Sepsis and the systemic inflammatory response syndrome Definitions
![Epidemiology Incidence of Sepsis [1993 -2001]. . . a 75% increase in. . . Epidemiology Incidence of Sepsis [1993 -2001]. . . a 75% increase in. . .](https://slidetodoc.com/presentation_image_h/1332232e04c6a1006abf59a6764f03e6/image-14.jpg)
- Slides: 47
• Sepsis and the systemic inflammatory response syndrome: Definitions, epidemiology, and prognosis
Sepsis Yasar. Kucukardalı MD Yeditepe University
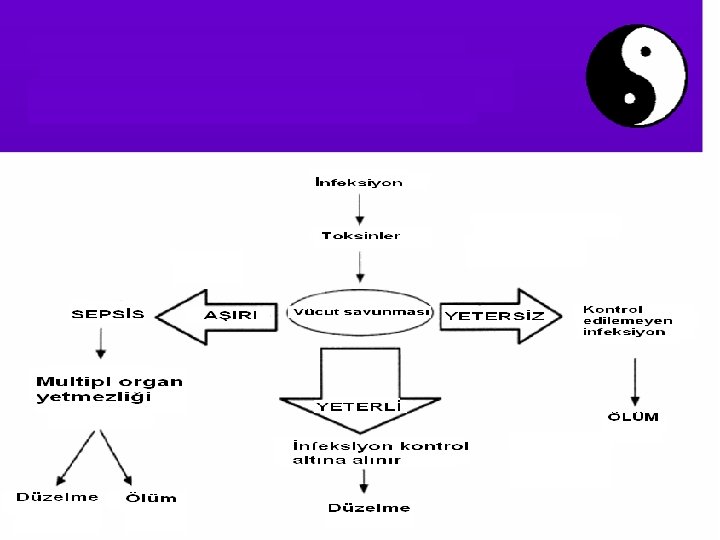
Infection • Infection is characterized by an inflammatory response to microorganisms, or the invasion of normally sterile host tissue by those organisms
Bacteremia • Bacteremia is defined as the presence of viable bacteria in the blood.
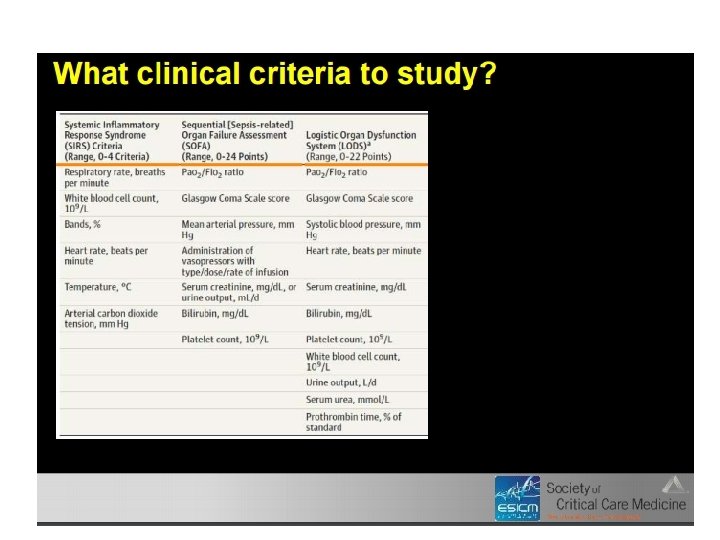
Systemic inflammatory response syndrome (SIRS) SIRS refers to the consequences of a dysregulated host inflammatory response. It is clinically recognized by the presence of two or more of the following • Temperature >38. 5ºC or <35ºC • Heart rate >90 beats/min • Respiratory rate >20 breaths/min or Pa. CO 2 <32 mm. Hg • WBC >12, 000 cells/mm 3, <4000 cells/mm 3, or >10 percent immature (band) forms SIRS can result from a variety of conditions, such as autoimmune disorders, pancreatitis, vasculitis, thromboembolism, burns, or surgery.
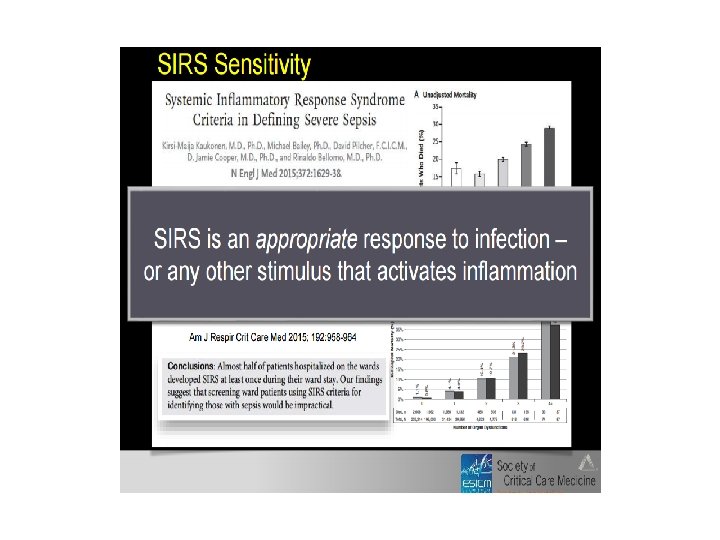
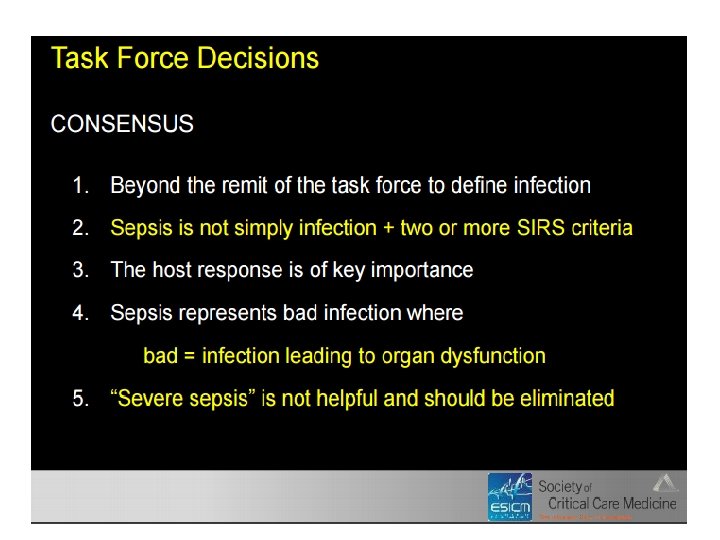
• The SIRS criteria do not necessarily indicate a dysregulated, life-threatening response. SIRS criteria are present in many hospitalized patients, including those who never develop infection and never incur adverse outcomes (poor discriminant validity)5 In addition, 1 in 8 patients admitted to critical care units in Australia and New Zealand with infection and new organ failure did not have the requisite minimum of 2 SIRS criteria to fulfill the definition of sepsis (poor concurrent validity) yet had protracted courses with significant morbidity and mortality.
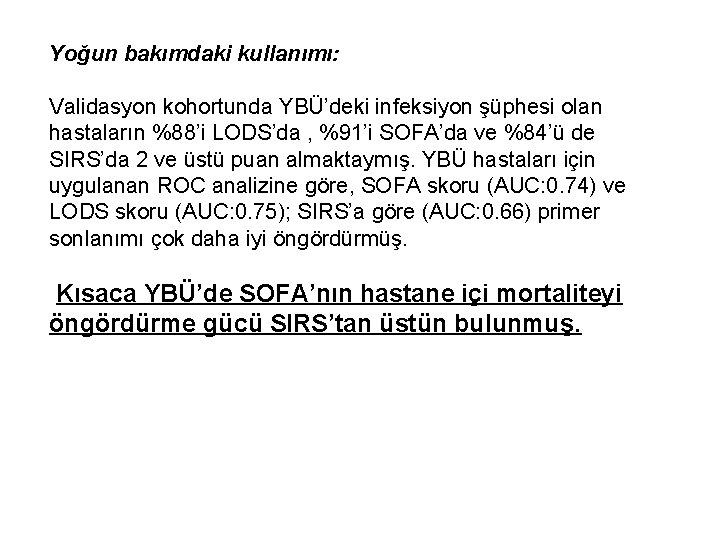
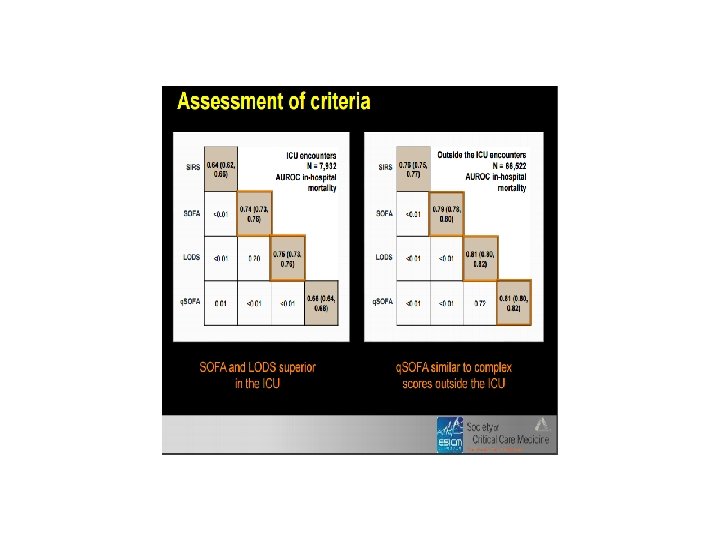
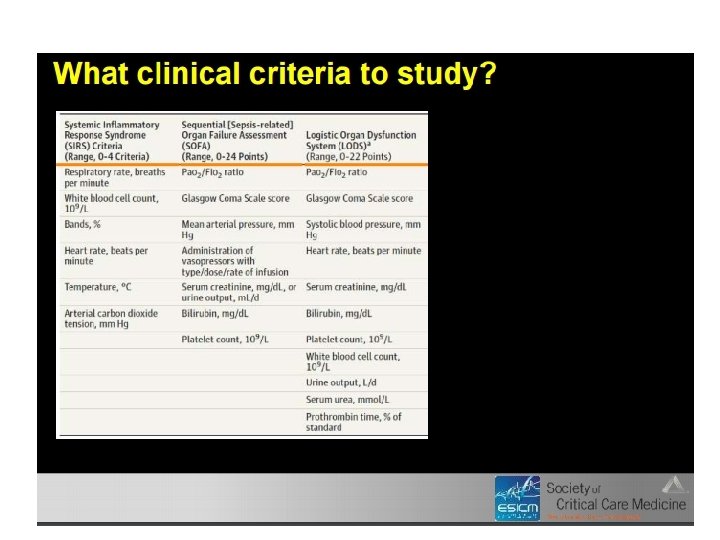
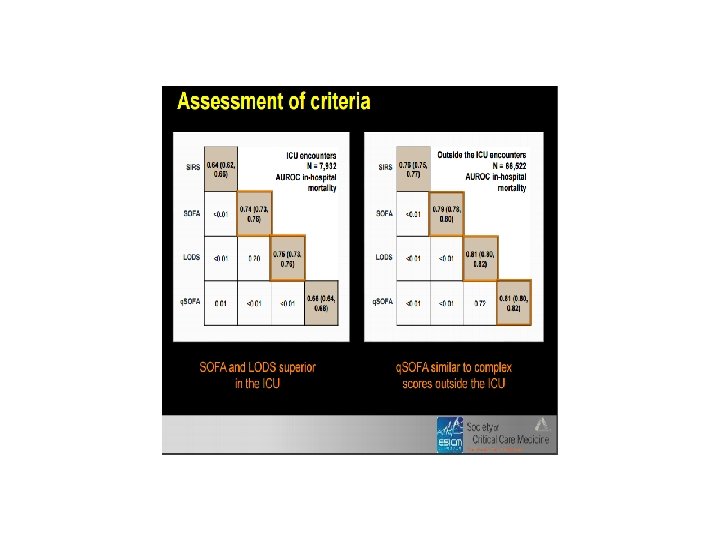
Yoğun bakımdaki kullanımı: Validasyon kohortunda YBÜ’deki infeksiyon şüphesi olan hastaların %88’i LODS’da , %91’i SOFA’da ve %84’ü de SIRS’da 2 ve üstü puan almaktaymış. YBÜ hastaları için uygulanan ROC analizine göre, SOFA skoru (AUC: 0. 74) ve LODS skoru (AUC: 0. 75); SIRS’a göre (AUC: 0. 66) primer sonlanımı çok daha iyi öngördürmüş. Kısaca YBÜ’de SOFA’nın hastane içi mortaliteyi öngördürme gücü SIRS’tan üstün bulunmuş.
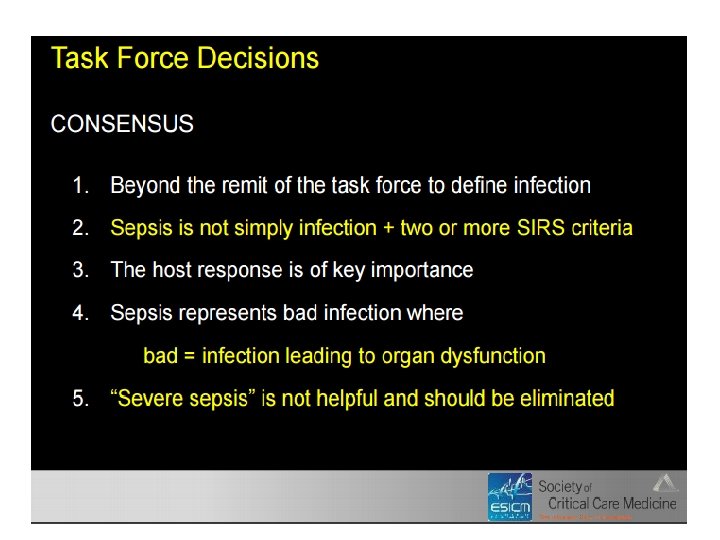
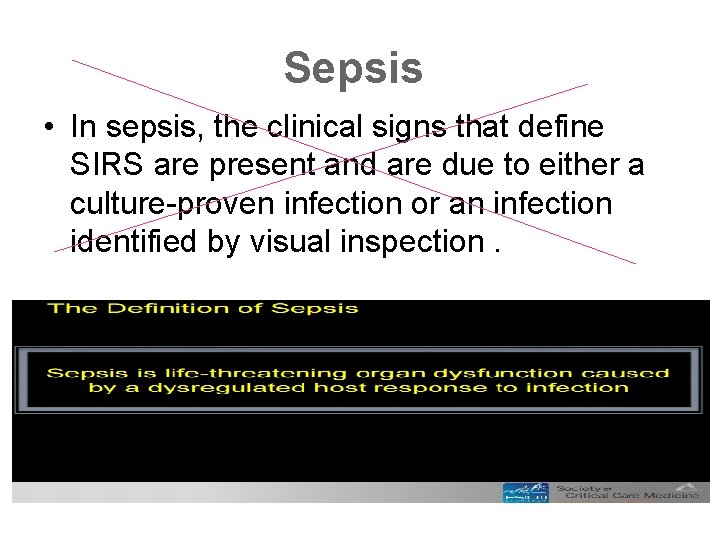
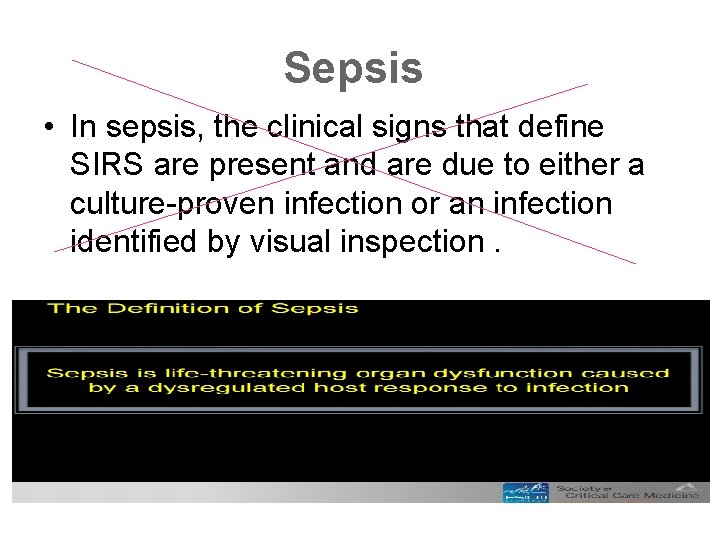
Sepsis • In sepsis, the clinical signs that define SIRS are present and are due to either a culture-proven infection or an infection identified by visual inspection.
13
![Epidemiology Incidence of Sepsis 1993 2001 a 75 increase in Epidemiology Incidence of Sepsis [1993 -2001]. . . a 75% increase in. . .](https://slidetodoc.com/presentation_image_h/1332232e04c6a1006abf59a6764f03e6/image-14.jpg)
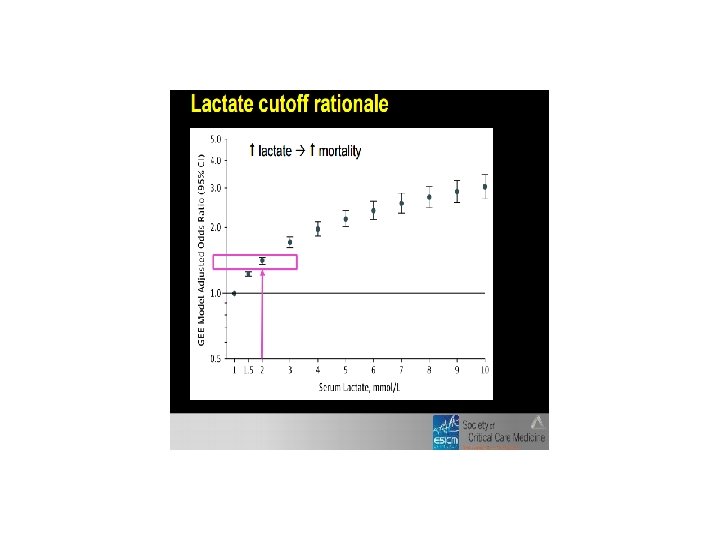
Epidemiology Incidence of Sepsis [1993 -2001]. . . a 75% increase in. . . severe sepsis. . . Mortality of Sepsis [1993 - 2001]. . . a 17% reduction in mortality. Martin, G. S. , Mannino, D. M. , Eaton, S. , & Moss, M. (2003). The epidemiology of sepsis in the United States from 1979 through 2000. New England Journal of Medicine, 348(16), 1546– 1554. Brun-Buisson, C. , Meshaka, P. , Pinton, P. , Vallet, B. , EPISEPSIS Study Group. (2004). EPISEPSIS: a reappraisal of the epidemiology and outcome of severe sepsis in French intensive care units. Intensive Care Medicine, 30(4), 580– 588. Harrison, D. A. , Welch, C. A. , & Eddleston, J. M. (2006). The epidemiology of severe sepsis in England, Wales and Northern Ireland, 1996 to 2004: secondary analysis of a high quality clinical database, the ICNARC Case Mix Programme Database. Critical Care, 10(2), R 42.
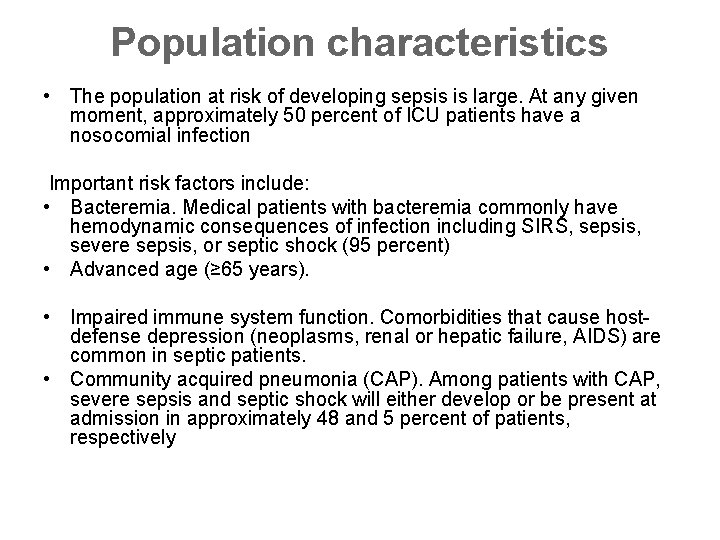
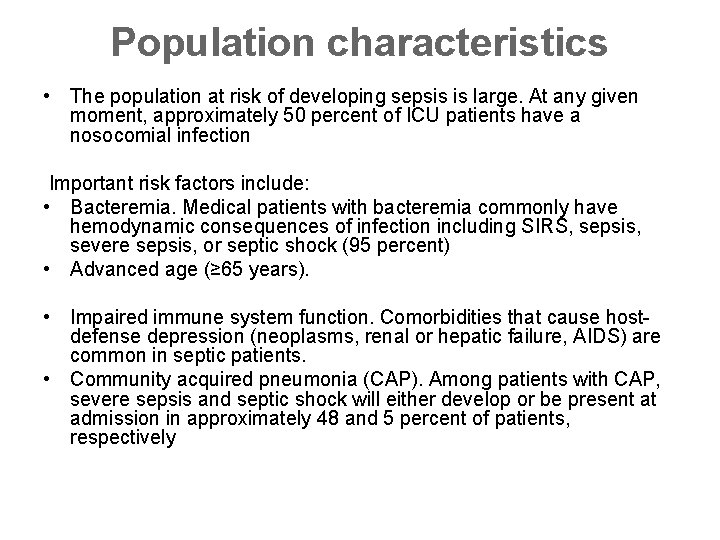
Population characteristics • The population at risk of developing sepsis is large. At any given moment, approximately 50 percent of ICU patients have a nosocomial infection Important risk factors include: • Bacteremia. Medical patients with bacteremia commonly have hemodynamic consequences of infection including SIRS, sepsis, severe sepsis, or septic shock (95 percent) • Advanced age (≥ 65 years). • Impaired immune system function. Comorbidities that cause hostdefense depression (neoplasms, renal or hepatic failure, AIDS) are common in septic patients. • Community acquired pneumonia (CAP). Among patients with CAP, severe sepsis and septic shock will either develop or be present at admission in approximately 48 and 5 percent of patients, respectively
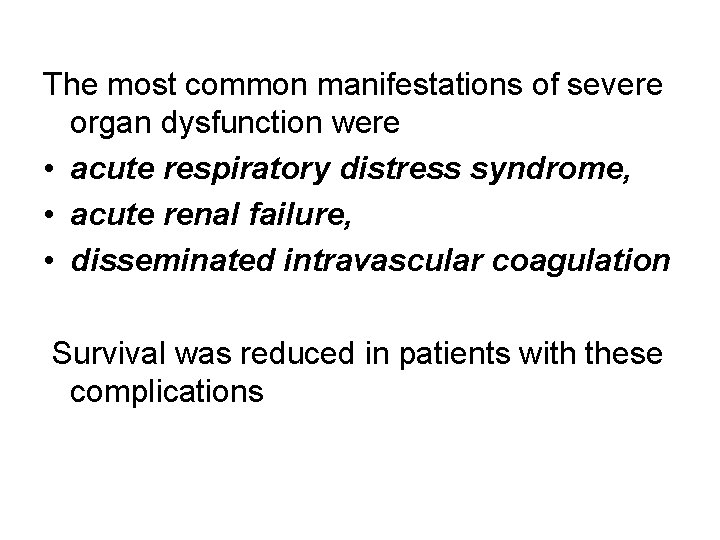
The most common manifestations of severe organ dysfunction were • acute respiratory distress syndrome, • acute renal failure, • disseminated intravascular coagulation Survival was reduced in patients with these complications
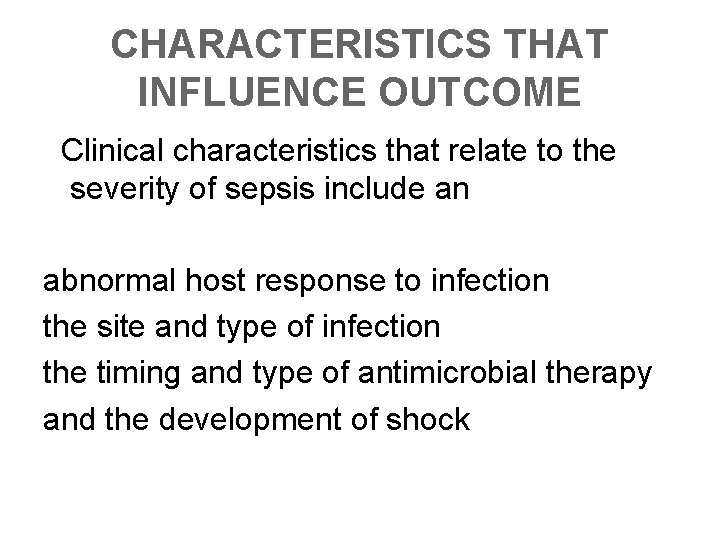
CHARACTERISTICS THAT INFLUENCE OUTCOME Clinical characteristics that relate to the severity of sepsis include an abnormal host response to infection the site and type of infection the timing and type of antimicrobial therapy and the development of shock
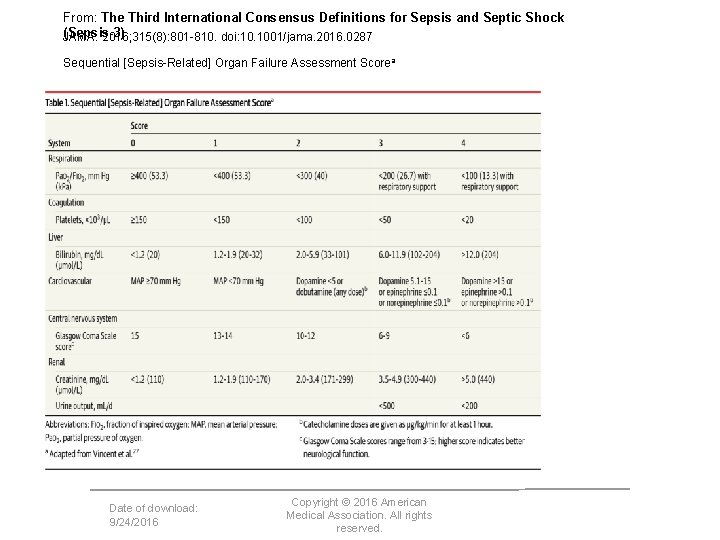
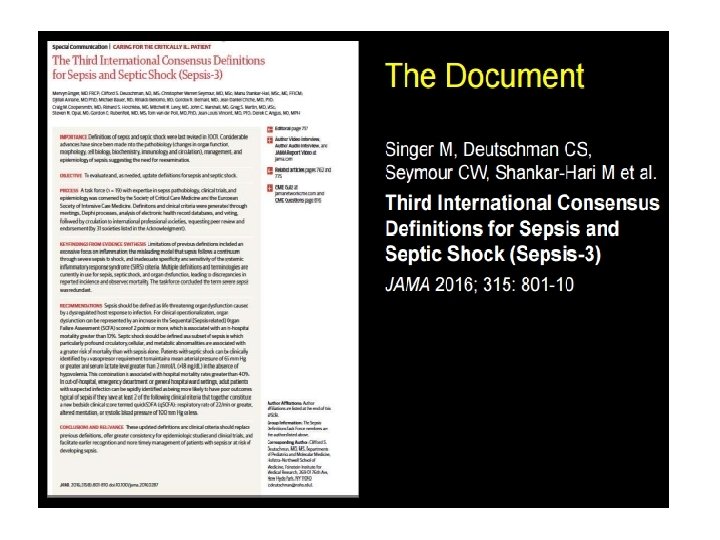
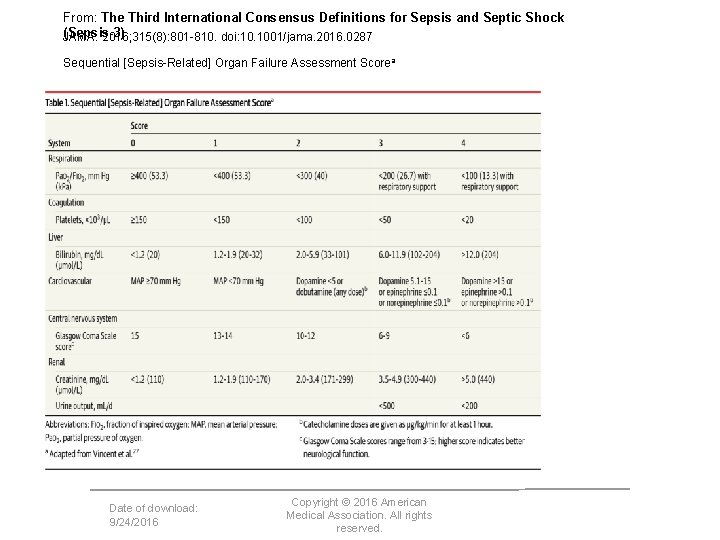
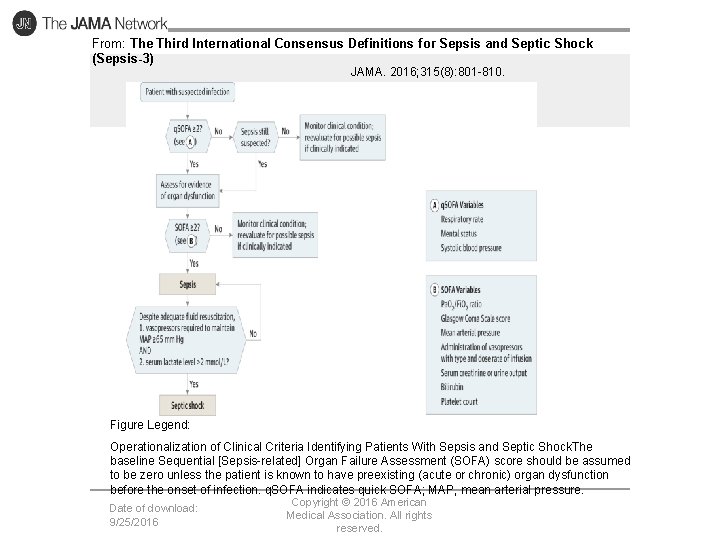
From: The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016; 315(8): 801 -810. doi: 10. 1001/jama. 2016. 0287 Sequential [Sepsis-Related] Organ Failure Assessment Scorea Date of download: 9/24/2016 Copyright © 2016 American Medical Association. All rights reserved.
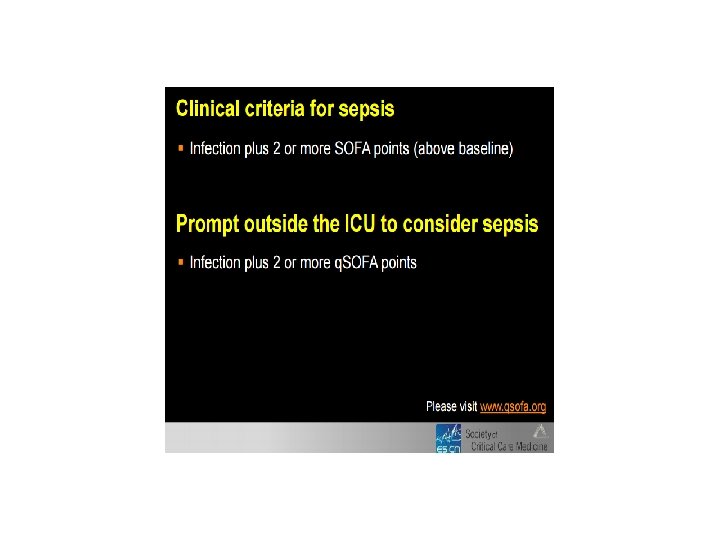
• Depending on a patient’s baseline level of risk, a SOFA score of 2 or greater identified a 2 - to 25 -fold increased risk of dying compared with patients with a SOFA score less than 2
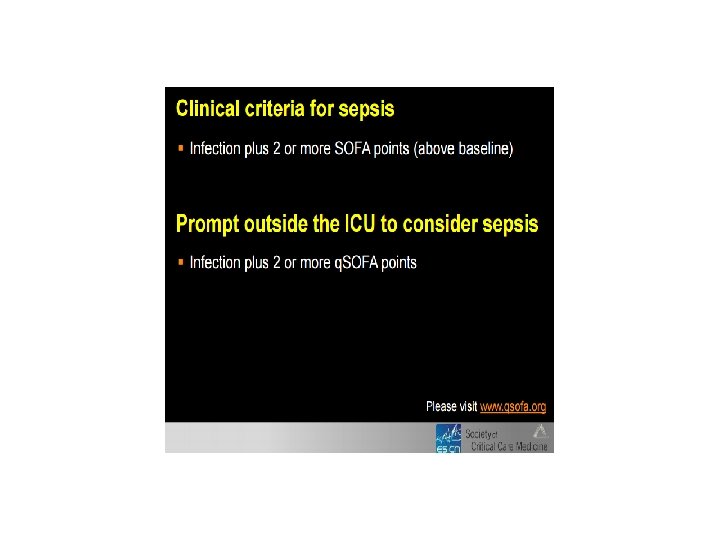
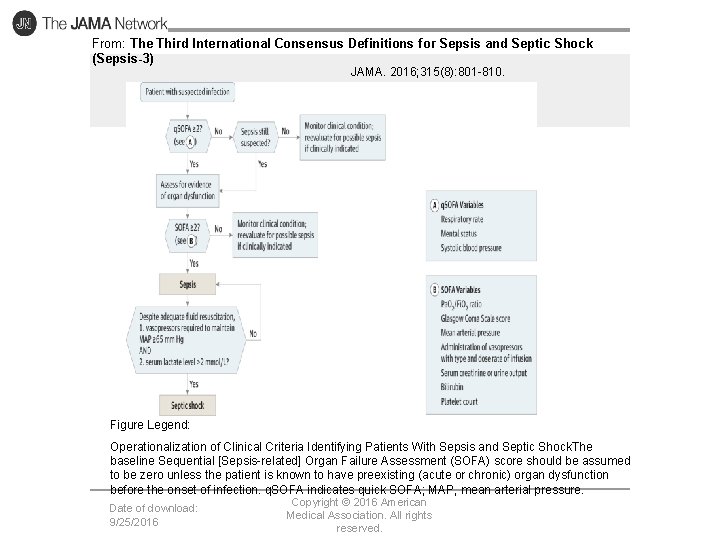
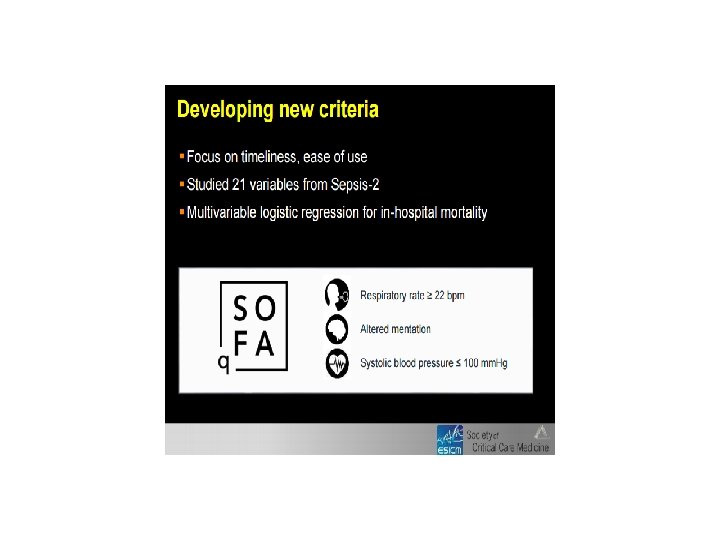
From: The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3) JAMA. 2016; 315(8): 801 -810. doi: 10. 1001/jama. 2016. 0287 Figure Legend: Operationalization of Clinical Criteria Identifying Patients With Sepsis and Septic Shock. The baseline Sequential [Sepsis-related] Organ Failure Assessment (SOFA) score should be assumed to be zero unless the patient is known to have preexisting (acute or chronic) organ dysfunction before the onset of infection. q. SOFA indicates quick SOFA; MAP, mean arterial pressure. Date of download: 9/25/2016 Copyright © 2016 American Medical Association. All rights reserved.
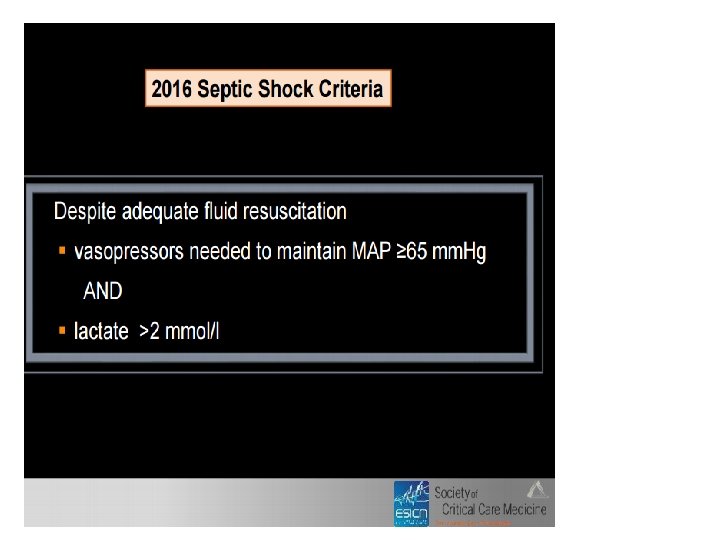
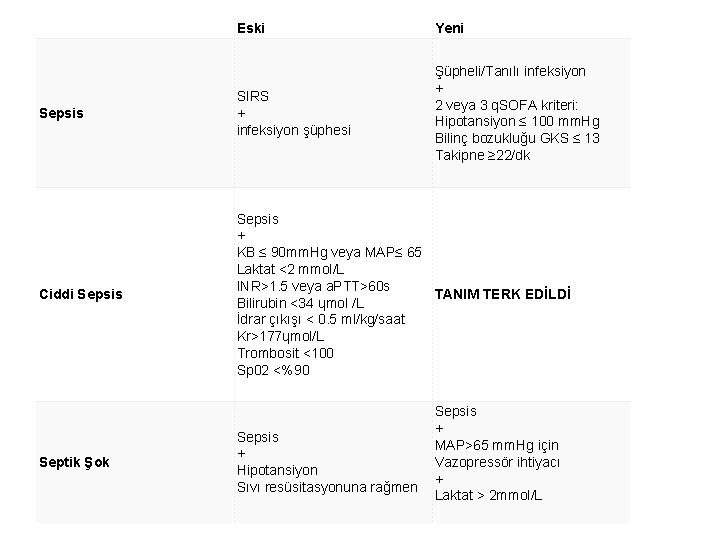
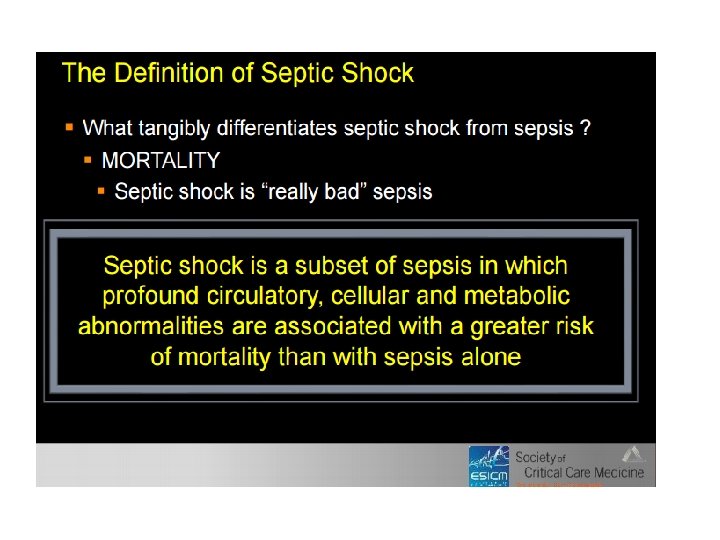
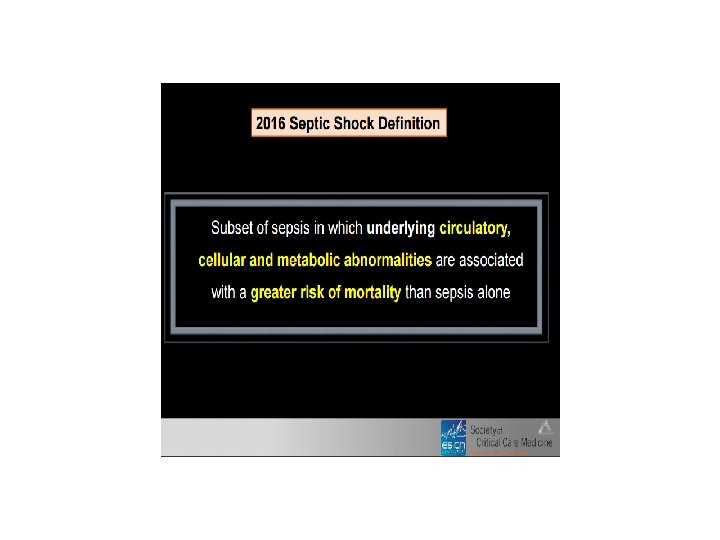
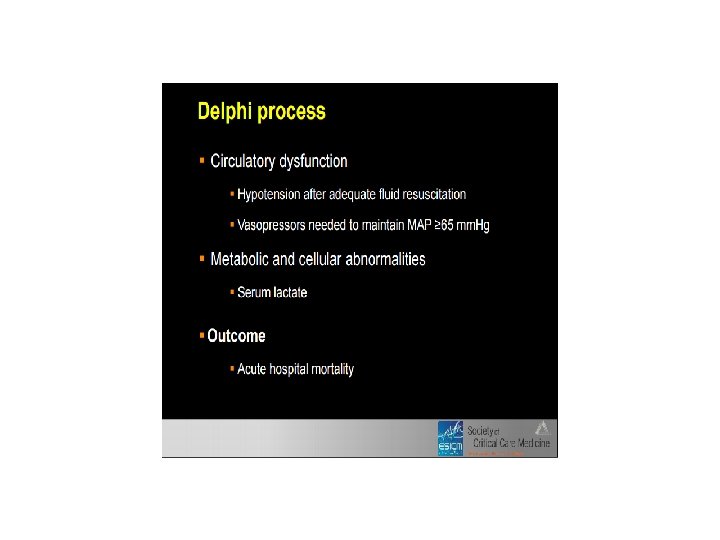
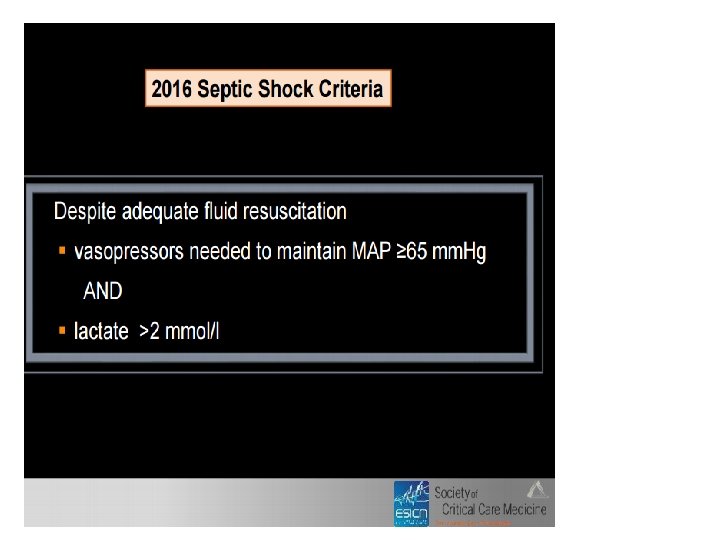
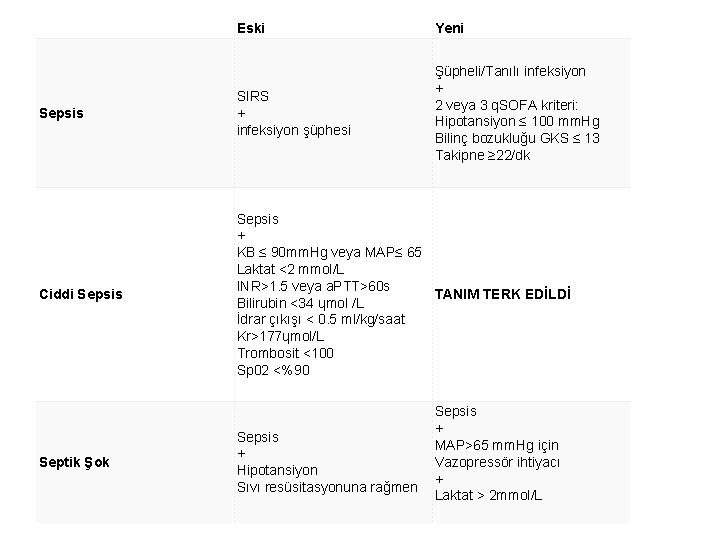
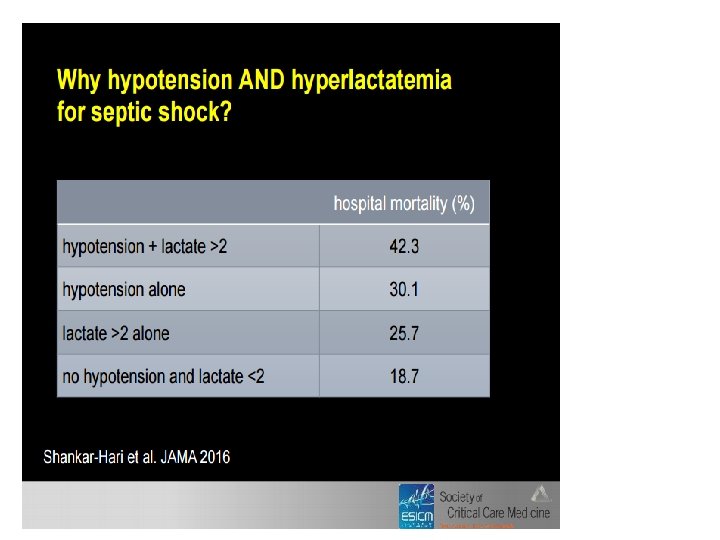
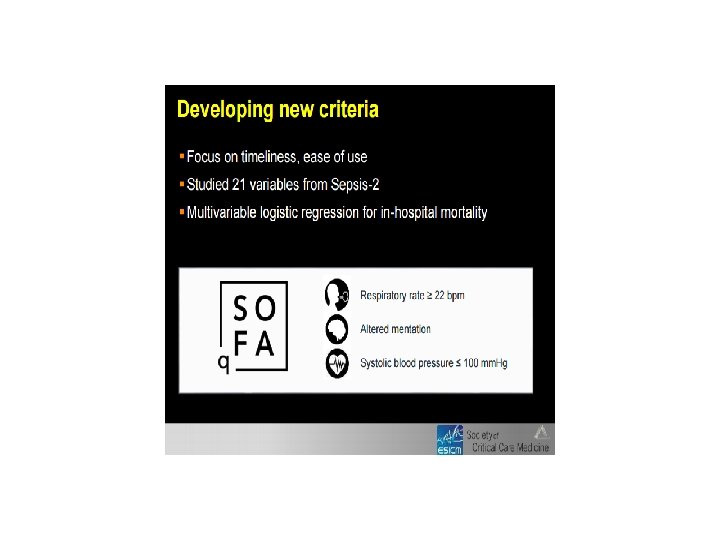
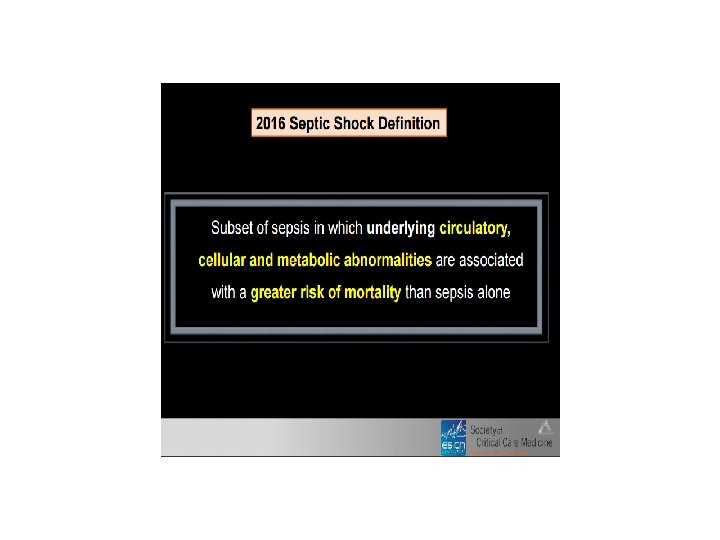
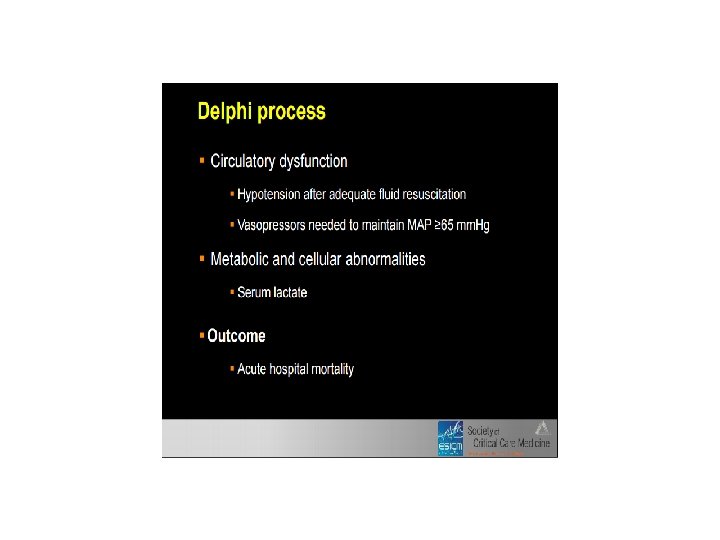
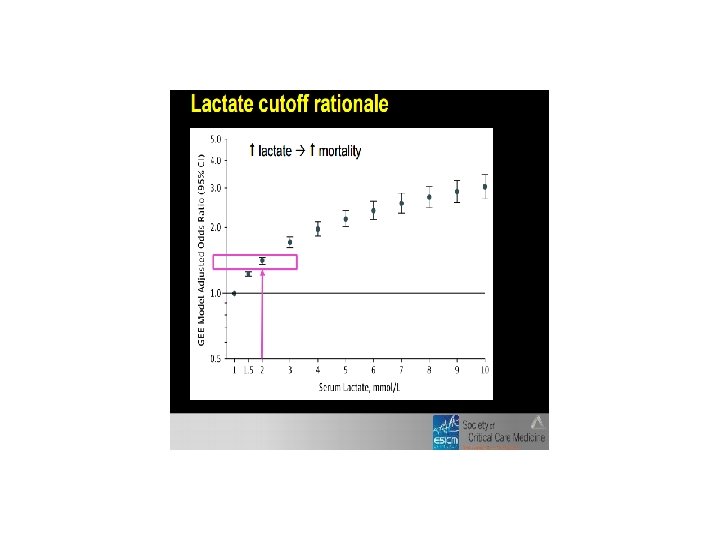
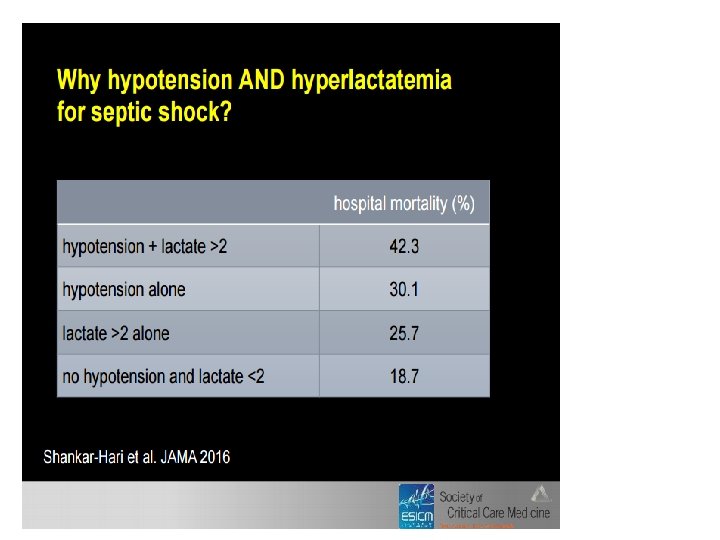
Eski Yeni Sepsis SIRS + infeksiyon şüphesi Şüpheli/Tanılı infeksiyon + 2 veya 3 q. SOFA kriteri: Hipotansiyon ≤ 100 mm. Hg Bilinç bozukluğu GKS ≤ 13 Takipne ≥ 22/dk Ciddi Sepsis + KB ≤ 90 mm. Hg veya MAP≤ 65 Laktat <2 mmol/L INR>1. 5 veya a. PTT>60 s TANIM TERK EDİLDİ Bilirubin <34 ɥmol /L İdrar çıkışı < 0. 5 ml/kg/saat Kr>177ɥmol/L Trombosit <100 Sp 02 <%90 Septik Şok Sepsis + Hipotansiyon Sıvı resüsitasyonuna rağmen Sepsis + MAP>65 mm. Hg için Vazopressör ihtiyacı + Laktat > 2 mmol/L
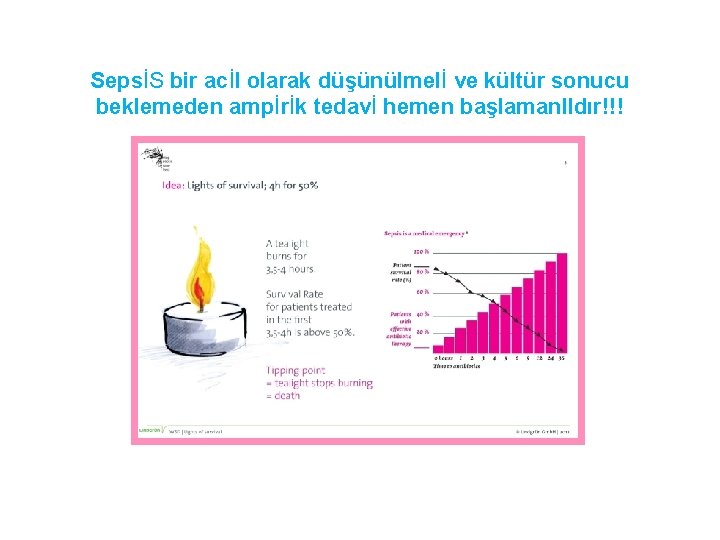
• 2 veya daha fazla semptom? • Sepsisten şüpheleniyorsan hızlı hareket et!!! • Her 1 saat mortaliteyi yaklaşık %8 düşürür…
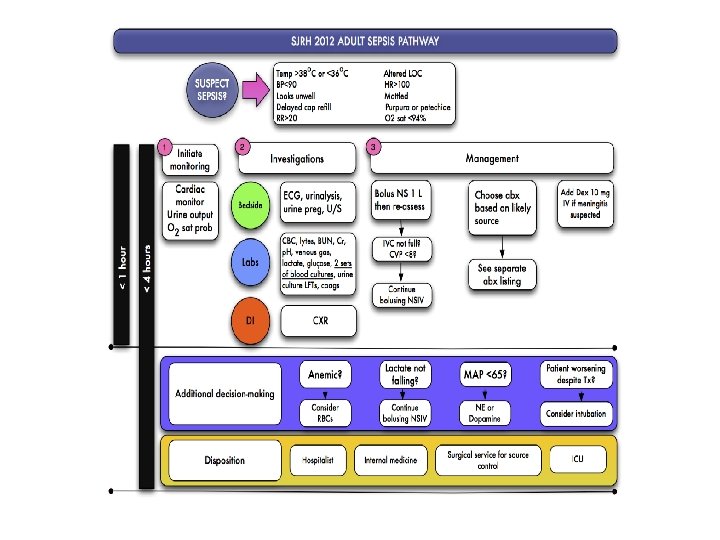
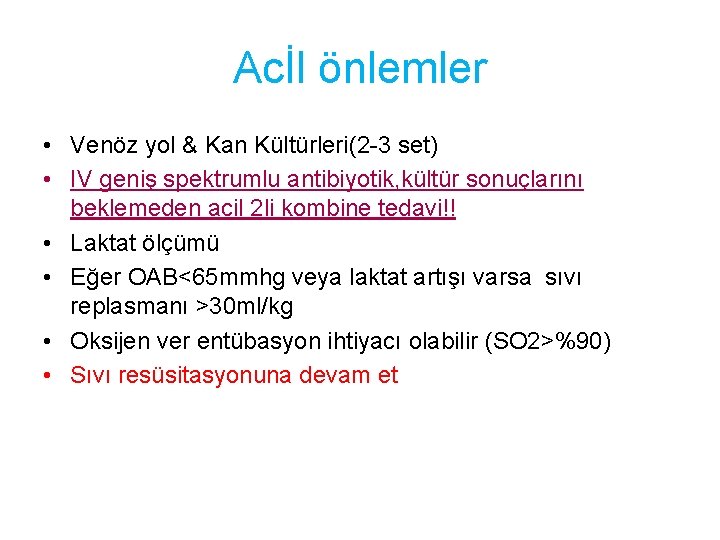
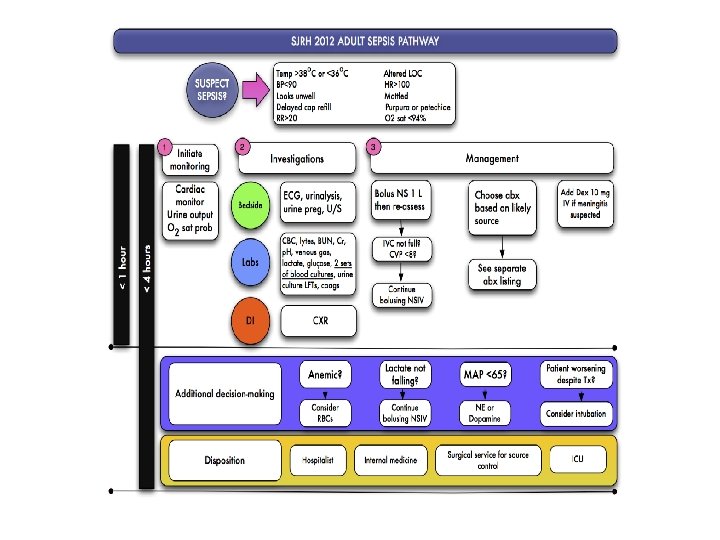
Acİl önlemler • Venöz yol & Kan Kültürleri(2 -3 set) • IV geniş spektrumlu antibiyotik, kültür sonuçlarını beklemeden acil 2 li kombine tedavi!! • Laktat ölçümü • Eğer OAB<65 mmhg veya laktat artışı varsa sıvı replasmanı >30 ml/kg • Oksijen ver entübasyon ihtiyacı olabilir (SO 2>%90) • Sıvı resüsitasyonuna devam et
Tedavinin amaci • • • SVP >8 mm. Hg OAB >65 mm. Hg (noradrenalin düşün) Scv. O 2 >%70 İdrar çıkımı >0. 5 ml/kg/saat Laktatın normale dönmesi Kaynağın tespiti ve kontrolü
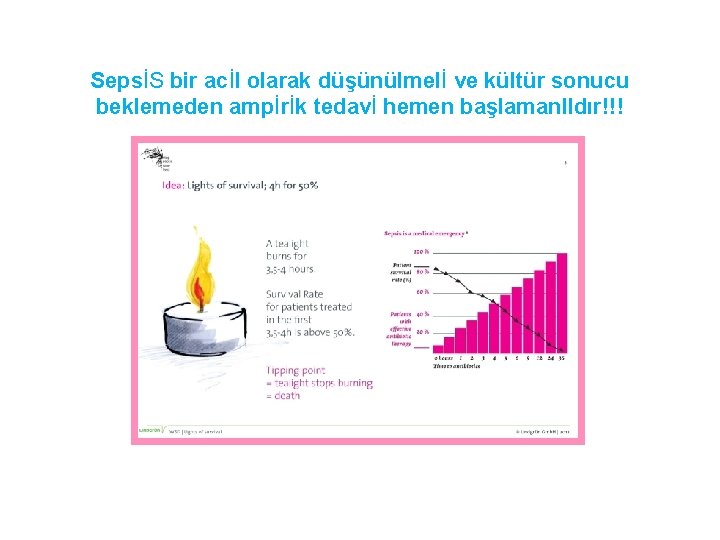
SepsİS bir acİl olarak düşünülmelİ ve kültür sonucu beklemeden ampİrİk tedavİ hemen başlamanl. Idır!!!
if Pseudomonas is an unlikely pathogen, we favor combining vancomycin with one of the following: • Cephalosporin, 3 rd or 4 th generation (eg, ceftriaxone or cefotaxime), or • Beta-lactam/beta-lactamase inhibitor (eg, piperacillintazobactam, ticarcillin-clavulanate), or • Carbapenem (eg, imipenem or meropenem).
Alternatively, if Pseudomonas is a possible pathogen, we combine vancomycin with two of the following • Antipseudomonal cephalosporin (eg, ceftazidime, cefepime), or • Antipseudomonal carbapenem (eg, imipenem, meropenem), or • Antipseudomonal beta-lactam/beta-lactamase inhibitor (eg, piperacillin-tazobactam, ticarcillin-clavulanate), or • Fluoroquinolone with good anti-pseudomonal activity (eg, ciprofloxacin), or • Aminoglycoside (eg, gentamicin, amikacin), or • Monobactam (eg, aztreonam)
Antibiotics Cultures / Antibiotics / Labs Cultures PRIOR to Antibiotics ( 2 Sets, one peripheral and one from any line older than 48 hrs) IV Abx within 3 hrs in the ED, within 1 hr in the ICU Broad Spectrum, combination therapy for neutropenic and patients with pseudomonas risk factors Vancomycin PLUS ……. Consider need for Source Control ! Drainage of abscess or cholangitis, removal of infected catheters, debridement or amputation of osteomyelitis
Once the patient's respiratory status has been stabilized, the adequacy of perfusion should be assessed. • Hypotension is the most common indicator that perfusion is inadequate. • However, critical hypoperfusion can also occur in the absence of hypotension, especially during early sepsis. • Common signs of hypoperfusion include cool, vasoconstricted skin due to redirection of blood flow to core organs (although warm, flushed skin may be present in the early phases of sepsis), obtundation or restlessness, oliguria or anuria, and lactic acidosis.
Once it has been established that hypoperfusion exists, early restoration of perfusion is necessary to prevent or limit multiple organ dysfunction, as well as reduce mortality • Tissue perfusion should be promptly restored using intravenous fluids, vasopressors, red blood cell transfusions, and inotropes • We recommend patients be managed with therapy aimed at achieving a central (or mixed) venous oxygen saturation ≥ 70 percent within six hours of presentation • It is reasonable to simultaneously aim for a central venous pressure 8 to 12 mm. Hg, • mean arterial pressure (MAP) ≥ 65 mm. Hg, • urine output ≥ 0. 5 m. L per kg per hour.
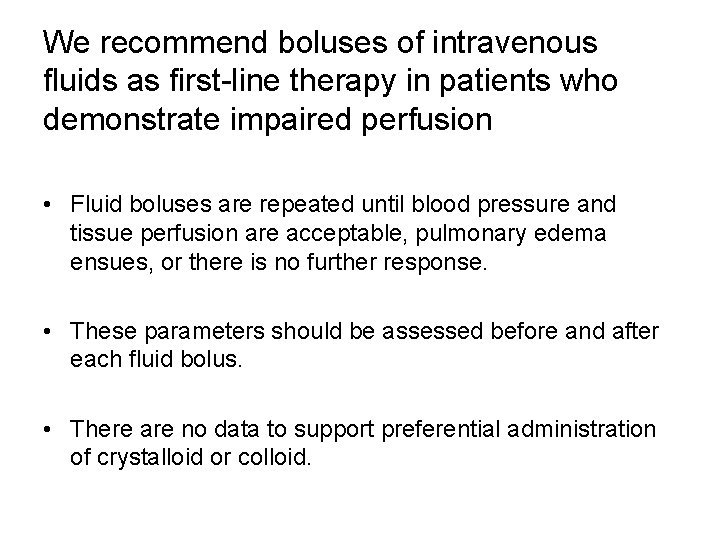
We recommend boluses of intravenous fluids as first-line therapy in patients who demonstrate impaired perfusion • Fluid boluses are repeated until blood pressure and tissue perfusion are acceptable, pulmonary edema ensues, or there is no further response. • These parameters should be assessed before and after each fluid bolus. • There are no data to support preferential administration of crystalloid or colloid.
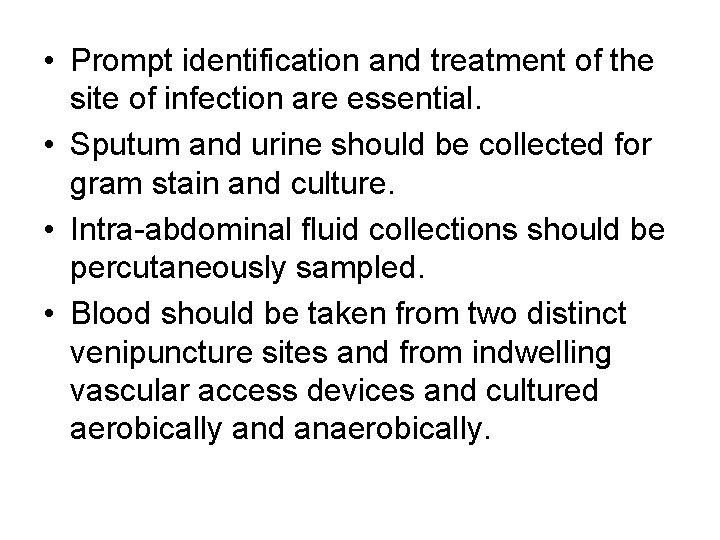
• Prompt identification and treatment of the site of infection are essential. • Sputum and urine should be collected for gram stain and culture. • Intra-abdominal fluid collections should be percutaneously sampled. • Blood should be taken from two distinct venipuncture sites and from indwelling vascular access devices and cultured aerobically and anaerobically.
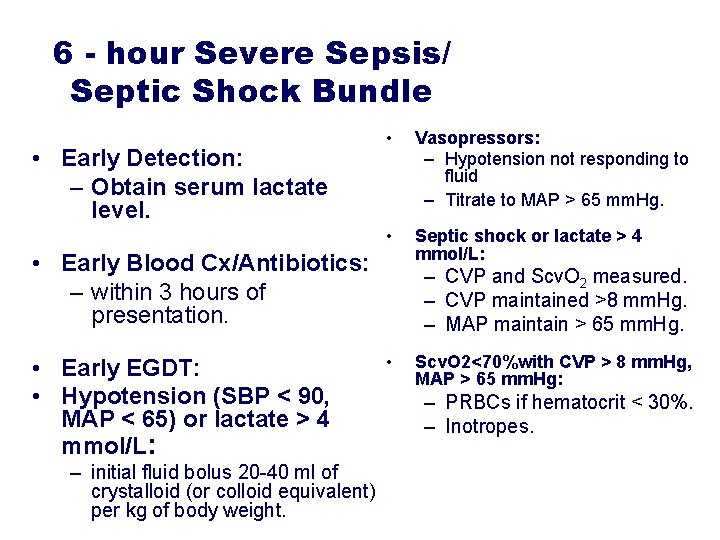
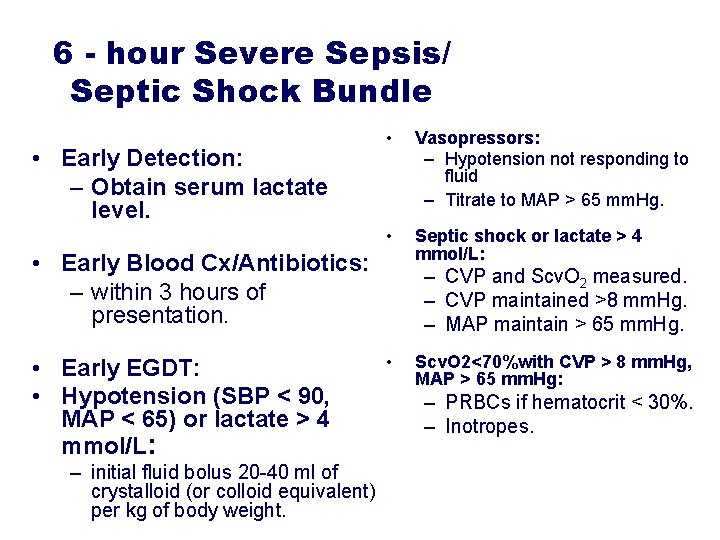
6 - hour Severe Sepsis/ Septic Shock Bundle • Early Detection: – Obtain serum lactate level. • Vasopressors: – Hypotension not responding to fluid – Titrate to MAP > 65 mm. Hg. • Septic shock or lactate > 4 mmol/L: • Early Blood Cx/Antibiotics: – within 3 hours of presentation. • Early EGDT: • Hypotension (SBP < 90, MAP < 65) or lactate > 4 mmol/L: – initial fluid bolus 20 -40 ml of crystalloid (or colloid equivalent) per kg of body weight. – CVP and Scv. O 2 measured. – CVP maintained >8 mm. Hg. – MAP maintain > 65 mm. Hg. • Scv. O 2<70%with CVP > 8 mm. Hg, MAP > 65 mm. Hg: – PRBCs if hematocrit < 30%. – Inotropes.
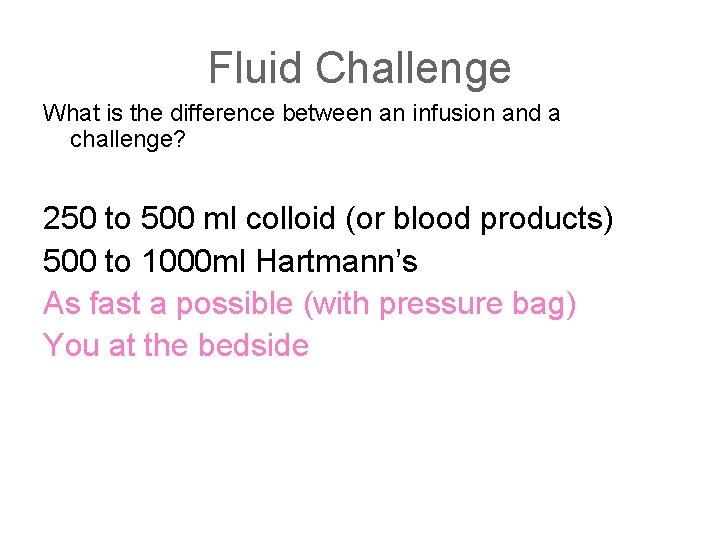
Fluid Challenge What is the difference between an infusion and a challenge? 250 to 500 ml colloid (or blood products) 500 to 1000 ml Hartmann’s As fast a possible (with pressure bag) You at the bedside
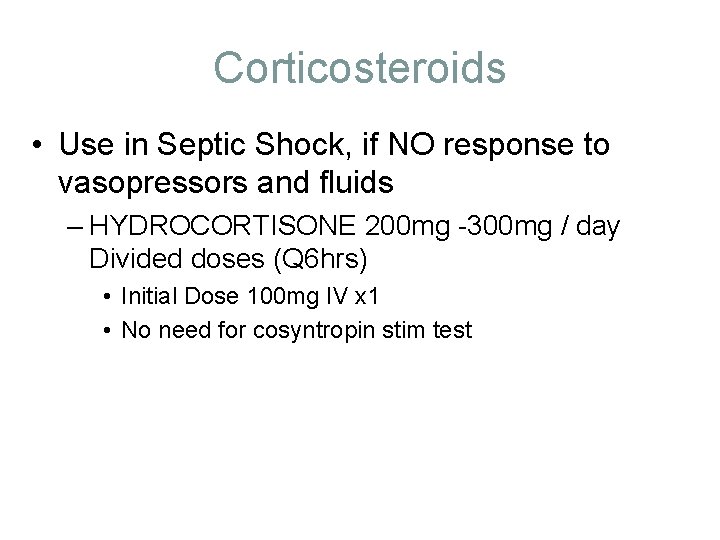
Corticosteroids • Use in Septic Shock, if NO response to vasopressors and fluids – HYDROCORTISONE 200 mg -300 mg / day Divided doses (Q 6 hrs) • Initial Dose 100 mg IV x 1 • No need for cosyntropin stim test
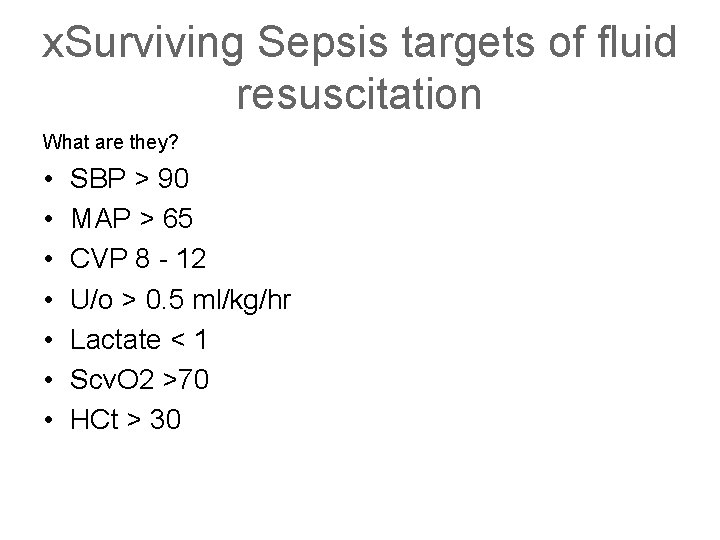
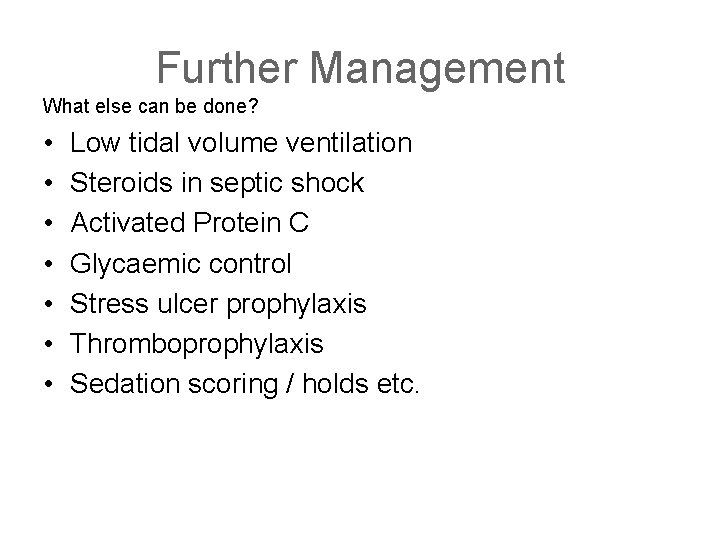
x. Surviving Sepsis targets of fluid resuscitation What are they? • • SBP > 90 MAP > 65 CVP 8 - 12 U/o > 0. 5 ml/kg/hr Lactate < 1 Scv. O 2 >70 HCt > 30
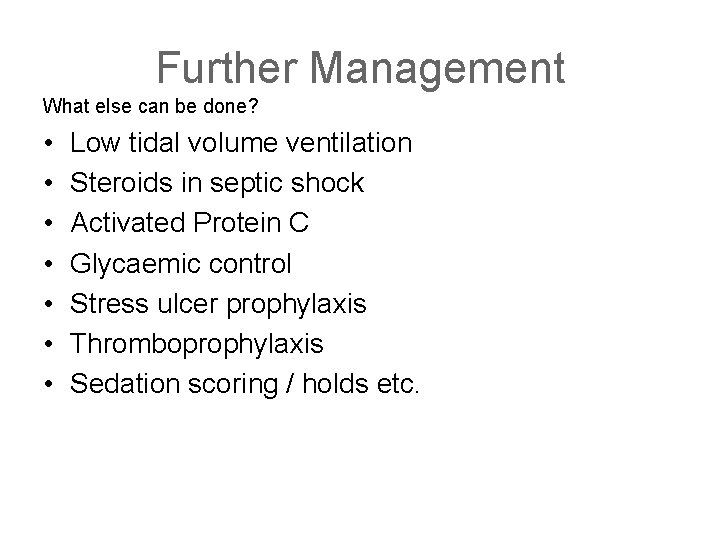
Further Management What else can be done? • • Low tidal volume ventilation Steroids in septic shock Activated Protein C Glycaemic control Stress ulcer prophylaxis Thromboprophylaxis Sedation scoring / holds etc.