Selected Controversies in Pre Hospital Emergency Care Moritz

















- Slides: 74

Selected Controversies in Pre -Hospital Emergency Care Moritz Haager PGY-2 Dr. Ian Wishart April 24, 2003
Objectives Does pre-hospital intubation improve patient outcomes? u Are ALS trained crews superior to BLS only systems? u Are current fluid resuscitation protocols appropriate? u
More is Better. Right? Development of ALS-capable EMS systems based on assumption that earlier provision of advanced interventions will improve outcomes u “The entire basis of prehospital care is directed toward straightforward treatments that make sense based on probable cause of early death” u u Hoyt. Ann Surg. 2003; 237: 161 -2
Multicenter Canadian Study of Prehospital Trauma Care u u Prospective cohort study of EMS systems in 3 major trauma centres 9045 pts treated by BLS-EMT, PMD-ALS, or MD-ALS • 36% inc in odds of dying for MD-ALS • 21% inc in odds of dying for ALS vs BLS • Differences significant even when stratified by Injury Severity Score u Conclude that EMS-ALS crews have no benefit in trauma victims in urban centers
Multicenter Canadian Study of Prehospital Trauma Care u Limitations • MD’s & PMD-ALS crews saw sicker pts • Significant differences in patient population b/w cities involved • Not a randomized study
The Bottomline None of the ALS interventions has been shown to be beneficial in sufficiently rigorous studies u Some (e. g. PASG, IV fluids, pediatric RSI) appear to worsen mortality u Lots of money, training, and ongoing experience required to aquire and maintain skills u
The Bottomline u “it will be difficult for us to accept since we have so much invested in training ALS skills & because of the intuitive nature of these practices for improving outcome” u Hoyt. Ann Surg. 2003; 237: 161 -2
AIRWAY u 1950’s – landmark studies by Elam & Safar demonstrate efficacy of rescue breathing in maintaining O 2 sats @ 90%

Methods for Airway Control u u BVM LMA / intubating LMA Combi-tube ETT • Definitive, but also most complicated u u Surgical airway Where does the balance of risking aspiration vs. failed airway capture lie? Which method is most expedient?
Evaluating Airway Methods u Variables to consider • Time spent capturing airway • Success rate of capturing airway • Complications particular to that method Aspiration u Failed airway u Surgical airway u • Training & experience required • Practicality in anticipated environment
Airway Protection u Non-invasive ventilation predisposes to gastric insufflation • Increased risk of aspiration • Decreased pulmonary compliance u Risk of insufflation increases with decreasing pulmonary compliance & LES tone • • • Ongoing cardiac arrest + CPR Asthma, COPD Obesity, supine position
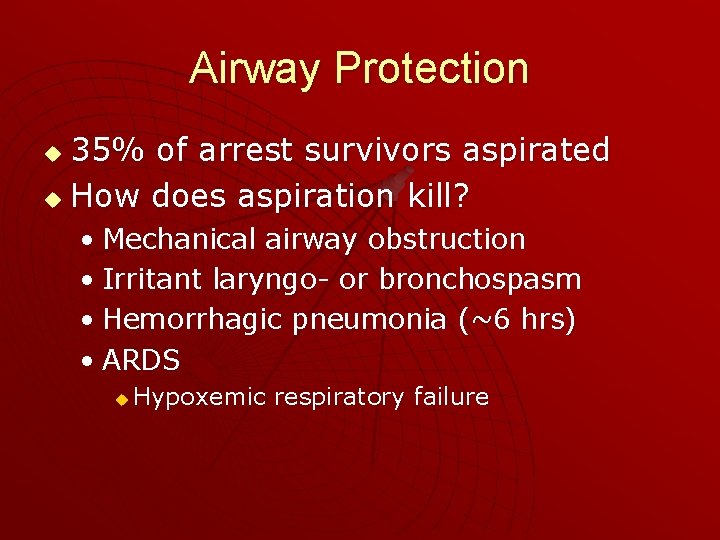
Airway Protection 35% of arrest survivors aspirated u How does aspiration kill? u • Mechanical airway obstruction • Irritant laryngo- or bronchospasm • Hemorrhagic pneumonia (~6 hrs) • ARDS u Hypoxemic respiratory failure
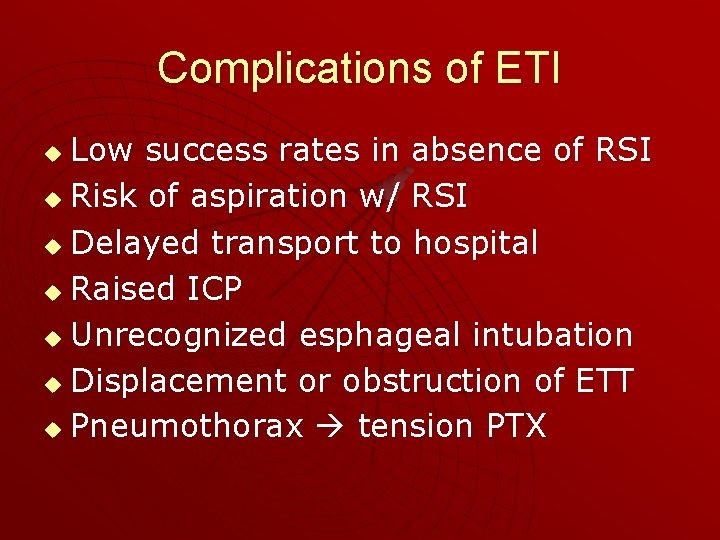
Complications of ETI Low success rates in absence of RSI u Risk of aspiration w/ RSI u Delayed transport to hospital u Raised ICP u Unrecognized esphageal intubation u Displacement or obstruction of ETT u Pneumothorax tension PTX u
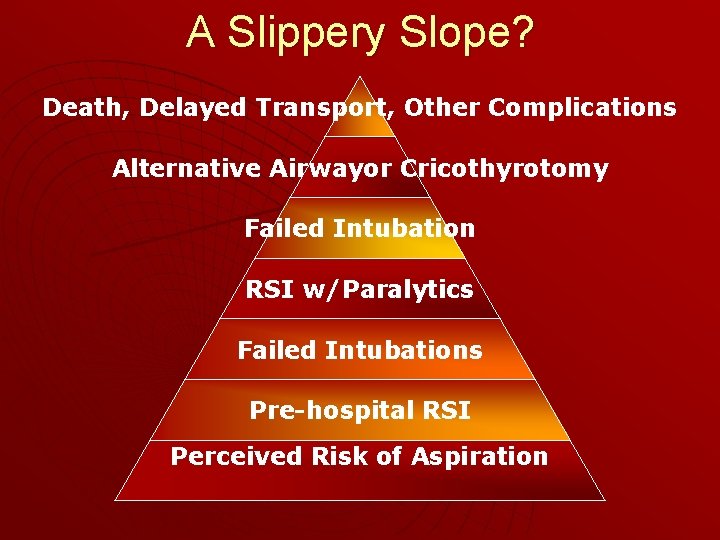
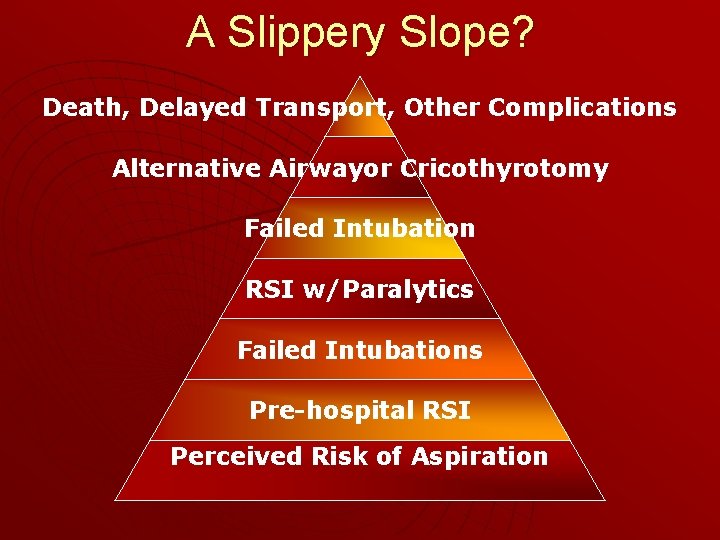
A Slippery Slope? Death, Delayed Transport, Other Complications Alternative Airwayor Cricothyrotomy Failed Intubation RSI w/Paralytics Failed Intubations Pre-hospital RSI Perceived Risk of Aspiration
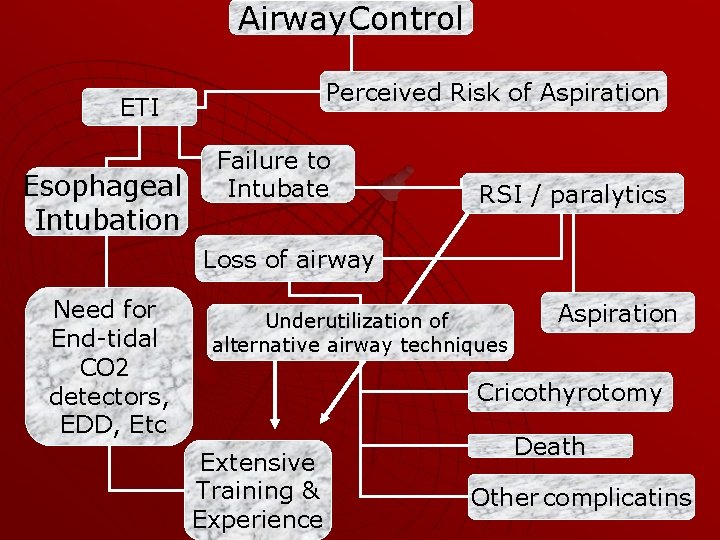
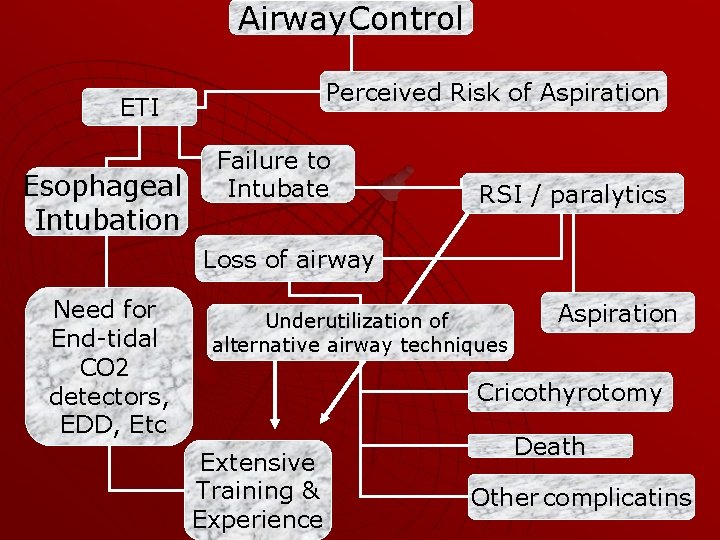
Airway. Control Perceived Risk of Aspiration ETI Esophageal Intubation Failure to Intubate RSI / paralytics Loss of airway Need for End-tidal CO 2 detectors, EDD, Etc Underutilization of alternative airway techniques Aspiration Cricothyrotomy Extensive Training & Experience Death Other complicatins

Should we just keep it simple? Paralytics only in select cases under strict medical control Cricothyrotomy training as true rescue airway only Adequate ventilation & oxygenation + quick transport to definitive care facility Use of LMA +/- ILMA BVM + OPA Combitube
BVM u “there needs to be some alternatives to BVM. Although its use has been encouraged for many years, most providers do not perform this skill well” u u Wayne et al. Prehosp Emerg Care. 1999; 3: 290 -6 “In unskilled hands, maintaining a patent airway whilst at the same time attempting to ventilate the patient is not easy and is performed badly…. alternative airway devices. . may be better than an OPA and BVM” u Nolan. Curr Opinion Crit Care. 2001; 7: 413 -21
Tidal Volume Balance b/w risk of gastric inflation and benefit of pulmonary ventilation u Several studies demonstrate that smaller TV’s decrease gastric distention, but may not achieve adequate P 02 unless suppl O 2 is used u ACLS 2000: u • W/ O 2 use TV 6 -7 ml/kg over 2 sec • W/O O 2 use TV 10 ml/kg over 2 sec

Pre-hospital RSI u u u Widespread use US; less in Canada Locally EMS RSI introduced 2000 Reported success rate 75 -96. 6% Complication rates 5 – 13% Cricothyrotomy rates 1. 1 – 14. 9% • Bulger et al. J Emerg Med 2002; 23: 181 -9 u u u Local success rate ~84% Calgary EMS 2 -10 tubes/yr Local cricothyrotomy rate ~3%
Components of EMS RSI System u NAEMSP Position Paper • Medical direction & supervison • Intensive training including OR-based experience & continuing education programs • Tools for placement confirmation & continous monitoring • Drug delivery & storage provisions • Standardized RSI protocols • Rescue methods & devices • QI / QA programs & performance reviews u Wang et al. Prehosp Emerg Care. 2001; 5: 40 -8
Intubation Conditions u The Field • Fewest helpers & equipment • Least trained & experienced personnel • Awkward positioning & access to pt • Difficulty maintaining calm environment
Intubation Conditions u The ED • More help • More equipment • Better trained & more experienced personnel • Better monitoring of patient • Calmer conditions • Ability to carry out advanced interventions under sterile conditons

ETT Training u 20 year review of Pre-hospital ETI in Whatcom County, Washington 1657 adults underwent RSI w/ sux u 210 (13%) aspirated (1. 2% after sux) u 96. 2% successfully intubated w/ sux u • 3 cricothyrotomies • 6 esophageal intubations • 131 pediatric pts u 97. 6% successfully intubated w/ sux u Wayne et al. Prehosp Emerg Care 1999; 13: 107 -9

ETT Training • Pre-hospital ETI Training in Whatcom County, Washington 2500 hrs to achieve certification u > 20 intubations in OR u > 1 ETI /month & 1/yr in OR to maintain certification in first 3 yrs u Subsequently > 1 ETI q 3 mo & 1 in OR u u Wayne et al. Prehosp Emerg Care. 1999; 3: 290 -6 • Seattle Similar training requirements u Animal lab q 2 yrs for surgical airway skills u u Bulger et al. J Emerg Med 2002; 23: 183 -9
Training u “no clear consensus on the number of intubations required to train prehospital personnel adequately or on the number they need to undertake to maintain their skills. In comparison with anesthesiology trainees, all these paramedic students are undertaking far fewer intubations. ” u u Nolan. Curr Opinion Crit Care. 2001; 7: 413 -21 Experience & success rate in anesthesia residents • >58 intubations req’d for >90% success rate • >90 intubations req’d for >95% success rate u Konrad et al. Anesth Analg. 1998; 86: 635 -9
Success Rate Pre-hospital intubation 75 -98. 4% u Paramedic students in OR setting u • 94% 1 st try LMA vs. 69% ETT • 10% failed ETT vs 0% LMA u u Pennant & Walker. Anest Analg 1992. 74: 531 -34 Novices trained on 110 pts in OR • 94% success with LMA vs. 51% w/ ETT u Davies et al. Lancet. 1990. 336: 977
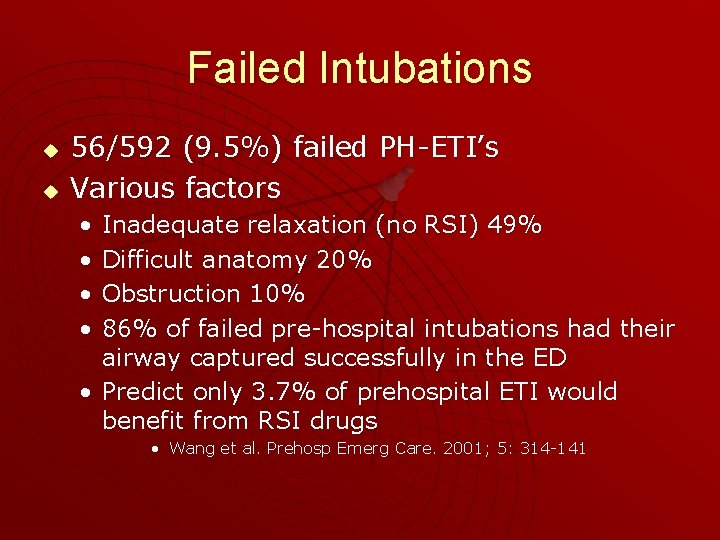
Failed Intubations u u 56/592 (9. 5%) failed PH-ETI’s Various factors • • Inadequate relaxation (no RSI) 49% Difficult anatomy 20% Obstruction 10% 86% of failed pre-hospital intubations had their airway captured successfully in the ED • Predict only 3. 7% of prehospital ETI would benefit from RSI drugs • Wang et al. Prehosp Emerg Care. 2001; 5: 314 -141
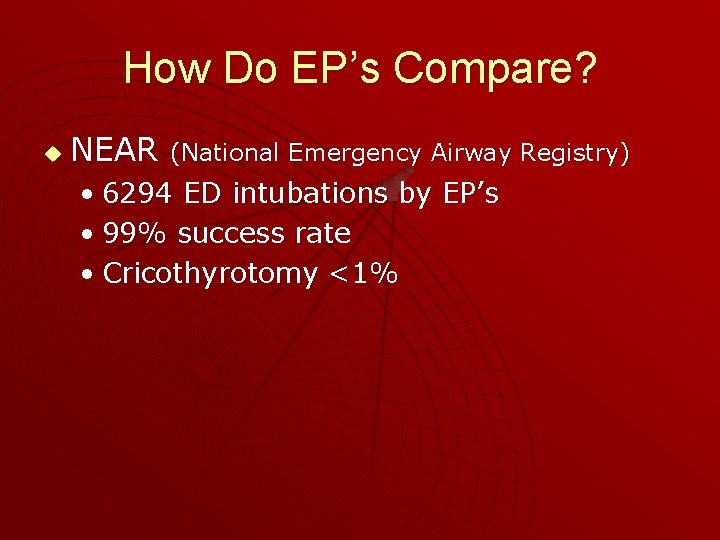
How Do EP’s Compare? u NEAR (National Emergency Airway Registry) • 6294 ED intubations by EP’s • 99% success rate • Cricothyrotomy <1%

RSI in Seattle u Retrospective study of 2614 pts who underwent intubation • 5. 4% intubation rate • 50% underwent RSI w/ Sux • 98. 4% success rate • 1. 1% surgical airway rate • 0. 6% unabale to achieve airway – BVM • No long-term outcome, # of intubation attempts, or scene time data u Bulger et al. J Emerg Med 2002; 23: 183 -9
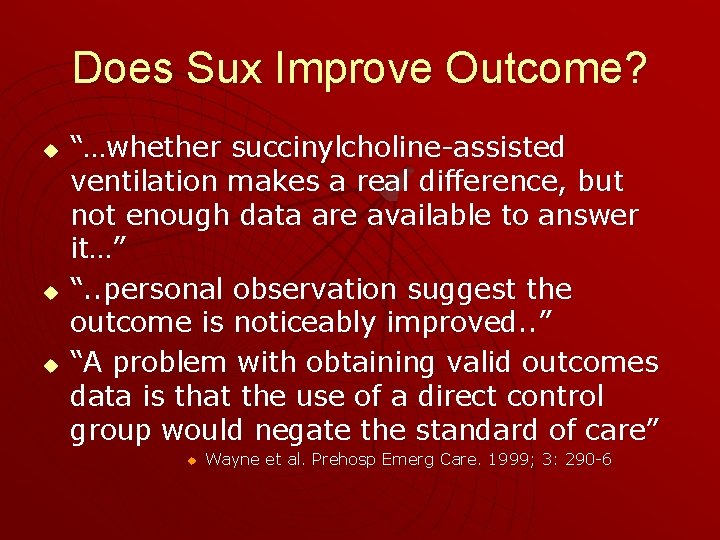
Does Sux Improve Outcome? u u u “…whether succinylcholine-assisted ventilation makes a real difference, but not enough data are available to answer it…” “. . personal observation suggest the outcome is noticeably improved. . ” “A problem with obtaining valid outcomes data is that the use of a direct control group would negate the standard of care” u Wayne et al. Prehosp Emerg Care. 1999; 3: 290 -6
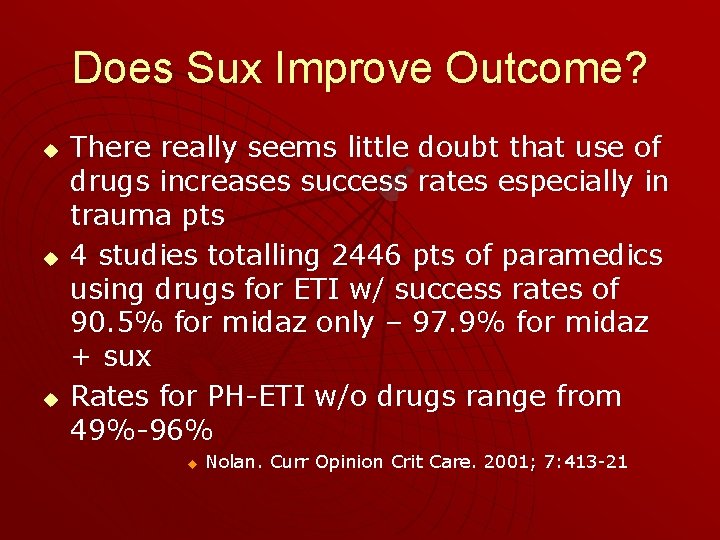
Does Sux Improve Outcome? u u u There really seems little doubt that use of drugs increases success rates especially in trauma pts 4 studies totalling 2446 pts of paramedics using drugs for ETI w/ success rates of 90. 5% for midaz only – 97. 9% for midaz + sux Rates for PH-ETI w/o drugs range from 49%-96% u Nolan. Curr Opinion Crit Care. 2001; 7: 413 -21
Prehospital RSI in CHI Prospective case-control study of 209 head-injured adult trauma victims compared to 627 handmatched controls u excluded pts intubated w/o RSI from both groups u all pts first had non-RSI attempts at ETI u paramedics had 8 hr training course in RSI u
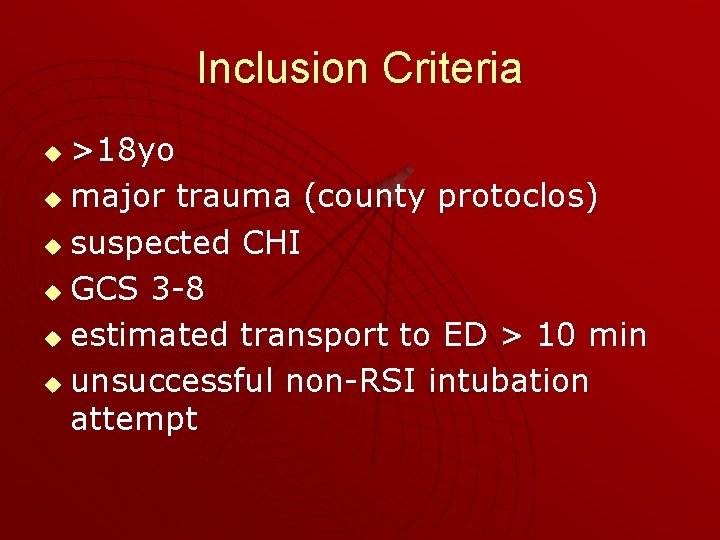
Inclusion Criteria >18 yo u major trauma (county protoclos) u suspected CHI u GCS 3 -8 u estimated transport to ED > 10 min u unsuccessful non-RSI intubation attempt u
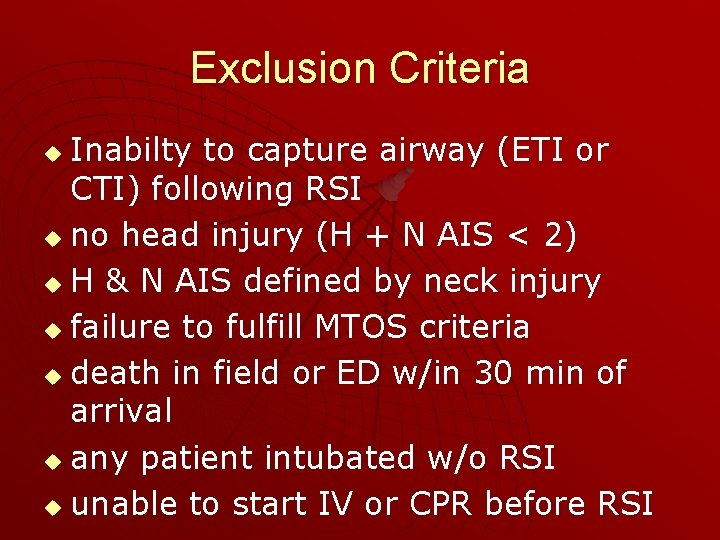
Exclusion Criteria Inabilty to capture airway (ETI or CTI) following RSI u no head injury (H + N AIS < 2) u H & N AIS defined by neck injury u failure to fulfill MTOS criteria u death in field or ED w/in 30 min of arrival u any patient intubated w/o RSI u unable to start IV or CPR before RSI u
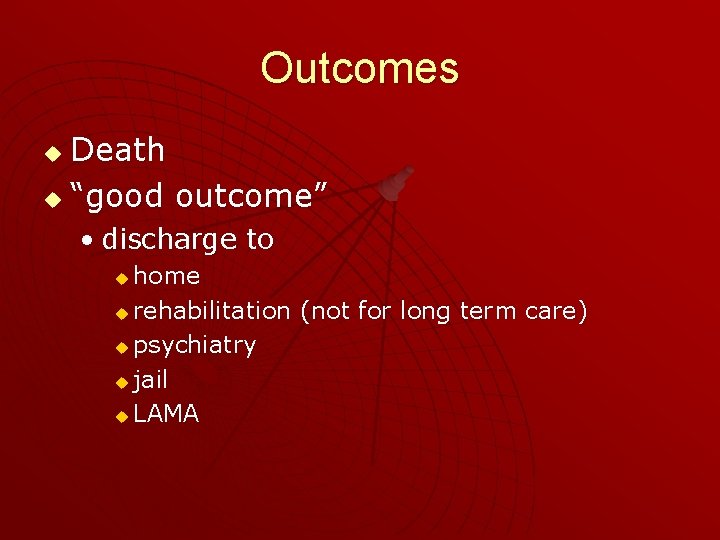
Outcomes Death u “good outcome” u • discharge to home u rehabilitation (not for long term care) u psychiatry u jail u LAMA u
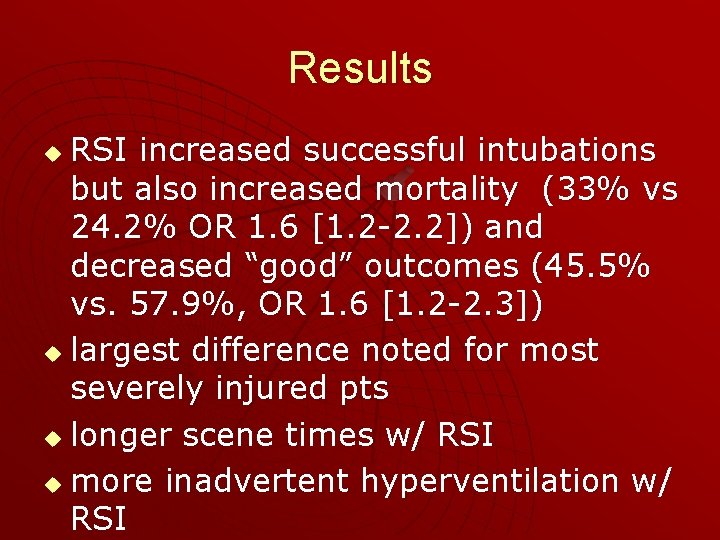
Results RSI increased successful intubations but also increased mortality (33% vs 24. 2% OR 1. 6 [1. 2 -2. 2]) and decreased “good” outcomes (45. 5% vs. 57. 9%, OR 1. 6 [1. 2 -2. 3]) u largest difference noted for most severely injured pts u longer scene times w/ RSI u more inadvertent hyperventilation w/ RSI u
Study Conclusions Prehospital RSI causes increased mortality and morbidity u Trial suspended until cause for increased mortality can be determined u
Criticisms Did not compare RSI-intubated pts w/ non-RSI intubated pts u by inclusion criteria, all pts had at least 2 attempts at intubation u minimal training & experience in RSI u 67 / 209 pts ultimately had minor or no head injury u no power calculation u not randomized u
My Conclusions Methodologic flaws make drawing conclusions difficult u Taken together with other recent studies suggests that prehospital RSI intubation may be harmful u
RSI Consensus meeting failed to embrace pre-hospital RSI u Lack of evidence for its benefit u u Wayne et al. Prehosp Emerg Care. 1999; 3: 290 -6
Complications u Surgical airway • 1. 1 – 14. 9% u A review of failed pre-hospital airway mgmt cases demonstrated • Questionable indications for intubation • Lack of alternative rescue techniques employed prior to cricothyrotomy • Extensive complications u Mizelle et al. Prehosp Emerg Care. 2002; 6: 472 -75

Unrecognized Esophageal Intubation u PH-ETI with drugs • 0. 4% rate in 2 retrospective studies u u u Wang et al. Prehosp Emerg Care. 2001; 5: 134 -41 Wang et al. Prehosp Emerg Care. 1999; 3: 377 -78 PH-ETI without drugs • Prospective observational study in urban EMS • 108 pts had ETT placement checked upon arrival in ED: u u u • • “Clearly misplaced” (epigastric sounds, vomitus per tube) – only in 4 / 27 pts not confirmed by direct laryngoscopy ETCO 3 for all pts Auscaultation & direct laryngoscopy 25% misplaced (18/27 in esophagus) ETCO 2 use in field purposely not recorded No central direct medical oversight of EMS Concluded rate of misplacement much higher than thought u Katz & Falk. Ann Emerg Med. 2001; 37: 62 -4

Verifying Tube Position u u u ETCO 2 is the recommended gold standard in all locations Prospective study of self-inflating bulb EDD in 65 pts intubated in ED for cardiac arrest EDD 100% (5/5) sens for esophageal placement, but 18 false +ve’s (poor spec) ETCO 2 100% sens for esophageal placement, but also no ETCO 2 in 26/60 tracheal intubations EDD & ETCO 2 together only have 90. 8% sensitivity for tracheal placement u u Tanigawa et al. Anesthesiology. 2000; 93: 1432 -6 Other studies suggest the syringe EDD is 99% sensitive for tracheal intubation u Bozeman et al. Ann Emerg Med 1996; 27: 595 -9

Verifying Tube Position u Other studies suggest the syringe EDD is 99% sensitive for tracheal intubation u u u u Prospective randomized X-over study 48 cardiac arrest pts intubated in ED SIB, Syringe ETT, & ETCO 2 No sig differences b/w the 2 EDD’s Similar sensitivity for tracheal intubation (70. 872. 9%) as previous study 100% sens (8) for esophageal intubation u u Bozeman et al. Ann Emerg Med 1996; 27: 595 -9 Tanigawa et al. Anesth Analg 2001; 92: 375 -8 All studies hampered by small sample size & lack of a consistent gold-standard
Outcome Data for ETI u “there are no well-controlled, prospective studies showing that outcome is influenced by tracheal intubation by paramedics” u Nolan. Curr Opinion Crit Care. 2001; 7: 413 -21
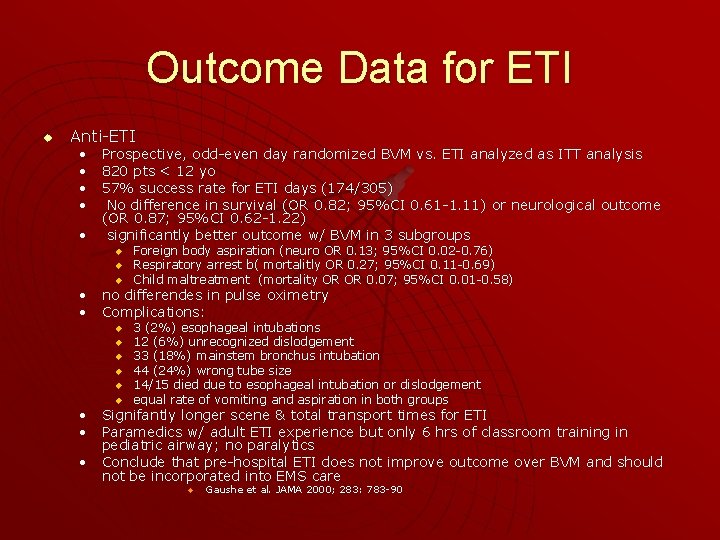
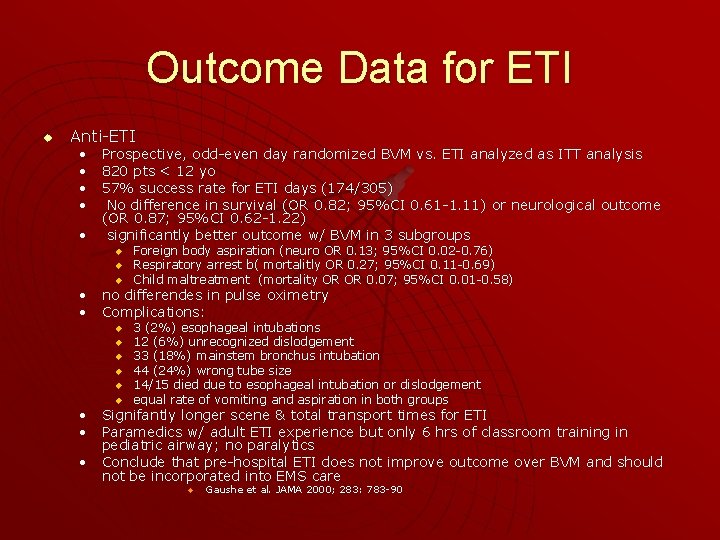
Outcome Data for ETI u Anti-ETI • Prospective, odd-even day randomized BVM vs. ETI analyzed as ITT analysis • 820 pts < 12 yo • 57% success rate for ETI days (174/305) • No difference in survival (OR 0. 82; 95%CI 0. 61 -1. 11) or neurological outcome (OR 0. 87; 95%CI 0. 62 -1. 22) • significantly better outcome w/ BVM in 3 subgroups u u u Foreign body aspiration (neuro OR 0. 13; 95%CI 0. 02 -0. 76) Respiratory arrest b( mortalitly OR 0. 27; 95%CI 0. 11 -0. 69) Child maltreatment (mortality OR OR 0. 07; 95%CI 0. 01 -0. 58) • no differendes in pulse oximetry • Complications: u u u 3 (2%) esophageal intubations 12 (6%) unrecognized dislodgement 33 (18%) mainstem bronchus intubation 44 (24%) wrong tube size 14/15 died due to esophageal intubation or dislodgement equal rate of vomiting and aspiration in both groups • Signifantly longer scene & total transport times for ETI • Paramedics w/ adult ETI experience but only 6 hrs of classroom training in pediatric airway; no paralytics • Conclude that pre-hospital ETI does not improve outcome over BVM and should not be incorporated into EMS care u Gaushe et al. JAMA 2000; 283: 783 -90

Outcome Data for ETI u Pro ETI • • Retrospective case-control study 1092 blunt trauma pts w/ GCS < 8 ALS crews, no paralytics or sedation 51. 7% intubated
• Significantly less mortality in ETI group (26%) vs non-ETI group (36%) for all comers, BUT more people able to be discharged home in non ETI group (63. 1% vs. 54. 8%) • odds ratio for mortality 1. 6 for all pts • odds ratio for mortality 3. 0 for isolated severe CHI subgroup (but no difference in morbidity) • also separately calculated Aeromedical data found sig increase in mortality for ETI pts (35%) vs non-intubated pts (21%) all comers - attributed to sicker pts • Concluded PH-ETI saves lives u Winchell & Hoyt. Arch Surg. 1997; 132: 592 -97

u Criticisms • no comparison of intubation attempts b/w groups • no data on why the non-ETI pts were not intubated • no scene time data • not randomized or prospective • don’t comment on discrepancies, and ignore other data • no sample size estimate / power calc’n
My Conclusions At best this study fails to show a difference in functional outcome u At worst it suggest that functional outcome is actually better in the non. ETI group, and that mortality is increased by ETI by aeromedical crews u
Anti Prehospital ETI u Grant et al. J Trauma. 2003; 54: 307 -11 • Prospective cohort study on 191 adult trauma pts • 41% intubated in field, 59% in ED • 92% blunt trauma
Inclusion & Exclusion Criteria u Inclusion • GCS < 8 + HAIS > 3 • intubated in field or in ED u Exclusion • death w/in 48 hrs • failed field intubations • extrication >30 min • on-site physicians • transfers
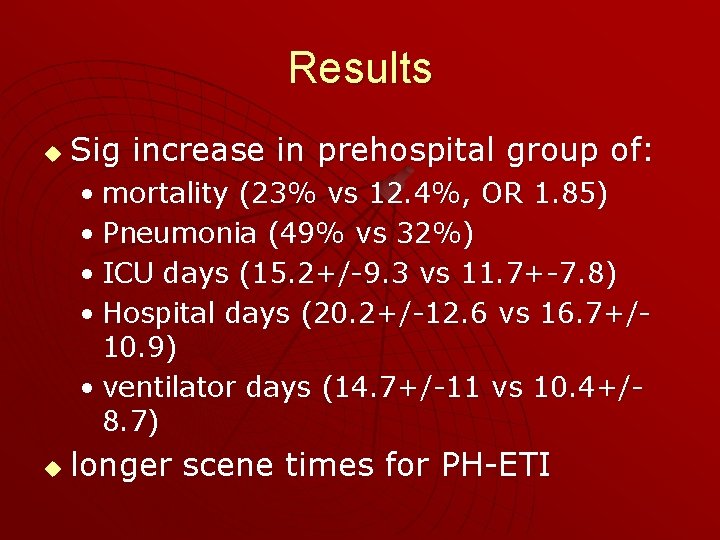
Results u Sig increase in prehospital group of: • mortality (23% vs 12. 4%, OR 1. 85) • Pneumonia (49% vs 32%) • ICU days (15. 2+/-9. 3 vs 11. 7+-7. 8) • Hospital days (20. 2+/-12. 6 vs 16. 7+/10. 9) • ventilator days (14. 7+/-11 vs 10. 4+/8. 7) u longer scene times for PH-ETI

Conclusions Field intubation associated with higher mortality & morbidity than intubation in the ED u recommend RCT to define more clearly which pts may benefit f u
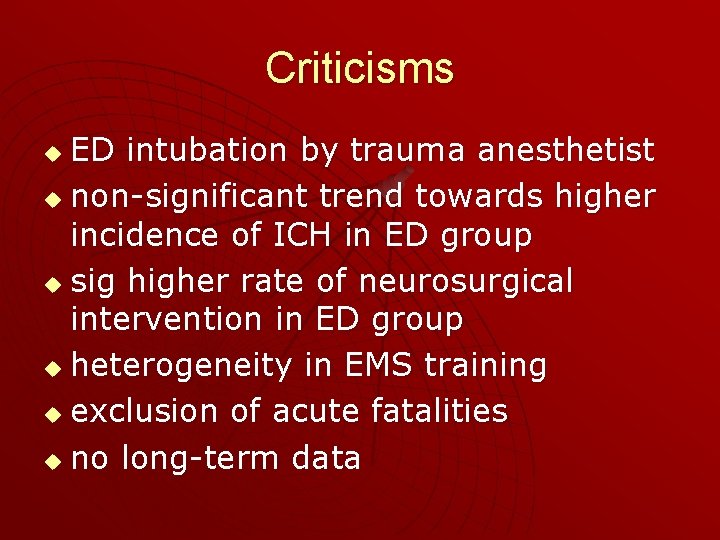
Criticisms ED intubation by trauma anesthetist u non-significant trend towards higher incidence of ICH in ED group u sig higher rate of neurosurgical intervention in ED group u heterogeneity in EMS training u exclusion of acute fatalities u no long-term data u
u “While the potential benefits of successful prehospital tracheal intubation remain controversial, the harm caused by unrecognized esophageal intubation is indisputable” u Nolan. Curr Opinion Crit Care. 2001; 7: 41321
LMA
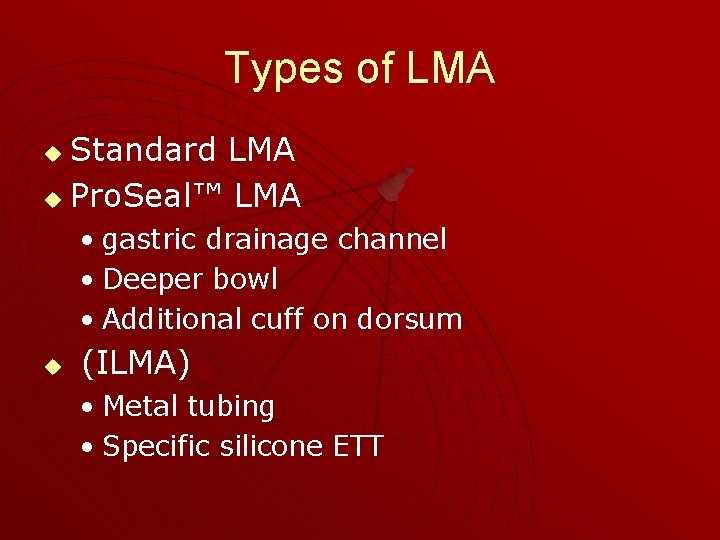
Types of LMA Standard LMA u Pro. Seal™ LMA u • gastric drainage channel • Deeper bowl • Additional cuff on dorsum u (ILMA) • Metal tubing • Specific silicone ETT
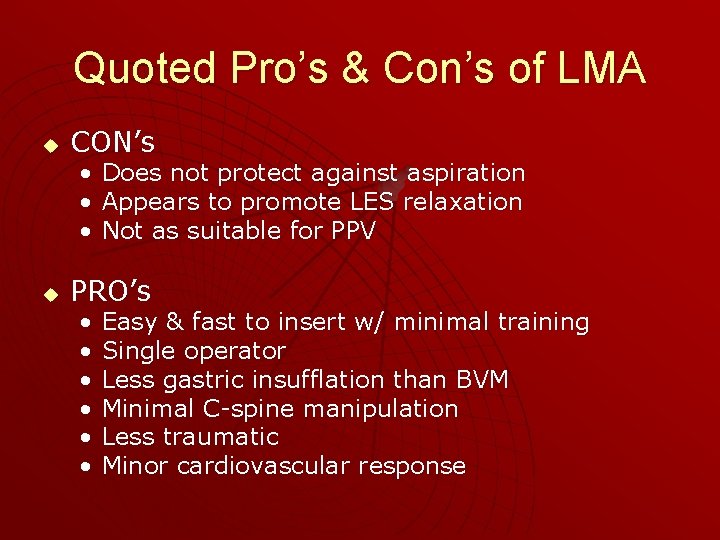
Quoted Pro’s & Con’s of LMA u CON’s • Does not protect against aspiration • Appears to promote LES relaxation • Not as suitable for PPV u PRO’s • • • Easy & fast to insert w/ minimal training Single operator Less gastric insufflation than BVM Minimal C-spine manipulation Less traumatic Minor cardiovascular response
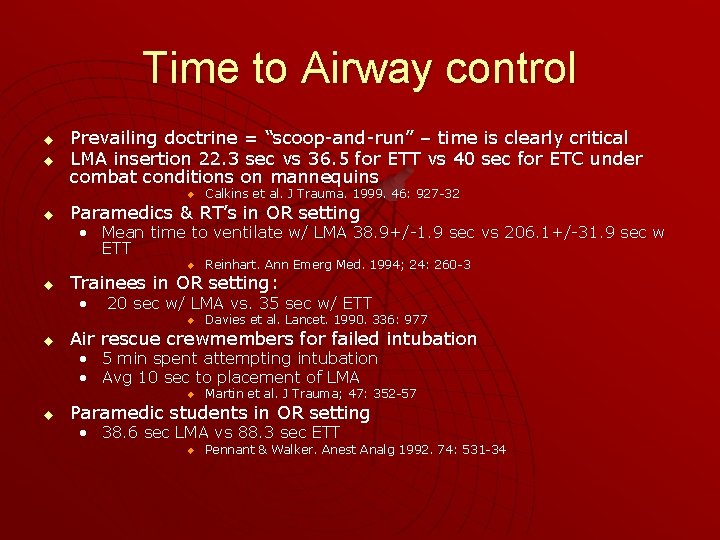
Time to Airway control u u Prevailing doctrine = “scoop-and-run” – time is clearly critical LMA insertion 22. 3 sec vs 36. 5 for ETT vs 40 sec for ETC under combat conditions on mannequins u u Calkins et al. J Trauma. 1999. 46: 927 -32 Paramedics & RT’s in OR setting • Mean time to ventilate w/ LMA 38. 9+/-1. 9 sec vs 206. 1+/-31. 9 sec w ETT u u Trainees in OR setting: • 20 sec w/ LMA vs. 35 sec w/ ETT u u Reinhart. Ann Emerg Med. 1994; 24: 260 -3 Davies et al. Lancet. 1990. 336: 977 Air rescue crewmembers for failed intubation • 5 min spent attempting intubation • Avg 10 sec to placement of LMA u u Martin et al. J Trauma; 47: 352 -57 Paramedic students in OR setting • 38. 6 sec LMA vs 88. 3 sec ETT u Pennant & Walker. Anest Analg 1992. 74: 531 -34

Training u Novice success w/ minimal training suggests minimal deterioration of skill over time • Davies et al. Lancet. 1990. 336: 977 u Significantly more instruction required for ETT than LMA • Pennant & Walker. Anest Analg 1992. 74: 531 -34 u Paramedics & RT’s previously trained in intubation but not LMA inserion in OR setting • Attempts 1 for LMA vs 2. 22+/-0. 21 for ETT • VA score of difficulty 8. 64 for LMA vs 67. 3 for ETT u Reinhart. Ann Emerg Med. 1994; 24: 260 -3
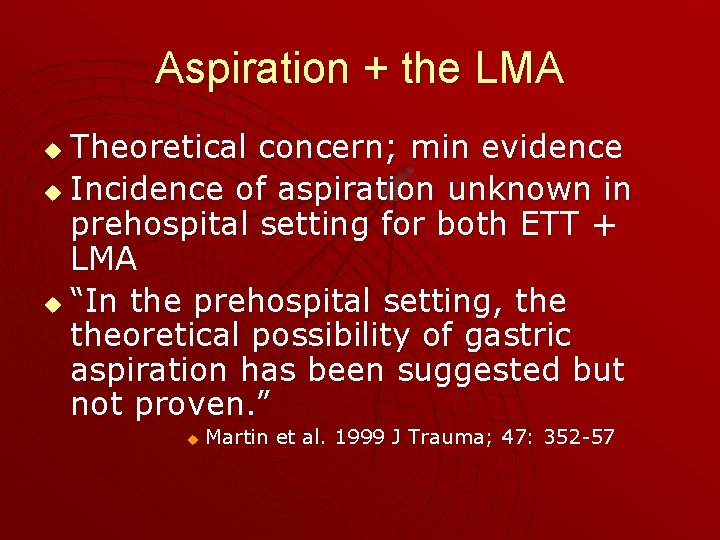
Aspiration + the LMA Theoretical concern; min evidence u Incidence of aspiration unknown in prehospital setting for both ETT + LMA u “In the prehospital setting, theoretical possibility of gastric aspiration has been suggested but not proven. ” u u Martin et al. 1999 J Trauma; 47: 352 -57
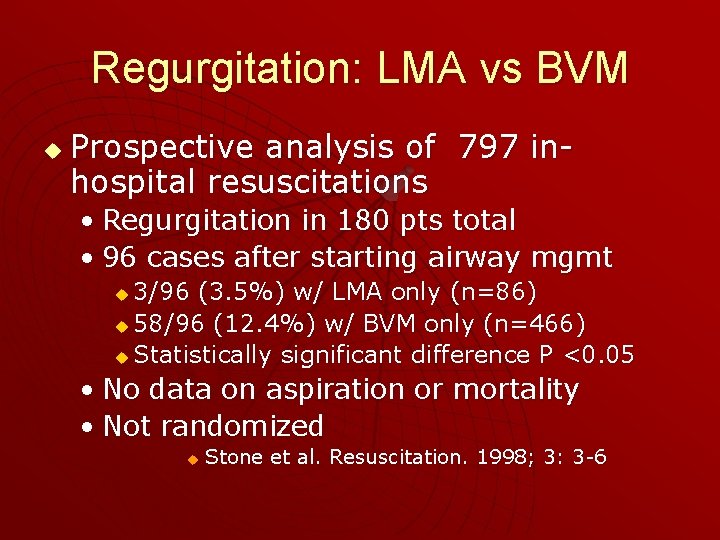
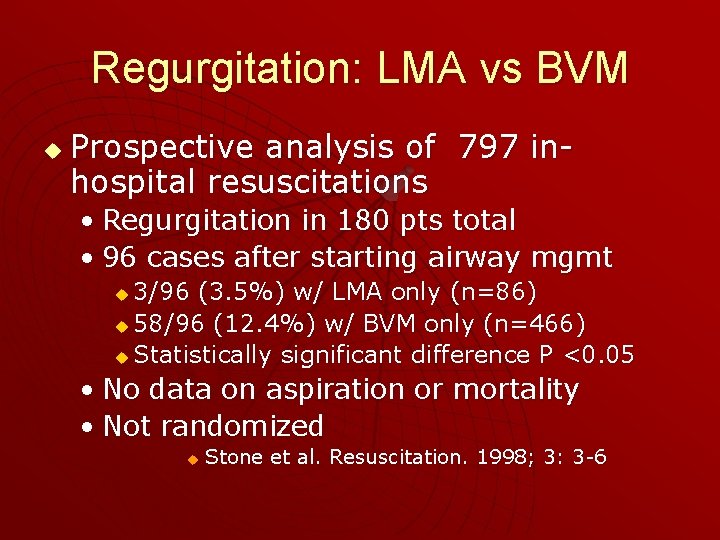
Regurgitation: LMA vs BVM u Prospective analysis of 797 inhospital resuscitations • Regurgitation in 180 pts total • 96 cases after starting airway mgmt 3/96 (3. 5%) w/ LMA only (n=86) u 58/96 (12. 4%) w/ BVM only (n=466) u Statistically significant difference P <0. 05 u • No data on aspiration or mortality • Not randomized u Stone et al. Resuscitation. 1998; 3: 3 -6
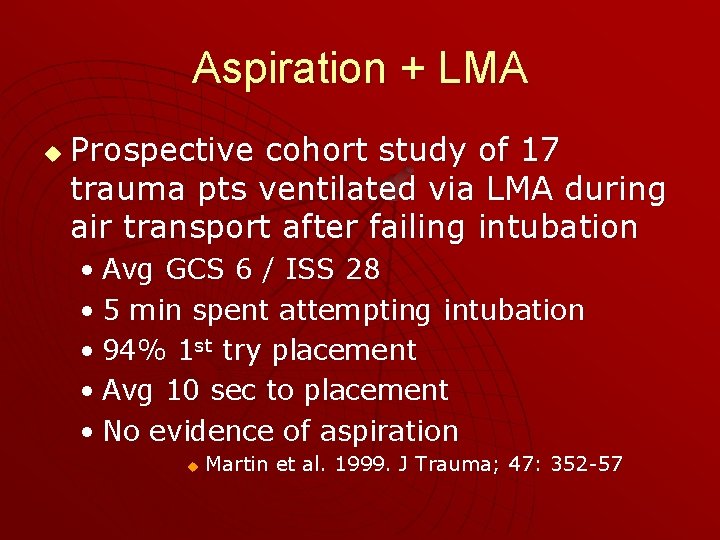
Aspiration + LMA u Prospective cohort study of 17 trauma pts ventilated via LMA during air transport after failing intubation • Avg GCS 6 / ISS 28 • 5 min spent attempting intubation • 94% 1 st try placement • Avg 10 sec to placement • No evidence of aspiration u Martin et al. 1999. J Trauma; 47: 352 -57

Aspiration + the LMA u Retrospective review of surgical pts • Aspiration 1/11960 (0. 009%) • Regurgitation 4/11960 (0. 03%) • 83. 5% elective, only 1. 36% > ASA III u u w/ ILMA risk is 2. 6/10000 elective + 11/10000 emergency cases u u Verghese et al. Anesth Analg. 1996; 82: 129 -133 Dries et al. Air Med J. 2001. 20: 35 -37 3/146 cases of vomitus in airway at time of replacement of LMA by ETT in ED in prospective analysis u Rumball & Mac. Donald. Prehosp Emerg Care. 1997; 1: 1 -10
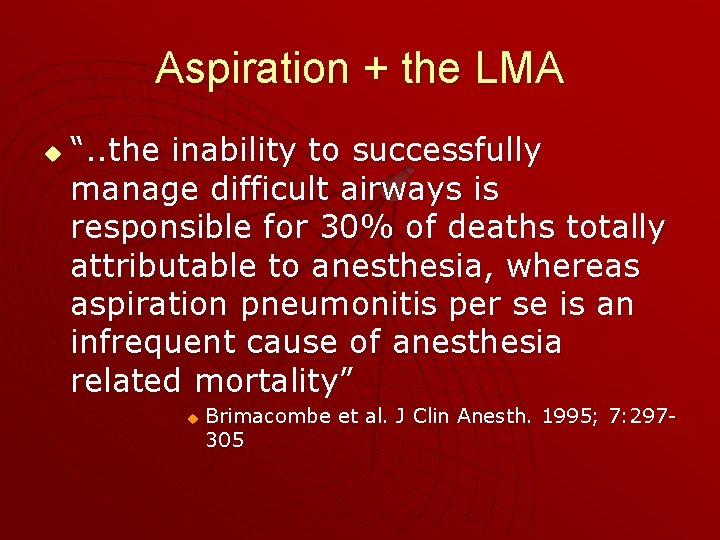
Aspiration + the LMA u “. . the inability to successfully manage difficult airways is responsible for 30% of deaths totally attributable to anesthesia, whereas aspiration pneumonitis per se is an infrequent cause of anesthesia related mortality” u Brimacombe et al. J Clin Anesth. 1995; 7: 297305
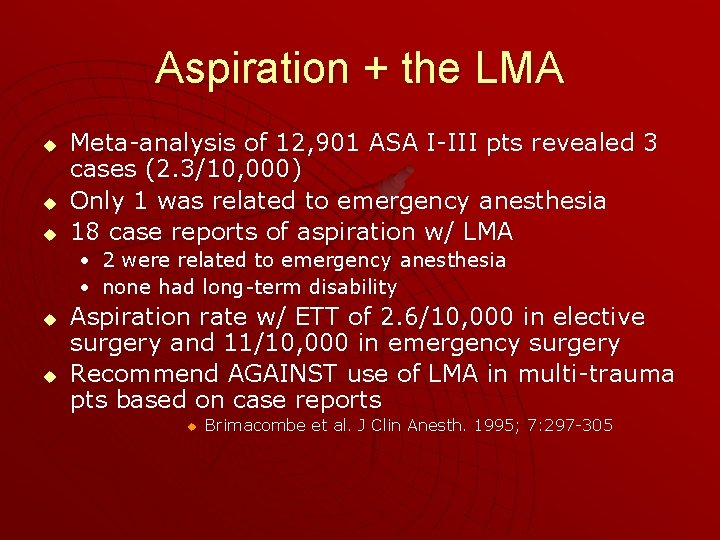
Aspiration + the LMA u u u Meta-analysis of 12, 901 ASA I-III pts revealed 3 cases (2. 3/10, 000) Only 1 was related to emergency anesthesia 18 case reports of aspiration w/ LMA • 2 were related to emergency anesthesia • none had long-term disability u u Aspiration rate w/ ETT of 2. 6/10, 000 in elective surgery and 11/10, 000 in emergency surgery Recommend AGAINST use of LMA in multi-trauma pts based on case reports u Brimacombe et al. J Clin Anesth. 1995; 7: 297 -305
LMA Insufficient data on LMA to make recommendations regarding its use in pre-hospital setting u “the group was concerned about the learning curve required for its use” u LMA provides some airway protection but is felt to be inferior to the ETT u u Wayne et al. Prehosp Emerg Care. 1999; 3: 290 -6

Combitube
Comitube u u Double lumen airway Distal & proximal cuffs Blind placement Provides some protection against aspiration
Combitube u Pros u Cons • Bulky, no pediatric sizes • Expensive • Esophageal rupture (> 3 cases reported) • May ventilate through wrong lumen
Which Airway Device? u u u Prospective pseudo-randomized crossover study of rural BLS crews comparing PTL, Combitube, LMA, + OA/BVM Some were OR-trained, others were manniquin-trained OR-trained EMT’s did better w/ LMA insertion than manniquin-trained crews All rated subjectively & objectively better than OA/BVM Combitube rated best for ventilation + preference by EMT’s but worst for ventilation when assessed by EP

u u u LMA best for ventilation in OR-trained group Aimilar rates of aspiration (1. 14 – 2. 05%) 4/57 autopsies had aspiration: 3 in PTLA u 1 in LMA u u No differences in survival-to-discharge No differences in On-scene – hospital times LMA has highest training costs but lowest operating costs and operational cost / life saved $417 vs $1650. 37 for combitube • Rumball & Mac. Donald. Prehosp Emerg Care. 1997; 1: 1 -10
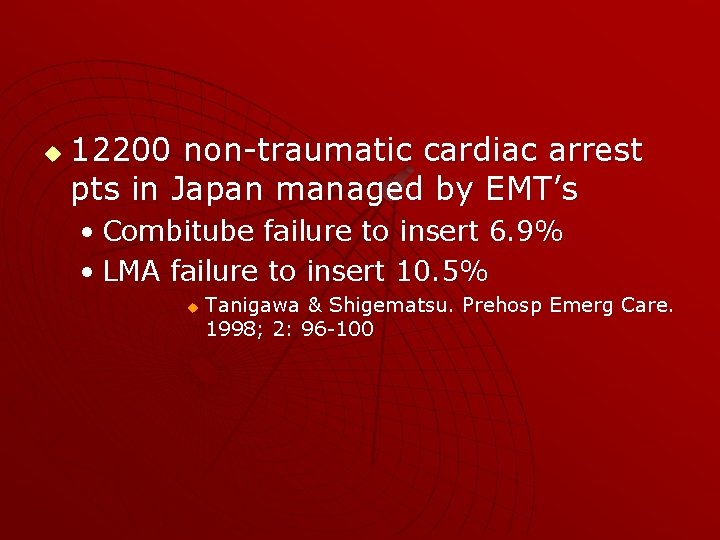
u 12200 non-traumatic cardiac arrest pts in Japan managed by EMT’s • Combitube failure to insert 6. 9% • LMA failure to insert 10. 5% u Tanigawa & Shigematsu. Prehosp Emerg Care. 1998; 2: 96 -100
 Controversies in sport
Controversies in sport Controversies in clinical psychology
Controversies in clinical psychology Activist trade policy
Activist trade policy Controversies in nursing
Controversies in nursing Sports in society issues and controversies
Sports in society issues and controversies Sports controversies
Sports controversies Sports controversies
Sports controversies Level of care primary secondary tertiary
Level of care primary secondary tertiary What is code white hospital
What is code white hospital West suburban er
West suburban er Emergency color codes in hospital
Emergency color codes in hospital Chec hospital
Chec hospital Chec certification
Chec certification Certified hospital emergency coordinator
Certified hospital emergency coordinator Znacznik pre /pre jest stosowany w celu wyświetlenia
Znacznik pre /pre jest stosowany w celu wyświetlenia Pre-hospital communication
Pre-hospital communication Cappagh hospital day ward
Cappagh hospital day ward Picotdc
Picotdc Moritz matern
Moritz matern Sap
Sap Symplicity moritz
Symplicity moritz Moritz wefelscheid
Moritz wefelscheid Franz moritz
Franz moritz Moritz zoppel
Moritz zoppel Witwe bolte sauerkraut
Witwe bolte sauerkraut Sarah moritz fröndenberg
Sarah moritz fröndenberg Moritz haager
Moritz haager Viyanada moritz schlick
Viyanada moritz schlick Moritz plümer
Moritz plümer Moritz zimmermann sap
Moritz zimmermann sap Moritz mueller swinburne
Moritz mueller swinburne Stephan moritz
Stephan moritz Moritz hermann jacobi
Moritz hermann jacobi Moritz zoppel
Moritz zoppel Moritz zoppel
Moritz zoppel Terry moritz
Terry moritz Hospital pharmacy space requirements
Hospital pharmacy space requirements Emergency care system framework
Emergency care system framework The standards of prehospital emergency care
The standards of prehospital emergency care Injuries first aid
Injuries first aid Emergency care enfield
Emergency care enfield Emergency care 13th edition
Emergency care 13th edition Emergency care and disaster preparation chapter 7
Emergency care and disaster preparation chapter 7 Chapter 54 basic emergency care
Chapter 54 basic emergency care Outdoor emergency care 6th edition
Outdoor emergency care 6th edition Care for a victim of an immunologic emergency
Care for a victim of an immunologic emergency Nhs 7 pillars
Nhs 7 pillars Chapter 8 emergency care first aid and disasters
Chapter 8 emergency care first aid and disasters Emergency care and disaster preparation
Emergency care and disaster preparation Prehospital emergency care 11th edition
Prehospital emergency care 11th edition Prehospital emergency care 11th edition study guide
Prehospital emergency care 11th edition study guide Prehospital emergency care 11th edition
Prehospital emergency care 11th edition Golden rules of emergency care
Golden rules of emergency care Introduction to emergency medical care
Introduction to emergency medical care Emergency care harrow
Emergency care harrow Interagency integrated triage tool
Interagency integrated triage tool Prehospital emergency care 11th edition
Prehospital emergency care 11th edition Introduction to emergency medical care
Introduction to emergency medical care Introduction to emergency medical care
Introduction to emergency medical care The goal of modern emergency care includes
The goal of modern emergency care includes Emergency care limmer
Emergency care limmer Introduction to emergency medical care
Introduction to emergency medical care Nursing intervention of cataract
Nursing intervention of cataract Pre post peri
Pre post peri Preoperative patient education ppt
Preoperative patient education ppt Pre operative care
Pre operative care Post operative care of lscs mother ppt
Post operative care of lscs mother ppt Changing trends in hospital care
Changing trends in hospital care Mt auburn primary care center
Mt auburn primary care center Nursing care of sick child
Nursing care of sick child National hospital care survey
National hospital care survey Tuen mun mental health centre
Tuen mun mental health centre National hospital ambulatory medical care survey
National hospital ambulatory medical care survey Doylestown wound center
Doylestown wound center Quantitative and qualitative examples
Quantitative and qualitative examples