Sepsis an update Dr Judith Joss MRCP FRCA



- Slides: 35
Sepsis- an update Dr Judith Joss MRCP, FRCA, DICM, FICM Consultant in Anaesthesia and Intensive Care Medicine Ninewells Hospital and Medical School, Dundee Maternal Critical Care Symposium 2016
‘SEPSIS 3’ The Third International Consensus Definitions for Sepsis and Septic Shock SCCM, ESICM taskforce JAMA. 2016; 315(8): 801 -810
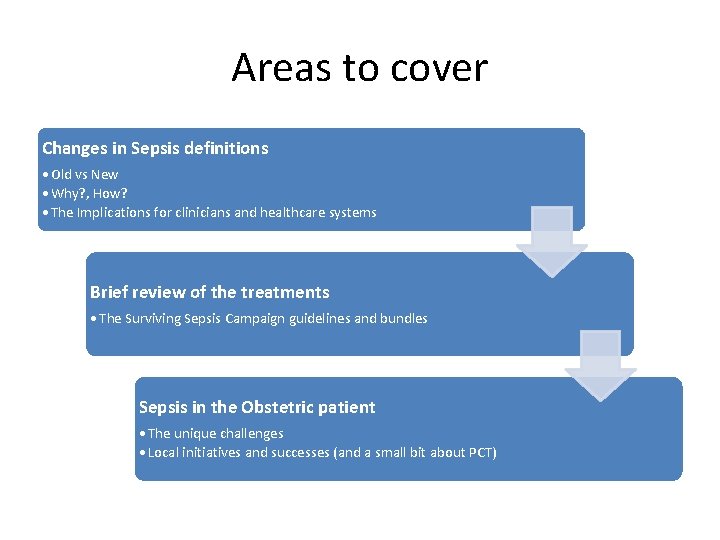
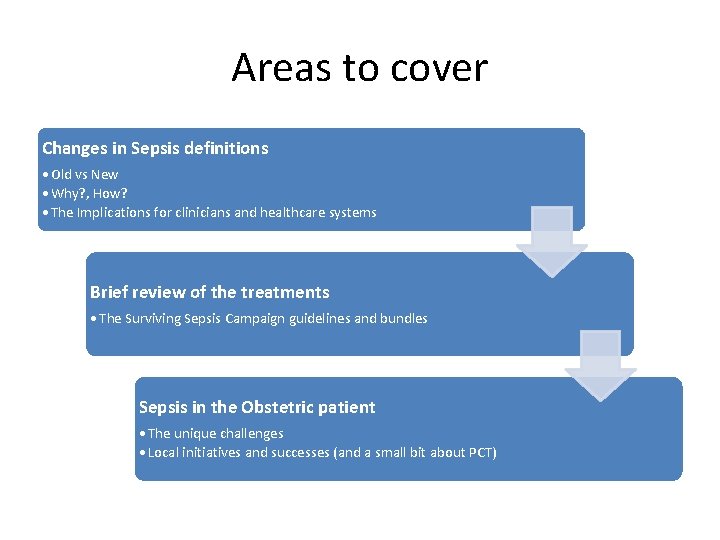
Areas to cover Changes in Sepsis definitions • Old vs New • Why? , How? • The Implications for clinicians and healthcare systems Brief review of the treatments • The Surviving Sepsis Campaign guidelines and bundles Sepsis in the Obstetric patient • The unique challenges • Local initiatives and successes (and a small bit about PCT)
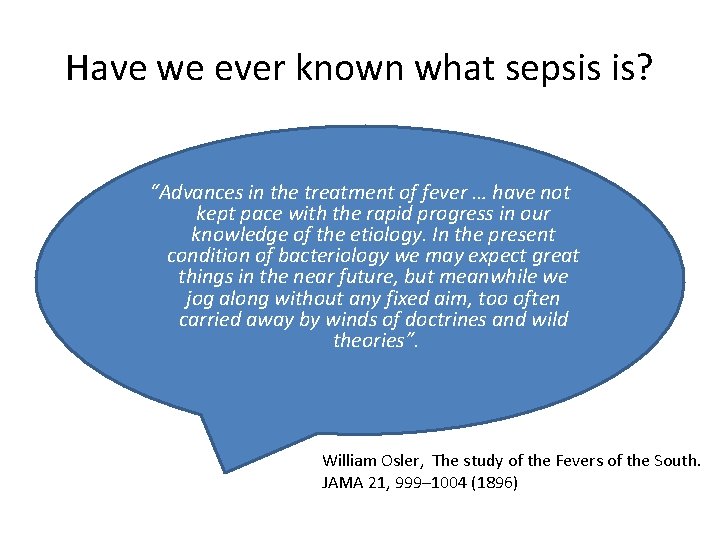
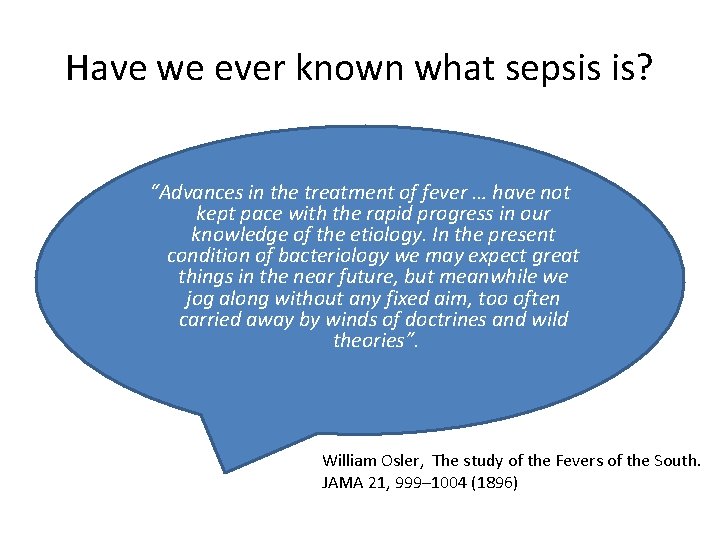
Have we ever known what sepsis is? “Advances in the treatment of fever … have not kept pace with the rapid progress in our knowledge of the etiology. In the present condition of bacteriology we may expect great things in the near future, but meanwhile we jog along without any fixed aim, too often carried away by winds of doctrines and wild theories”. William Osler, The study of the Fevers of the South. JAMA 21, 999– 1004 (1896)
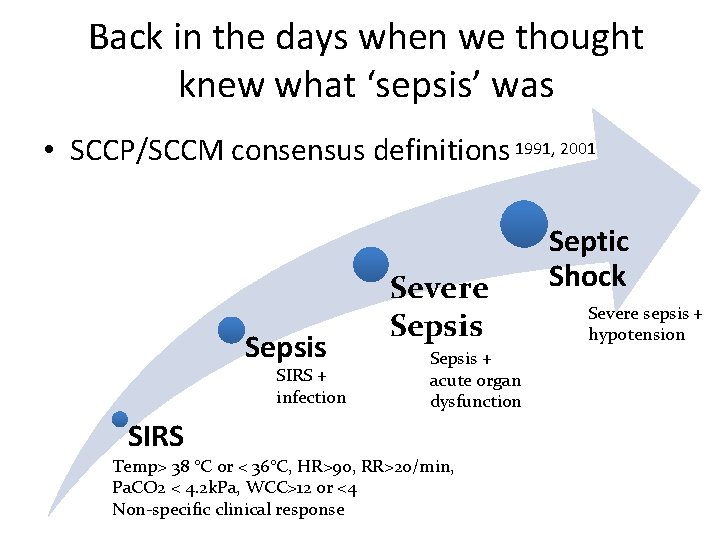
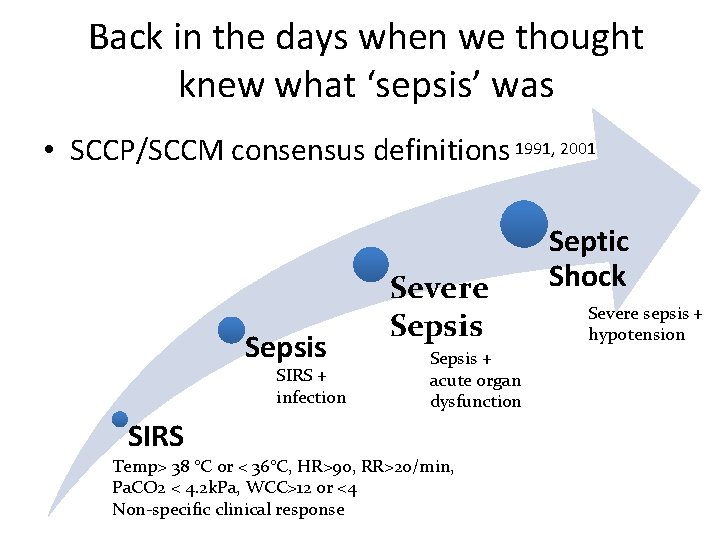
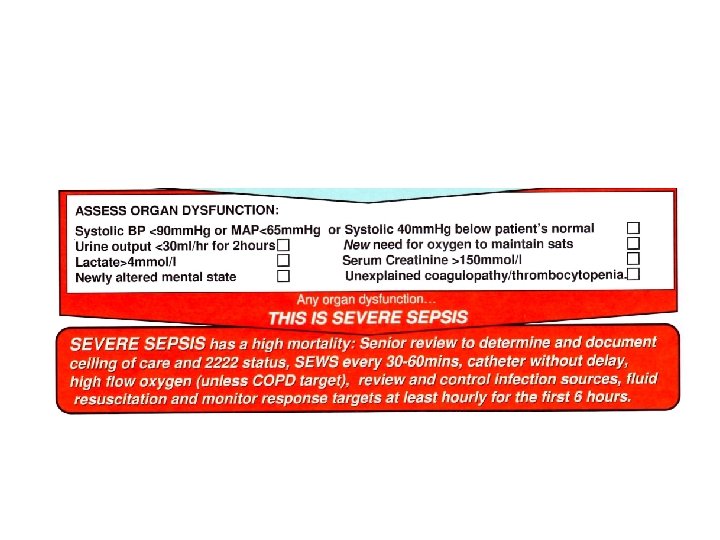
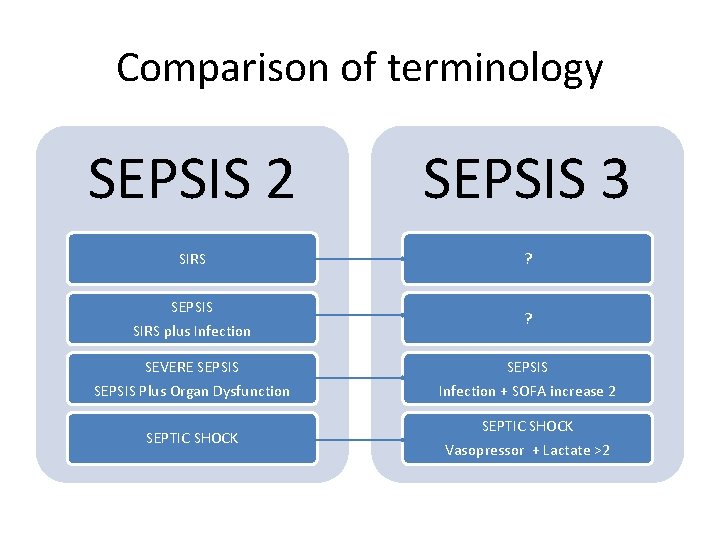
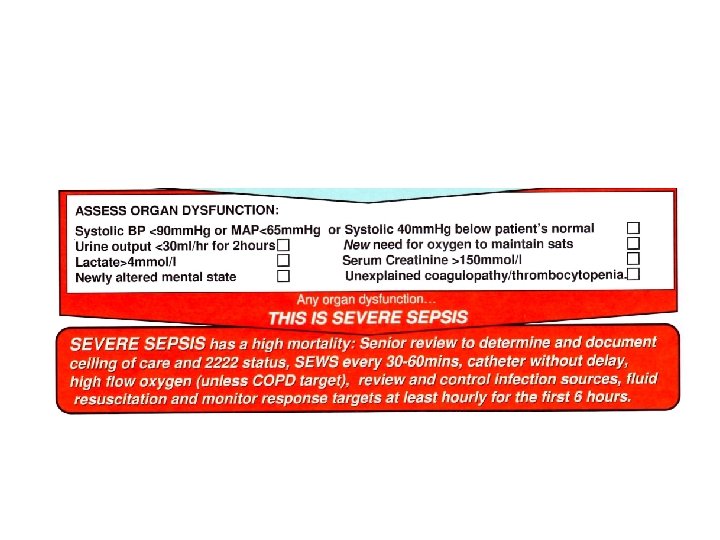
Back in the days when we thought knew what ‘sepsis’ was • SCCP/SCCM consensus definitions 1991, 2001 Sepsis SIRS + infection SIRS Severe Sepsis + acute organ dysfunction Temp> 38 °C or < 36°C, HR>90, RR>20/min, Pa. CO 2 < 4. 2 k. Pa, WCC>12 or <4 Non-specific clinical response Septic Shock Severe sepsis + hypotension

Did we need a new definition? SIRS • Overly non specific • 4: 5 patients with SIRS dont have infection • 1: 8 with infection causing organ dysfunction dont have SIRS • Greater understanding New of science of infection, knowledge cell biology and organ dysfunction Research • We had a research problem!! With good evidence of inconsistencies in terminology
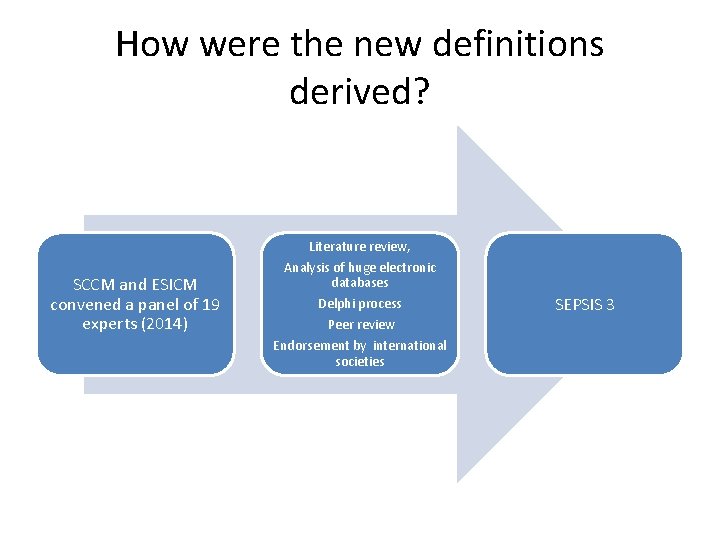
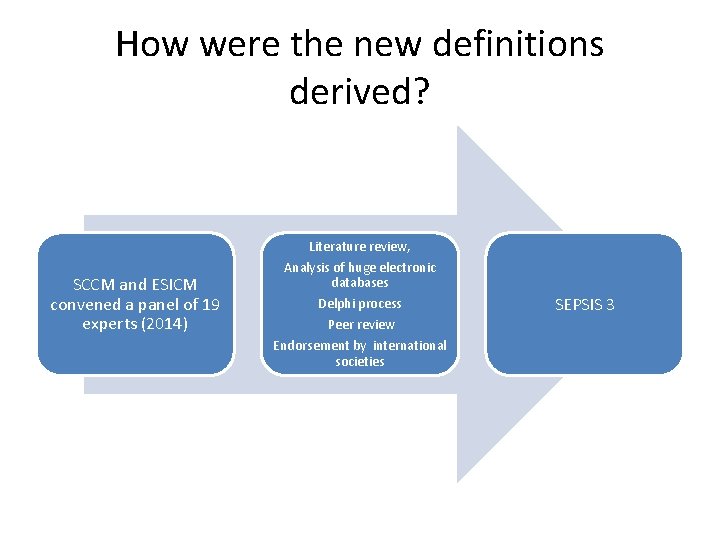
How were the new definitions derived? Literature review, SCCM and ESICM convened a panel of 19 experts (2014) Analysis of huge electronic databases Delphi process Peer review Endorsement by international societies SEPSIS 3
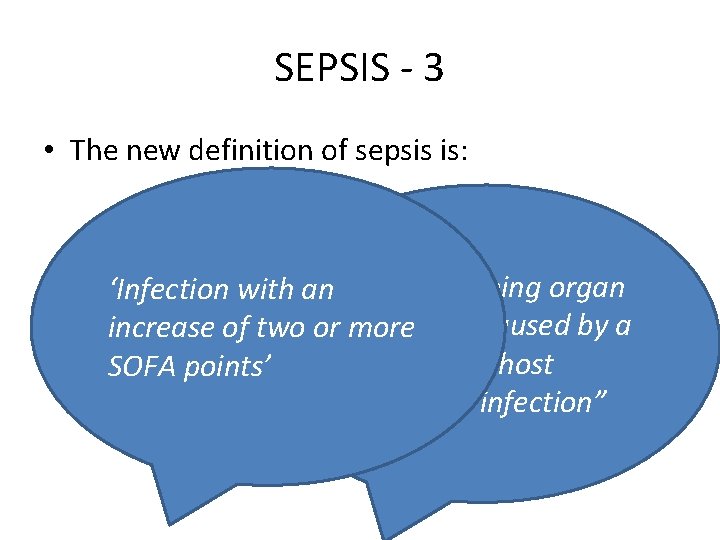
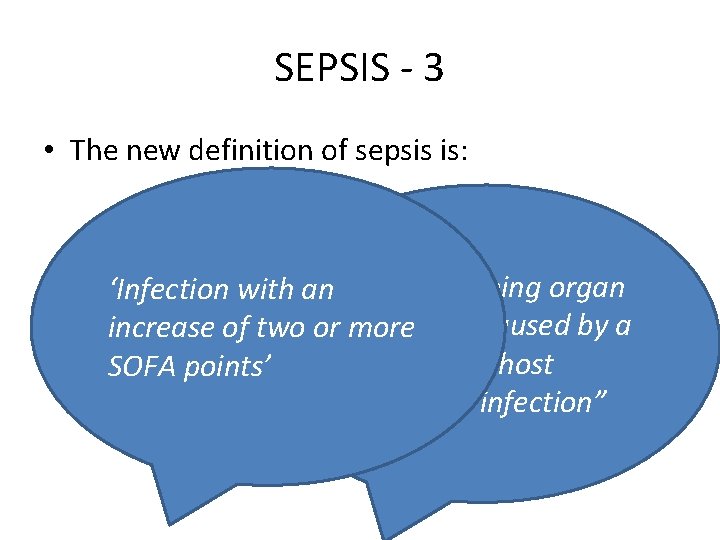
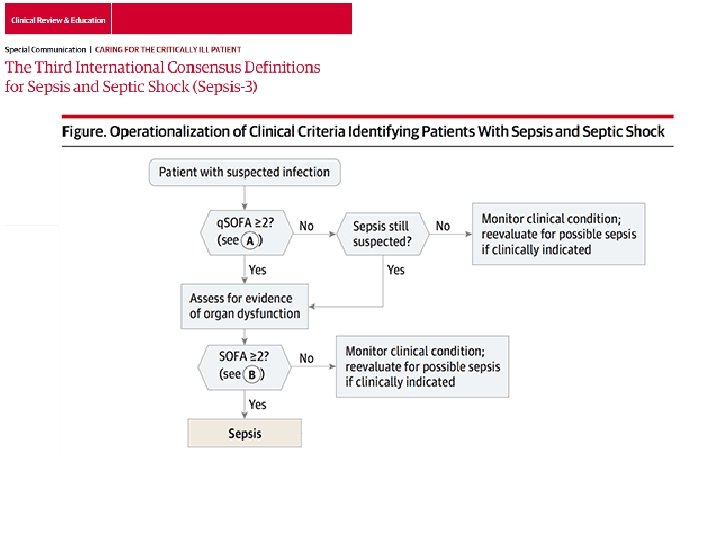
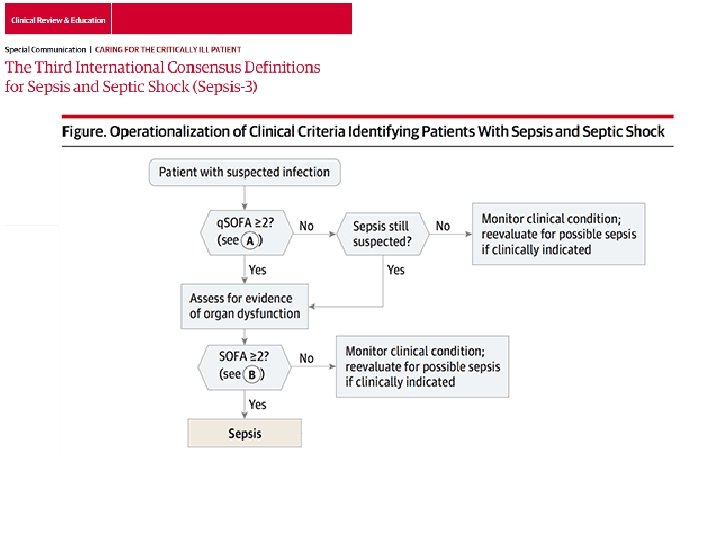
SEPSIS - 3 • The new definition of sepsis is: ‘Infection with an“Life threatening organ dysfunction caused by a increase of two or more dysregulated host SOFA points’ response to infection”
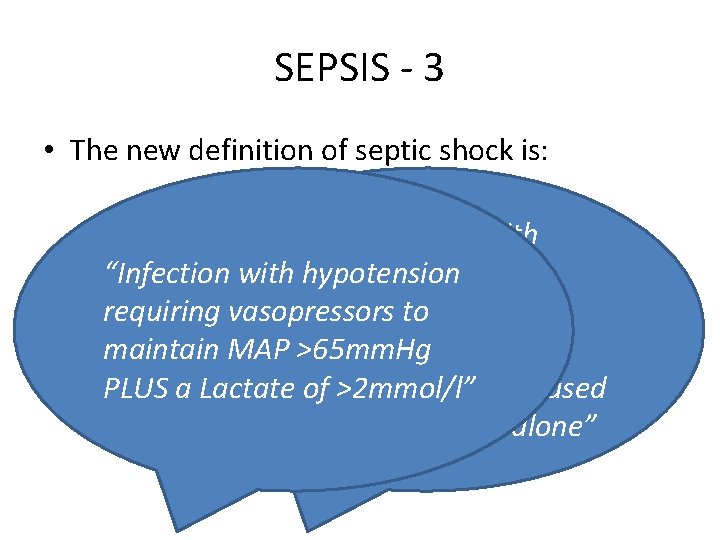
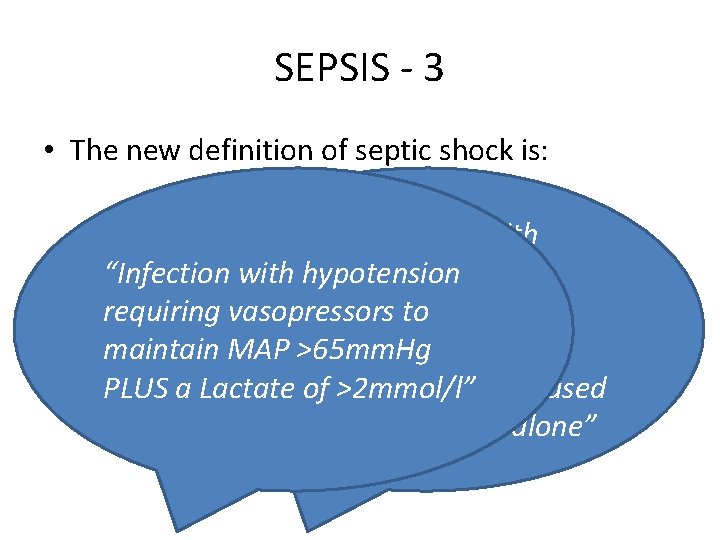
SEPSIS - 3 • The new definition of septic shock is: “A subset of sepsis with “Infection particularly with hypotension profound requiring vasopressors to circulatory, cellular and maintain MAP >65 mm. Hg metabolic abnormalities PLUS a Lactate associated of >2 mmol/l” with an increased mortality than sepsis alone”

SOFA SCORE
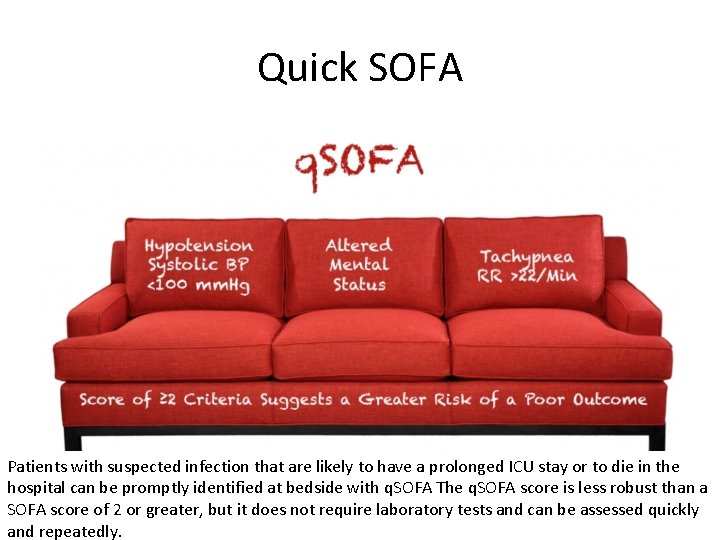
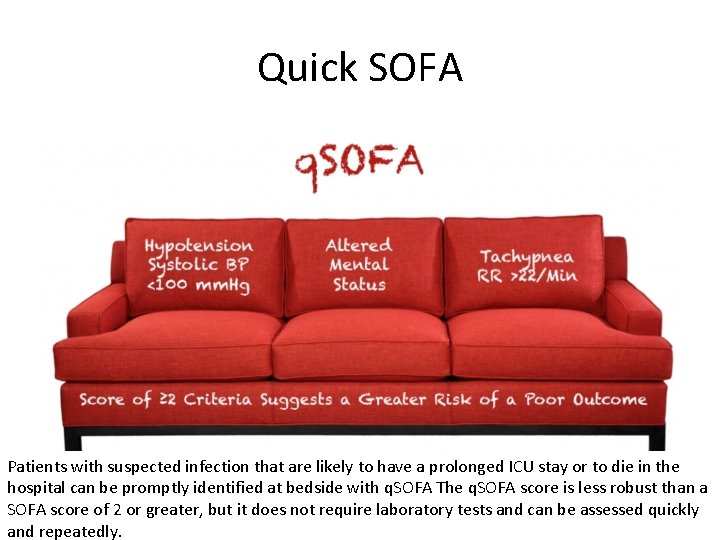
Quick SOFA Patients with suspected infection that are likely to have a prolonged ICU stay or to die in the hospital can be promptly identified at bedside with q. SOFA The q. SOFA score is less robust than a SOFA score of 2 or greater, but it does not require laboratory tests and can be assessed quickly and repeatedly.
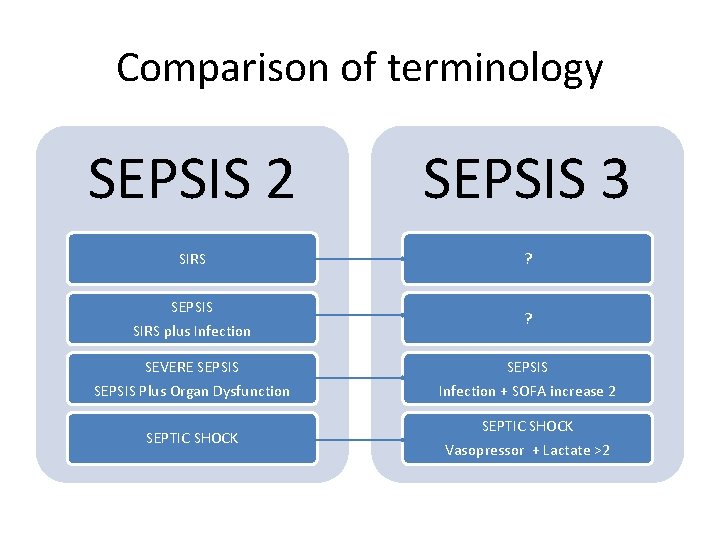
Comparison of terminology SEPSIS 2 SEPSIS 3 SIRS ? SEPSIS SIRS plus Infection ? SEVERE SEPSIS Plus Organ Dysfunction Infection + SOFA increase 2 SEPTIC SHOCK Vasopressor + Lactate >2
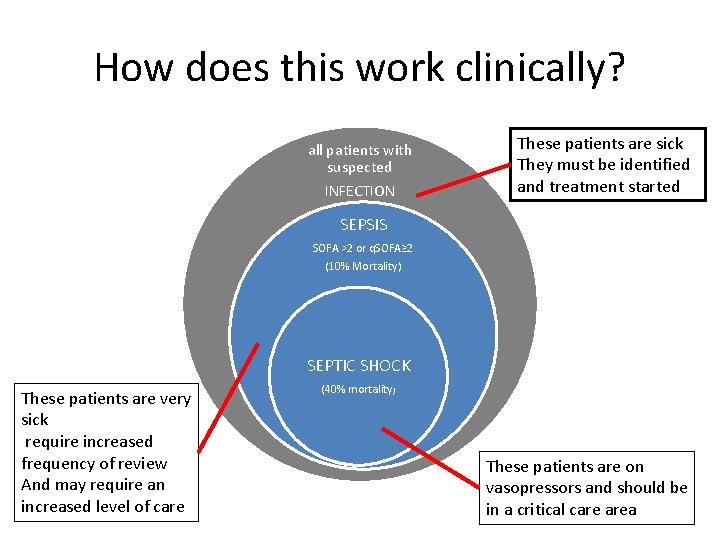
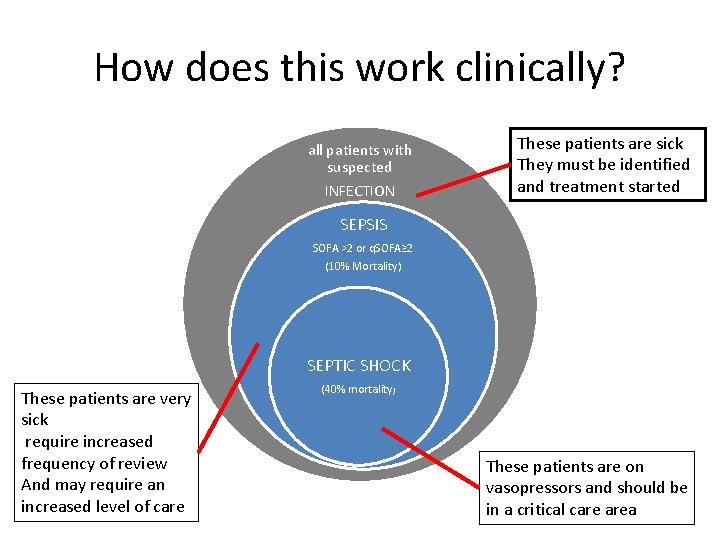
How does this work clinically? all patients with suspected INFECTION These patients are sick They must be identified and treatment started SEPSIS SOFA >2 or q. SOFA≥ 2 (10% Mortality) SEPTIC SHOCK These patients are very sick require increased frequency of review And may require an increased level of care (40% mortality) These patients are on vasopressors and should be in a critical care area
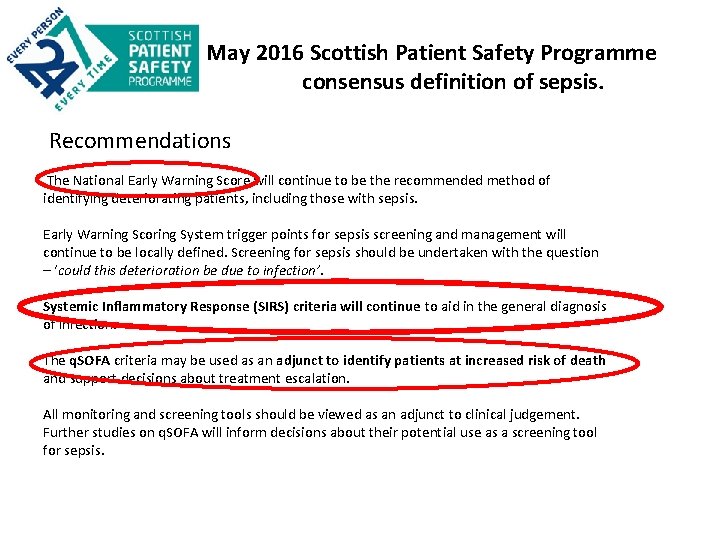
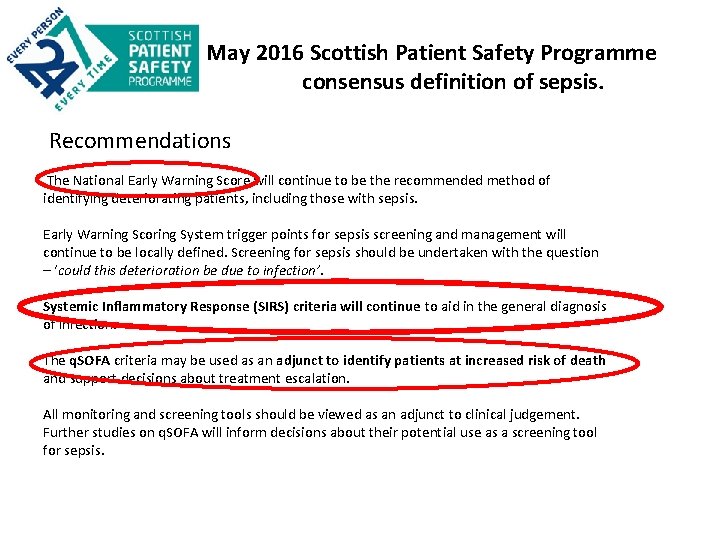
May 2016 Scottish Patient Safety Programme consensus definition of sepsis. Recommendations The National Early Warning Score will continue to be the recommended method of identifying deteriorating patients, including those with sepsis. Early Warning Scoring System trigger points for sepsis screening and management will continue to be locally defined. Screening for sepsis should be undertaken with the question – ‘could this deterioration be due to infection’. Systemic Inflammatory Response (SIRS) criteria will continue to aid in the general diagnosis of infection. The q. SOFA criteria may be used as an adjunct to identify patients at increased risk of death and support decisions about treatment escalation. All monitoring and screening tools should be viewed as an adjunct to clinical judgement. Further studies on q. SOFA will inform decisions about their potential use as a screening tool for sepsis.
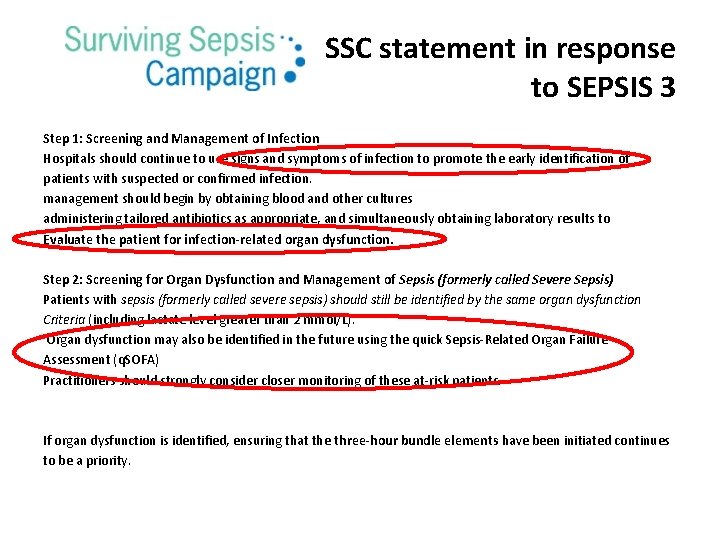
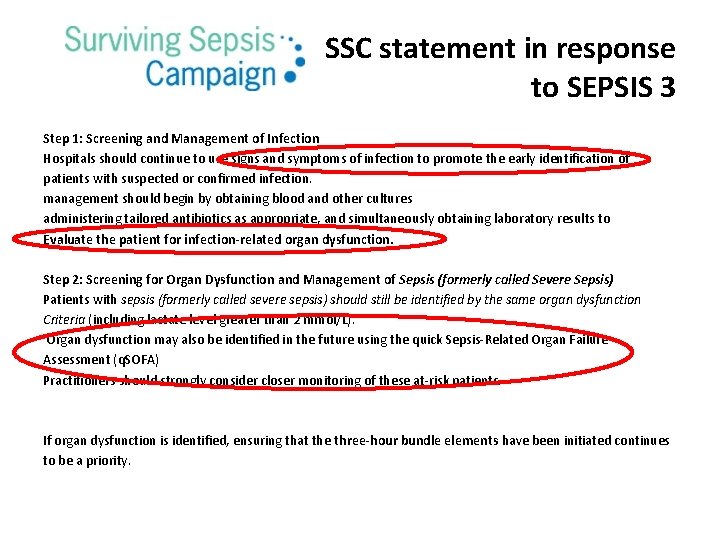
SSC statement in response to SEPSIS 3 Step 1: Screening and Management of Infection Hospitals should continue to use signs and symptoms of infection to promote the early identification of patients with suspected or confirmed infection. management should begin by obtaining blood and other cultures administering tailored antibiotics as appropriate, and simultaneously obtaining laboratory results to Evaluate the patient for infection-related organ dysfunction. Step 2: Screening for Organ Dysfunction and Management of Sepsis (formerly called Severe Sepsis) Patients with sepsis (formerly called severe sepsis) should still be identified by the same organ dysfunction Criteria (including lactate level greater than 2 mmol/L). Organ dysfunction may also be identified in the future using the quick Sepsis-Related Organ Failure Assessment (q. SOFA) Practitioners should strongly consider closer monitoring of these at-risk patients. If organ dysfunction is identified, ensuring that the three-hour bundle elements have been initiated continues to be a priority.
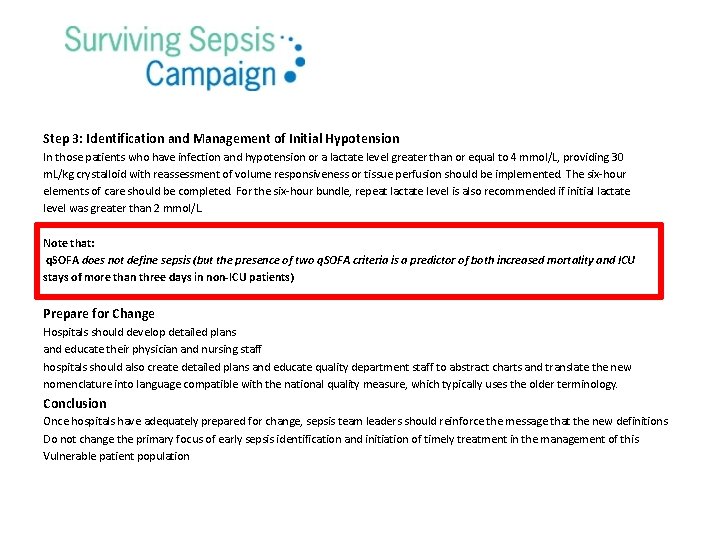
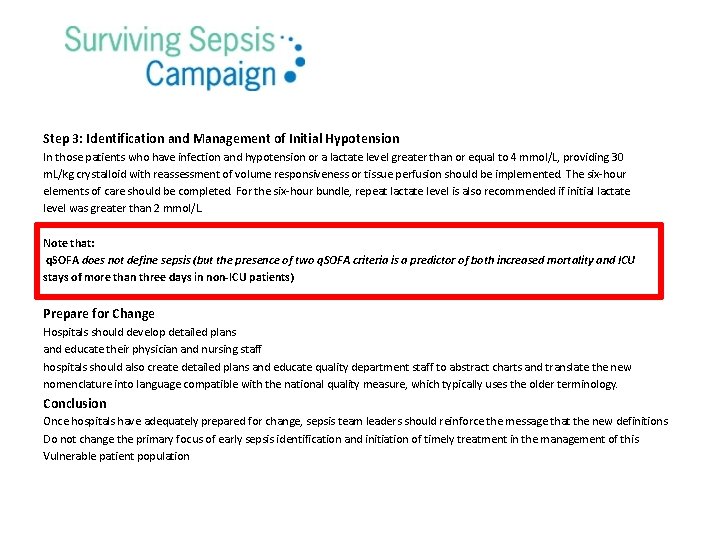
Step 3: Identification and Management of Initial Hypotension In those patients who have infection and hypotension or a lactate level greater than or equal to 4 mmol/L, providing 30 m. L/kg crystalloid with reassessment of volume responsiveness or tissue perfusion should be implemented. The six-hour elements of care should be completed. For the six-hour bundle, repeat lactate level is also recommended if initial lactate level was greater than 2 mmol/L. Note that: q. SOFA does not define sepsis (but the presence of two q. SOFA criteria is a predictor of both increased mortality and ICU stays of more than three days in non-ICU patients) Prepare for Change Hospitals should develop detailed plans and educate their physician and nursing staff hospitals should also create detailed plans and educate quality department staff to abstract charts and translate the new nomenclature into language compatible with the national quality measure, which typically uses the older terminology. Conclusion Once hospitals have adequately prepared for change, sepsis team leaders should reinforce the message that the new definitions Do not change the primary focus of early sepsis identification and initiation of timely treatment in the management of this Vulnerable patient population
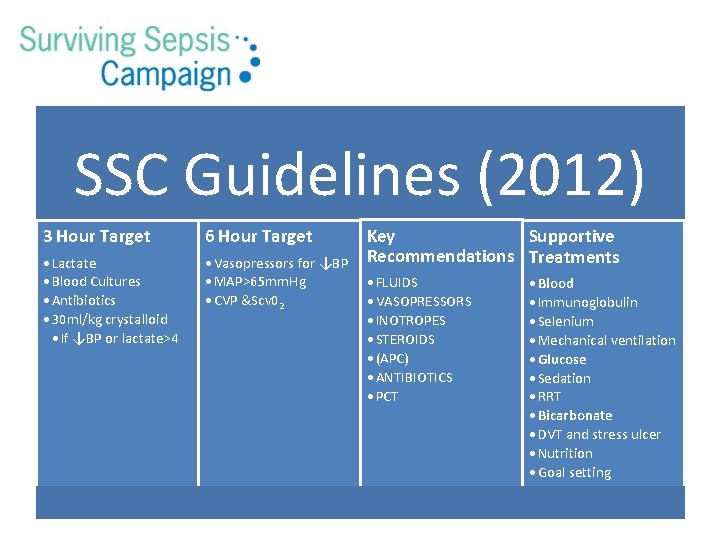
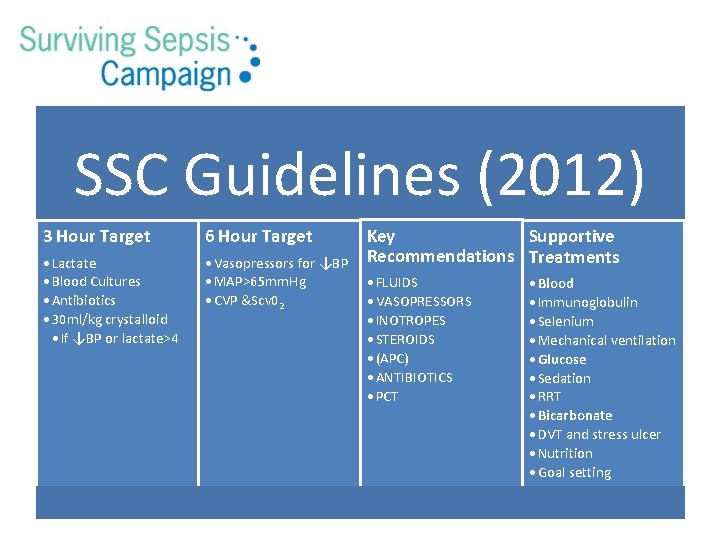
SSC Guidelines (2012) 3 Hour Target 6 Hour Target • Lactate • Blood Cultures • Antibiotics • 30 ml/kg crystalloid • If ↓BP or lactate>4 • Vasopressors for ↓BP • MAP>65 mm. Hg • CVP &Scv 02 Key Supportive Recommendations Treatments • FLUIDS • VASOPRESSORS • INOTROPES • STEROIDS • (APC) • ANTIBIOTICS • PCT • Blood • Immunoglobulin • Selenium • Mechanical ventilation • Glucose • Sedation • RRT • Bicarbonate • DVT and stress ulcer • Nutrition • Goal setting

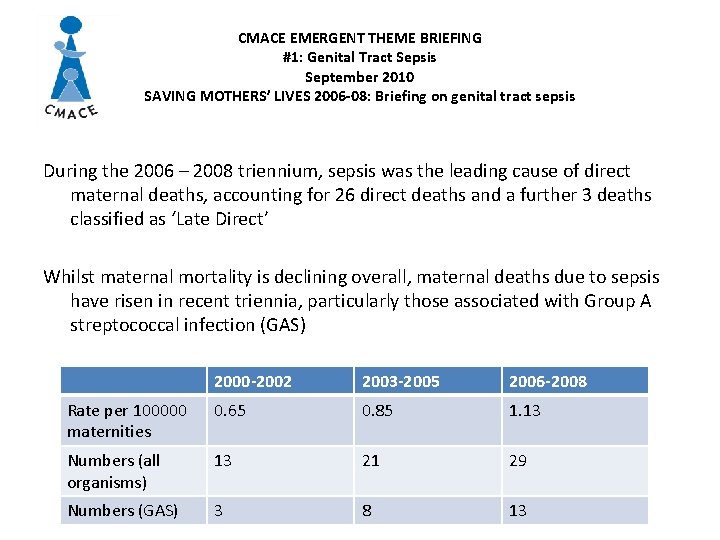
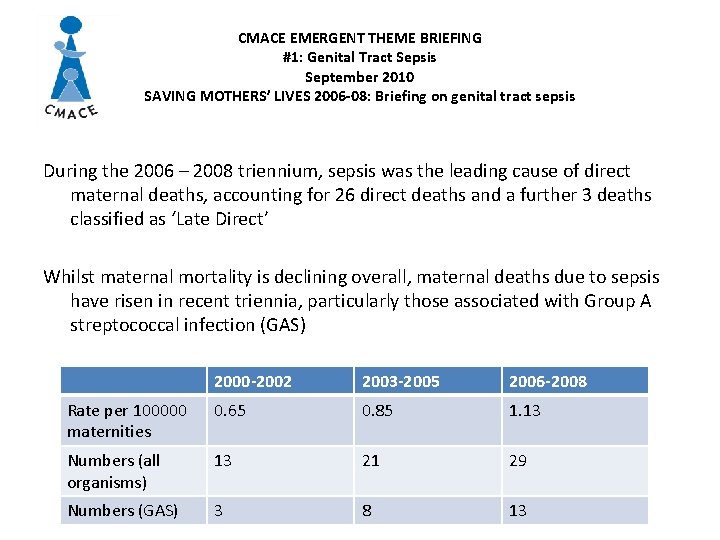
CMACE EMERGENT THEME BRIEFING #1: Genital Tract Sepsis September 2010 SAVING MOTHERS’ LIVES 2006 -08: Briefing on genital tract sepsis During the 2006 – 2008 triennium, sepsis was the leading cause of direct maternal deaths, accounting for 26 direct deaths and a further 3 deaths classified as ‘Late Direct’ Whilst maternal mortality is declining overall, maternal deaths due to sepsis have risen in recent triennia, particularly those associated with Group A streptococcal infection (GAS) 2000 -2002 2003 -2005 2006 -2008 Rate per 100000 maternities 0. 65 0. 85 1. 13 Numbers (all organisms) 13 21 29 Numbers (GAS) 3 8 13
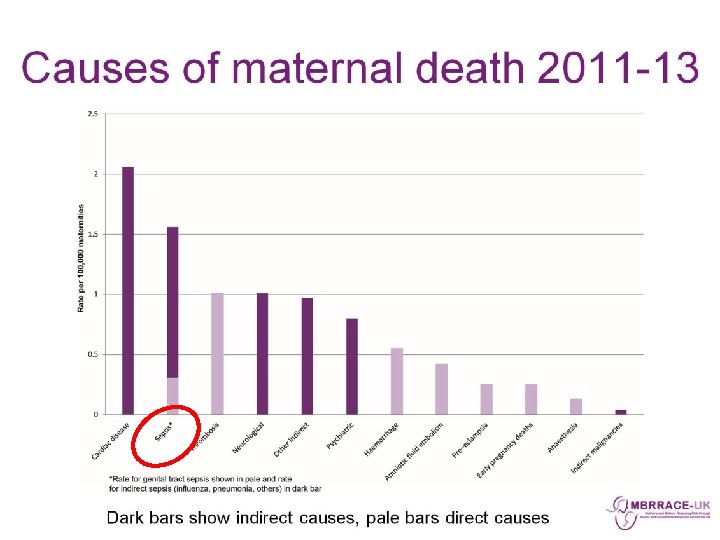
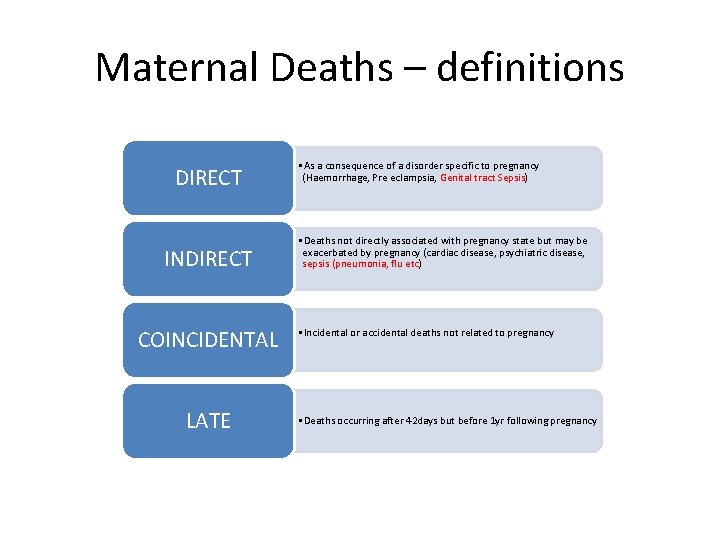
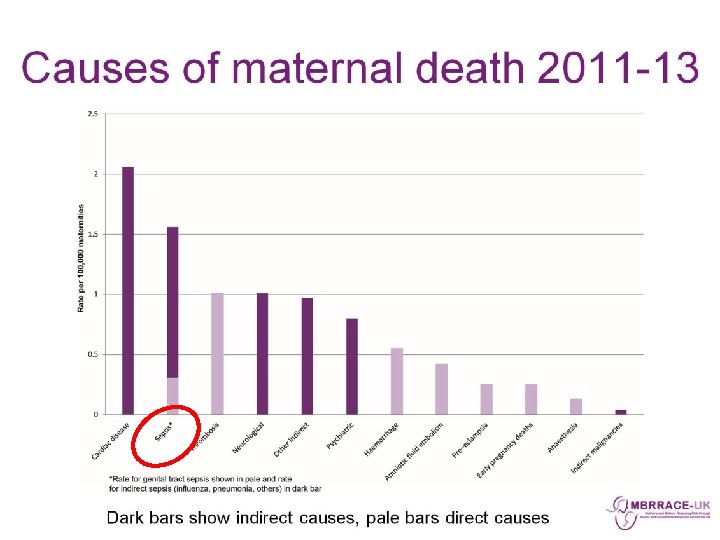
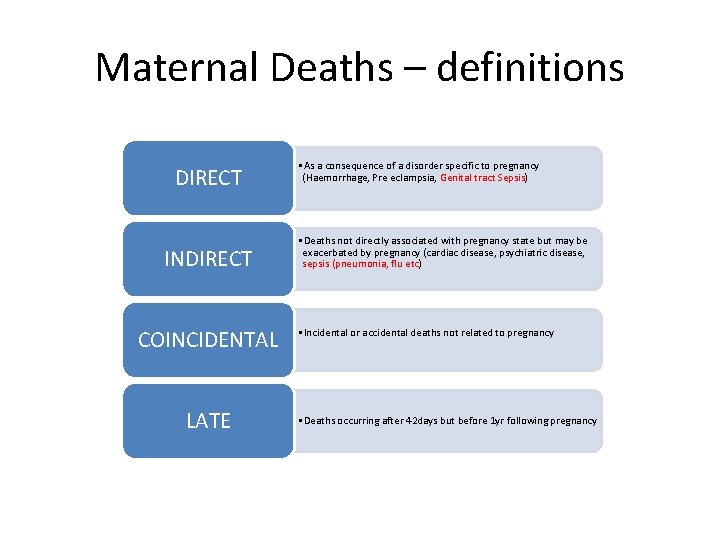
Maternal Deaths – definitions DIRECT INDIRECT COINCIDENTAL LATE • As a consequence of a disorder specific to pregnancy (Haemorrhage, Pre eclampsia, Genital tract Sepsis) • Deaths not directly associated with pregnancy state but may be exacerbated by pregnancy (cardiac disease, psychiatric disease, sepsis (pneumonia, flu etc) • Incidental or accidental deaths not related to pregnancy • Deaths occurring after 42 days but before 1 yr following pregnancy
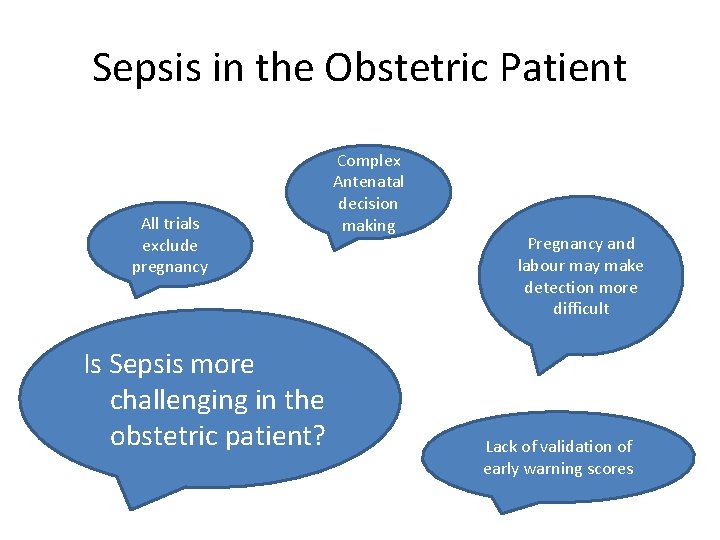
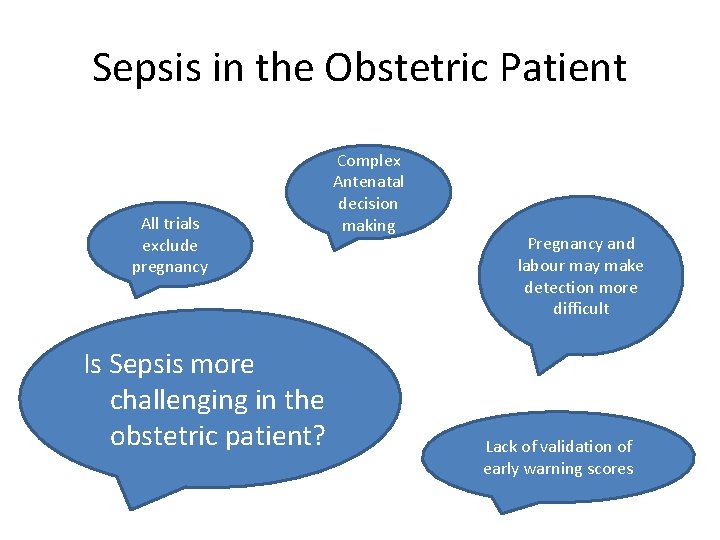
Sepsis in the Obstetric Patient All trials exclude pregnancy Is Sepsis more challenging in the obstetric patient? Complex Antenatal decision making Pregnancy and labour may make detection more difficult Lack of validation of early warning scores
National Maternity Modified SIRS Criteria Any 2 or more: • - Temp < 36 or > 38 o. C • - HR > 100 bpm • - WCC <4 or > 16 x 109/L • - RR > 20 bpm • - Altered mental state
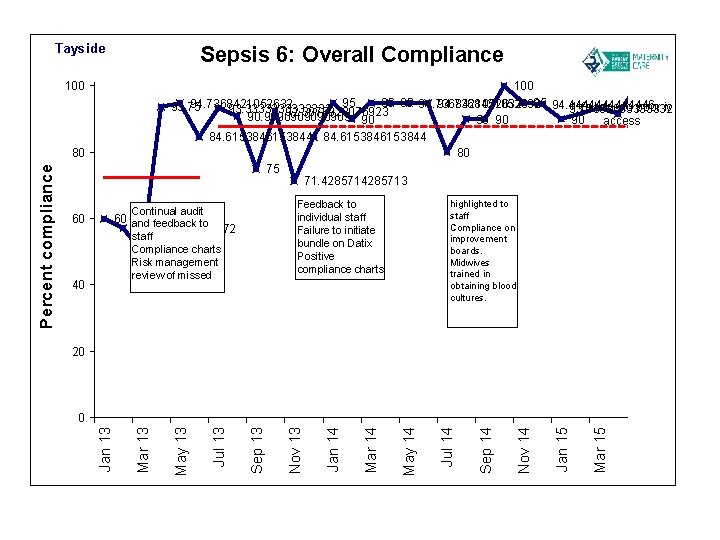
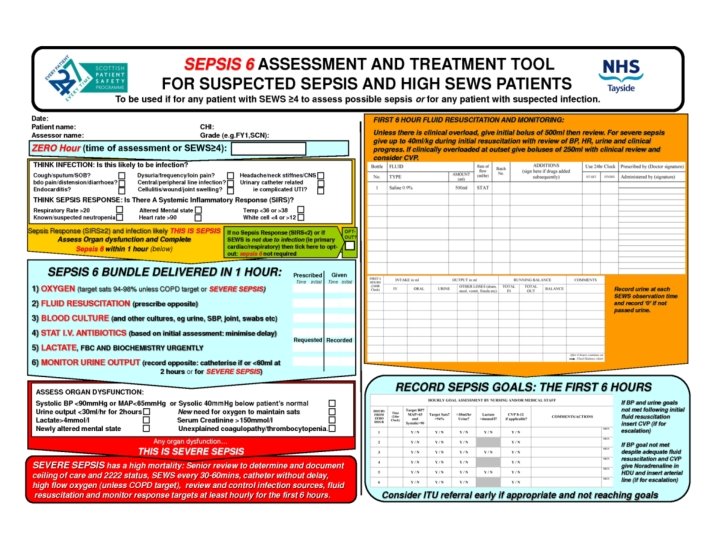
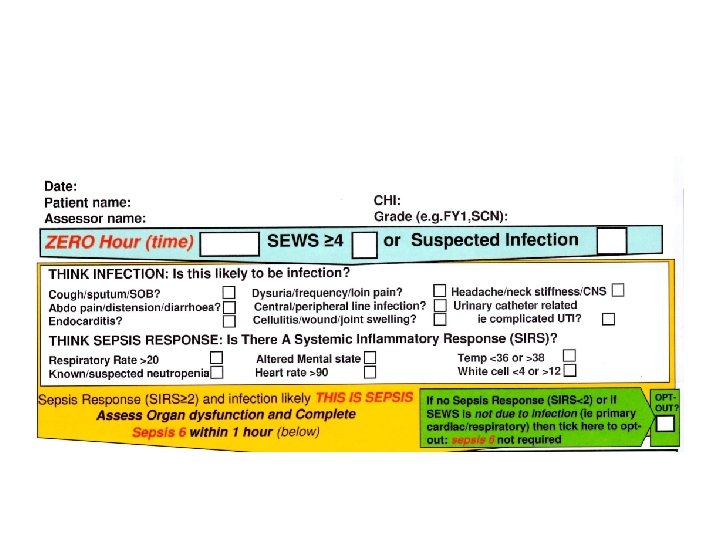
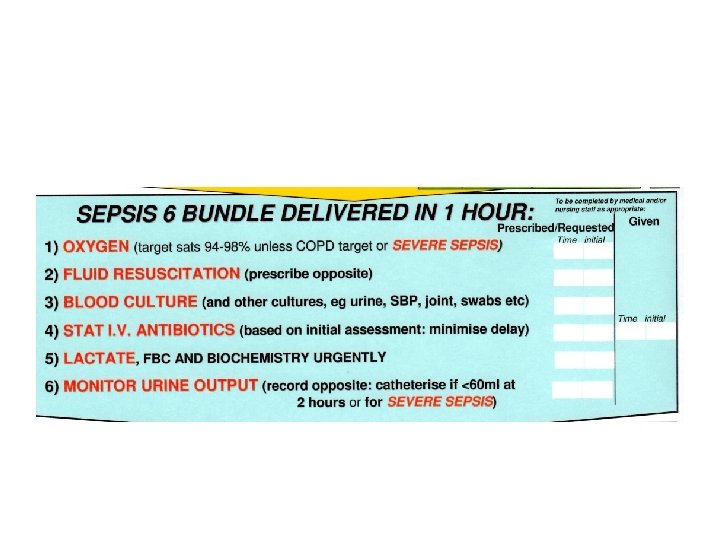
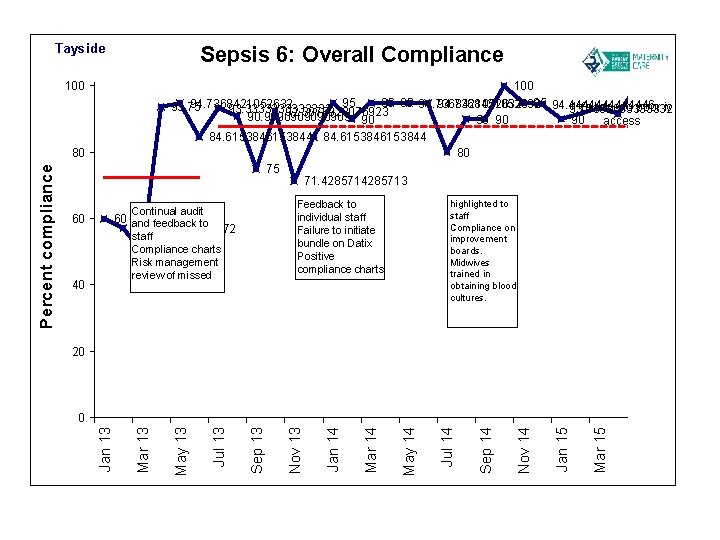
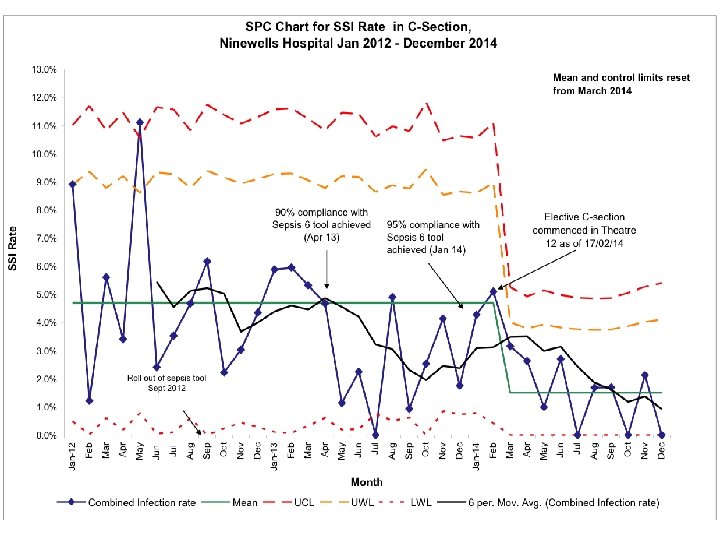
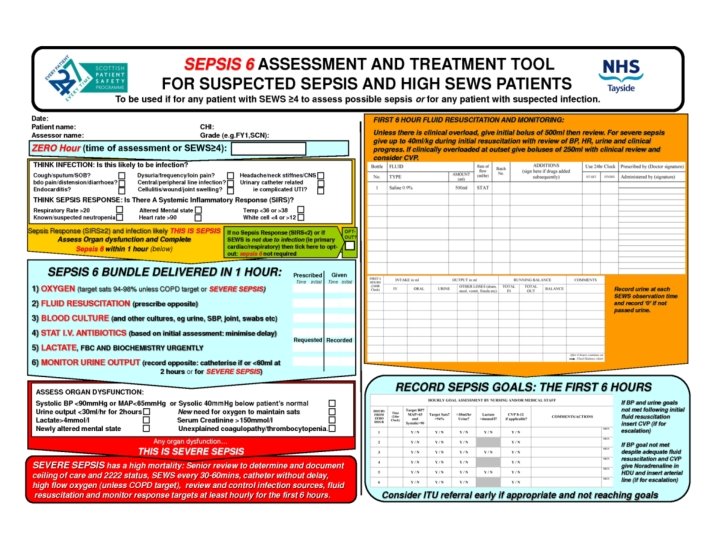
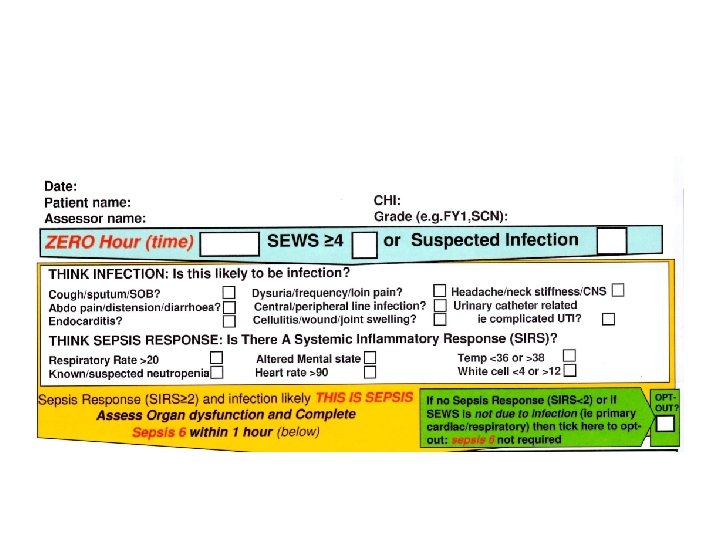
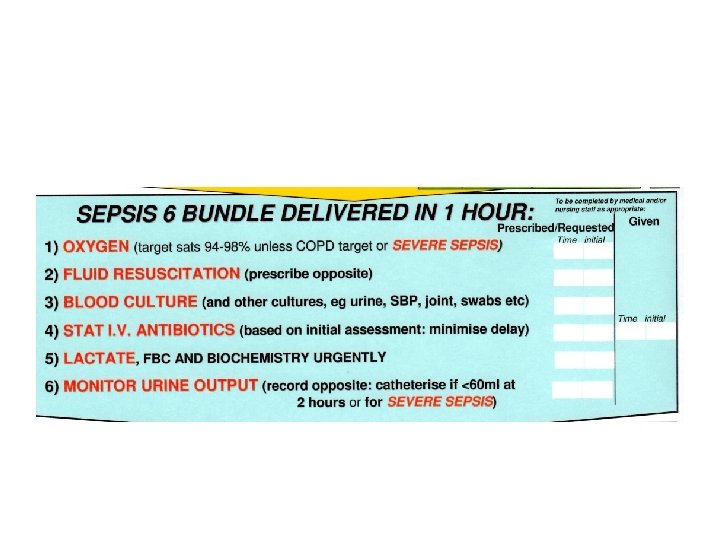
Tayside Sepsis 6: Overall Compliance 100 95 95 95 94. 7368421052632 95 94. 4444446 94. 7368421052632 1 fail due to poor iv 93. 75 93. 3333333333332 92. 3076923 90. 9090909 90 90 access 84. 6153846153844 80 75 71. 4285713 60 40 highlighted to staff Compliance on improvement boards. Midwives trained in obtaining blood cultures. Feedback to individual staff Failure to initiate bundle on Datix Positive compliance charts Continual audit 60 and feedback to 57. 1428572 staff Compliance charts 50 Risk management review of missed 20 Mar 15 Jan 15 Nov 14 Sep 14 Jul 14 May 14 Mar 14 Jan 14 Nov 13 Sep 13 Jul 13 May 13 Mar 13 0 Jan 13 Percent compliance 80
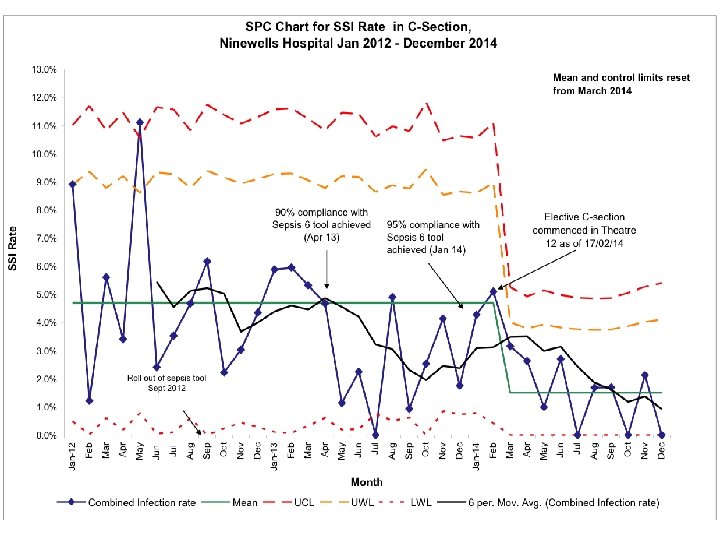
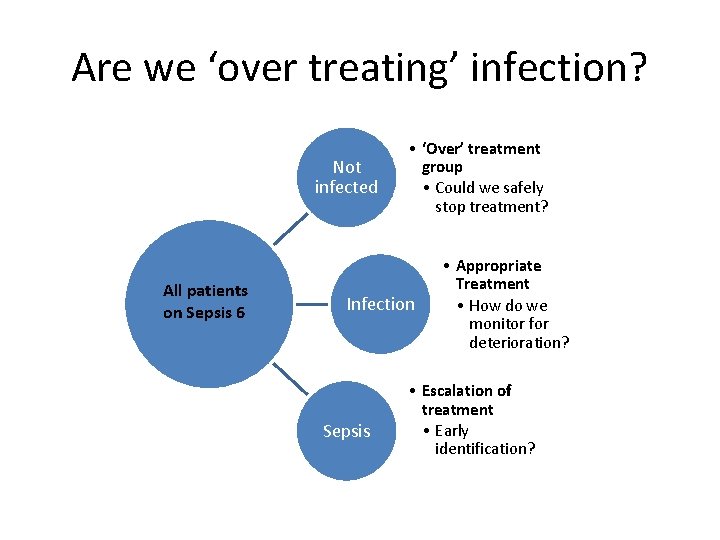
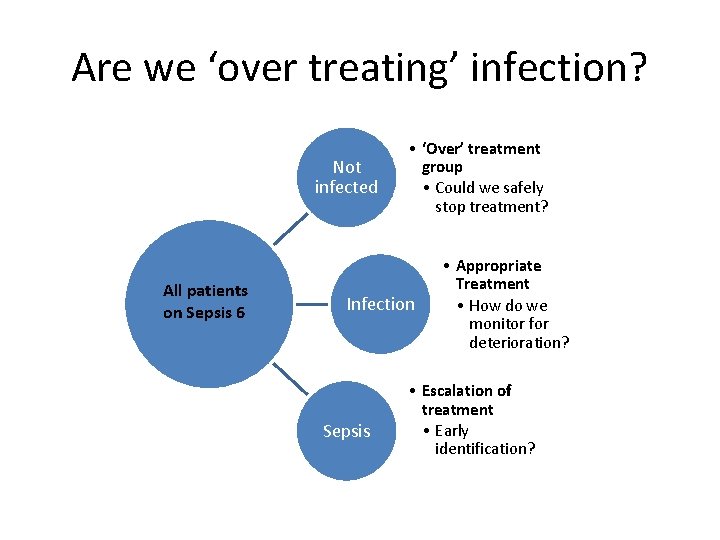
Are we ‘over treating’ infection? Not infected All patients on Sepsis 6 • ‘Over’ treatment group • Could we safely stop treatment? Infection Sepsis • Appropriate Treatment • How do we monitor for deterioration? • Escalation of treatment • Early identification?
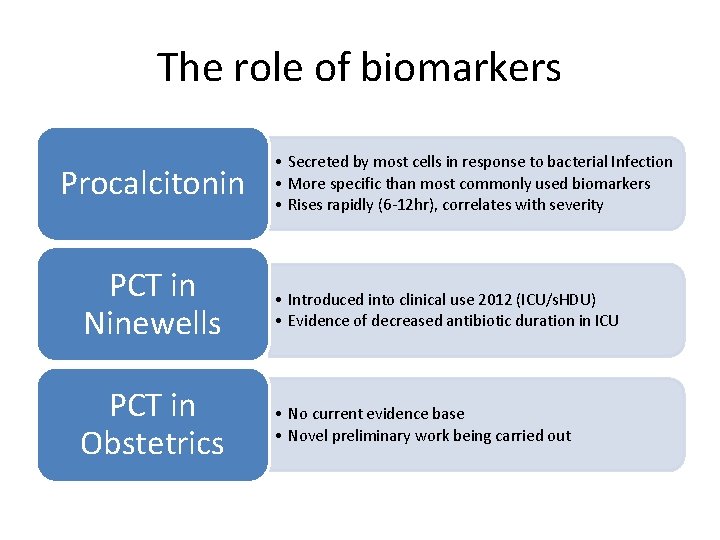
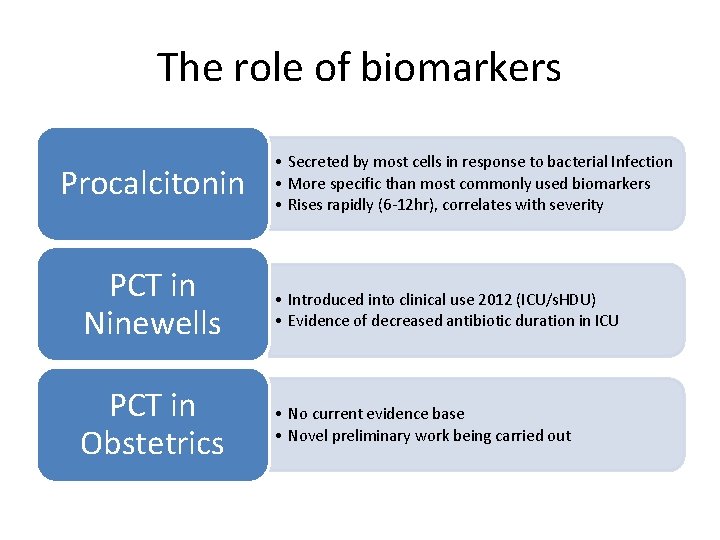
The role of biomarkers Procalcitonin • Secreted by most cells in response to bacterial Infection • More specific than most commonly used biomarkers • Rises rapidly (6 -12 hr), correlates with severity PCT in Ninewells • Introduced into clinical use 2012 (ICU/s. HDU) • Evidence of decreased antibiotic duration in ICU PCT in Obstetrics • No current evidence base • Novel preliminary work being carried out
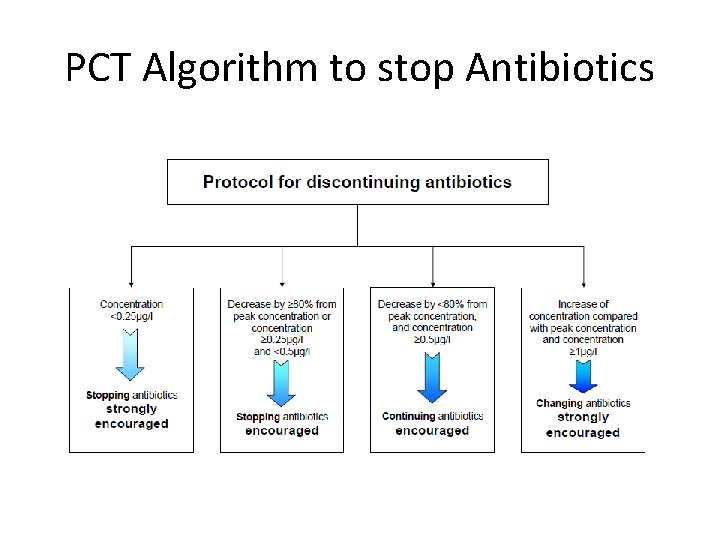
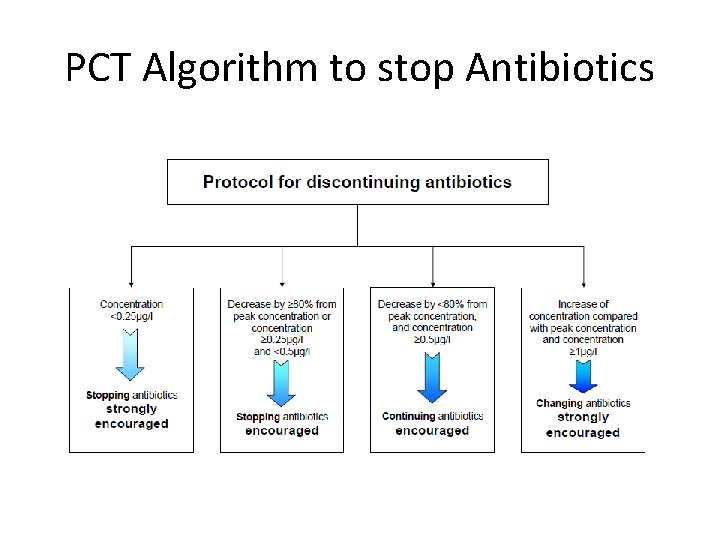
PCT Algorithm to stop Antibiotics
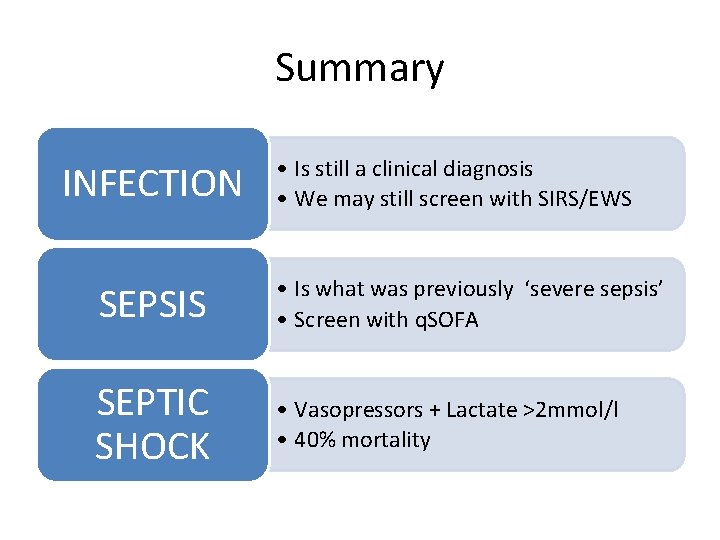
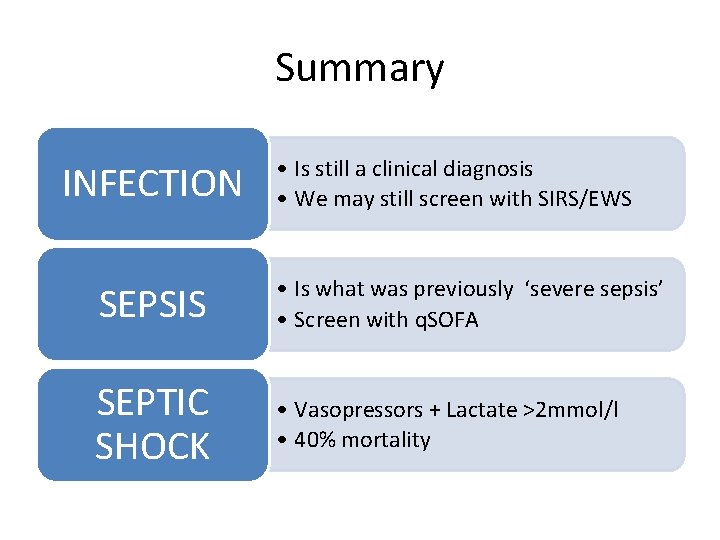
Summary INFECTION • Is still a clinical diagnosis • We may still screen with SIRS/EWS SEPSIS • Is what was previously ‘severe sepsis’ • Screen with q. SOFA SEPTIC SHOCK • Vasopressors + Lactate >2 mmol/l • 40% mortality
Acknowledgements Dr Pamela Johnston Consultant Anaesthetist Dr Pauline Lynch Consultant Obstetrician Dr Katy Orr O&G registrar, j. joss@nhs. net