SENSORY EXAMINATION PT 6280 Clinical Assessment University of
- Slides: 49
SENSORY EXAMINATION PT 6280: Clinical Assessment University of Minnesota Division of Physical Therapy Teresa Bisson, PT, DPT, NCS, ATP
Read Before Class • Guyton and Hall – Textbook of Medical Physiology, 13 th ed • Go to MNCAT link: https: //primo. lib. umn. edu/primoexplore/fulldisplay? docid=UMN_ALMA 51623776890001701&context=L&vid= TWINCITIES&search_scope=all_campus&tab=default_tab&lang=en_US • Click on “Elsevier Clinical. Key Books” • Do NOT click on “Ebrary (Twin Cities)” • Click on “ 48. Somatic Sensations: I. General Organization, the Tactile and Position Senses” • Read through (and including) “Spatial Orientation of Signals from Different Parts in the Body in Somatosensory Area I” • Skip from “Layers of Somatosensory Cortex and Their Function” through “Power Law“ • Resume reading at “Position Senses” and finish to end
Objectives for today and Friday The student will be able to: • Identify and discuss the rationale for conducting a sensory examination • Describe the basic anatomy of the sensory system • Describe tracts that carry sensory information • Perform sensation and deep tendon reflex testing accurately and with good technique • Discuss factors that may interfere with sensory testing • Identify type of injury given the distribution of sensory loss
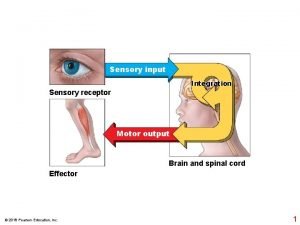
Purposes of the Sensory System • Code and transmit information about the body and the environment • Safety/protection • Influences motor responses/mobility
Rationale for Sensory Examination • Assess integrity of the sensory system • Source/cause of nerve injury • Degree of sensory loss/impairment • Impact on movement! • Understand patient safety risks • Prevent secondary complications • Prognosis of injury/recovery • Formulate goals • Plan appropriate therapeutic intervention
What are we trying to figure out? • When the cause of sensory loss is known: is the sensory loss following a pattern consistent with the diagnosis? • When the cause of sensory loss is unknown: where in the system has the injury occurred? • Cortex and/or subcortical structures • Spinal cord • Spinal nerve root • Peripheral nerve(s)
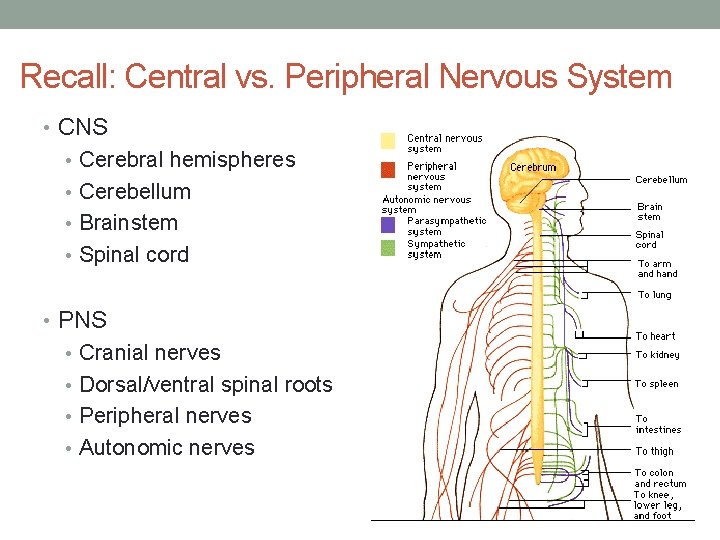
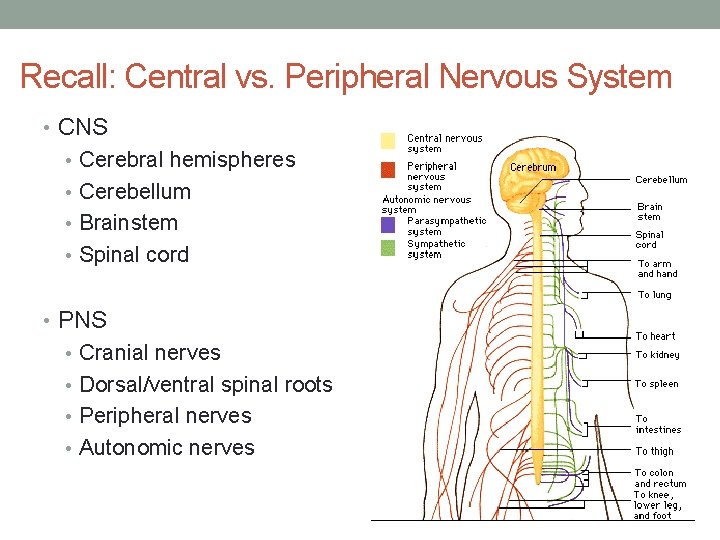
Recall: Central vs. Peripheral Nervous System • CNS • Cerebral hemispheres • Cerebellum • Brainstem • Spinal cord • PNS • Cranial nerves • Dorsal/ventral spinal roots • Peripheral nerves • Autonomic nerves
WORKING FROM THE OUTSIDE IN…. . Receptors Peripheral nerves Spinal cord pathways Subcortical structures Cortex
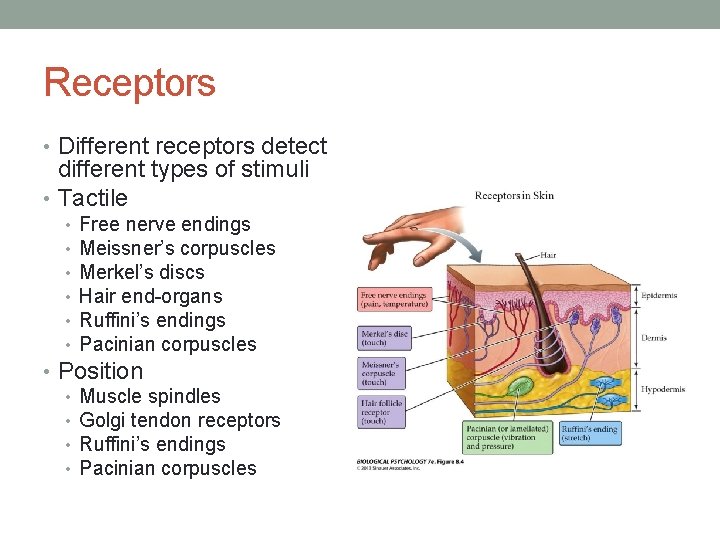
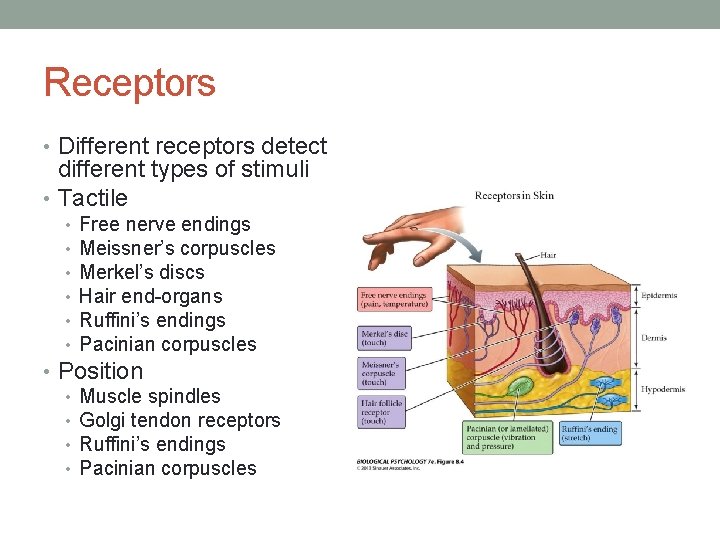
Receptors • Different receptors detect different types of stimuli • Tactile • • • Free nerve endings Meissner’s corpuscles Merkel’s discs Hair end-organs Ruffini’s endings Pacinian corpuscles • Position • Muscle spindles • Golgi tendon receptors • Ruffini’s endings • Pacinian corpuscles
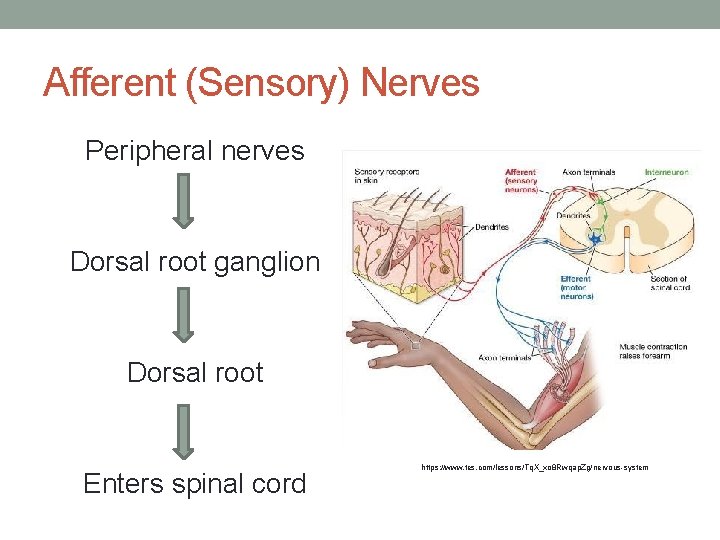
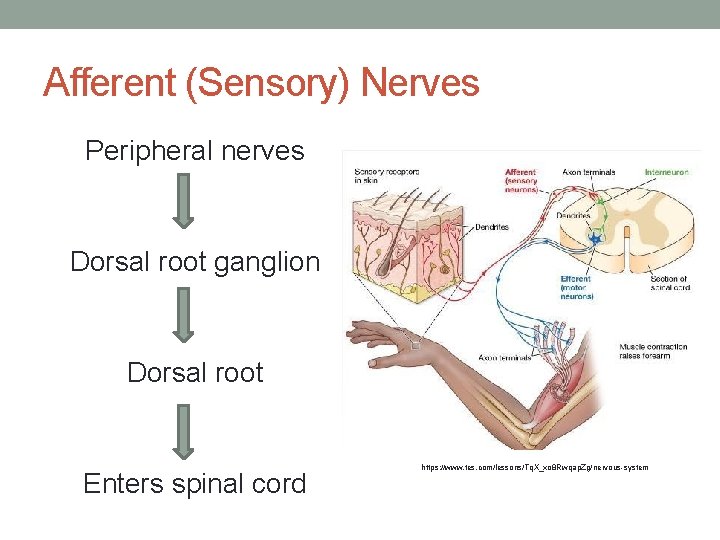
Afferent (Sensory) Nerves Peripheral nerves Dorsal root ganglion Dorsal root Enters spinal cord https: //www. tes. com/lessons/Tq. X_xo 8 Rwqap. Zg/nervous-system
Spinal Cord Pathways • Dorsal Column-Medial Lemniscus System • Spinothalamic Tracts • Anterior • Lateral
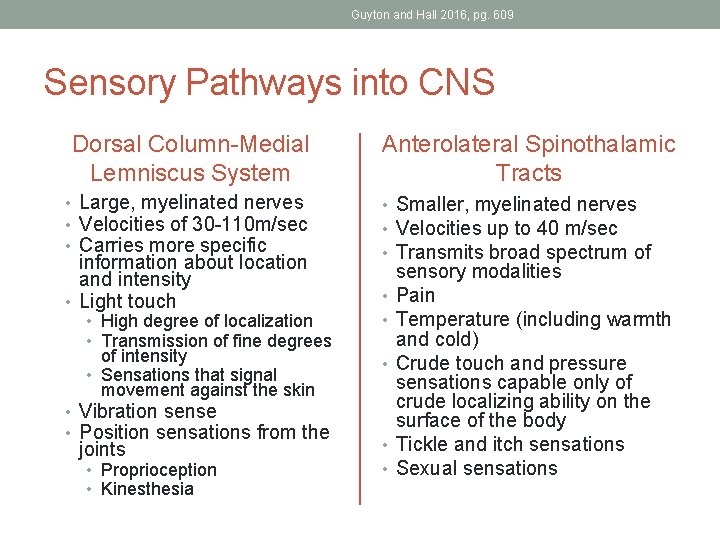
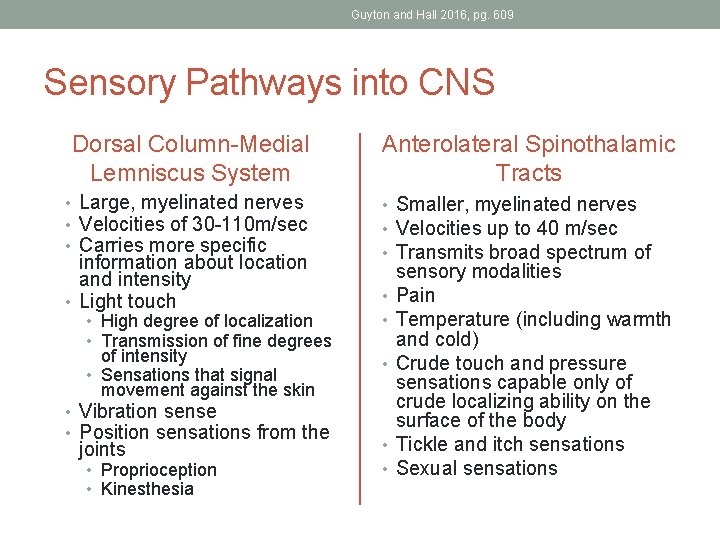
Guyton and Hall 2016, pg. 609 Sensory Pathways into CNS Dorsal Column-Medial Lemniscus System • Large, myelinated nerves • Velocities of 30 -110 m/sec • Carries more specific information about location and intensity • Light touch • High degree of localization • Transmission of fine degrees of intensity • Sensations that signal movement against the skin • Vibration sense • Position sensations from the joints • Proprioception • Kinesthesia Anterolateral Spinothalamic Tracts • Smaller, myelinated nerves • Velocities up to 40 m/sec • Transmits broad spectrum of • • • sensory modalities Pain Temperature (including warmth and cold) Crude touch and pressure sensations capable only of crude localizing ability on the surface of the body Tickle and itch sensations Sexual sensations
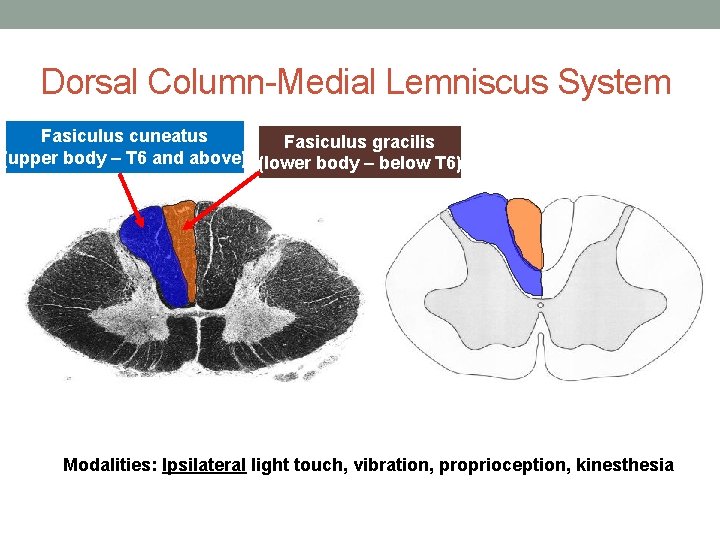
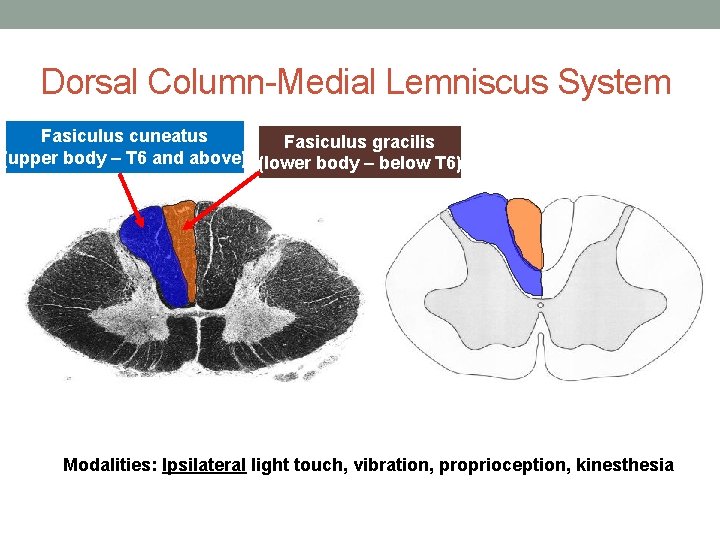
Dorsal Column-Medial Lemniscus System Fasiculus cuneatus Fasiculus gracilis (upper body – T 6 and above) (lower body – below T 6) Modalities: Ipsilateral light touch, vibration, proprioception, kinesthesia
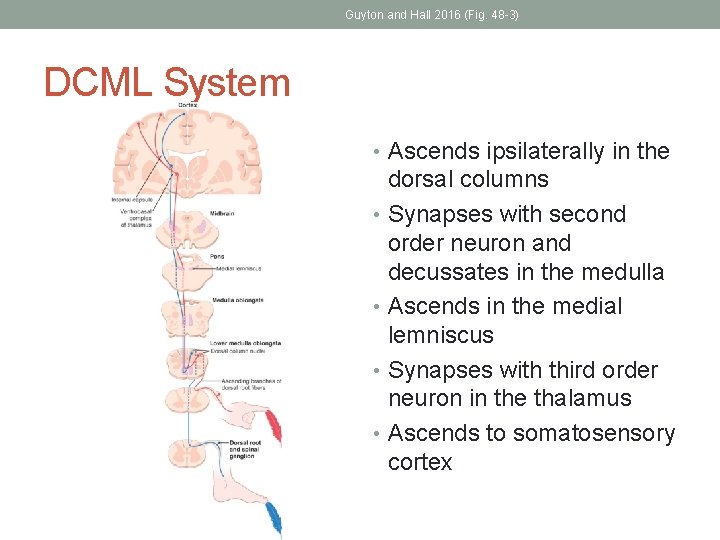
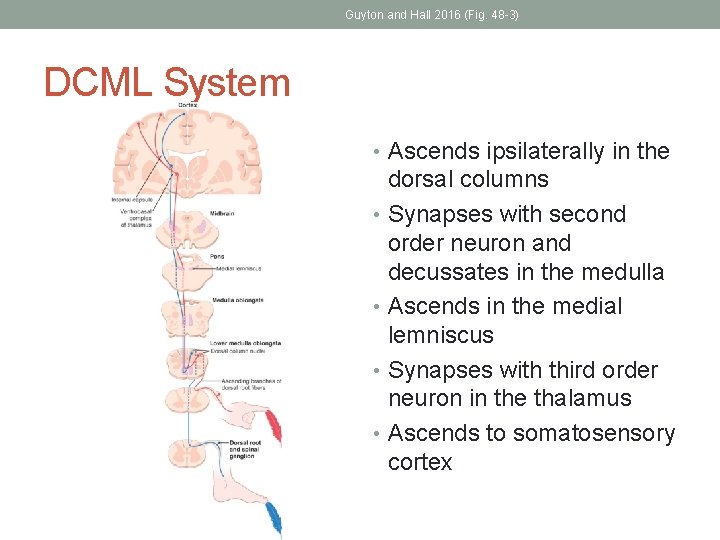
Guyton and Hall 2016 (Fig. 48 -3) DCML System • Ascends ipsilaterally in the dorsal columns • Synapses with second order neuron and decussates in the medulla • Ascends in the medial lemniscus • Synapses with third order neuron in the thalamus • Ascends to somatosensory cortex
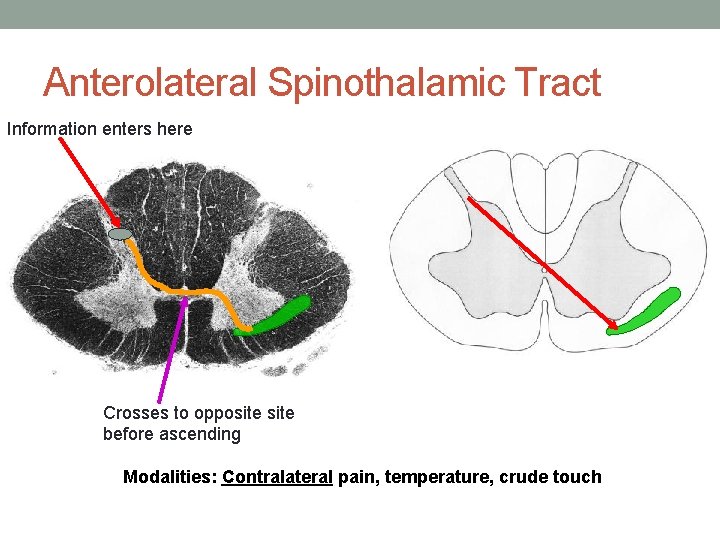
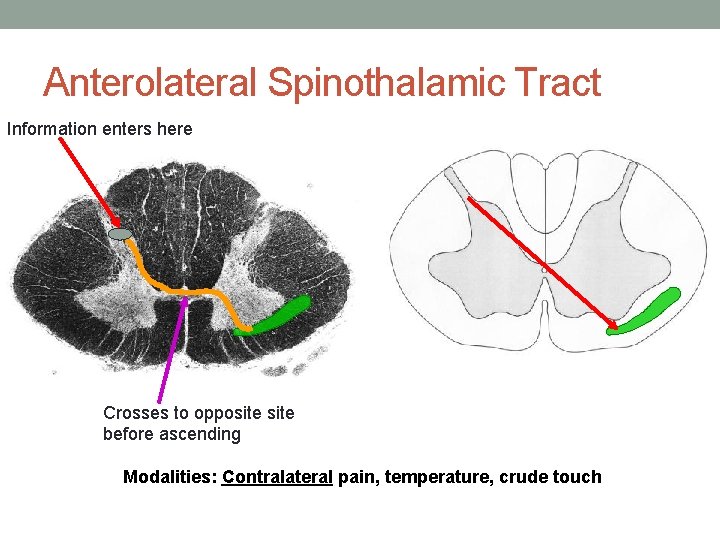
Anterolateral Spinothalamic Tract Information enters here Crosses to opposite before ascending Modalities: Contralateral pain, temperature, crude touch
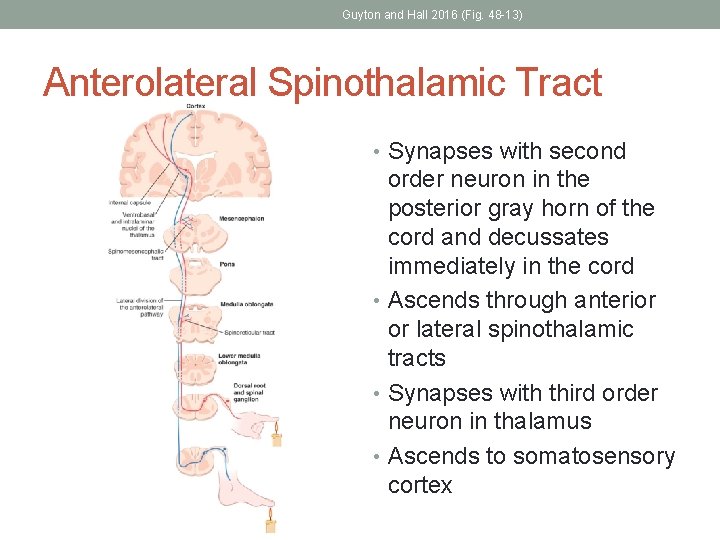
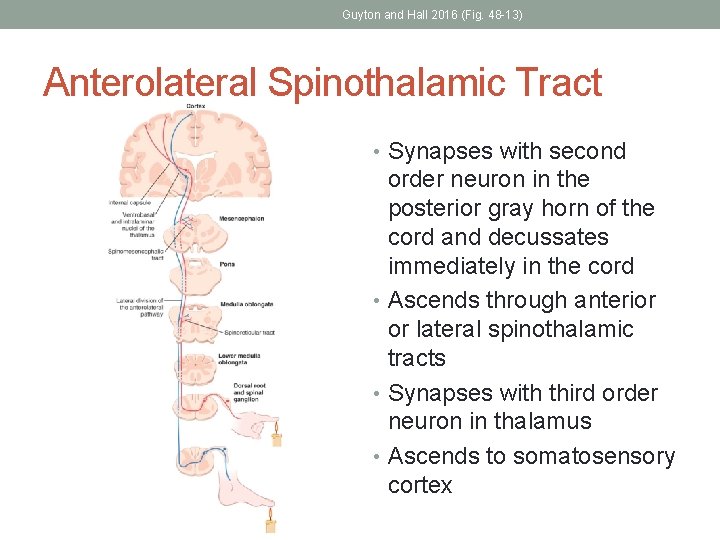
Guyton and Hall 2016 (Fig. 48 -13) Anterolateral Spinothalamic Tract • Synapses with second order neuron in the posterior gray horn of the cord and decussates immediately in the cord • Ascends through anterior or lateral spinothalamic tracts • Synapses with third order neuron in thalamus • Ascends to somatosensory cortex
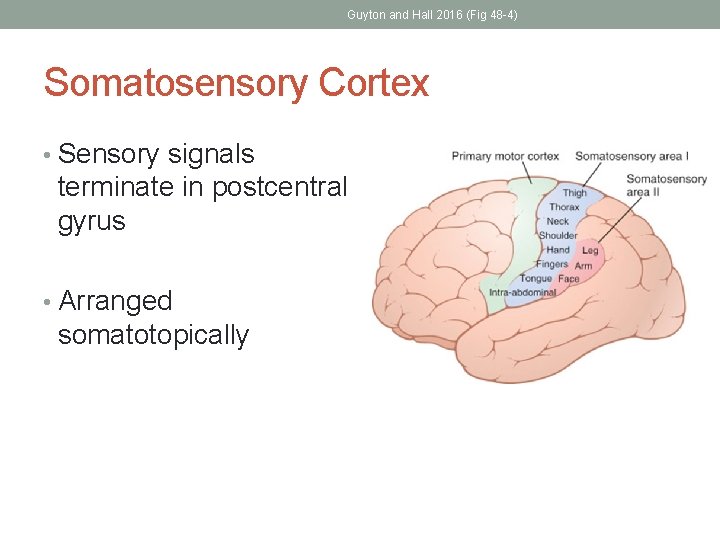
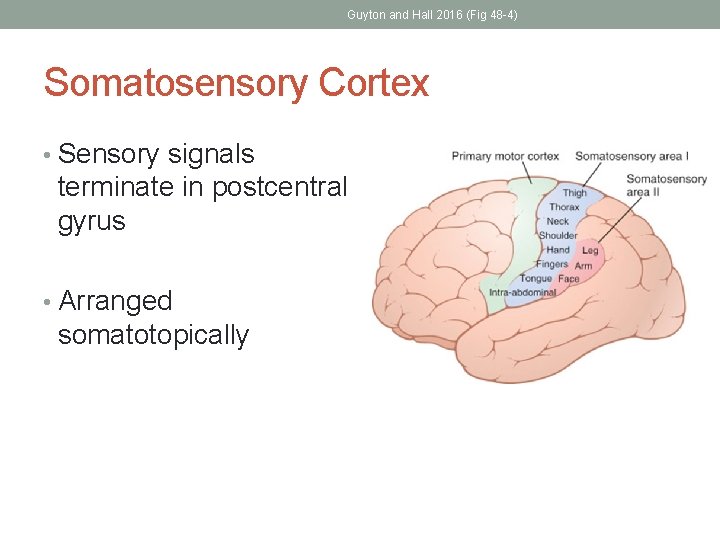
Guyton and Hall 2016 (Fig 48 -4) Somatosensory Cortex • Sensory signals terminate in postcentral gyrus • Arranged somatotopically
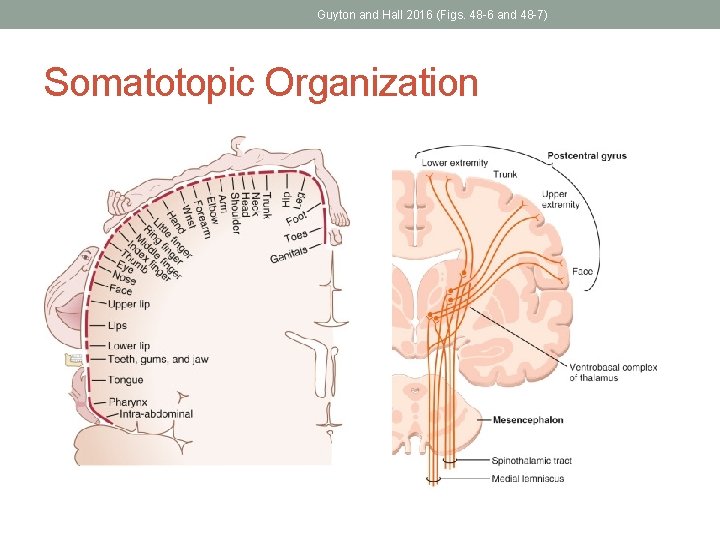
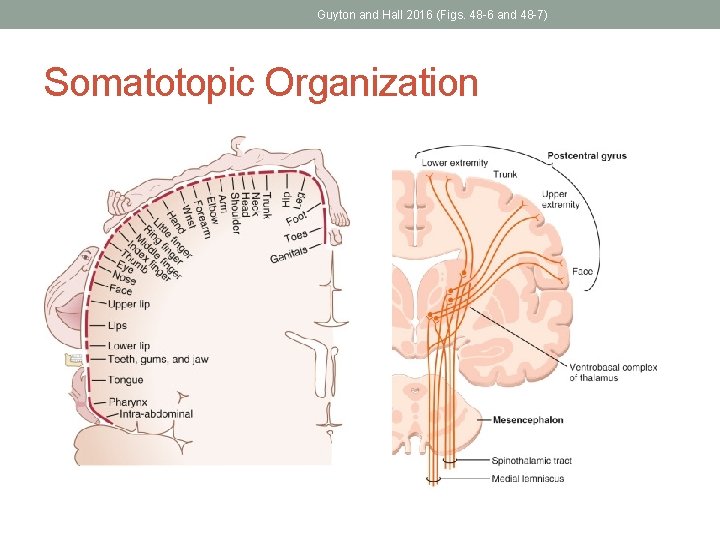
Guyton and Hall 2016 (Figs. 48 -6 and 48 -7) Somatotopic Organization
PATTERNS OF NERVE INJURY
Peripheral Nerve Damage • Cutaneous nerve distributions = areas of skin supplied by a peripheral nerve. • Deficits in cutaneous nerve distributions indicate impingement or damage at the level of the peripheral nerve. • Recall that a peripheral nerve contains fibers from several individual spinal roots
Reeves and Swenson 2008 (Ch. 9) Peripheral Nerve Damage • Peripheral neuropathy • Mononeuropathy • Usually due to trauma, compression, entrapment • Exs: Carpal Tunnel Syndrome, Bell’s Palsy • Polyneuropathy • Diabetes – vascular related • Nutritional deficiencies • Toxin exposure • Ex: Chemotherapy Induced Peripheral Neuropathy (CIPN) • Infections (Lyme disease, syphilis, HIV) • PNS conditions • Injury/trauma
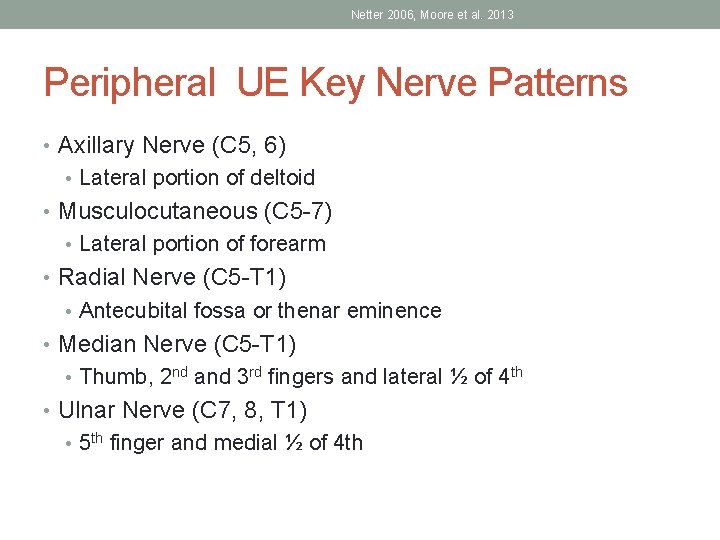
Netter 2006, Moore et al. 2013 Peripheral UE Key Nerve Patterns • Axillary Nerve (C 5, 6) • Lateral portion of deltoid • Musculocutaneous (C 5 -7) • Lateral portion of forearm • Radial Nerve (C 5 -T 1) • Antecubital fossa or thenar eminence • Median Nerve (C 5 -T 1) • Thumb, 2 nd and 3 rd fingers and lateral ½ of 4 th • Ulnar Nerve (C 7, 8, T 1) • 5 th finger and medial ½ of 4 th
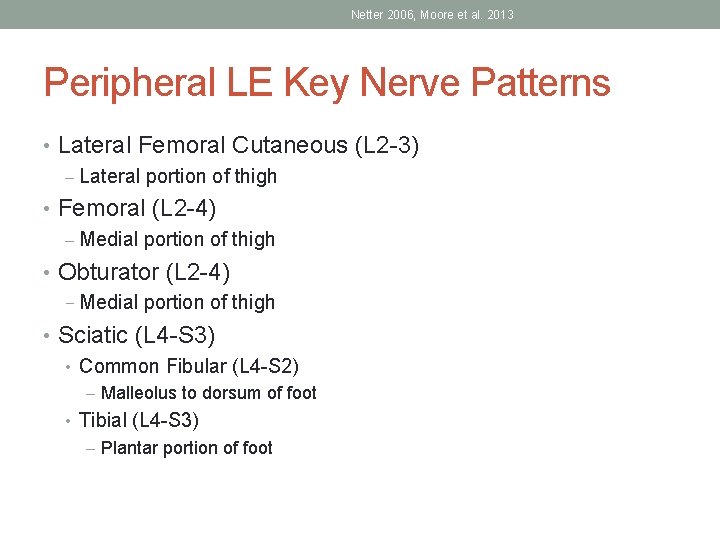
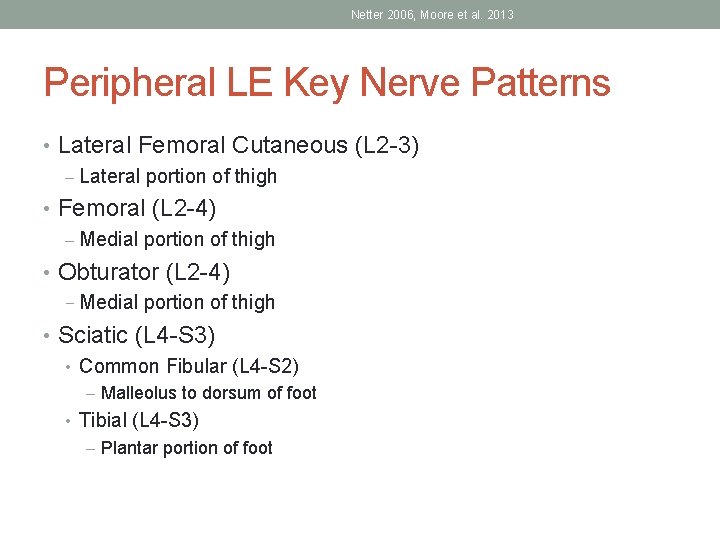
Netter 2006, Moore et al. 2013 Peripheral LE Key Nerve Patterns • Lateral Femoral Cutaneous (L 2 -3) – Lateral portion of thigh • Femoral (L 2 -4) – Medial portion of thigh • Obturator (L 2 -4) − Medial portion of thigh • Sciatic (L 4 -S 3) • Common Fibular (L 4 -S 2) – Malleolus to dorsum of foot • Tibial (L 4 -S 3) – Plantar portion of foot
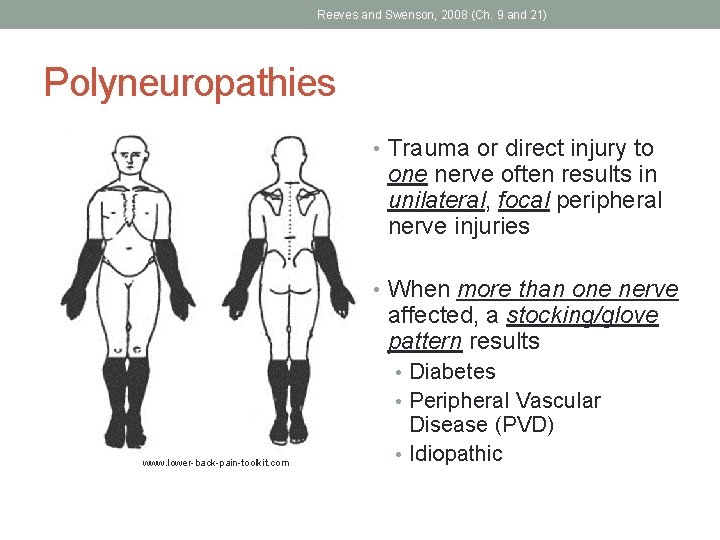
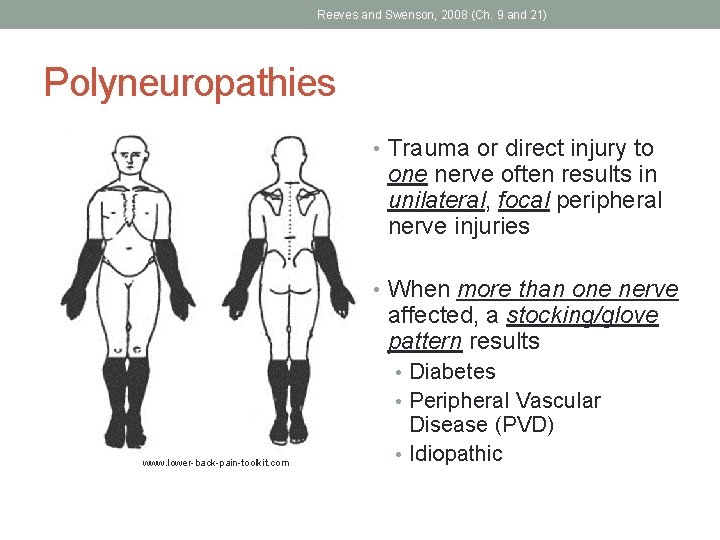
Reeves and Swenson, 2008 (Ch. 9 and 21) Polyneuropathies • Trauma or direct injury to one nerve often results in unilateral, focal peripheral nerve injuries • When more than one nerve affected, a stocking/glove pattern results • Diabetes • Peripheral Vascular www. lower-back-pain-toolkit. com Disease (PVD) • Idiopathic
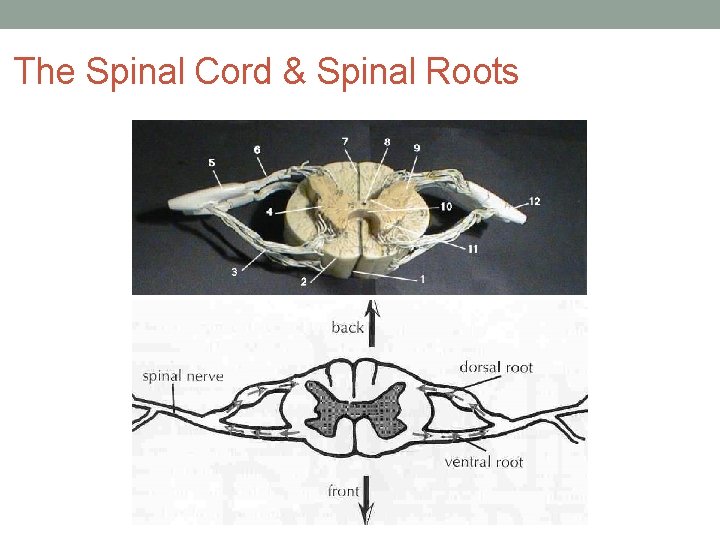
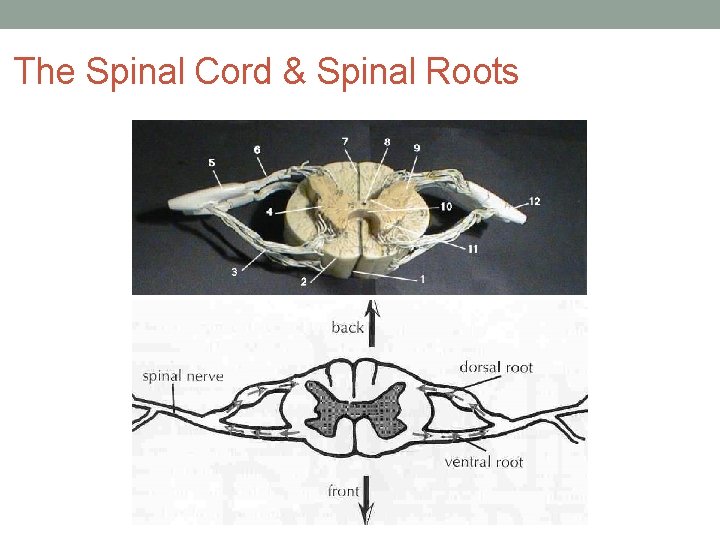
The Spinal Cord & Spinal Roots
Reeves and Swenson, 2008 (Ch. 9) Spinal Root Damage • Dermatome = an area of skin supplied by fibers from a single spinal nerve root. • Deficits in dermatomal regions indicate impingement or damage at the level of the spinal root • Some overlap with cutaneous distributions
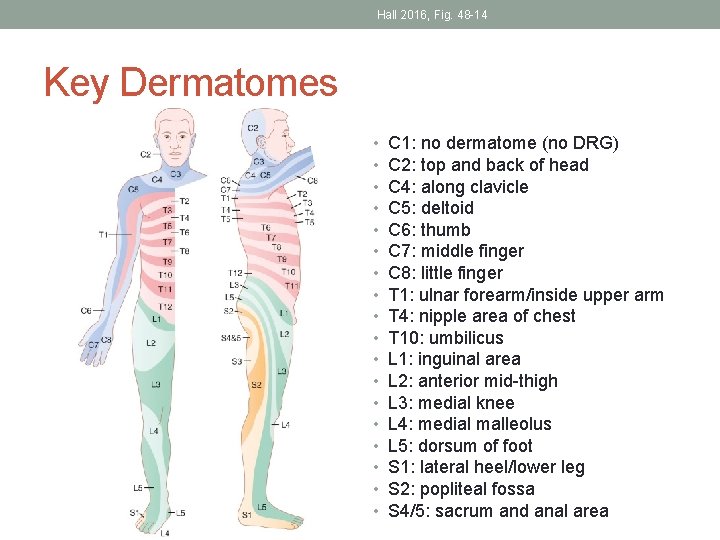
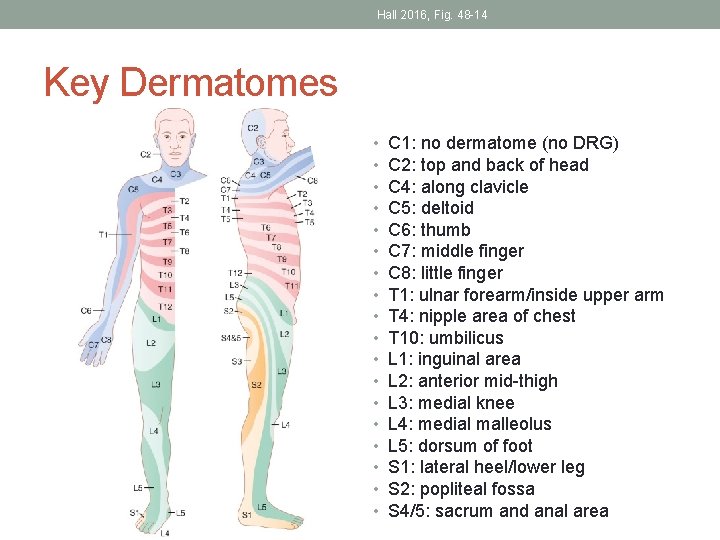
Hall 2016, Fig. 48 -14 Key Dermatomes • • • • • C 1: no dermatome (no DRG) C 2: top and back of head C 4: along clavicle C 5: deltoid C 6: thumb C 7: middle finger C 8: little finger T 1: ulnar forearm/inside upper arm T 4: nipple area of chest T 10: umbilicus L 1: inguinal area L 2: anterior mid-thigh L 3: medial knee L 4: medial malleolus L 5: dorsum of foot S 1: lateral heel/lower leg S 2: popliteal fossa S 4/5: sacrum and anal area
Reeves and Swenson, 2008 (Ch. 9) Spinal Root Damage • Radiculopathy • Intervertebral disc herniation • Narrowed foramina due to spondylosis/spine arthritis • Herpes zoster (shingles) • Commonly tingling, slight loss, and sharp, shooting pain
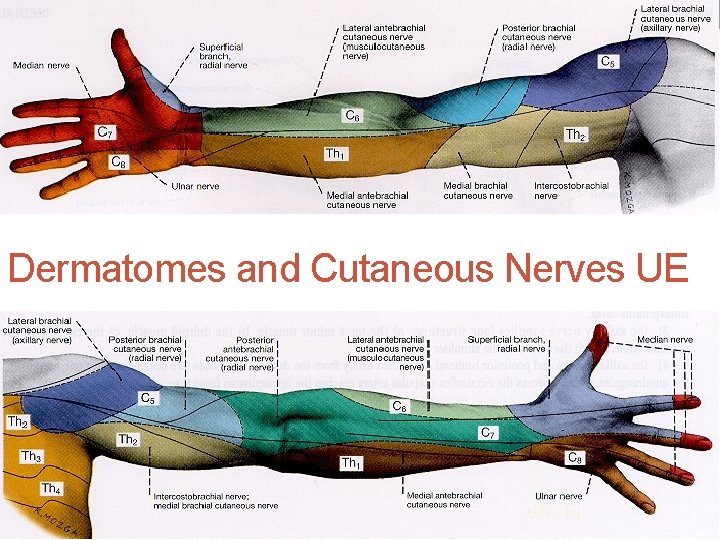
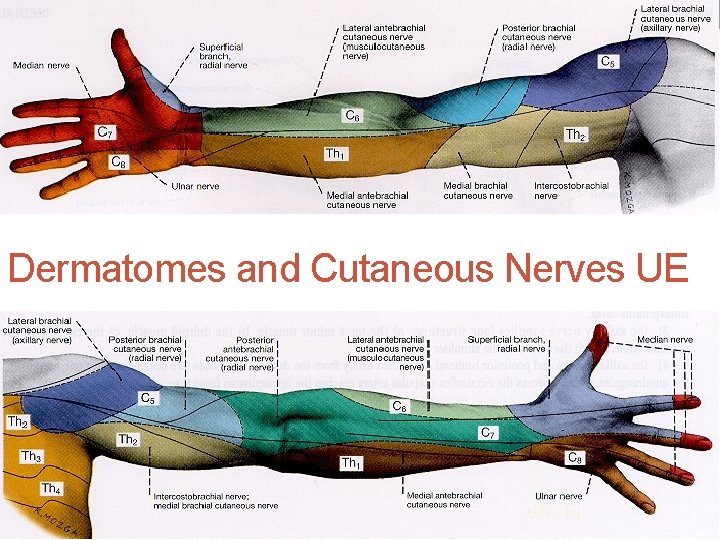
Dermatomes and Cutaneous Nerves UE
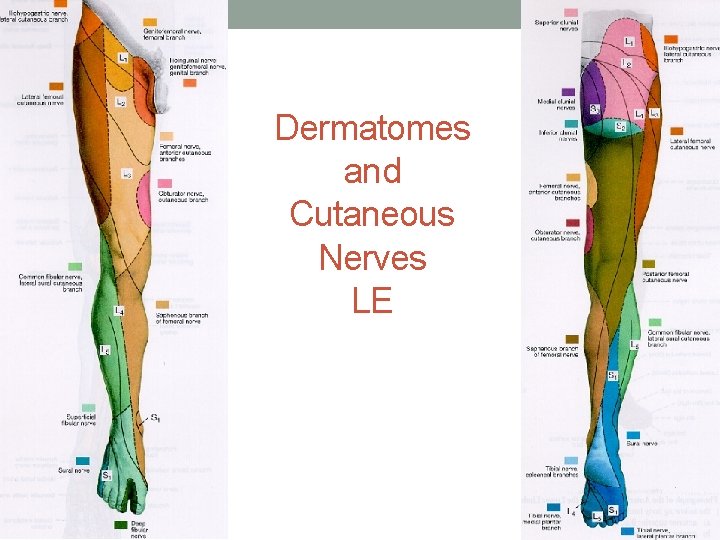
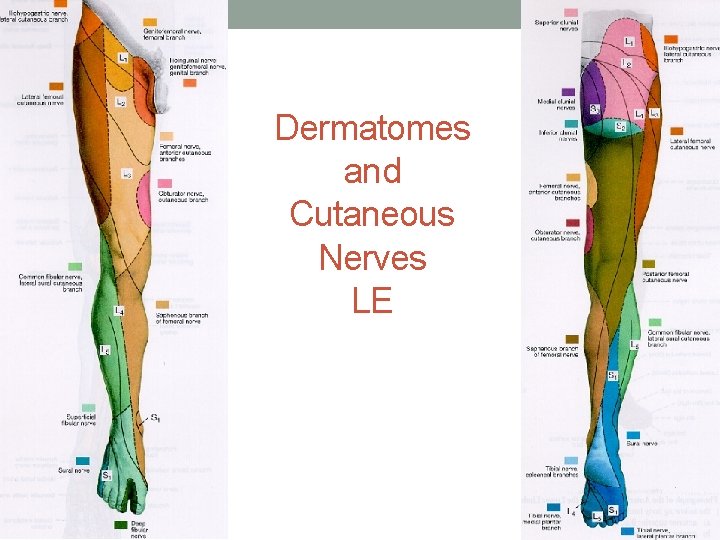
Dermatomes and Cutaneous Nerves LE
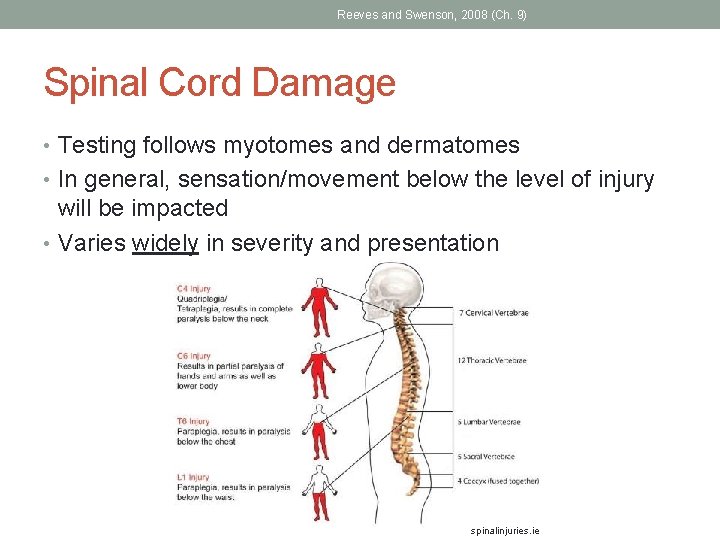
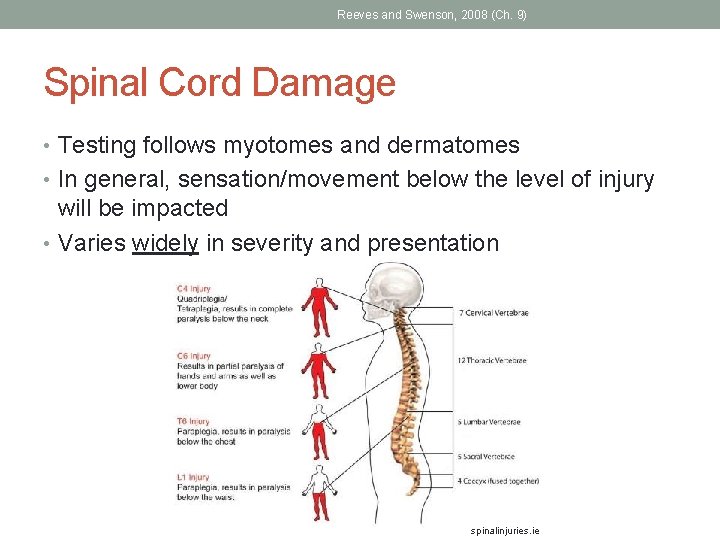
Reeves and Swenson, 2008 (Ch. 9) Spinal Cord Damage • Testing follows myotomes and dermatomes • In general, sensation/movement below the level of injury will be impacted • Varies widely in severity and presentation spinalinjuries. ie
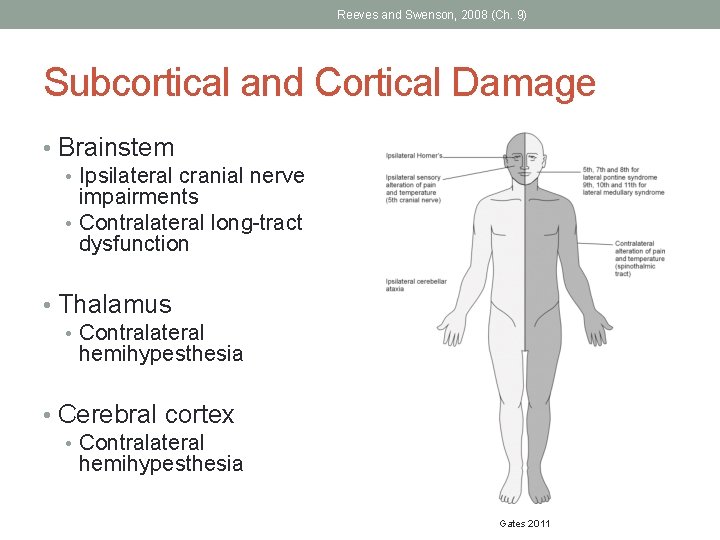
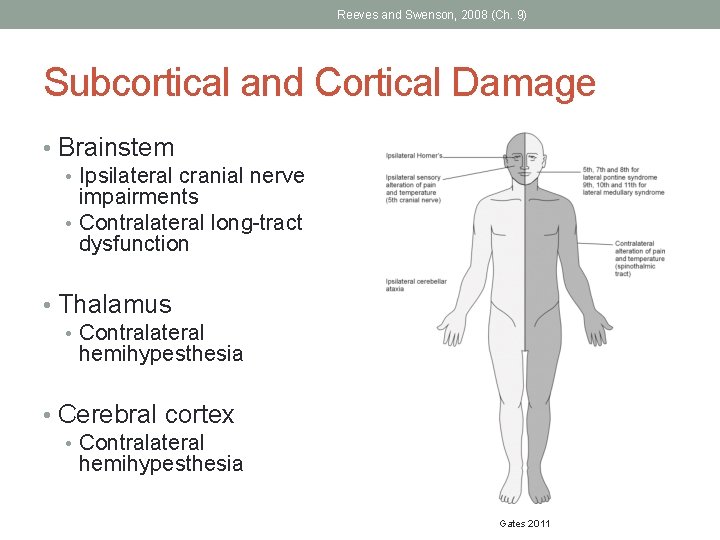
Reeves and Swenson, 2008 (Ch. 9) Subcortical and Cortical Damage • Brainstem • Ipsilateral cranial nerve impairments • Contralateral long-tract dysfunction • Thalamus • Contralateral hemihypesthesia • Cerebral cortex • Contralateral hemihypesthesia Gates 2011
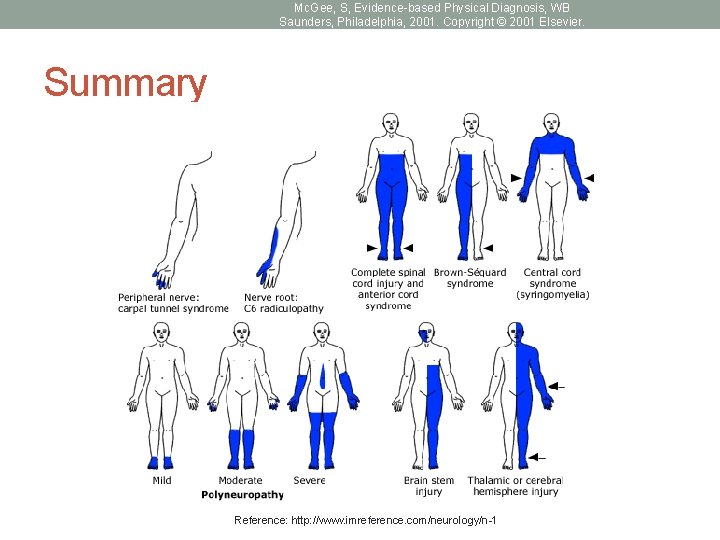
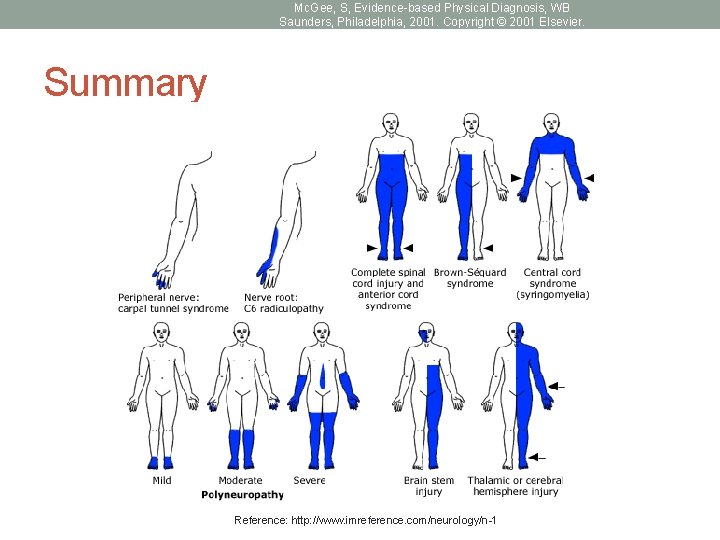
Mc. Gee, S, Evidence-based Physical Diagnosis, WB Saunders, Philadelphia, 2001. Copyright © 2001 Elsevier. Summary Reference: http: //www. imreference. com/neurology/n-1
TESTING SENSATION Setup/Guidelines Techniques
Chui and Schmitz 2014 Setup • Patient relaxed in a supported position • Bare skin/extremity to be tested exposed with appropriate draping • Quiet environment • Equipment gathered
Chui and Schmitz 2014 General Techniques • Demo with patient’s eyes open first • Test with patient’s eyes closed/vision occluded • Don’t give clues and discourage guessing • Minimize extraneous input • Repeat stimulus enough times to get a clear picture • Recommend 10 repetitions on each area of each limb • Apply stimuli systematically, but randomly to patient • Vary timing and rhythm of stimuli • Note accuracy and speed of response • Give the patient time to respond • When possible, establish baseline or “normal” • Test painful areas last
Factors that may interfere… • Understanding/cognition • Communication • Attention span • Memory • Psychological factors • Pain
TESTING SPECIFIC MODALITIES Partner up!
Chui and Schmitz 2014 Tests of Superficial Sensation • Light touch • Use tapered cotton wisp • American Spinal Injury Association recommendations: • Apply wisp lightly and briefly across the skin • Moving over a distance not to exceed 1 cm • Patient responds “yes” when light touch is felt • Can also use a brush or tissue
Chui and Schmitz 2014 Tests of Superficial Sensation • Pain • Use clean safety pin • Patient reports if stimulus is “sharp” or “dull” • Temperature • Use stoppered test tubes • Patient reports if stimulus is “hot” or “cold”
Feng, Schlosser & Sumpio, 2009 and 2011 Monofilament Testing • Most frequently used with people with diabetes or other peripheral nerve injuries • For loss of protective sensation • More quantitative • 5. 07/10 g filament most commonly used • Do not apply the filament to ulcers, callouses, scars or necrotic tissue • Test 10 points in random sequence (see next slide) • Loss of sensation at any of the points indicates high risk for ulceration and/or LE amputation in individuals with diabetes
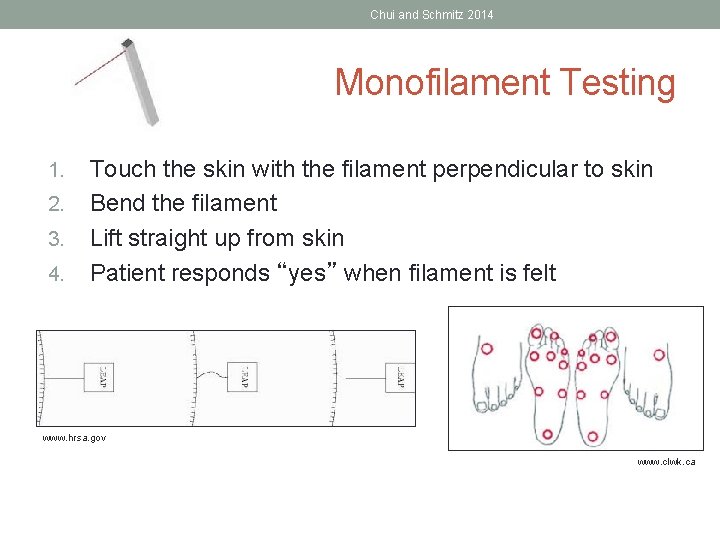
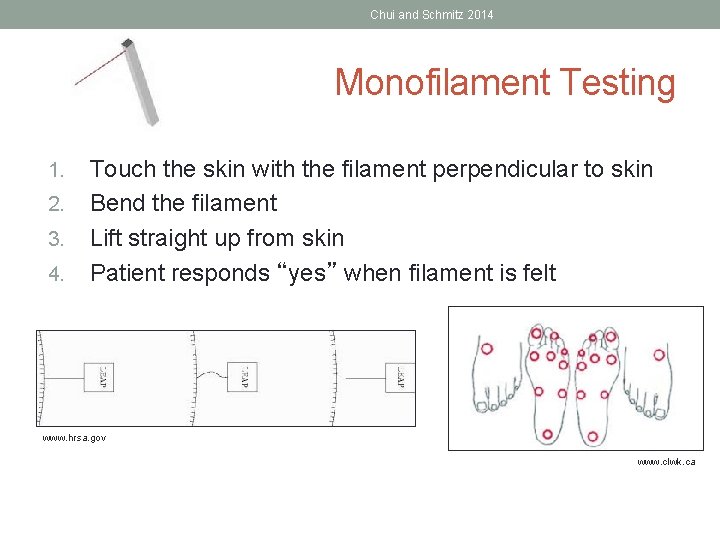
Chui and Schmitz 2014 Monofilament Testing 1. 2. 3. 4. Touch the skin with the filament perpendicular to skin Bend the filament Lift straight up from skin Patient responds “yes” when filament is felt www. hrsa. gov www. clwk. ca
Chui and Schmitz 2014 Tests of Deep Sensation • Proprioception • Tests joint position sense at rest • Patient responds if the body part is “up” or “down” relative to last position • Kinesthesia • Tests awareness of movement • Patient describes the motion while the extremity is moving • Alternatively: Patient duplicates/mirrors movement with other extremity • Vibration • Use 128 Hz tuning fork
Chui and Schmitz 2014 Proprioception/Kinesthesia • Therapist’s grip should be constant and minimal • Finger-tip grip over a bony prominence • Avoid superficial sensation input • Remove clothing • Do not place hand on muscle bellies or tendons • Keep joint and surrounding body segments from contacting plinth
Chui and Schmitz 2014 Vibration Sense • One of first sensations lost in vascular diseases • 128 Hz tuning fork • Hold stem of the fork – do not touch the tines • Briskly hit tuning fork on palm • Place base on the area being tested • Location is debated depending on source used • Ball of foot, toes, fingers • Bony prominences • Patient indicates if stimulus is vibrating (yes) or non-vibrating (no) • Alternately: patient can indicate when they can no longer feel the vibration (time) • Use ear phones to block the sound OR randomly stop vibration before placing tuning fork
Chui and Schmitz 2014 Tests of Cortical Sensation • Making sense of sensory information • Ability to localize a stimuli or to discriminate between number or type of stimuli presented • Options: • Tactile localization • 2 point discrimination • Stereognosis (hand) • Graphesthesia • Bilateral simultaneous stimulation • Barognosis
Questions? ? • To be continued on Friday…. .
References • Blumenfeld H. Neuroanatomy through Clinical Cases. Sinauer Associates, • • • Inc, Sunderland, MA, 2002: 70 -72. Chui KK & Schmitz TJ. Examination of Sensory Function. In: O’Sullivan SB, Schmitz TJ & Fulk GD, eds. Physical Rehabilitation. 6 th ed. Philadelphia, PA: FA Davis; 2014: 87 -123, 184. Feng Y, Scholsser FJ, Sumpio BE. The Semmes Weinstein monofilament examination as a screening tool for diabetic peripheral neuropathy. J Vasc Surg. 2009; 50: 675 -82. Feng Y, Scholsser FJ, Sumpio BE. The Semmes Weinstein monofilament examination is a significant predictor of the risk of foot ulceration and amputation in patients with diabetes mellitus. J Vasc Surg. 2011; 53: 220 -6. Hall JE. Chapter 48: Somatic Sensations: I. General Organization, the Tactile and Position Senses. In: Hall JE, Guyton AC, eds. Guyton and Hall Textbook of Medical Physiology. 13 th ed. Philadelphia, PA: Elsevier, Inc; 2016: 607 -619. Gates P. Work out where the problem is in the brainstem using ‘the rule of 4’. Practical Neurology. 2011; 11: 167 -172.
References • Martin JH, Jessell TM. Anatomy of the somatic sensory system. • • In: Kandel R, Schwartz JH, Jessel TM, eds. Principles of Neural Science. New York, NY: Elsevier; 1991. Moore KL, Dalley AF, Agur AMR. Clinically Oriented Anatomy. 7 th ed. Baltimore, MA: Williams and Wilkins; 2013. Netter FH. Atlas of Human Anatomy. 4 th ed. Philadelphia, PA: Saunders Elsevier; 2006. Reeves AG, Swenson RS. Neuromuscular System Disorders. In: Disorders of the Nervous System. Available online: https: //www. dartmouth. edu/~dons/part_3/chapter_21. html. 2008. Reeves AG, Swenson RS. Sensory System Evaluation. In: Disorders of the Nervous System. Available online: https: //www. dartmouth. edu/~dons/part_1/chapter_9. html. 2008.
 6280/160
6280/160 6280/160
6280/160 Cow physical exam
Cow physical exam Wither pinch test
Wither pinch test Tyson pillow md
Tyson pillow md Withers pinch test
Withers pinch test Ospe and osce
Ospe and osce Objective structured clinical examination
Objective structured clinical examination Virtual university examination software
Virtual university examination software Vamc slums examination
Vamc slums examination Penilaian klinis
Penilaian klinis Cas clinical assessment
Cas clinical assessment Abcd method in nutrition
Abcd method in nutrition Clinical assessment protocols
Clinical assessment protocols National clinical assessment service
National clinical assessment service University clinical center tuzla
University clinical center tuzla Penn state university clinical psychology
Penn state university clinical psychology University clinical center tuzla
University clinical center tuzla Anz aptitude test
Anz aptitude test Walden student assistance program
Walden student assistance program Essential elements of portfolio assessment
Essential elements of portfolio assessment Define dynamic assessment
Define dynamic assessment Portfolio assessment matches assessment to teaching
Portfolio assessment matches assessment to teaching 詹景裕
詹景裕 Sensory similes
Sensory similes 11 sentence paragraph
11 sentence paragraph Define sensory details
Define sensory details Sensory ethnography
Sensory ethnography Figurative language warm up
Figurative language warm up Sensory figure of harriet tubman
Sensory figure of harriet tubman Anatomy of visual system
Anatomy of visual system Recognizing imagery
Recognizing imagery Structure of the sensory system
Structure of the sensory system Classification of sensory system
Classification of sensory system Sensory system organs
Sensory system organs Sensory cup analogy
Sensory cup analogy What are the different types of sensory receptors
What are the different types of sensory receptors Classification of sensory receptors
Classification of sensory receptors Sensory receptors in the eye
Sensory receptors in the eye Sensory processing disorder dsm
Sensory processing disorder dsm Tina champagne sensory modulation
Tina champagne sensory modulation Exteroceptors examples
Exteroceptors examples Jane horwood sensory circuits
Jane horwood sensory circuits Types of sensory disorders
Types of sensory disorders Septum pellucidum
Septum pellucidum Sensory figure
Sensory figure Sensory epithelia
Sensory epithelia Sensory adaptation definition
Sensory adaptation definition Sensory adaptation
Sensory adaptation Ischiadic nerve
Ischiadic nerve