Screening Geriatric Assessment and Interventions Texte courant Pierre


- Slides: 65
Screening, Geriatric Assessment and Interventions Texte courant Pierre Soubeyran and Siri Rostoft
Disclosure No conflict of interests
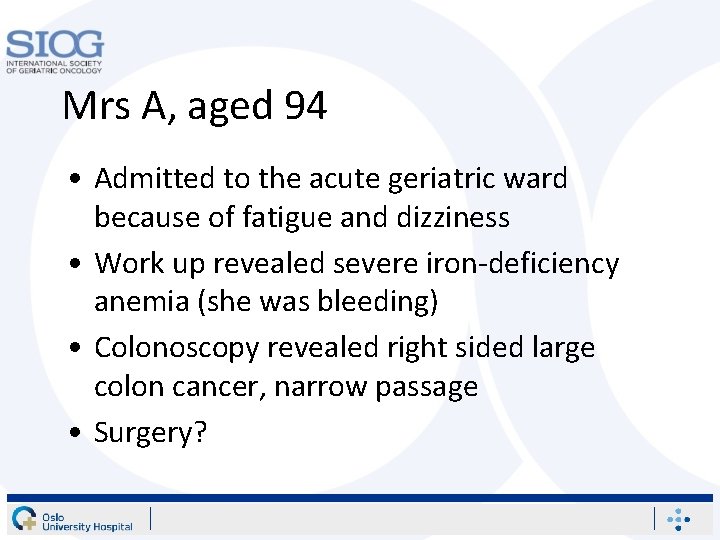
Mrs A, aged 94 • Admitted to the acute geriatric ward because of fatigue and dizziness • Work up revealed severe iron-deficiency anemia (she was bleeding) • Colonoscopy revealed right sided large colon cancer, narrow passage • Surgery?
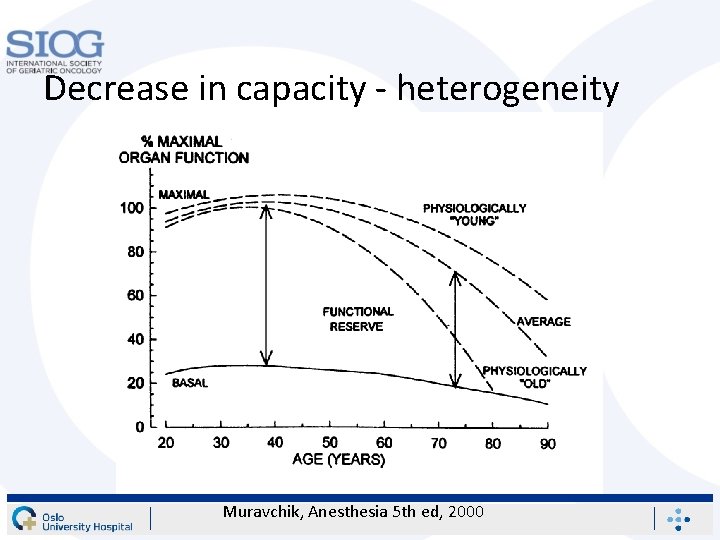
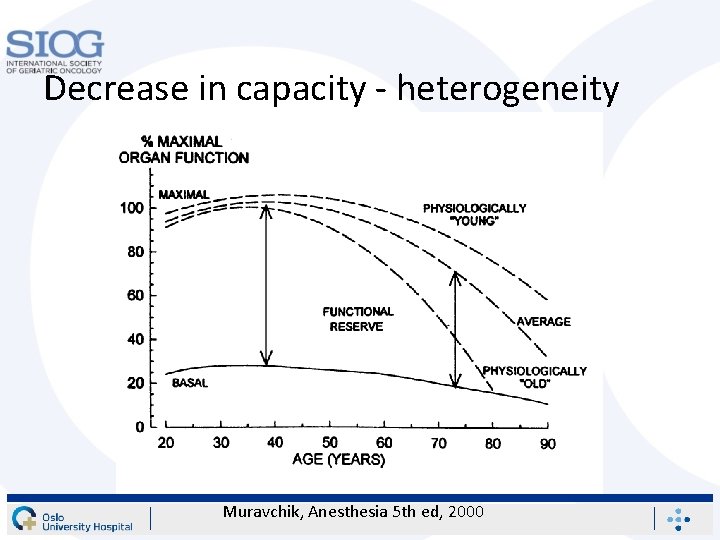
Decrease in capacity - heterogeneity Muravchik, Anesthesia 5 th ed, 2000
What factors to consider? • Discuss for 2 -3 minutes with the person next to you
Screening tools Relevance for the management of cancer patients Pierre Soubeyran, MD, Ph. D Institut Bergonié, Université Bordeaux
What is the final goal ? • Better treat patients – Ensure tumor control, as much as possible – Limit the risk of adverse events • which may lead to dependencies or even death • Maintain quality of life – Patient is still leaving at home – Still autonomous with no sequellae – Cancer is controlled (cured ? )
Available data for screening • Standard evaluation – Performance status • At baseline • A few months before – Organ function • Creatinine clearance • Liver tests… – Nutritional status • Weight, albumin… • Geriatric assessment – Designed for the oldest – To be implemented in oncology 9
How many Risk Groups ? • Heterogeneous population • Three groups (or even more) – Fit – Intermediate – Frail
How to design screening tools ? • Various solutions – Identify a specific vulnerable profile • Vulnerable geriatric profile – Questionnaires, Fried criteria • Non feasibility of a specific treatment – Or Identify predictors of unacceptable events • Early death, functional decline, toxicity
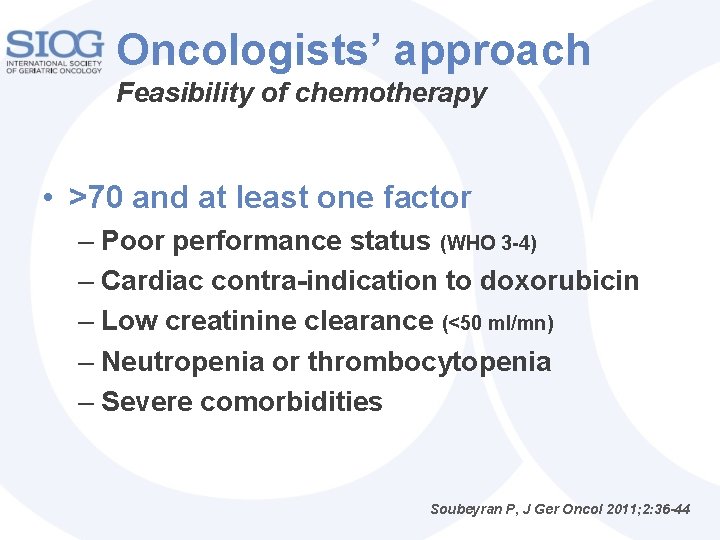
Oncologists’ approach Feasibility of chemotherapy • >70 and at least one factor – Poor performance status (WHO 3 -4) – Cardiac contra-indication to doxorubicin – Low creatinine clearance (<50 ml/mn) – Neutropenia or thrombocytopenia – Severe comorbidities Soubeyran P, J Ger Oncol 2011; 2: 36 -44
Another approach Predictors of unacceptable events • Events which would have changed your initial decision, would you have known it may occur later… – Early death – Functional decline – Hospitalization for toxicity
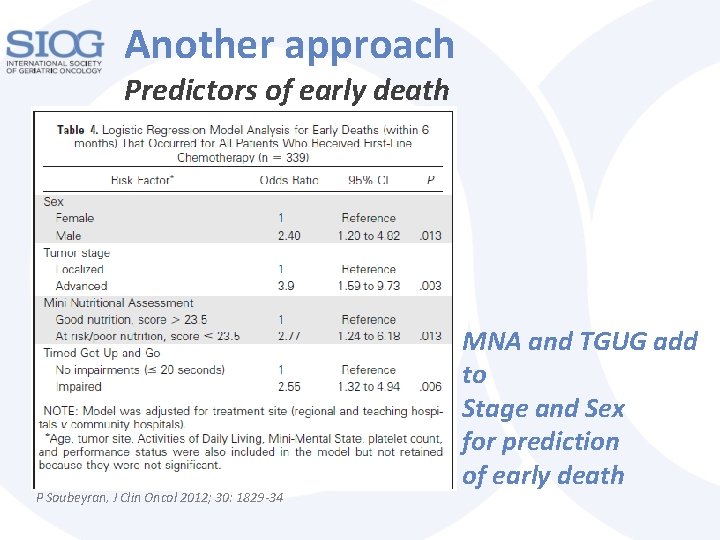
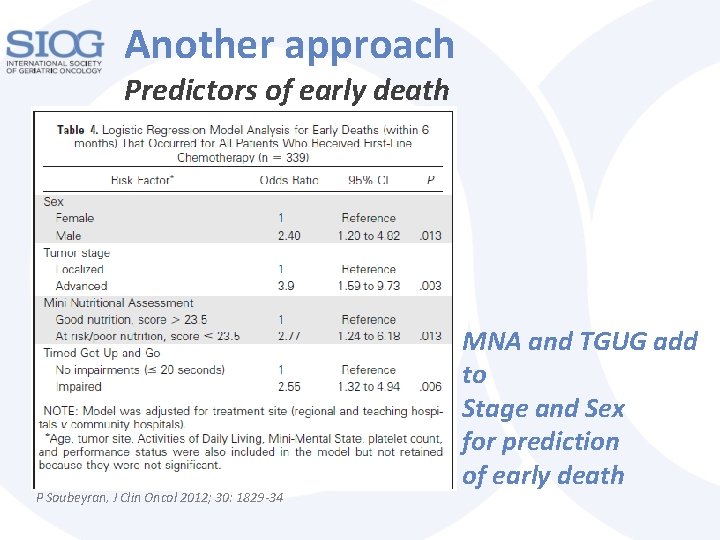
Another approach Predictors of early death P Soubeyran, J Clin Oncol 2012; 30: 1829 -34 MNA and TGUG add to Stage and Sex for prediction of early death
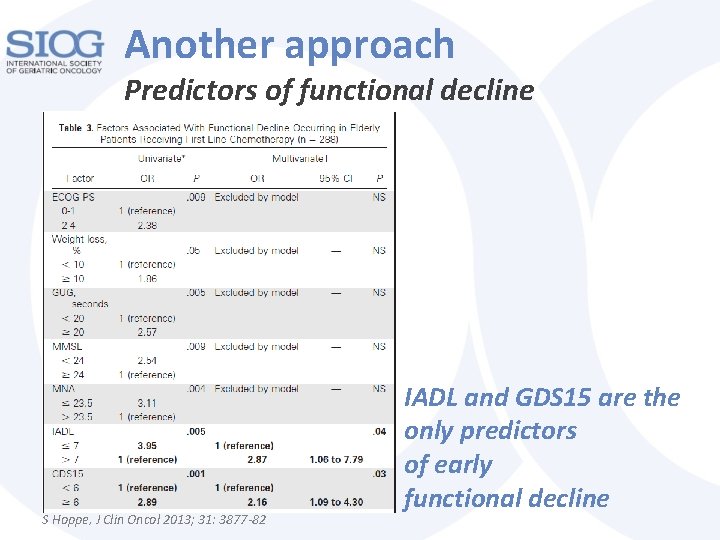
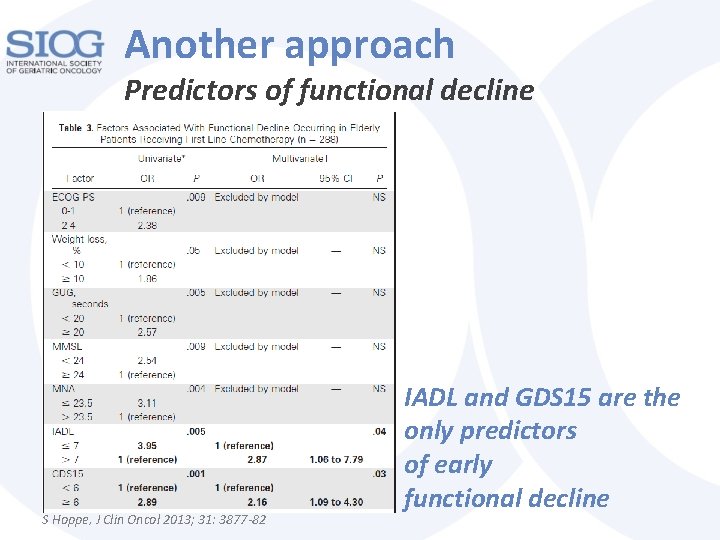
Another approach Predictors of functional decline S Hoppe, J Clin Oncol 2013; 31: 3877 -82 IADL and GDS 15 are the only predictors of early functional decline
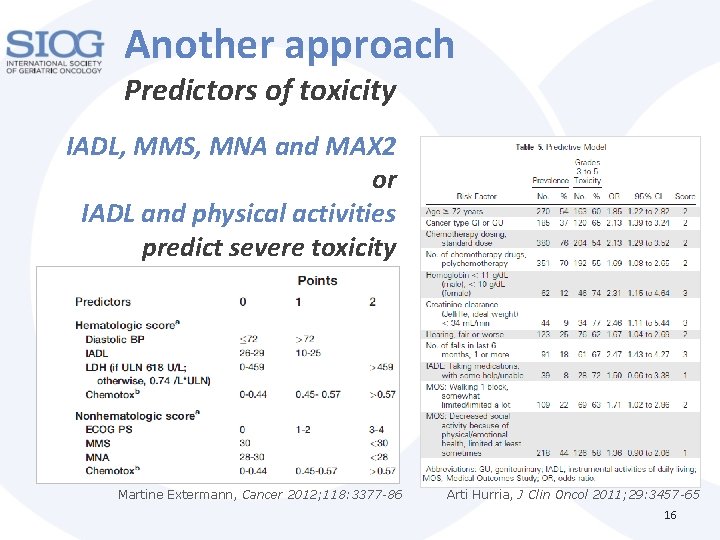
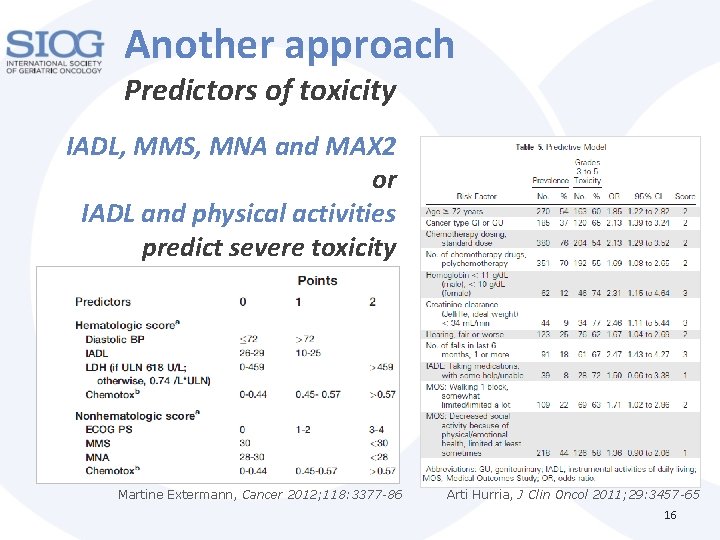
Another approach Predictors of toxicity IADL, MMS, MNA and MAX 2 or IADL and physical activities predict severe toxicity Martine Extermann, Cancer 2012; 118: 3377 -86 Arti Hurria, J Clin Oncol 2011; 29: 3457 -65 16
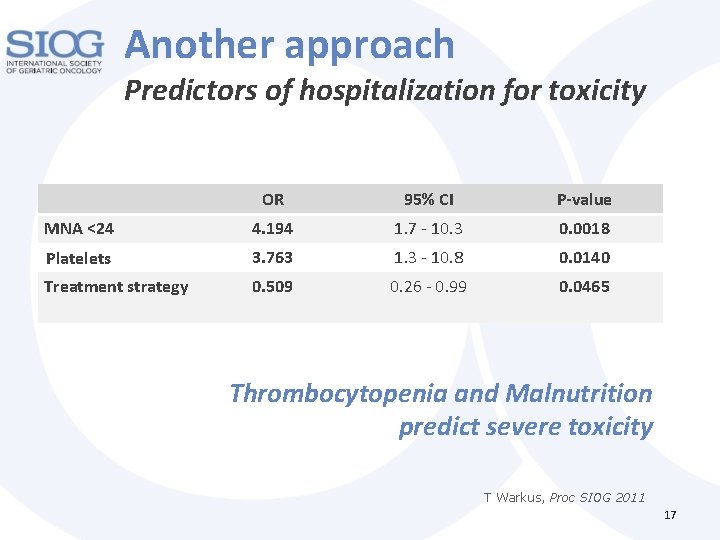
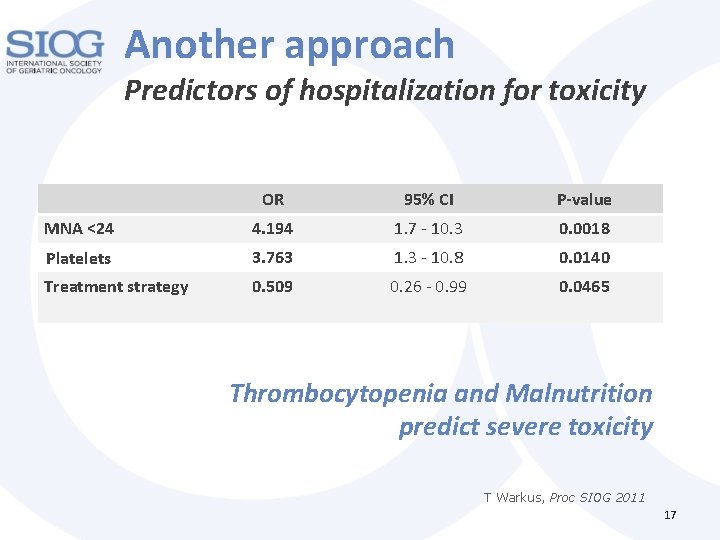
Another approach Predictors of hospitalization for toxicity OR 95% CI P-value MNA <24 4. 194 1. 7 - 10. 3 0. 0018 Platelets 3. 763 1. 3 - 10. 8 0. 0140 Treatment strategy 0. 509 0. 26 - 0. 99 0. 0465 Thrombocytopenia and Malnutrition predict severe toxicity T Warkus, Proc SIOG 2011 17
Too many patients to evaluate Most CGA tools are useful CGA is time-consuming Need for Screening tools
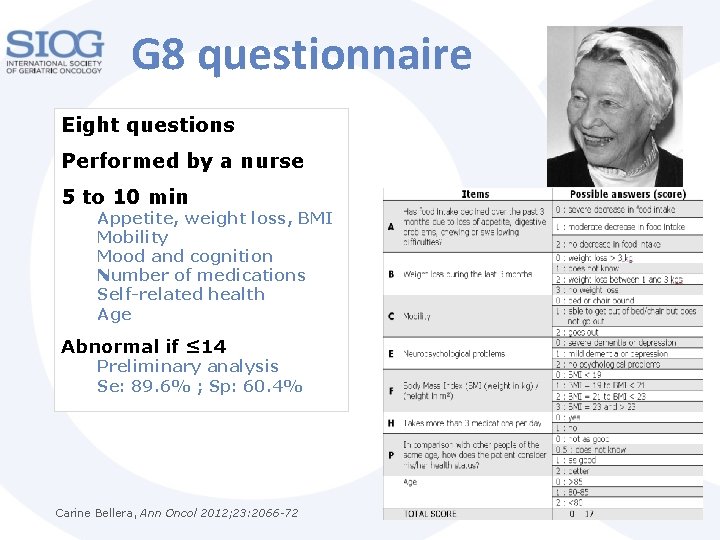
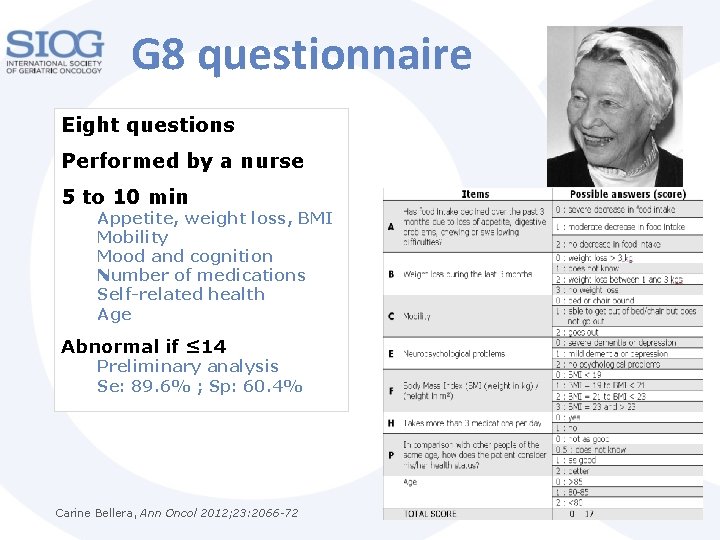
G 8 questionnaire Eight questions Performed by a nurse 5 to 10 min Appetite, weight loss, BMI Mobility Mood and cognition Number of medications Self-related health Age Abnormal if ≤ 14 Preliminary analysis Se: 89. 6% ; Sp: 60. 4% Carine Bellera, Ann Oncol 2012; 23: 2066 -72
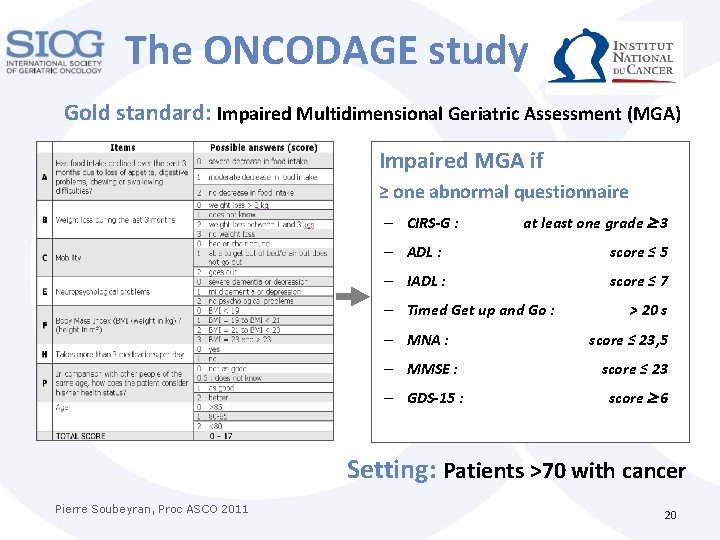
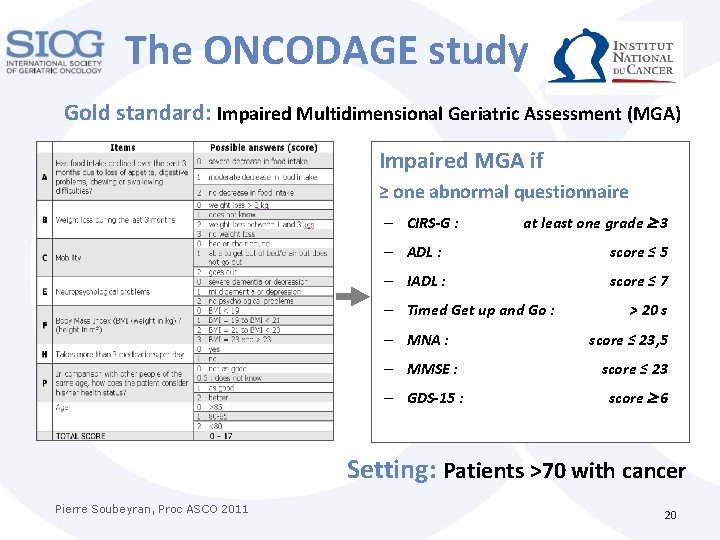
The ONCODAGE study Gold standard: Impaired Multidimensional Geriatric Assessment (MGA) Impaired MGA if ≥ one abnormal questionnaire – CIRS-G : at least one grade 3 – ADL : score ≤ 5 – IADL : score ≤ 7 – Timed Get up and Go : – MNA : > 20 s score ≤ 23, 5 – MMSE : score ≤ 23 – GDS-15 : score 6 Setting: Patients >70 with cancer Pierre Soubeyran, Proc ASCO 2011 20
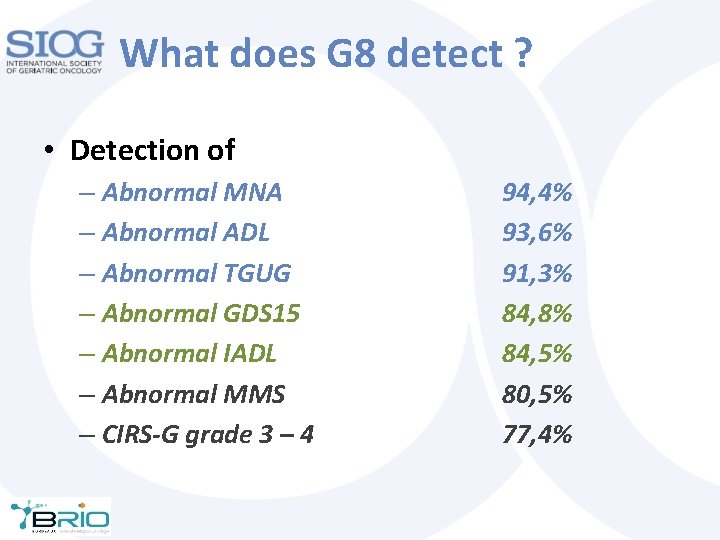
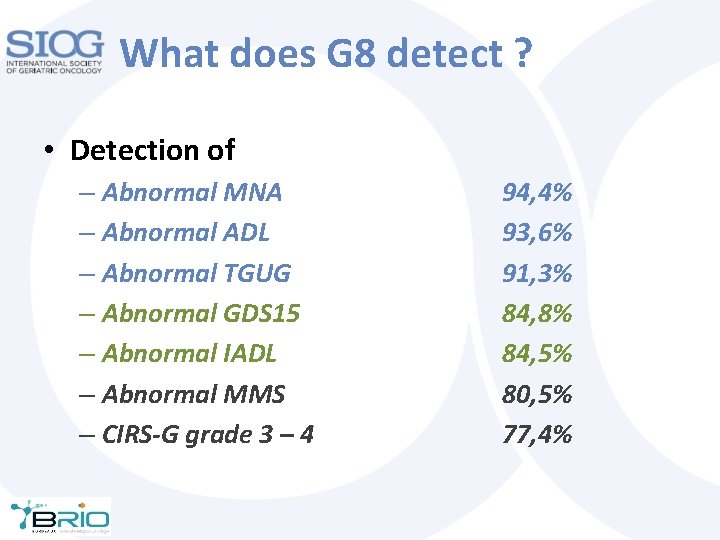
What does G 8 detect ? • Detection of – Abnormal MNA – Abnormal ADL – Abnormal TGUG – Abnormal GDS 15 – Abnormal IADL – Abnormal MMS – CIRS-G grade 3 – 4 94, 4% 93, 6% 91, 3% 84, 8% 84, 5% 80, 5% 77, 4%
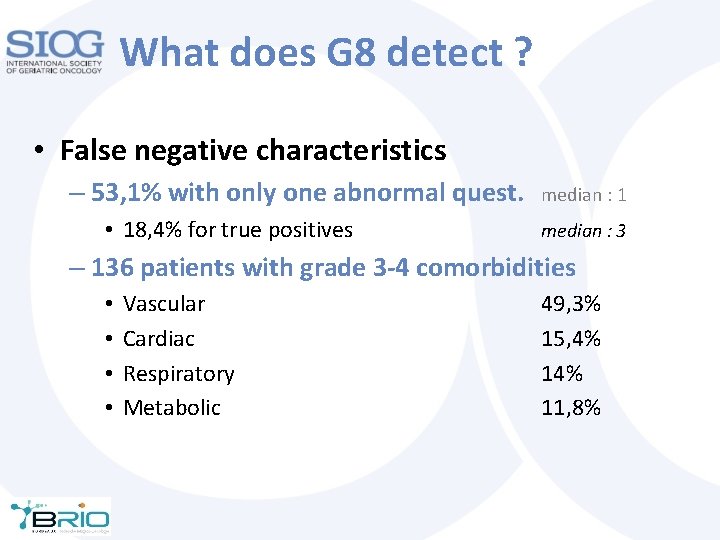
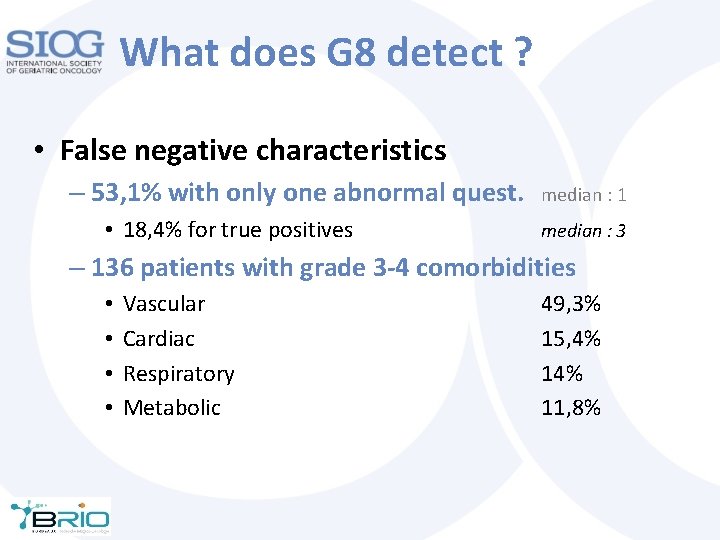
What does G 8 detect ? • False negative characteristics – 53, 1% with only one abnormal quest. • 18, 4% for true positives median : 1 median : 3 – 136 patients with grade 3 -4 comorbidities • • Vascular Cardiac Respiratory Metabolic 49, 3% 15, 4% 11, 8%
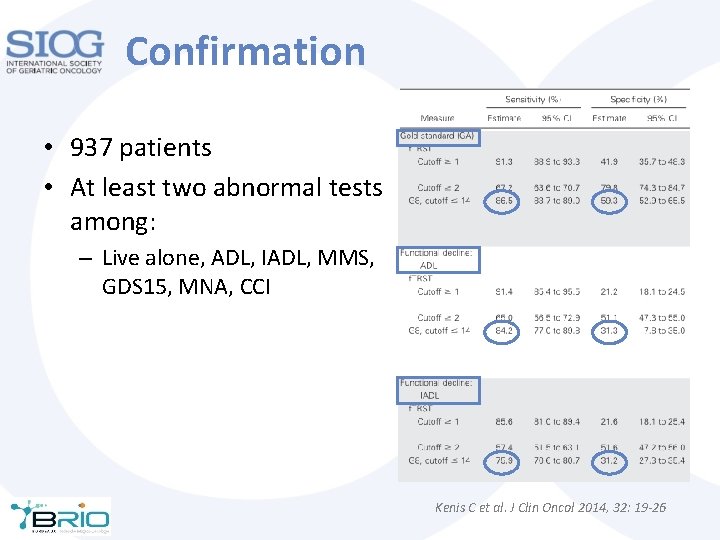
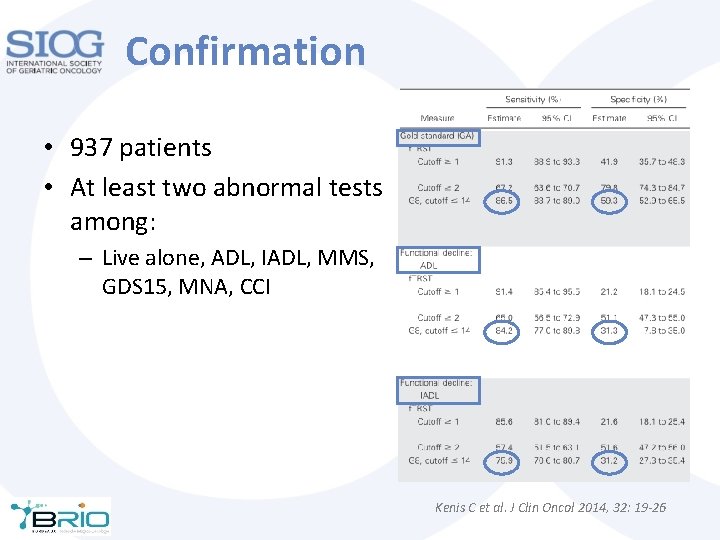
Confirmation • 937 patients • At least two abnormal tests among: – Live alone, ADL, IADL, MMS, GDS 15, MNA, CCI Kenis C et al. J Clin Oncol 2014, 32: 19 -26
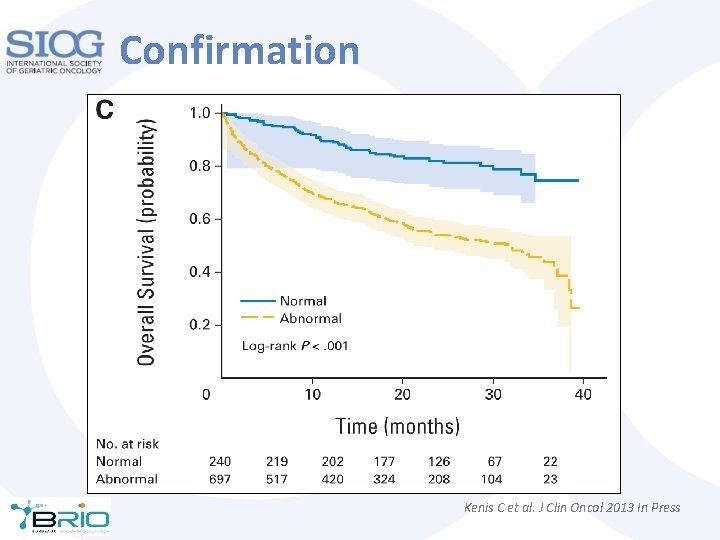
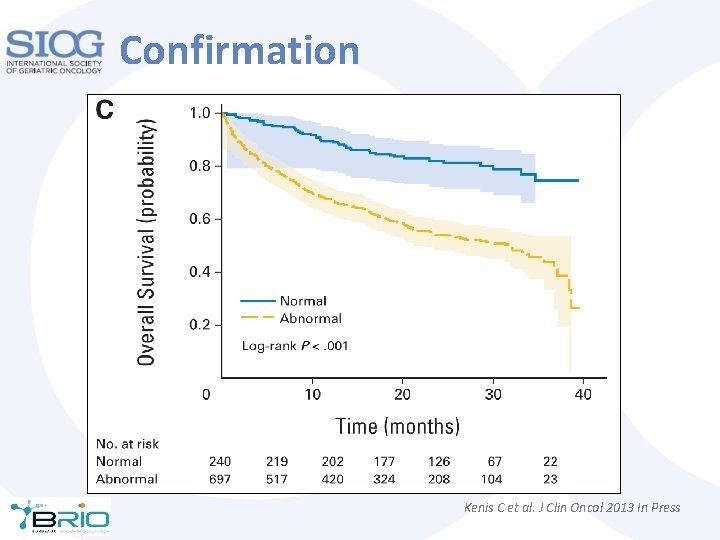
Confirmation Kenis C et al. J Clin Oncol 2013 In Press
What to do when the screening tool is positive ?
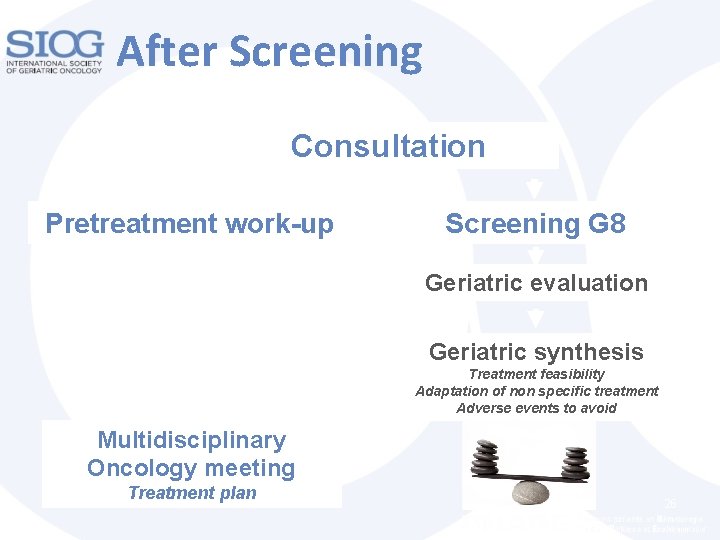
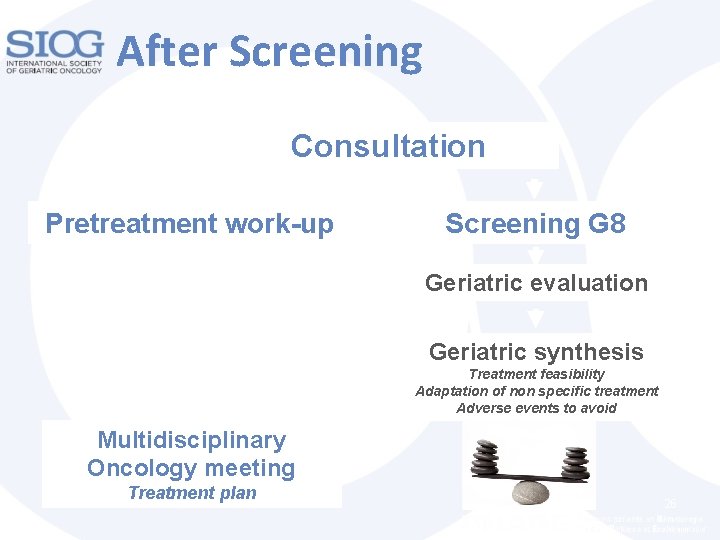
After Screening Consultation Pretreatment work-up Screening G 8 Geriatric evaluation Geriatric synthesis Treatment feasibility Adaptation of non specific treatment Adverse events to avoid Multidisciplinary Oncology meeting Treatment plan 26
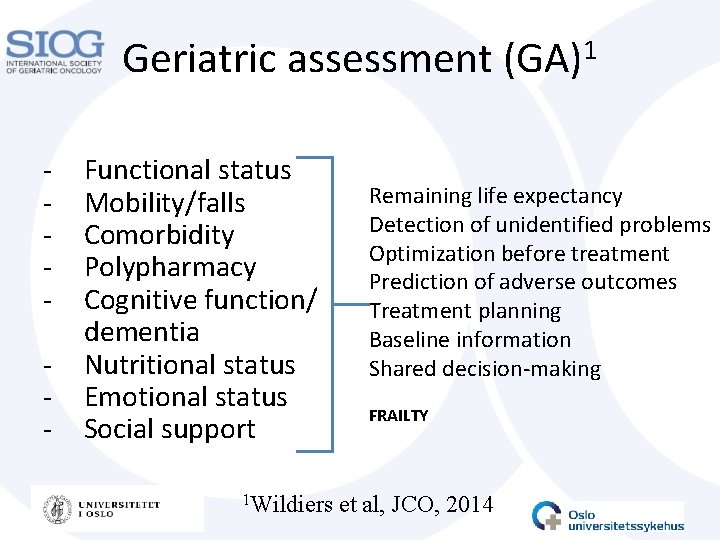
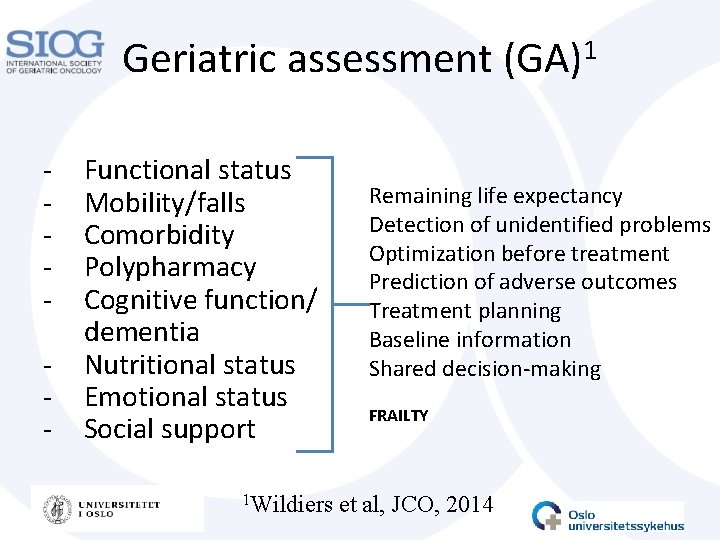
Geriatric assessment - Functional status Mobility/falls Comorbidity Polypharmacy Cognitive function/ dementia Nutritional status Emotional status Social support 1 Wildiers 1 (GA) Remaining life expectancy Detection of unidentified problems Optimization before treatment Prediction of adverse outcomes Treatment planning Baseline information Shared decision-making FRAILTY et al, JCO, 2014
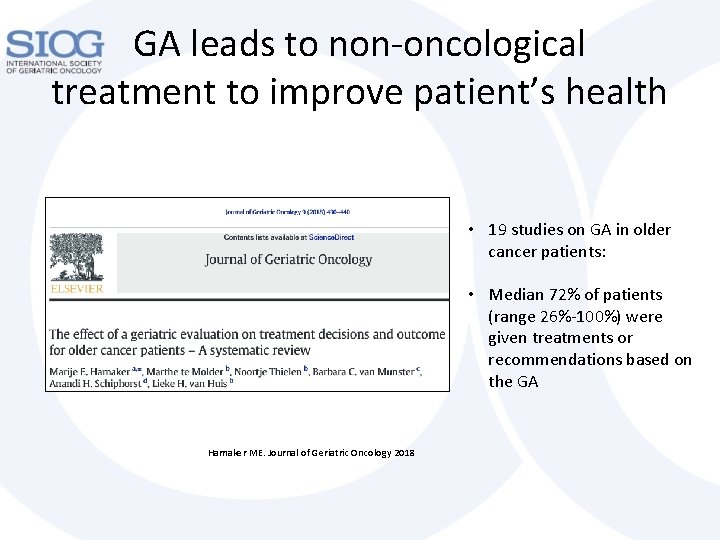
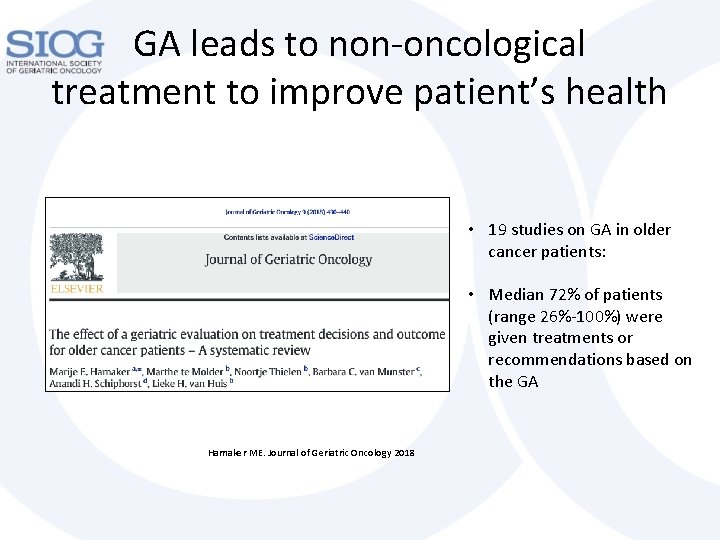
GA leads to non-oncological treatment to improve patient’s health • 19 studies on GA in older cancer patients: • Median 72% of patients (range 26%-100%) were given treatments or recommendations based on the GA Hamaker ME. Journal of Geriatric Oncology 2018

GA leads to changes in oncological treatment • Systematic review of 11 studies: • 28% of patients had their oncological treatment-plan changed after the GA • Of these, the majority had treatment changed to a less intensive regime Hamaker ME. Journal of Geriatric Oncology 2018.
Journal of Surgical Research 193 (2015) 265 -272
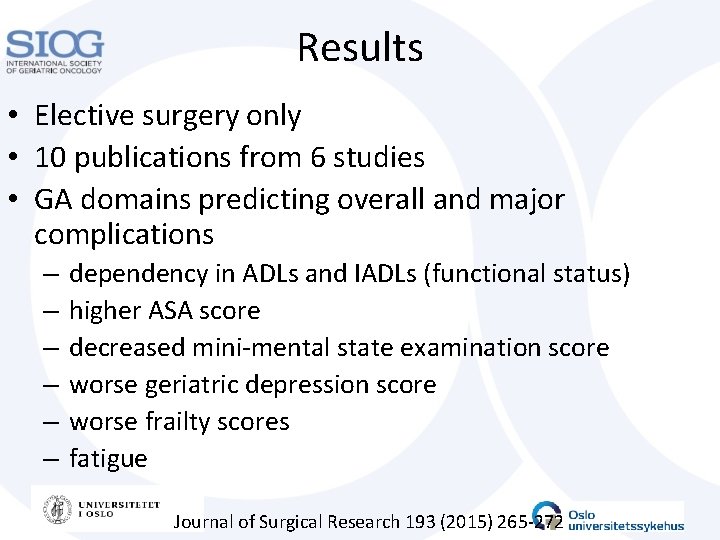
Results • Elective surgery only • 10 publications from 6 studies • GA domains predicting overall and major complications – – – dependency in ADLs and IADLs (functional status) higher ASA score decreased mini-mental state examination score worse geriatric depression score worse frailty scores fatigue Journal of Surgical Research 193 (2015) 265 -272
Results cont. • Age was not an independent predictor of morbidity in any studies • No GA domains predicted postoperative mortality (low mortality rates in elective surgery) • Frailty predicted readmissions • Functional status and frailty predicted discharge to a nursing home Journal of Surgical Research 193 (2015) 265 -272
Geriatric assessment Categorization Fit Intermediate Frail
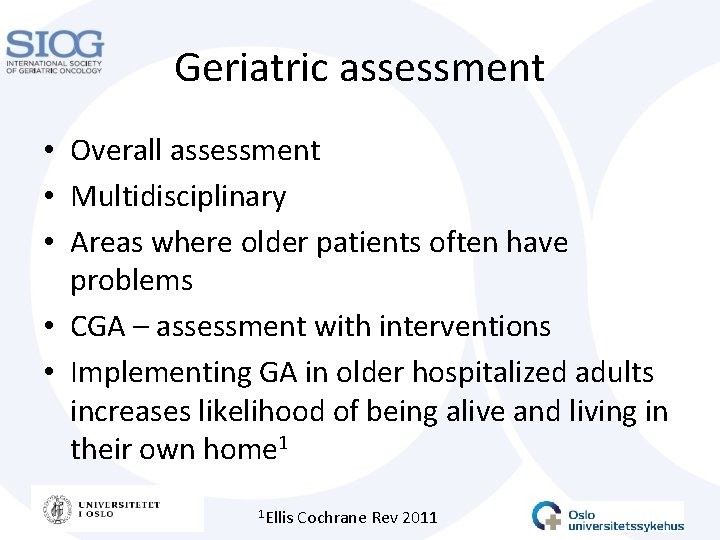
Geriatric assessment • Overall assessment • Multidisciplinary • Areas where older patients often have problems • CGA – assessment with interventions • Implementing GA in older hospitalized adults increases likelihood of being alive and living in their own home 1 1 Ellis Cochrane Rev 2011
Mrs A – Geriatric Assessment • Functional status: Dependence in IADL. Needed help shopping. Problems walking, uses a cane. TUG > 20 sec • Comorbidity: Heart failure – but is the diagnosis correct? She can walk one flight of stairs without being out of breath. Stroke in 2008, no apparent sequela. Reduced vision and reduced hearing. • Polypharmacy: beta blocker and diuretics
• Nutritional status: No appetite last month (due to tumour), weight loss, at risk of malnutrition • Cognitive function: MMSE 27/30, she appeared adequate in conversation, she could discuss treatment options • Emotional status: No symptoms of depression
Recommendation • She had some frailty indicators, risk of postoperative complications high • Complications from tumour at present (anemia, weight loss) • Risk in emergency surgery much higher than elective surgery • Operated electively, had some complications, survived, discharged home
Self-assessment • What are the major components of a GA? • Why is a GA useful in the cancer setting?
A FEW WORDS ABOUT FUNCTIONAL STATUS
Question for the audience • How do we measure functional status? • What influences on your functional status? • Mention examples from clinic
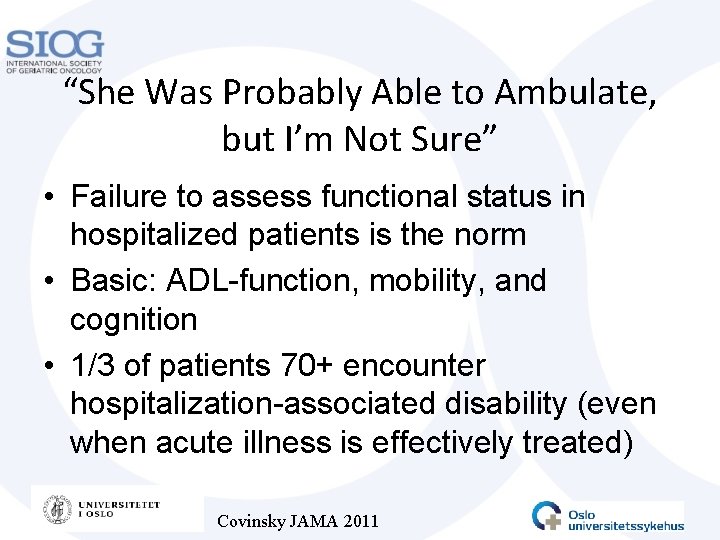
“She Was Probably Able to Ambulate, but I’m Not Sure” • Failure to assess functional status in hospitalized patients is the norm • Basic: ADL-function, mobility, and cognition • 1/3 of patients 70+ encounter hospitalization-associated disability (even when acute illness is effectively treated) Covinsky JAMA 2011
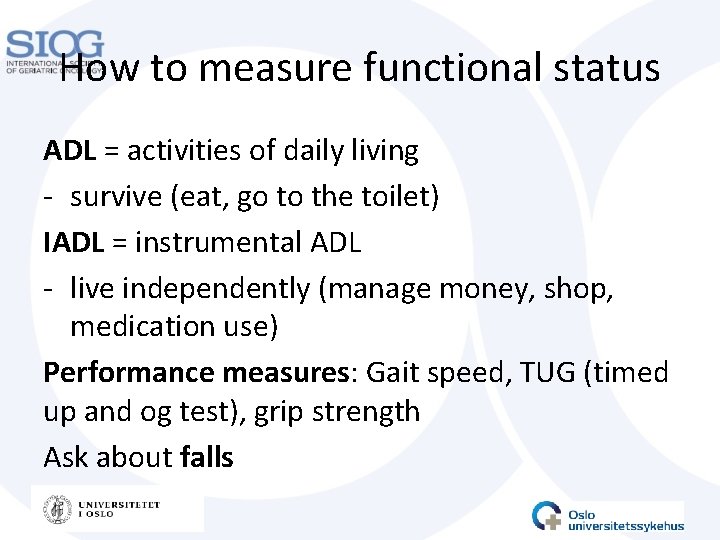
How to measure functional status ADL = activities of daily living - survive (eat, go to the toilet) IADL = instrumental ADL - live independently (manage money, shop, medication use) Performance measures: Gait speed, TUG (timed up and og test), grip strength Ask about falls
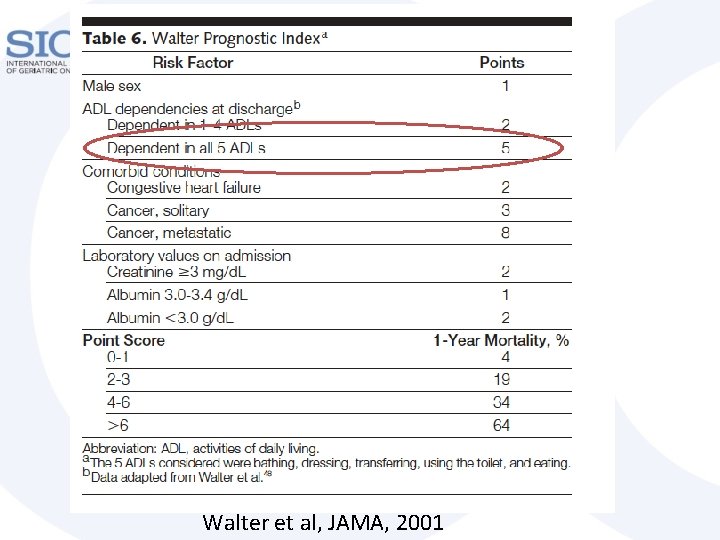
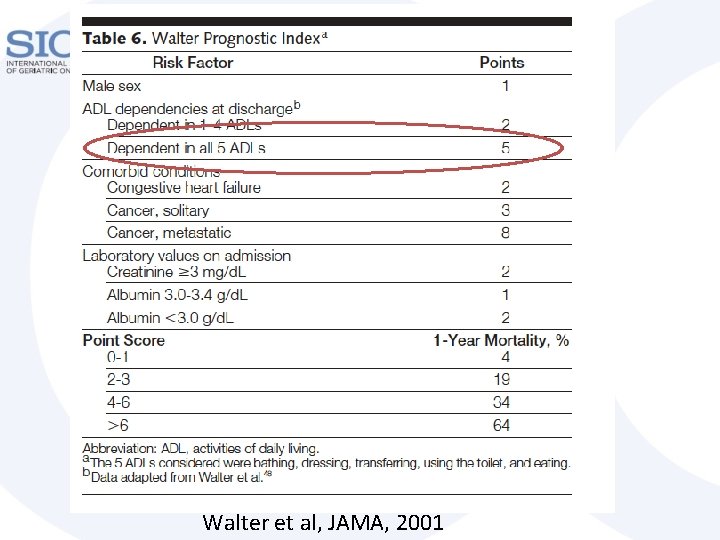
Walter et al, JAMA, 2001
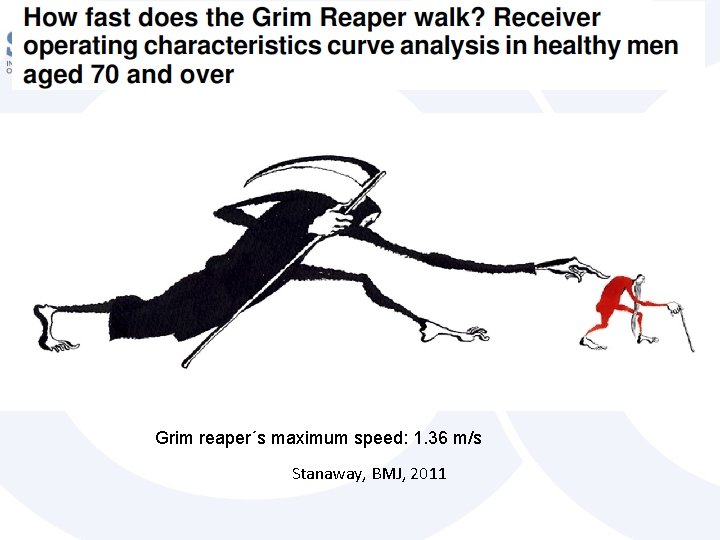
Grim reaper´s maximum speed: 1. 36 m/s Stanaway, BMJ, 2011
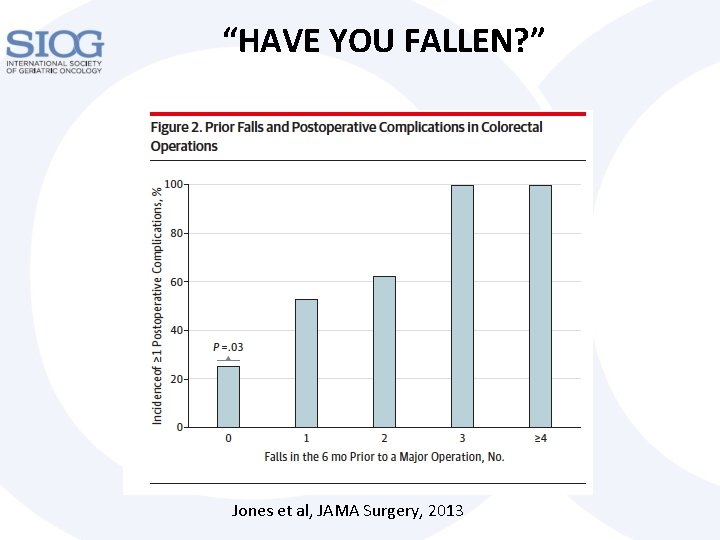
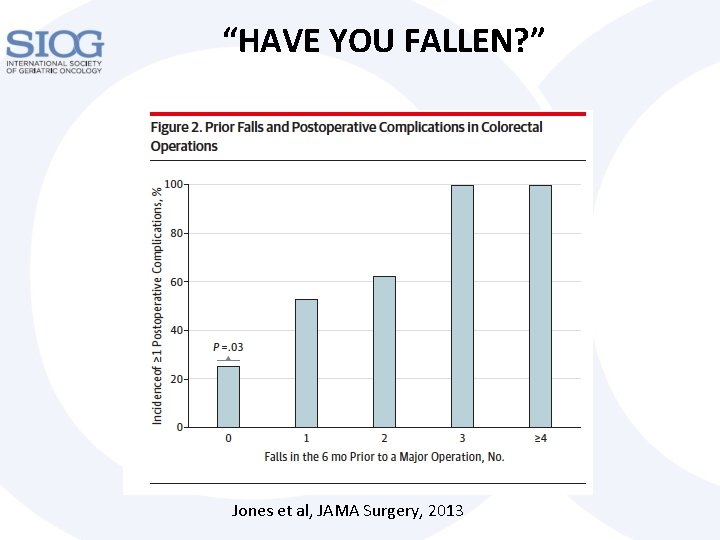
“HAVE YOU FALLEN? ” Jones et al, JAMA Surgery, 2013
COMORBIDITY
Why is comorbidity relevant? • Discuss with the person next to you for a few minutes • How do you assess comorbidity in your clinical practice?
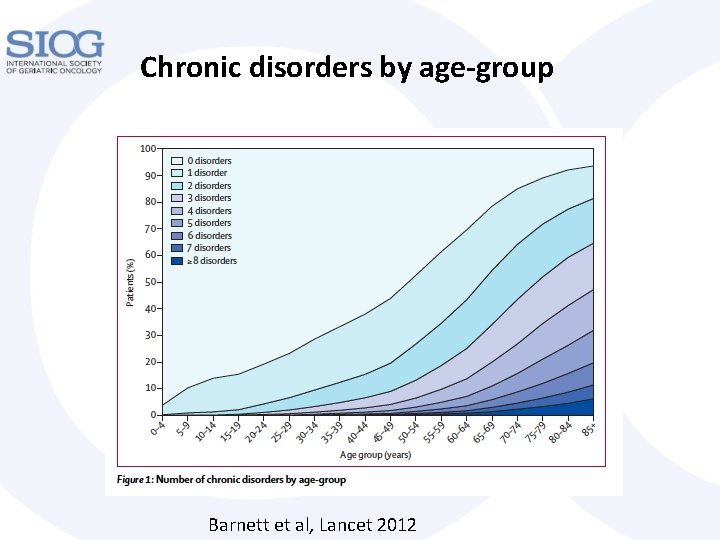
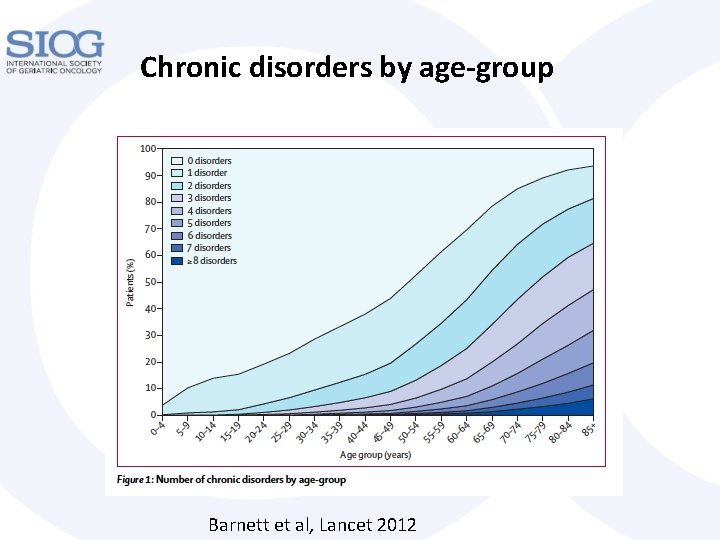
Chronic disorders by age-group Barnett et al, Lancet 2012
Optimization of comorbidities • Geriatrician? • Internal medicine specialist? • Subspecialist, i. e. cardiologist? • Core activity in the acute geriatric ward • Competing risks
Polypharmacy • Specific talk
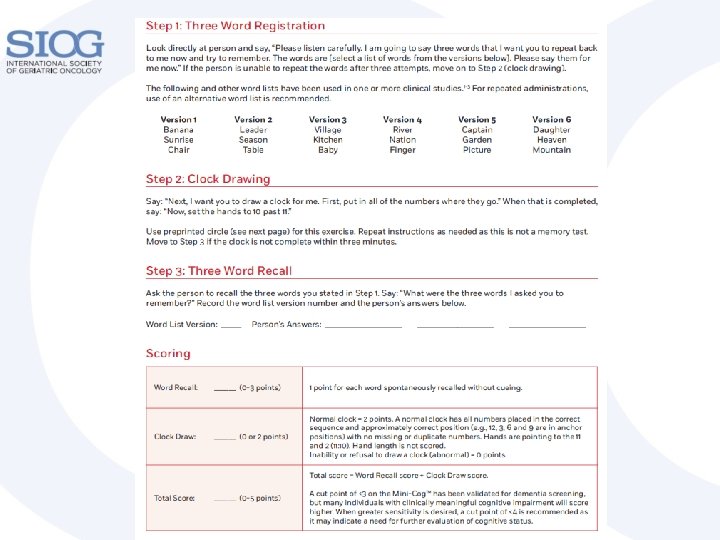
Cognitive function • Mild cognitive impairment • Dementia • Screening instruments, MMSE, MOCA, Mini. Cog • Why important?
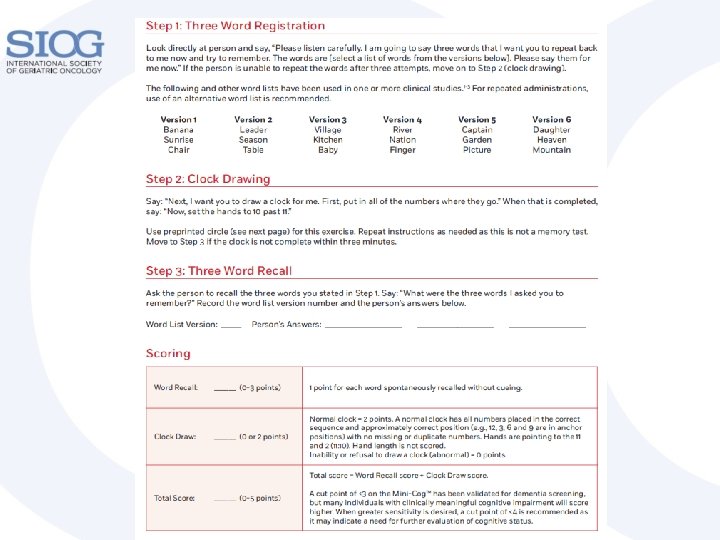
CLOCK-DRAWING TEST
Why important? • Consent, discussing preferences • Prognosis • Treatment planning, delirium • Baseline - chemobrain
NUTRITIONAL STATUS
Malnutrition • Differs between countries – in Norway malnutrition is the dominant problem • Tool: mini nutritional assessment (MNA) among others • Definite risk factor – but do interventions help? • How to intervene?
EMOTIONAL STATUS
Emotional function Depression, anxiety and distress Common among older people Common among cancer patients Risk factors are pain and physical distress Fear of impeding mortality Protective: Attachment security, self-esteem, sense of meaning and purpose • Treatment options? • • •
Study (depression)1 • Older cancer patients (>70) receiving chemotherapy (n=344) • 45% depressed • Risk factor: malnutrition at baseline 1 Duc et al. Psychooncology, 2016

SOCIAL SUPPORT
Social support • Fundamental for treatment planning • Population level – sociodemographic factors strong predictors for receiving treatment and survival • Caregivers may be frail • Patient may be main caregiver – influences motivation for treatment
GA COMPLETED – WHAT NOW?
Geriatric assessment 1 (GA) Shared decision-making Remaining life expectancy Detection of unidentified problems Prediction of adverse outcomes Treatment planning Baseline information Optimization before/during treatment Ongoing assessments necessary 1 Wildiers et al, JCO, 2014
SUMMARY • The heterogeneity increases with increasing age • We need to assess frailty rather than looking at chronological age alone when deciding treatment • Geriatric assessment provides a practical approach to older patients • GA is necessary in many older cancer patients for a number of reasons
THANK YOU FOR YOUR ATTENTION QUESTIONS?