Senolytic Therapy and Amyloid Beta Plaques Drug Therapy
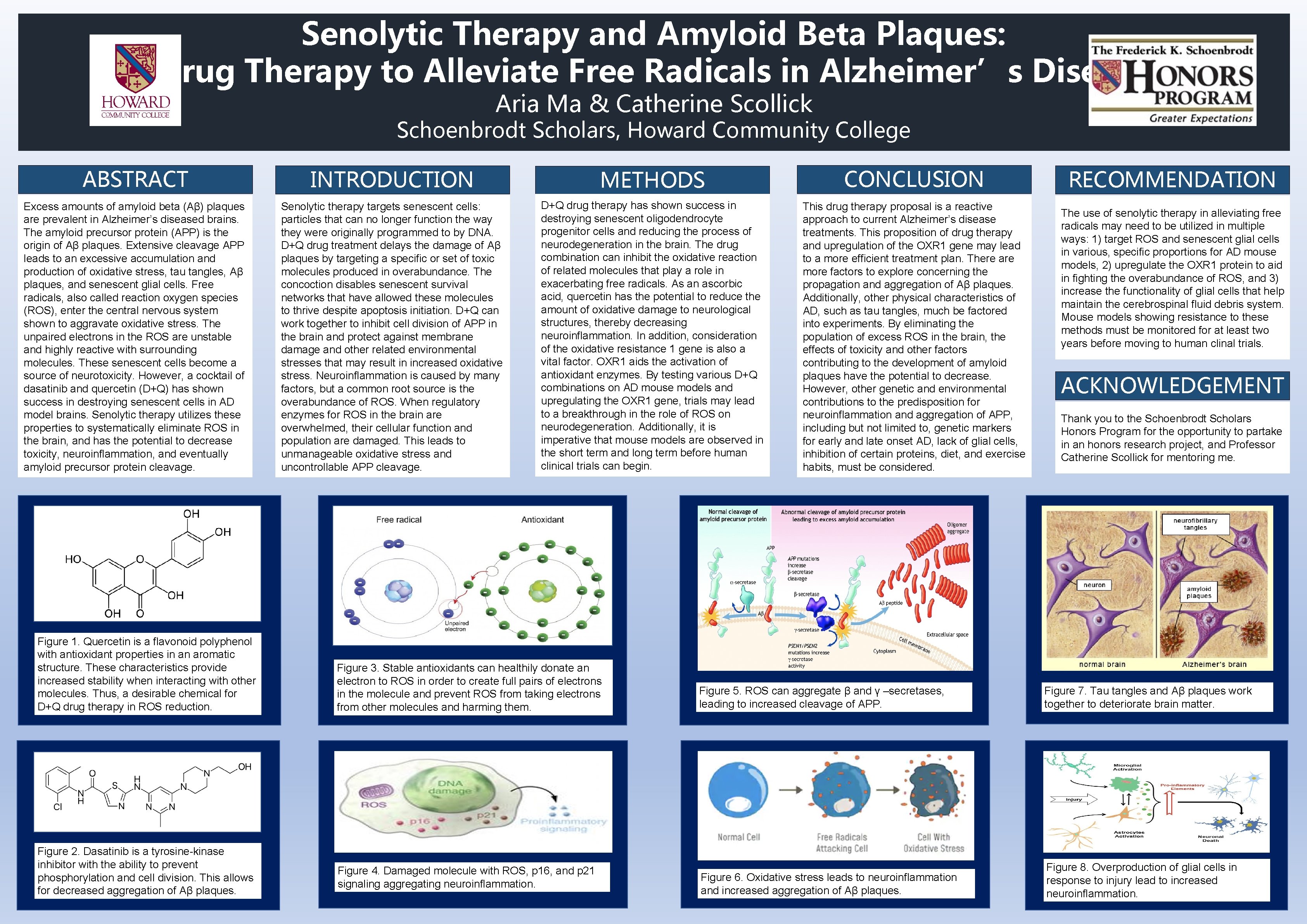
Senolytic Therapy and Amyloid Beta Plaques: Drug Therapy to Alleviate Free Radicals in Alzheimer’s Disease Aria Ma & Catherine Scollick Schoenbrodt Scholars, Howard Community College ABSTRACT INTRODUCTION METHODS CONCLUSION Excess amounts of amyloid beta (Aβ) plaques are prevalent in Alzheimer’s diseased brains. The amyloid precursor protein (APP) is the origin of Aβ plaques. Extensive cleavage APP leads to an excessive accumulation and production of oxidative stress, tau tangles, Aβ plaques, and senescent glial cells. Free radicals, also called reaction oxygen species (ROS), enter the central nervous system shown to aggravate oxidative stress. The unpaired electrons in the ROS are unstable and highly reactive with surrounding molecules. These senescent cells become a source of neurotoxicity. However, a cocktail of dasatinib and quercetin (D+Q) has shown success in destroying senescent cells in AD model brains. Senolytic therapy utilizes these properties to systematically eliminate ROS in the brain, and has the potential to decrease toxicity, neuroinflammation, and eventually amyloid precursor protein cleavage. Senolytic therapy targets senescent cells: particles that can no longer function the way they were originally programmed to by DNA. D+Q drug treatment delays the damage of Aβ plaques by targeting a specific or set of toxic molecules produced in overabundance. The concoction disables senescent survival networks that have allowed these molecules to thrive despite apoptosis initiation. D+Q can work together to inhibit cell division of APP in the brain and protect against membrane damage and other related environmental stresses that may result in increased oxidative stress. Neuroinflammation is caused by many factors, but a common root source is the overabundance of ROS. When regulatory enzymes for ROS in the brain are overwhelmed, their cellular function and population are damaged. This leads to unmanageable oxidative stress and uncontrollable APP cleavage. D+Q drug therapy has shown success in destroying senescent oligodendrocyte progenitor cells and reducing the process of neurodegeneration in the brain. The drug combination can inhibit the oxidative reaction of related molecules that play a role in exacerbating free radicals. As an ascorbic acid, quercetin has the potential to reduce the amount of oxidative damage to neurological structures, thereby decreasing neuroinflammation. In addition, consideration of the oxidative resistance 1 gene is also a vital factor. OXR 1 aids the activation of antioxidant enzymes. By testing various D+Q combinations on AD mouse models and upregulating the OXR 1 gene, trials may lead to a breakthrough in the role of ROS on neurodegeneration. Additionally, it is imperative that mouse models are observed in the short term and long term before human clinical trials can begin. This drug therapy proposal is a reactive approach to current Alzheimer’s disease treatments. This proposition of drug therapy and upregulation of the OXR 1 gene may lead to a more efficient treatment plan. There are more factors to explore concerning the propagation and aggregation of Aβ plaques. Additionally, other physical characteristics of AD, such as tau tangles, much be factored into experiments. By eliminating the population of excess ROS in the brain, the effects of toxicity and other factors contributing to the development of amyloid plaques have the potential to decrease. However, other genetic and environmental contributions to the predisposition for neuroinflammation and aggregation of APP, including but not limited to, genetic markers for early and late onset AD, lack of glial cells, inhibition of certain proteins, diet, and exercise habits, must be considered. Figure 1. Quercetin is a flavonoid polyphenol with antioxidant properties in an aromatic structure. These characteristics provide increased stability when interacting with other molecules. Thus, a desirable chemical for D+Q drug therapy in ROS reduction. Figure 2. Dasatinib is a tyrosine-kinase inhibitor with the ability to prevent phosphorylation and cell division. This allows for decreased aggregation of Aβ plaques. Figure 3. Stable antioxidants can healthily donate an electron to ROS in order to create full pairs of electrons in the molecule and prevent ROS from taking electrons from other molecules and harming them. Figure 4. Damaged molecule with ROS, p 16, and p 21 signaling aggregating neuroinflammation. RECOMMENDATION The use of senolytic therapy in alleviating free radicals may need to be utilized in multiple ways: 1) target ROS and senescent glial cells in various, specific proportions for AD mouse models, 2) upregulate the OXR 1 protein to aid in fighting the overabundance of ROS, and 3) increase the functionality of glial cells that help maintain the cerebrospinal fluid debris system. Mouse models showing resistance to these methods must be monitored for at least two years before moving to human clinal trials. ACKNOWLEDGEMENT S Scholars Thank you to the Schoenbrodt Honors Program for the opportunity to partake in an honors research project, and Professor Catherine Scollick for mentoring me. Figure 5. ROS can aggregate β and γ –secretases, leading to increased cleavage of APP. Figure 7. Tau tangles and Aβ plaques work together to deteriorate brain matter. Figure 6. Oxidative stress leads to neuroinflammation and increased aggregation of Aβ plaques. Figure 8. Overproduction of glial cells in response to injury lead to increased neuroinflammation.
- Slides: 1