Seizure Disorder o Distubance in the electrical activity

Seizure Disorder o Distubance in the electrical activity of the brain o Recurrent seizures is epilepsy
EPILEPSY DEFINITION o Is recurrent (2 or more) unprovoked seizures o Transient provoked seizures caused by fever electrolyte imbalance toxic exposure head injury Are not classified as epilepsy
Status epilepticus o Continuous seizures >30 minutes , generalized or focal , during which the patient remains unconscious or has 2 or more sequential seizures without full recovery of consciousness between seizures.
Etiology o 70% Unknown cause o 30% are due to the following: n n n Head trauma Poisoning Infection Maternal injury Brain tumor and CVA
Classification of epilepsy o 3 classifications o 1 - accordind to semiology : generalized partial : simple , complex o 2 -according to cause : idiopathic sypmtomatic cryptogenic 3 -according to clinical + EEG + age : syndromic classification
PARTIAL SEIZURES ( one half of the body ) o a. Simple partial (no impairment of consciousness) - motor/sensory/autonomic/psychic o b. Complex partial (impairment of consciousness) - simple evolving to complex - complex from outset o c. Partial seizures evolving to secondary GTCS ( generalized tonic clonic seziure)
GENERALIZED SEIZURES The first clinical and EEG changes indicate involvement of both cerebral hemispheres. o a. Absence ( less than 30 sec , just staring ) o b. Myoclonic o c. Clonic (jerking) o d. Tonic o e. Tonic-clonic o f. Atonic ( )ﻻﺯﻡ ﻳﻮﻗﻊ • Female 4 -8 y • Stare /not talk • Eyes roll up • Seconds • Eeg : generalized diffuse spiky waves • Ethusuxamide + valproic acid
Generalized convulsive (grand mal) or generalized tonic-clonic o sudden, immediate loss of consciousness o o o without warning initial generalized tonic contraction and posture (causing fall and epileptic cry) then, generalized, bisynchronous rhythmic forceful jerking movements slowing of the frequency of the convulsive movements Typically last 1 -3 minutes post-ictal exhaustion, sleep, disorientation
West syndrome o Infantile spasm o Described>150 yr ago o Triad of: - Infantile spasm - Arrest psychomotor development Developmental delay - Hypsarrythmia EEG term (by eeg) high amplitude irregular waves or spikes. ﺍﻧﺴﻰ ﻳﻌﻨﻲ ﺍﺫﺍ ﻣﺎ ﻋﻨﺪﻩ ﻣﻮﺿﻮﻉ ﺍﻟﻮﻳﺴﺖ ﺳﻨﺪﺭﻭﻡ
West synd cont Occure in clusters , not jerking , time: on getting sleep or on wake up (transitions from sleep to wakefulness) Type pf seizures : Infantil spasm o Spasm : flexor extensor mixed o Onset peak 4 -7 months ﻳﻌﻨﻲ ﺍﺫﺍ ﻛﺎﻥ ﺍﻟﺴﻨﺔ ﺍﻻﻭﻟﻰ ﻧﻮﺭﻣﺎﻝ o Alwayas before 1 yr age 13 ﻭﺑﻠﺸﺖ ﻉ ﺩﻭﺭﻟﻚ ﺗﺸﺨﻴﺺ ﺛﺎﻧﻲ , ﺷﻬﺮ o Treatment : Or Prednisone - ACTH - VIGABATRIN
EVALUATION o Detailed history o Physical examination o EEG o Labs o Imaging technique
HISTORY o Carefull detailed history corner stone for accurate diagnosis o Video tape the event diagnostic o Ask parents to mimic the event o Physician may mimic different seizure type to find a match with the child event
Phisical examination o Anthroprometric parameteres measured and plotted o Vital signs fever---hypothermia Bl. P bradicardia alt concious ICP o Meningeal signs neck stiffiness meningencephalities subarachnoide hemorrage cerebellar herniation
Physical exam cont o Examination of skull shape fontanelle size tension sututre prem closure wide separation
Physical examination cont o Ophthalmic examination ﻣﻬﻢ ﺻﻮﺭ lisch nodule retinitis pigmentosa cherry red spots ( retinal artery occlusion)
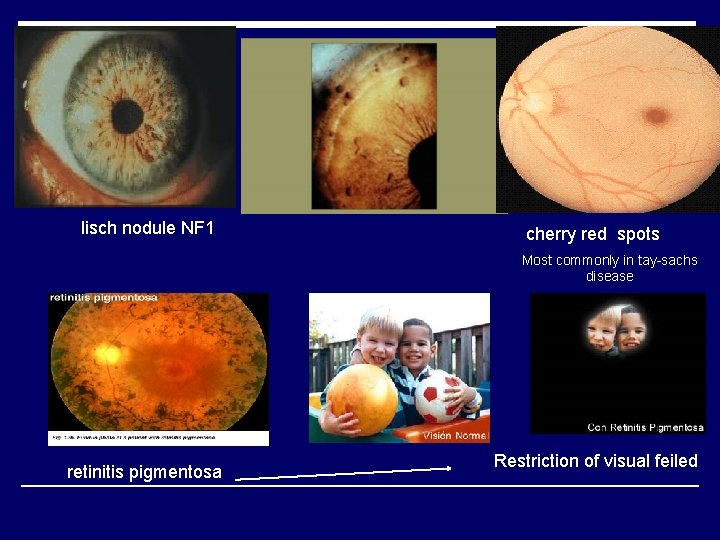
lisch nodule NF 1 cherry red spots Most commonly in tay-sachs disease retinitis pigmentosa Restriction of visual feiled
Physical examination o Abdominal examination organomegaly storage disease o Hyperventilation test For absence seizures
Physical examination cont Skin examination ash leaf spots ( hypopigmentation) facial angioma café au lait spot

Sturge weber syndrome Port wine stain(capillary angioma) in the periorbital area (affect the ophthalmic divistion of trigeminal nerve) they have ipsilateral calcification of blood vessels of brain : Intractable complex partial seizure , mental retardation Diadnosed by brain CT (calcification) Angiofibroma , appear in the second decade (after 10 year old) , in tuberus scelerosis Hypopigment ed , ash leaf , tubrus sclerosis café au lait Spot NF
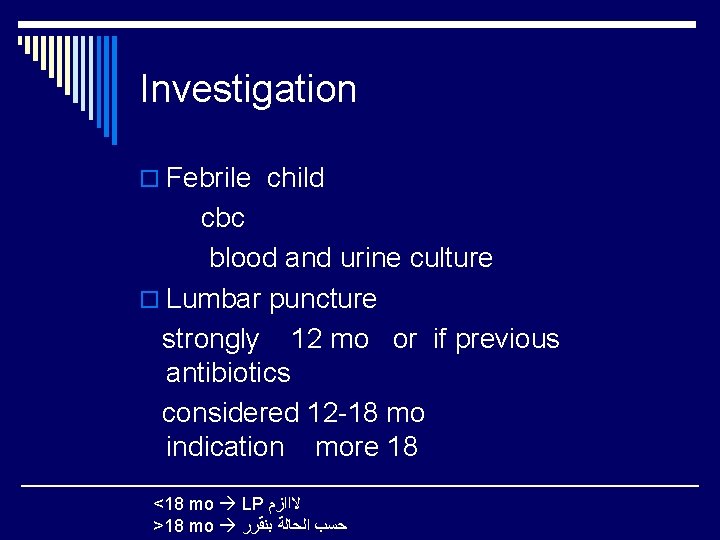
Investigation o Febrile child cbc blood and urine culture o Lumbar puncture strongly 12 mo or if previous antibiotics considered 12 -18 mo indication more 18 <18 mo LP ﻻﺍﺍﺯﻡ >18 mo ﺣﺴﺐ ﺍﻟﺤﺎﻟﺔ ﺑﻨﻘﺮﺭ
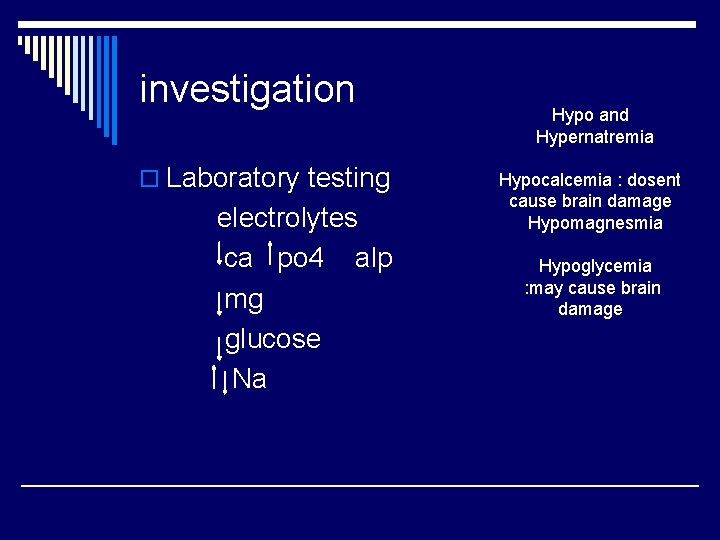
investigation o Laboratory testing electrolytes ca po 4 alp mg glucose Na Hypo and Hypernatremia Hypocalcemia : dosent cause brain damage Hypomagnesmia Hypoglycemia : may cause brain damage
electroencephalogaphy o EEG 56% abnormal in newly dx epileptics repeat additional 11% 20% of epileptics repeatedly normal EEG 5% of normal children epileptiformeactivity
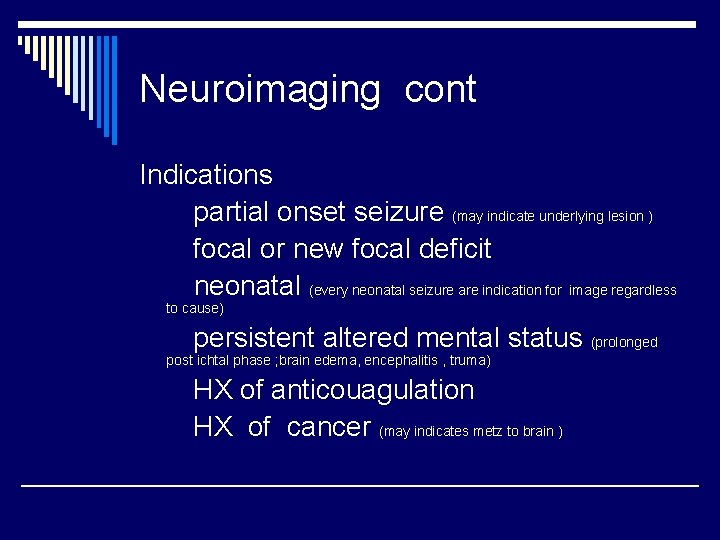
Neuroimaging cont Indications partial onset seizure (may indicate underlying lesion ) focal or new focal deficit neonatal (every neonatal seizure are indication for image regardless to cause) persistent altered mental status (prolonged post ichtal phase ; brain edema, encephalitis , truma) HX of anticouagulation HX of cancer (may indicates metz to brain )
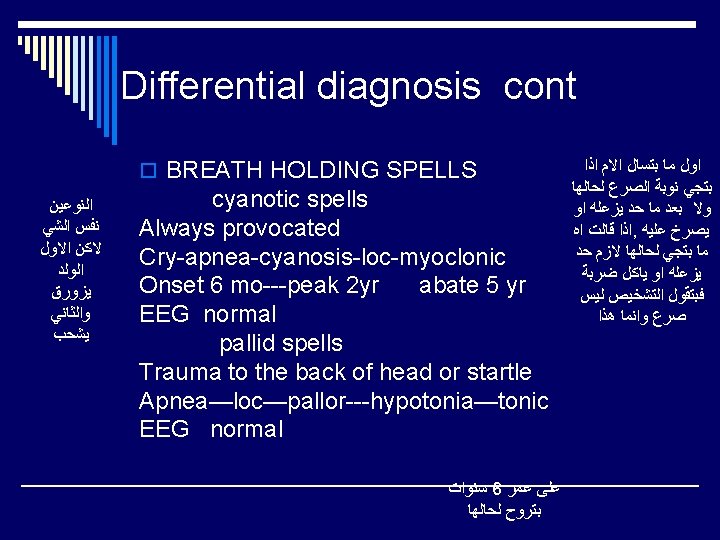
Differential diagnosis cnt SYNCOPE Decrease blood flow----hypotension Loss of conciousness—deviation of eyes Provoked by pain fear excitement Rare before 10 -12 years More in females
Differential diagnosis cont o Prolonged Q-T syndrome sudden LOC during exercise or emotional orstressfull experience Onset late childhood or adolescence during event recover or die
Prognostic factores o Good outcome o Single seizure type ( rate/ short) o No additional impairment o Late age of onset o Episode is related to illness with full recovery or was provoked o Short seizures o Low rate of seizures o Good response to AEDs
Prognostic factor o o o o Adverse outcome Multiple seizure type Additional neurological impairment especially in cognitive function Early age of onset Spontaneous seizures Status epilepticus High rate of seizures Poor response to AEDs
Treatment o Medication o Vagus Nerve stimulator o Surgical o Dietary
Emergency treatment for seizures o Tonic-Clonic (Grand Mal) n Remain calm and protect the patient from injury n Cushion head n Loosen tight neckwear n Turn on side n Remove objects from mouth if possible without injuring the oral cavity n As seizure ends, orient the patient and offer help

Medication

DRUGS NAME YEAR • • Zonisamide Leveteracetam Tagabine Topiramate Lamotrigine Felbamate Gabapentin Vigabatrin - 2000 1999 1998 1996 1994 1993 1992 • • • Valproic Acid Carbamazepine Ethosuximide Primidone Phenytoin Phenobarbitone - 1973 1965 1950 1938 1912
Phenobarbitone (Luminal) • Used for all types and all ages. • Nowadays also used for treatment of neonatal seizures, and status epilepticus • Side effects: • 1)In children Hyperactivity, cognitive impairment. • 2)In adults • Sedation
Phenytoin (Epanuten) • Broad spectrum • The drug of choice in Status epilepticus • Follows Zero-order pharmacokinetics • Side effects: • 1)May reach toxic levels • 2)Hirsutism • 3)Coarse features • 4)Hypertrophic gums • 5)Nystagmus ( dose) • 6)Ataxia ( dose) • 7)Coma ( dose)
Ethusoximide (Zarontin) • Narrow spectrum • The drug of choice in Absence epilepsy • Side effects: • 1) Skin rash • 2)Agranulocytosis ﻳﻌﻨﻲ ﻣﺎ ﺑﺰﺑﻂ ﺗﻌﻄﻴﻪ ﻻﻱ ﻧﻮﻉ ﺛﺎﻧﻲ ﻏﻴﺮ ﺍﻻﺑﺴﻨﺲ ﺳﻴﺠﺮ
Carbamazipine (Tegretol) • The drug of choice in Partial seizures, also used in complex seizures, and secondary generalization. • Also used in treatment of trigeminal neuralgia. • Side effects: • 1) Skin rash • 2) Agranulocytosis • 3) Hyponatremia Contraindicated for pregnant
Valproic acid (Depakine) • Broad spectrum • A component in all antiepileptic regimens. • When given with Lamotrigine, the dose should be lowered to (1/10 th) of the usual dose, since Valproic acid increases the half life of Lamotrigine. • Side effects: 1)Hepatotoxic 2)Transient hair loss 3)Weight gain Contraindicated for pregnant

Vigabatrin (Sabril) • New generation antieplipletic drugs • The drug of choice in West syndrome( which results from tuberculous sclerosis) • Side effects: 1)Visual field defects
Great ﻛﺜﻴﺮ ﻣﻨﻴﻴﻴﺢ Gabapentin (Neurontin) • Broad spectrum • Has no interactions with other drugs • Safe to be used in organ failure( Liver or renal failure) • Used in treatment of neuropathic pain
Gabapentin (Neurontin)

Lamotrigine (Lamictal) • Broad spectrum • Side effects: • 1) Measeles like rash • 2) Stevens Johnson syndrome Similar for valproic acid but doesn’t cause teratogenicty so safe in pregnancy (the only one can be givin in pregnancy)
Topiramate (Topamax) Small doses ﻭ ﺑﺰﻳﺪﻫﺎ ﺷﻮﻱ • Broad spectrum • Used for intractable partial complex seizures especially in combination with tegretol • Also used in prophylaxis of migraine • Side effects: • 1)Renal stones • 2)Decreases attention and ability to concentrate
Levetiracetam (Keppra) • Used for children and neonate age group • Used as an adjuvant, not used as a primary drug.
Treatment Choice of AEDs type of seizures type of syndrome EEG pattern
Treatment o AEDs should be effective few side effect cost effective
Treatment o Primary generalized ﻛﻞ ﺍﻷﻨﻮﺍﻉ valproic acid phenytoin phenobarbitone lamotigine topiramate
Treatment o Infantile spasm steroids vigabatrin benzodiazepine lamotrigine topiramate
Treatment o Partial seizures carbamazepine lamotrigine valproic acid topiramate vigabatrin gabapentin
Treatment ABSENCE EPILEPSY ethosuxamide valproic acid lamotrigine topiramate clobazam
Treatment o MOST OF AEDs start small dose then increase if max dose reached no response serum level routine drug level discouraged o MONOTHERAPY avoide interaction better compliance o BEFORE switching to another drug reconsider DX
Treatment SIDE EFFECT o Most are idiosyncratic o Skin rash o Steven johonson syndrome o Hepatotoxicity o pancreatitis
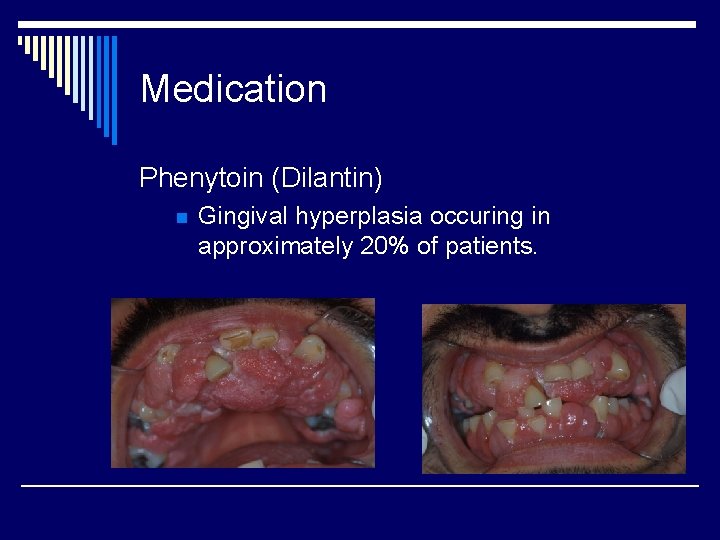
Medication Phenytoin (Dilantin) n Gingival hyperplasia occuring in approximately 20% of patients.

Steven johonson syndrome : more than 3 mucus membranes
Guidelines for discontinuation AEDs o seizure free 2 -5 years on AEDs mean 3. 5 years o single type of partial generalized seizures o normal neurological and IQ examination o EEG normalized with treatment Dose end should be tapered
Vagus Nerve Stimulator intractable partial seizures o Limited for localization related epilepsy o Implanted device o Stimulates the left vagus nerve for 30 seconds every five minutes o 30% experiences 50% reduction in seizure activity
Surgical o First surgery in 1886 o Only utilized when medication cannot achieve satisfactory control
TREATMENT OF EPILEPSY SURGERY INDICATIONS: intractable partial seizures intractable hemiepilepsy Mesial temporal sclerosis best outcome from surgery ﺍﺣﺴﻦ ﻭﺣﺪﻩ ﺑﺘﺘﺠﺎﻭﺏ ﻣﻊ ﺍﻟﺠﺮﺍﺣﺔ
Acid blood thought to be stabilzer for neurons Dietary Ketogenic diet (Metabolic shift-Ketosis state) n n High fat and oils High calorie Low in proteins Low in carbohydrates

o. THANK YOU
- Slides: 61