Sem Physio 11 Microcirculation peripheral circulation Prof dr
- Slides: 35
Sem Physio 11 – Microcirculation; peripheral circulation Prof. dr. Željko Dujić
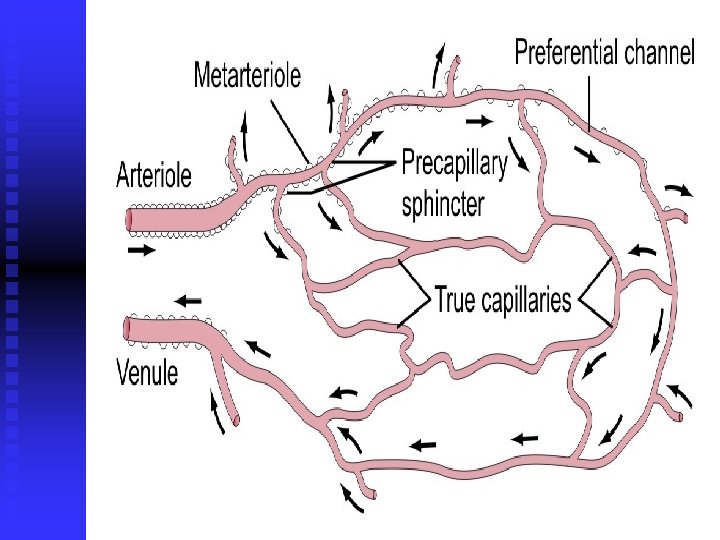
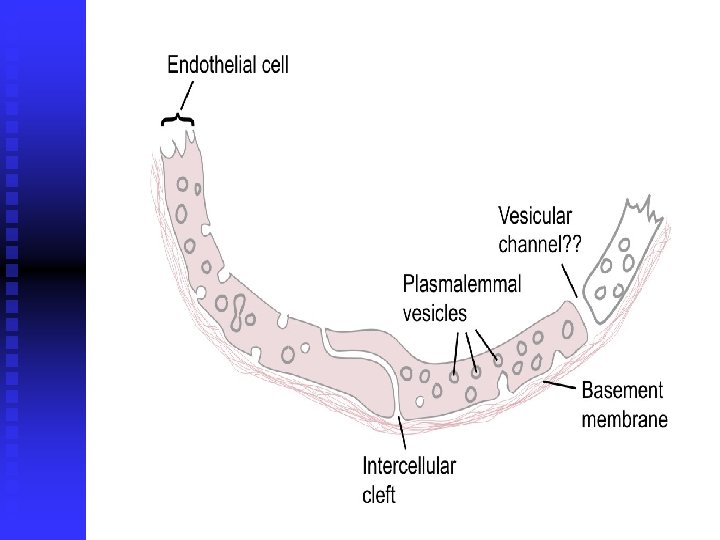
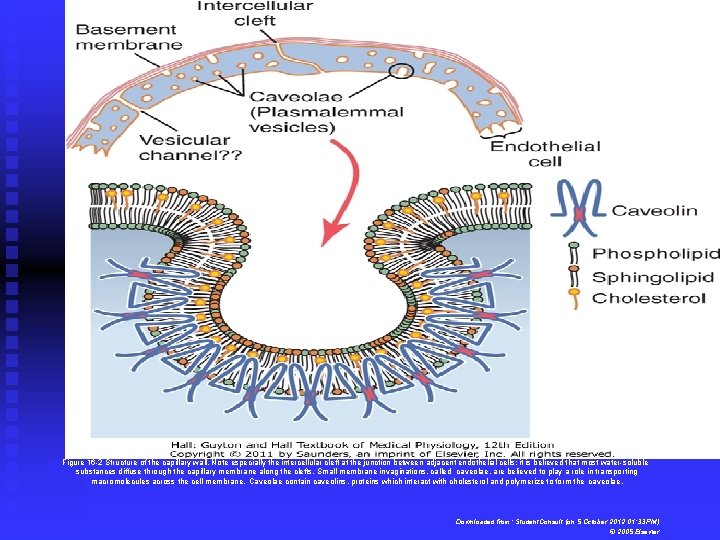
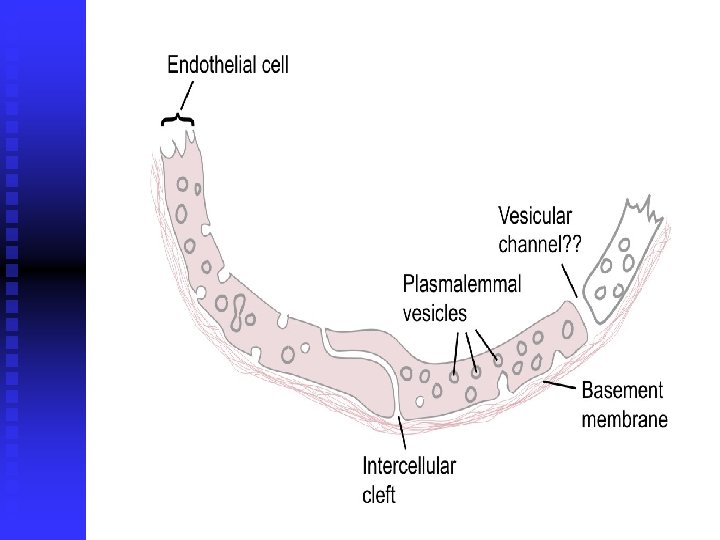
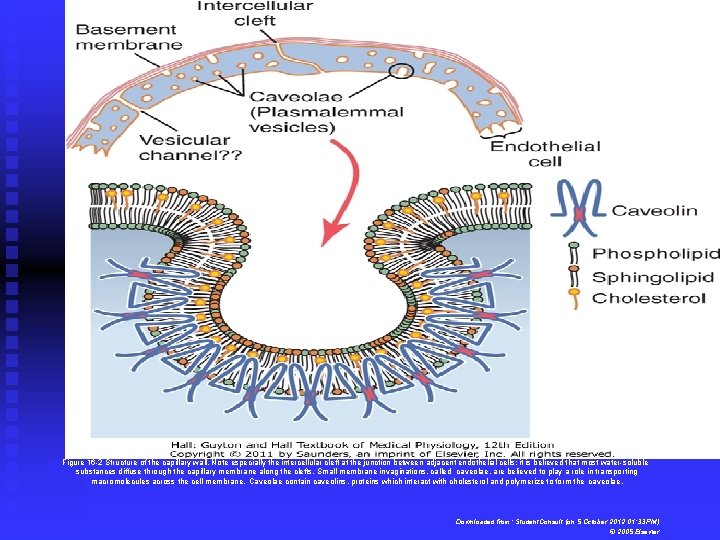
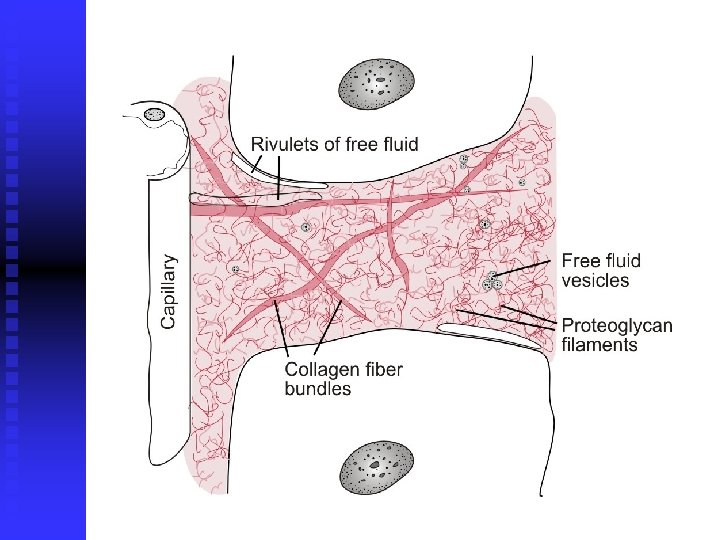
Figure 16 -2 Structure of the capillary wall. Note especially the intercellular cleft at the junction between adjacent endothelial cells; it is believed that most water-soluble substances diffuse through the capillary membrane along the clefts. Small membrane invaginations, called caveolae, are believed to play a role in transporting macromolecules across the cell membrane. Caveolae contain caveolins, proteins which interact with cholesterol and polymerize to form the caveolae. Downloaded from: Student. Consult (on 5 October 2012 01: 33 PM) © 2005 Elsevier
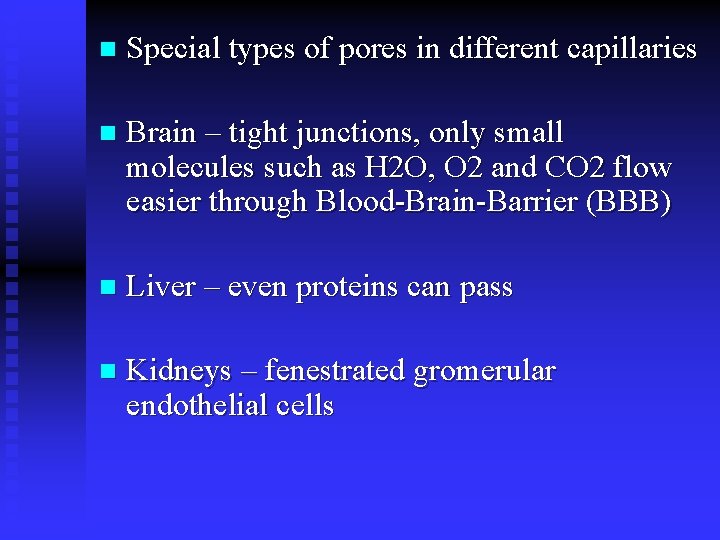
n Special types of pores in different capillaries n Brain – tight junctions, only small molecules such as H 2 O, O 2 and CO 2 flow easier through Blood-Brain-Barrier (BBB) n Liver – even proteins can pass n Kidneys – fenestrated gromerular endothelial cells
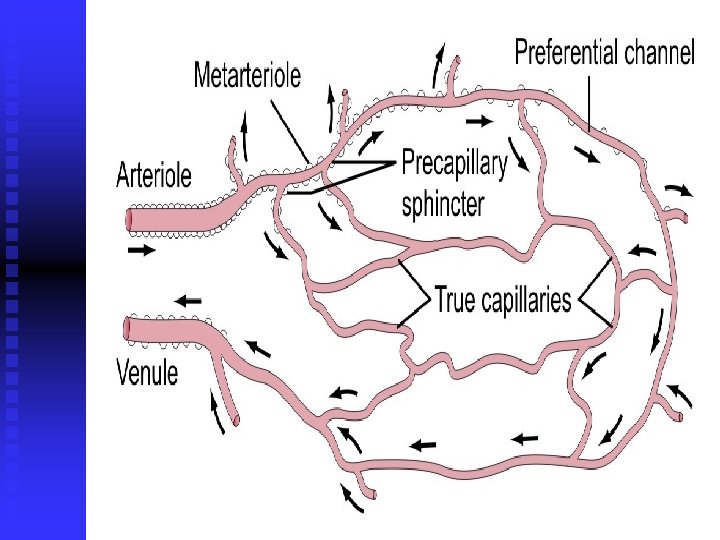
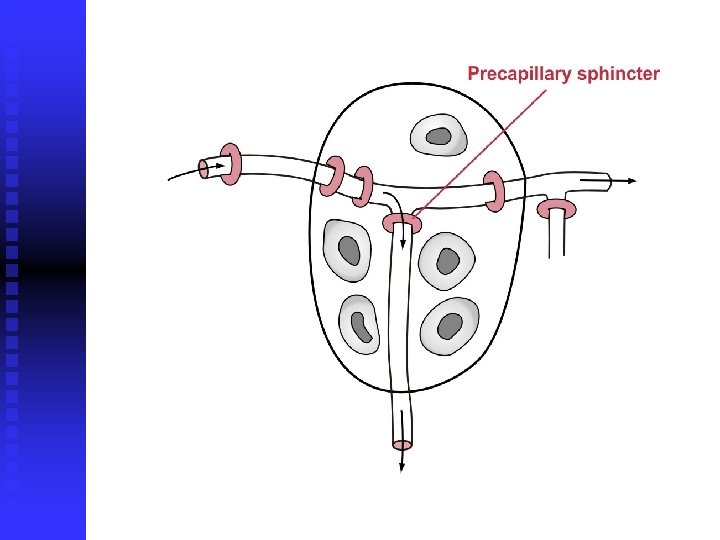
n Vasomotion and it’s regulation n Diffusibility through capillary membrane (extremes water pearmeability = 1, and albumins; permeability = 0)
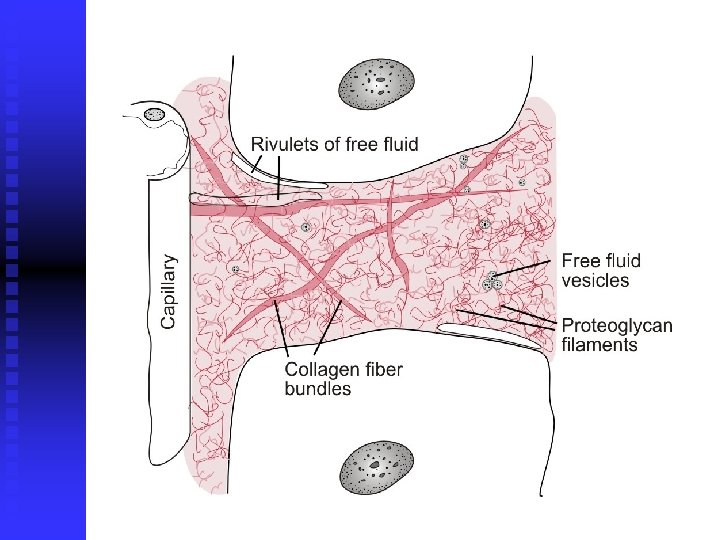
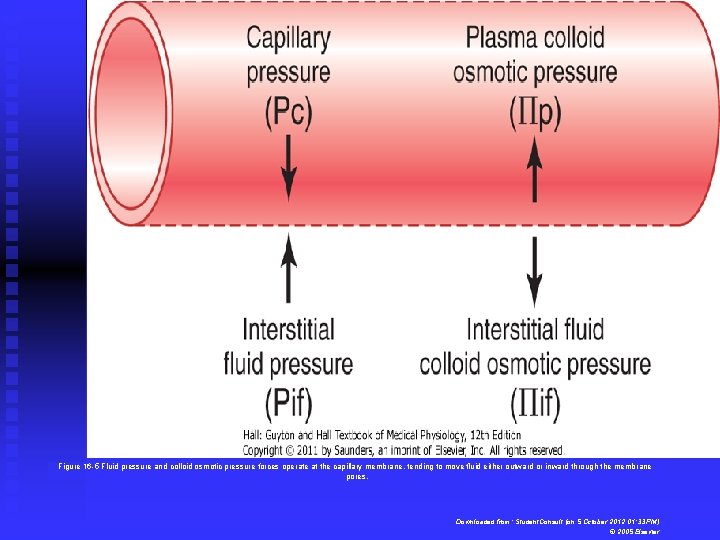
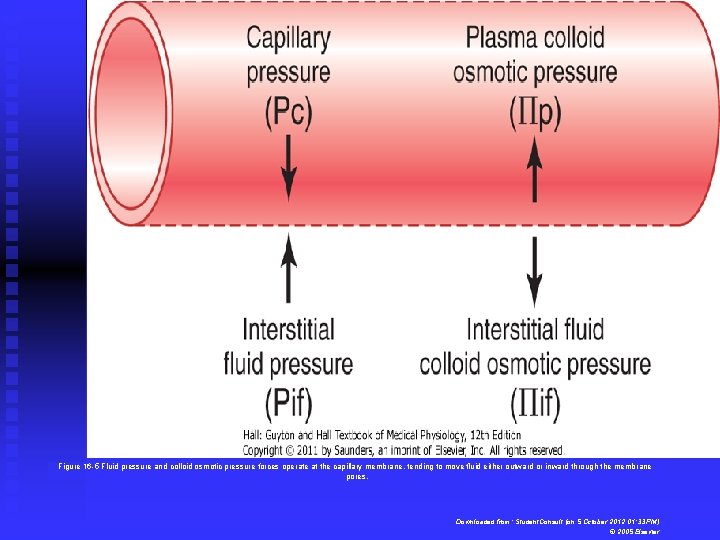
Figure 16 -5 Fluid pressure and colloid osmotic pressure forces operate at the capillary membrane, tending to move fluid either outward or inward through the membrane pores. Downloaded from: Student. Consult (on 5 October 2012 01: 33 PM) © 2005 Elsevier
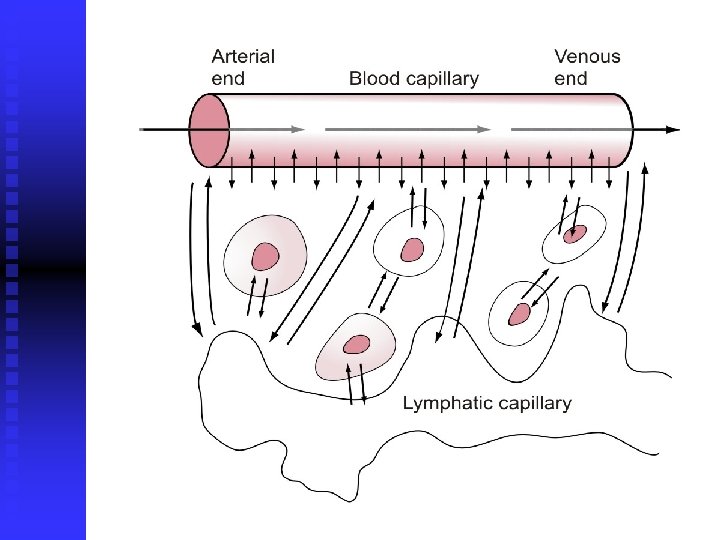
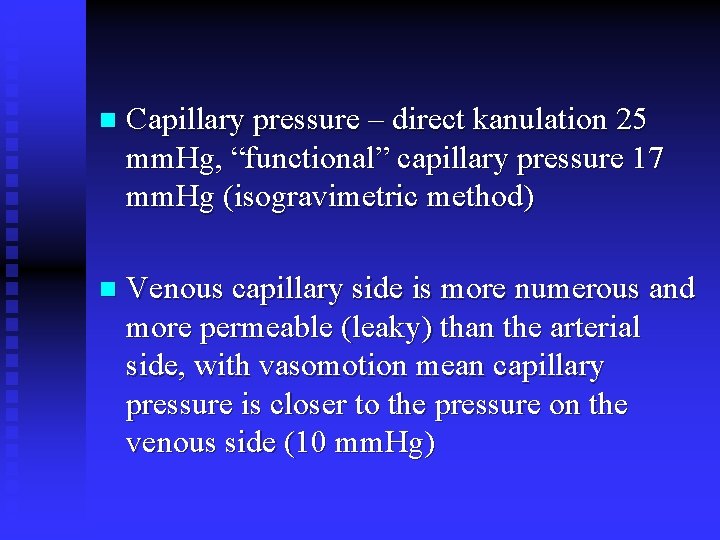
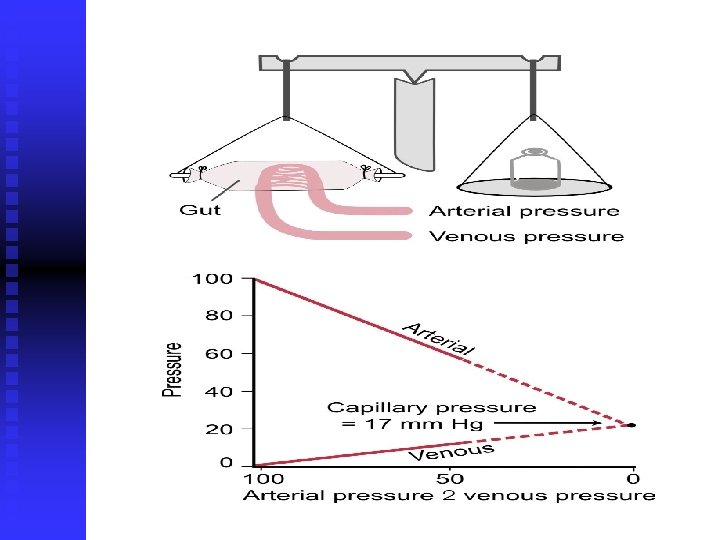
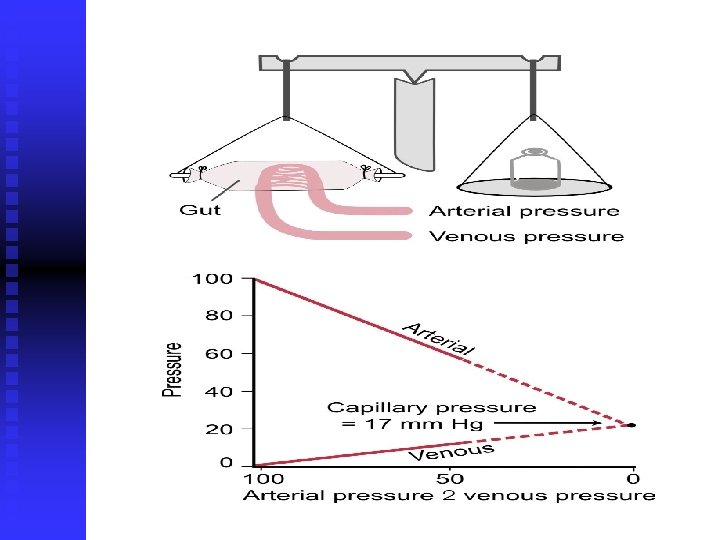
n Capillary pressure – direct kanulation 25 mm. Hg, “functional” capillary pressure 17 mm. Hg (isogravimetric method) n Venous capillary side is more numerous and more permeable (leaky) than the arterial side, with vasomotion mean capillary pressure is closer to the pressure on the venous side (10 mm. Hg)
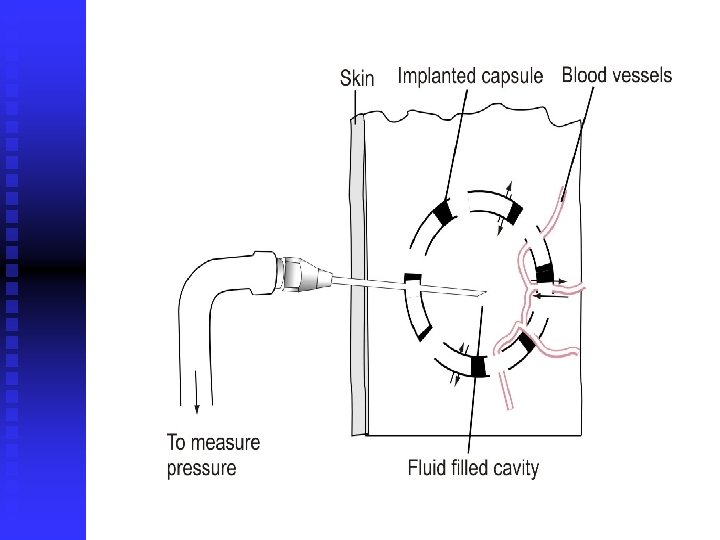
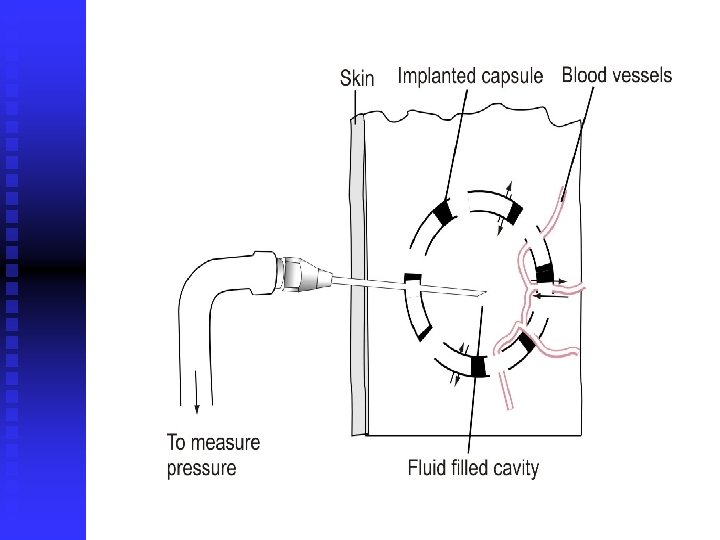
n Micropipete measurement, implanted hollow capsules, cotton wick n Average value – 3 mm. Hg n Interstitial fluid pressure in tightly encalpulated tissues (although positive still negative in relation to capsular pressure)
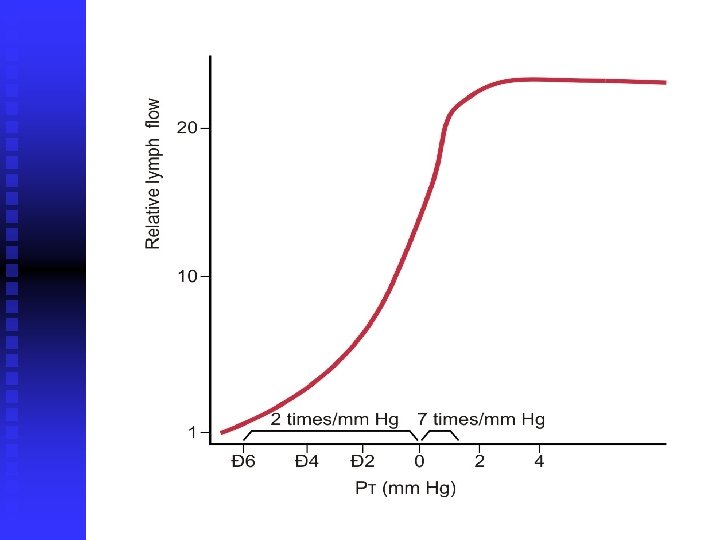
n Plasma colloid osmotic pressure (28 mm. Hg) – 19 mm. Hg caused by dissolved protein and 9 mm. Hg by Donnan effect and interstitial fluid colloid pressure (8 mm. Hg, due to 30 g/L protein concentration), importance of albumins n Net outward force (filtration) on the arterial side of capillaries 13 mm. Hg and net inward (reapsorption) pressure of 7 mm. Hg on the venous side n Net outward pressure of 0. 3 mm. Hg n Filtration coefficient – very small in brain, high in liver and GI (small intestines)
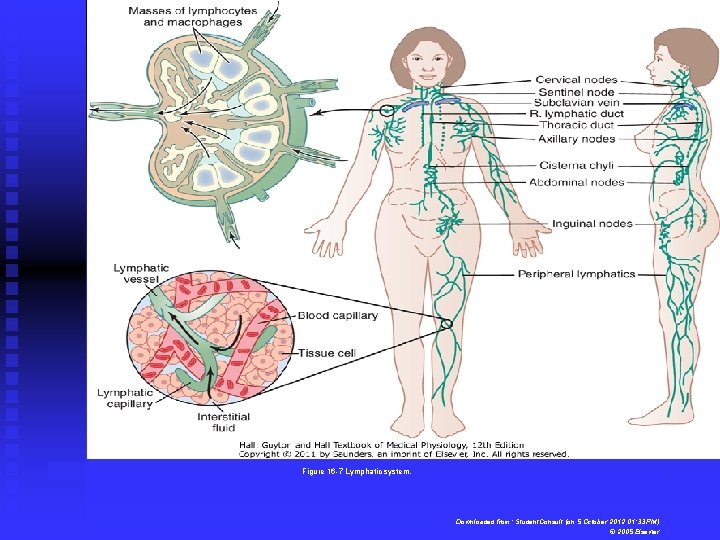
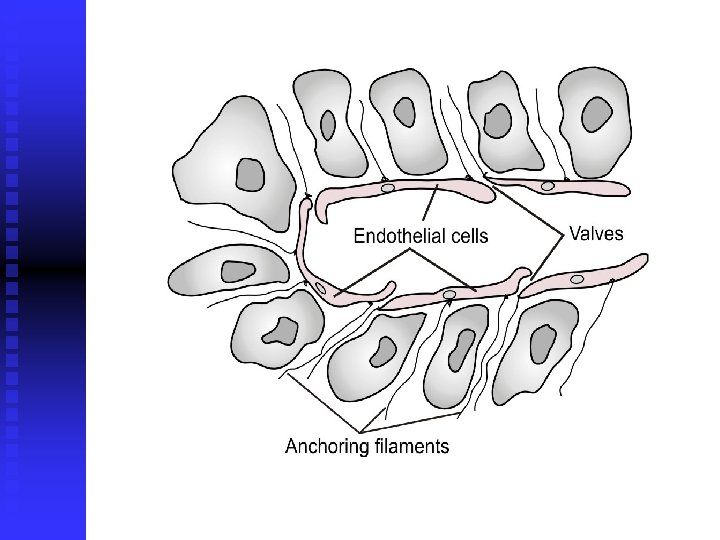
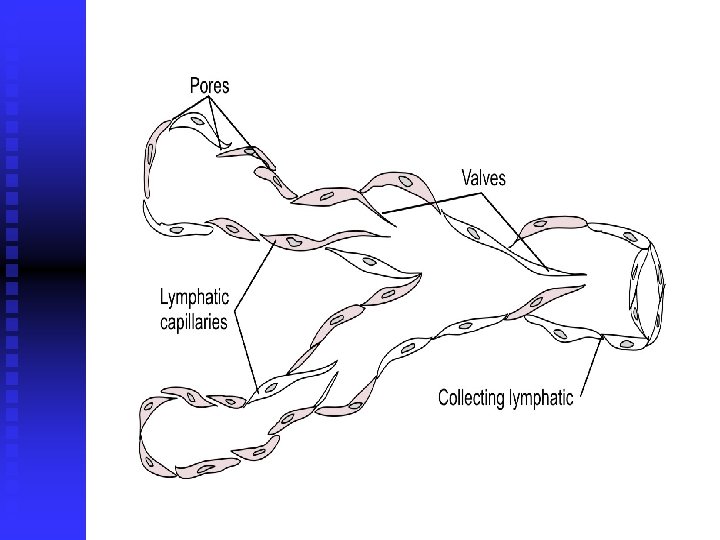
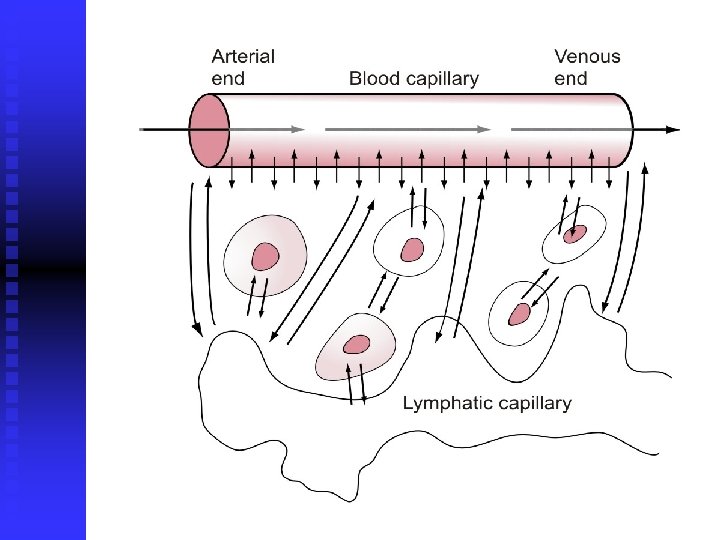
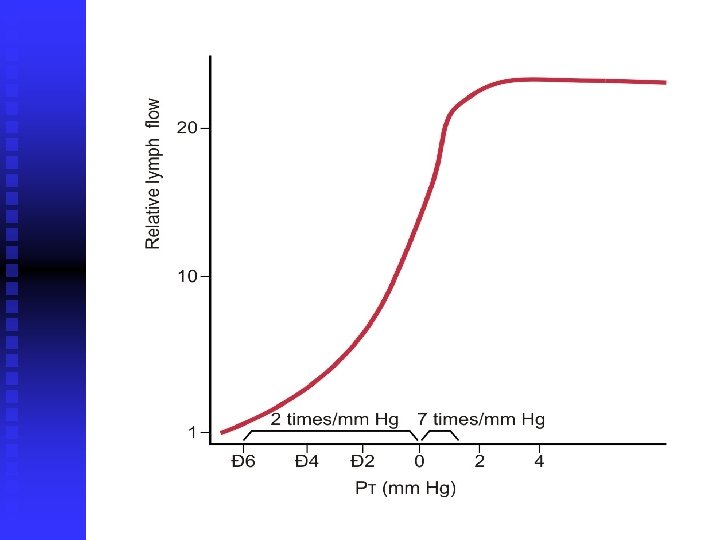
n Lymph channels in the body (exceptions brain, bone, endomysium of the muscle, superficial skin), lymph flow 2 -3 L/day, lymph pump, reapsorption of fats, bacterial inactivation n Lymph flow dependence on the relation between interstitial fluid pressure and the activity of lymph pump
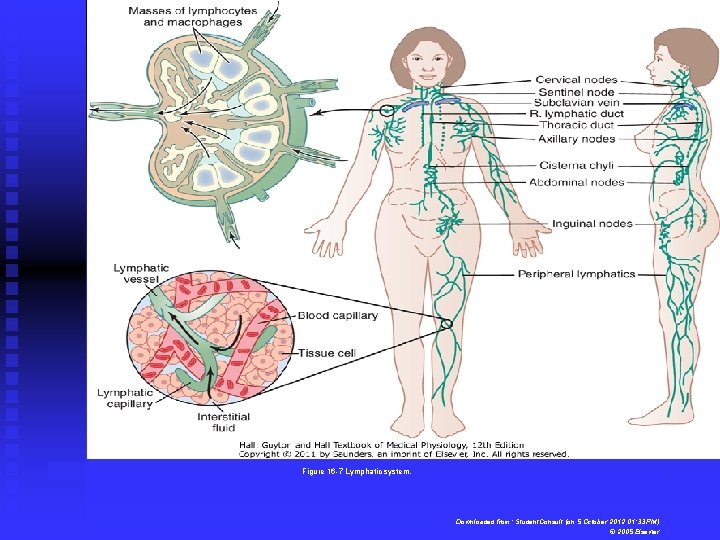
Figure 16 -7 Lymphatic system. Downloaded from: Student. Consult (on 5 October 2012 01: 33 PM) © 2005 Elsevier
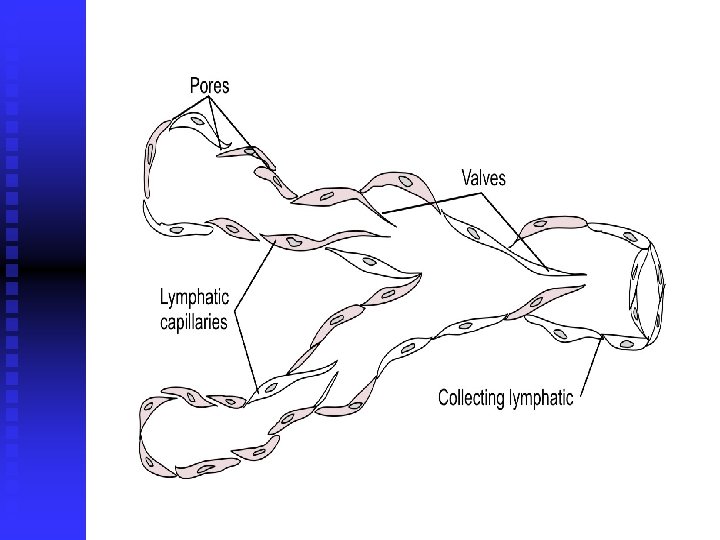
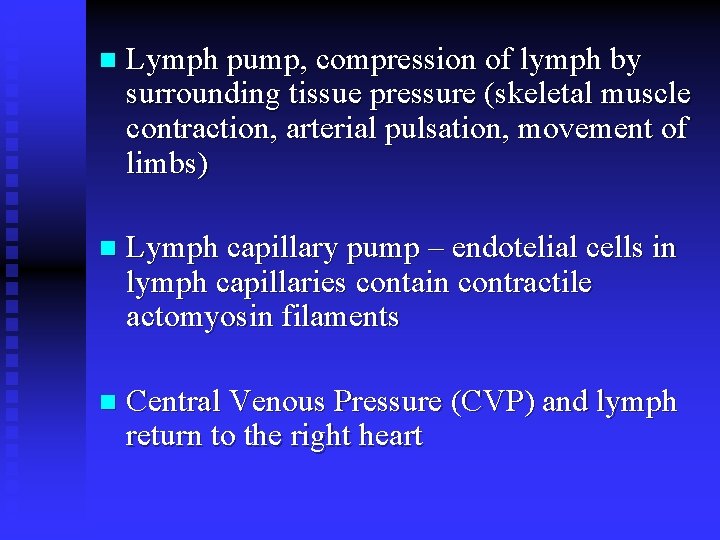
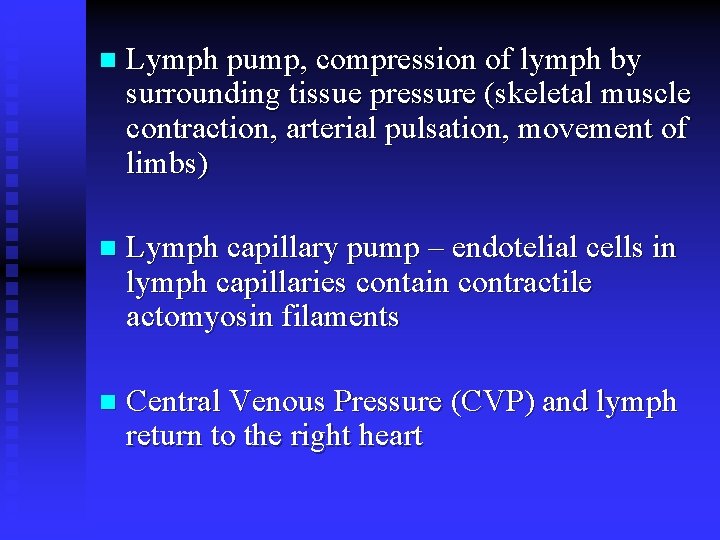
n Lymph pump, compression of lymph by surrounding tissue pressure (skeletal muscle contraction, arterial pulsation, movement of limbs) n Lymph capillary pump – endotelial cells in lymph capillaries contain contractile actomyosin filaments n Central Venous Pressure (CVP) and lymph return to the right heart
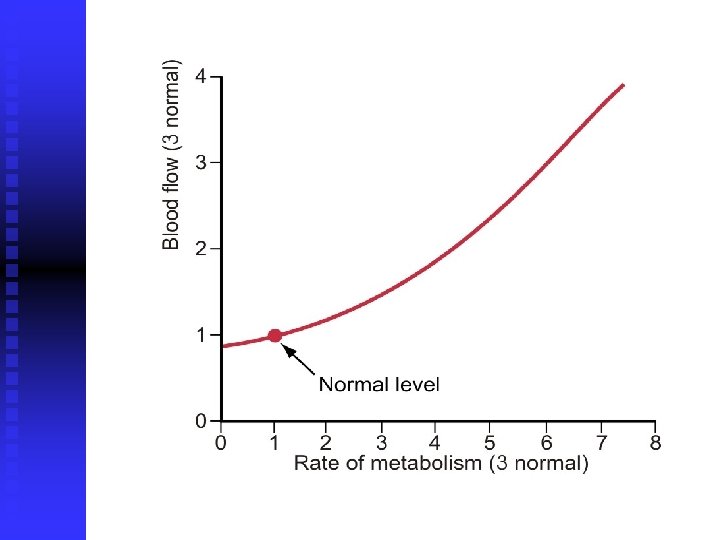
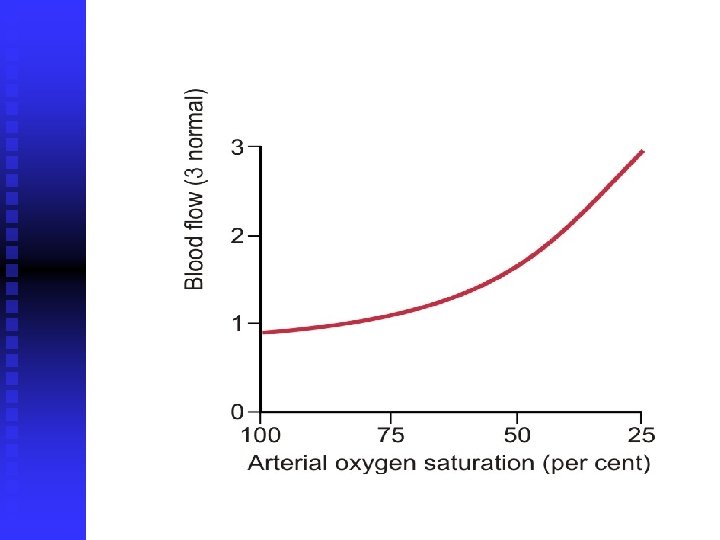
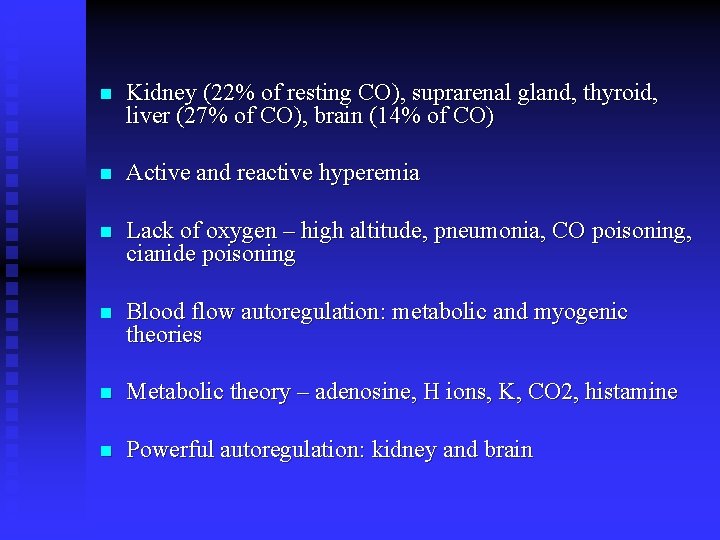
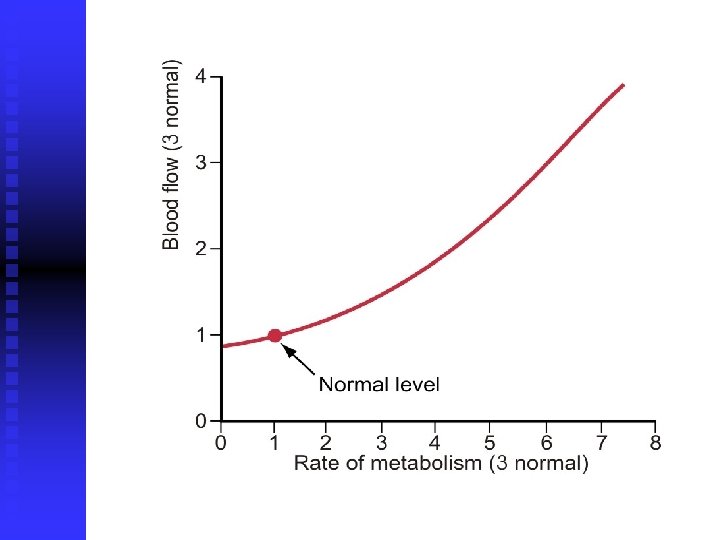
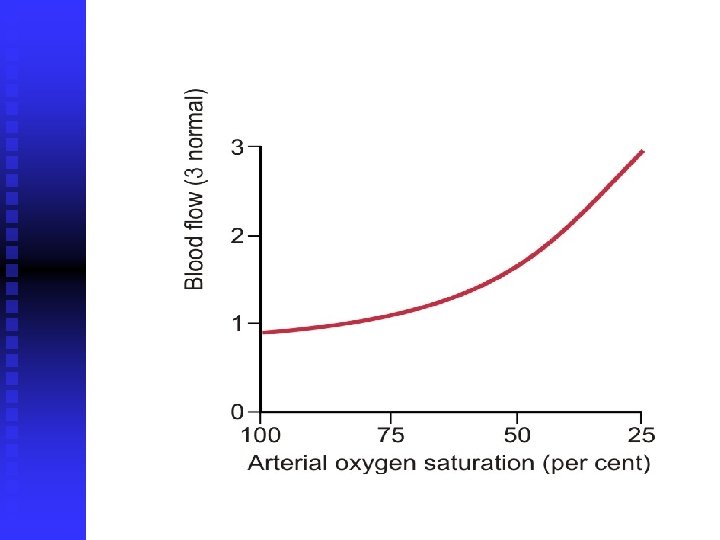
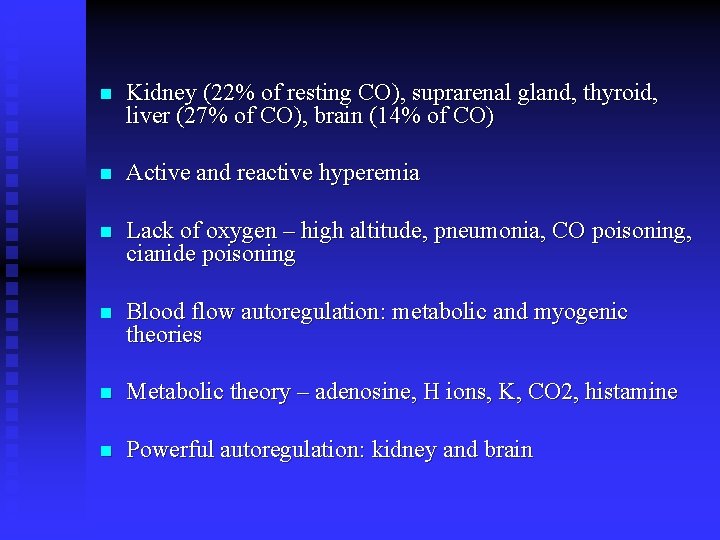
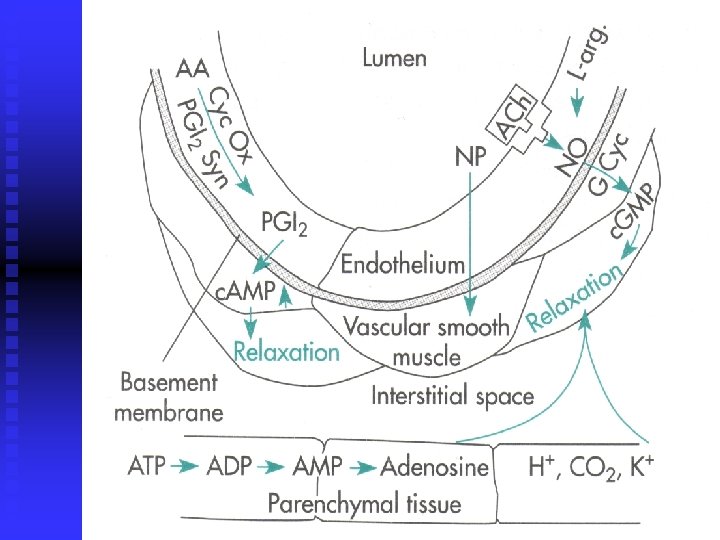
n Kidney (22% of resting CO), suprarenal gland, thyroid, liver (27% of CO), brain (14% of CO) n Active and reactive hyperemia n Lack of oxygen – high altitude, pneumonia, CO poisoning, cianide poisoning n Blood flow autoregulation: metabolic and myogenic theories n Metabolic theory – adenosine, H ions, K, CO 2, histamine n Powerful autoregulation: kidney and brain
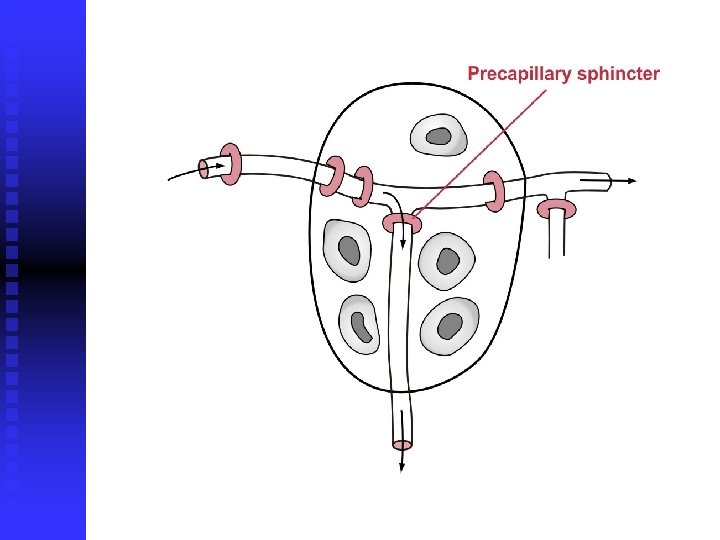
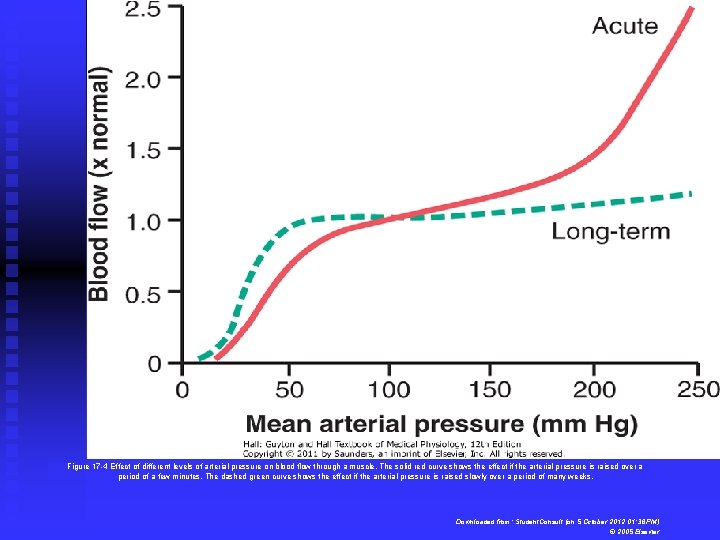
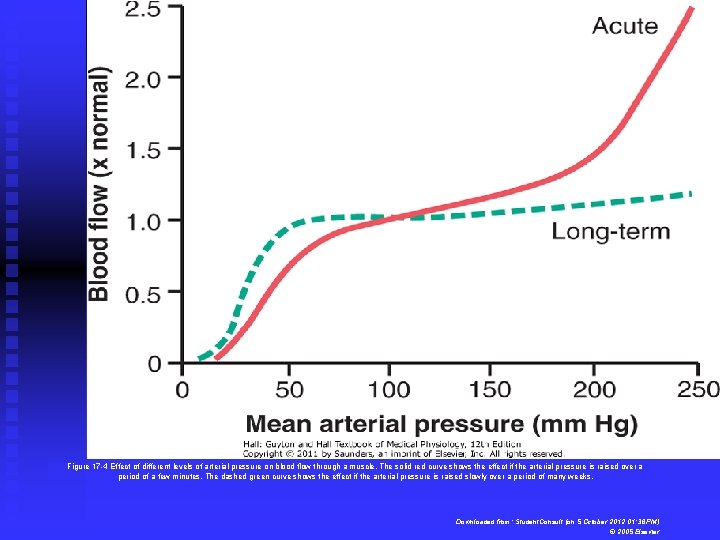
Figure 17 -4 Effect of different levels of arterial pressure on blood flow through a muscle. The solid red curve shows the effect if the arterial pressure is raised over a period of a few minutes. The dashed green curve shows the effect if the arterial pressure is raised slowly over a period of many weeks. Downloaded from: Student. Consult (on 5 October 2012 01: 36 PM) © 2005 Elsevier
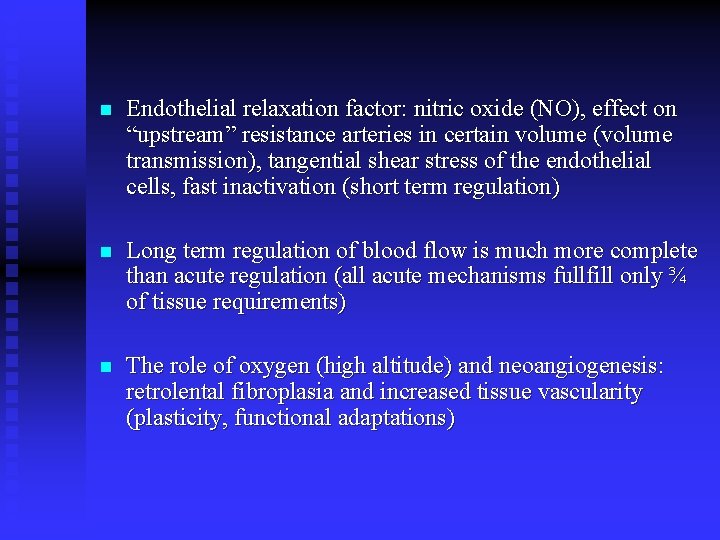
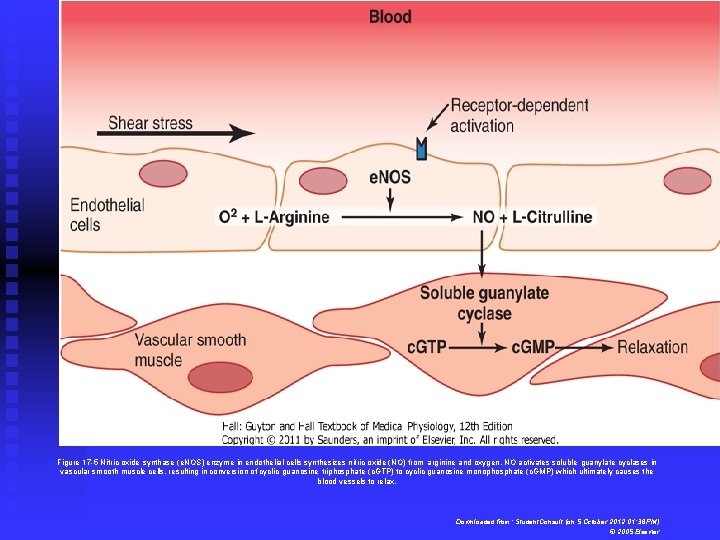
n Endothelial relaxation factor: nitric oxide (NO), effect on “upstream” resistance arteries in certain volume (volume transmission), tangential shear stress of the endothelial cells, fast inactivation (short term regulation) n Long term regulation of blood flow is much more complete than acute regulation (all acute mechanisms fullfill only ¾ of tissue requirements) n The role of oxygen (high altitude) and neoangiogenesis: retrolental fibroplasia and increased tissue vascularity (plasticity, functional adaptations)
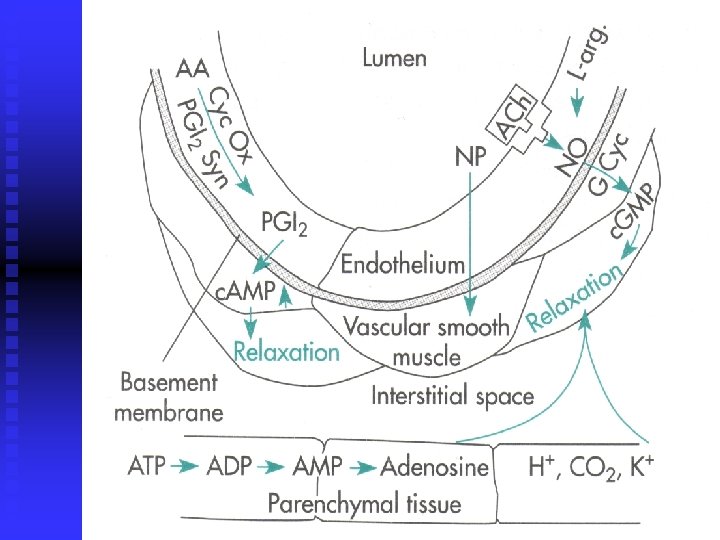
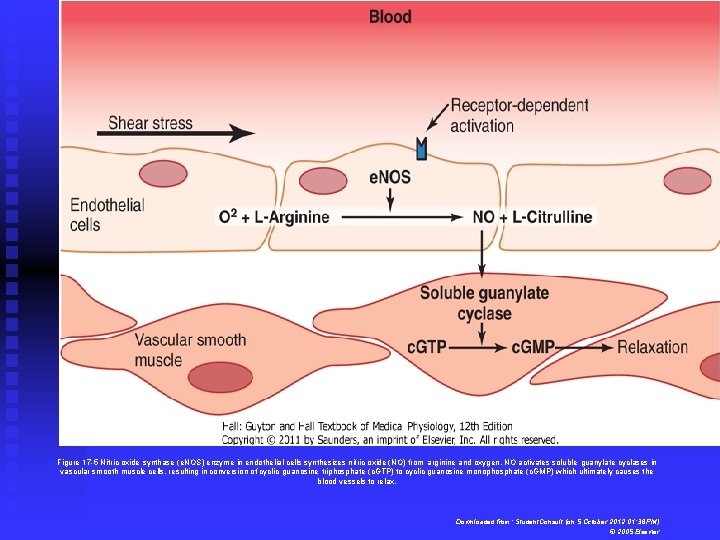
Figure 17 -5 Nitric oxide synthase (e. NOS) enzyme in endothelial cells synthesizes nitric oxide (NO) from arginine and oxygen. NO activates soluble guanylate cyclases in vascular smooth muscle cells, resulting in conversion of cyclic guanosine triphosphate (c. GTP) to cyclic guanosine monophosphate (c. GMP) which ultimately causes the blood vessels to relax. Downloaded from: Student. Consult (on 5 October 2012 01: 36 PM) © 2005 Elsevier
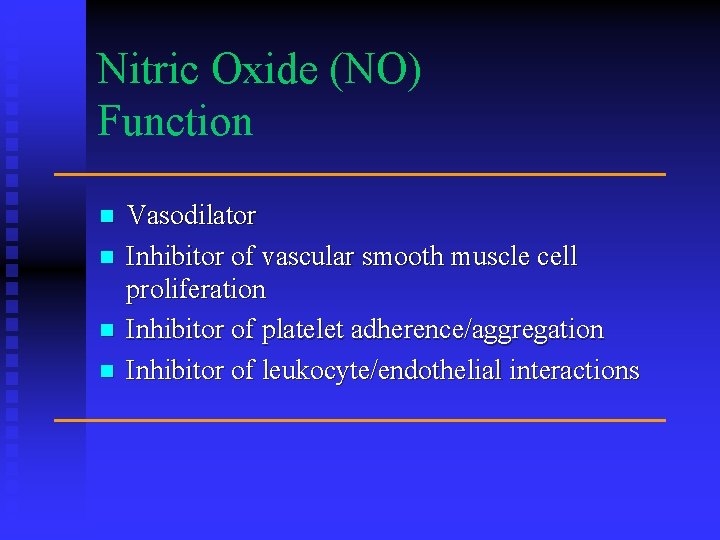
Nitric Oxide (NO) Function n n Vasodilator Inhibitor of vascular smooth muscle cell proliferation Inhibitor of platelet adherence/aggregation Inhibitor of leukocyte/endothelial interactions
Endothelin-1 (ET-1) n Peptide first sequenced in 1988 Most potent vasoconstrictor in humans n Maintenance of basal arterial vasomotor tone n Strong chemoattractant for circulating monocytes and macrophage activation “proatherogenic” n
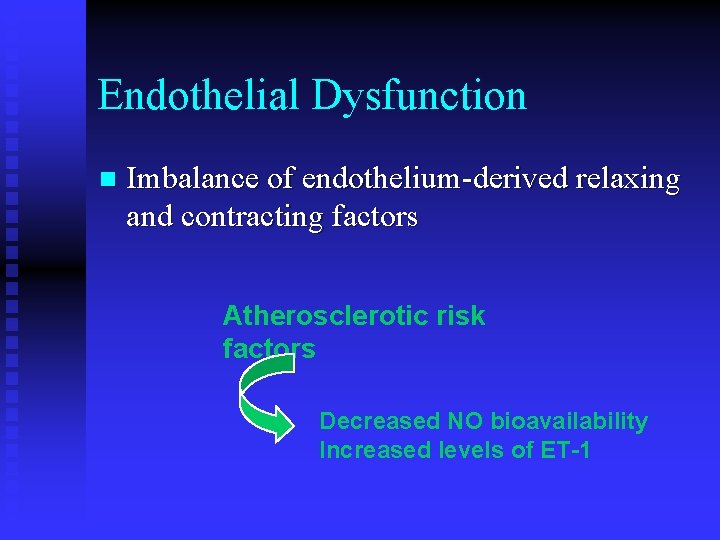
Endothelial Dysfunction n Imbalance of endothelium-derived relaxing and contracting factors Atherosclerotic risk factors Decreased NO bioavailability Increased levels of ET-1
n Vascular endothelial growth factor (VEGF), fibroblast growth factor (FGF), angiogenin – increase angiogenesis, steroid hormones have negative effect n Vascularity is determined by a maximal blood flow and not by the average n Colateral circulation – 60. year old human
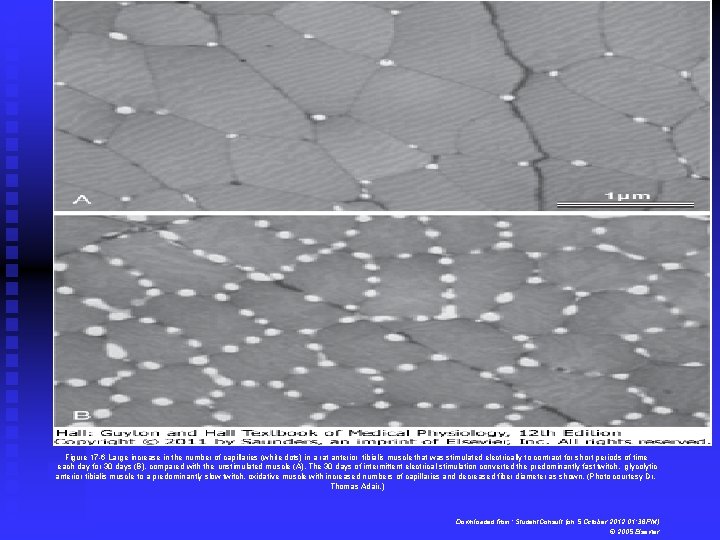
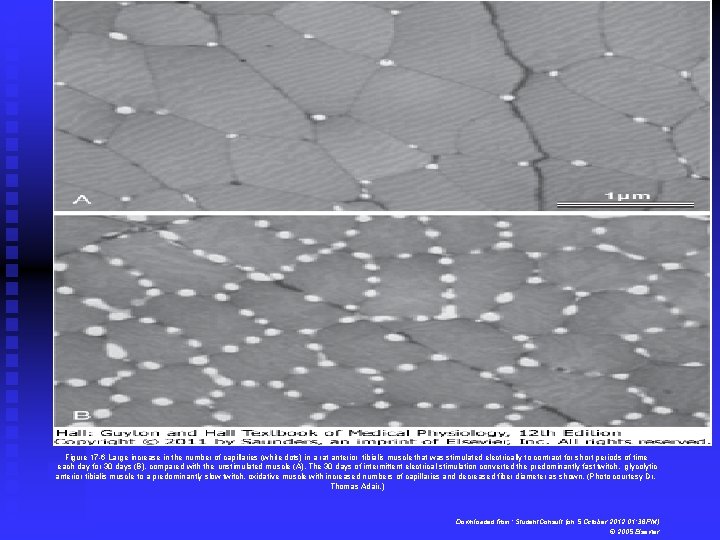
Figure 17 -6 Large increase in the number of capillaries (white dots) in a rat anterior tibialis muscle that was stimulated electrically to contract for short periods of time each day for 30 days (B), compared with the unstimulated muscle (A). The 30 days of intermittent electrical stimulation converted the predominantly fast twitch, glycolytic anterior tibialis muscle to a predominantly slow twitch, oxidative muscle with increased numbers of capillaries and decreased fiber diameter as shown. (Photo courtesy Dr. Thomas Adair. ) Downloaded from: Student. Consult (on 5 October 2012 01: 36 PM) © 2005 Elsevier
n Humoral mediators: vasoconstrictors: epinephrine and norepinephrine (alpha i beta effect), angiotensin II, vasopressin (physiologically only ADH), endothelin n Vasodilators: bradykinin (alpha-2 globulin formed by liver, enzyme kalikrein, kalidin and bradykinin products, inaktivation by carboxypeptidase – the same enzyme activates AII) and inflammation, salivary glands, skin; histamine
n n n Increased calcium – vasocontriction Increased potassium - vasodilatation Increased magnesium – strong vasodilatation Acidosis – vasodilatation, small reduction vasoconstriction, larger reduction vasodilatation Increased CO 2 – vasodilatation, direct, indirect vasoconstriction due to increased central sympathetic activity (basal activity 1 -2 Hz)