Seize the Moment Promotion of Lean Principles in






- Slides: 21

Seize the Moment: Promotion of Lean Principles in Moving from Paper to Electronic Provider Documentation at an Academic Medical Center Kai Xu, M. D. John D. Mc. Greevey III, M. D. Joel Betesh, M. D. University of Pennsylvania Health System
Disclosure No relevant relationships with commercial interests to disclose. 2 AMIA 2018 Clinical Informatics Conference
Learning Objectives After participating in this session the learner should be better able to: • Appreciate the opportunity to change documentation practices through EHR adoption • Understand the advantages of APSO formatted notes • Recognize the delicate balance between giving providers structure vs freedom 3 AMIA 2018 Clinical Informatics Conference
Problem • Penn Medicine had historically relied on paper charts for inpatient documentation until 2017 • Challenges with paper charts include: • Inability to access provider notes when not physically at the patient’s location • Lack of standardization in note formatting and content • Illegibility of handwriting • Fully electronic health record (EHR) in outpatient practices for over 10 years • New hospitals with different EHRs joining the health system 4 AMIA 2018 Clinical Informatics Conference
Opportunity • Migrate to a single EHR (Penn. Chart) for both inpatient and outpatient practices across the health system • Learn from ambulatory experience • Highly variable documentation practices • Bloated notes • Outdated content • Develop documentation templates that are consistent with best practices guidelines to improve standardization, quality, and readability 5 AMIA 2018 Clinical Informatics Conference
Lean Principles • Limit number of default inpatient note templates to standardize the look and feel of a note and for ease of maintenance • • Note types • Initial H&P notes • Consult notes • Progress notes Departments • Medicine, Surgery, Obstetrics, Pediatrics, Neonatal, PM&R and Psychiatry • Change to Assessment, Plan, Subjective, Objective (APSO) format for progress notes to improve readability • Discourage automatic insertion of data elements available elsewhere in EHR • Use collapsible headers to hide automated data elements 6 AMIA 2018 Clinical Informatics Conference
Implementation • Inpatient Penn. Chart went live at the Hospital of the University of Pennsylvania on March 4, 2017 • Over 2, 000 attending physicians, 1, 000 trainees, 250 advanced practice providers attended a four hour training class and a personalization lab • Training abbreviated from vendor recommendation as most providers have received training for outpatient EHR 7 AMIA 2018 Clinical Informatics Conference
Chart Audit • Charts were reviewed 12 days post go-live • Six busiest inpatient medical services were selected • Surgical services were excluded as there was high patient turnover and daily attending documentation was not the norm • All signed provider notes within 24 hours of the audit were reviewed for adherence to the core template and APSO format for progress notes 8 AMIA 2018 Clinical Informatics Conference
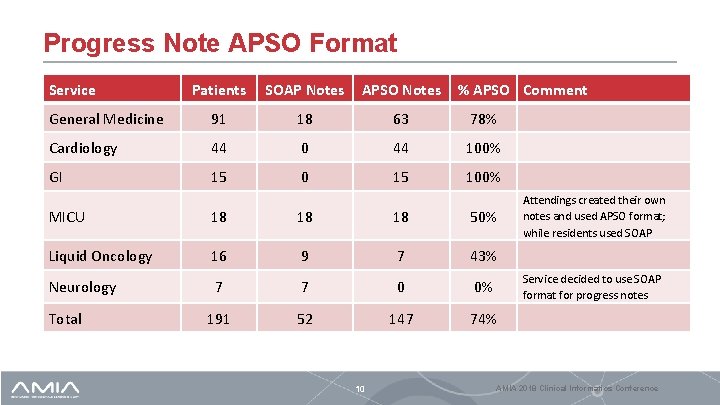
Results • 191 patient charts were included from the 6 selected services • 225 provider notes were reviewed • All 26 H&Ps and consult notes were generated using the prescribed format • Progress notes showed more variability 9 AMIA 2018 Clinical Informatics Conference
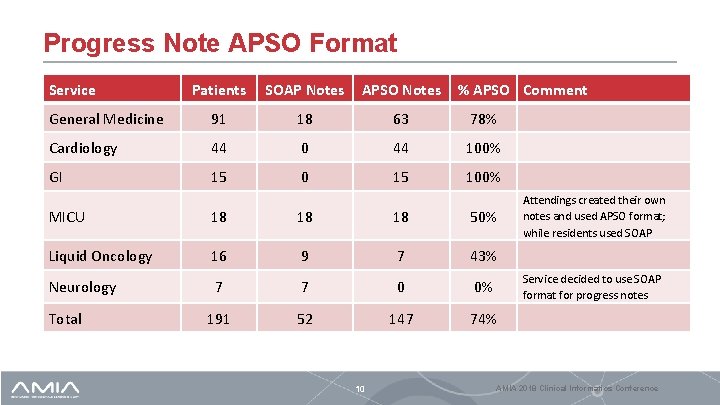
Progress Note APSO Format Service Patients SOAP Notes APSO Notes % APSO Comment General Medicine 91 18 63 78% Cardiology 44 0 44 100% GI 15 0 15 100% MICU 18 18 18 50% Liquid Oncology 16 9 7 43% Neurology 7 7 0 0% 191 52 147 74% Total 10 Attendings created their own notes and used APSO format; while residents used SOAP Service decided to use SOAP format for progress notes AMIA 2018 Clinical Informatics Conference
One Year Later • Chart audited again 1 year after Penn. Chart implementation • Same six services were selected • All provider progress notes completed over a 24 hour period were reviewed for adherence to the core template and APSO format • Attending attestations were reviewed format • When an attending creates a progress note in addition to a housestaff or advanced practitioner note, it is treated as an attestation 11 AMIA 2018 Clinical Informatics Conference

Progress Note APSO Format 1 Year Later Service Patients Progress Notes Attending Attestations APSO SOAP % APSO General Medicine 102 96 23 81% 27 35 44% Cardiology 83 79 10 89% 43 26 62% GI 18 17 1 94% 0 9 0% MICU 22 15 4 79% 18 0 100% Liquid Oncology 42 23 24 49% 0 33 0% Neurology 31 1 43 2% 0 12 0% Total 298 231 105 69% 88 115 43% 12 AMIA 2018 Clinical Informatics Conference
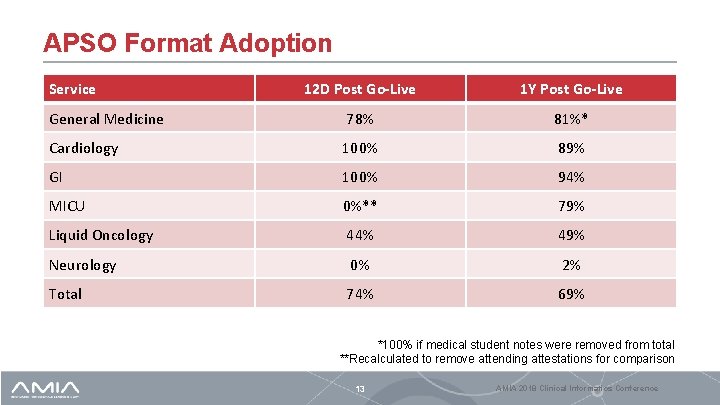
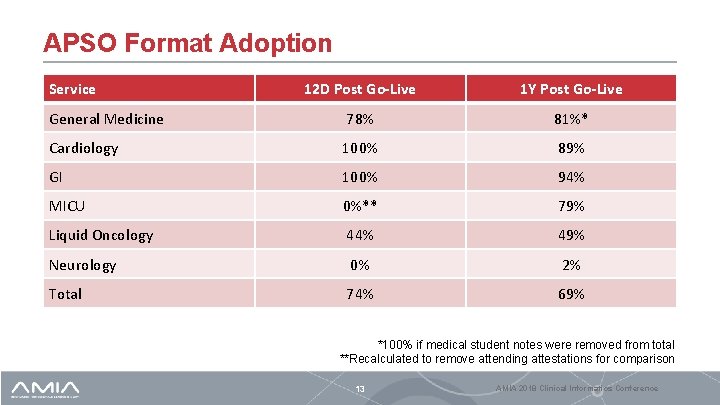
APSO Format Adoption Service 12 D Post Go-Live 1 Y Post Go-Live General Medicine 78% 81%* Cardiology 100% 89% GI 100% 94% MICU 0%** 79% Liquid Oncology 44% 49% Neurology 0% 2% Total 74% 69% *100% if medical student notes were removed from total **Recalculated to remove attending attestations for comparison 13 AMIA 2018 Clinical Informatics Conference
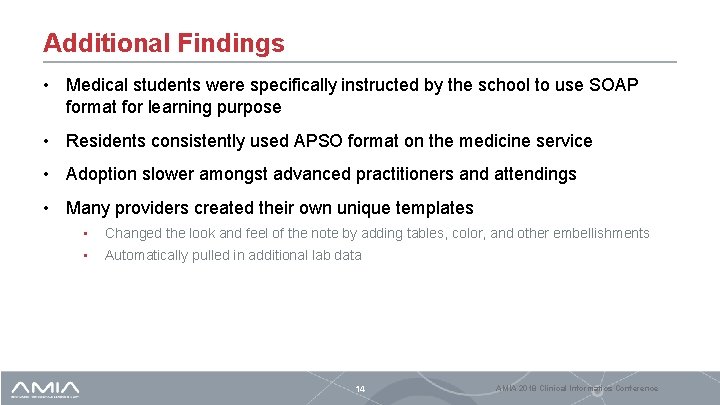
Additional Findings • Medical students were specifically instructed by the school to use SOAP format for learning purpose • Residents consistently used APSO format on the medicine service • Adoption slower amongst advanced practitioners and attendings • Many providers created their own unique templates • Changed the look and feel of the note by adding tables, color, and other embellishments • Automatically pulled in additional lab data 14 AMIA 2018 Clinical Informatics Conference
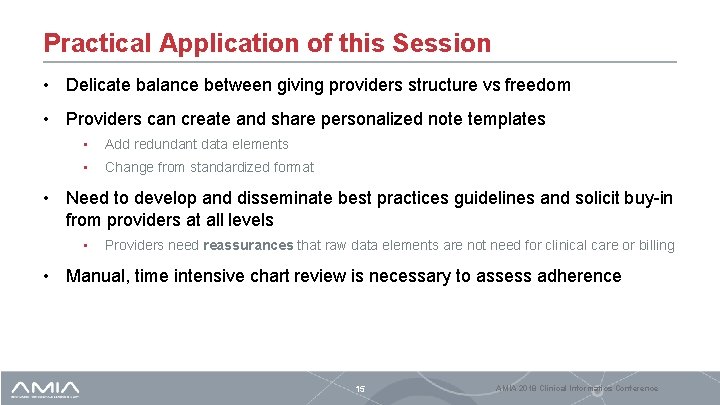
Practical Application of this Session • Delicate balance between giving providers structure vs freedom • Providers can create and share personalized note templates • Add redundant data elements • Change from standardized format • Need to develop and disseminate best practices guidelines and solicit buy-in from providers at all levels • Providers need reassurances that raw data elements are not need for clinical care or billing • Manual, time intensive chart review is necessary to assess adherence 15 AMIA 2018 Clinical Informatics Conference
Question An advantage of the APSO (Assessment, Plan, Subjective, Objective) note over a SOAP (Subjective, Objective, Assessment, Plan) note in the EHR is: A. Supported by extensive high quality literature B. Easier for the reader of the note to find the key elements of decision making of the note author C. Protects against notes being bloated with info pulled in from elsewhere in the record D. APSO has been used more than SOAP over the last few decades 16 AMIA 2018 Clinical Informatics Conference

Answer A. Supported by extensive high quality literature B. Easier for the reader of the note to find the key elements of decision making of the note author C. Protects against notes being bloated with info pulled in from elsewhere in the record D. APSO has been used more than SOAP over the last few decades Explanation: Correct answer = B. By putting the assessment and plan at the top of the note, the reader can immediately see thought processes of the note writer without any scrolling. A is not correct. While we did find supportive literature, we did not find extensive literature and it did not include randomized studies. C is not correct since nothing about the APSO format protects against note bloat. D is simply wrong. The dominant form of provider documentation has been in SOAP format 17 AMIA 2018 Clinical Informatics Conference
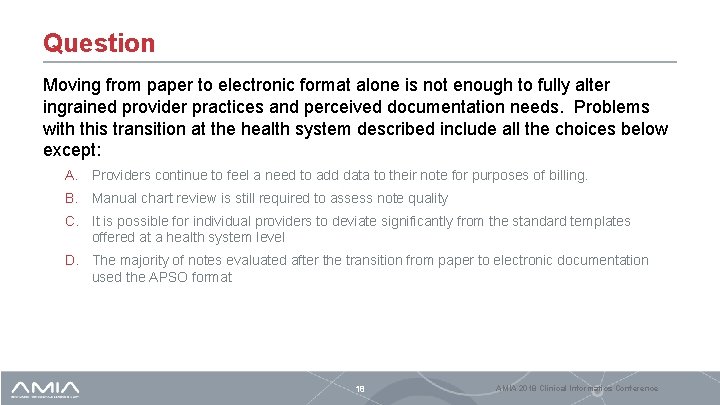
Question Moving from paper to electronic format alone is not enough to fully alter ingrained provider practices and perceived documentation needs. Problems with this transition at the health system described include all the choices below except: A. Providers continue to feel a need to add data to their note for purposes of billing. B. Manual chart review is still required to assess note quality C. It is possible for individual providers to deviate significantly from the standard templates offered at a health system level D. The majority of notes evaluated after the transition from paper to electronic documentation used the APSO format 18 AMIA 2018 Clinical Informatics Conference

Answer A. Providers continue to feel a need to add data to their note for purposes of billing. B. Manual chart review is still required to assess note quality C. It is possible for individual providers to deviate significantly from the standard templates offered at a health system level D. The majority of notes evaluated after the transition from paper to electronic documentation used the APSO format Explanation: This is documented in the table in our paper. Answers A, B and C were all problems we found with our transition to the electronic documentation. 19 AMIA 2018 Clinical Informatics Conference

AMIA is the professional home for more than 5, 400 informatics professionals, representing frontline clinicians, researchers, public health experts and educators who bring meaning to data, manage information and generate new knowledge across the research and healthcare enterprise. AMIA 2018 Clinical Informatics Conference | amia. org @AMIAInformatics @AMIAinformatics Official Group of AMIA @AMIAInformatics #Why. Informatics 20

Thank you! Kai. Xu@uphs. upenn. edu Joel. Betesh@uphs. upenn. edu John. Mc. Greevey@uphs. upenn. edu
 Seize the day poem
Seize the day poem Carpe diem literary definition
Carpe diem literary definition Arena basic process
Arena basic process Food laws and regulations in pakistan pdf
Food laws and regulations in pakistan pdf Why does prince prospero invite a thousand
Why does prince prospero invite a thousand Dans ma chambre il y a in english
Dans ma chambre il y a in english Why were the tyrants able to seize control in athens
Why were the tyrants able to seize control in athens Jit and lean production
Jit and lean production Lean warehousing principles
Lean warehousing principles 5 principles of lean
5 principles of lean Principles of sales promotion
Principles of sales promotion Hình ảnh bộ gõ cơ thể búng tay
Hình ảnh bộ gõ cơ thể búng tay Slidetodoc
Slidetodoc Bổ thể
Bổ thể Tỉ lệ cơ thể trẻ em
Tỉ lệ cơ thể trẻ em Chó sói
Chó sói Chụp phim tư thế worms-breton
Chụp phim tư thế worms-breton Bài hát chúa yêu trần thế alleluia
Bài hát chúa yêu trần thế alleluia Môn thể thao bắt đầu bằng chữ đua
Môn thể thao bắt đầu bằng chữ đua Thế nào là hệ số cao nhất
Thế nào là hệ số cao nhất Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Công của trọng lực
Công của trọng lực