Sepsis 2016 Core Measures Recognition and Management S


- Slides: 69
Sepsis 2016 Core Measures Recognition and Management S
Tom Ahrens Ph. D RN FAAN S Research Scientist at Barnes-Jewish Hospital, St. Louis, MO S No conflicts of interest to report
SEP-1 Core Measure S Suspected infection S 2 or more signs of SIRS S Evidence of organ dysfunction S Elevated lactate is one example
Time Zero When the patient meets criteria for severe sepsis S
CMS Core Measure S Measure Description: This measure will focus on patients aged 18 years and older who present with symptoms of severe sepsis or septic shock. These patients will be eligible for the 3 hour (severe sepsis) and/or 6 hour (septic shock) early management bundle. S Numerator Statement: If: measure lactate level obtain blood cultures prior to antibiotics administer broad spectrum antibiotics administer 30 ml/kg crystalloid for hypotension or lactate >=4 mmol/L
What is sepsis? S Sepsis is the body’s immune system response to an infection S Bacteria, virus, protozoan S Instead of a localized response to an infection (like a pneumonia), sepsis is a systemic response that can be catastrophic S Highest cost to US hospitals (AHRQ) S Leading cause of death in hospitals
New Definitions
New Sepsis Definition q. SOFA S An alteration in mental status (not the GCS) S A decrease in SBP of less than 100 mm Hg S A respiratory rate > 22 bpm
Sequential Organ Failure Assessment SOFA Scores S
Method of Predicting Outcomes in Critically Ill Patients S An initial SOFA score of < 9 predicted a mortality of < 33% S A SOFA > 11 predicted mortality of 95%
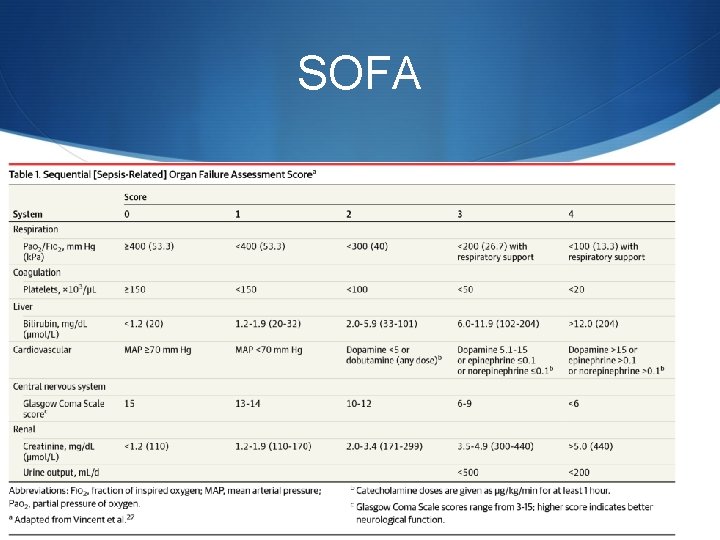
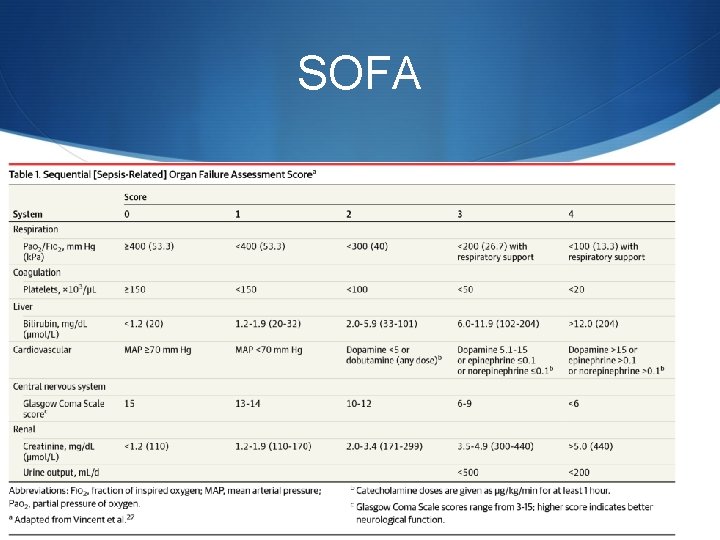
SOFA
Key Differences in New Definition S Sepsis as infection and 2 or more SIRS is now just an infection S Severe sepsis is now sepsis S Septic shock is S Blood lactate > 2 mmol/L despite volume resuscitation S Hypotension that persists after fluid resuscitation and requires vasopressors S Sepsis definition now will carry a higher risk of death and increased ICU LOS
Rationale for New Definition S Based on review of 2 million patients in sepsis studies S SIRS based on expert opinion S SIRS should still be used when evaluating sepsis

Controversy with New Definition
Controversies with New Definition S Not a screening tool S A better sepsis definition S Concern is a delay in sepsis identification
Benefits and Barriers S Improved S Patient identification S Coding and reimbursement S SOI/ROM S Reduced mortality S Improved compliance with bundles S Barriers S Multidisciplinary cooperation S Funding S Education
Can your staff recognize sepsis? Sepsis can be subtle until it is so obvious you can’t miss it S
62 year old admitted to hospital with hip infection S On admission S T – 38. 5 S RR – 24 S P – 104 S WBC – 19, 000 S Where should he be admitted?
36 hours post admission Urine output drops – What should be done? S

48 hours post admission Pulse oximeter drops and becomes difficult to read – what should be done? S
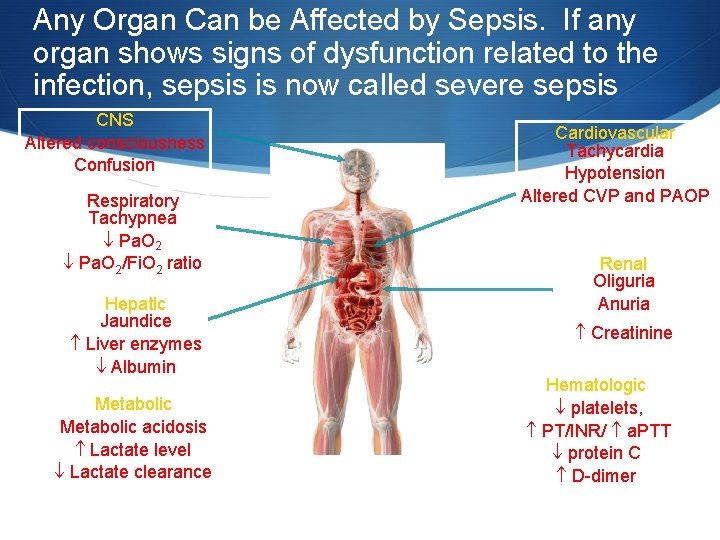
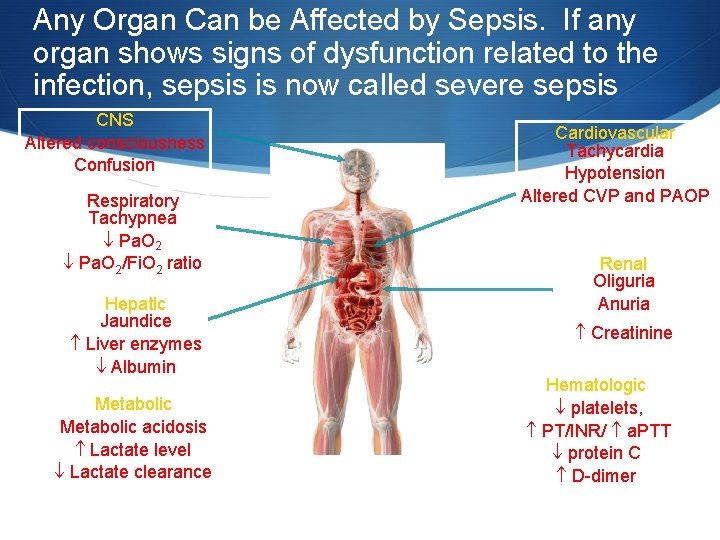
Any Organ Can be Affected by Sepsis. If any organ shows signs of dysfunction related to the infection, sepsis is now called severe sepsis CNS Altered consciousness Confusion Respiratory Tachypnea Pa. O 2/Fi. O 2 ratio Hepatic Jaundice Liver enzymes Albumin Metabolic acidosis Lactate level Lactate clearance Cardiovascular Tachycardia Hypotension Altered CVP and PAOP Renal Oliguria Anuria Creatinine Hematologic platelets, PT/INR/ a. PTT protein C D-dimer Modified from criteria published in: Balk RA. Crit Care Clin. 2000; 16: 337 -352. Kleinpell RM. Crit Care Nurs Clin N Am 2003; 15: 27 -34.
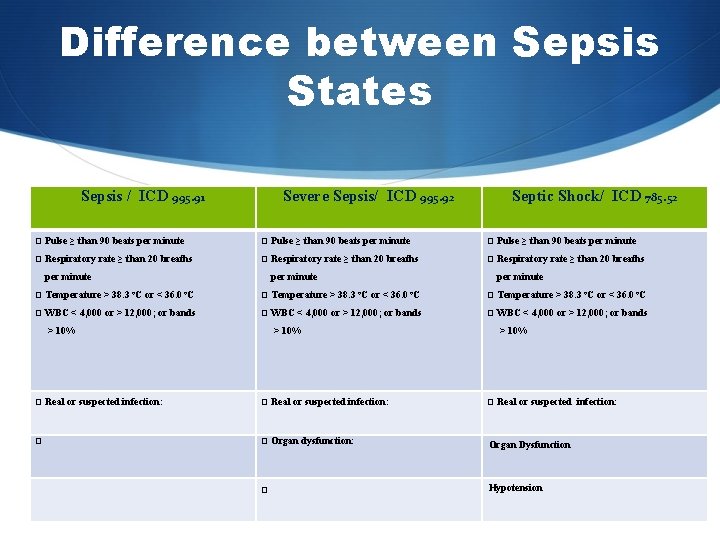
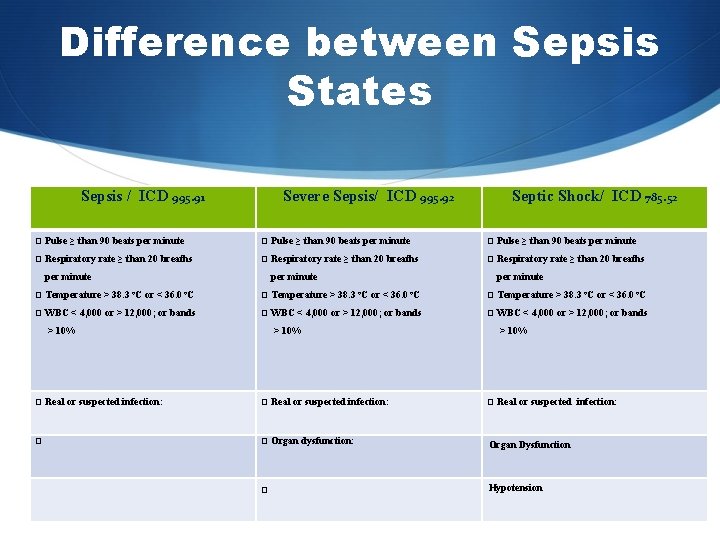
Difference between Sepsis States Sepsis / ICD 995. 91 Severe Sepsis/ ICD 995. 92 Septic Shock/ ICD 785. 52 Pulse ≥ than 90 beats per minute Respiratory rate ≥ than 20 breaths per minute Temperature > 38. 3 per minute o. C or < 36. 0 o. C WBC < 4, 000 or > 12, 000; or bands Temperature > 38. 3 per minute 36. 0 o. C Temperature > 38. 3 o. C or < 36. 0 o. C WBC < 4, 000 or > 12, 000; or bands > 10% o. C or < > 10% Real or suspected infection: Organ dysfunction: Organ Dysfunction Hypotension
Key to Success in Sepsis Management S Prevent infections! Don’t let sepsis start S Rapid Identification S If sepsis is present, rapid treatment is needed
Pathophysiology of Sepsis What do we need to know S
The Power of Our Immune System “Our arsenals for fighting off bacteria are so powerful, and involve so many different defense mechanisms, that we are more in danger from them than from the invaders. “We live in the midst of explosive devices; we are mined!” Lewis Thomas - 1972 Germs, New England Journal Of Medicine DR 32708 3000093662 1204. 5 Copyright © 2004, Eli Lilly and Company. All rights reserved. Xigris is a registered trademark of Eli Lilly and Company.
Power of the Immune System Vaccine Schedule – Too Much? 14 Vaccines now Recommended S What causes immune response is number of proteins that cause reaction - Epitopes S 100 years ago only vaccine was against smallpox S Large virus, 200 epitope inducing proteins S Todays 14 vaccines have 160 epitope inducing proteins S Immune system has to respond, immediately at birth, millions of bacteria S Each of these bacteria have 2 -6 thousand protein which can induce epitopes S Within days, a human baby has 100 trillion bacteria in and on them (we have 10 trillion cells)
A Single Cold Virus Has More Protein Inducing Epitopes than All Vaccinations Combined S Given the number of B cells in the bloodstream, the average number of epitopes contained in a vaccine, rapidity with which a sufficient quantity of antibodies could be made: S Babies could respond to 100, 000 vaccines at one time.
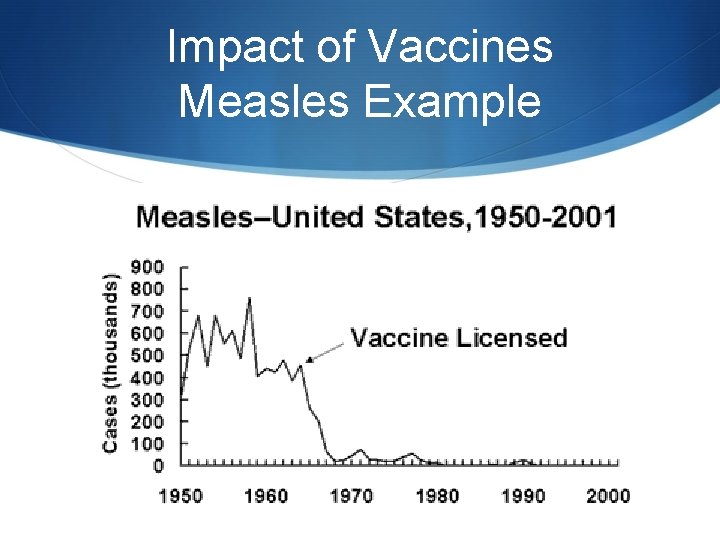
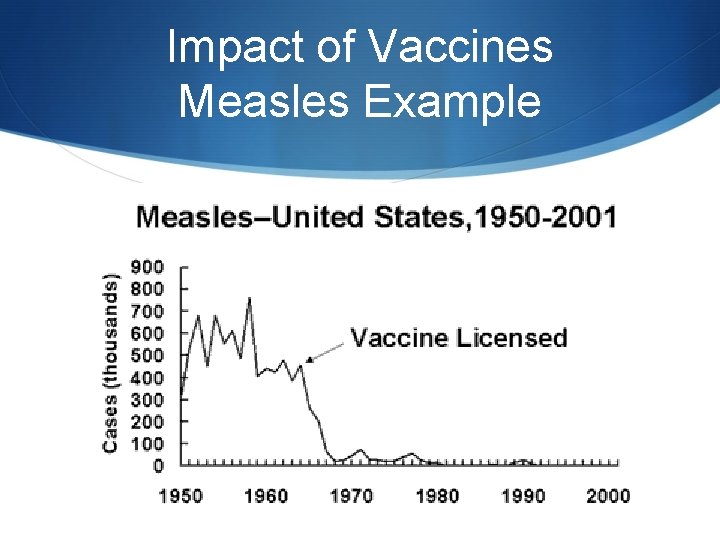
Impact of Vaccines Measles Example
But few bacteria are dangerous S Only a small amount of bacteria and viruses are dangerous S Those are not likely to be on the floor S But they can be on your hands or in the air S Protecting yourself
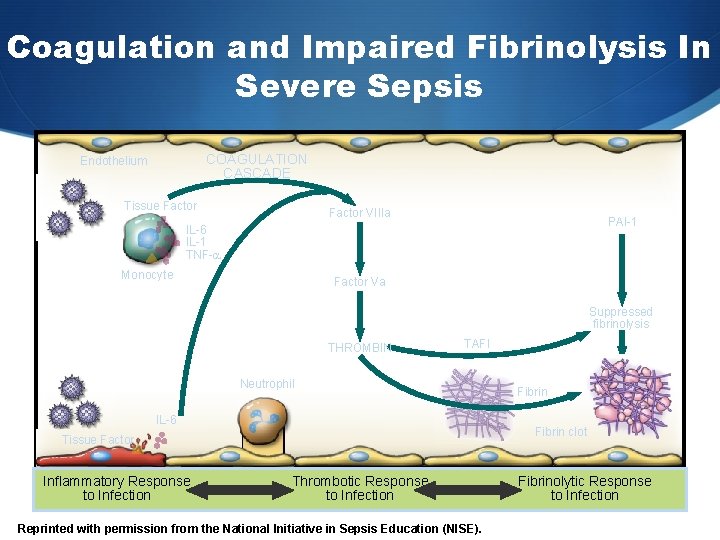
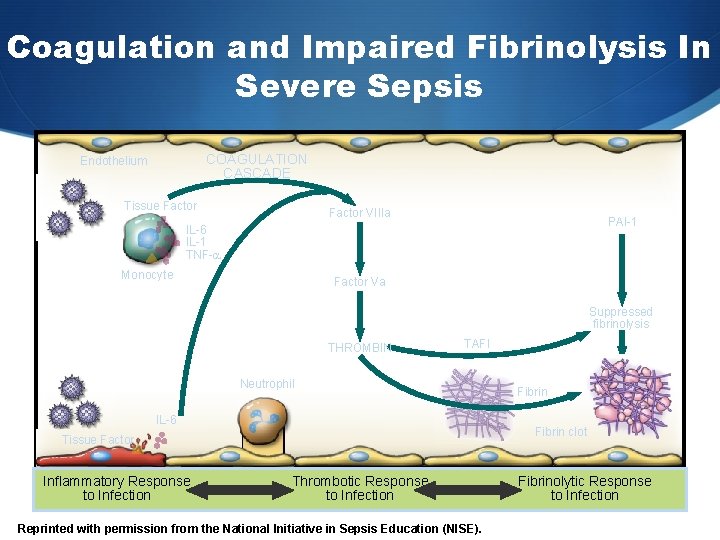
Coagulation and Impaired Fibrinolysis In Severe Sepsis COAGULATION CASCADE Endothelium Tissue Factor VIIIa PAI-1 IL-6 IL-1 TNF- Monocyte Factor Va Suppressed fibrinolysis THROMBIN TAFI Neutrophil IL-6 Fibrin clot Tissue Factor Inflammatory Response to Infection Fibrin Thrombotic Response to Infection Reprinted with permission from the National Initiative in Sepsis Education (NISE). Fibrinolytic Response to Infection
“Except on few occasions, the patient appears to die from the body's response to infection rather than from it. ” Sir William Osler – 1904 The Evolution of Modern Medicine
The Response to Pathogens, Involving "Cross-Talk" among Many Immune Cells, Including Macrophages, Dendritic Cells, and CD 4 T Cells Hotchkiss, R. S. et al. N Engl J Med 2003; 348: 138 -150
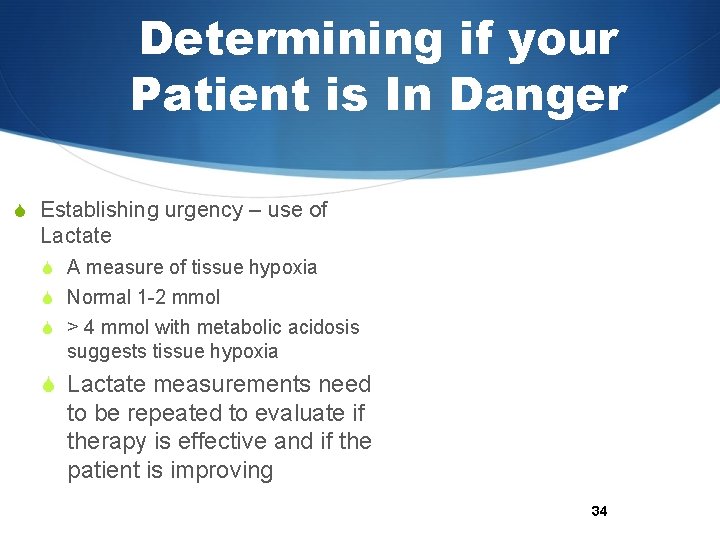
Determining if your Patient is In Danger S Establishing urgency – use of Lactate S A measure of tissue hypoxia S Normal 1 -2 mmol S > 4 mmol with metabolic acidosis suggests tissue hypoxia S Lactate measurements need to be repeated to evaluate if therapy is effective and if the patient is improving 34
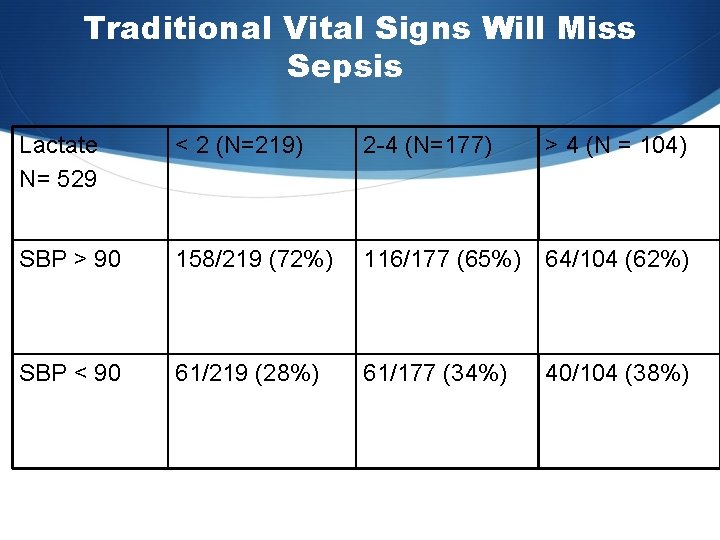
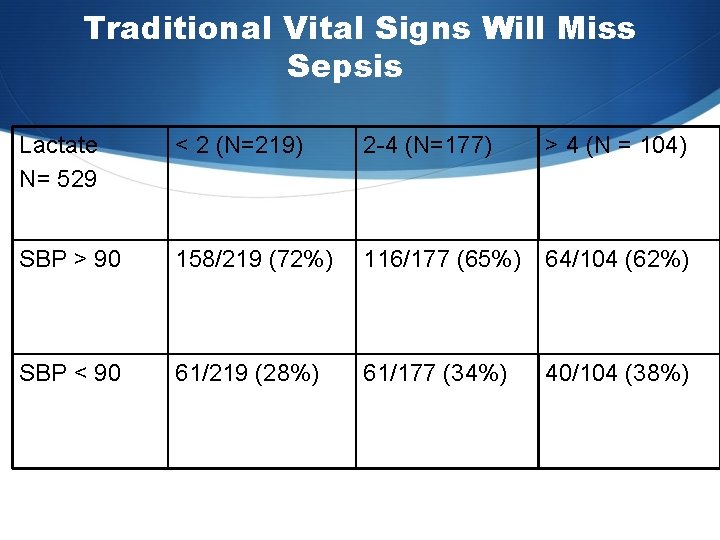
Traditional Vital Signs Will Miss Sepsis Lactate N= 529 < 2 (N=219) 2 -4 (N=177) > 4 (N = 104) SBP > 90 158/219 (72%) 116/177 (65%) 64/104 (62%) SBP < 90 61/219 (28%) 61/177 (34%) 40/104 (38%)
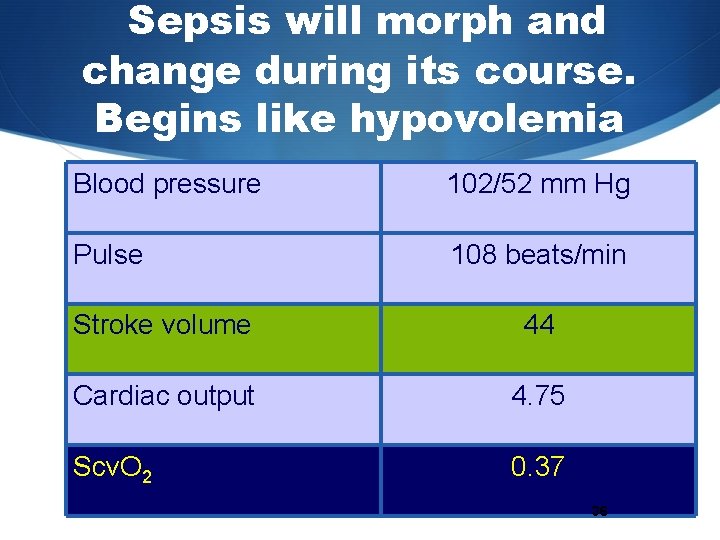
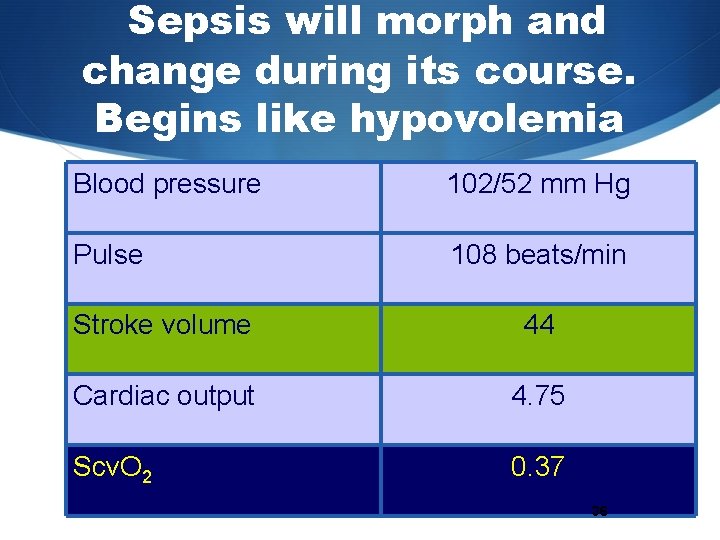
Sepsis will morph and change during its course. Begins like hypovolemia Blood pressure 102/52 mm Hg Pulse 108 beats/min Stroke volume 44 Cardiac output 4. 75 Scv. O 2 0. 37 36
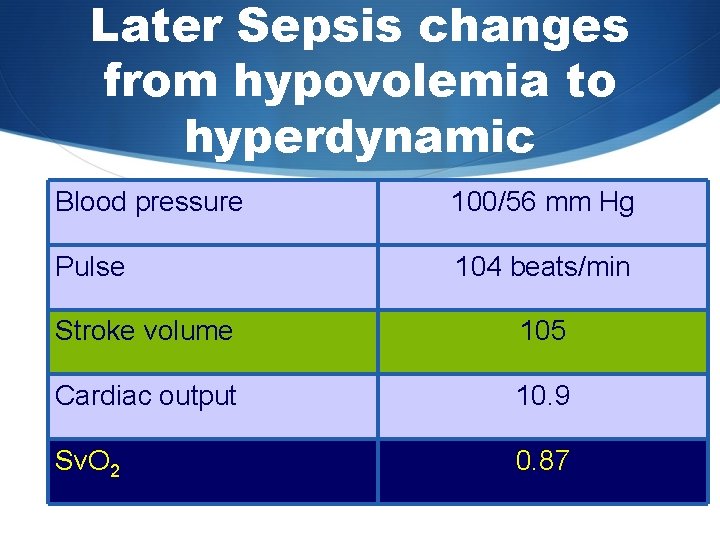
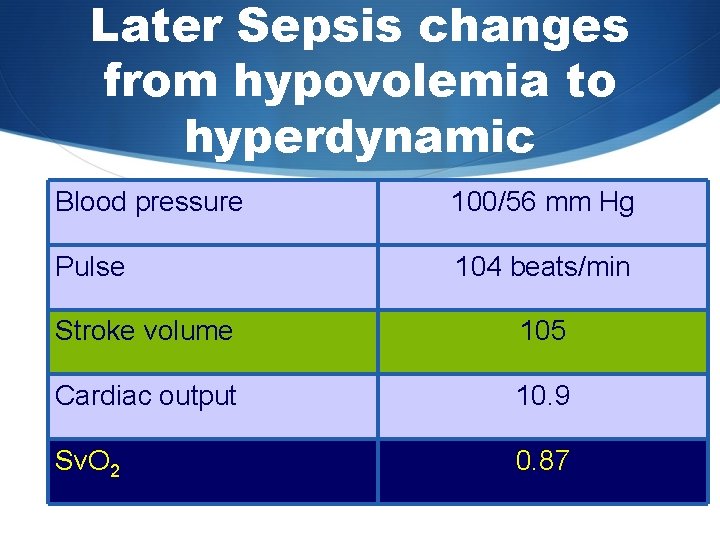
Later Sepsis changes from hypovolemia to hyperdynamic Blood pressure 100/56 mm Hg Pulse 104 beats/min Stroke volume 105 Cardiac output 10. 9 Sv. O 2 0. 87
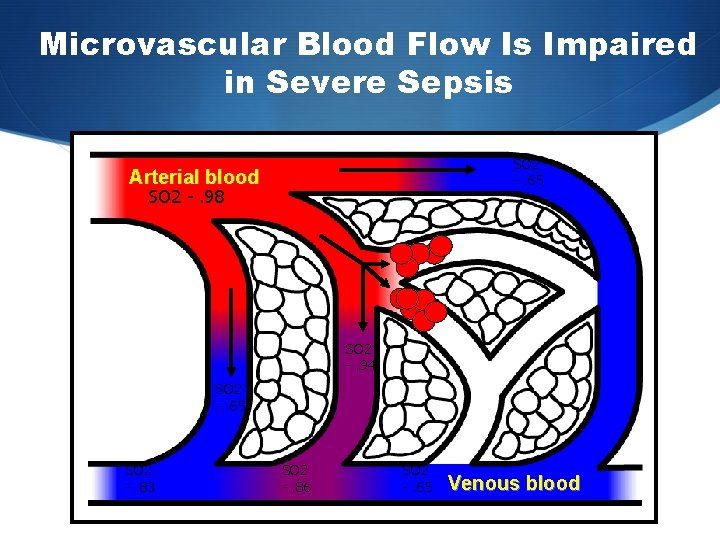
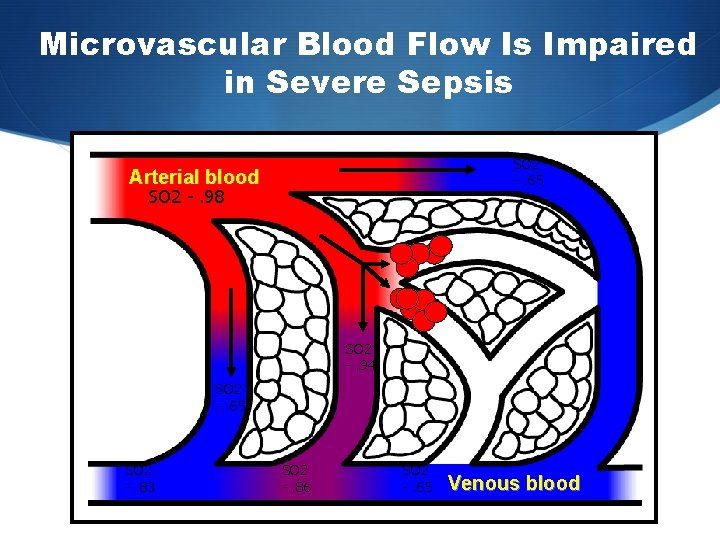
Microvascular Blood Flow Is Impaired in Severe Sepsis SO 2 -. 65 Arterial blood SO 2 -. 98 SO 2 -. 94 SO 2 -. 65 SO 2 -. 83 SO 2 -. 86 SO 2 -. 65 Venous blood
Sepsis often progresses when the host cannot contain the primary infection S A problem most often related to S characteristics of the microorganism, S such as a high burden of infection S the presence of super antigens and other virulence factors, S resistance to phagocytosis S antibiotic resistance.
Cell dysoxia S Epithelial cells have diminished oxygen consumption S due to a depletion of nicotinamide adenine dinucleotide (NAD) S Concept of cell stunning or hibernation
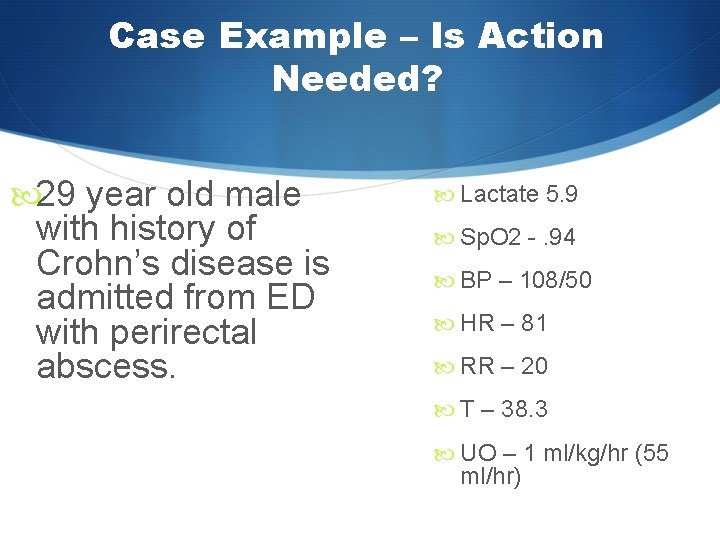
Case Example – Is Action Needed? 29 year old male with history of Crohn’s disease is admitted from ED with perirectal abscess. Lactate 5. 9 Sp. O 2 -. 94 BP – 108/50 HR – 81 RR – 20 T – 38. 3 UO – 1 ml/kg/hr (55 ml/hr)
How do We Identify Sepsis Now? In absence of biomarkers, must rely on crude physical indicators S
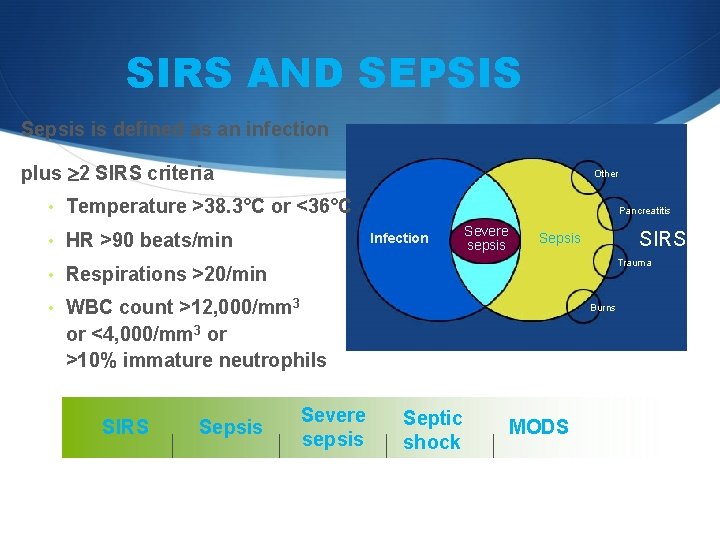
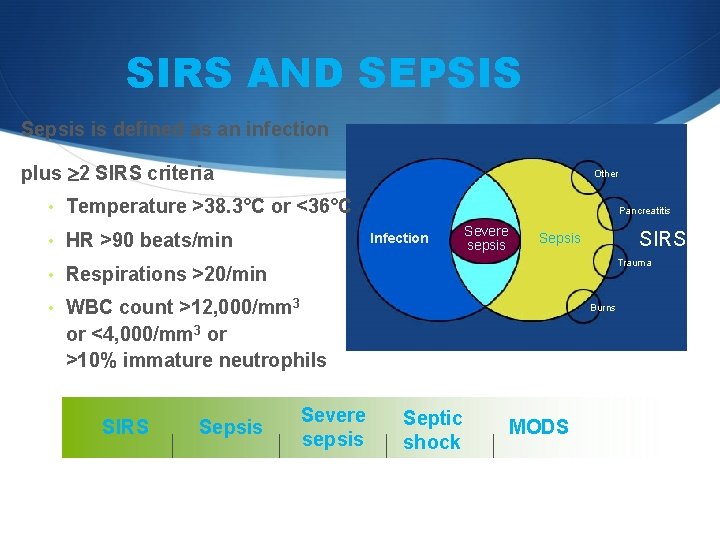
SIRS AND SEPSIS Sepsis is defined as an infection plus 2 SIRS criteria Other • Temperature >38. 3°C or <36°C • HR >90 beats/min Pancreatitis Infection Severe sepsis SIRS Sepsis Trauma • Respirations >20/min • WBC count >12, 000/mm 3 Burns or <4, 000/mm 3 or >10% immature neutrophils SIRS Sepsis Severe sepsis Levy MM, et al. Crit Care Med. 2003; 31: 1250 -1256. Septic shock MODS
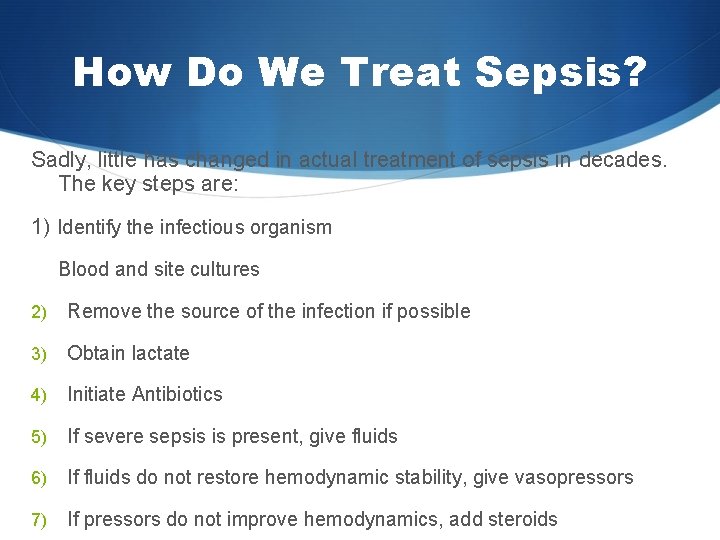
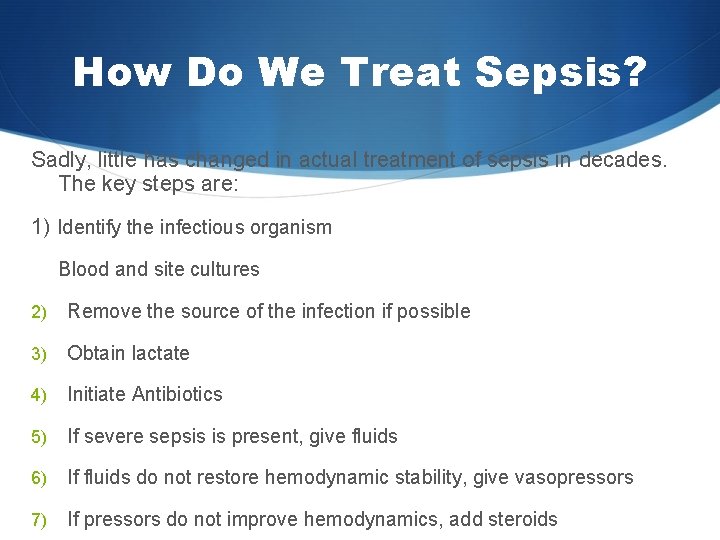
How Do We Treat Sepsis? Sadly, little has changed in actual treatment of sepsis in decades. The key steps are: 1) Identify the infectious organism Blood and site cultures 2) Remove the source of the infection if possible 3) Obtain lactate 4) Initiate Antibiotics 5) If severe sepsis is present, give fluids 6) If fluids do not restore hemodynamic stability, give vasopressors 7) If pressors do not improve hemodynamics, add steroids
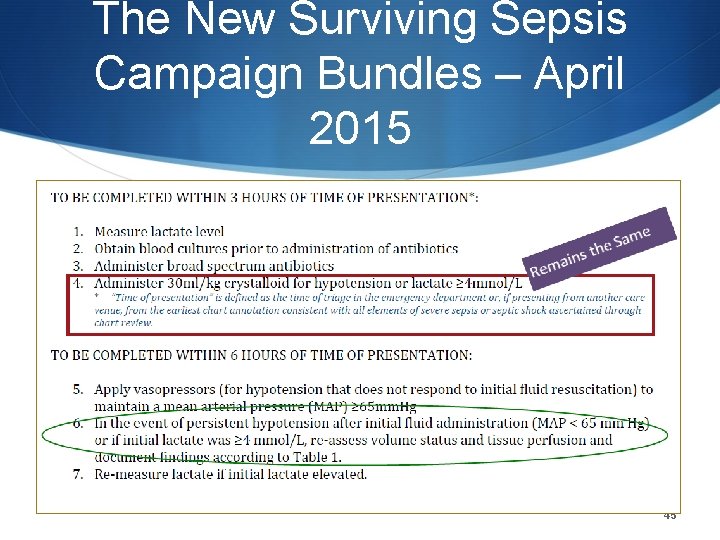
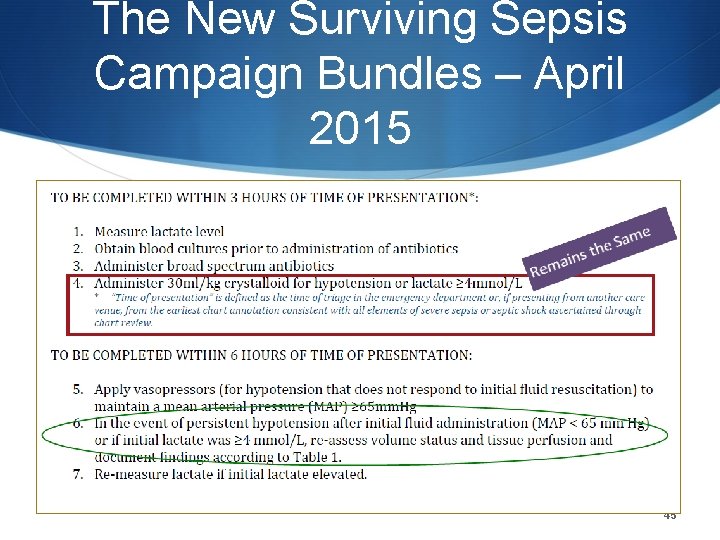
The New Surviving Sepsis Campaign Bundles – April 2015 45
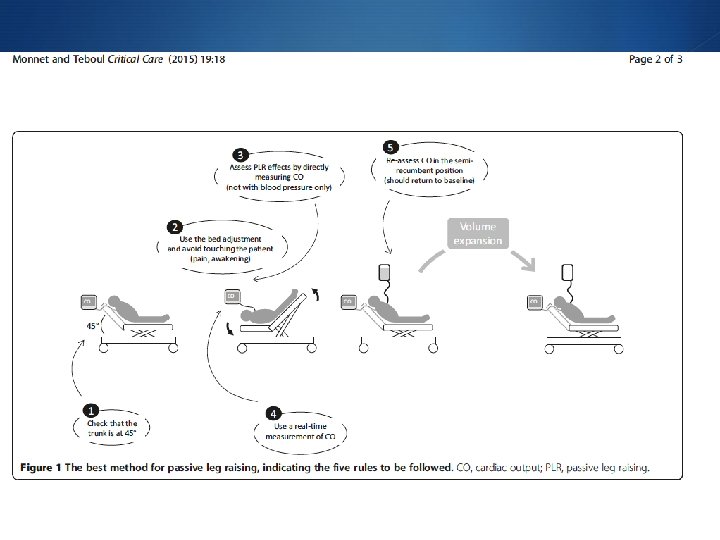
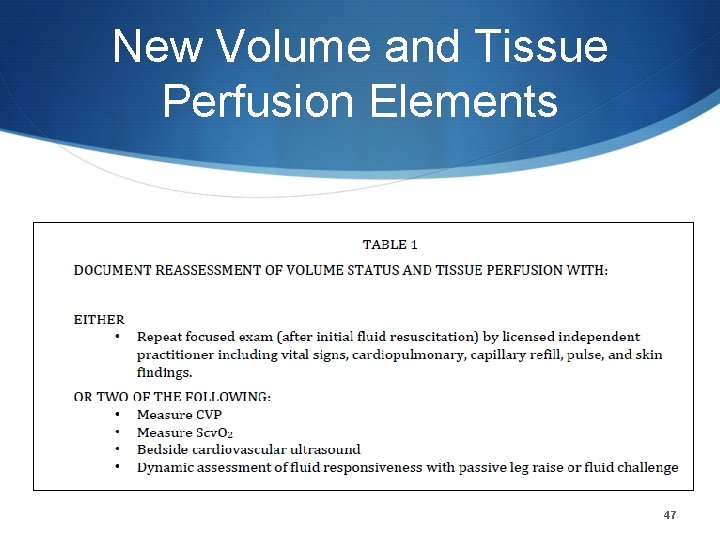
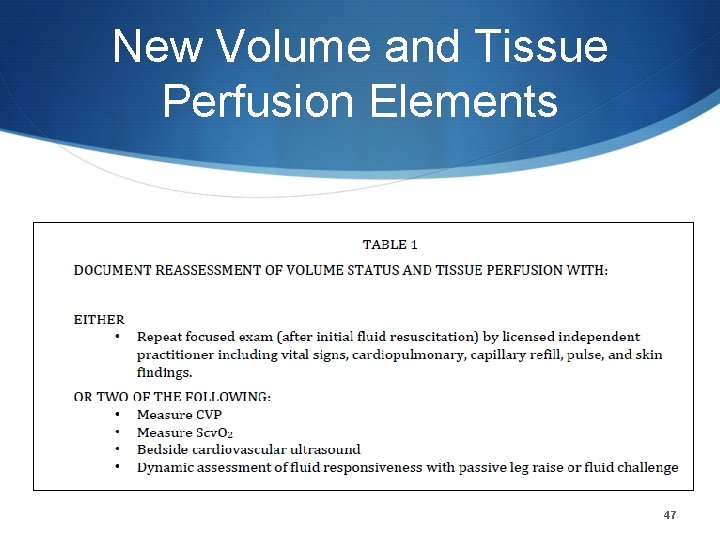
New Volume and Tissue Perfusion Elements 47
History of Treating Severe Sepsis Clinical tx – fluids, vasopressors & antibiotics Afelimomab Anti TNF F monoclonol antibody fragment Pafase A 2 s. PL
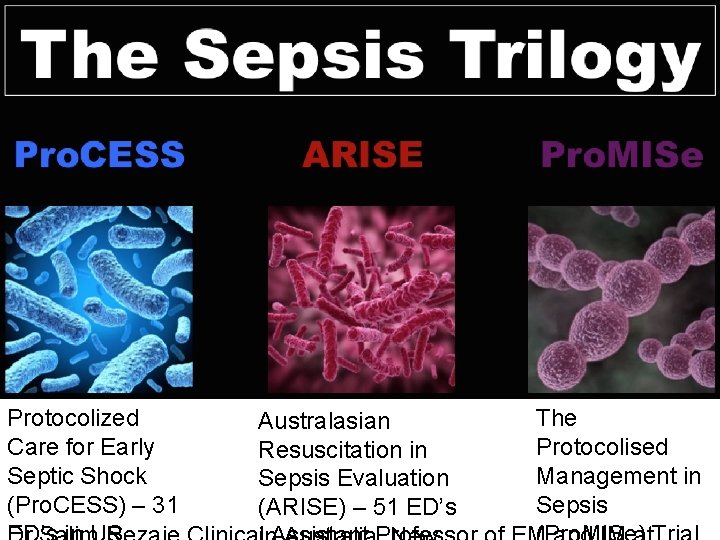
Protocolized Care for Early Septic Shock (Pro. CESS) – 31 Australasian Resuscitation in Sepsis Evaluation (ARISE) – 51 ED’s The Protocolised Management in Sepsis
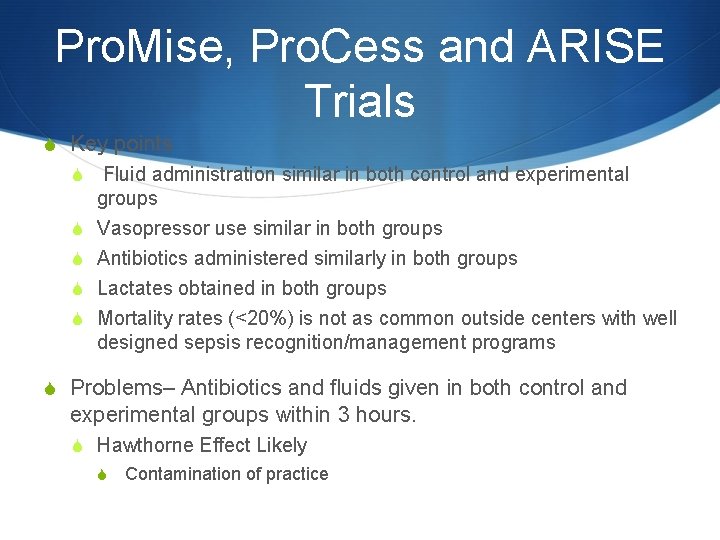
Pro. Mise, Pro. Cess and ARISE Trials S Key points S Fluid administration similar in both control and experimental S S groups Vasopressor use similar in both groups Antibiotics administered similarly in both groups Lactates obtained in both groups Mortality rates (<20%) is not as common outside centers with well designed sepsis recognition/management programs S Problems– Antibiotics and fluids given in both control and experimental groups within 3 hours. S Hawthorne Effect Likely S Contamination of practice
Take away Points S If Patients are S identified early, S Receive antibiotics EARLY S receive IVF EARLY S Then Scv. O 2 and CVP monitoring does not seem to add a benefit S BUT EGDT with Scv. O 2 not really tested since resuscitation had already occurred
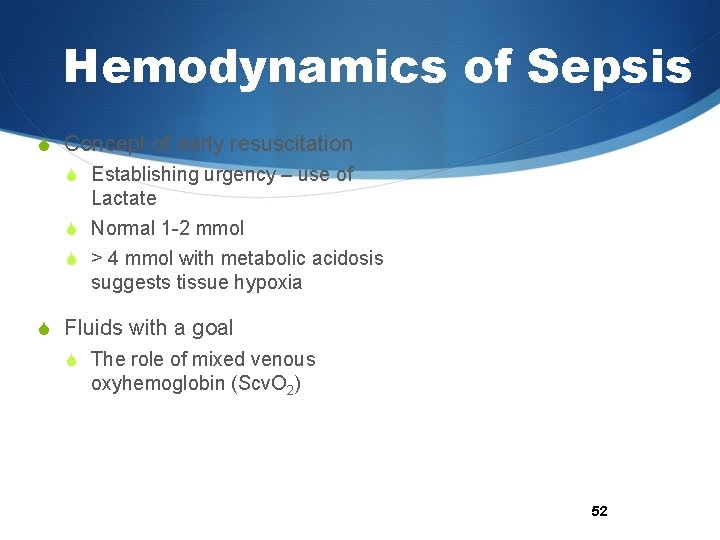
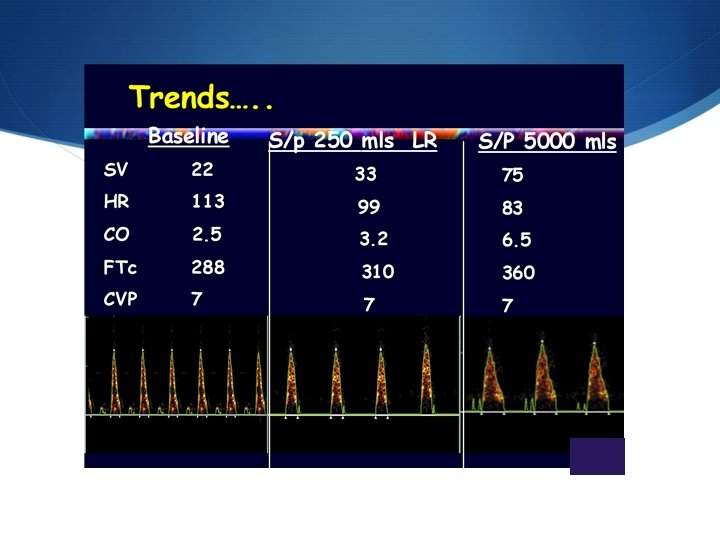
Hemodynamics of Sepsis S Concept of early resuscitation S Establishing urgency – use of Lactate S Normal 1 -2 mmol S > 4 mmol with metabolic acidosis suggests tissue hypoxia S Fluids with a goal S The role of mixed venous oxyhemoglobin (Scv. O 2) 52
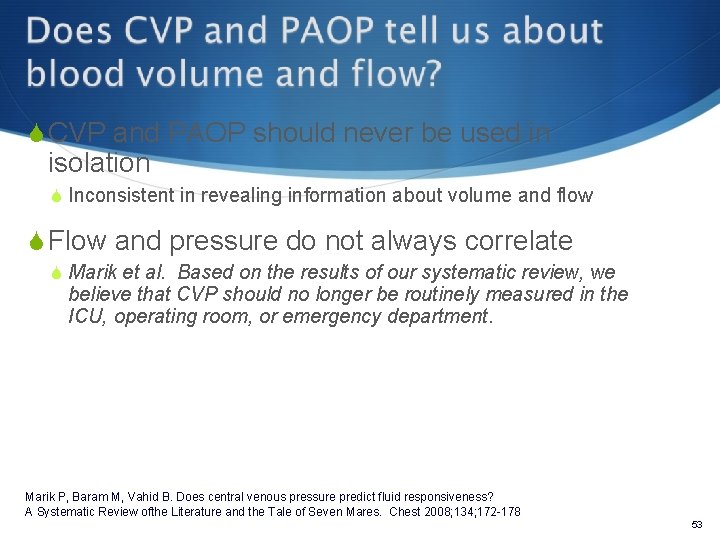
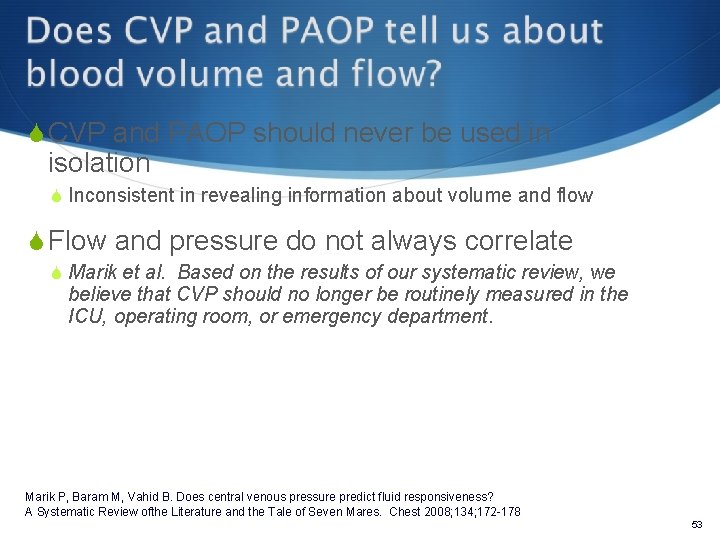
S CVP and PAOP should never be used in isolation S Inconsistent in revealing information about volume and flow S Flow and pressure do not always correlate S Marik et al. Based on the results of our systematic review, we believe that CVP should no longer be routinely measured in the ICU, operating room, or emergency department. Marik P, Baram M, Vahid B. Does central venous pressure predict fluid responsiveness? A Systematic Review ofthe Literature and the Tale of Seven Mares. Chest 2008; 134; 172 -178 53
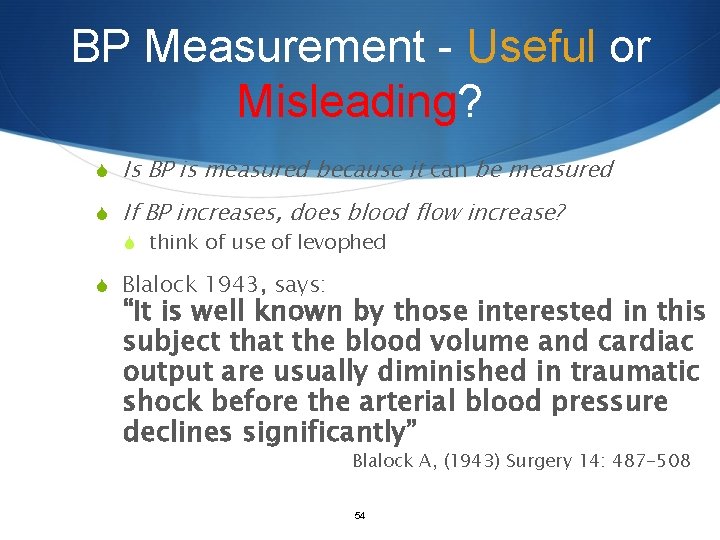
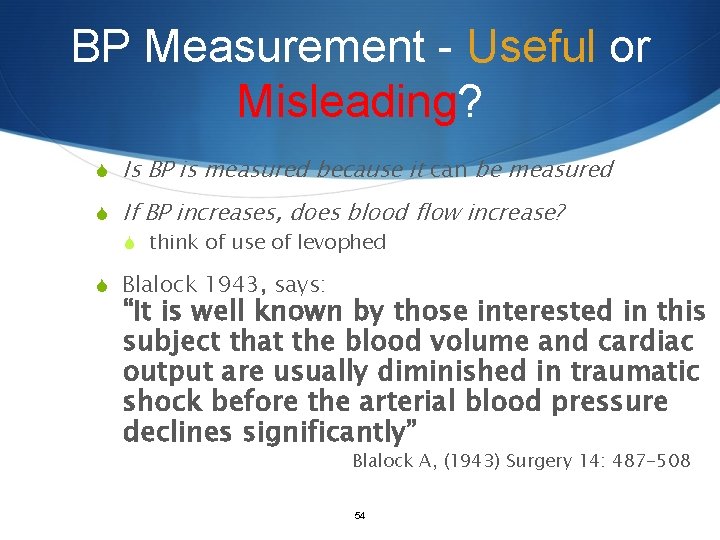
BP Measurement - Useful or Misleading? S Is BP is measured because it can be measured S If BP increases, does blood flow increase? S think of use of levophed S Blalock 1943, says: “It is well known by those interested in this subject that the blood volume and cardiac output are usually diminished in traumatic shock before the arterial blood pressure declines significantly” Blalock A, (1943) Surgery 14: 487 -508 54
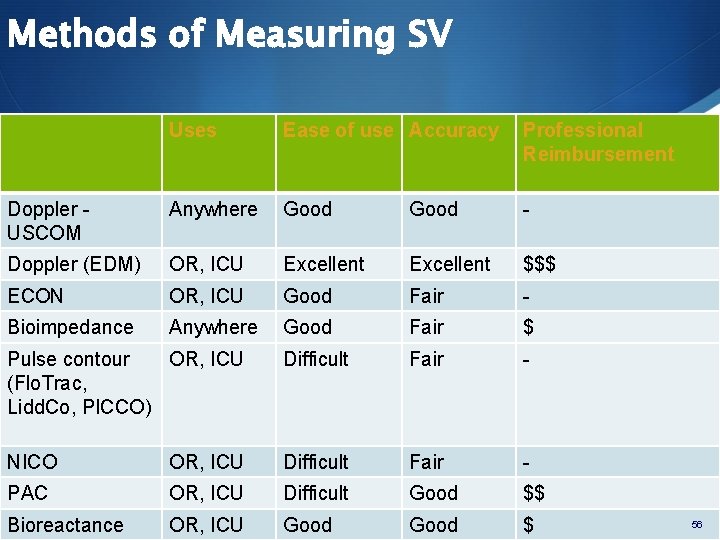
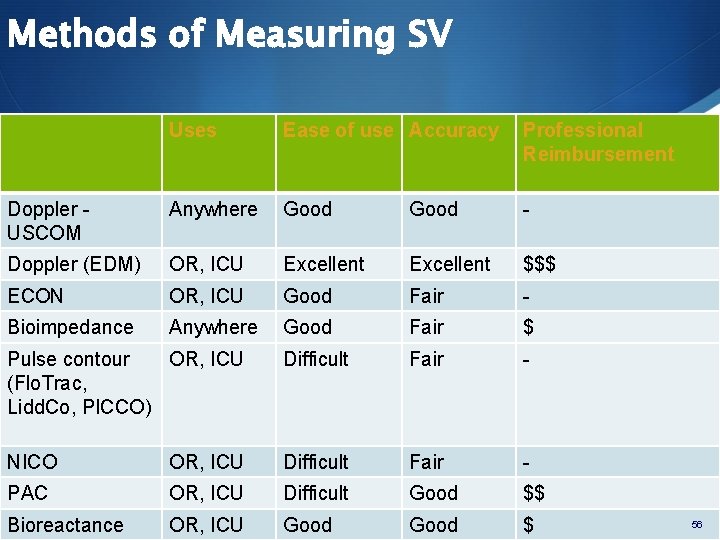
Methods of Measuring SV Uses Ease of use Accuracy Professional Reimbursement Doppler - USCOM Anywhere Good - Doppler (EDM) OR, ICU Excellent $$$ ECON OR, ICU Good Fair - Bioimpedance Anywhere Good Fair $ Pulse contour OR, ICU (Flo. Trac, Lidd. Co, PICCO) Difficult Fair - NICO OR, ICU Difficult Fair - PAC OR, ICU Difficult Good $$ Bioreactance OR, ICU Good $ 56
Non invasive CO/SV measurement
Diagnostics S Cultures as clinically appropriate before antimicrobial therapy if no significant delay (> 45 mins) in the start of antimicrobial(s) (grade 1 C). At least 2 sets of blood cultures (both aerobic and anaerobic bottles) be obtained before antimicrobial therapy with at least 1 drawn percutaneously and 1 drawn through each vascular access device, unless the device was recently (<48 hrs) inserted (grade 1 C). S Imaging studies performed promptly to confirm a potential source of infection (UG).
Antibiotics S Administration of effective intravenous antimicrobials within the first hour of recognition of septic shock (grade 1 B) and severe sepsis without septic shock (grade 1 C) as the goal of therapy. S Broad spectrum antibiotics should be initiated Initial empiric anti-infective therapy of one or more drugs that have activity against all likely pathogens and that penetrate in adequate concentrations into tissues presumed to be the source of sepsis (grade 1 B). S Antimicrobial regimen should be reassessed daily for potential deescalation (grade 1 B). S S Use of low procalcitonin levels or similar biomarkers to assist the clinician in the discontinuation of empiric antibiotics in patients who initially appeared septic, but have no subsequent evidence of infection (grade 2 C).
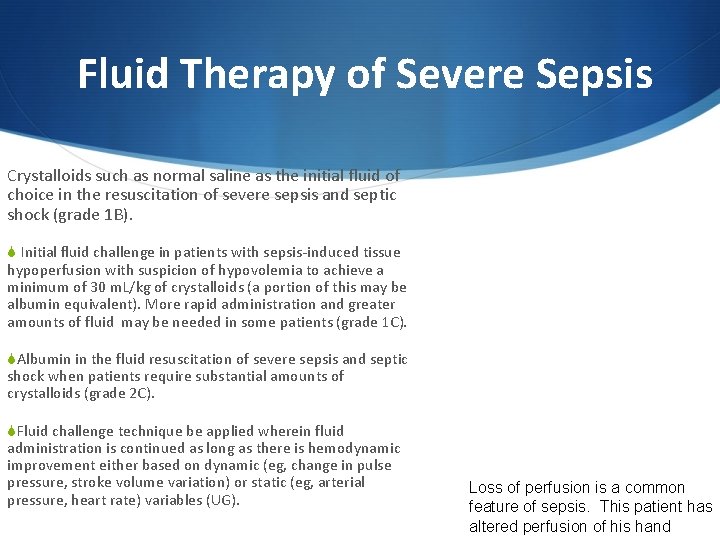
Fluid Therapy of Severe Sepsis Crystalloids such as normal saline as the initial fluid of choice in the resuscitation of severe sepsis and septic shock (grade 1 B). S Initial fluid challenge in patients with sepsis-induced tissue hypoperfusion with suspicion of hypovolemia to achieve a minimum of 30 m. L/kg of crystalloids (a portion of this may be albumin equivalent). More rapid administration and greater amounts of fluid may be needed in some patients (grade 1 C). SAlbumin in the fluid resuscitation of severe sepsis and septic shock when patients require substantial amounts of crystalloids (grade 2 C). SFluid challenge technique be applied wherein fluid administration is continued as long as there is hemodynamic improvement either based on dynamic (eg, change in pulse pressure, stroke volume variation) or static (eg, arterial pressure, heart rate) variables (UG). Loss of perfusion is a common feature of sepsis. This patient has altered perfusion of his hand
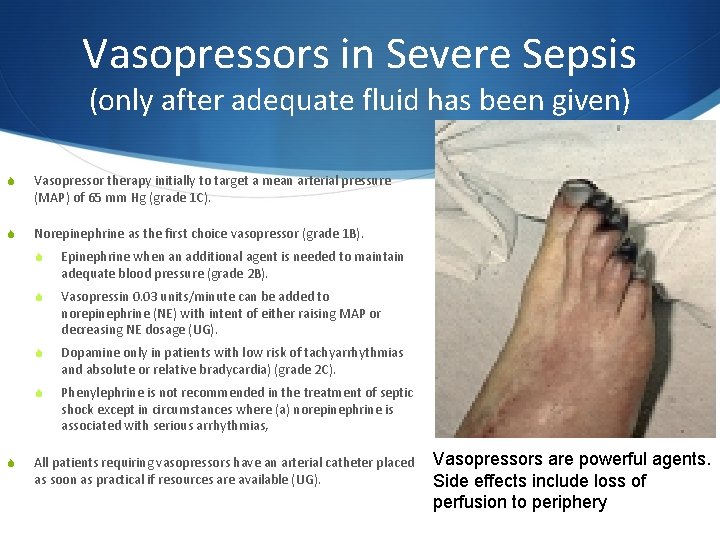
Vasopressors in Severe Sepsis (only after adequate fluid has been given) S Vasopressor therapy initially to target a mean arterial pressure (MAP) of 65 mm Hg (grade 1 C). S Norepinephrine as the first choice vasopressor (grade 1 B). S S Epinephrine when an additional agent is needed to maintain adequate blood pressure (grade 2 B). S Vasopressin 0. 03 units/minute can be added to norepinephrine (NE) with intent of either raising MAP or decreasing NE dosage (UG). S Dopamine only in patients with low risk of tachyarrhythmias and absolute or relative bradycardia) (grade 2 C). S Phenylephrine is not recommended in the treatment of septic shock except in circumstances where (a) norepinephrine is associated with serious arrhythmias, All patients requiring vasopressors have an arterial catheter placed as soon as practical if resources are available (UG). Vasopressors are powerful agents. Side effects include loss of perfusion to periphery
Corticosteroids in Severe Sepsis S Intravenous hydrocortisone only if adequate fluid resuscitation and vasopressor therapy are unable to restore hemodynamic stability S suggest intravenous hydrocortisone alone at a dose of 200 mg per day (grade 2 C). S In treated patients hydrocortisone tapered when vasopressors are no longer required (grade 2 D). S When hydrocortisone is given, use continuous flow (grade 2 D).
Setting Goals S Discuss goals of care and prognosis with patients and families (grade 1 B). S Sepsis has a high mortality rate. Families should understand recognize that determining what the patient’s wishes are may help dictate the aggressiveness of therapy S Incorporate goals of care into treatment and end-of-life care planning, utilizing palliative care principles where appropriate (grade 1 B). S Address goals of care as early as feasible, but no later than within 72 hours of ICU admission (grade 2 C).
Summary S Prevent Infections S Early treatment S Identify agent S Remove source S Antibiotics S Fluids S Pressors S Steroids S Set goals for end of life
Case Study 1 S
• 63 year old male in MICU with CAP, pneumothorax • Progressing well but on day 4 • Develops spontaneous pneumothorax • RLL infiltrate Case Study 1 • Temp increases to 39. 1 • P – 122 • BP – 82/52 (following EGDT) • WBC 16, 500 • Is SOB, requires intubation, 50% FIO 2, AMV • 12/14, Vt – 500 ccs, PEEP +10 • Day 4 • Sp. O 2 -. 92, Pa. O 2 64 (P/F ratio > 100), p. H 7. 28, Pa. CO 2 32, HCO 3 - 17 • Sepsis is suspected with treatment rapidly started • Has received EGDT • 4 L NS • Lactate 6. 2 • Platelets – 110, 000
What to do? S What is happening? S Any therapies missing? S Family communication issues?
Case Study 2 • 33 -year-old, 150 kg female with failed gastric bypass • Bowel was nicked during surgery • 4 days post-op develops • • wound infection 8 liters of fluids over past 48 hours On cefotaxime and gentamicin Norepinephrine at 10 µg/min Hydrocortisone 200 mg IV daily PEEP 12 cm H 2 O, Fi. O 2 90% Sedated (RASS – -2) Lactate 5. 9
Summary S Recognize sepsis early S All infections should be examined for signs of SIRS S IF sepsis is present S Obtain blood or site cultures S Obtain lactate S Initiate antibiotics S If organ failure is present, or increased lactate – give 30 ml/kg of fluids S If these measures are done in a timely basis, sepsis mortality can be reduced 50%