Seizures Diagnosis and Management in the Hospital Melody
- Slides: 40
Seizures Diagnosis and Management in the Hospital Melody Calla, PA-C Physician Assistant Department of Neurology North. Shore University Health. System
Objectives �Describe and define different types of seizures. �Identify common causes of seizures �Discuss acute hospital management of seizures
Definitions �Seizure �Caused by abnormal cortical neuronal activity, resulting in sudden and transient alteration of awareness, somatosensory, visual, motor, and/or behavioral changes �A symptom due to an underlying pathology (head trauma, hemorrhage/stroke, metabolic dysfunction, drug exposure, tumor) or other disorder without a clear cause
Definitions �Epilepsy – 2014 International League Against Epilepsy (ILAE) updated definition: �Recurrent unprovoked seizures (two or more unprovoked seizures at least 24 hours apart). �Heightened tendency toward future recurrent unprovoked seizure over the next 10 years (single seizure with abnormal EEG or MRI). Can be associated with prior stroke, CNS infection, traumatic brain injury �Diagnosis of an epilepsy syndrome
Definitions �Status epilepticus �Continuous seizures lasting >5 minutes �At least two discrete seizures occurring without return to baseline in between �May also include persistent seizure activity despite appropriate doses of two anti-epileptic drugs (AED) �Historically, “single epileptic seizure of >30 minutes duration or a series of epileptic seizures during which function is not regained between ictal events in a 30 minute period. ”
Incidence/Epidemiology �The cumulative life time incidence of having at least one seizure is 9%. The cumulative life time incidence of having epilepsy is 3%. �This is because 1/3 of the 9% incidence consists of children with uncomplicated febrile seizures, another 1/3 consists of patients who have only one seizure in the setting of a medical illness. The remaining 1/3 consists of patients who will be diagnosed with epilepsy.
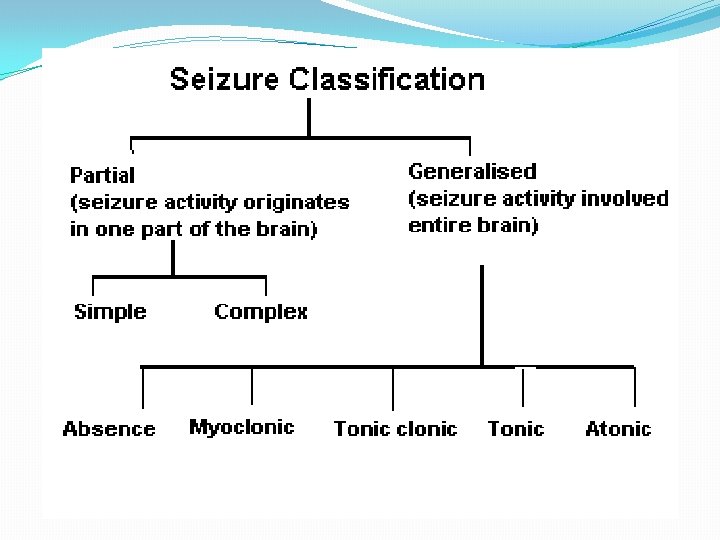
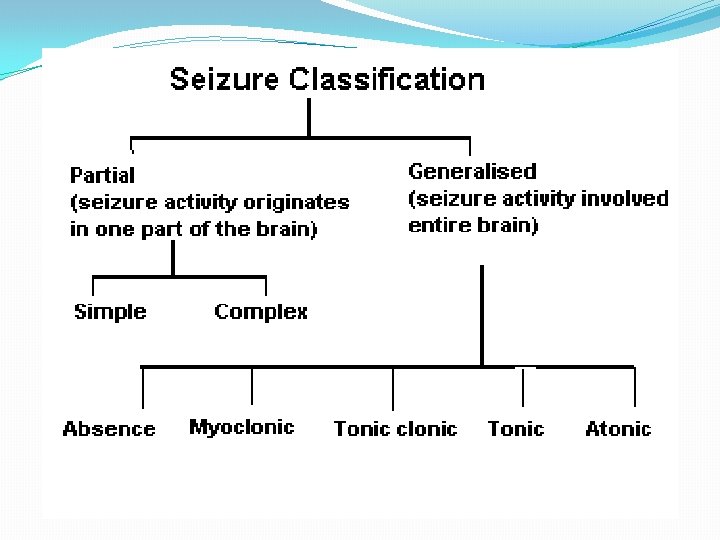
Seizure types �Partial (focal seizures) �Most common seizure type in adults �Caused by abnormal activity originating in a single region of the brain �Simple: no alteration of consciousness �Motor cortex: rhythmic jerking in 1 body part �Temporal lobe aura: epigastric rising, fear, déjà vu �Complex: impaired or alteration of consciousness �Automatisms: lip smacking, fumbling of fingers �Secondary generalized
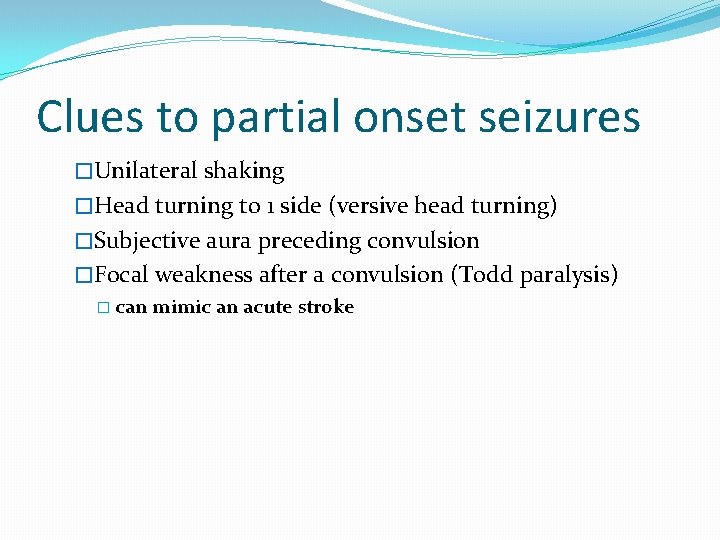
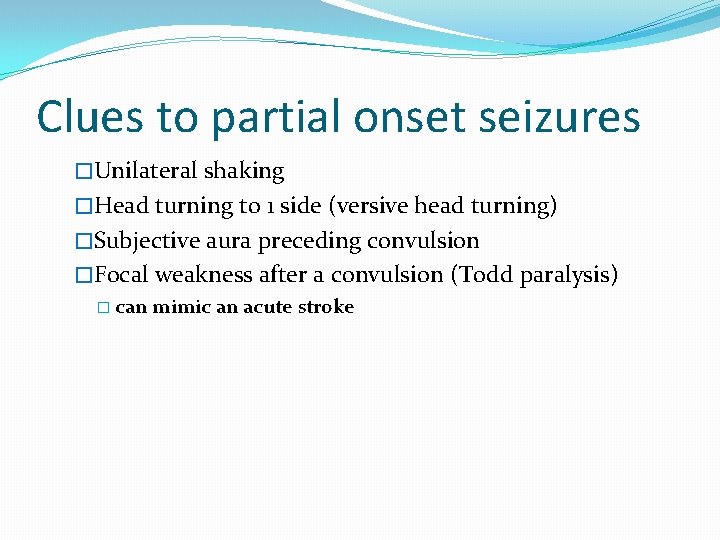
Clues to partial onset seizures �Unilateral shaking �Head turning to 1 side (versive head turning) �Subjective aura preceding convulsion �Focal weakness after a convulsion (Todd paralysis) � can mimic an acute stroke
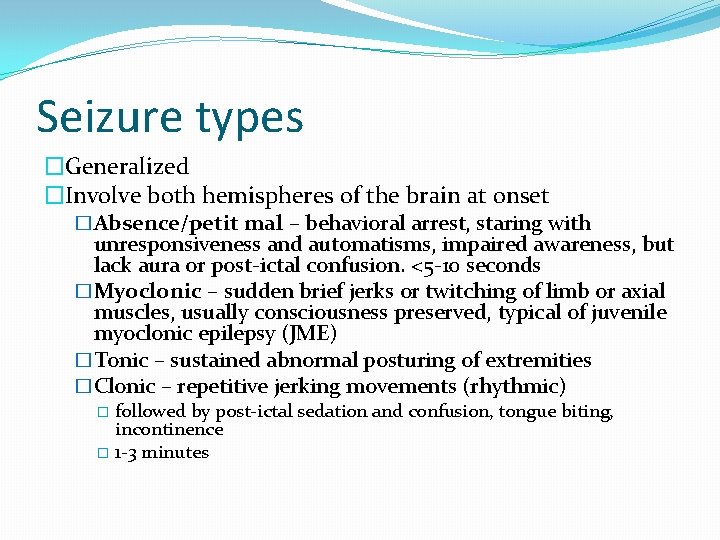
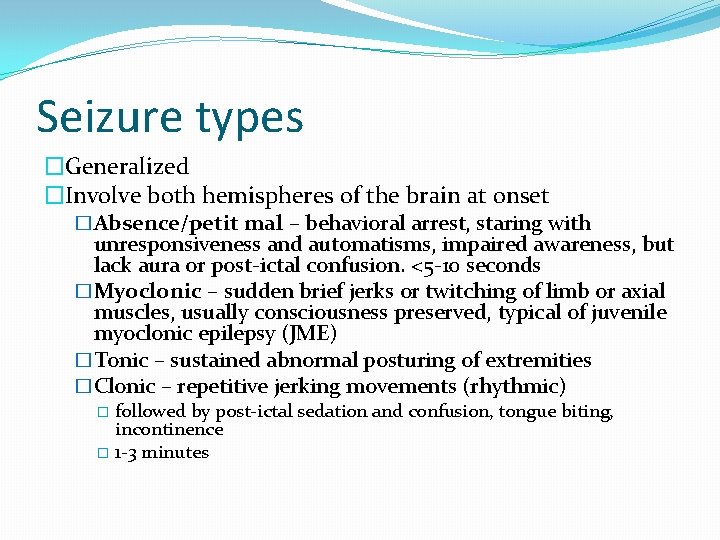
Seizure types �Generalized �Involve both hemispheres of the brain at onset �Absence/petit mal – behavioral arrest, staring with unresponsiveness and automatisms, impaired awareness, but lack aura or post-ictal confusion. <5 -10 seconds �Myoclonic – sudden brief jerks or twitching of limb or axial muscles, usually consciousness preserved, typical of juvenile myoclonic epilepsy (JME) �Tonic – sustained abnormal posturing of extremities �Clonic – repetitive jerking movements (rhythmic) followed by post-ictal sedation and confusion, tongue biting, incontinence � 1 -3 minutes �
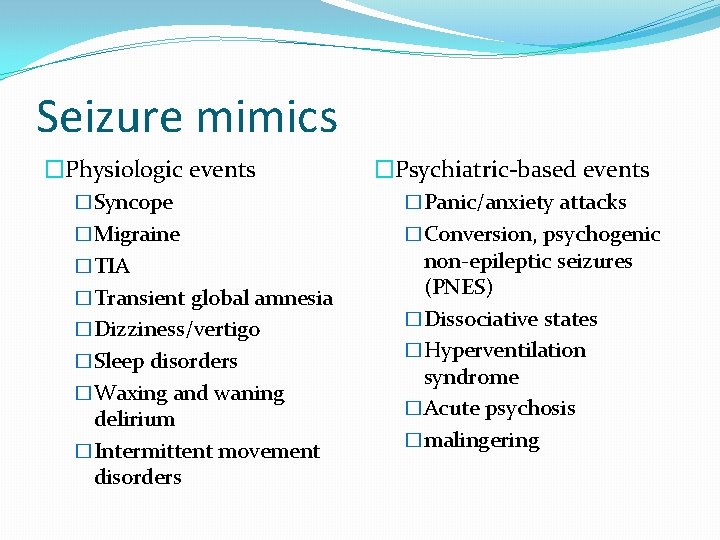
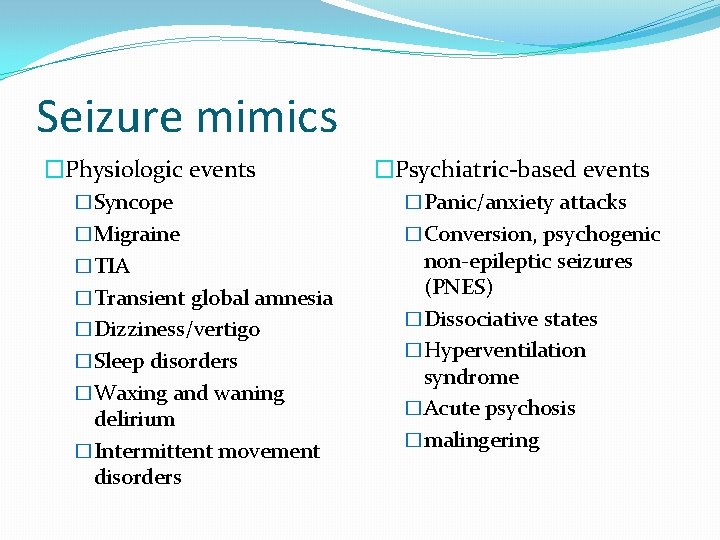
Seizure mimics �Physiologic events �Psychiatric-based events �Syncope �Panic/anxiety attacks �Migraine �Conversion, psychogenic �TIA �Transient global amnesia �Dizziness/vertigo �Sleep disorders �Waxing and waning delirium �Intermittent movement disorders non-epileptic seizures (PNES) �Dissociative states �Hyperventilation syndrome �Acute psychosis �malingering
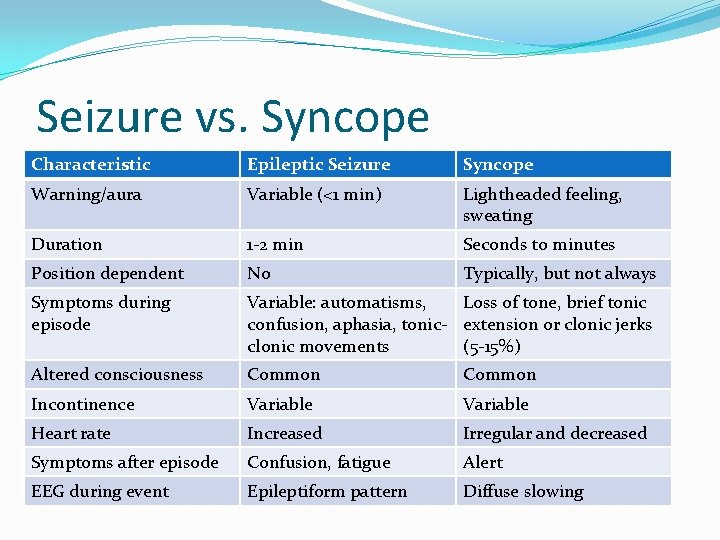
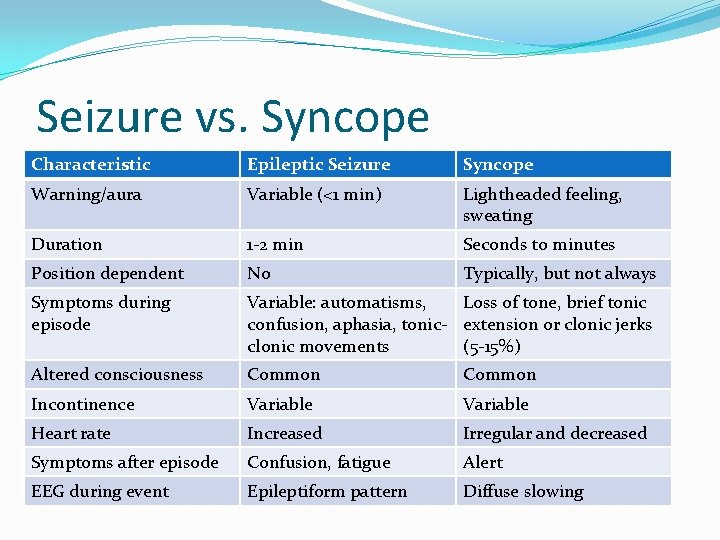
Seizure vs. Syncope Characteristic Epileptic Seizure Syncope Warning/aura Variable (<1 min) Lightheaded feeling, sweating Duration 1 -2 min Seconds to minutes Position dependent No Typically, but not always Symptoms during episode Variable: automatisms, Loss of tone, brief tonic confusion, aphasia, tonic- extension or clonic jerks clonic movements (5 -15%) Altered consciousness Common Incontinence Variable Heart rate Increased Irregular and decreased Symptoms after episode Confusion, fatigue Alert EEG during event Epileptiform pattern Diffuse slowing
Seizure mimics �TIA �Duration �Negative symptoms (weakness, numbness, vision loss, aphasia, etc) �Positive symptoms during a seizure however negative symptoms can occur after
Seizure mimics �Non-epileptic behavioral spells (Psychogenic seizures) �Description of event � Typically eyes are closed � Head nodding or shaking � Pelvic thrusting � Non-rhythmic movements in extremities � Can be different with each event � Tip of tongue biting �Can still have unresponsiveness, post-ictal confusion
Favoring epileptic seizures �Aura �Brief duration (1 -2 min) �Post-ictal confusion �Abnormal posturing �Amnesia for the event �Incontinence �Events arising from sleep �Self-injury (lateral tongue biting) �Eyes open at the event onset
Evaluation �Determine whether the episode of loss of consciousness was a seizure or other event. �History �Prior seizures (including febrile), family history of epilepsy �Head trauma �Cerebrovascular disease, Cardiovascular disease, Diabetes �Cancer �Substance abuse �Intracranial infection �Recent travel, occupation �Congenital brain malformation, cerebral degeneration
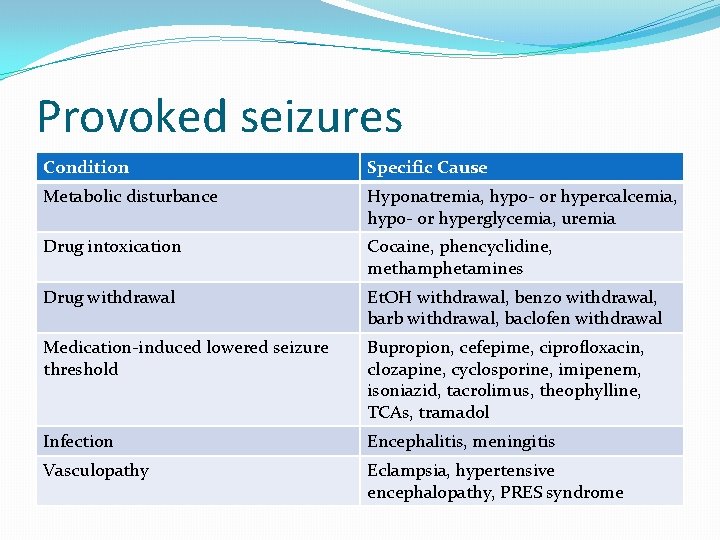
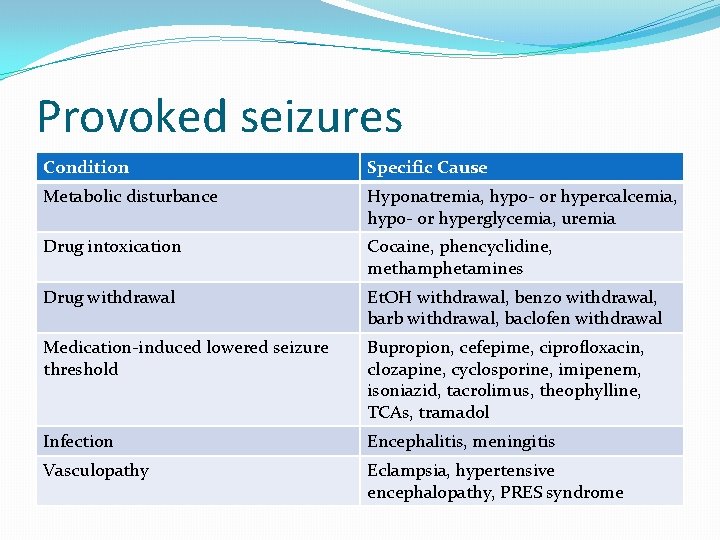
Provoked seizures Condition Specific Cause Metabolic disturbance Hyponatremia, hypo- or hypercalcemia, hypo- or hyperglycemia, uremia Drug intoxication Cocaine, phencyclidine, methamphetamines Drug withdrawal Et. OH withdrawal, benzo withdrawal, barb withdrawal, baclofen withdrawal Medication-induced lowered seizure threshold Bupropion, cefepime, ciprofloxacin, clozapine, cyclosporine, imipenem, isoniazid, tacrolimus, theophylline, TCAs, tramadol Infection Encephalitis, meningitis Vasculopathy Eclampsia, hypertensive encephalopathy, PRES syndrome
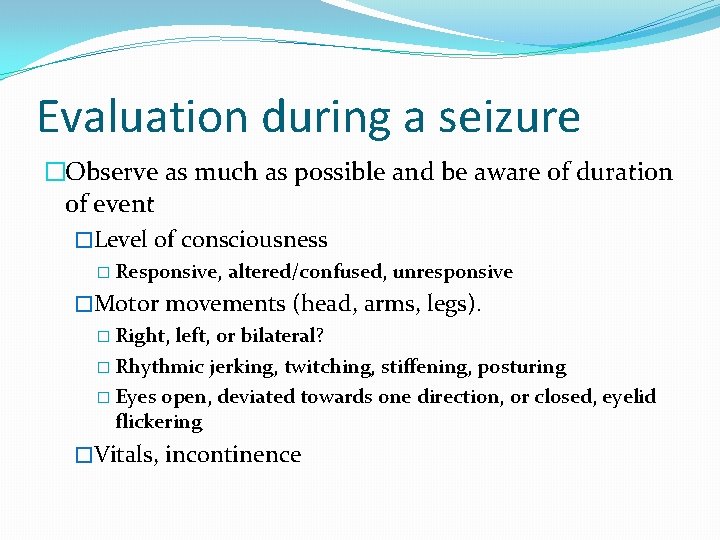
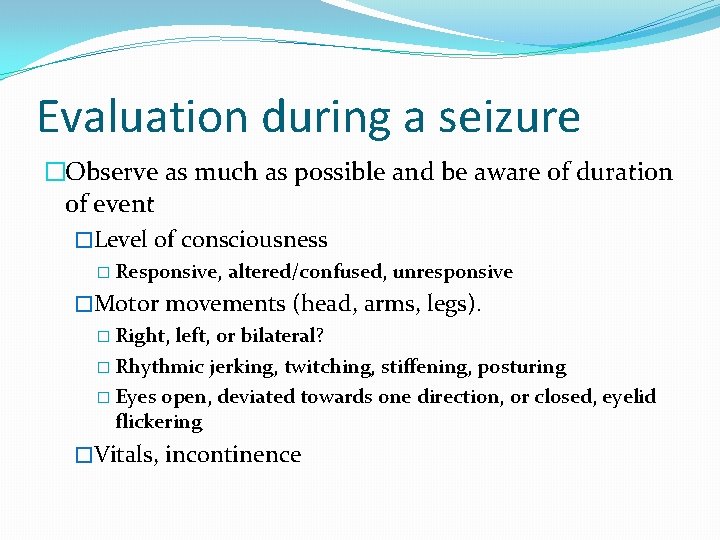
Evaluation during a seizure �Observe as much as possible and be aware of duration of event �Level of consciousness � Responsive, altered/confused, unresponsive �Motor movements (head, arms, legs). � Right, left, or bilateral? � Rhythmic jerking, twitching, stiffening, posturing � Eyes open, deviated towards one direction, or closed, eyelid flickering �Vitals, incontinence
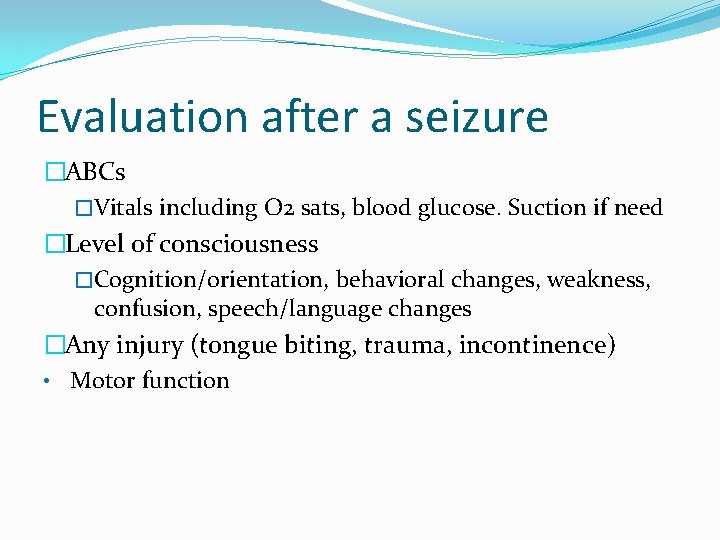
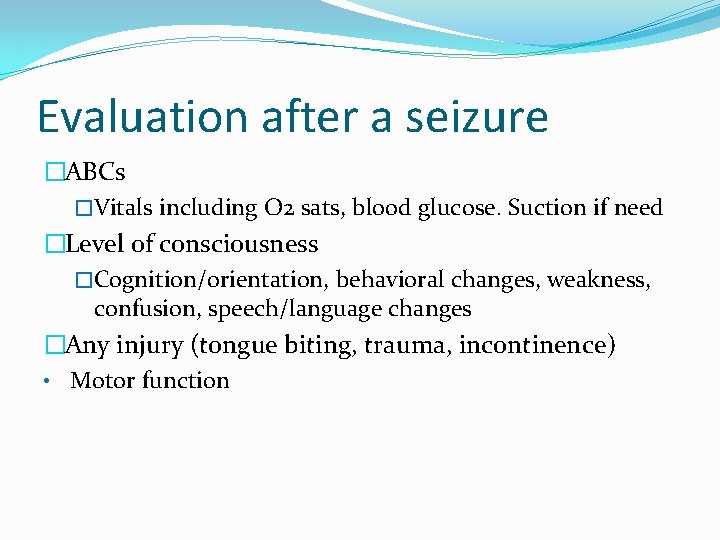
Evaluation after a seizure �ABCs �Vitals including O 2 sats, blood glucose. Suction if need �Level of consciousness �Cognition/orientation, behavioral changes, weakness, confusion, speech/language changes �Any injury (tongue biting, trauma, incontinence) • Motor function
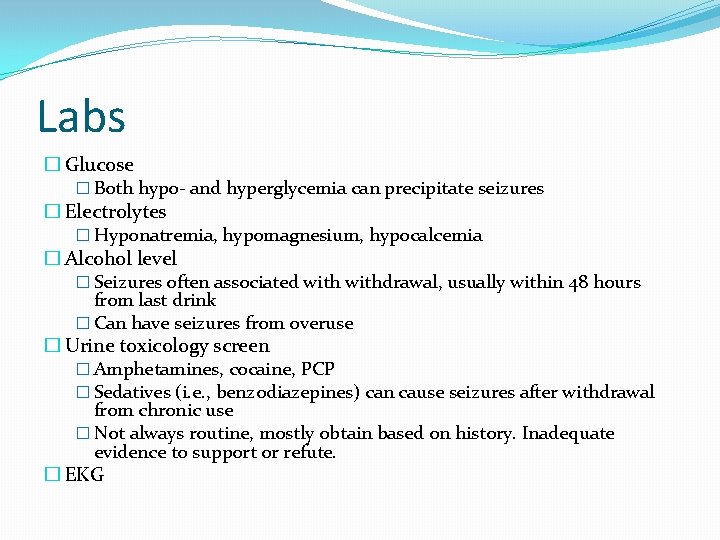
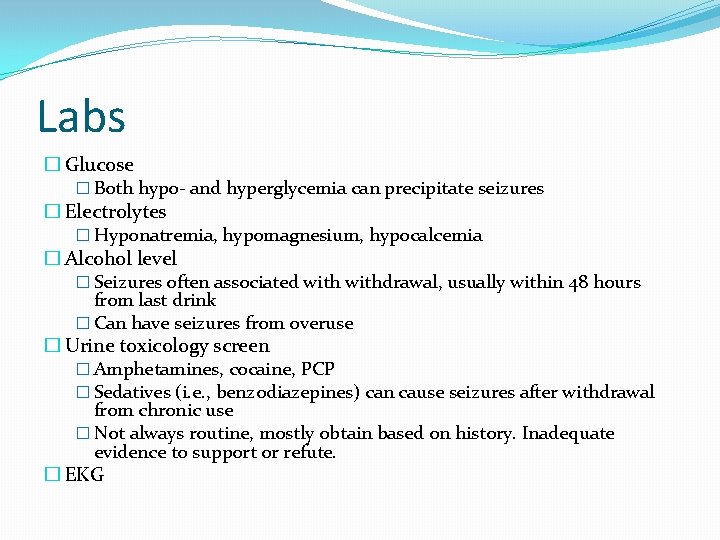
Labs � Glucose � Both hypo- and hyperglycemia can precipitate seizures � Electrolytes � Hyponatremia, hypomagnesium, hypocalcemia � Alcohol level � Seizures often associated withdrawal, usually within 48 hours from last drink � Can have seizures from overuse � Urine toxicology screen � Amphetamines, cocaine, PCP � Sedatives (i. e. , benzodiazepines) can cause seizures after withdrawal from chronic use � Not always routine, mostly obtain based on history. Inadequate evidence to support or refute. � EKG
Labs �Prolactin �Limited role as a diagnostic test for epileptic seizures �May rise shortly after generalized tonic-clonic seizures and sometimes focal seizures �Low sensitivity, so a normal may be seen in a real seizure as well as non-epileptic event
Labs �Lumbar puncture for cerebrospinal fluid (CSF) �Not typically routine unless presentation supports acute infectious process involving central nervous system or cancer history (in which carcinomatous meningitis or leptomeningeal disease is suspected). �A prolonged seizure itself can cause a pleocytosis in CSF making results misleading.
Neuroimaging �In the acute setting, CT head without contrast to evaluate for bleed and/or mass �MRI brain with and without gadolinium is ideal �Tumor, vascular malformation, posttraumatic changes, mesial temporal sclerosis, cortical malformations �Include “seizure protocol” in comment section of the order so thin cuts of temporal lobes can be obtained.
Electroencephalogram (EEG) �If possible, obtain as close as possible to seizure activity �Normal EEG does not exclude presence of a seizure disorder. �helps support the evidence. �May consider treatment with an abnormal EEG (epileptiform discharges) after a single seizure �Presence of epileptiform abnormality does not always indicate seizure disorder �take into context of the patient and current situation �Medication effects, renal failure, or other acute encephalopathy
Electroencephalogram (EEG) �Video EEG �Useful in identifying or classifying the seizure disorder or spell (non-epileptic)
Treatment of seizures �Benzodiazepines �Lorazepam 0. 1 mg/kg IV given at 2 mg/min �longer half life than Diazepam � Side effects - respiratory/cardiovascular depression, somnolence, which can confuse resolution of seizure/post-ictal phase vs persistent seizures.
Selection of AEDs �No single AED is recommended for the initial treatment of epilepsy. �~50% will respond to the 1 st AED �Factors to consider: �Epilepsy syndrome �Age �Sex �Comorbidities �Drug side effects �Cost
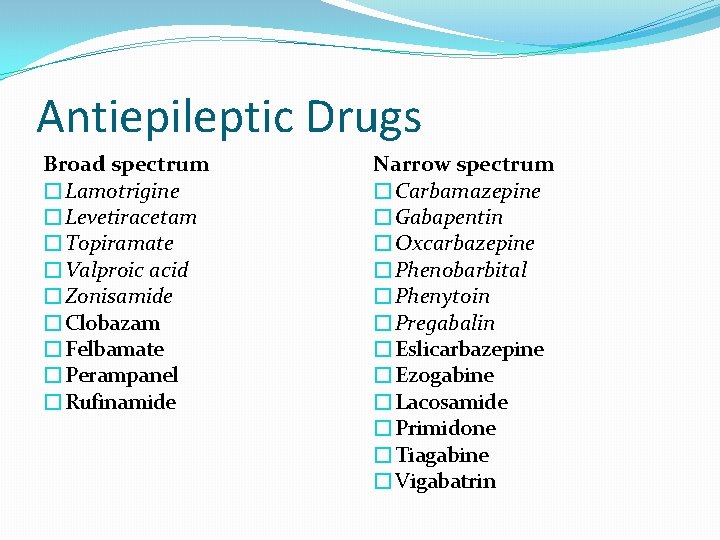
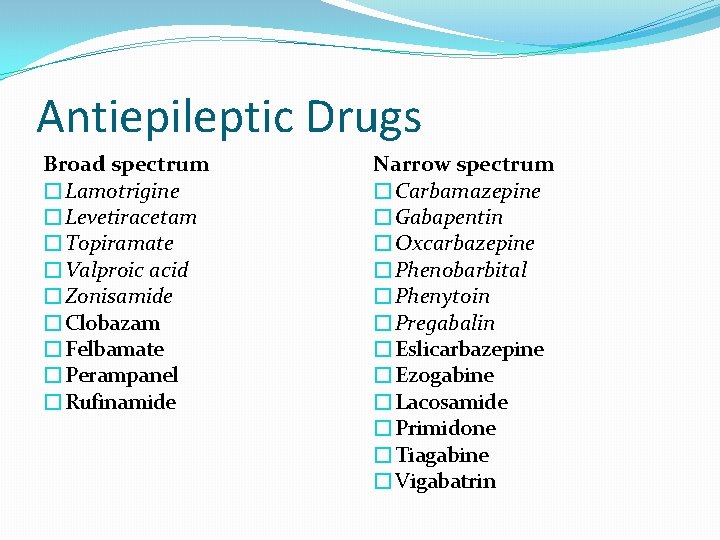
Antiepileptic Drugs Broad spectrum �Lamotrigine �Levetiracetam �Topiramate �Valproic acid �Zonisamide �Clobazam �Felbamate �Perampanel �Rufinamide Narrow spectrum �Carbamazepine �Gabapentin �Oxcarbazepine �Phenobarbital �Phenytoin �Pregabalin �Eslicarbazepine �Ezogabine �Lacosamide �Primidone �Tiagabine �Vigabatrin
Treatment of Seizures �Phenytoin/Fosphenytoin �Fosphenytoin is prodrug to Phenytoin, lacks a diluent that Phenytoin has in its formulation. �At North. Shore, IV Phenytoin not available �Dosing is the same: load 15 -20 mg/kg. �Obtain post-load Dilantin level ~2 hours, helps in maintenance dosing (typically 5 mg/kg/day). �When given IV, maintenance dose every 8 hours due to short half-life �Oral dosing: Phenytoin ER caps (100 mg, 200 mg, 30 mg), chewable 50 mg, suspension �Side effects: hypotension, bradycardia, cardiac arrhythmia , ataxia (toxic), nystagmus, skin rash, gingival hyperplasia, vitamin D deficiency, purple glove syndrome (IV)
Treatment of Seizures �Fosphenytoin/Phenytoin (continued) �Protein binding � Drug levels may need to be adjusted in hypoalbuminemia � Adjusted concentration = measured total concentration divided by [(0. 2 x albumin) + 0. 1]. �Metabolism – CYP 450 family � Enhance anticoagulant effects of Vitamin K antagonists (Warfarin). Conversely, vitamin K antagonists increase serum concentration of Phenytoin � Decrease serum concentration of Valproic Acid (Depakote)
Treatment of seizures �Levetiracetam (Keppra) �Loading dose: 1000 -2000 mg IV �Maintenance dose: starts at 500 mg twice a day �Maximum 3000 mg daily total. Doses beyond can be used but no evidence of additional benefit. �Formulation: 250 mg, 500 mg, 750 mg, 1000 mg tablets, suspension, IV. � Cannot be crushed
Treatment of seizures �Levetiracetam (continued) �Dose adjustment in renal impairment, based on Creatinine Clearance �Dose 500 mg-1000 mg every 24 hours in patients with end-stage renal dialysis requiring hemodialysis (HD) or peritoneal dialysis (PD). �Twice daily dosing in patients receiving continuous renal replacement therapy (CRRT)
Treatment of seizures �Levetiracetam (continued) �Drug level commonly used to monitor compliance and in patients with renal impairment �Side effects: behavioral changes (aggression, anger, anxiety, irritability), fatigue
Treatment of seizures �Valproic Acid (Depakote, Depakene, Depacon) �Loading dose: 15 -20 mg/kg IV �Maintenance dose: 10 -15 mg/kg/day, can be increased by 5 -10 mg/kg/day at weekly intervals (or quicker if needed in hospital setting) �Formulation: Regular, delayed or extended release in 125 mg, 250 mg, 500 mg capsules, tablets, suspension, sprinkles �Metabolism: liver � Not ideal for patients with hepatic impairment �Side effects: tremor, nausea, diarrhea, thrombocytopenia (dose related), weight gain
Treatment of seizures �Phenobarbital �Loading dose: 20 mg/kg IV �Maintenance dose: 1 -5 mg/kg/day, 12 hours after loading dose �Metabolism: liver via CYP system �Side effects: hypotension, respiratory depression, sedation �Half life is ~79 hours, thus obtaining a “therapeutic level” can take several days
Treatment considerations �Enzyme-inducers (Phenytoin, Oxcarbazepine, Phenobarbital) can interact with other liver-metabolized drugs (including BCPs) and can increase risk of osteoporosis and hypercholesterolemia. �Valproic Acid avoid as a 1 st-line drug in women of childbearing age due to risk of congenital and cognitive abnormalities in offspring. �Lamotrigine – consider in women, older patients, depression or other mood disorders �Topiramate and Zonisamide – can be used for both generalized and partial epilepsy; assoc. with weight loss; risk of kidney stones �Levetiracetam and Gabapentin – useful in the elderly since it doesn’t interact with the other medications they may be on.
Brain tumors – primary and metastatic �When presenting with a seizure, use of non-enzyme inducing AED is ideal (Levetiracetam) to avoid potential drug interactions with chemotherapies. �No history of seizure and no plan for neurosurgical procedure: N 0 prophylaxis is recommended. �No history of seizure with neurosurgical resection: short duration of perioperative prophylaxis is recommended as long as patient remains seizure free.
Driving �https: //www. epilepsy. com/driving-laws �In IL, physicians are not required to report patients with epilepsy to the state �However, physicians may report when patients act against medical advice �There is no set seizure-free period prior to resumption of driving � 6 months is a common time frame � Other variables may be associated alteration of awareness. Simple partial seizures may have shorter time frame (3 months) � Patients should be aware of the responsibility should an accident occur during the restrictive period
When to Treat � 2 or more unprovoked seizures �After a single seizure with ≥ 1 risk factors: �>65 yrs old �History of significant head trauma �partial seizure �Post-ictal Todd paralysis �focal finding on EEG or brain �If both MRI and EEG are normal after a single unprovoked seizure, 2 yr recurrence risk ~30 -40% �Early treatment is justified in those for whom any seizure recurrence would have significant consequences related to driving, working, and general safety.
Conclusions �Seizures is a common neurologic condition presenting to the Emergency Department �Recognition of specific clinical characteristics and risk factors help to differentiate between seizure and other neurologic disorders. �Prompt evaluation of a seizure event and treatment helps improve patient outcomes.