Sepsis A Practical Predictive Paradigm Jeremy Barnett MD
~ Sepsis ~ A Practical Predictive Paradigm Jeremy Barnett MD ~ Auburn Hospital Department of Critical Care Amy Gutman MD ~ HAHV Department of Emergency Medicine Amy. Gutman@HAHV. org; jbarnett@auburnhospital. org
Objectives • Not teaching “sepsis” • Importance of predictive testing, early identification & aggressive management • Key concepts of disease process & pathophysiology behind management decisions
New Paradigm, Old “Disease” • 26 million people worldwide annually • Leading cause of death in US hospitals • Mortality increases 8% for every hour 8% • Highest 30 day readmission rate treatment delayed • #1 hospitalization cost (>$20 billion annually) • >80% sepsis deaths preventable with rapid • One person dies every 2 minutes from sepsis • > Prostate cancer, breast cancer & AIDS combined diagnosis & treatment • >75, 000 maternal deaths annually worldwide jamanetwork. com; www. hcup-us. ahrq. gov/reports/statbriefs/sb 196 -Readmissions-Trends-High-Volume-Conditions. jsp; www. ncbi. nlm. nih. gov/pubmed/20375891; www. hcupus. ahrq. gov/reports/statbriefs/sb 160. jsp

Forget (Almost) Everything You Know
Bye SIRS…. • Appropriate, regulated host response to infection • Parameters useful for provisional diagnosis of inflammation / infection • Sepsis not simply infection + two or more SIRS criteria, but infection leading to organ dysfunction
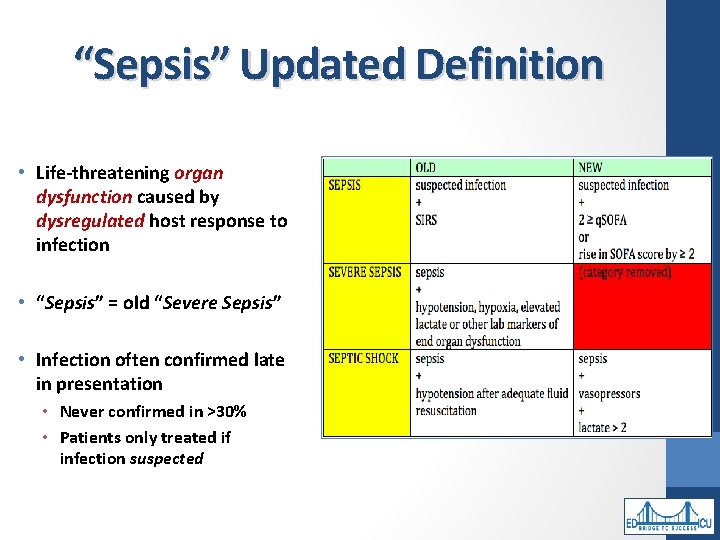
“Sepsis” Updated Definition • Life-threatening organ dysfunction caused by dysregulated host response to infection • “Sepsis” = old “Severe Sepsis” • Infection often confirmed late in presentation • Never confirmed in >30% • Patients only treated if infection suspected
What Is Septic Shock? • Profound circulatory, cellular & metabolic abnormalities with greater mortality risk than sepsis alone • Dysfunctional “organ” is “cellular” • Elevated lactate • Despite fluid resuscitation, vasopressors required maintain MAP ≥ 65 mm. Hg
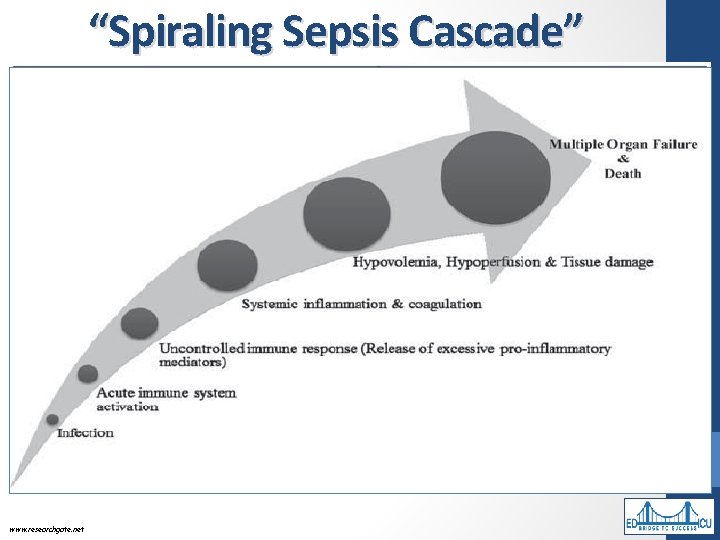
“Spiraling Sepsis Cascade” www. researchgate. net
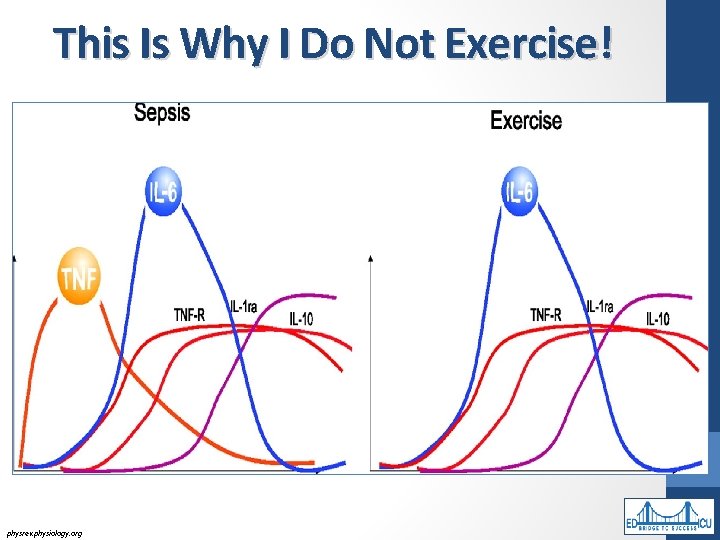
This Is Why I Do Not Exercise! physrev. physiology. org
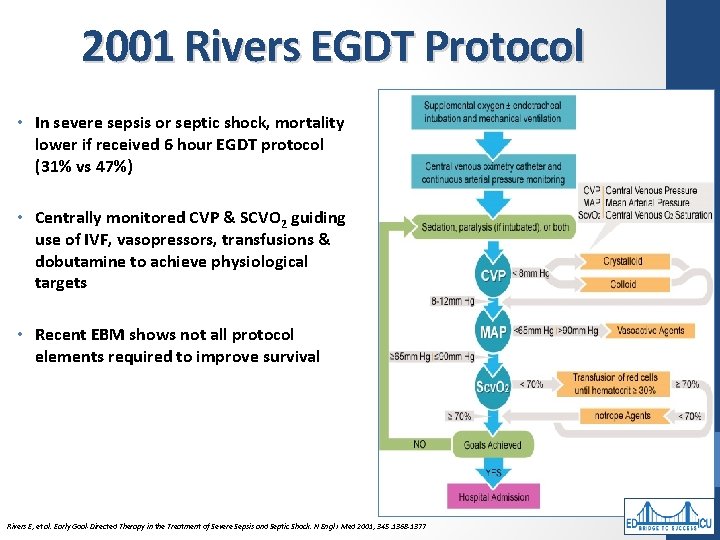
2001 Rivers EGDT Protocol • In severe sepsis or septic shock, mortality lower if received 6 hour EGDT protocol (31% vs 47%) • Centrally monitored CVP & SCVO 2 guiding use of IVF, vasopressors, transfusions & dobutamine to achieve physiological targets • Recent EBM shows not all protocol elements required to improve survival Rivers E, et al. Early Goal-Directed Therapy in the Treatment of Severe Sepsis and Septic Shock. N Engl J Med 2001; 345: 1368 -1377
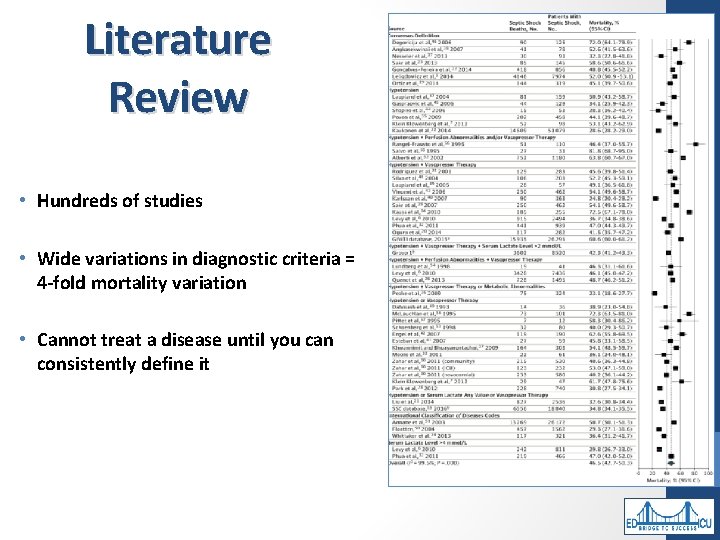
Literature Review • Hundreds of studies • Wide variations in diagnostic criteria = 4 -fold mortality variation • Cannot treat a disease until you can consistently define it
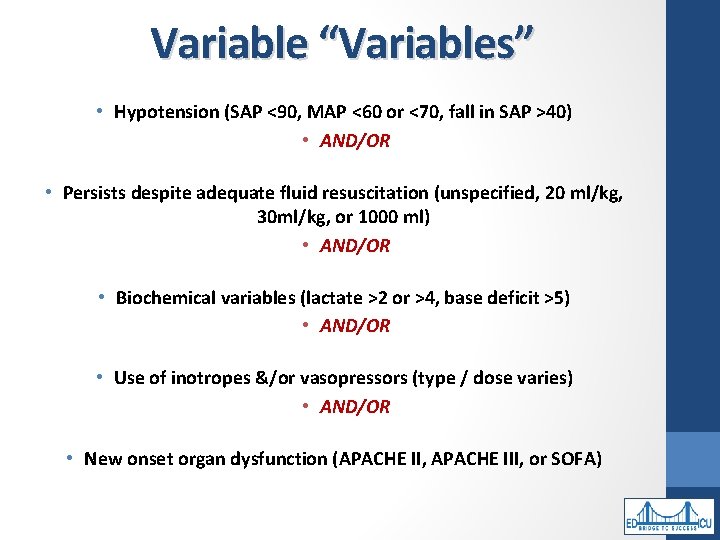
Variable “Variables” • Hypotension (SAP <90, MAP <60 or <70, fall in SAP >40) • AND/OR • Persists despite adequate fluid resuscitation (unspecified, 20 ml/kg, 30 ml/kg, or 1000 ml) • AND/OR • Biochemical variables (lactate >2 or >4, base deficit >5) • AND/OR • Use of inotropes &/or vasopressors (type / dose varies) • AND/OR • New onset organ dysfunction (APACHE II, APACHE III, or SOFA)
Sepsis Scoring Systems
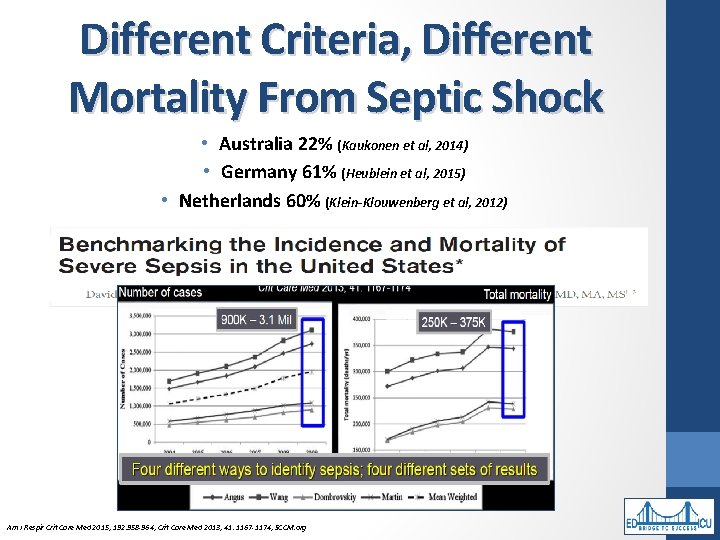
Different Criteria, Different Mortality From Septic Shock • Australia 22% (Kaukonen et al, 2014) • Germany 61% (Heublein et al, 2015) • Netherlands 60% (Klein-Klouwenberg et al, 2012) Am J Respir Crit Care Med 2015; 192: 958 -964; Crit Care Med 2013; 41: 1167 -1174; SCCM. org
Definition Changes Therefore Are Not Simply Semantics
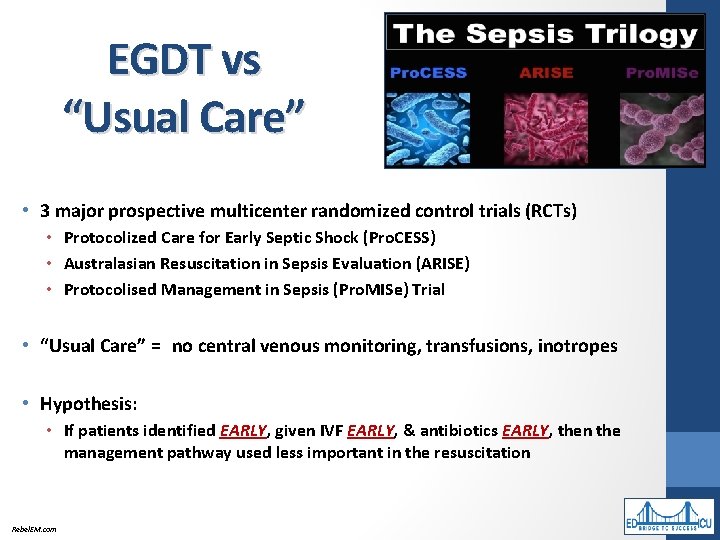
EGDT vs “Usual Care” • 3 major prospective multicenter randomized control trials (RCTs) • Protocolized Care for Early Septic Shock (Pro. CESS) • Australasian Resuscitation in Sepsis Evaluation (ARISE) • Protocolised Management in Sepsis (Pro. MISe) Trial • “Usual Care” = (no central venous monitoring, transfusions, inotropes • Hypothesis: • If patients identified EARLY, given IVF EARLY, & antibiotics EARLY, then the management pathway used less important in the resuscitation Rebel. EM. com
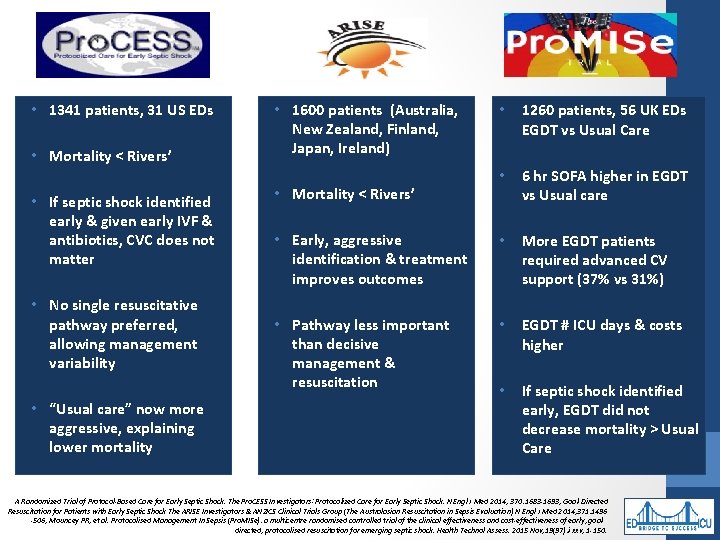
• 1341 patients, 31 US EDs • Mortality < Rivers’ • If septic shock identified early & given early IVF & antibiotics, CVC does not matter • No single resuscitative pathway preferred, allowing management variability • “Usual care” now more aggressive, explaining lower mortality • 1600 patients (Australia, New Zealand, Finland, Japan, Ireland) • 1260 patients, 56 UK EDs EGDT vs Usual Care • 6 hr SOFA higher in EGDT vs Usual care • Early, aggressive identification & treatment improves outcomes • More EGDT patients required advanced CV support (37% vs 31%) • Pathway less important than decisive management & resuscitation • EGDT # ICU days & costs higher • If septic shock identified early, EGDT did not decrease mortality > Usual Care • Mortality < Rivers’ A Randomized Trial of Protocol-Based Care for Early Septic Shock. The Pro. CESS Investigators ; Protocolized Care for Early Septic Shock. N Engl J Med 2014; 370: 1683 -1693; Goal-Directed Resuscitation for Patients with Early Septic Shock The ARISE Investigators & ANZICS Clinical Trials Group (The Australasian Resuscitation in Sepsis Evaluation) N Engl J Med 2014; 371: 1496 -506; Mouncey PR, et al. Protocolised Management In Sepsis (Pro. MISe): a multicentre randomised controlled trial of the clinical effectiveness and cost-effectiveness of early, goaldirected, protocolised resuscitation for emerging septic shock. Health Technol Assess. 2015 Nov; 19(97): i-xxv, 1 -150.
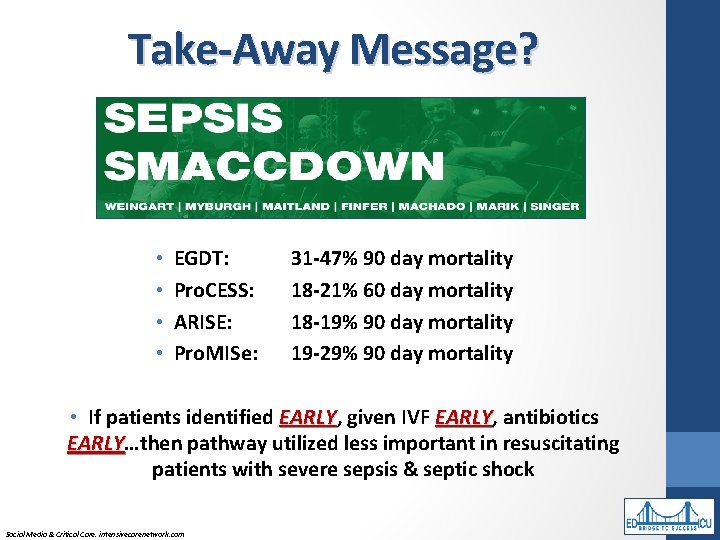
Take-Away Message? • • EGDT: Pro. CESS: ARISE: Pro. MISe: 31 -47% 90 day mortality 18 -21% 60 day mortality 18 -19% 90 day mortality 19 -29% 90 day mortality • If patients identified EARLY, given IVF EARLY, antibiotics EARLY…then pathway utilized less important in resuscitating EARLY patients with severe sepsis & septic shock Social Media & Critical Care. intensivecarenetwork. com
Sepsis “ 6 (ish)” • 0 - 60 minutes • • Lactic Acid Blood Cultures Antibiotics 30 m. L/kg IVF • 61 – 180 minutes • Vasopressors if MAP <65 mm. Hg • Re-assess volume status & tissue perfusion • Re-check Lactic Acid BJM. 2001; 345: 1368 -77
EBM Guidelines § IV antimicrobials within 1 st hour of septic shock recognition (Grade 1 B) & severe sepsis without septic shock (Grade 1 C) § Initial empiric / appropriate antimicrobials >1 drugs with activity against all likely pathogens (Grade 1 B) Crit Care Med 2013; 41: 580 -637
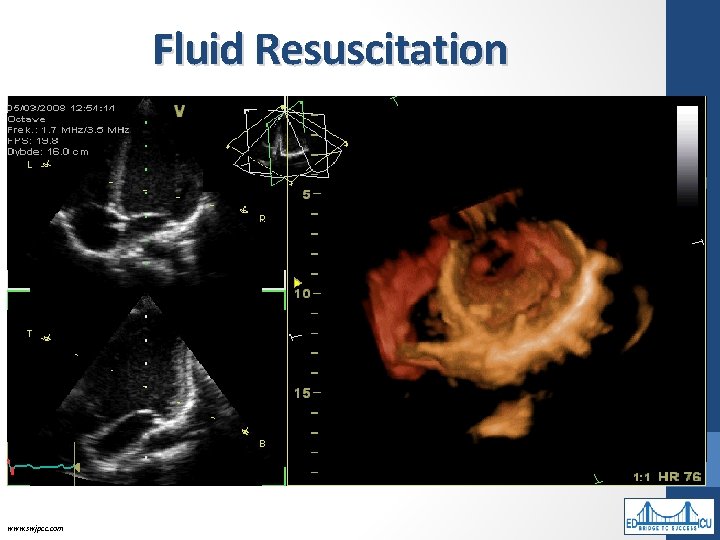
Fluid Resuscitation • Rapid 30 m. L/kg crystalloid administration with response assessment • Often require >4 -6 liters • Crystalloids titrated to adequate tissue perfusion • CVP increase >2 mm. Hg, CVP >8 -12 mm. Hg, or signs of volume overload • Non-invasive CVP estimation • Ultrasonography • IVC diameter as surrogate for volume status • 50% difference predicts CVP <8 mm. Hg with >92% sensitivity & specificity • UOP • <0. 5 ml/kg/hr prompts measures to increase cardiac output www. swjpcc. com
Crystalloid IVF Resuscitation Risks • 4 RCT meta-analysis: no mortality reduction • 18 trials with historical controls: significant survival increase • Though most patients with severe sepsis “functionally hypovolemic” monitoring right ventricular volume for overload essential to avoid acute cor pulmonale
Early Antibiotics • “For the greatest survival benefit, give antibiotics as early as possible and always within one hour of emergency department presentation or, for ward -based patients, recognition of severe sepsis or septic shock” • Decrease physiologic response to infection, limit injury from microbial activity / toxin production, slow progression to multi-organ dysfunction • Microbial load increases as infection progresses • Cytokine release occurring when antibiotics given more severe later in cascade • Research links early antibiotics & survival, with confounders: • • Failure to correct for illness severity Failure to determine if appropriate antibiotic choice LITFL. com; Australian Therapeutic Guidelines (2014)
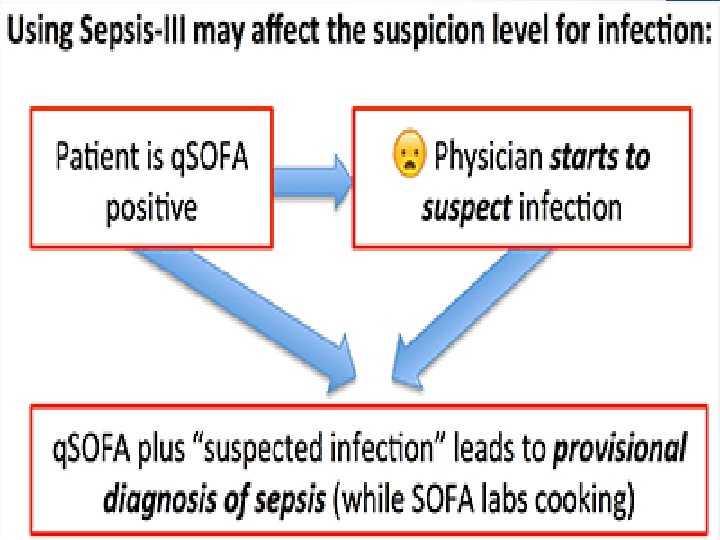
Quick SOFA Sequential Organ Failure Assessment • Identifies patients at risk of sepsis • 2 q. SOFA criteria predict increased mortality & prolonged ICU stays
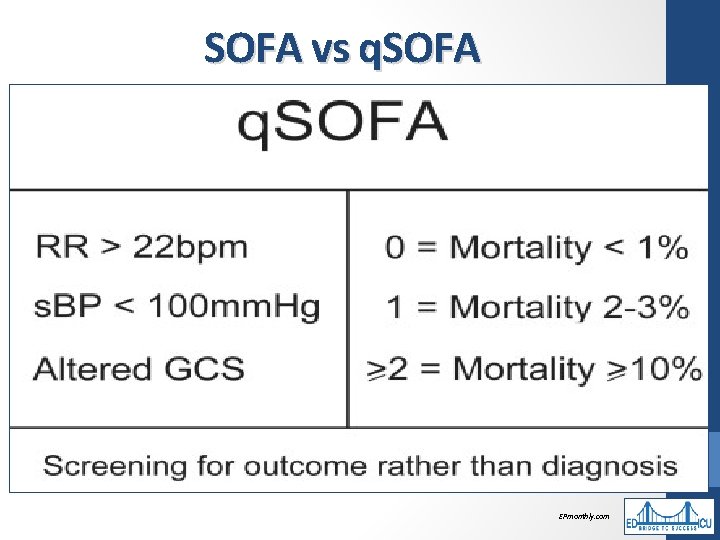
SOFA vs q. SOFA EPmonthly. com
• In ICU, SOFA has greater predictive validity than q. SOFA • Outside ICU, q. SOFA has similar predictive validity to complex scores • Focus on timeliness, ease of use • 21 variables from Sepsis-2 • Most predictive: Infection plus >2 SOFA points www. qsofa. org
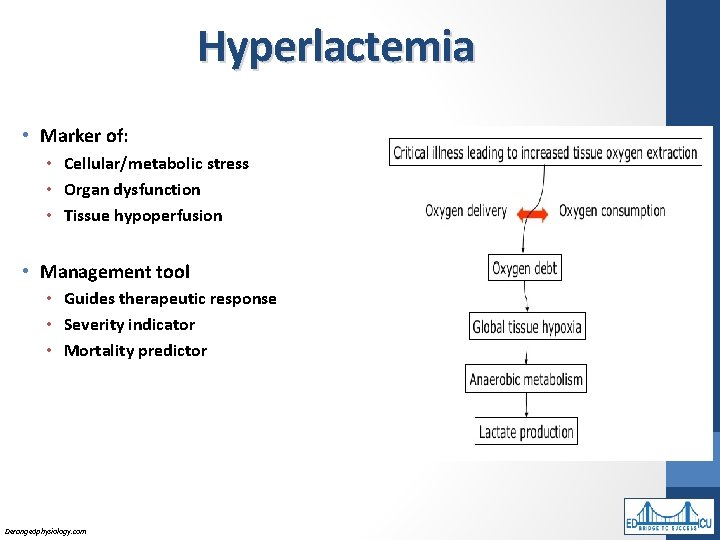
Hyperlactemia • Marker of: • Cellular/metabolic stress • Organ dysfunction • Tissue hypoperfusion • Management tool • Guides therapeutic response • Severity indicator • Mortality predictor Derangedphysiology. com
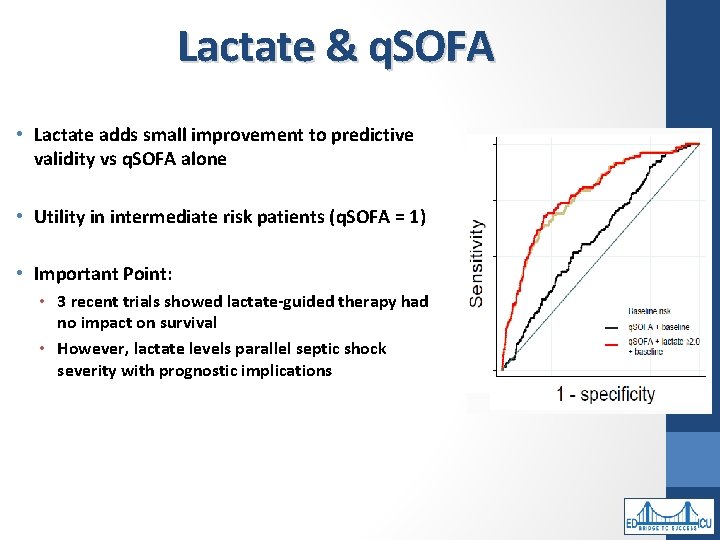
Lactate & q. SOFA • Lactate adds small improvement to predictive validity vs q. SOFA alone • Utility in intermediate risk patients (q. SOFA = 1) • Important Point: • 3 recent trials showed lactate-guided therapy had no impact on survival • However, lactate levels parallel septic shock severity with prognostic implications
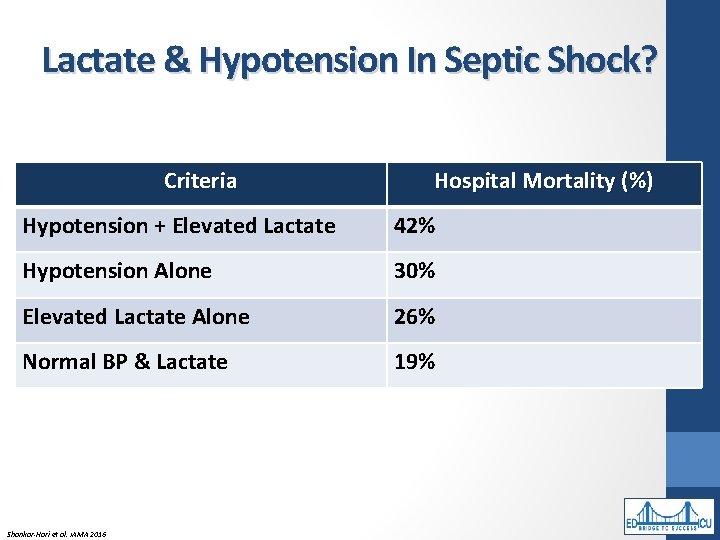
Lactate & Hypotension In Septic Shock? Criteria Hospital Mortality (%) Hypotension + Elevated Lactate 42% Hypotension Alone 30% Elevated Lactate Alone 26% Normal BP & Lactate 19% Shankar-Hari et al. JAMA 2016
So…Sepsis 6 “ish” • 0 -60 minutes • Check Lactic Acid • Send Blood Cultures • Give Antibiotics • 30 m. L/kg IVF • 61 – 180 minutes • Vasopressors if MAP <65 mm. Hg • Re-assess Volume Status & Tissue Perfusion • Re-Check Lactic Acid
Blood Cultures • Clinical & lab parameters independently correlate with bacteremia • Hypoalbuminemia, AKI, UTI • Chills, fever, hypothermia, hypotension • Leukocytosis, left shift of neutrophils, neutropenia • Peaking fever more sensitive than leukocytosis to predict bacteremia • Obtain cultures before antimicrobials initiated if doesn’t delay administration (Grade 1 C)
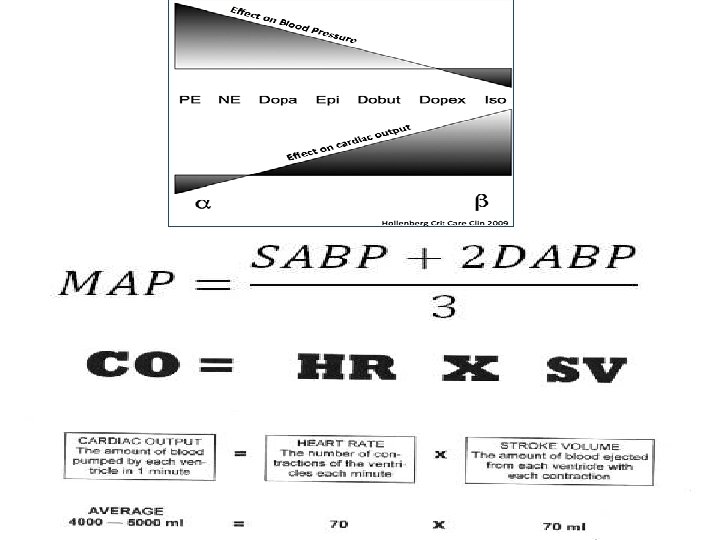
Vasopressors • Septic shock unresponsive to 30 ml/kg IVF (Grade 1 C) • Simultaneously with fluid resuscitation targeting MAP >65 mm. Hg (Grade 1 C) • Norepinephrine (Levophed) • 1 st line vasopressor (Grade 1 B) • Increases MAP via vasoconstriction, little effect on HR, SV, & CO • Epinephrine • If norepinephrine insufficient to maintain MAP >65 mm. Hg (Grade 2 B) • Vasopressin • Additive to norepinephrine to improve perfusion • Dopamine • Increases HR, SV & CO to increase MAP
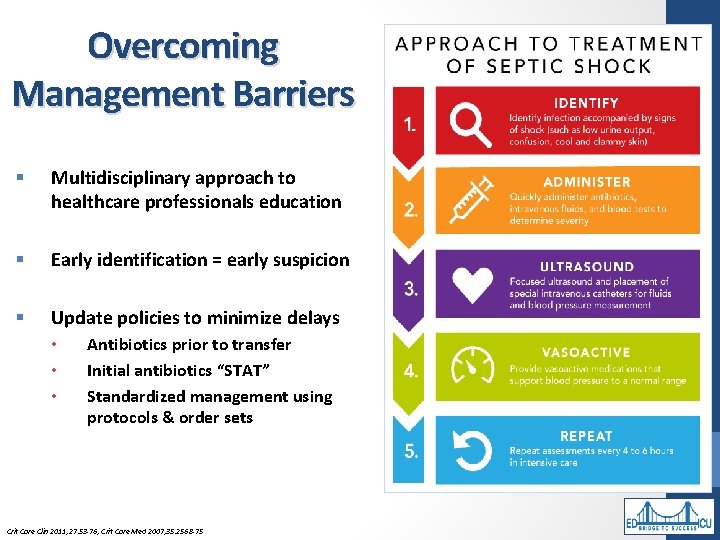
Overcoming Management Barriers § Multidisciplinary approach to healthcare professionals education § Early identification = early suspicion § Update policies to minimize delays • • • Antibiotics prior to transfer Initial antibiotics “STAT” Standardized management using protocols & order sets Crit Care Clin 2011; 27: 53 -76; Crit Care Med 2007; 35: 2568 -75
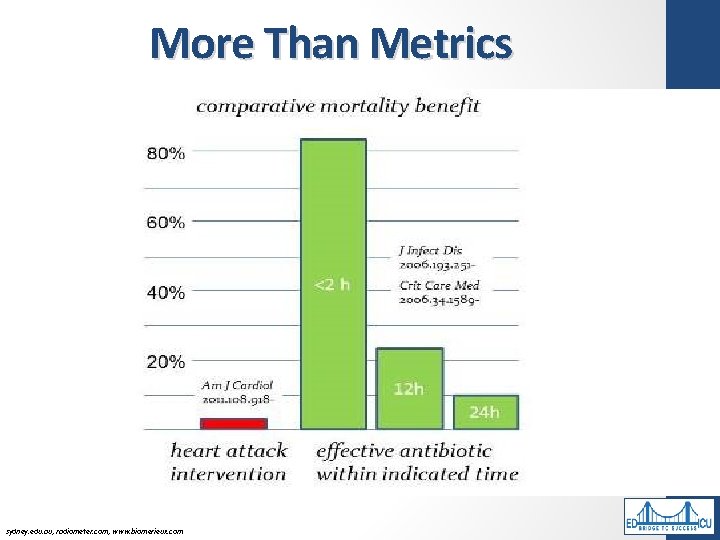
More Than Metrics sydney. edu. au; radiometer. com; www. biomerieux. com
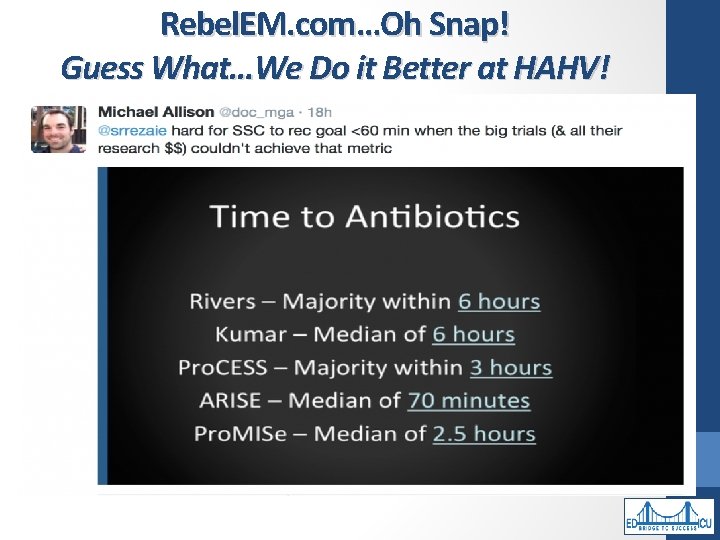
Rebel. EM. com…Oh Snap! Guess What…We Do it Better at HAHV!
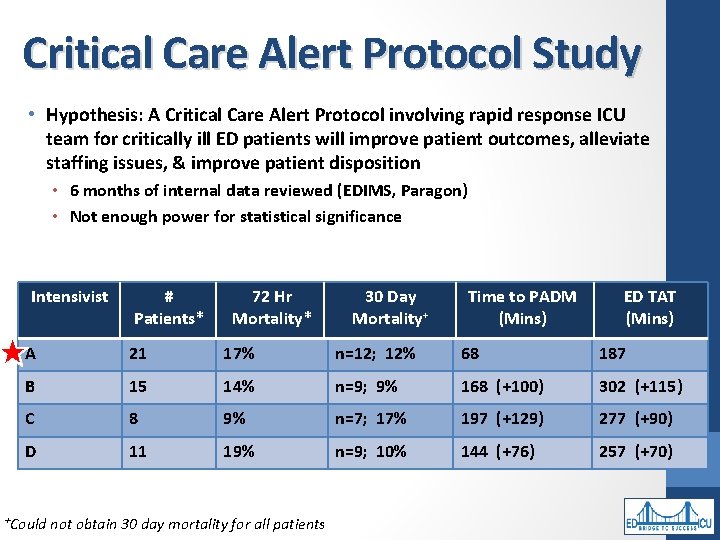
Critical Care Alert Protocol Study • Hypothesis: A Critical Care Alert Protocol involving rapid response ICU team for critically ill ED patients will improve patient outcomes, alleviate staffing issues, & improve patient disposition • 6 months of internal data reviewed (EDIMS, Paragon) • Not enough power for statistical significance Intensivist # 72 Hr Patients* Mortality* 30 Day Mortality+ Time to PADM (Mins) ED TAT (Mins) A 21 17% n=12; 12% 68 187 B 15 14% n=9; 9% 168 (+100) 302 (+115) C 8 9% n=7; 17% 197 (+129) 277 (+90) D 11 19% n=9; 10% 144 (+76) 257 (+70) +Could not obtain 30 day mortality for all patients
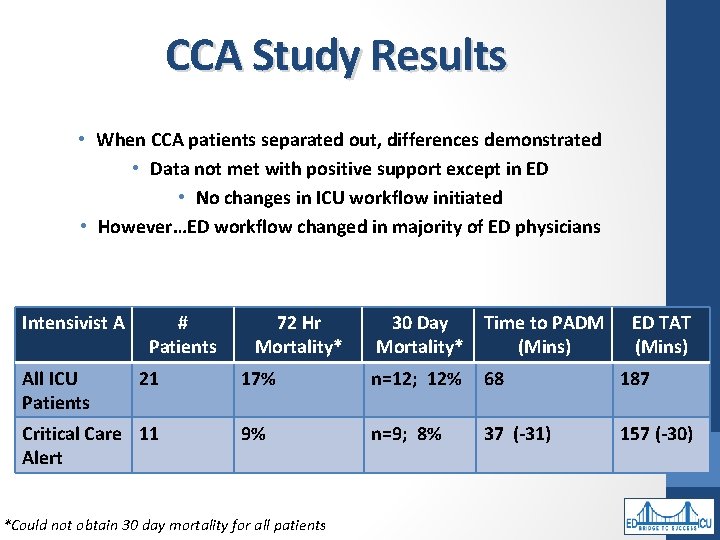
CCA Study Results • When CCA patients separated out, differences demonstrated • Data not met with positive support except in ED • No changes in ICU workflow initiated • However…ED workflow changed in majority of ED physicians Intensivist A All ICU Patients # 72 Hr Patients Mortality* 21 Critical Care 11 Alert 30 Day Time to PADM Mortality* (Mins) ED TAT (Mins) 17% n=12; 12% 68 187 9% n=9; 8% 37 (-31) 157 (-30) *Could not obtain 30 day mortality for all patients
References • • • • Conservative fluid therapy in septic shock: an example of targeted therapeutic minimization. Crit Care. 2014; 18(4): 481. SCCM/ESICM: The 3 rd International Consensus Definitions for Sepsis & Septic Shock. The Sepsis Definitions Task Force. New definitions: Why, How & What. Query September 2016. CRISMA Center. University of Pittsburgh Departments of Critical Care & Emergency Medicine www. sccm. org/sepsisredefined. Queried September 2016 Surviving Sepsis Campaign. www. survivingsepsis. org. Queried September 2016. Singer M, et al. 3 rd International Consensus Definitions for Sepsis & Septic Shock (Sepsis-3). JAMA. 2016 Feb 23; 315(8): 801 -810. Seymour CW, et al. Assessment of clinical criteria for sepsis: for the 3 rd international consensus definition for sepsis & septic shock (Sepsis-3). JAMA. 2016 Feb 23; 315(8): 762 -774. Seymour CW, et al. Application of a framework to assess the usefulness of alternative sepsis criteria. Crit Care Med. 2016 Mar; 44(3): e 122 -e 130. Levy MM, et al. Surviving Sepsis Campaign: association between performance metrics and outcomes in a 7. 5 -year study. Crit Care Med. 2015 Jan; 43(1): 3 -12. Wells D. Appropriate timing & dosing of antibiotics in sepsis. Auburn University Harrison School of Pharmacy. Queried September 2016. Fish, J. University of Wisconsin Hospital. Trauma and Life Center. Appropriate timing and dosing of antibiotics in sepsis. Queried Sept 2016 Kumar A, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006 Jun; 34(6): 1589 -96. Rivers E, Nguyen B, et al. Early Goal-Directed Therapy Collaborative Group. Early Goal-Directed Therapy in the Treatment of Severe Sepsis and Septic Shock. NEJM. 2001; 345: 1368 -1377 Process/ARISE/Pro. MISe Methodology Writing Committee. Harmonizing international trials of early goal-directed resuscitation for severe sepsis and septic shock: Methodology of Pro. CESS, ARISE, and Pro. MISe. Intensive Care Med. 2013 Oct; 39(10): 1760 -75. The Pro. CESS Investigators. A Randomized Trial of Protocol-Based Care for Early Septic Shock. NEJM. 2014; 370: 1683 -1693
Conclusions Amy. Gutman@hahv. org; jdbarnett@auburnhospital. org • No more “SIRS” • “Sepsis” now “Severe Sepsis” • “Septic shock” is a subset of sepsis in which underlying circulatory, cellular and metabolic abnormalities associated with a greater risk of mortality than sepsis alone • Treat patient in front of you & do not wait until criteria met as early identification & management key to survival • Understand the “why” of what we do, not just the metrics • Thank you for the invitation!
- Slides: 39