SECOND HEART SOUNDPHYSIOLOGY PATHOPHYSIOLOGY DR PRADEEP SREEKUMAR Key

- Slides: 56
SECOND HEART SOUNDPHYSIOLOGY & PATHOPHYSIOLOGY DR PRADEEP SREEKUMAR
“Key to auscultation of heart”-Leatham 2 components-first designated as aortic and second as Pulmonary Normally splits into 2 components during inspiration and narrows in expiration Respiratory variation first described by Potain (1866)
Physiology Closure of the aortic and pulmonic valves initiates the series of events that produces the second heart sound. The main audible components results from vibrations of the cardiac structures after valve closure.
Genesis of Second. Heart sound • Most accepted theory is by Robert Rushmer. • States that heart sounds are produced by abrupt acceleration and deceleration of blood masses contained by an elastic boundary. • Decelaration of blood columns attended upon by closure of semilunar valve produces second heart sound. • Stein and colleagues modification-Heart sounds are produced by pressure gradients created across closed elastic valves.
The second sound originates from aftervibrations in the cusps and in the walls and blood columns of the great vessels and their respective ventricles. The energy from these oscillations comes from sudden deceleration of retrograde flow of the column of blood in the aorta and pulmonary artery
Softer pulmonic sound is confined to pulmonary area Louder aortic sound is heard all over precordium Splitting of second heart sound is normally confined to second left intercostal space Must be separated by more than 20 msec (0. 20 sec) in order to be differentiated and heard as two distinct sounds.
Determinants of Intensity • Intensity depends on atrio ventricular pressure gradients across closed semilunar valves. • Intracardiac sound intensity produced by a vibrating elastic membrane is related to its rate of deflection. • Amplitude and rate of valve distension would be more related to rate of change of diastolic pressure gradient than to its absolute value.
• d. P/d. T of right heart is much less on right side than left side of heart. • Hence P 2 is significantly softer than A 2. • Depression of LV functon decreases intensity of A 2.
Why is A 2 before P 2 ? Pulmonary arterial pressure is less than aortic pressure (Pulmonary resistance to forward flow from ventricle is less than aortic resistance ie pulmonary impedance is less than aortic impedance. )
As pulmonary impedance is less, even after right ventricular systolic contraction blood continues to flow through valve until pulmonary arterial pressure increases more than right ventricle). As aortic impedance is more , it stops blood flow through the aortic valve before itself.
Hangout interval A measure of impedance in the pulmonary artery system. In the highly compliant (low-resistance, highcapacitance) pulmonary vascular bed, the hangout interval , is a determinant ofduration of right ventricular ejection. Hang out interval may vary from 30 to 120 msec in the pulmonary vascular bed.
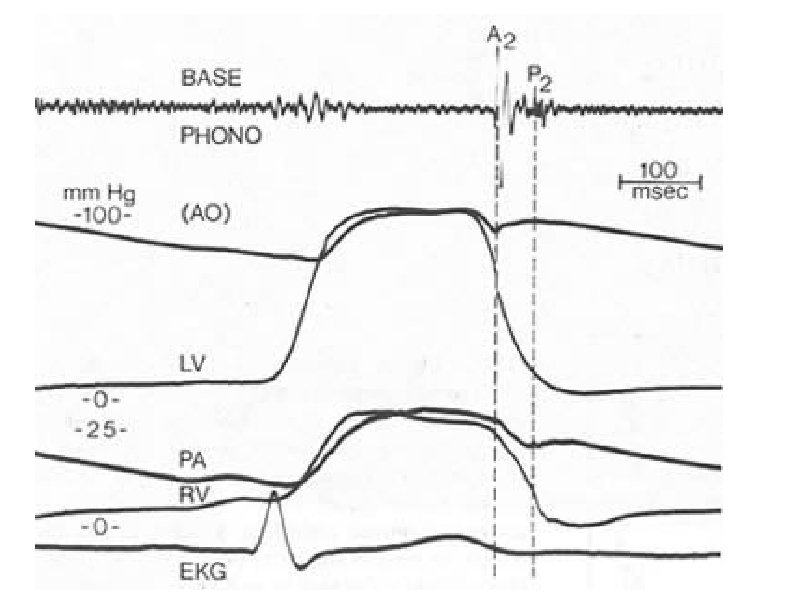
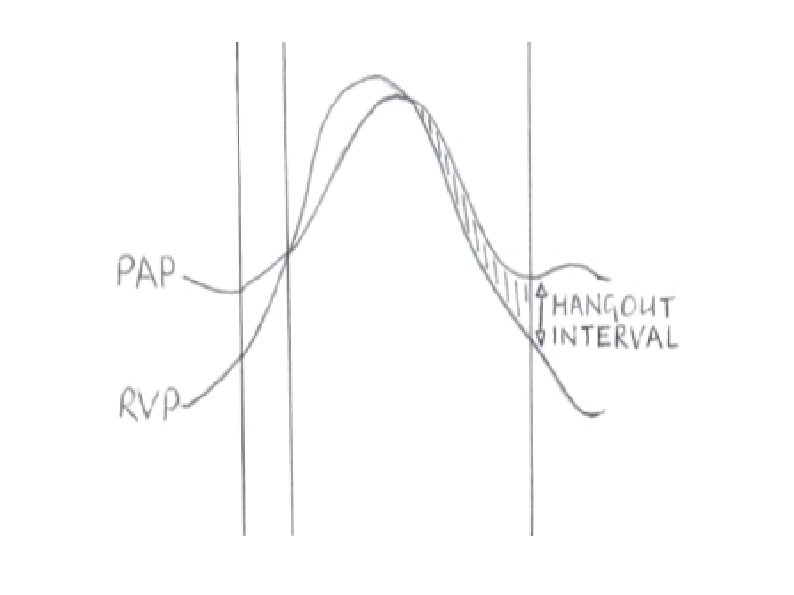
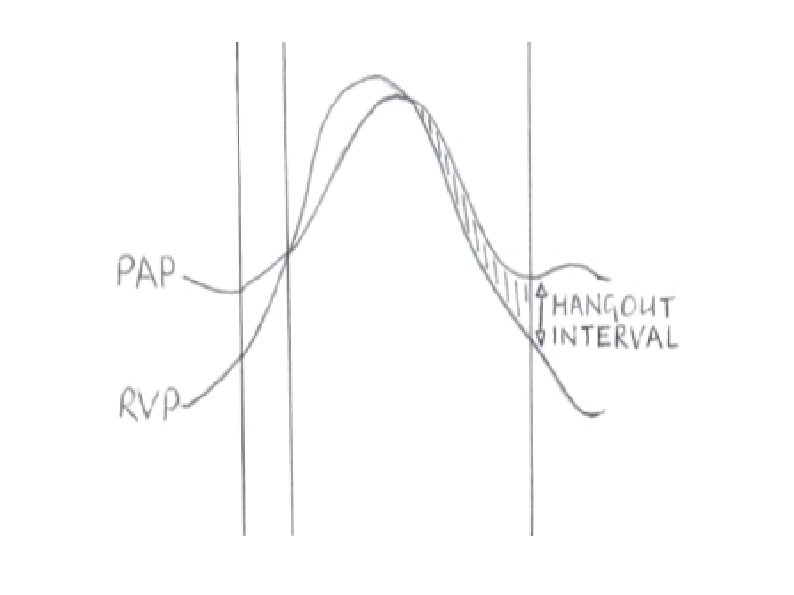
What is hangout interval? • • • Semilunar valve is expected to close at point of cross over of ventricular and arterial pressure. In reality it is not so. Time interval from cross over of pressures to actual occurance of sound is called HANGOUT interval
Why does pulmonary valve remain open even after pressure equilisation? • According to Newton’s first law of motion, “every body continues to move at constant speed unless acted upon by an external force” • In this case, the blood continues to flow from the right ventricle even after the pressure in the right ventricle and the pulmonary artery becomes equal
• Just like a rolling ball is stopped by the friction offered by the ground, the ejection of blood is stopped by the resistance offered by the pulmonary vasculature • Since the pulmonary vascular resistance is low compared to the systemic vascular resistance, it takes some time for the blood flow from the right ventricle to stop • This corresponds to the hangout interval
• In the left side of the heart, because impedance is much greater, the hangout interval between the aorta and left ventricular pressure curves is negligible (less than or equal to 5 msec). • The hangout interval therefore correlates closely with impedance of the vascular bed into which blood is being injected. • Its duration is inversely related to vascular impedance.
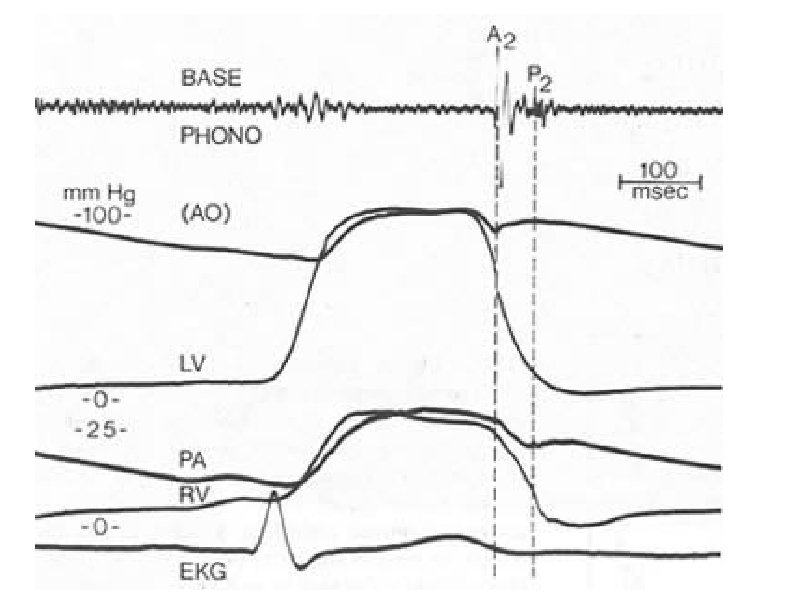
QP 2 interval The interval from the onset of the Q wave of the electrocardiogram to the first high frequency component of the pulmonic closure sound recorded from the external phonocardiogram. Q-A 2 interval An indirect measurement of the total duration of the left ventricular electromechanical systole. The interval from the onset of the Q wave of the electrocardiogram to the first high frequency compnent of the aortic closure sound recorded from the external phonocardiogram
• A 2 P 2 -The duration of splitting of the second heart sound. The difference between the Q-P 2, and the Q-A 2 Q –P 2 -Q-A 2. . • This interval can also be measured directly as the interval between the first high frequency component of the aortic and pulmonary closure sounds as measured from the external phonocardiogramn.
• True approximation of the total duration of right ventricular electromechanical systole is derived by subtractinig the hangout interval from the QP 2, interval. • Hangout interval -The interval separating the pressure cross over from the pulmonary artery incissura
• Hangout interval is lesser on Aortic (30 msec)than Pulmonary side(80 msec) – Higher pressure – Less distensibility Depends on interrelated factors like o pressure beyond the valve o dilatation of the artery o distensibility of arterial system o vascular impedance o phase of respiration.
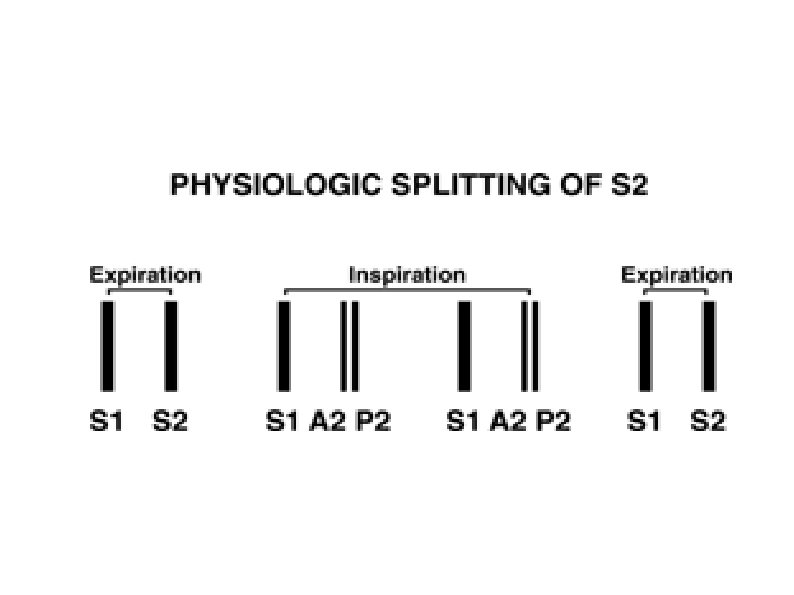
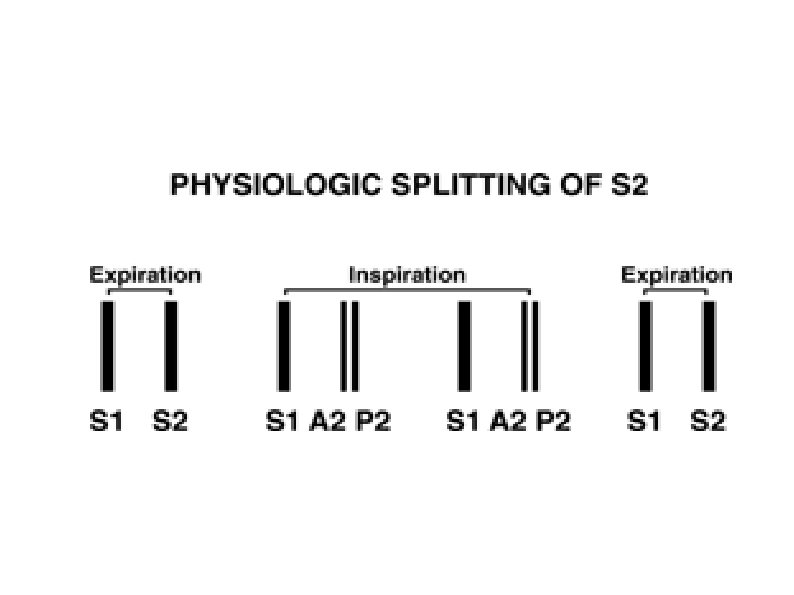
Normal physiological splitting during respiration: Inspiration lowers impedance in the pulmonary circuit Prolongs the hangout interval Delays pulmonic valve closure Audible splitting of A 2 and P 2.
Expiration Decreased hangout interval Pulmonic valve closure is earlier A 2–P 2 interval is separated by less than 30 msec (narrow split) Sounds single to the ear if less than 20 msec
Traditional view Inspiratory drop in intrathoracic pressure Greater venous return to the right ventricle Pooling of blood in the lungs Decreased return to the left ventricle
On expiration, the reverse occurs The increase in right ventricular volume prolonged rightsided ejection time and delayed P 2 Decrease in left ventricular volume reduced left-sided ejection time and caused A 2 to occur earlier.
The delayed P 2 and early A 2 associated with inspiration, is an interplay between changes in the pulmonary vascular impedance and changes in systemic and pulmonary venous return.
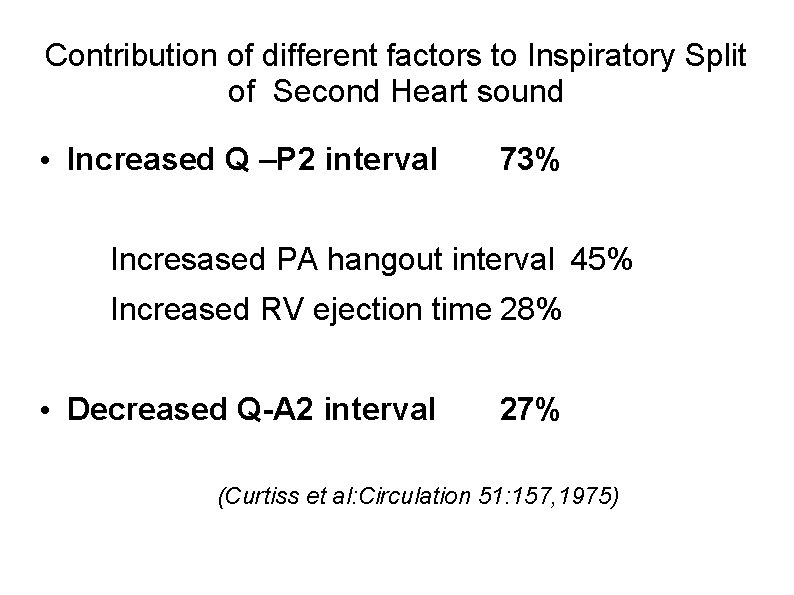
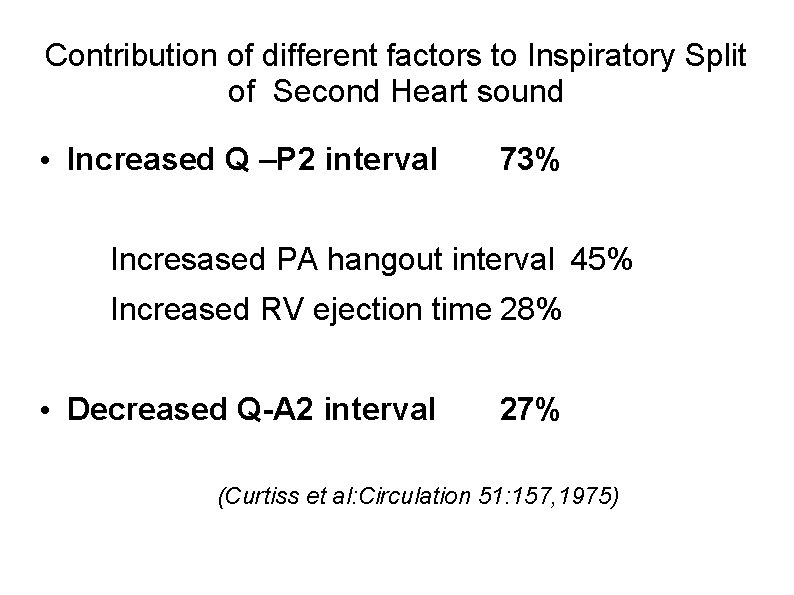
Contribution of different factors to Inspiratory Split of Second Heart sound • Increased Q –P 2 interval 73% Incresased PA hangout interval 45% Increased RV ejection time 28% • Decreased Q-A 2 interval 27% (Curtiss et al: Circulation 51: 157, 1975)
Clinical Significance With quiet respiration, A 2 will normally precede P 2 by 0. 02 to 0. 08 second (mean, 0. 03 to 0. 04 sec) with inspiration. In younger subjects inspiratory splitting averages 0. 04 to 0. 05 second during quiet respiration.
With expiration, A 2 and P 2 may be superimposed and are rarely split as much as 0. 04 second. If the second sound is split by greater than 0. 04 second on expiration, it is usually abnormal.
Presence of audible splitting during expiration (i. e. , the ability to hear two distinct sounds during expiration) is of greater significance at the bedside in identifying underlying cardiac pathology than is the absolute inspiratory increase in the A 2–P 2 interval.
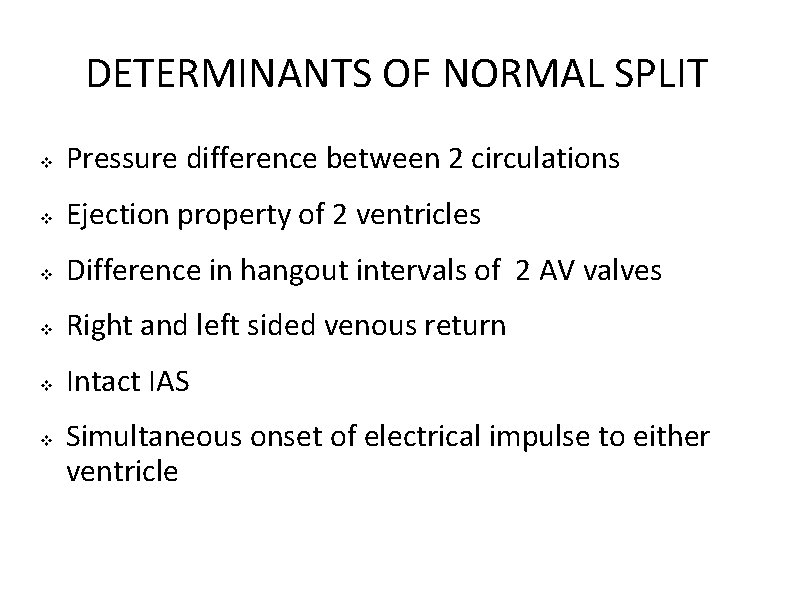
DETERMINANTS OF NORMAL SPLIT Pressure difference between 2 circulations Ejection property of 2 ventricles Difference in hangout intervals of 2 AV valves Right and left sided venous return Intact IAS Simultaneous onset of electrical impulse to either ventricle
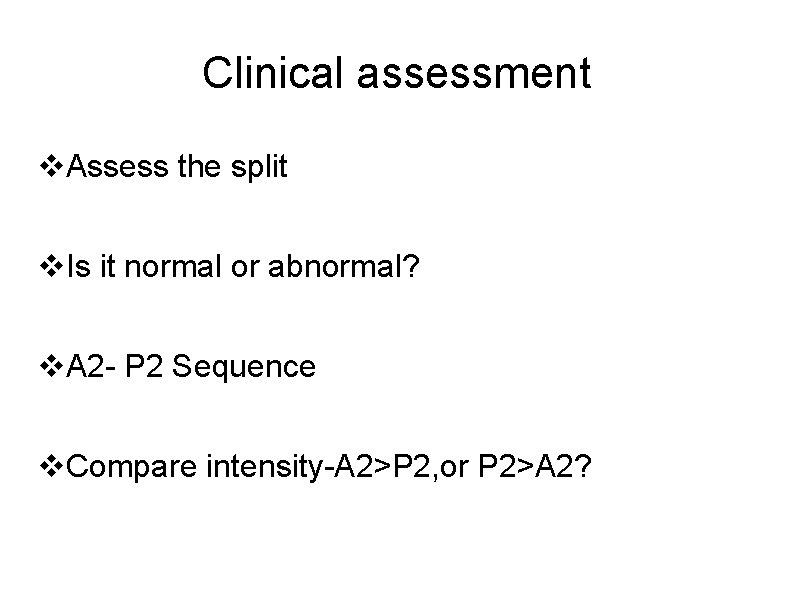
Clinical assessment Assess the split Is it normal or abnormal? A 2 - P 2 Sequence Compare intensity-A 2>P 2, or P 2>A 2?
LOUDNESS/INTENSITY
LOUD A 2 Elevated pressure beyond the valve Systemic hypertension- “tambour “ quality Dilated ascending aorta • • • Aneurysm of ascending aorta Aortic root disease Thickened but mobile aortic leaflets Congenital bicuspid aortic valve
LOUD P 2 • Graham Steell describes p 2 in pulmonary hypertension”…. . extreme accentuation of the pulmonary second sound is always present, the closure of semilunar valves being generally perceptible as to the hand placed over the pulmonary area, as a sharp thud……”
• • • An accentuated P 2 can be transmitted to mid or lower left sternal edge and, when very loud throughout precordium. Splitting can be made out in other areas Decreased AP chest dimensions(loss of thorasic kyphosis) may produce loud P 2 Infants and children, p 2 louder due to higher pulmonary arterial pressures
LOUD P 2 • Pulmonary arterial hypertension – • higher closing pressure of valve, dilated pa Left to right shunts – – increased flow across the valve, increased valve excursion dilated pulmonary artery
Diminished A 2 • Aortic Stenosis • Aortic regurgitation Extensive leaflet distortion Fibrosis of aortic leaflets Calcification of Aortic valve
Diminished Pulmonic sound • – Thick chest wall – Pulmonary stenosis – Dysplastic valve
Absent – tetrology of fallot – transposition of great arteries – truncus arteriosus – pulmonary atresia – absent pulmonary valve
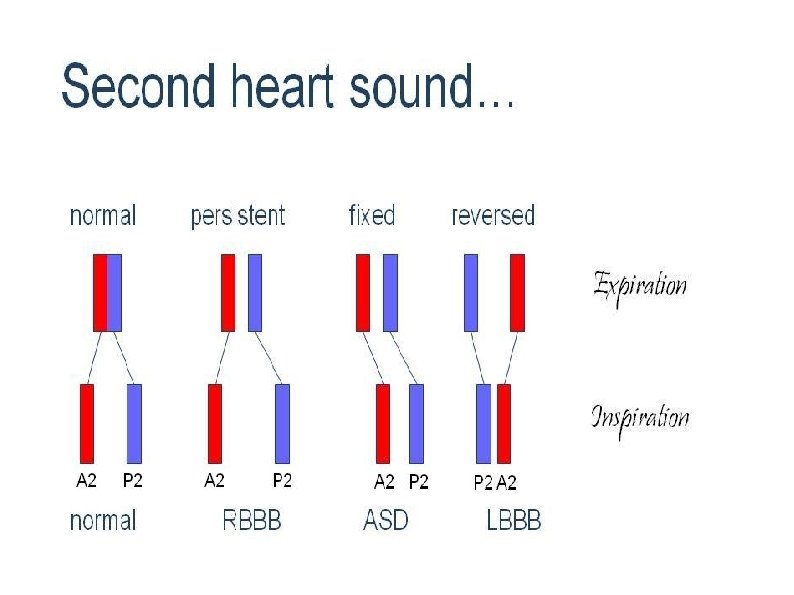
Abnormal splitting of the second heart sound (1) single (2) splitting, with normal respiratory variation (3) splitting without respiratory variation (fixed splitting) (4) reversed (paradoxical) splitting.
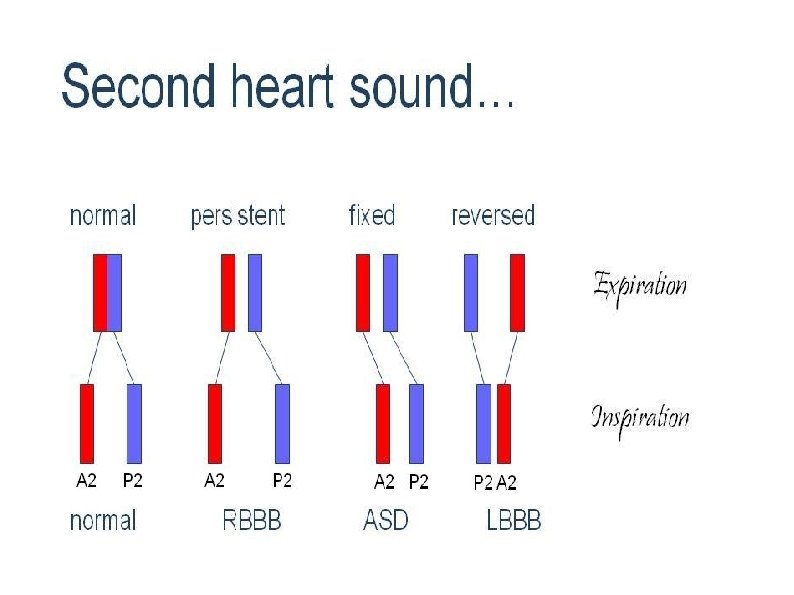
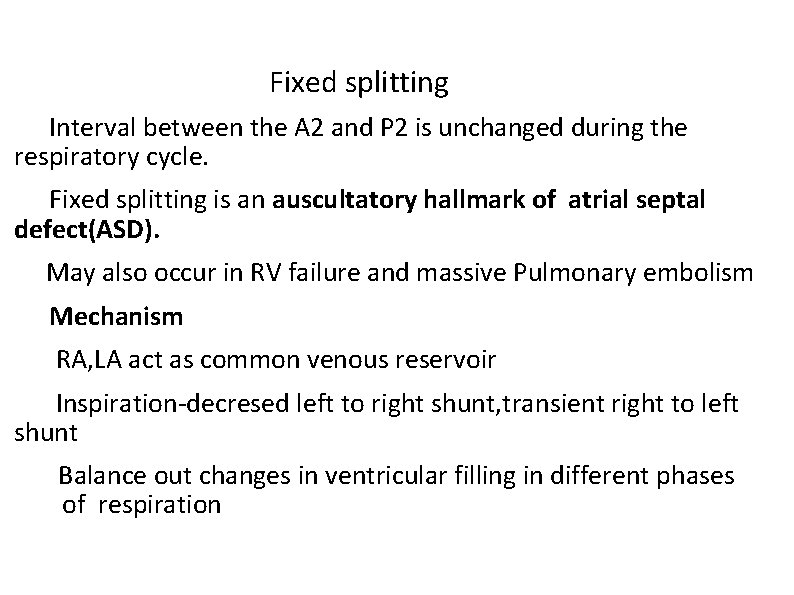
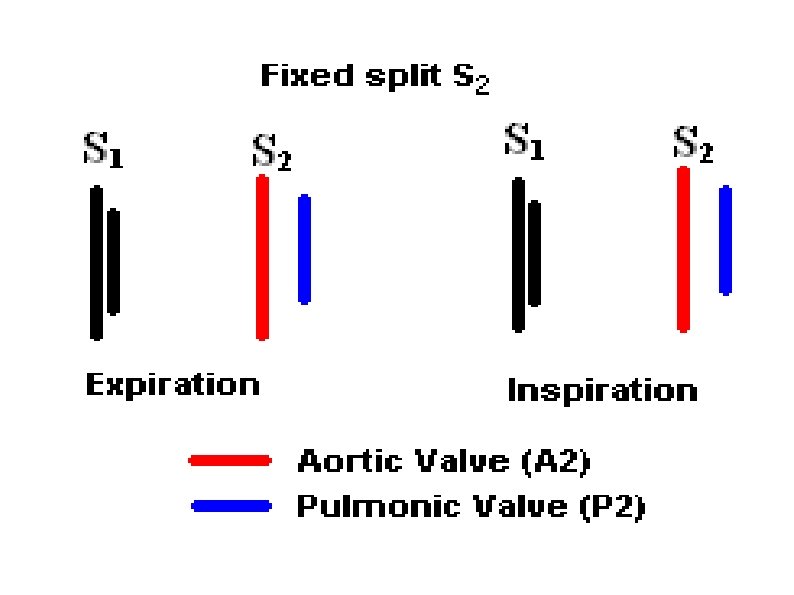
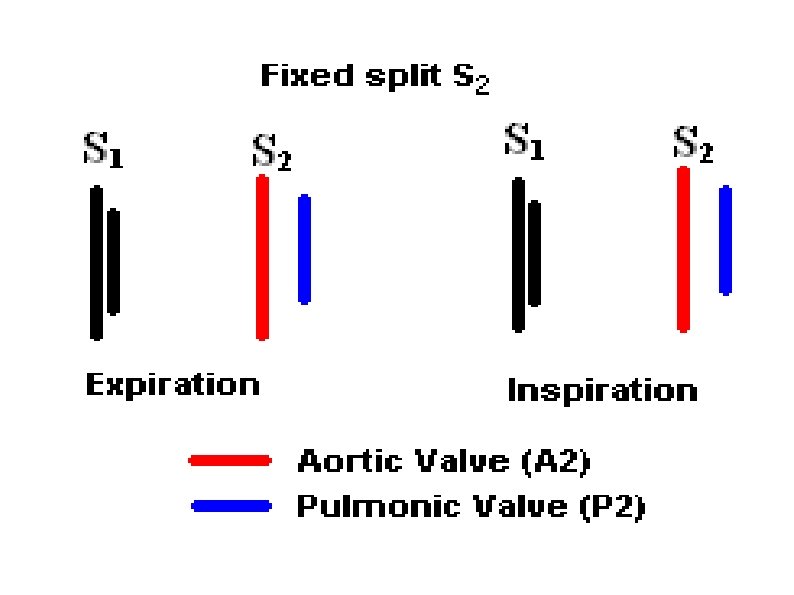
Fixed splitting Interval between the A 2 and P 2 is unchanged during the respiratory cycle. Fixed splitting is an auscultatory hallmark of atrial septal defect(ASD). May also occur in RV failure and massive Pulmonary embolism Mechanism RA, LA act as common venous reservoir Inspiration-decresed left to right shunt, transient right to left shunt Balance out changes in ventricular filling in different phases of respiration
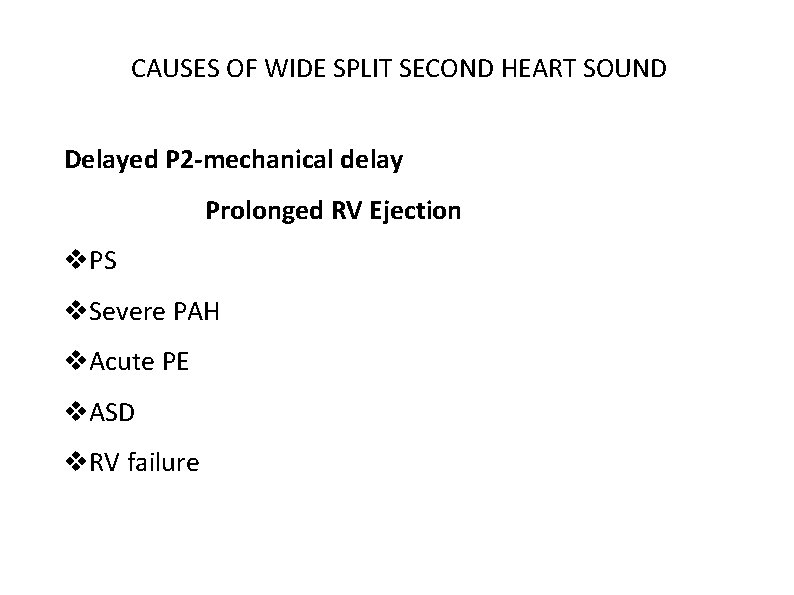
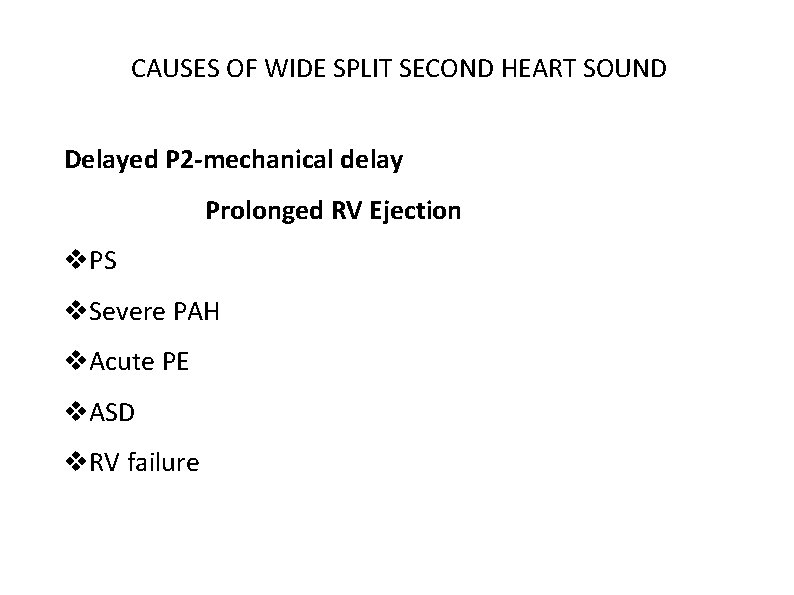
CAUSES OF WIDE SPLIT SECOND HEART SOUND Delayed P 2 -mechanical delay Prolonged RV Ejection PS Severe PAH Acute PE ASD RV failure
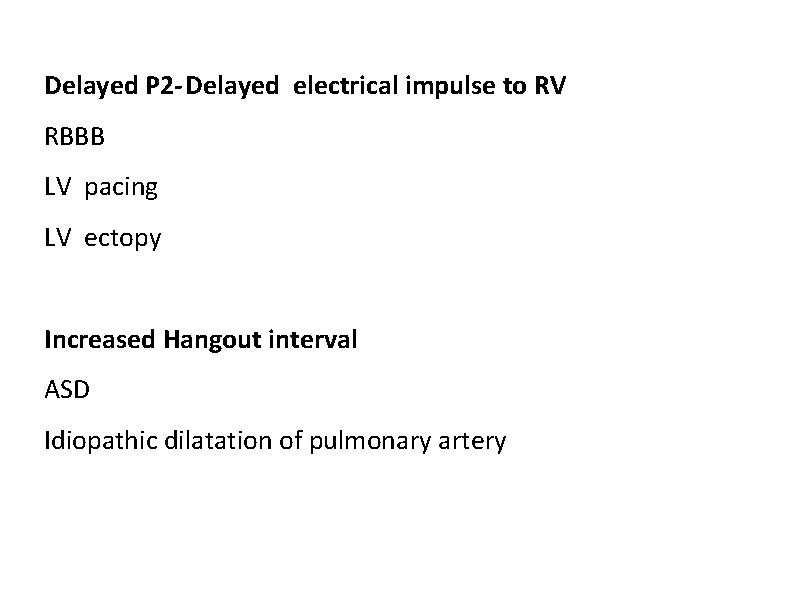
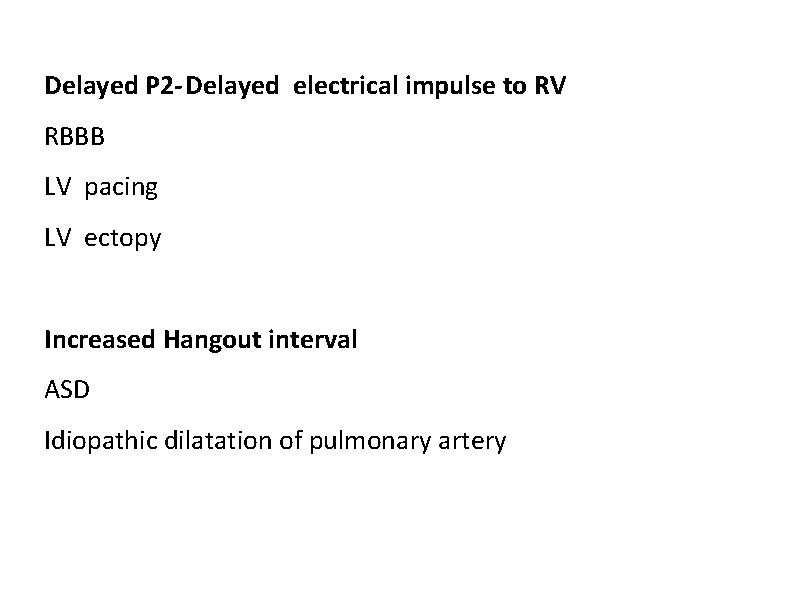
Delayed P 2 -Delayed electrical impulse to RV RBBB LV pacing LV ectopy Increased Hangout interval ASD Idiopathic dilatation of pulmonary artery
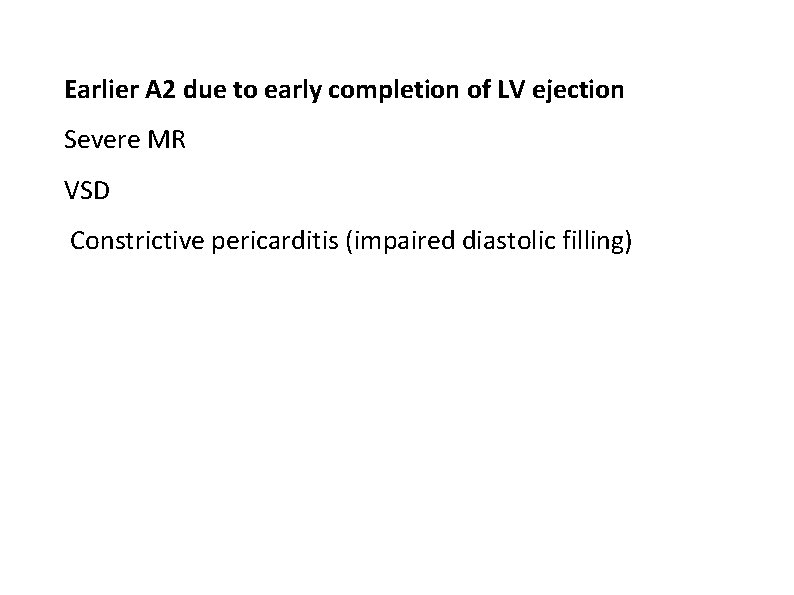
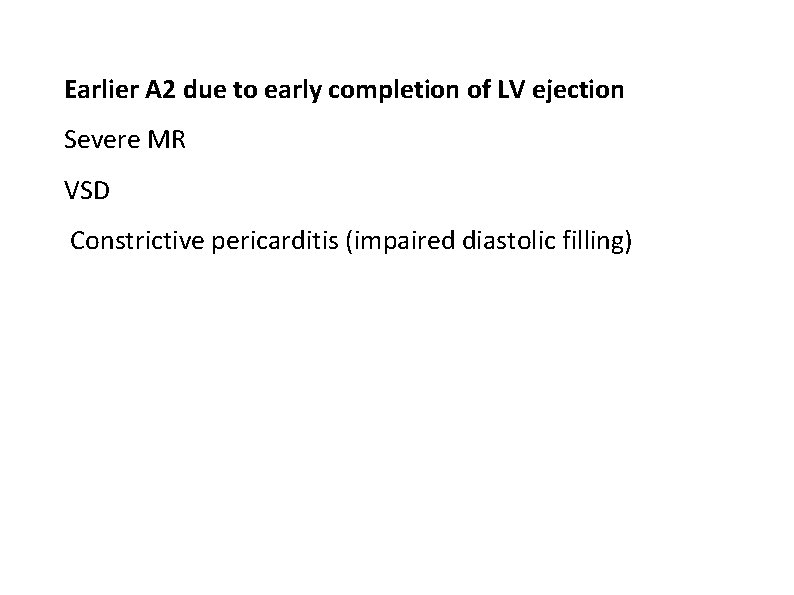
Earlier A 2 due to early completion of LV ejection Severe MR VSD Constrictive pericarditis (impaired diastolic filling)
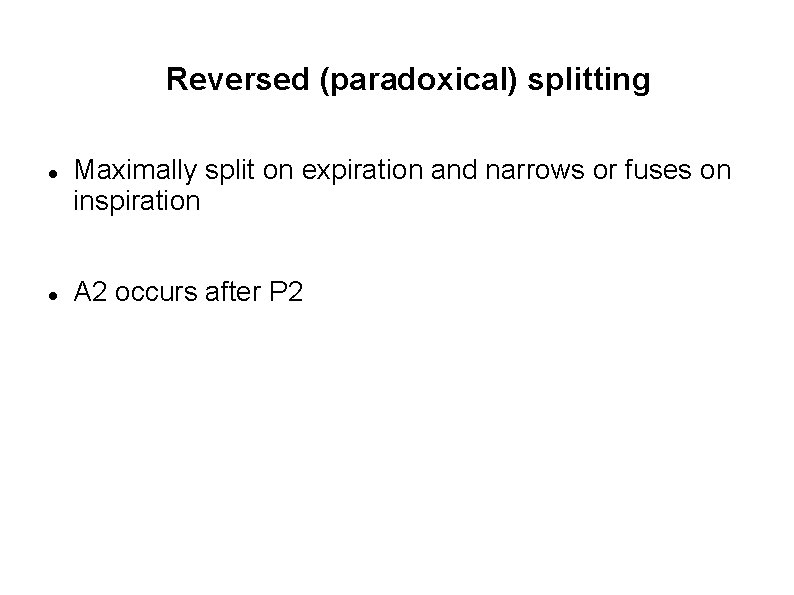
Reversed (paradoxical) splitting Maximally split on expiration and narrows or fuses on inspiration A 2 occurs after P 2
TYPES OF REVERSE SPLIT Type 1: Classical reverse split Type 2: S 2 reversal only in expiration(P 2 -A 2), normal in inspiration(A 2 -P 2) Type 3 paradox: S 2 single in both phases of respiration (reverse split not detected by human ear as interval is less than 20 msec both in inspiration and expiration) Pseudo Reverse Split
REVERSE SPLITTING OF SECOND HEART SOUND Delayed A 2 Delayed electrical activation of LV LBBB RVpacing RV ectopy
Prolonged LV systole Severe AS, Severe systemic hypertension Hypertrophic cardiomyopathy PDA Increased hangout interval on Aortic Side Aneurysm of ascending aorta Early Pulmonic closure Type B WPW syndrome(early activation of RV) TR, Right atrial myxoma
Persistently single When S 2 remains single throughout the respiratory cycle, one component is absent or the two components are persistently synchronous. The most common cause of a single S 2 is inaudibility of the P 2 in older adults with increased anteroposterior chest dimensions.
SINGLE SECOND SOUND Truncus arteriosus Pulmonary atresia Transposition of great vessels AS PS Pulmonary artery hypertension TOF
• Single semilunar valve may produce multiple sounds rarely as in case of Truncus arteriosus with a quadricuspid valve

THANK YOU