Section 3 Medical Nutrition Therapy Copyright 2003 Delmar
- Slides: 28
Section 3 Medical Nutrition Therapy Copyright © 2003 Delmar Learning, a Thomson Learning company
Chapter 23 Nutritional Care of Clients Copyright © 2003 Delmar Learning, a Thomson Learning company
Objectives § § Chapter 23 Describe how illness and surgery can affect the nutrition of clients Identify and describe three or more nutrition-related health problems that are common among elderly clients needing long-term care Copyright © 2003 Delmar Learning, a Thomson Learning company 3
Objectives § § Chapter 23 Demonstrate correct procedures for feeding a bedridden client Explain the importance of adapting the family’s meal to suit the client’s nutritional requirements Copyright © 2003 Delmar Learning, a Thomson Learning company 4
Nutritional Care Fever, nausea, fear, depression, chemotherapy, and radiation can destroy appetite. Vomiting, diarrhea, chemotherapy, radiation, and some medications can reduce or prevent absorption of nutrients. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 5
Protein Energy Malnutrition When the increased needs for energy and protein are not met by food intake, the body must use its stores of glycogen and fat. Body breaks down its own tissues to provide protein for energy. Protein-energy malnutrition can be a problem among hospitalized clients. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 6
Protein Energy Malnutrition PEM can delay wound healing, contribute to anemia, depress the immune system and increase susceptibility to infections. Symptoms of PEM include weight loss and dry, pale skin. Iatrogenic malnutrition is malnourishment as a result of hospitalization. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 7
Improving the Client’s Nutrition Formal nutritional assessments should be made on a regular basis. All members of the health care team should be alert to signs of malnutrition every day. Listen to client’s concerns and watch reaction to food served. Include dietitian in plan of care. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 8
Feeding the Client In the home, the family menu should serve as the basis of the client’s meal whenever possible. Omit or add certain foods as necessary. Vary the method of preparation if needed. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 9
Serving the Meal When serving food at the bedside, tray should be lined with a pretty cloth or paper liner. Attractive dishes should be used. Food should be arranged attractively. Utensils arranged conveniently. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 10
Serving the Meal Serve water, as well as another beverage. Serve food at proper temperature. Give client the opportunity to use the bedpan and to wash before the meal is served. Client should be in a comfortable position. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 11
Serving the Meal Any unpleasant sights should be removed. Pleasant conversation during preparation can improve the client’s mood. Tray should be placed so that it is easy for the client to feed self. If client needs help, prepare items by opening containers and anticipating needs. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 12
Serving the Meal Client should be given sufficient time to eat. If meal is interrupted, warm food should be re-heated. Help client brush teeth after meal. Document intake per facility policy. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 13
Feeding the Client Sit near the side of the bed. Small amounts of food should be placed toward the back of the mouth with a slight pressure on the tongue with the spoon or fork. Clients should not be fed with a syringe. If paralyzed, food and straw should be placed on nonparalyzed side of the mouth. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 14
Feeding the Client Allow client to help self as much as possible. If client begins to choke, help her or him sit up straight. Do not give food or water while the client is choking. Client’s mouth should be wiped as needed. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 15
Feeding the Client A client diagnosed with dysphagia will require a specialized diet. Depending upon the swallowing abnormality, the client may need pureed foods with either thin or thickened liquids. A dysphagic client should not use straws. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 16
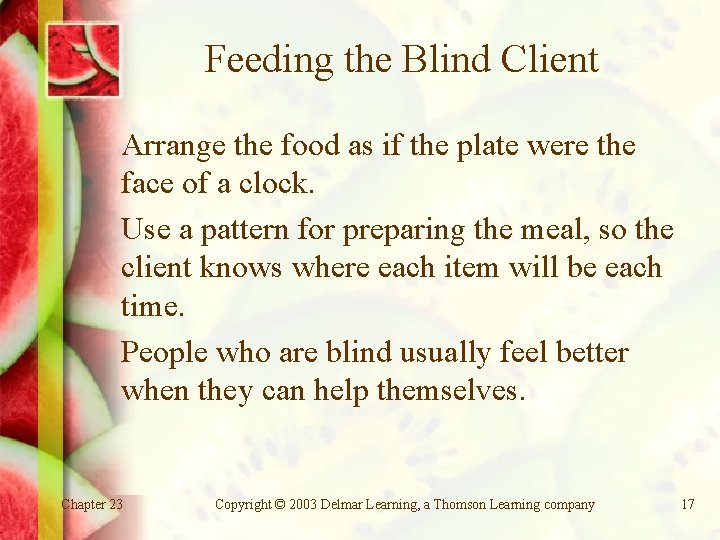
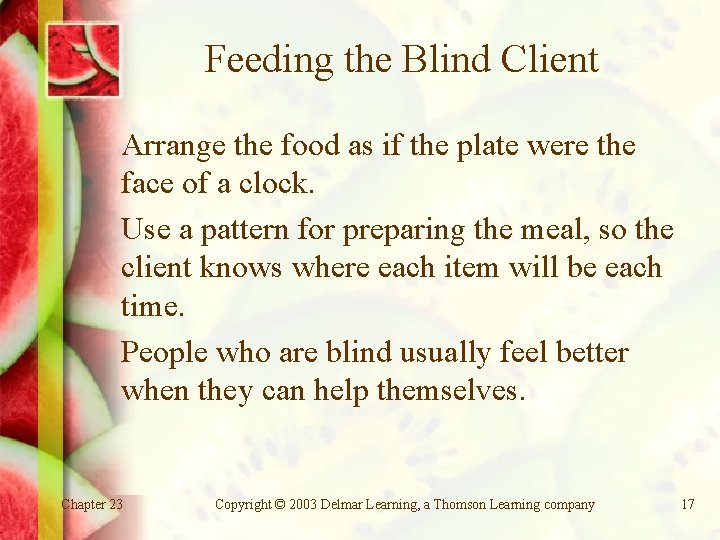
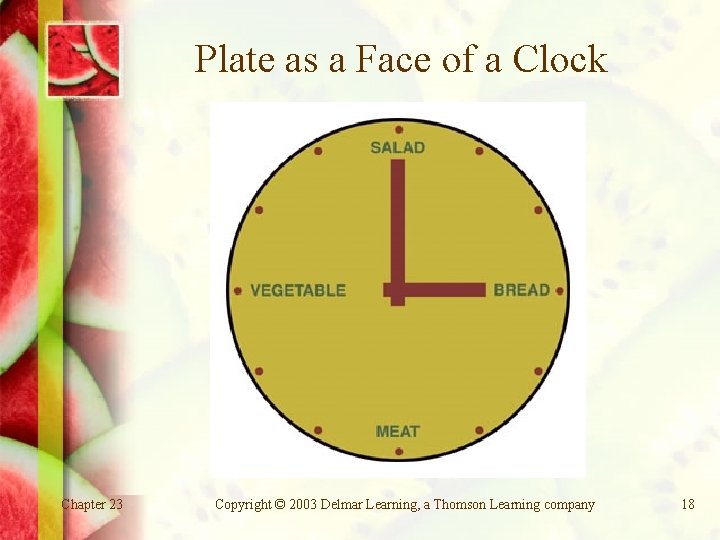
Feeding the Blind Client Arrange the food as if the plate were the face of a clock. Use a pattern for preparing the meal, so the client knows where each item will be each time. People who are blind usually feel better when they can help themselves. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 17
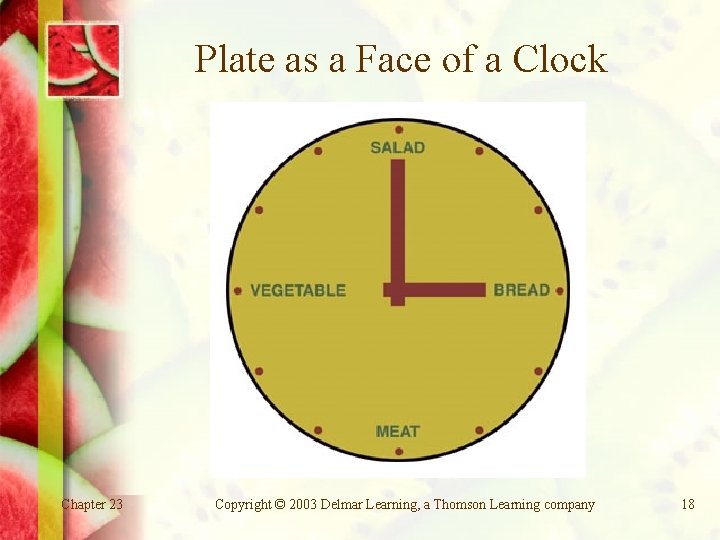
Plate as a Face of a Clock Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 18
Physical Problems of the Institutionalized Elderly Majority of people 85 and over have at least one chronic disease such as arthritis, osteoporosis, diabetes mellitus, cardiovascular disease, mental disorder. These conditions affect their attitudes, physical activities, appetites and, thus, nutritional status. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 19
Physical Problems of the Institutionalized Elderly PEM is a major problem for this population. Anemia can develop and contribute to fatigue, confusion and depression. Sufficient animal protein and vitamin C should be provided in the diet. Pressure ulcers (bedsores) can develop in bedridden clients. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 20
Physical Problems of the Institutionalized Elderly Healing of pressure ulcers requires treatment of the ulcer, relief of the pressure, a high-kcal diet with sufficient protein, vitamin C and zinc supplements. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 21
Physical Problems of the Institutionalized Elderly Constipation can be caused by inadequate fiber, fluid, or exercise. Other causes include medication; reduced peristalsis; or former abuse of laxatives. Treatment includes increasing fluid, fiber, and exercise. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 22
Physical Problems of the Institutionalized Elderly Diarrhea can be caused by lack of muscle tone in the colon. An increase of fiber in the diet combined with supplemental vitamins and minerals may be helpful. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 23
Physical Problems of the Institutionalized Elderly The sense of smell declines with age and the appetite diminishes. Xerostomia (dry mouth) can be caused by disease or medications. Drinking water, eating frequent small meals, and chewing sugar-free gums or candies may be helpful. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 24
Physical Problems of the Institutionalized Elderly Dysphagia (difficulty swallowing) can result from a stroke, closed head trauma, head or neck cancer, surgery, or Alzheimer’s and other diseases. Many dysphagia clients must have thickened liquids. Dysphagia clients should always be in an upright position when eating. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 25
Conclusion Illness and surgery can have devastating effects on client’s nutritional status. PEM can be a significant problem in hospitals. Bedridden client should be given the bedpan and allowed to wash hands before meal. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 26
Conclusion Client should be encouraged to feed self. However, help should be offered and needs anticipated. The client who is blind can eat more easily if food is arranged in a set pattern on the plate. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 27
Conclusion Provide pleasant conversation and atmosphere. Record type of diet, time of meal, client’s appetite, and type and amount of food eaten. Nutrition-related health problems in the elderly can sometimes be relieved with proper treatment. Chapter 23 Copyright © 2003 Delmar Learning, a Thomson Learning company 28