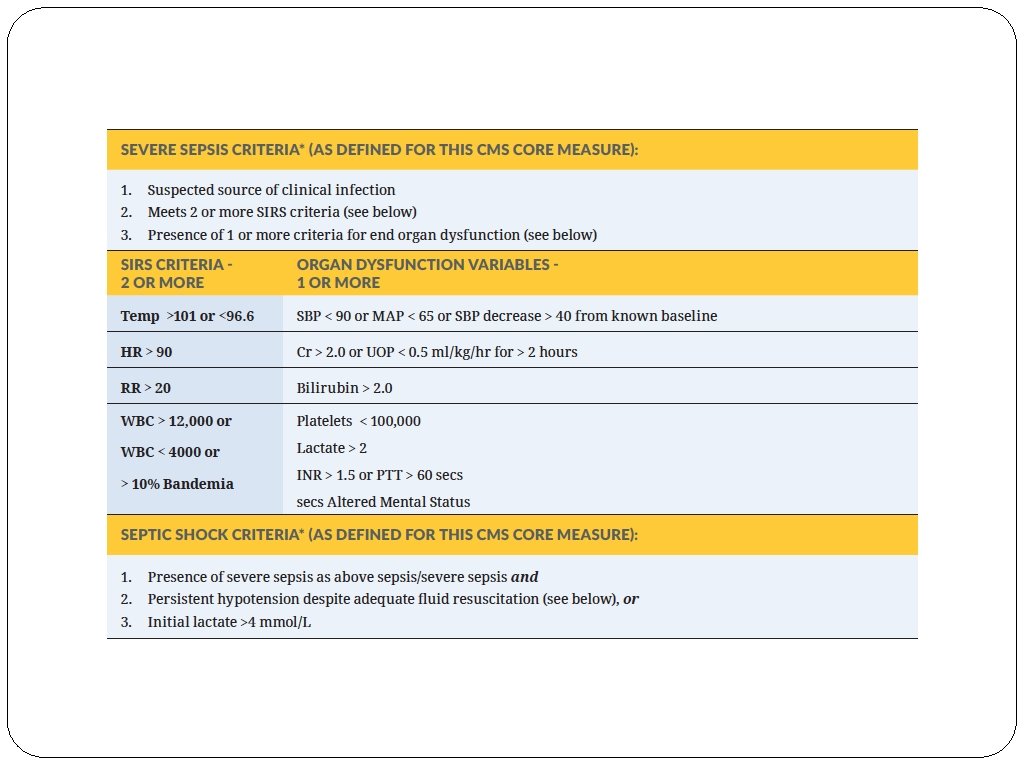
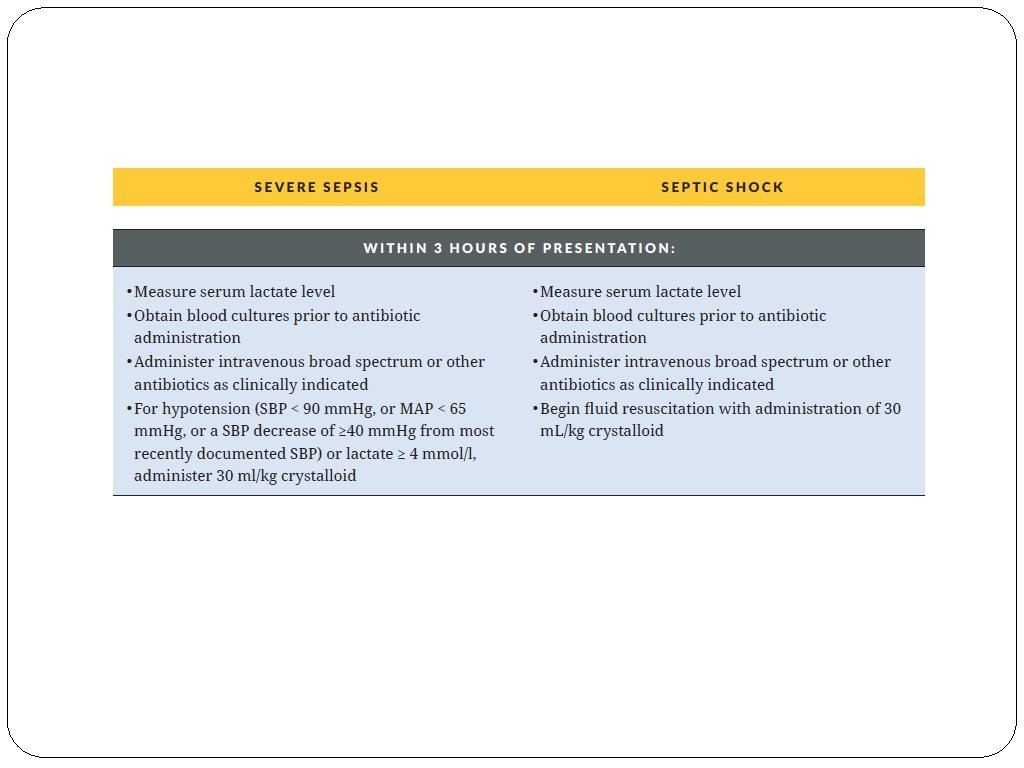
First some definitions (you can’t treat what you don’t recognize) � What is “SIRS”? Systemic inflammatory response syndrome � What is “sepsis? ” SIRS criteria (need ≥ 2 out of 4) • Temp >38. 3 C or < 36 C • HR > 90 bpm • RR >20/min or p. CO 2 <32 mm. Hg • WBC < 4000, >12000, or >10% bands • SIRS and a SUSPECTED infection � Severity of sepsis? (and why it matters) � Sepsis � Severe sepsis 20 -35% mortality � Septic shock 30 -70% mortality SEPSIS is a MEDICAL EMERGENCY
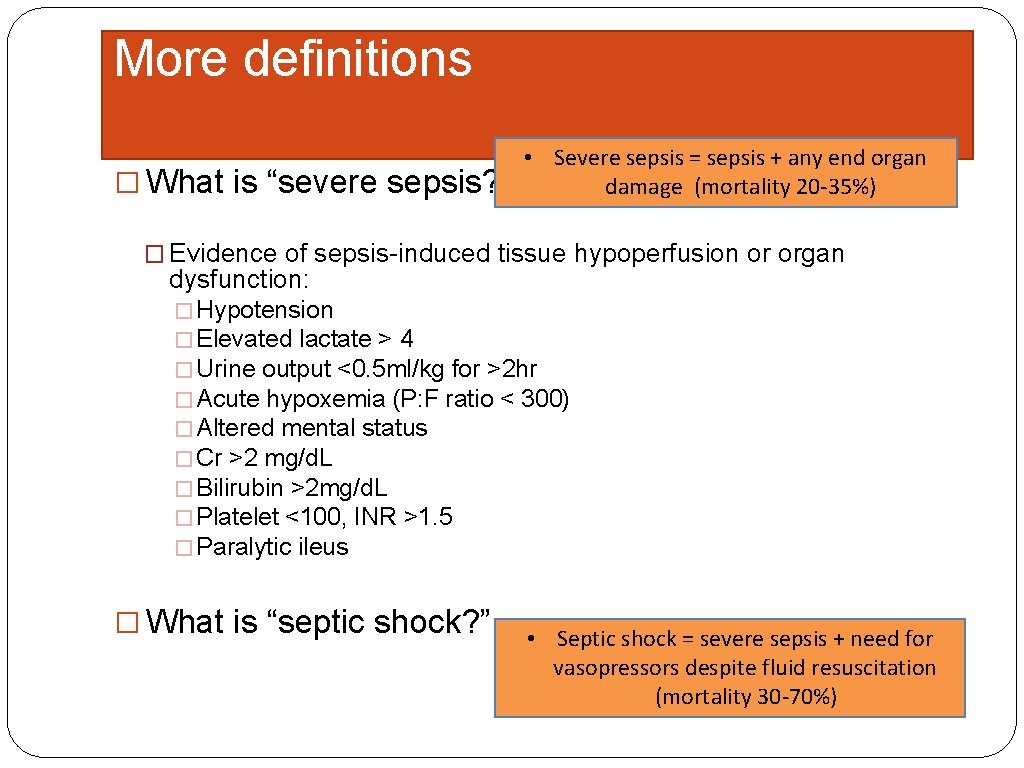
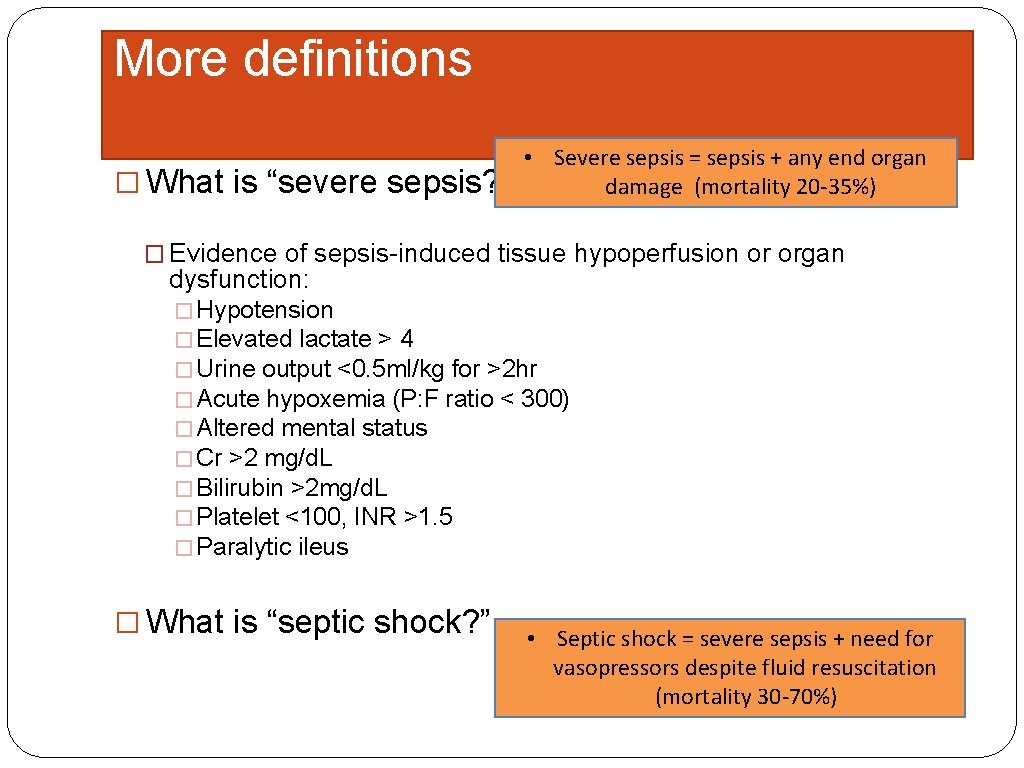
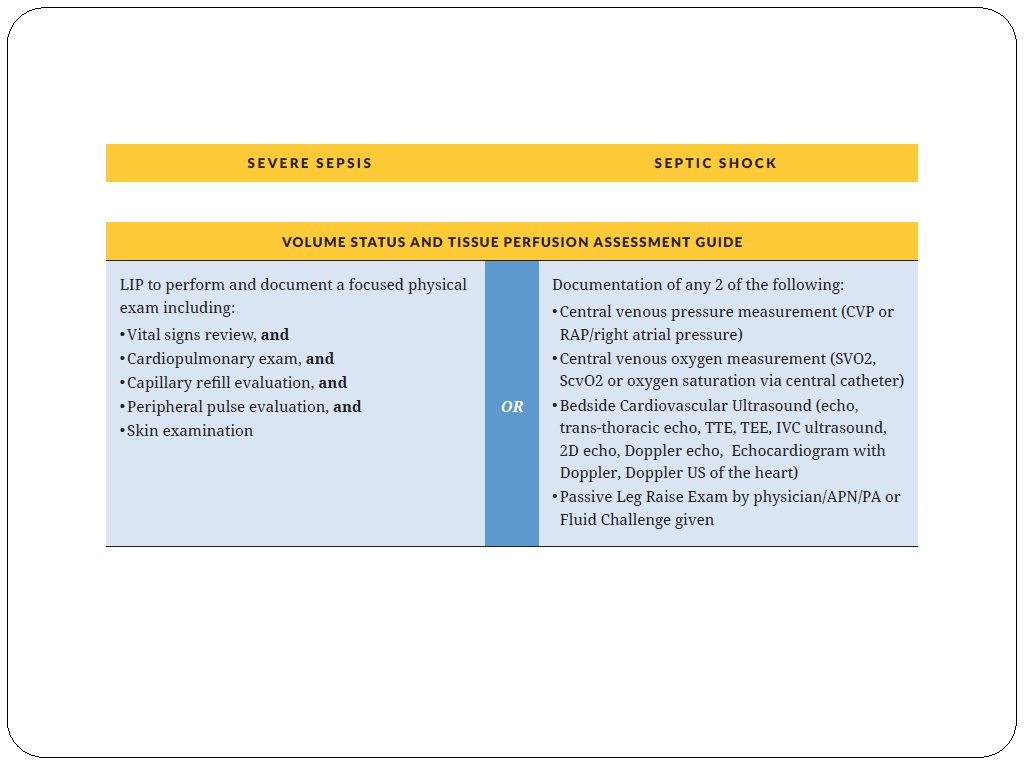
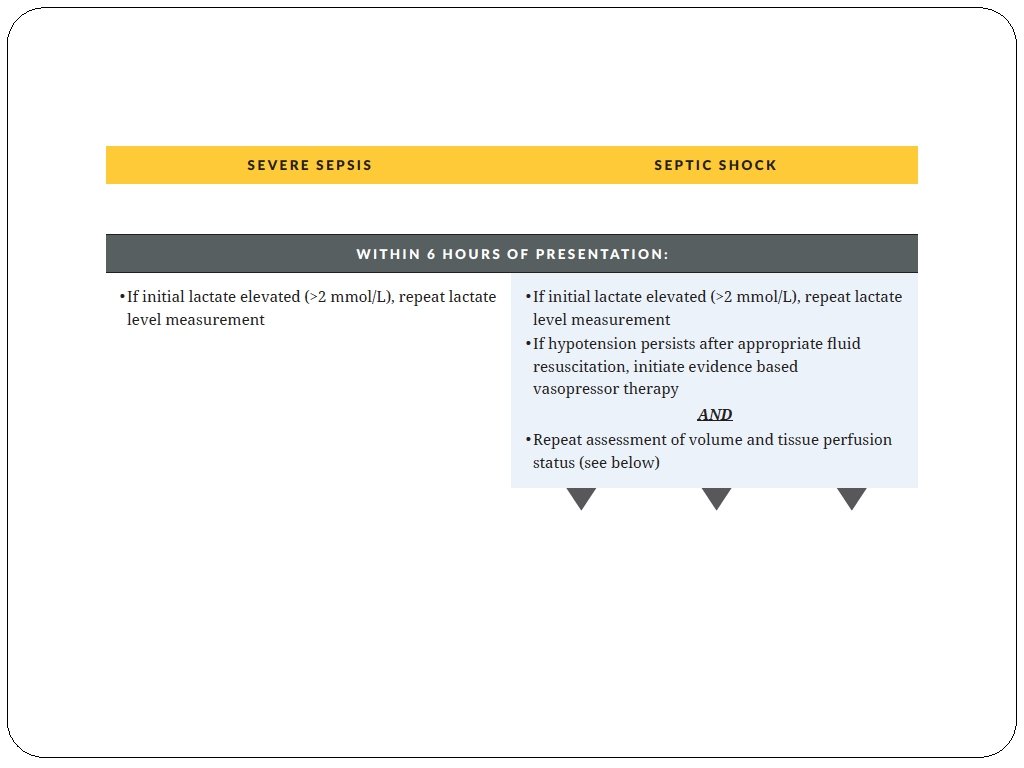
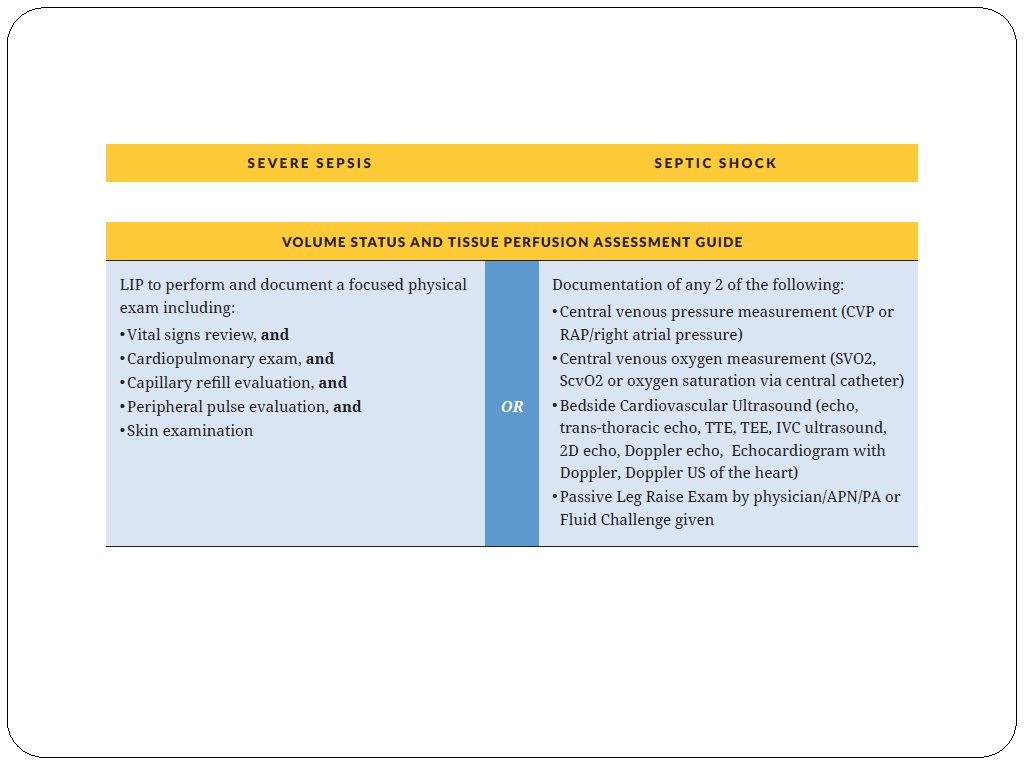
More definitions � What is “severe sepsis? ” • Severe sepsis = sepsis + any end organ damage (mortality 20 -35%) � Evidence of sepsis-induced tissue hypoperfusion or organ dysfunction: � Hypotension � Elevated lactate > 4 � Urine output <0. 5 ml/kg for >2 hr � Acute hypoxemia (P: F ratio < 300) � Altered mental status � Cr >2 mg/d. L � Bilirubin >2 mg/d. L � Platelet <100, INR >1. 5 � Paralytic ileus � What is “septic shock? ” • Septic shock = severe sepsis + need for vasopressors despite fluid resuscitation (mortality 30 -70%)
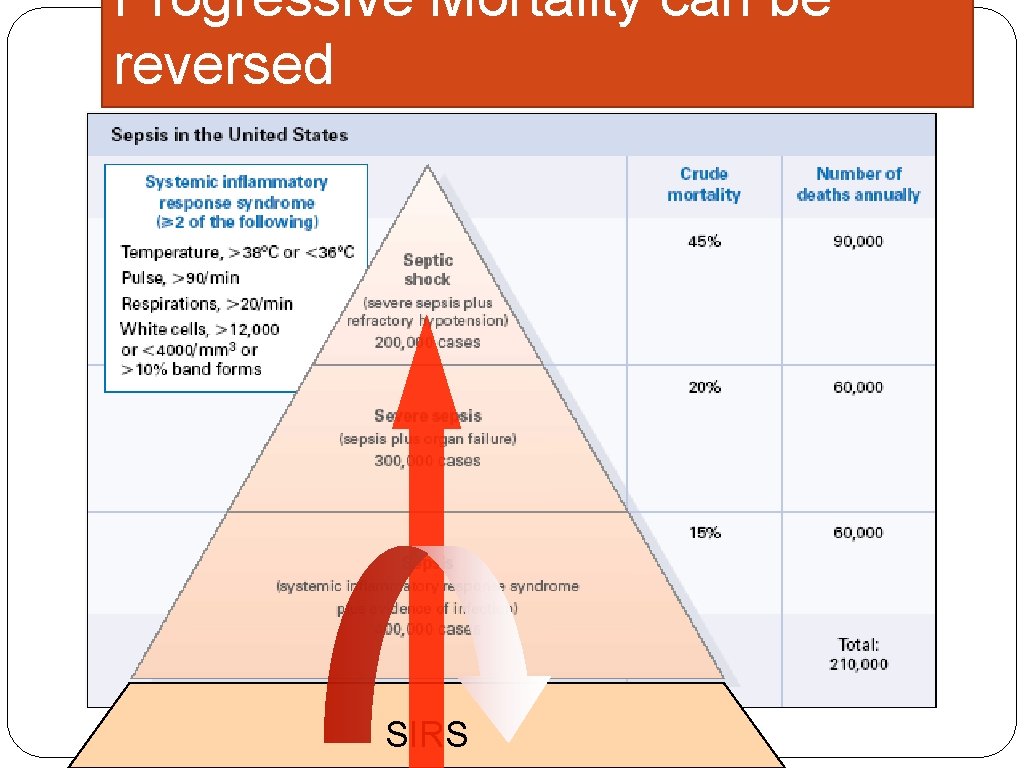
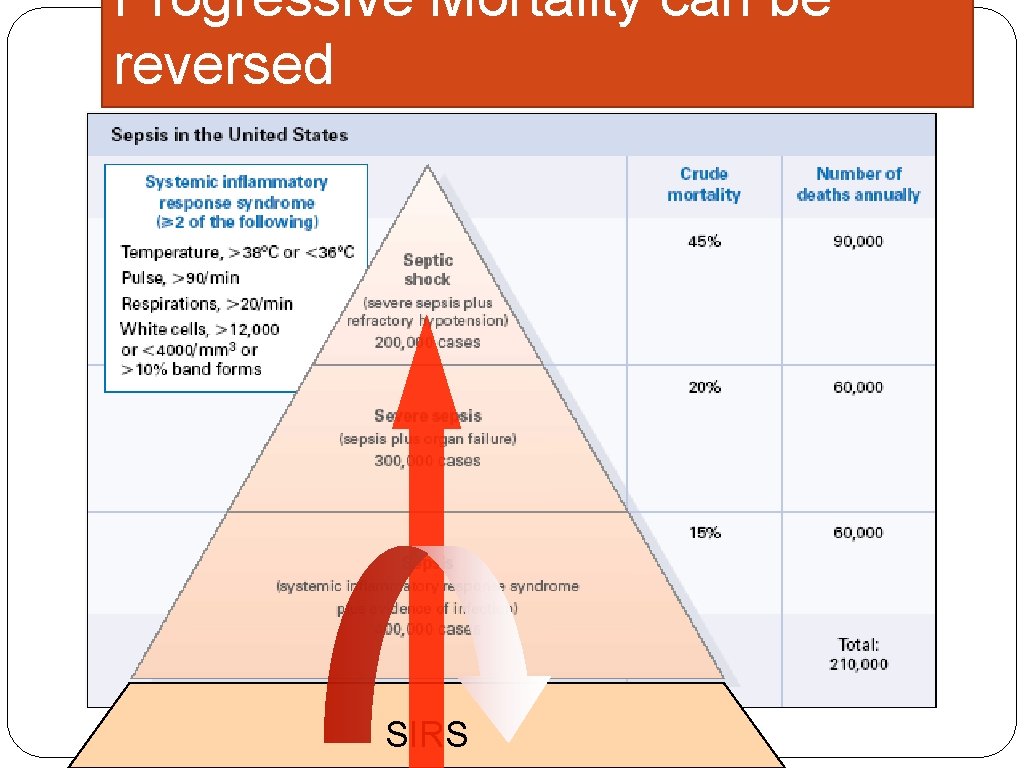
Progressive Mortality can be reversed SIRS
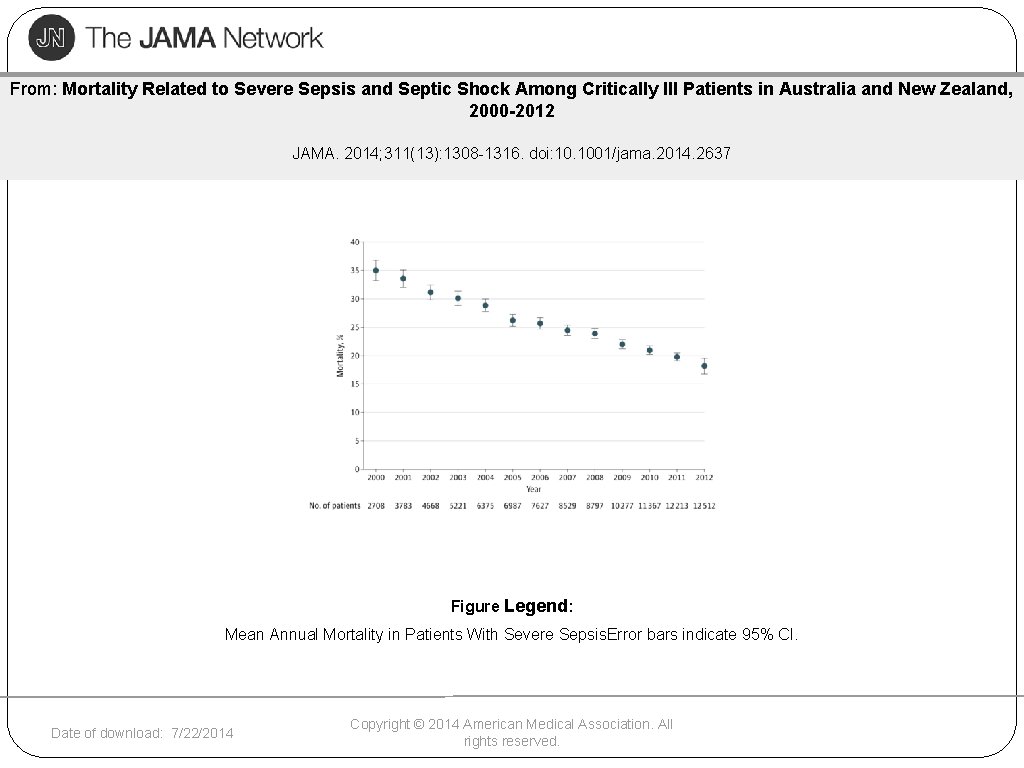
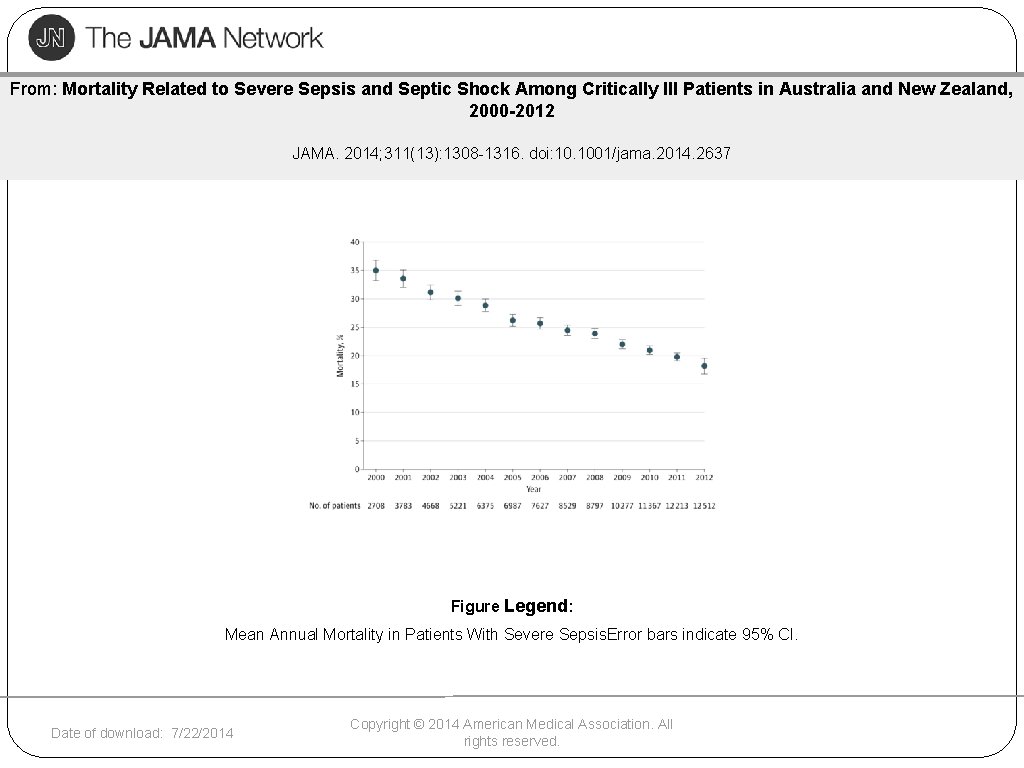
From: Mortality Related to Severe Sepsis and Septic Shock Among Critically Ill Patients in Australia and New Zealand, 2000 -2012 JAMA. 2014; 311(13): 1308 -1316. doi: 10. 1001/jama. 2014. 2637 Figure Legend: Mean Annual Mortality in Patients With Severe Sepsis. Error bars indicate 95% CI. Date of download: 7/22/2014 Copyright © 2014 American Medical Association. All rights reserved.
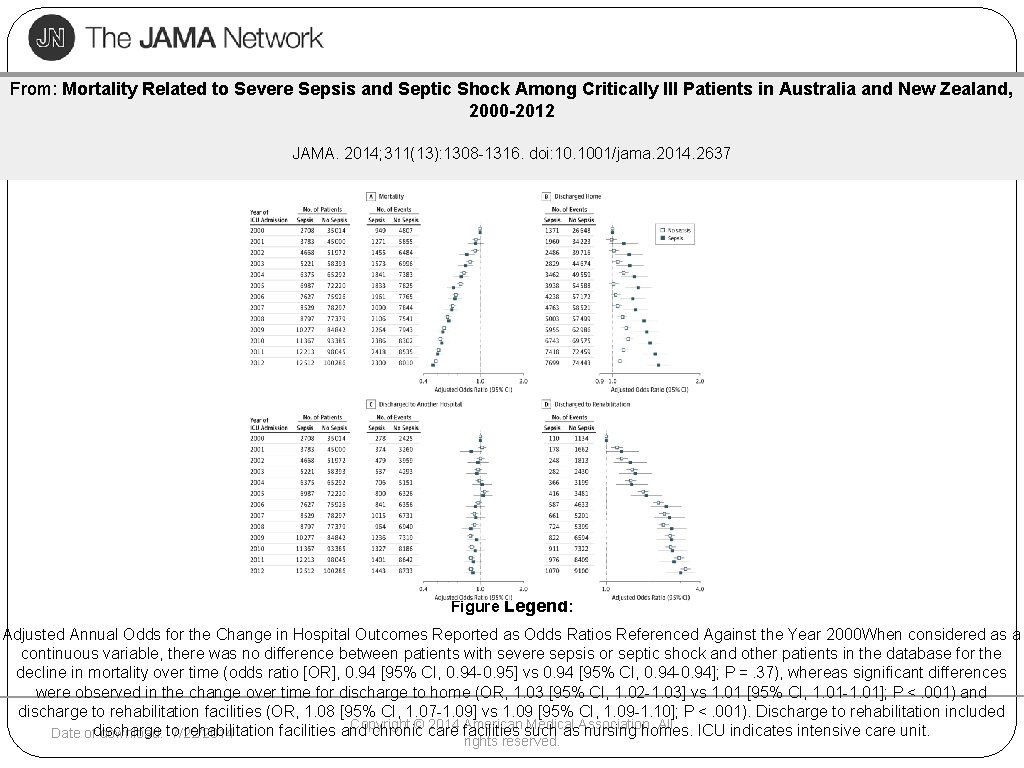
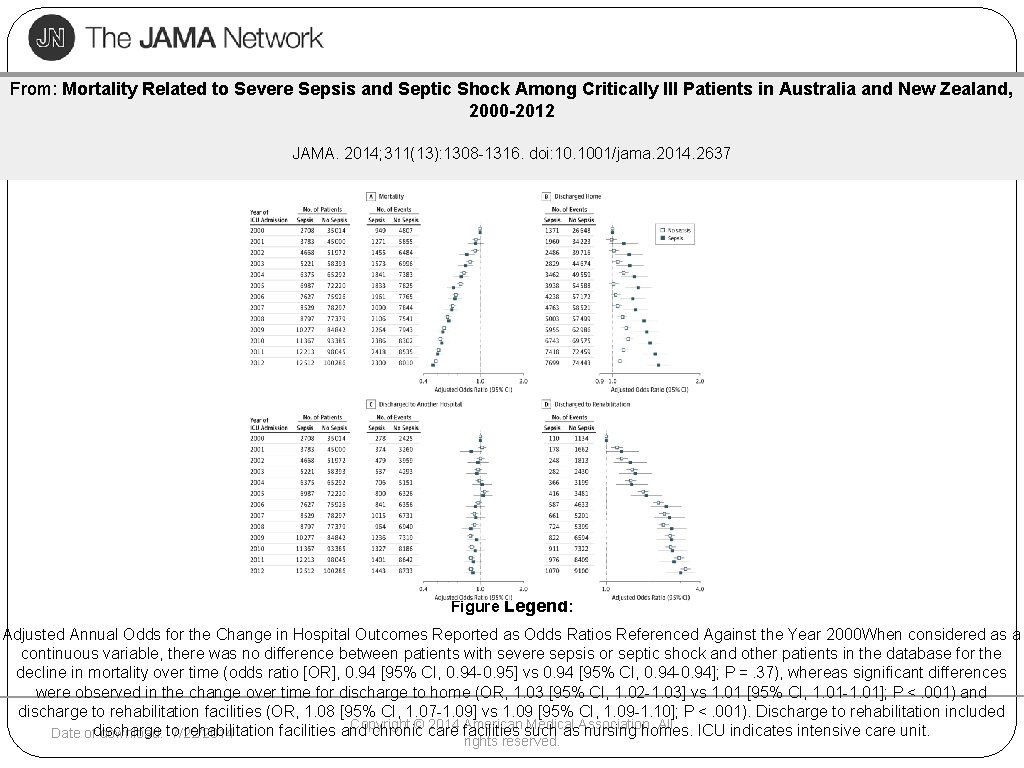
From: Mortality Related to Severe Sepsis and Septic Shock Among Critically Ill Patients in Australia and New Zealand, 2000 -2012 JAMA. 2014; 311(13): 1308 -1316. doi: 10. 1001/jama. 2014. 2637 Figure Legend: Adjusted Annual Odds for the Change in Hospital Outcomes Reported as Odds Ratios Referenced Against the Year 2000 When considered as a continuous variable, there was no difference between patients with severe sepsis or septic shock and other patients in the database for the decline in mortality over time (odds ratio [OR], 0. 94 [95% CI, 0. 94 -0. 95] vs 0. 94 [95% CI, 0. 94 -0. 94]; P =. 37), whereas significant differences were observed in the change over time for discharge to home (OR, 1. 03 [95% CI, 1. 02 -1. 03] vs 1. 01 [95% CI, 1. 01 -1. 01]; P <. 001) and discharge to rehabilitation facilities (OR, 1. 08 [95% CI, 1. 07 -1. 09] vs 1. 09 [95% CI, 1. 09 -1. 10]; P <. 001). Discharge to rehabilitation included Copyright © care 2014 facilities American such Medical All rehabilitation facilities and chronic as. Association. nursing homes. ICU indicates intensive care unit. Date ofdischarge download: to 7/22/2014 rights reserved.
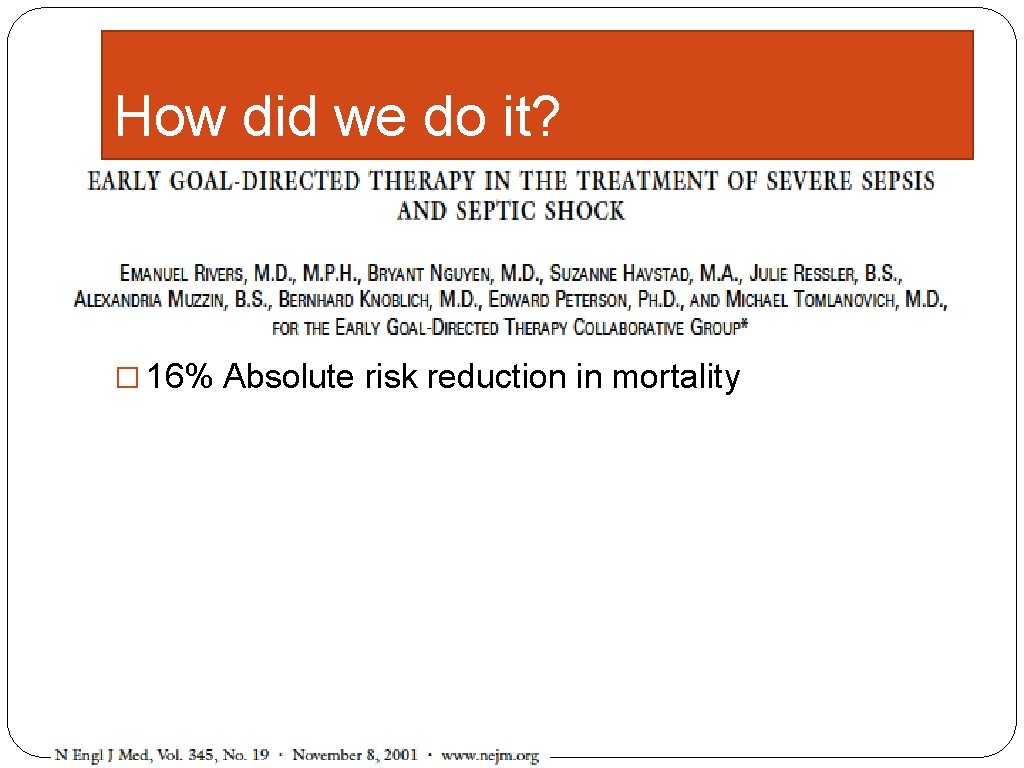
How did we do it? � Randomized trial of usual care v. early goal directed therapy � 263 patients � 16% Absolute risk reduction in mortality
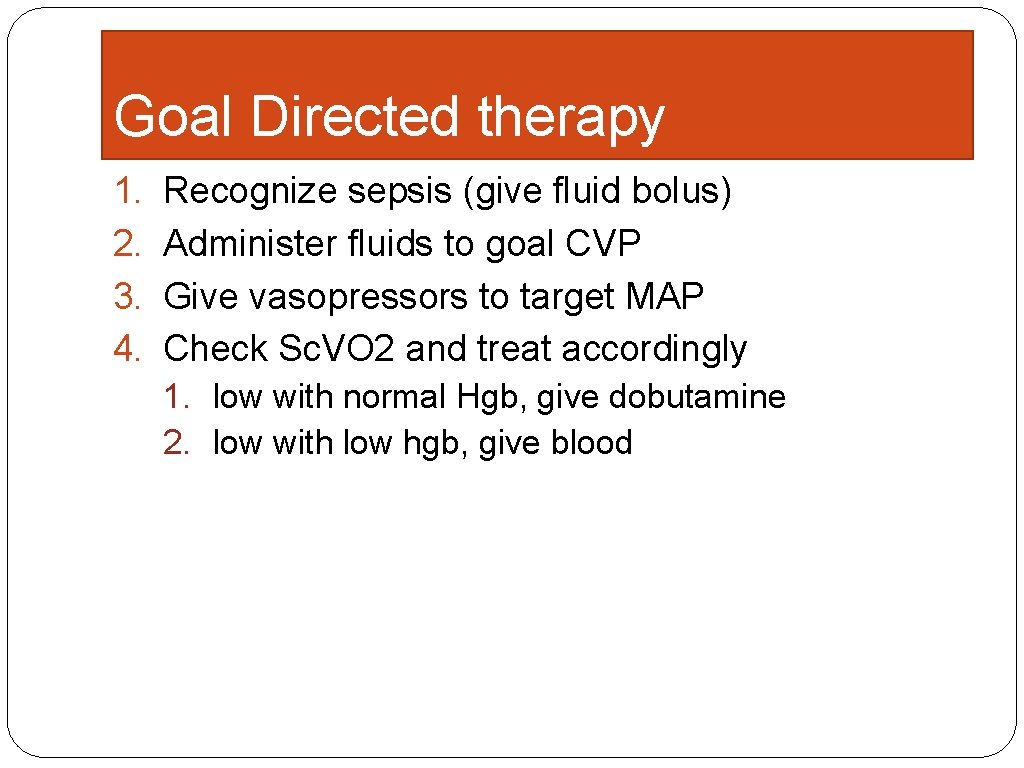
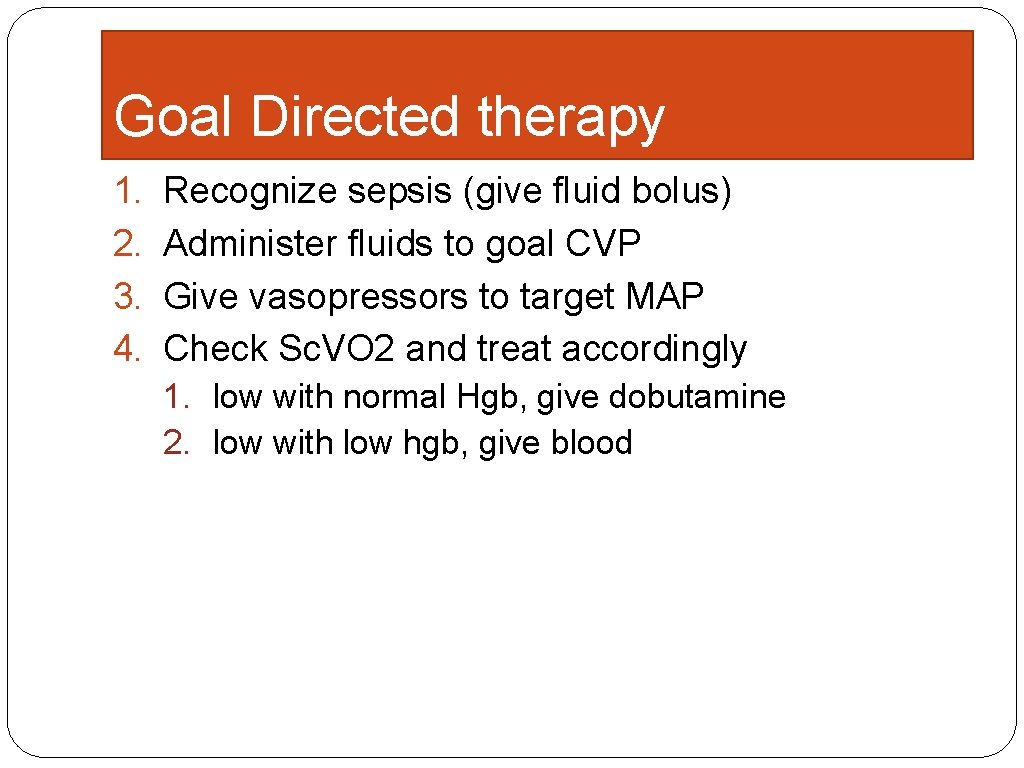
Goal Directed therapy 1. 2. 3. 4. Recognize sepsis (give fluid bolus) Administer fluids to goal CVP Give vasopressors to target MAP Check Sc. VO 2 and treat accordingly 1. low with normal Hgb, give dobutamine 2. low with low hgb, give blood
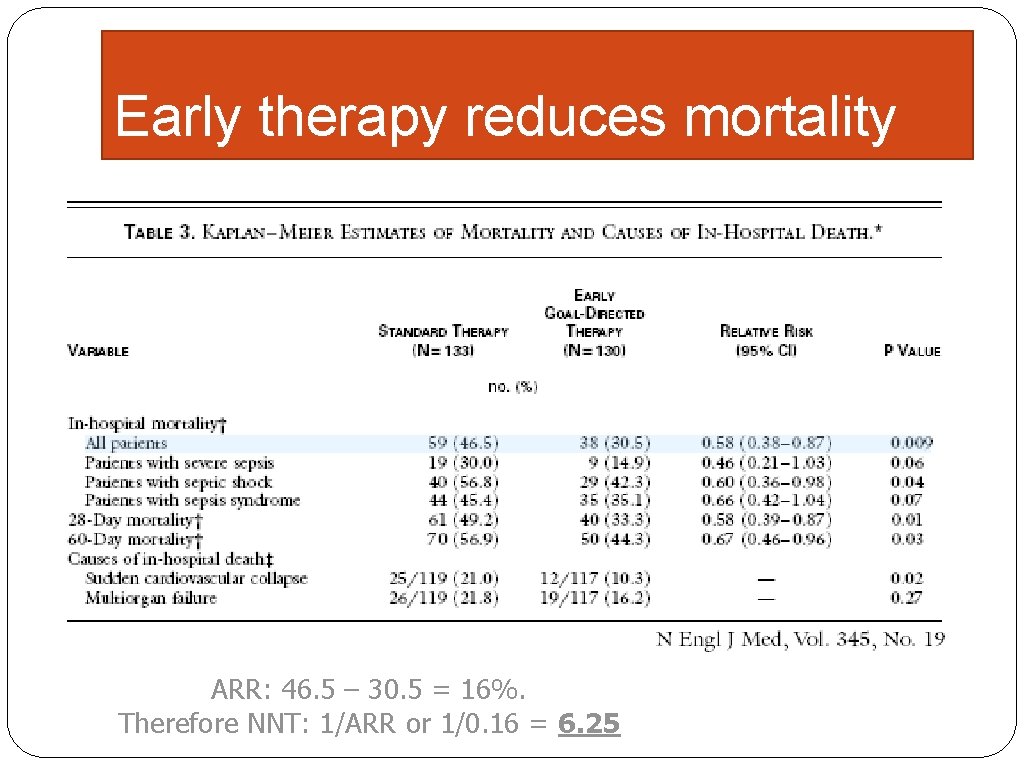
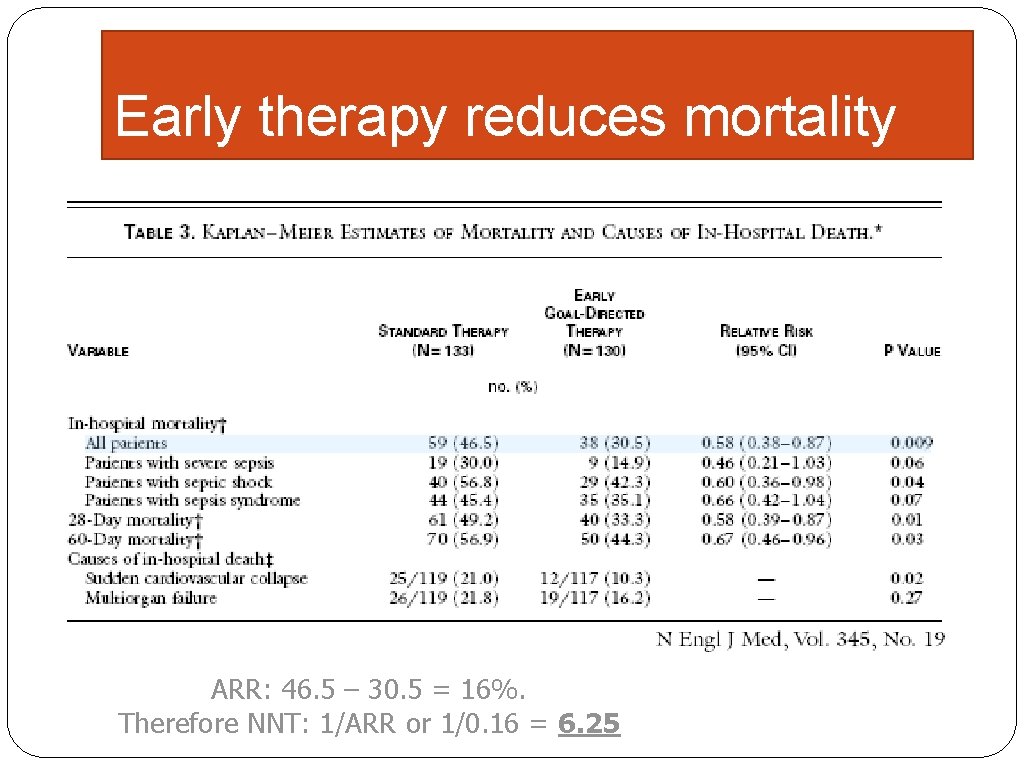
Early therapy reduces mortality ARR: 46. 5 – 30. 5 = 16%. Therefore NNT: 1/ARR or 1/0. 16 = 6. 25
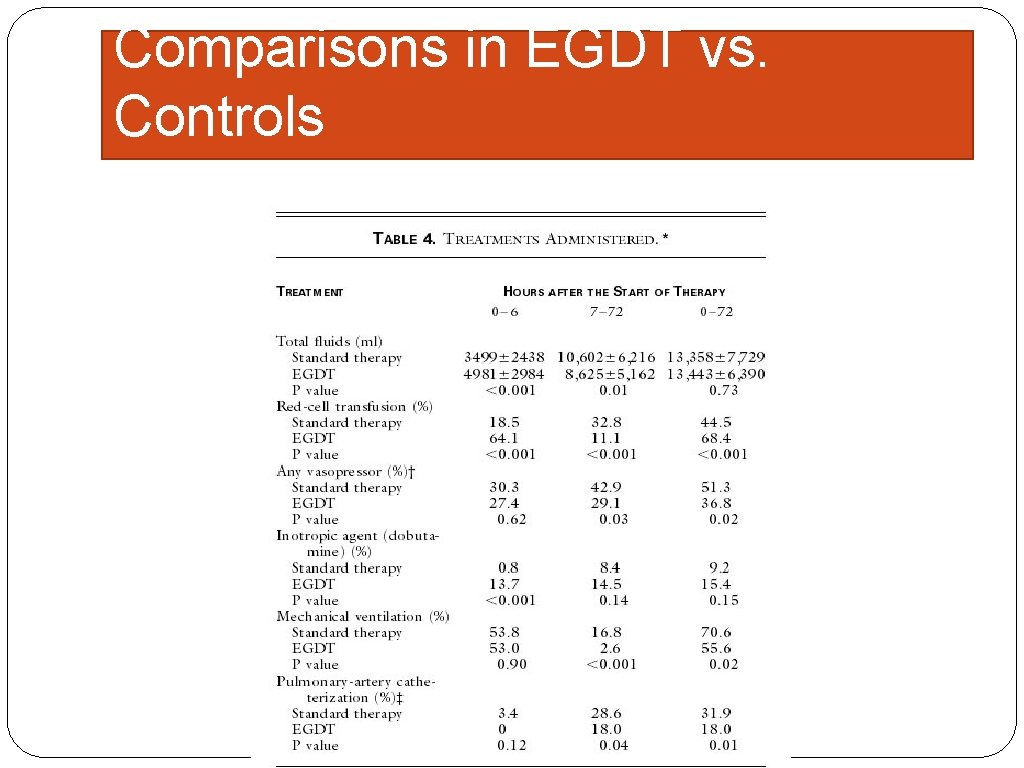
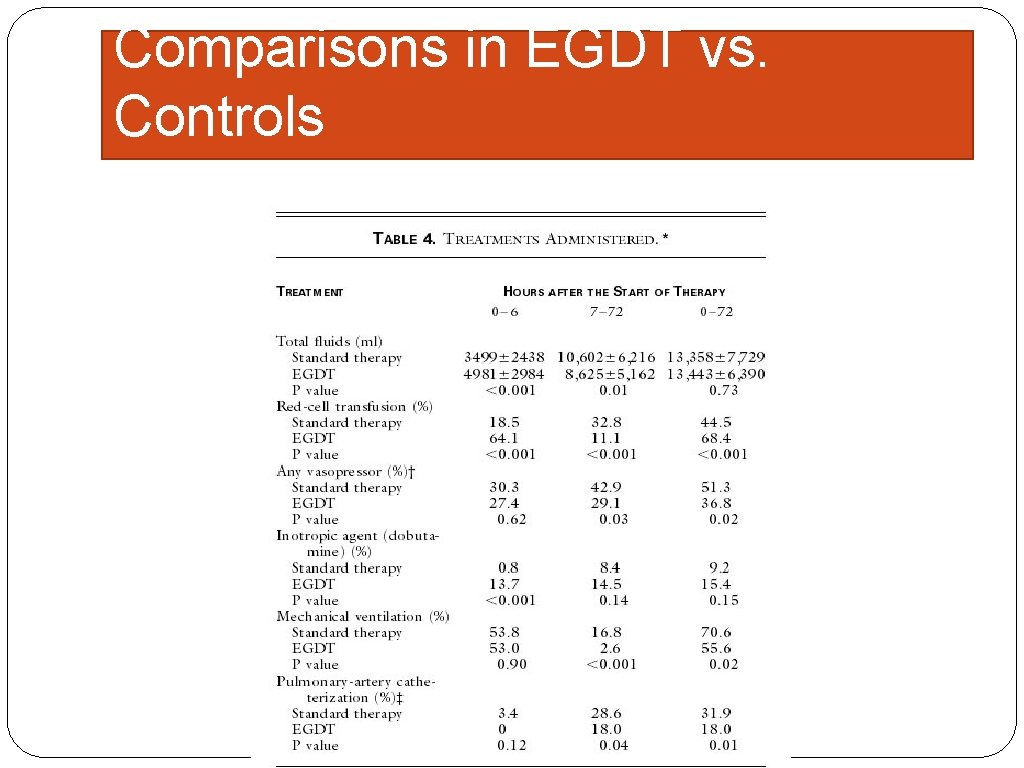
Comparisons in EGDT vs. Controls
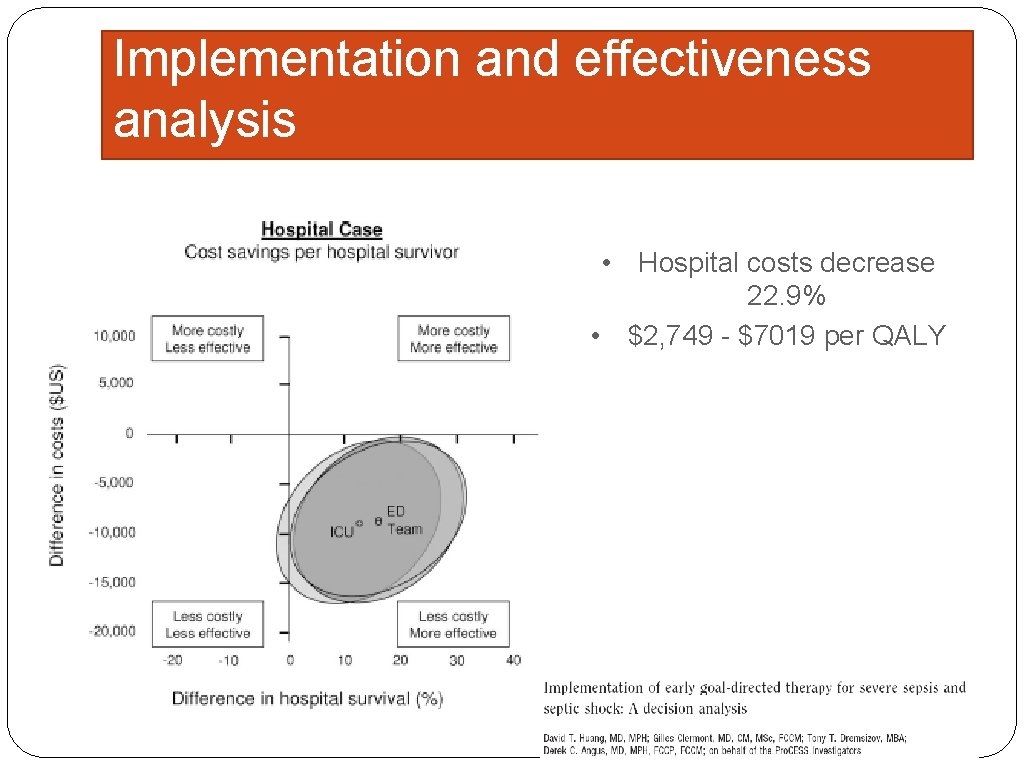
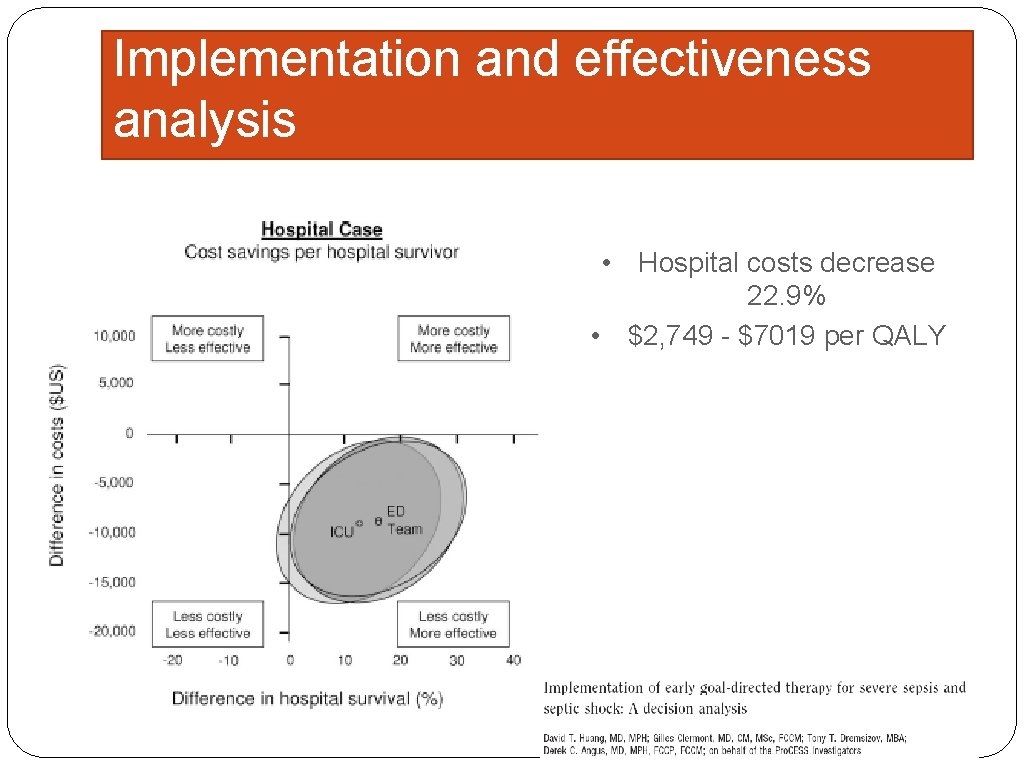
Implementation and effectiveness analysis • Hospital costs decrease 22. 9% • $2, 749 - $7019 per QALY
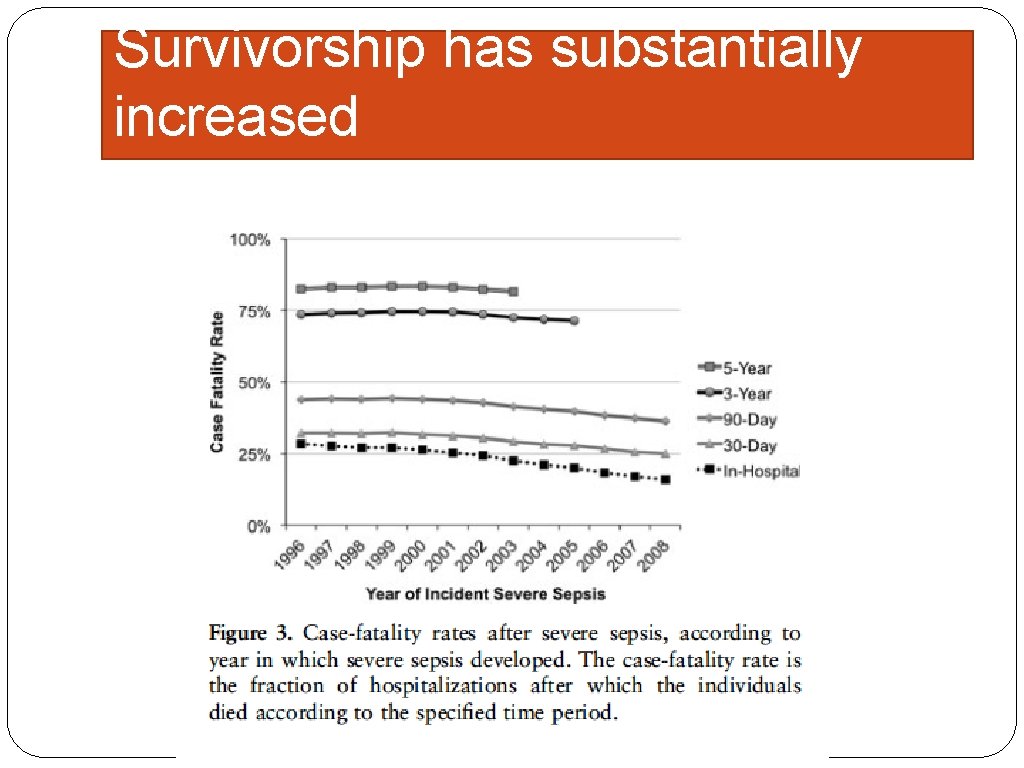
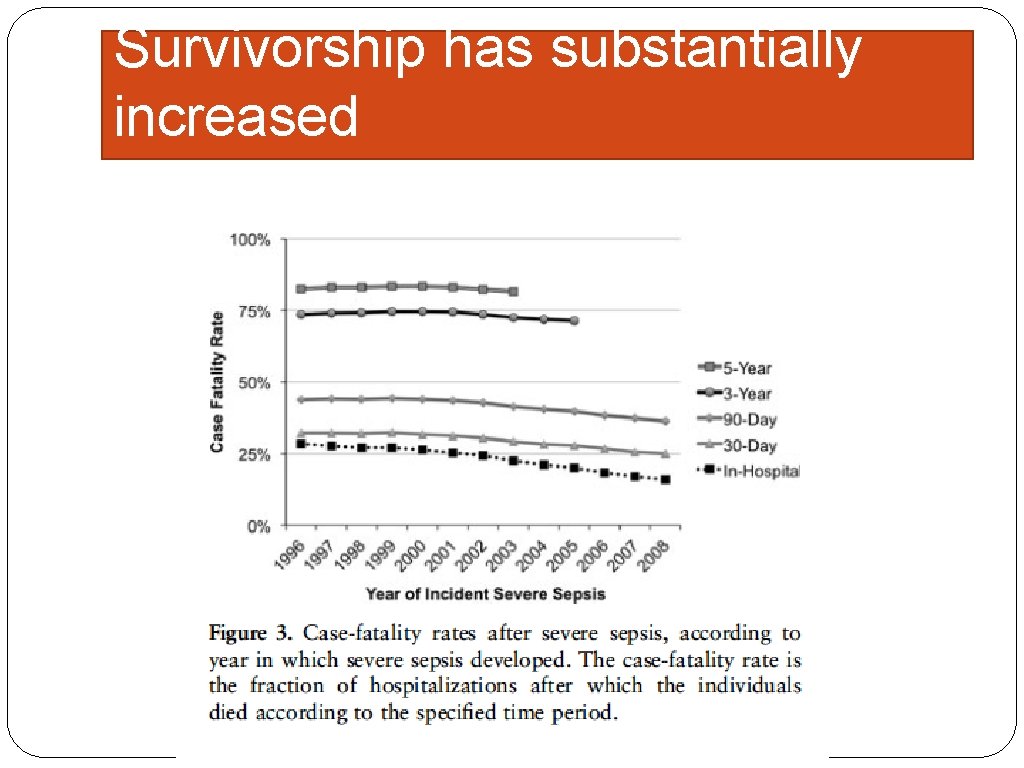
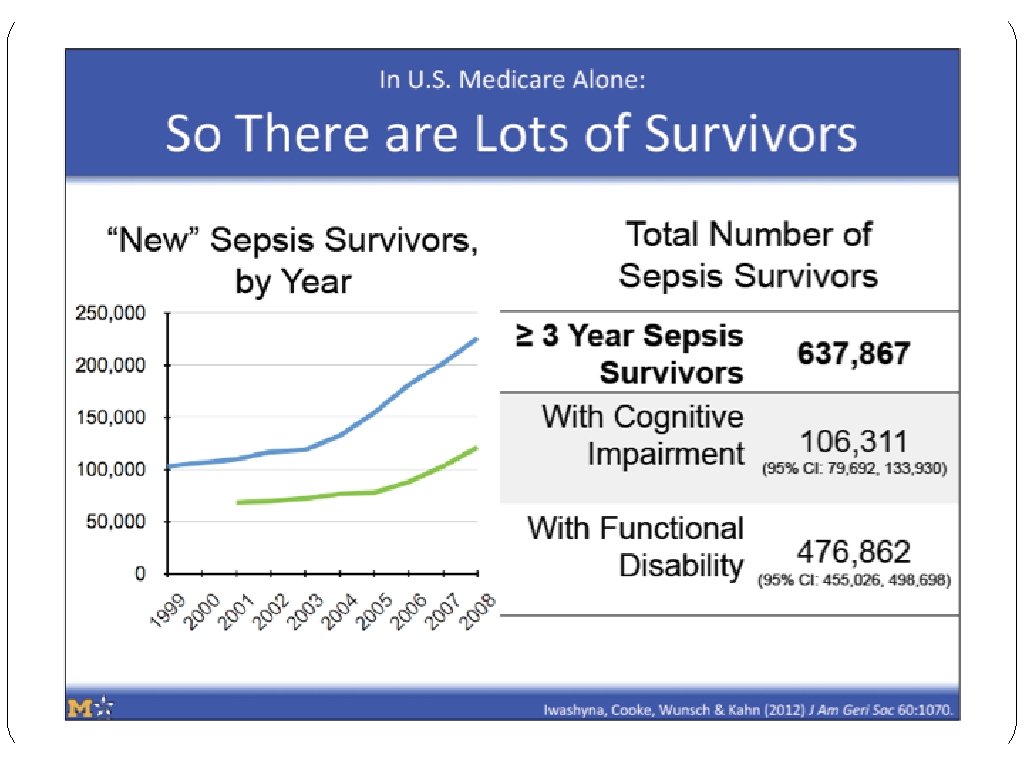
Survivorship has substantially increased
But now I’m told goal-directed therapy is dead
Pro. CESS Trial Objectives �Study EGDT in multi-center format �Compare 3 protocols �Wild-type resuscitation �Protocol guided standard care �Protocol guided EGDT
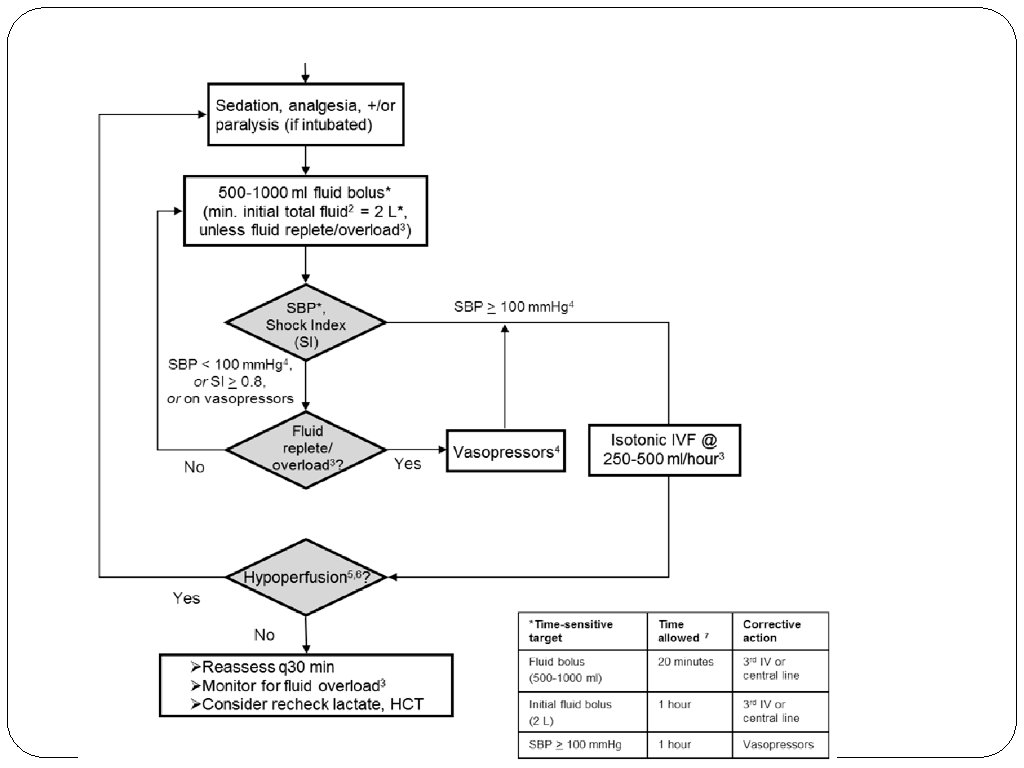
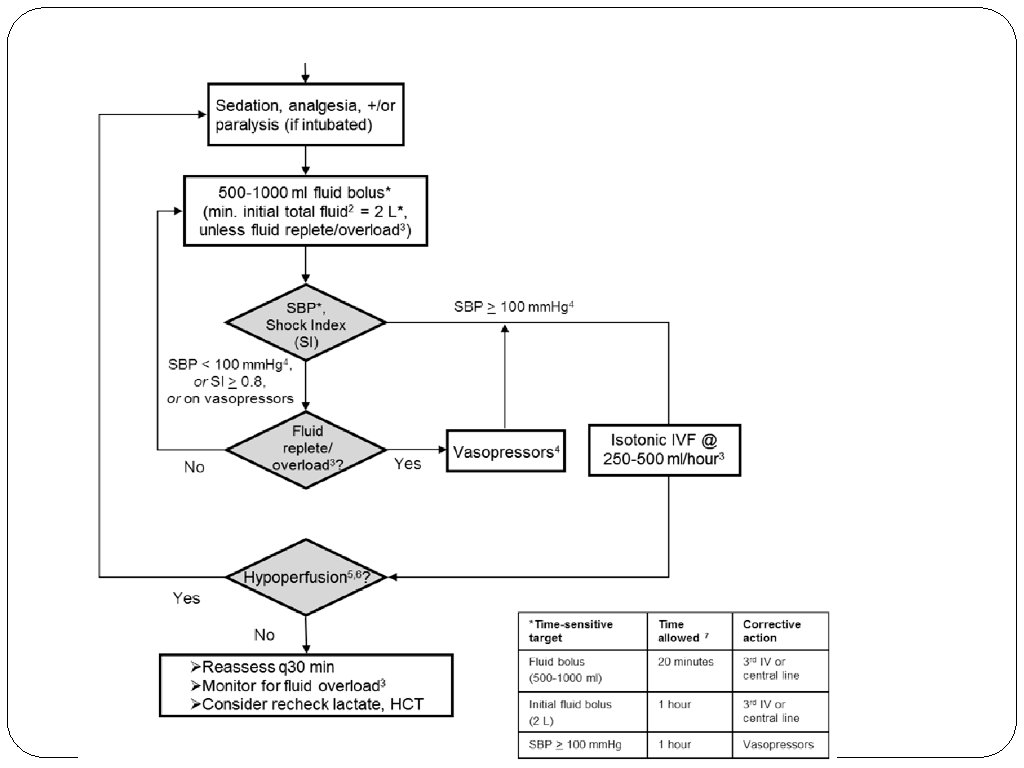
Interventions
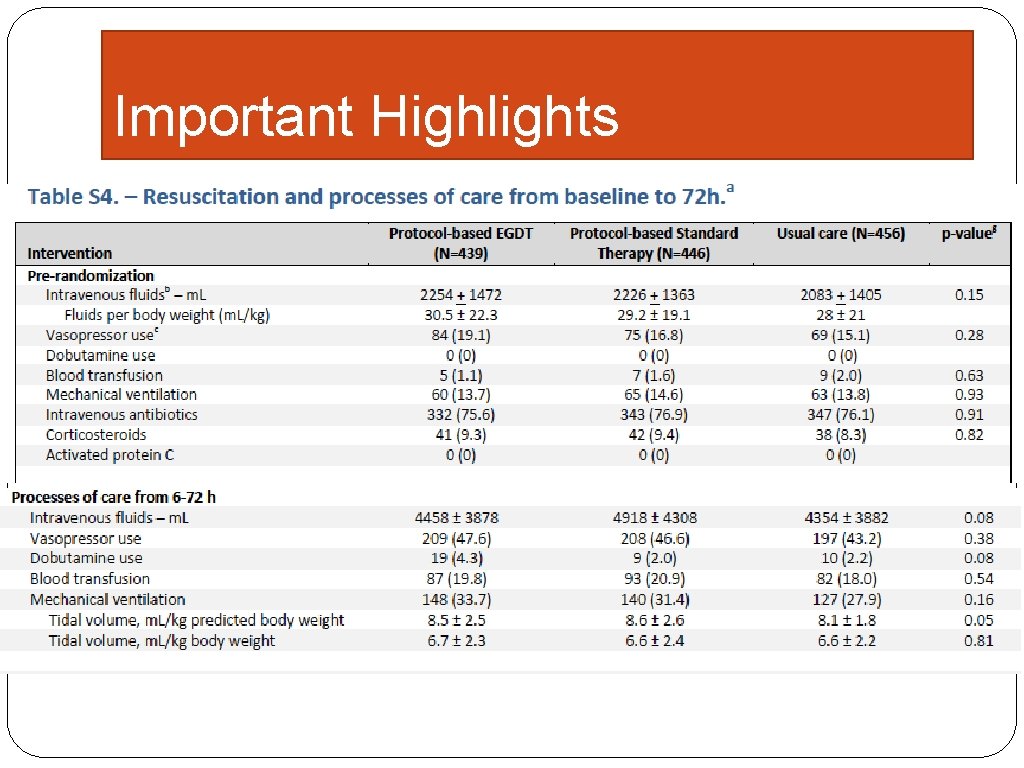
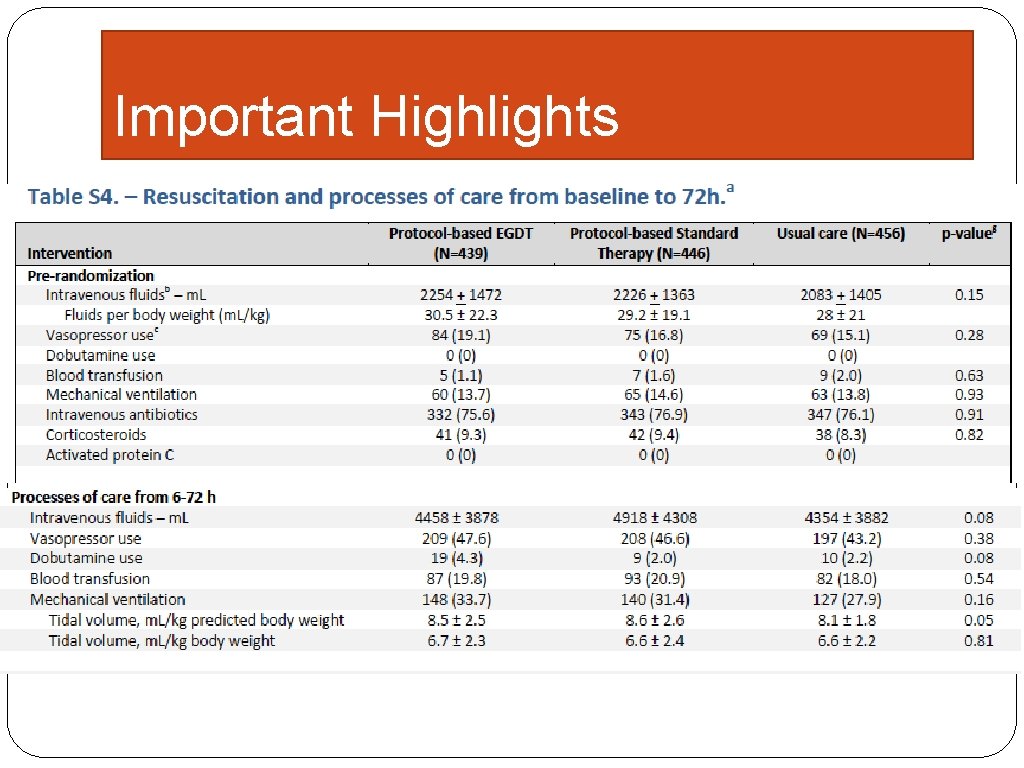
Important Highlights
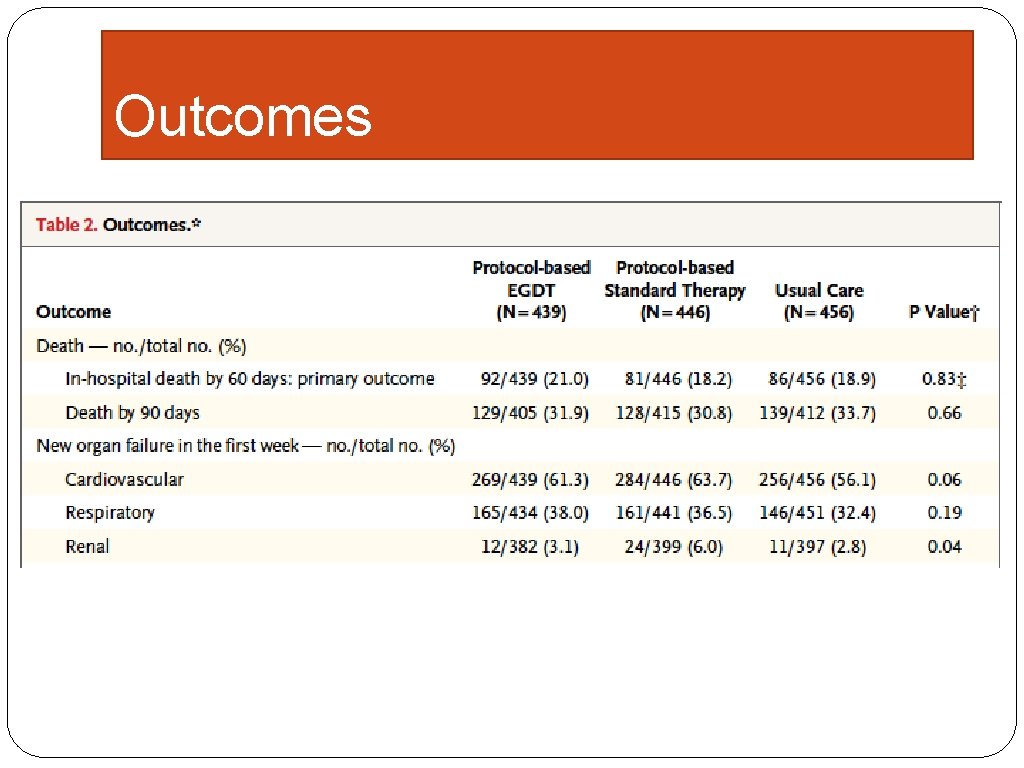
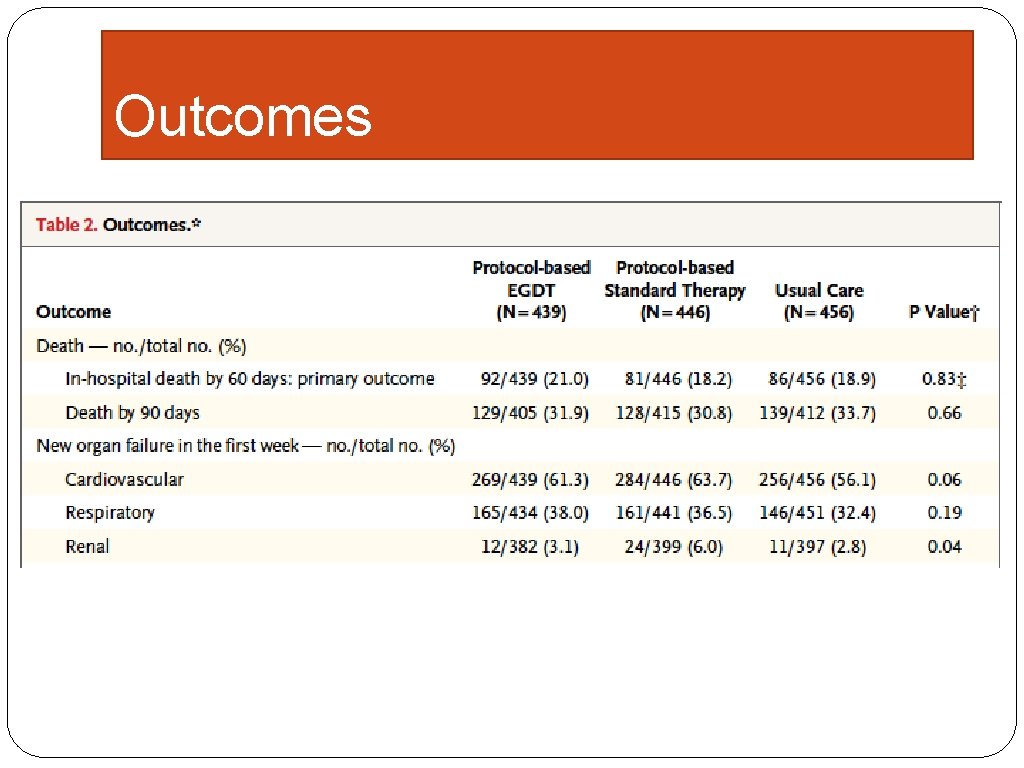
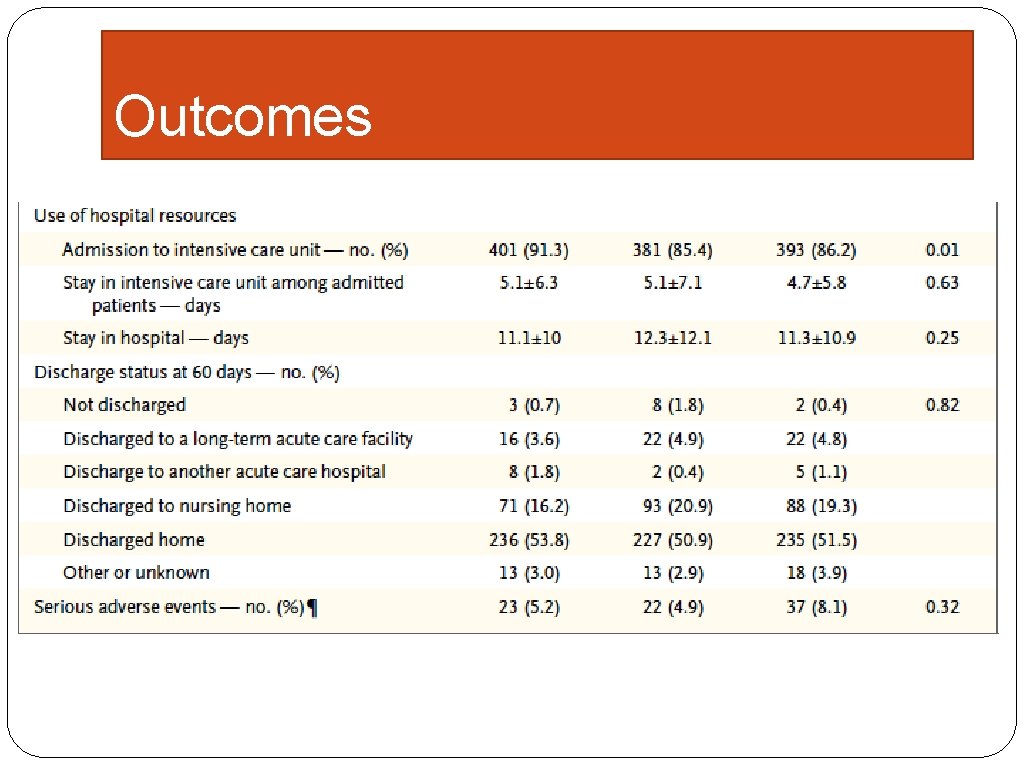
Outcomes
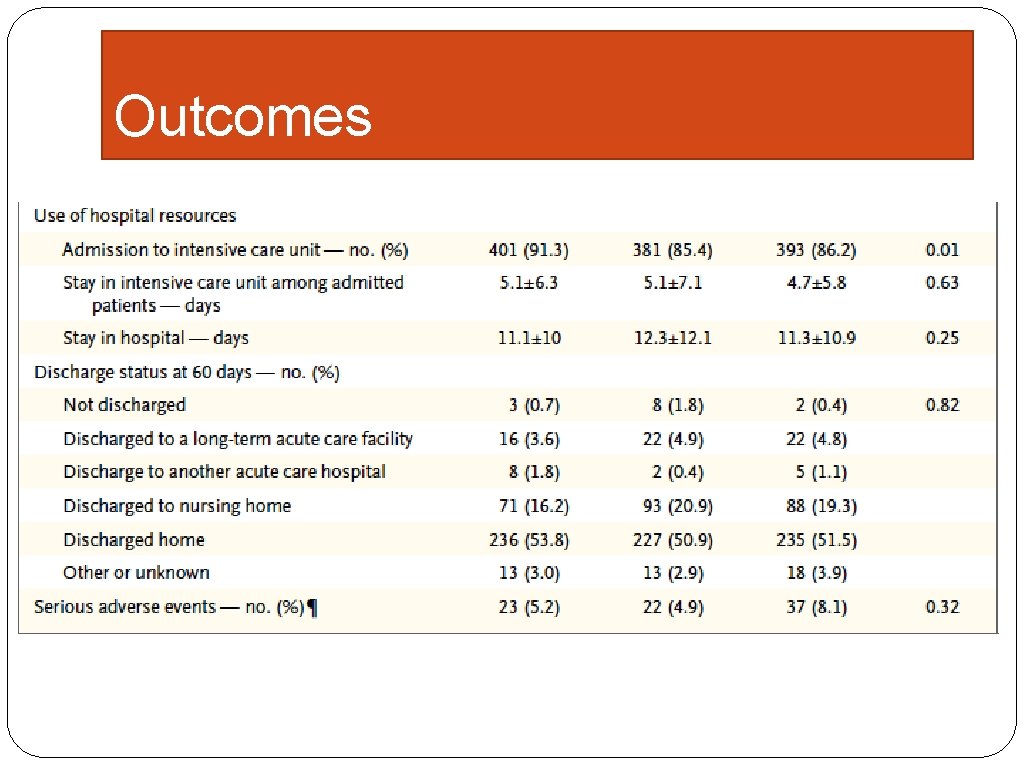
Outcomes
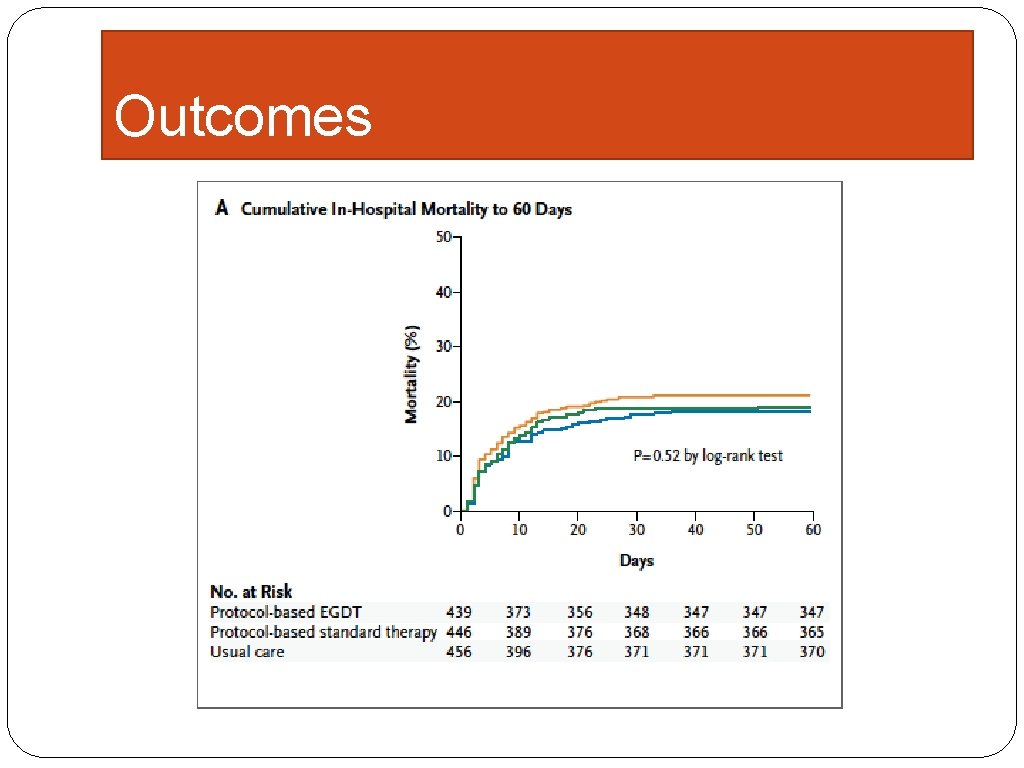
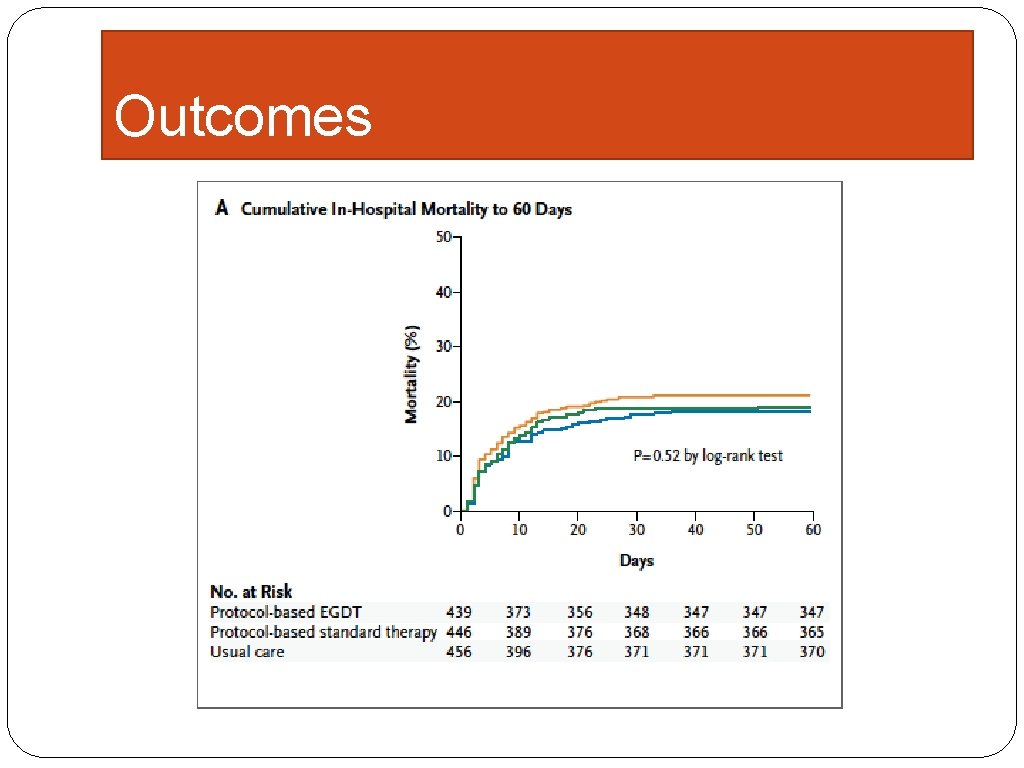
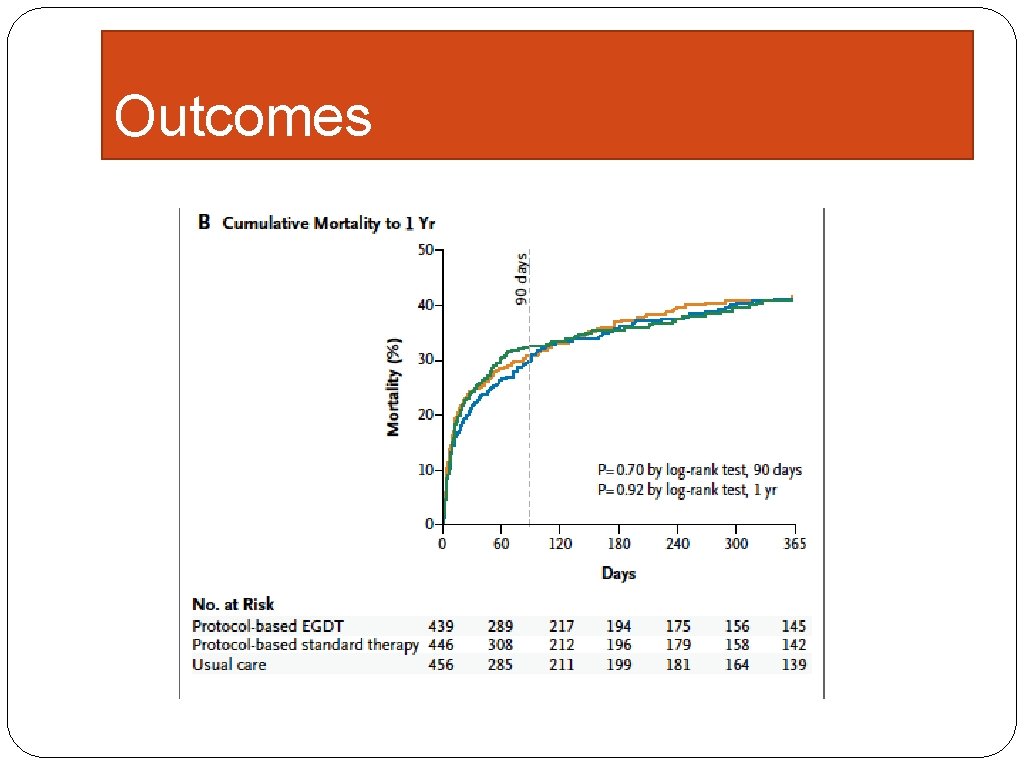
Outcomes
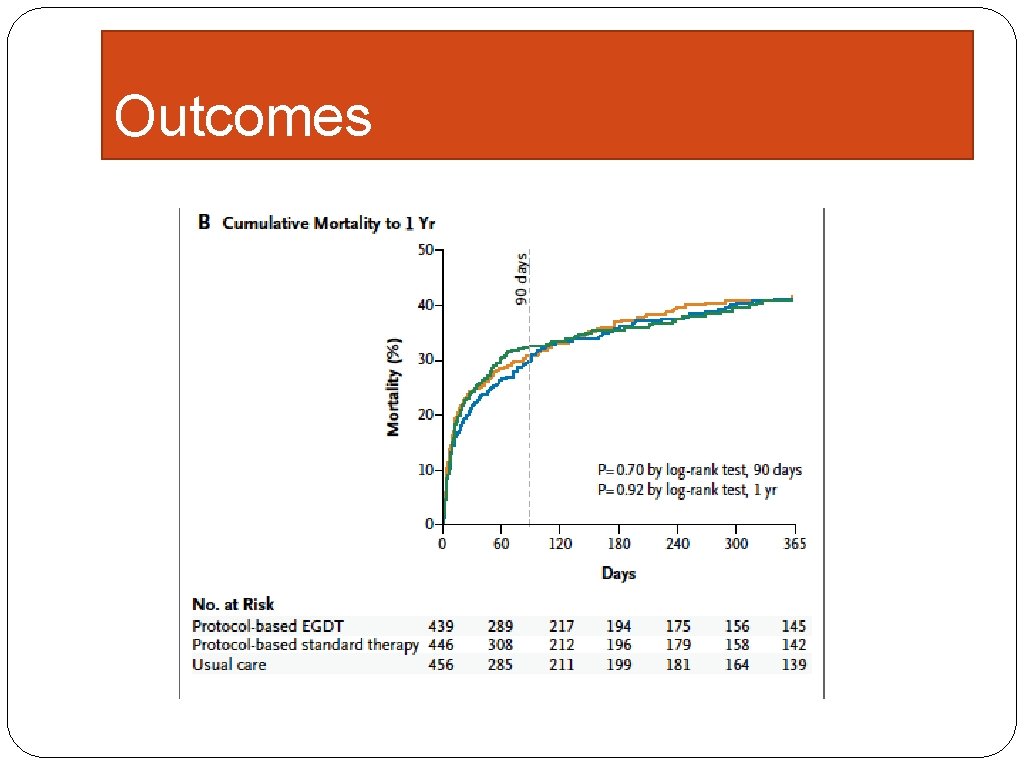
Outcomes
What is important �All of these patients received fluids equivalent to Rivers et al EGDT � 97%+ antibiotics within 6 hours �>70% received antibiotics prior to enrollment �All “identified” as sepsis
Editorial
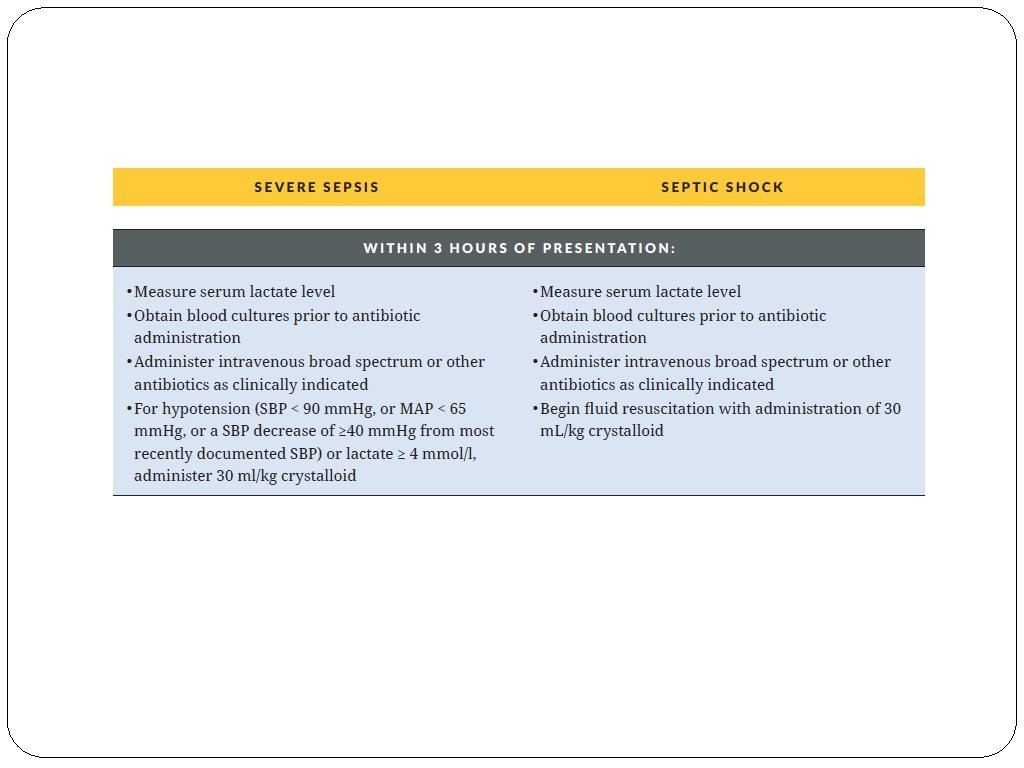
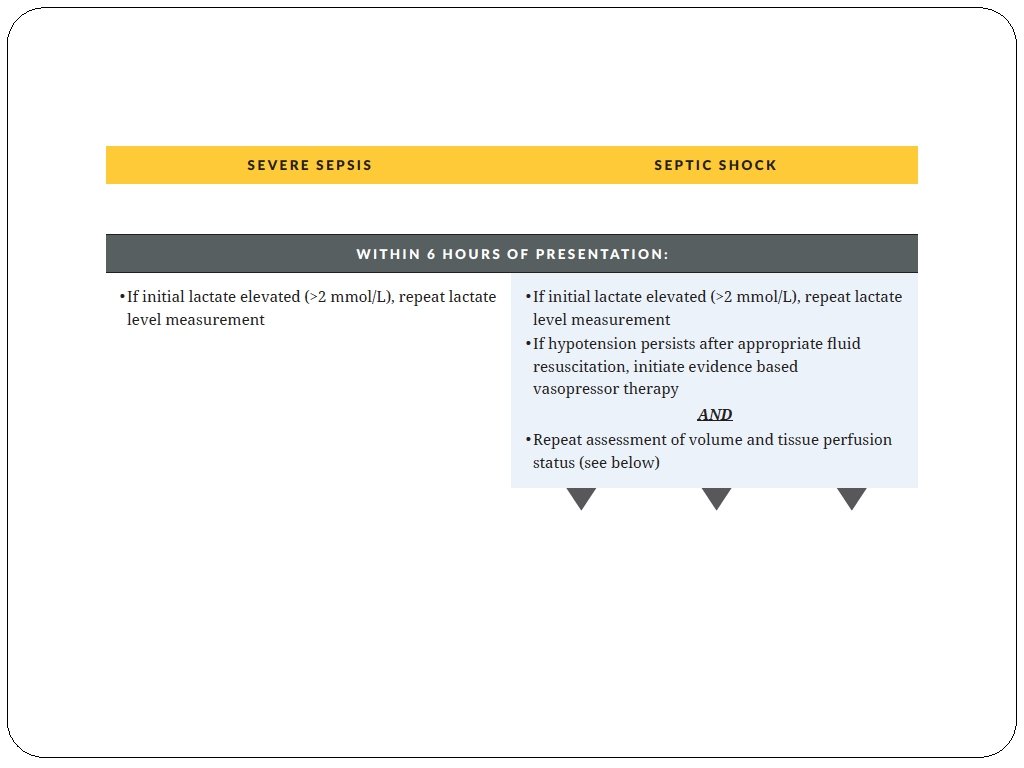
What should we do now? �Our best recommendations are those of the core measures �However, everything starts with EARLY recognition and a sense of medical emergency
Identifying those at risk and making early diagnosis
Be suspicious…. . �The key trait for making early diagnosis is having a constantly elevated index of suspicion �Physicians need to look for sepsis in the same way they look for stroke or AMI, in fact, it is probably more important
Some thoughts on early diagnosis
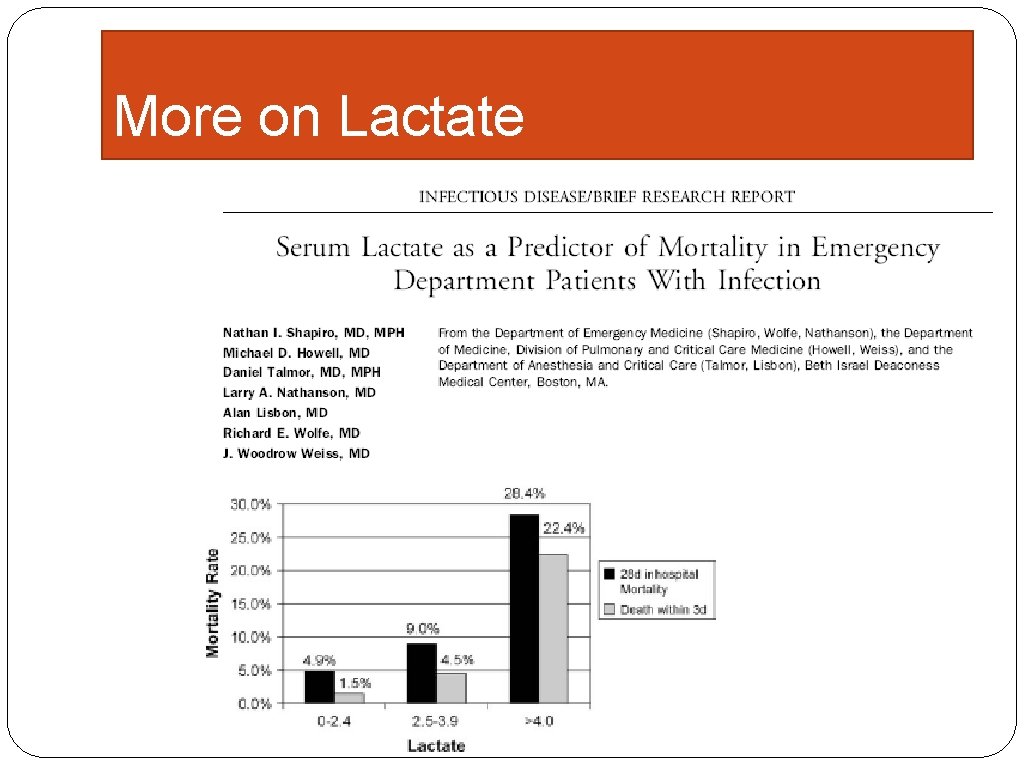
A role for lactate? � ED at Beth Israel Hospital in Boston � 1287 patients with lactates drawn
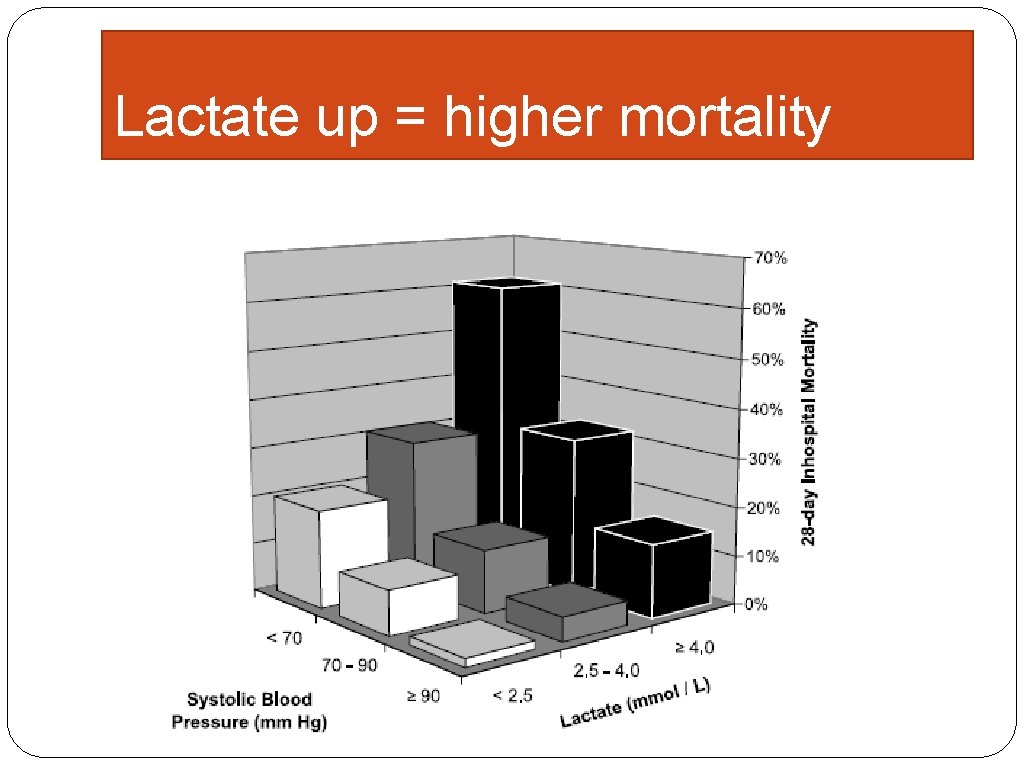
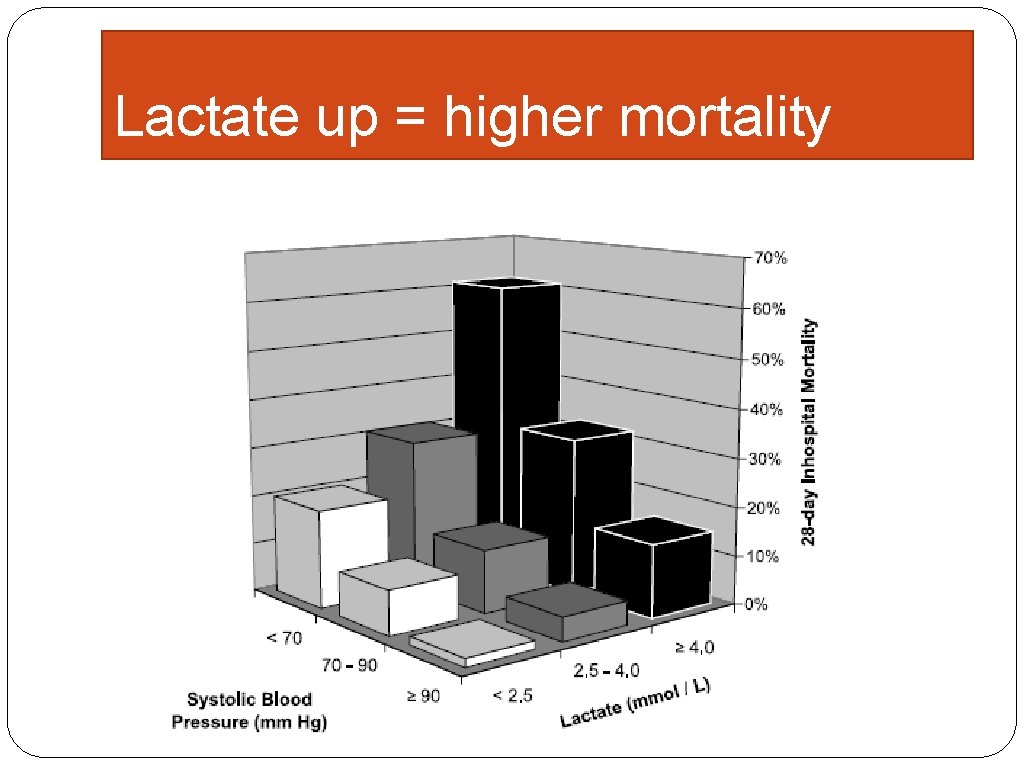
Lactate up = higher mortality
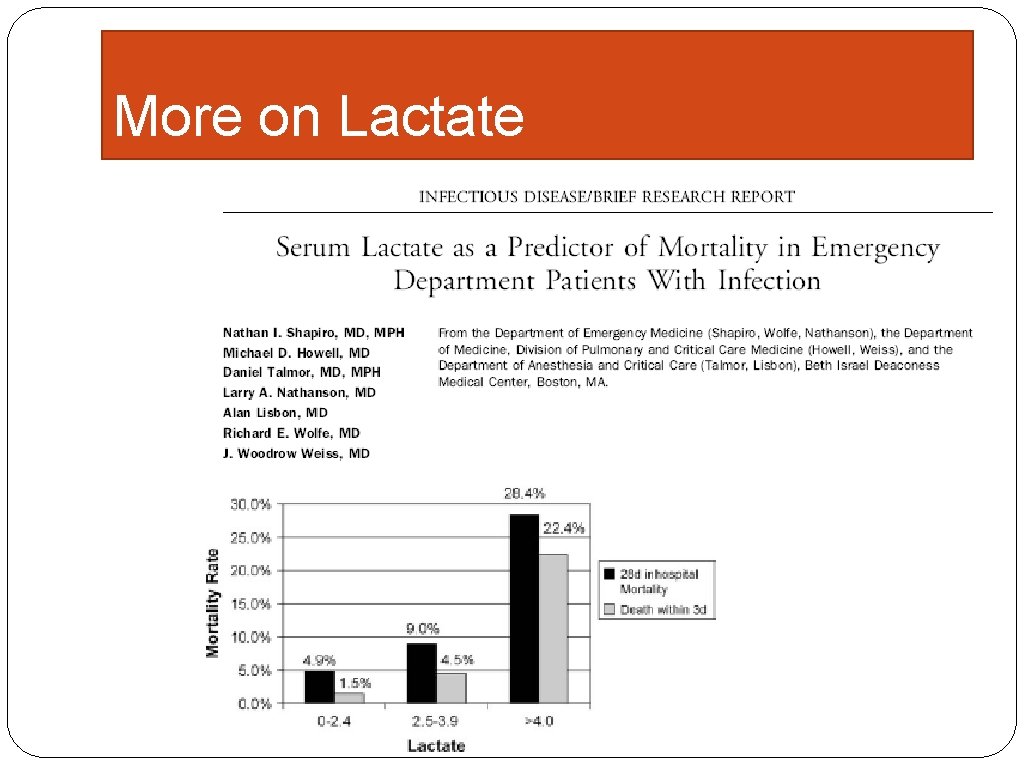
More on Lactate
Blood pressure changes?
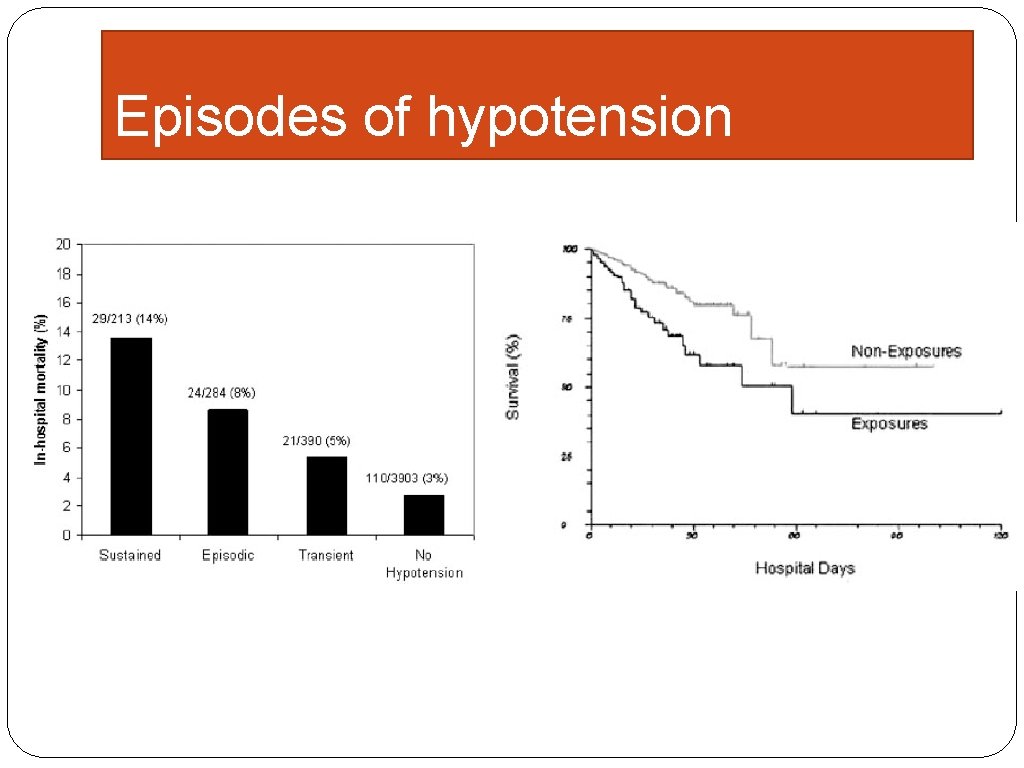
Isolated low BP? � 4700 consecutive ED admissions screened for any episode of low BP � 887 cases found
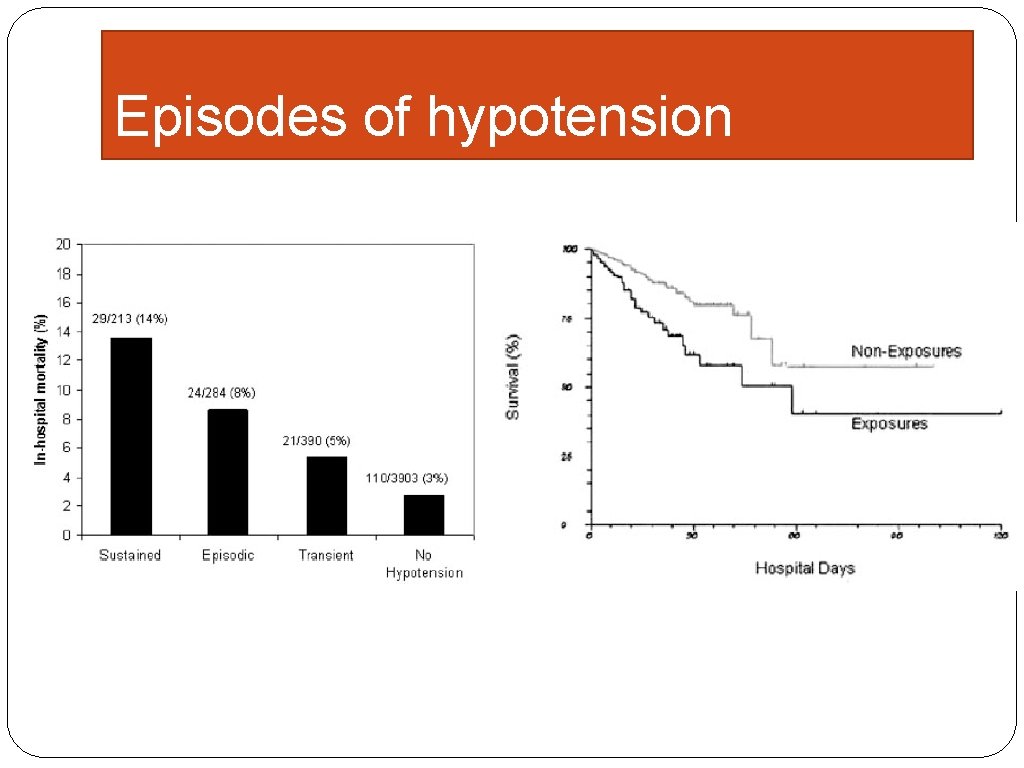
Episodes of hypotension
Core Measures �In development since before 2007 �Extremely complicated measures �“specifications manual” = 63 pages long! �labelled as SEP-1
Strategies � Create a culture of passion for the care of septic patients � Become an evangelist! � Take every moment to coach up the team � Sepsis care is a TEAM effort � Teach away medical mythology � create pathways and order sets that leverage current practices in other areas into best sepsis care
Common Myths 1. Avoiding Fluids in certain patient populations 1. Renal failure 2. Heart failure 2. Giving Normal Saline because the potassium is high 3. There is a “maximum” vasopressor dose 4. We give fluids to raise the blood pressure
Myth #1 � I am commonly told that people “didn’t want to give too much fluid” due to either heart failure or renal failure � The 30 cc/kg bolus septic patients need is well tolerated by almost everyone. � Avoiding sufficient fluids is practicing as per the control group in Dr. Rivers goal-directed trial � Sepsis associated renal failure is much harder to reverse if we fail to restore perfusion
Myth #2 � It is common to avoid Lactated Ringer’s if there is acute kidney injury or elevated potassium due to potassium content � There is only 4 m. Eq/L of potassium � LR is a neutral p. H buffered solution vs. NS that has a p. H of 4. 5 and causes a hyperchloremic acidosis � Most hyperkalemia is due to acidosis related cellular shifts. correcting the acidosis fixes the hyperkalemia.
Myth #3 �The patient is on “max” norepi �There is simply no such thing. They need what they need. I have used doses as high as 4 mkg/kg/min (>400 mkg/min) in patients who survive.
Myth # 4 �Fluids are given to raise the blood pressure �Fact: fluids fill the ventricles and improve stroke volume/cardiac output. �If cardiac output doesn’t increase with fluid, the patient will NOT benefit from more fluid. Use vasopressors.
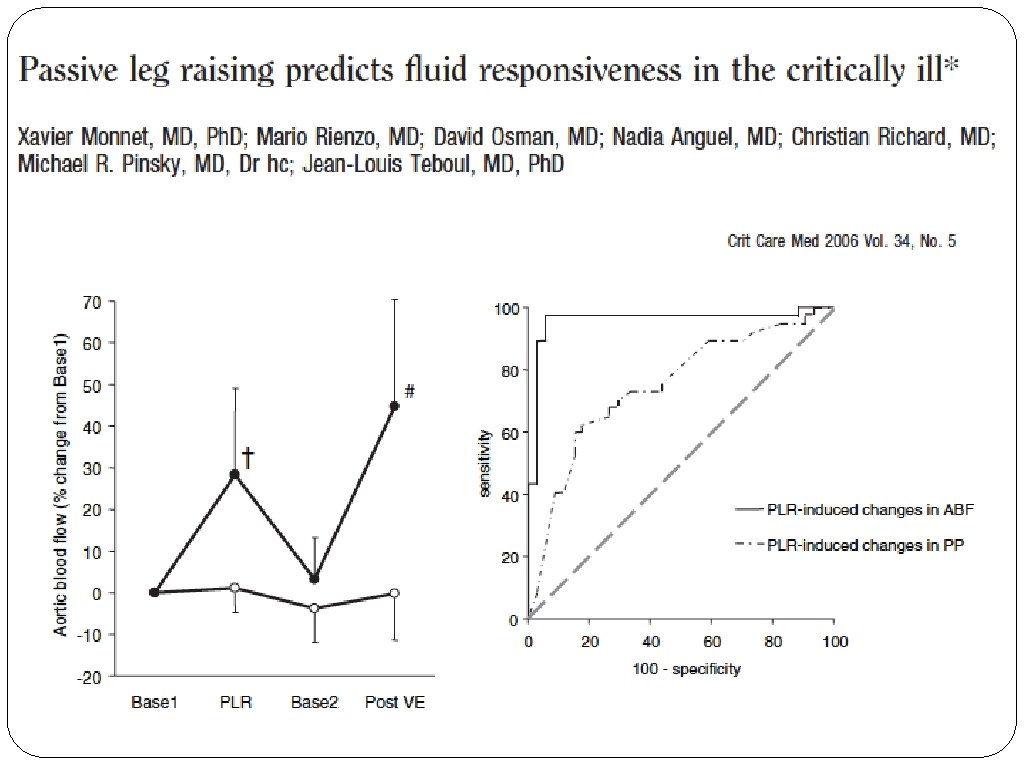
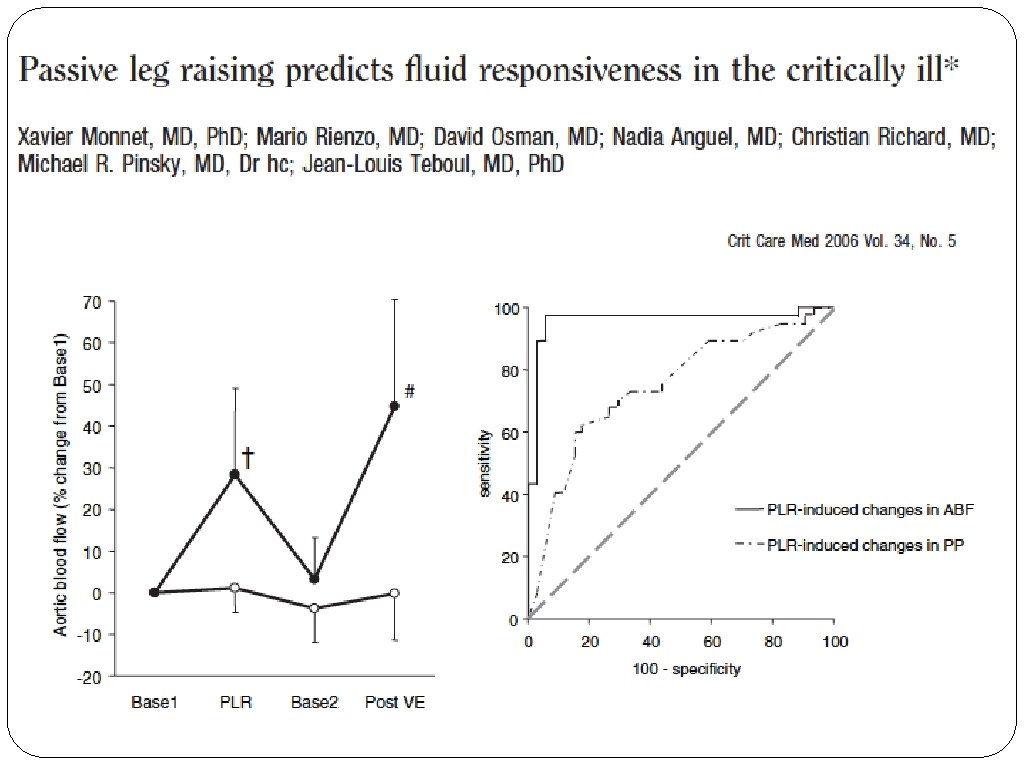
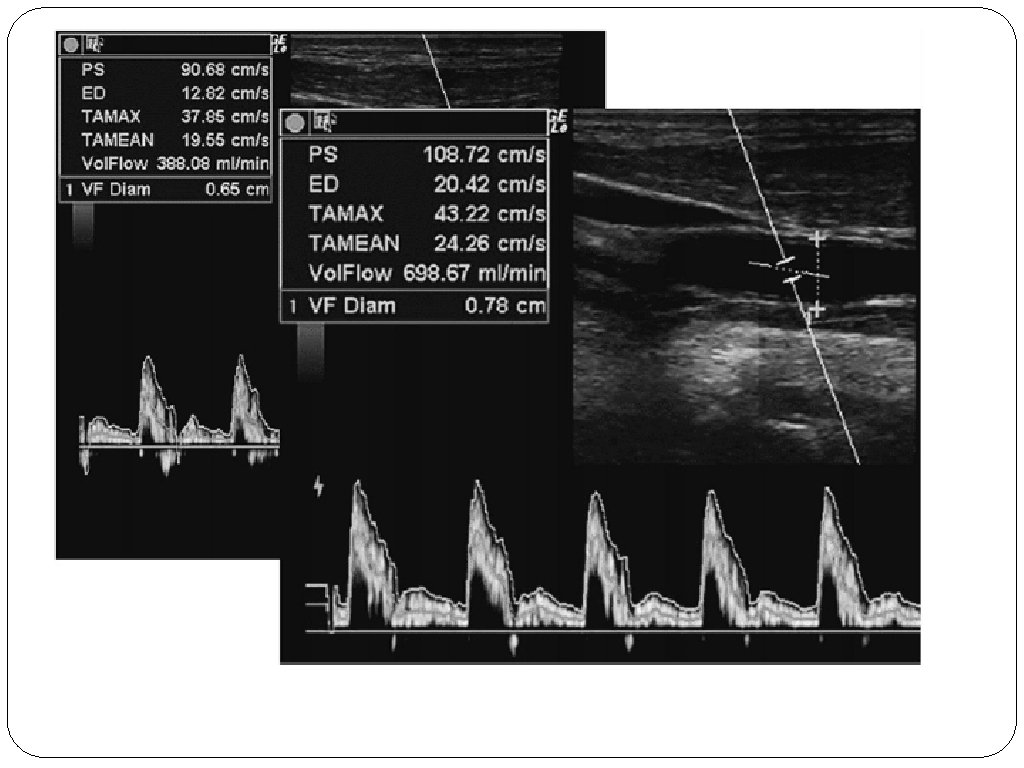
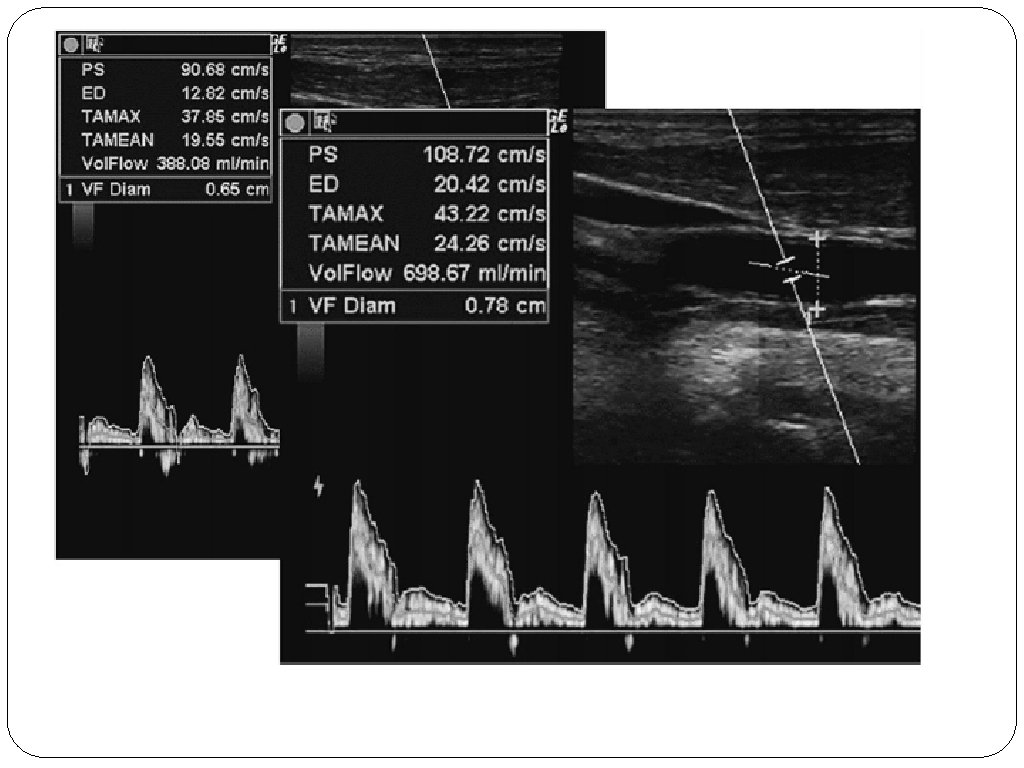
Straight leg raise
Antibiotics
� Retrospective data collection at 22 centers � All patients with sepsis � Evaluated appropriate abx by whether it fit guidelines or covered eventual cultures
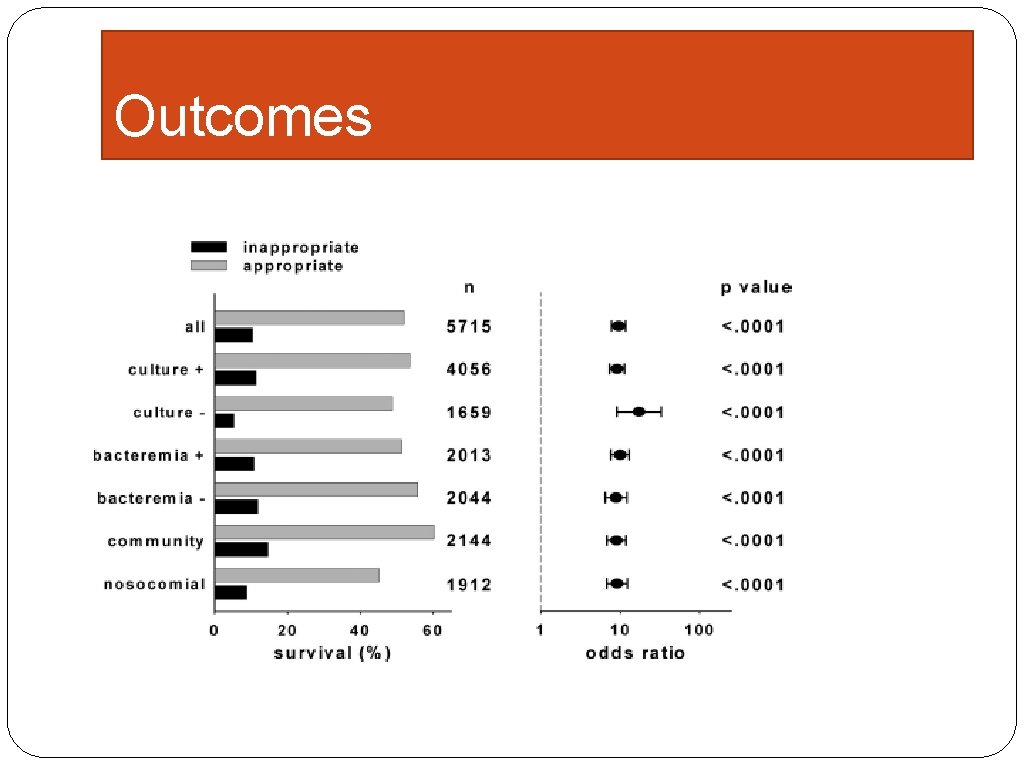
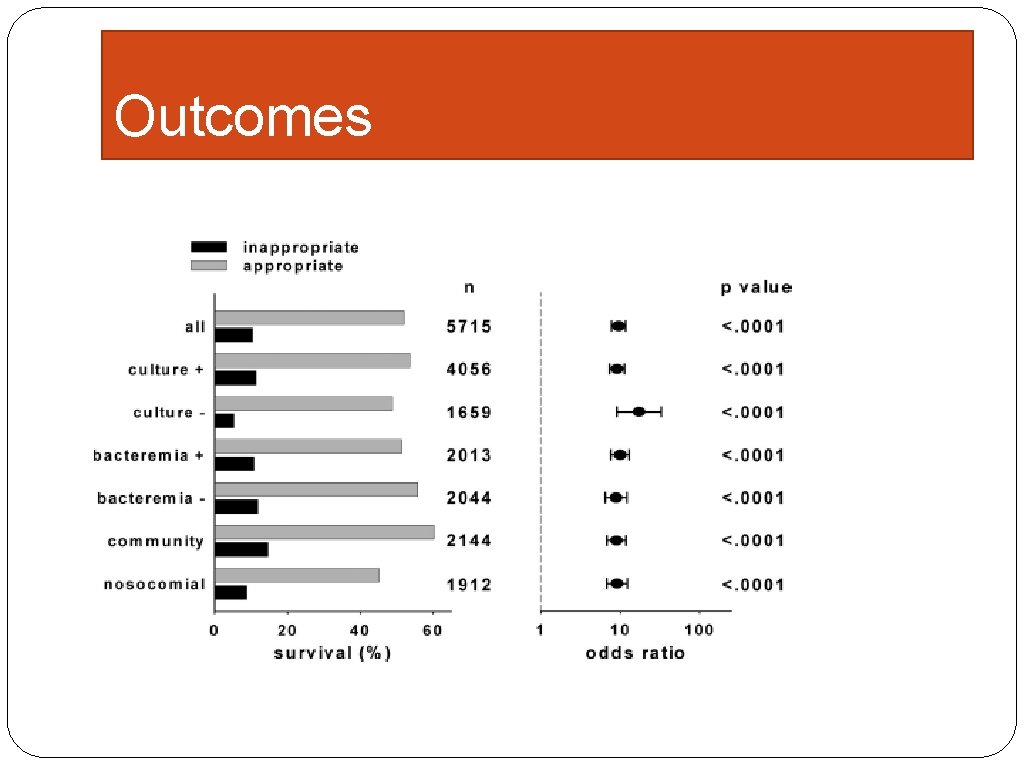
Outcomes
Summary � Sepsis is a MEDICAL EMERGENCY � Sepsis care has evolved substantially over 15 years with significantly reduced mortality � The core of sepsis care is: � Early diagnosis � Early fluids � Early antibiotics � The new core measures reflect these data
Advice �Find committed and motivated people �Give them the time, tools and authority to work on this system �Support the message every day �Be prepared for this to take a long time Daniel S. Hagg Assistant Professor, Director of MICU Director of Inpatient Quality for the Department of Medicine Oregon Health and Sciences University 503 -494 -6668 or Cell 503 -228 -0459