SDOH Social Determinates of Health Barriers to Care
SDOH Social Determinates of Health Barriers to Care Plan Concerns
Issues Identified Baltimore 2018 SDOH • FHIR condition does not adequately support the concept of Concern that is not tied to a problem • A SDOH concern can be about another party, not the patient yet directly impacts the patient • What information can be gleaned from Social Media
Care Plan DAM Discussions on SDOH • SDOH is the bright shiny object (rightly so) • Multiple projects • Does HL 7 Patient Care need to define a standard • Should we generate: Draft Ballot for comment - internal - just have to consider comments. Or Informative ballot- have to resolve comments, becomes public. = a committee document. Has no updates. Or Full CDA Template and FHIR Resource
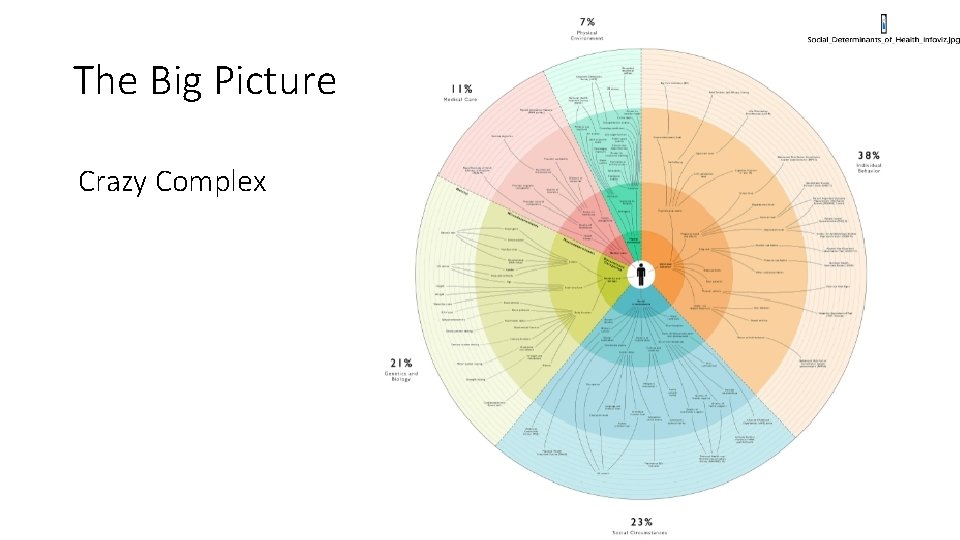
The Big Picture Crazy Complex
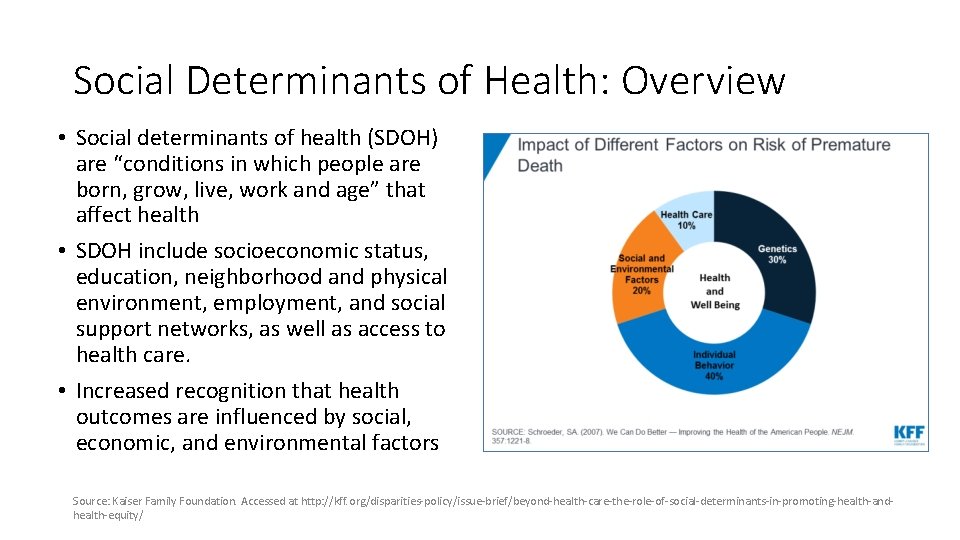
Social Determinants of Health: Overview • Social determinants of health (SDOH) are “conditions in which people are born, grow, live, work and age” that affect health • SDOH include socioeconomic status, education, neighborhood and physical environment, employment, and social support networks, as well as access to health care. • Increased recognition that health outcomes are influenced by social, economic, and environmental factors Source: Kaiser Family Foundation. Accessed at http: //kff. org/disparities-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-andhealth-equity/
Growing body of evidence that shows: • Social determinants of health (SDOH) play a powerful role in shaping health and health outcomes • 80% of clinical outcomes attributable to factors outside traditional MD - patient relationship (RWJ) • Average life expectancy is reduced by 15 -20 years just by living in low income communities (due to stroke, DM, chronic bronchitis etc) (JAMA, 2017) • Growing theory suggests that addressing social needs can potentially improve health outcomes and spending
SDOH Becoming a Central Component CMS Public Sector Examples • CMS launched “Accountable Health Communities” model (2016): • States’ Medicaid reforms include SDOH • Connect Medicare & Medicaid patients to community services • Ohio - Program where providers connect patients with social services • Test whether identifying and addressing SDOH needs affect costs and utilization • Massachusetts - Adjust provider payments for social risk factors • 32 grants awarded for 5 yr model: • 12 - navigation services • 20 - drive partner alignment • Minnesota - Identify those risk factors which are most predictive of cost and performance • Connecticut – Advanced Medical Home models factor in SDOH
Private Payors are also Investing in SDOH • 8 th Annual Industry Pulse Report by the Health. Care Executive Group: • 80% of payers believe that addressing the SDOH will be key to improve their population health programs • Payers are taking action to address SDOH • Community programs • Screenings • Value-based care initiatives • Adding SDOH into clinical workflows • Authors state: payers are starting to realize the organizational benefits and long-term returns for actively addressing SDOH
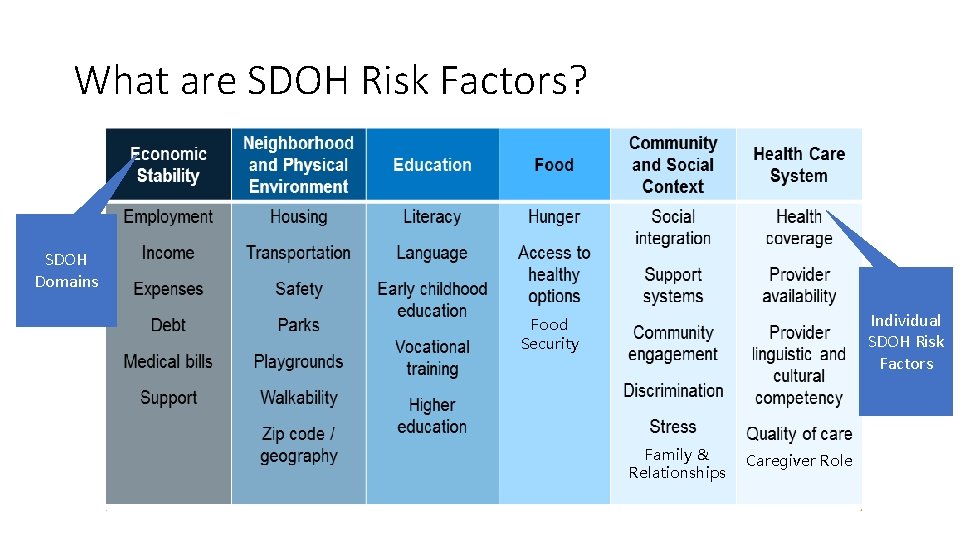
What are SDOH Risk Factors? SDOH Domains Individual SDOH Risk Factors Food Security Family & Relationships Caregiver Role
SIREN Social Determinants of Health (SDOH) Value Sets Standardization Project • The SDOH Project will: • Develop SDOH data elements and associated value sets to support documentation across clinical screening, diagnosis, and treatment activities within EHR systems; • Develop a consensus-based set of recommendations on how best to group these data elements for interoperable electronic exchange and aggregation across clinical, community-based, research, and population health systems. • This project will focus on three priority SDOH domains: transportation, food security, and housing stability and quality (based on existing research and linking these with health)
SIREN How can you participate? • The SDOH Value Sets Standardization Project will be facilitated using an open, free, and transparent platform that promotes broad stakeholder engagement from diverse stakeholder groups spanning clinical and community-based providers, health IT vendors, digital technology innovators, health systems, implementers, standards development organizations (SDOs), payers, researchers, and consumer advocates. • An accessible collaboration site will provide information on how interested groups can join the project, sign up for the distribution list, view the meeting schedule, and obtain information on the project. • Project meetings will be facilitated via online video conferencing; all meeting materials and project deliverables will be published online. What is the timeline? • Project will run from January 2019 until October 2019; weekly 1 -hour meetings will be scheduled for the first phase of the project. • To learn more about the project and/or to express interest participating, please contact Evelyn Gallego • (evelyn. gallego@emiadvisors. net) and Lynette Elliott (lynette. elliott@emiadvisors. net)
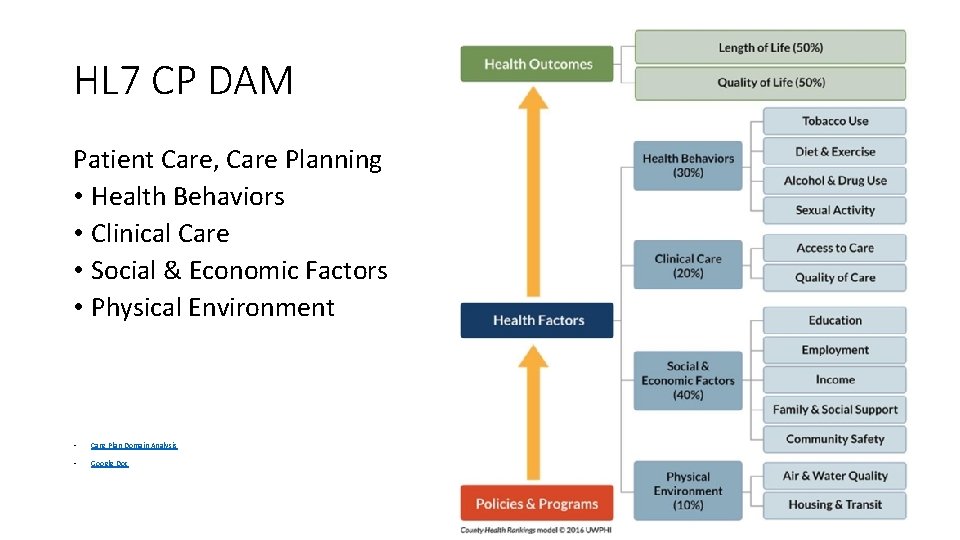
HL 7 CP DAM Patient Care, Care Planning • Health Behaviors • Clinical Care • Social & Economic Factors • Physical Environment • Care Plan Domain Analysis • Google Doc
Sources of SDOH Patient Information • SDOH Information Collection Options? 1. Existing documentation in patient population 2. New documentation (Provider) 3. Patient Entered
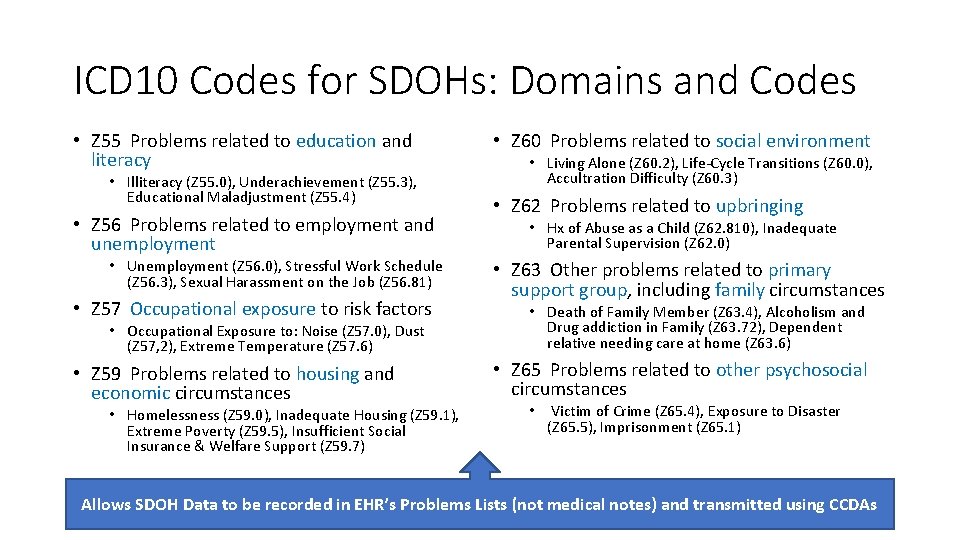
ICD 10 Codes for SDOHs: Domains and Codes • Z 55 Problems related to education and literacy • Illiteracy (Z 55. 0), Underachievement (Z 55. 3), Educational Maladjustment (Z 55. 4) • Z 56 Problems related to employment and unemployment • Unemployment (Z 56. 0), Stressful Work Schedule (Z 56. 3), Sexual Harassment on the Job (Z 56. 81) • Z 57 Occupational exposure to risk factors • Occupational Exposure to: Noise (Z 57. 0), Dust (Z 57, 2), Extreme Temperature (Z 57. 6) • Z 59 Problems related to housing and economic circumstances • Homelessness (Z 59. 0), Inadequate Housing (Z 59. 1), Extreme Poverty (Z 59. 5), Insufficient Social Insurance & Welfare Support (Z 59. 7) • Z 60 Problems related to social environment • Living Alone (Z 60. 2), Life-Cycle Transitions (Z 60. 0), Accultration Difficulty (Z 60. 3) • Z 62 Problems related to upbringing • Hx of Abuse as a Child (Z 62. 810), Inadequate Parental Supervision (Z 62. 0) • Z 63 Other problems related to primary support group, including family circumstances • Death of Family Member (Z 63. 4), Alcoholism and Drug addiction in Family (Z 63. 72), Dependent relative needing care at home (Z 63. 6) • Z 65 Problems related to other psychosocial circumstances • Victim of Crime (Z 65. 4), Exposure to Disaster (Z 65. 5), Imprisonment (Z 65. 1) Allows SDOH Data to be recorded in EHR’s Problems Lists (not medical notes) and transmitted using CCDAs
Extracting SDOH Data from EHR - Structured Data • ICD 10 provides a starting framework to map and standardize EHR • Disparate SDOH codes exists within ICD 9, SNOMED, and LOINC – no framework • Manually align definitions and create crosswalks
Extracting SDOH Data from EHR - Unstructured Data Codes Alone are Insufficient in Capturing All SDOH Data from EHR • Keyword Searches • Determine multitude of ways SDOH is referenced and abbreviated • Manual review of initial search results • Develop pattern matching search process
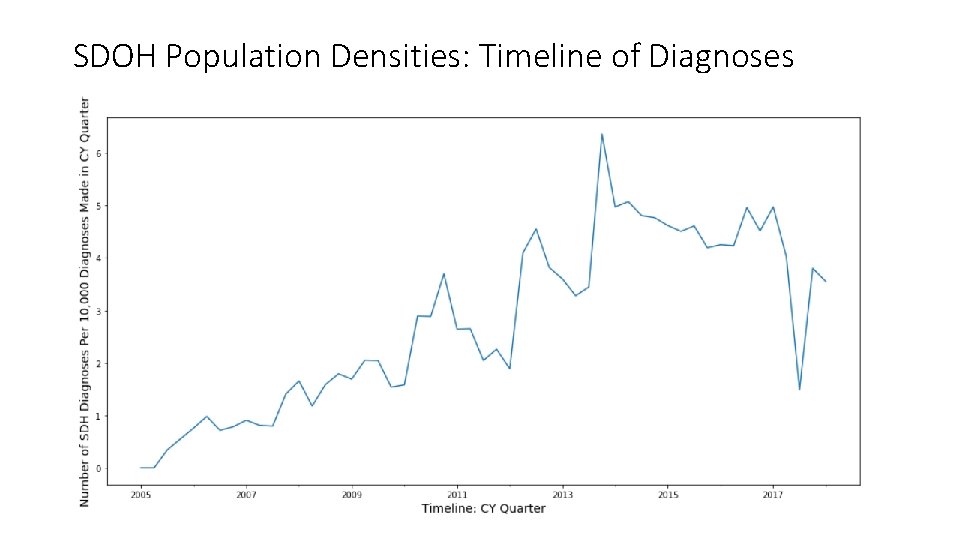
SDOH Population Densities: Timeline of Diagnoses

Standardized Rankings Rank SDOH - Std Name 1 DISRUPTION OF FAMILY BY SEPARATION OR DIVORCE 2 DISAPPEARANCE OR DEATH OF FAMILY MEMBER 3 UNEMPLOYMENT, UNSPECIFIED 4 PROBLEMS RELATED TO LIVING ALONE 5 ALCOHOLISM AND/OR DRUG ADDICTION IN FAMILY 6 OTHER PHYSICAL AND MENTAL STRAIN RELATED TO WORK 7 OTHER SPECIFIED PROBLEMS RELATED TO PRIMARY SUPPORT GROUP 8 UNDERACHIEVEMENT IN SCHOOL 9 PROBLEMS IN RELATIONSHIP WITH SPOUSE OR PARTNER 10 DEPENDENT RELATIVE NEEDING CARE AT HOME 11 PROBLEM RELATED TO PRIMARY SUPPORT GROUP, UNSPECIFIED 12 CHILD IN WELFARE CUSTODY 13 PARENT-BIOLOGICAL CHILD CONFLICT 14 HOMELESSNESS • 14 (out of 96 SDOHs) account for 90% of total unique SDOH diagnoses
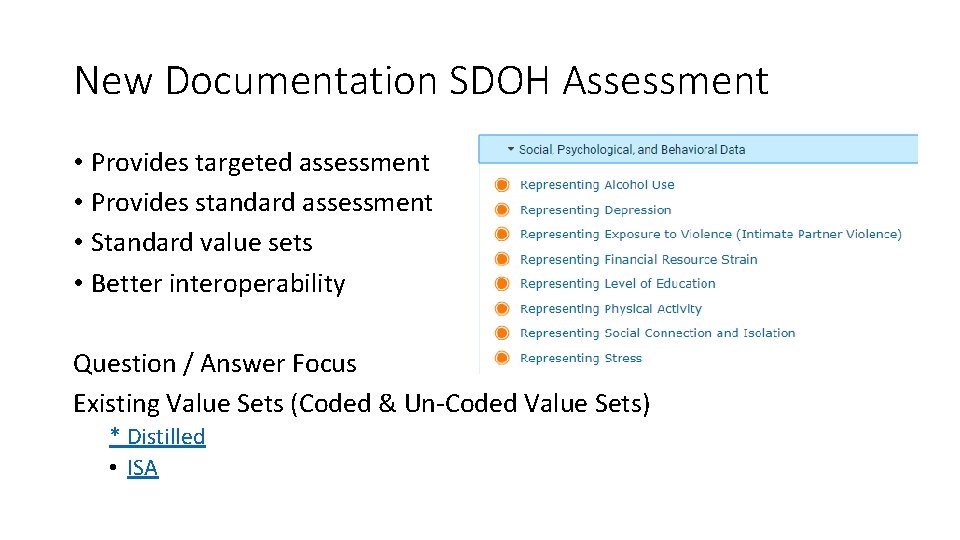
New Documentation SDOH Assessment • Provides targeted assessment • Provides standard assessment • Standard value sets • Better interoperability Question / Answer Focus Existing Value Sets (Coded & Un-Coded Value Sets) * Distilled • ISA
Full Charting For CP DAM Categories e. g. • Mind Mapping
FHIR Approach • Experimenting with FHIR • An alternative option may be CIMI

Source Compare • VISIO
Add Content Resources • Specific patient questions the US will probably have to use • ISA • CMS • And This Distilled
- Slides: 24