Screening for Lung Cancer using Low Dose CT






- Slides: 37
Screening for Lung Cancer using Low Dose CT: State of the Art and Controversies Philippe GRENIER University Pierre et Marie Curie (UPMC), Pitié-Salpêtrière Hospital, Paris, FRANCE
Rationale for lung cancer screening Lung cancer remains the leading cause of cancerrelated death among men and women in the world The 5 -year survival rate of 10 -15% has been roughly unchanged for the past two decades despite treatment advances At diagnosis, most lung cancers are already at advanced stage Mountain. Chest; 1997. 111: 1710 Strauss. Surg Oncol Clin N Am 1999; 8: 747
Rationale for lung cancer screening Early stage lung cancer patients have a much higher 5 -year survival rate (between 60 and 80%) Changing smoking habits could reduce lung cancer incidence and deaths Cessation programs have long-term cessation rates of only 20% to 35% at one year The risk for lung cancer does not decrease for many years after smoking cessation Pisters. J Clin Oncol 2005; 23: 3270
Lung Cancer Screening with Chest Radiography with or without Sputum Cytologic Examination Some lower-quality evidence (case-control studies) has shown benefit Higher-quality evidence (randomized controled trials) conducted in the 80’s has not (the screened groups had the same number of death from lung cancer as the control group) Humphrey. Ann Intern Med 2004; 140: 740
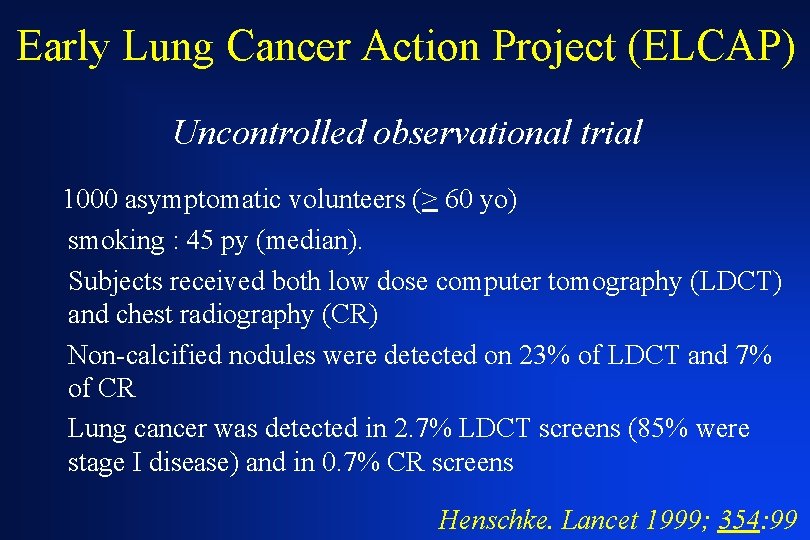
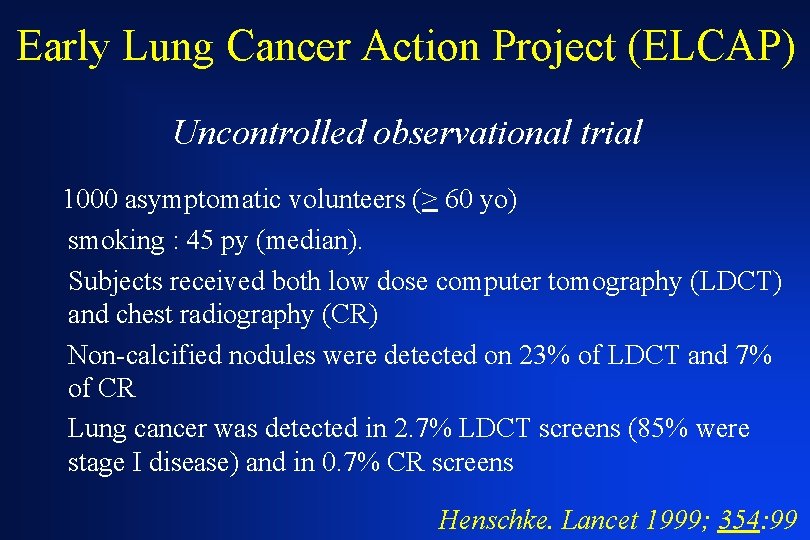
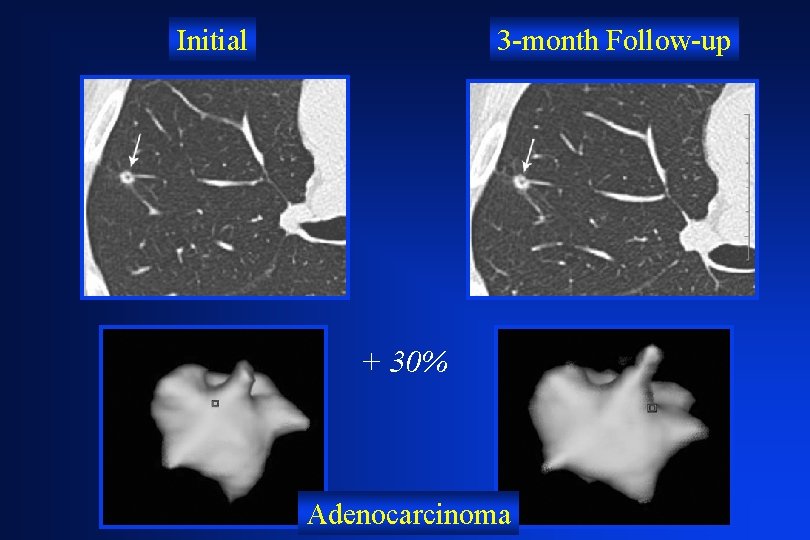
Early Lung Cancer Action Project (ELCAP) Uncontrolled observational trial 1000 asymptomatic volunteers (> 60 yo) smoking : 45 py (median). Subjects received both low dose computer tomography (LDCT) and chest radiography (CR) Non-calcified nodules were detected on 23% of LDCT and 7% of CR Lung cancer was detected in 2. 7% LDCT screens (85% were stage I disease) and in 0. 7% CR screens Henschke. Lancet 1999; 354: 99
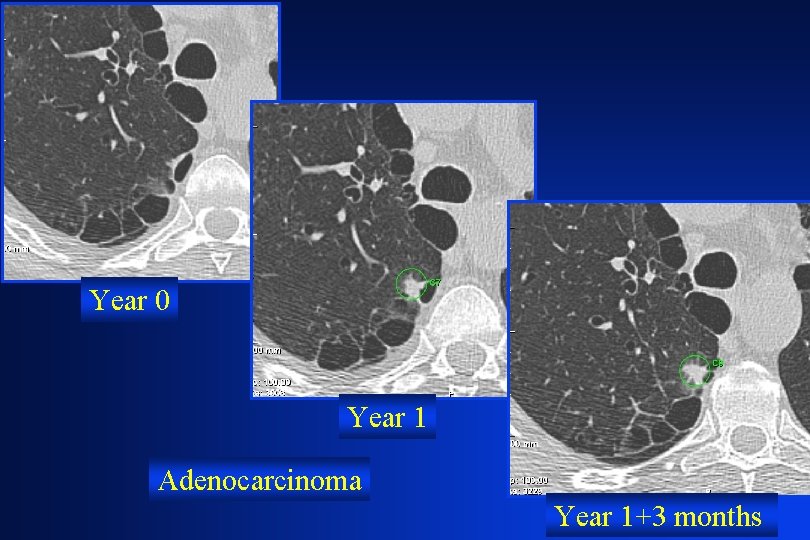
Year 0 Year 1 Adenocarcinoma Year 1+3 months
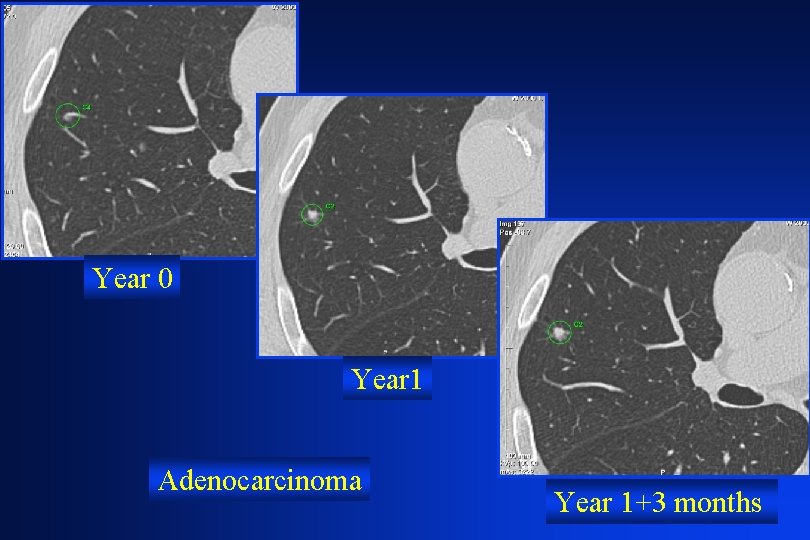
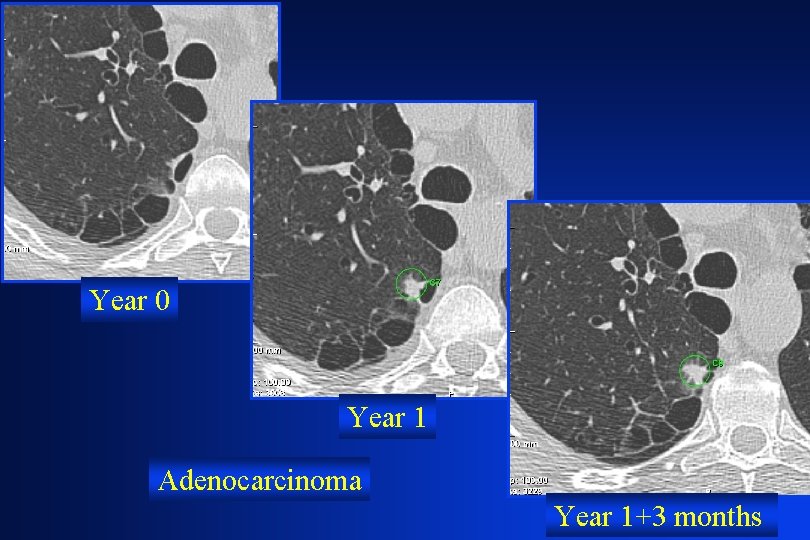
Year 0 Year 1 Adenocarcinoma Year 1+3 months
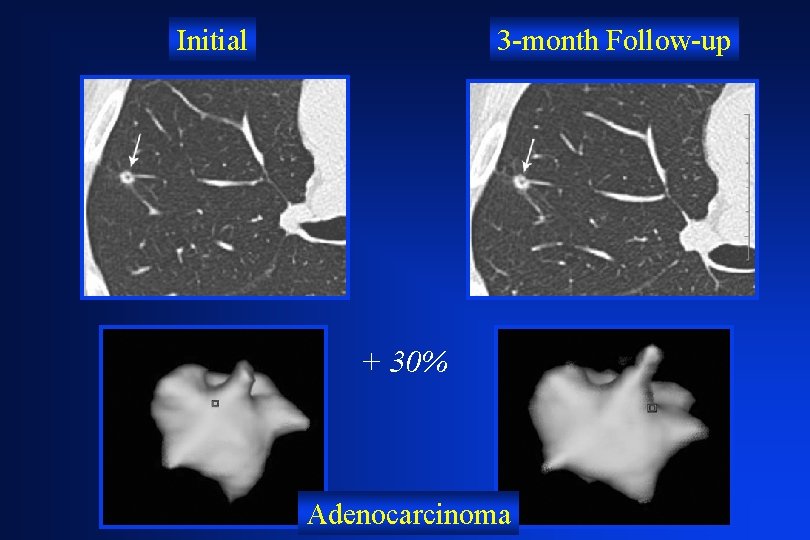
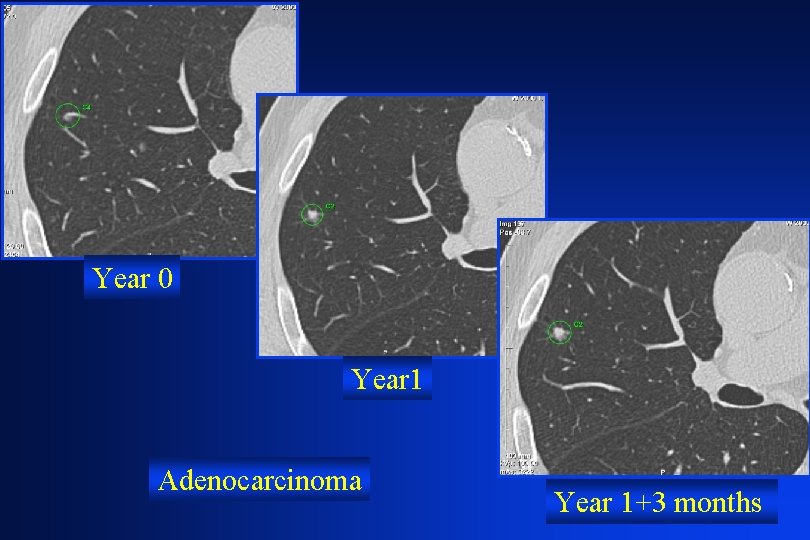
Initial 3 -month Follow-up + 30% Adenocarcinoma
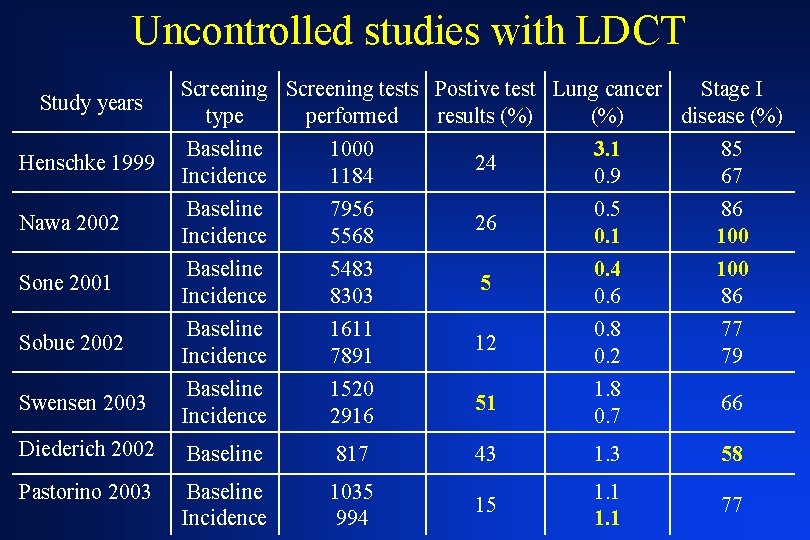
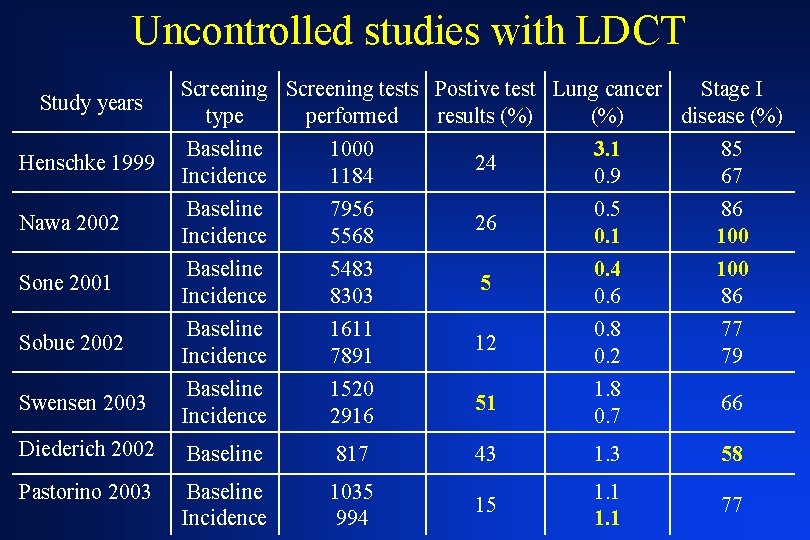
Uncontrolled studies with LDCT Study years Screening tests Postive test Lung cancer Stage I type performed results (%) disease (%) Henschke 1999 Baseline Incidence 1000 1184 24 3. 1 0. 9 85 67 Nawa 2002 Baseline Incidence 7956 5568 26 0. 5 0. 1 86 100 Sone 2001 Baseline Incidence 5483 8303 5 0. 4 0. 6 100 86 Sobue 2002 Baseline Incidence 1611 7891 12 0. 8 0. 2 77 79 Swensen 2003 Baseline Incidence 1520 2916 51 1. 8 0. 7 66 Diederich 2002 Baseline 817 43 1. 3 58 Pastorino 2003 Baseline Incidence 1035 994 15 1. 1 77
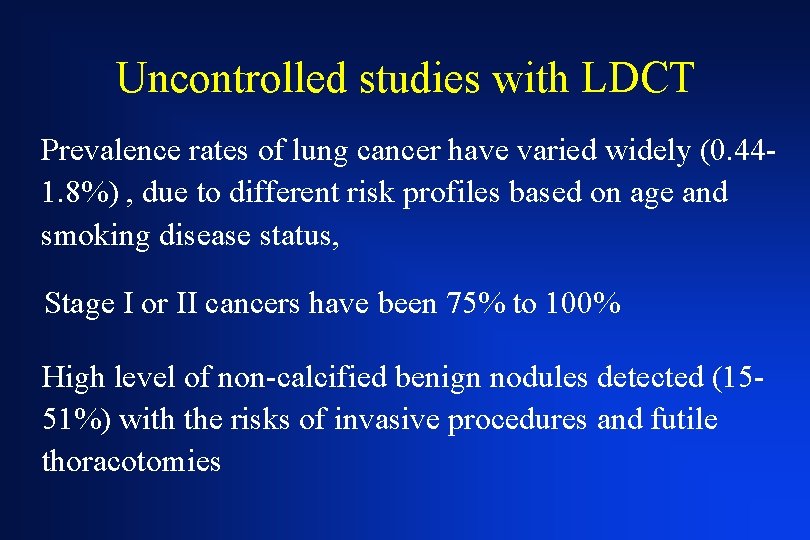
Uncontrolled studies with LDCT Prevalence rates of lung cancer have varied widely (0. 441. 8%) , due to different risk profiles based on age and smoking disease status, Stage I or II cancers have been 75% to 100% High level of non-calcified benign nodules detected (1551%) with the risks of invasive procedures and futile thoracotomies
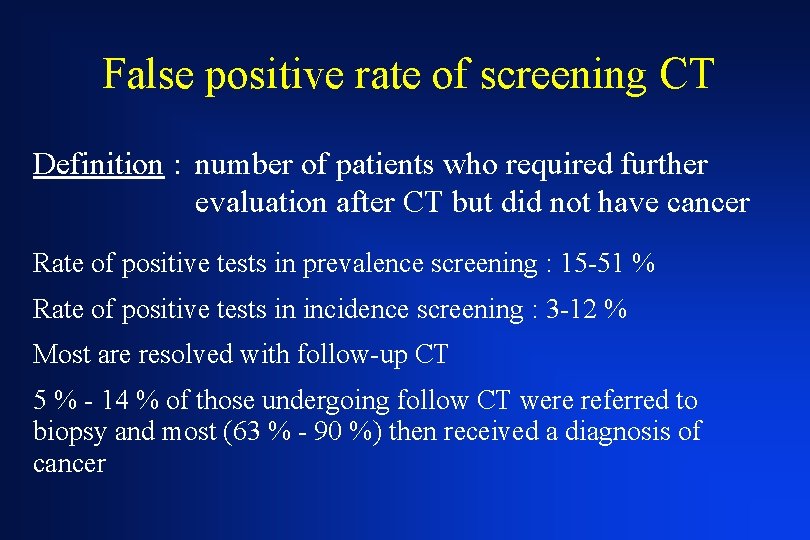
False positive rate of screening CT Definition : number of patients who required further evaluation after CT but did not have cancer Rate of positive tests in prevalence screening : 15 -51 % Rate of positive tests in incidence screening : 3 -12 % Most are resolved with follow-up CT 5 % - 14 % of those undergoing follow CT were referred to biopsy and most (63 % - 90 %) then received a diagnosis of cancer
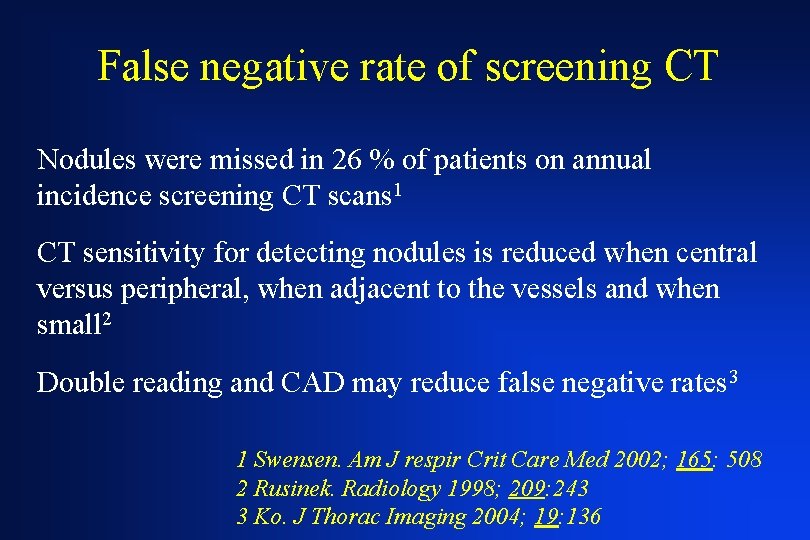
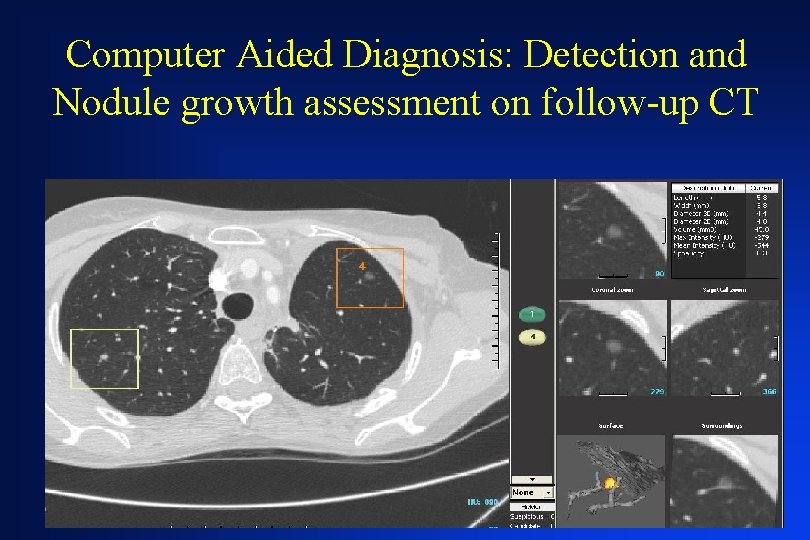
False negative rate of screening CT Nodules were missed in 26 % of patients on annual incidence screening CT scans 1 CT sensitivity for detecting nodules is reduced when central versus peripheral, when adjacent to the vessels and when small 2 Double reading and CAD may reduce false negative rates 3 1 Swensen. Am J respir Crit Care Med 2002; 165: 508 2 Rusinek. Radiology 1998; 209: 243 3 Ko. J Thorac Imaging 2004; 19: 136
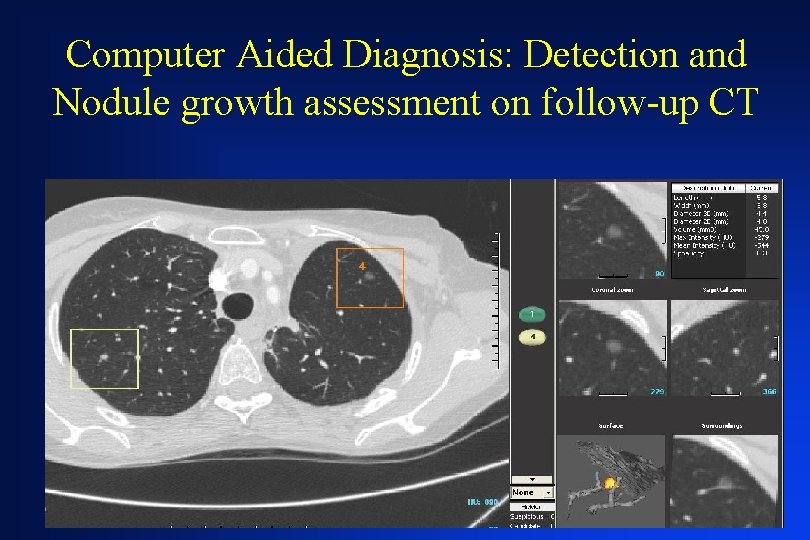
Computer Aided Diagnosis: Detection and Nodule growth assessment on follow-up CT

Strategy for indeterminate nodule (more than 50 y. o. smoker) Size < 4 mm 4 - 8 mm > 8 mm CT Follow-up* 12 months CT Follow-up* 3 -6, 6 -9, 9 -12, 12 -24 months Biopsy or resection Mc. Mahon. Radiology. 2005 ; 237: 395 -400 Alternative: FDG-PET or contrast enhanced CT + Biopsy or resection

Survival of patients with stage I lung cancer detected on CT screening 31, 567 asymptomatic persons at risk for lung cancer were screened using LDCT (1993 -2005) 412/484 (85%) had clinical stage I lung cancer and estimated 10 -year survival rate was 88% Among 302/412 who underwent surgical resection within 1 month after diagnosis, the 10 -year survival rate was 92% The 8 participants with clinical stage I who did not receive treatment died within 5 years after diagnosis Henschke. N Engl J Med. 2006; 355: 1763
Are Increasing 5 -Year Survival Rates Evidence of Success Against Cancer? There is little correlation between the change in 5 -year survival for a specific tumor and the change in tumorrelated mortality The change in 5 -year survival is positively correlated with the change in the tumor incidence rate Welch. JAMA; 2000; 283: 2975
Uncontrolled studies with LDCT Lung cancer can be diagnosed at a significantly earlier stage with CT screening. However whether this will translate to a mortality benefit is unclear
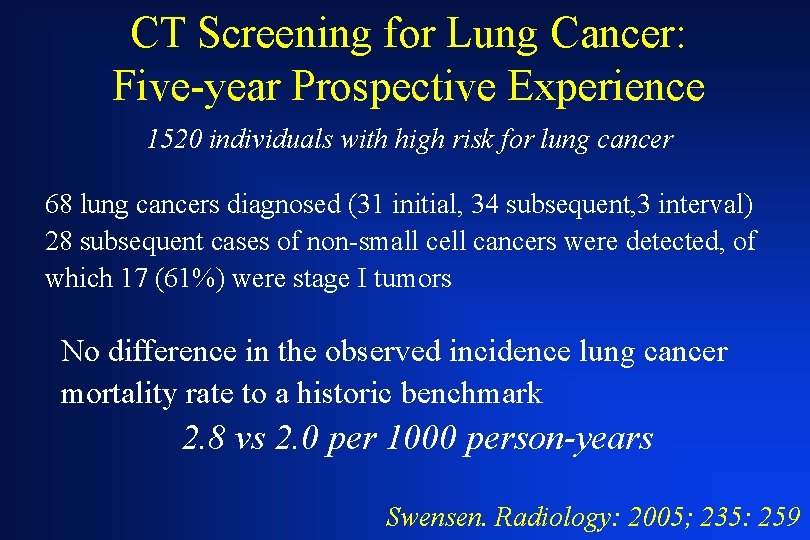
CT Screening for Lung Cancer: Five-year Prospective Experience 1520 individuals with high risk for lung cancer 68 lung cancers diagnosed (31 initial, 34 subsequent, 3 interval) 28 subsequent cases of non-small cell cancers were detected, of which 17 (61%) were stage I tumors No difference in the observed incidence lung cancer mortality rate to a historic benchmark 2. 8 vs 2. 0 per 1000 person-years Swensen. Radiology: 2005; 235: 259

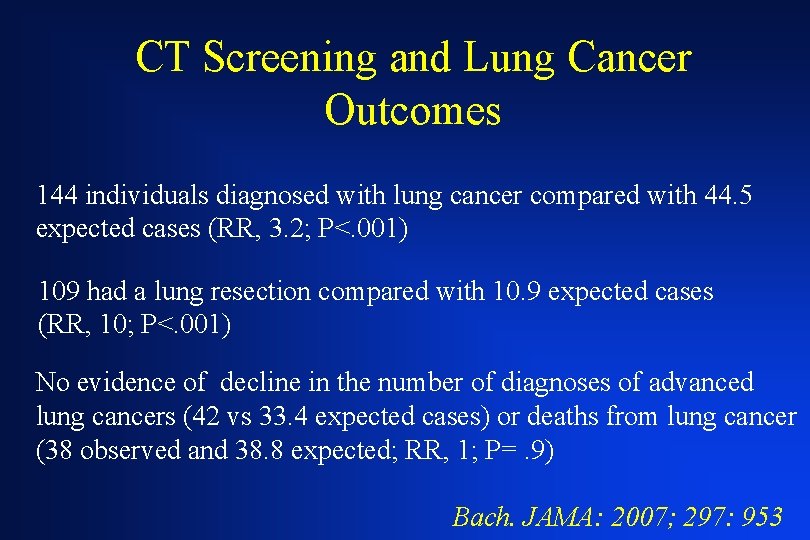
CT Screening and Lung Cancer Outcomes Longitudinal analysis of 3246 individuals current or former smokers screened for lung cancer in academic centers with a follow-up of 3. 9 years Comparison of predicted with observed number of new lung cancer cases, lung cancer resections, advanced lung cancer cases, and deaths from lung cancer Bach. JAMA: 2007; 297: 953
CT Screening and Lung Cancer Outcomes 144 individuals diagnosed with lung cancer compared with 44. 5 expected cases (RR, 3. 2; P<. 001) 109 had a lung resection compared with 10. 9 expected cases (RR, 10; P<. 001) No evidence of decline in the number of diagnoses of advanced lung cancers (42 vs 33. 4 expected cases) or deaths from lung cancer (38 observed and 38. 8 expected; RR, 1; P=. 9) Bach. JAMA: 2007; 297: 953
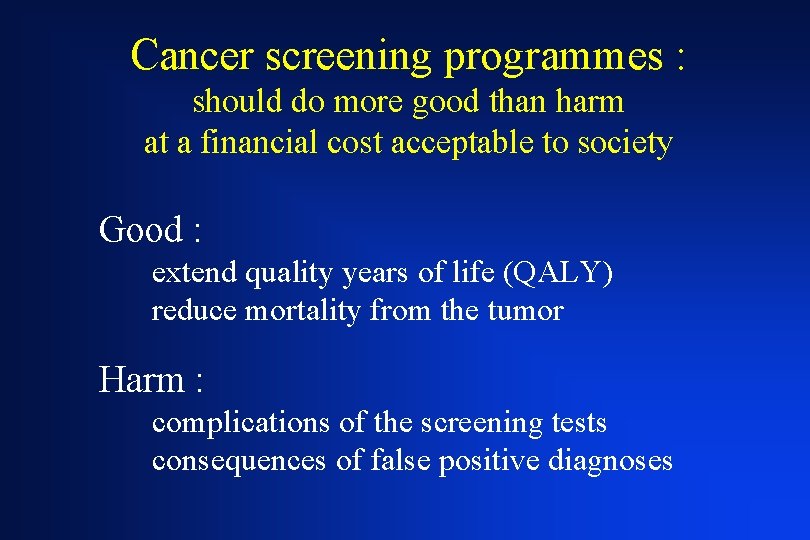
Cancer screening programmes : should do more good than harm at a financial cost acceptable to society Good : extend quality years of life (QALY) reduce mortality from the tumor Harm : complications of the screening tests consequences of false positive diagnoses

Lead-Time Bias Survival time Time Screened group Diagnosis confirmed Patient dies Lead time Survival time Time Control group Symptoms Diagnosis confirmed Patient dies
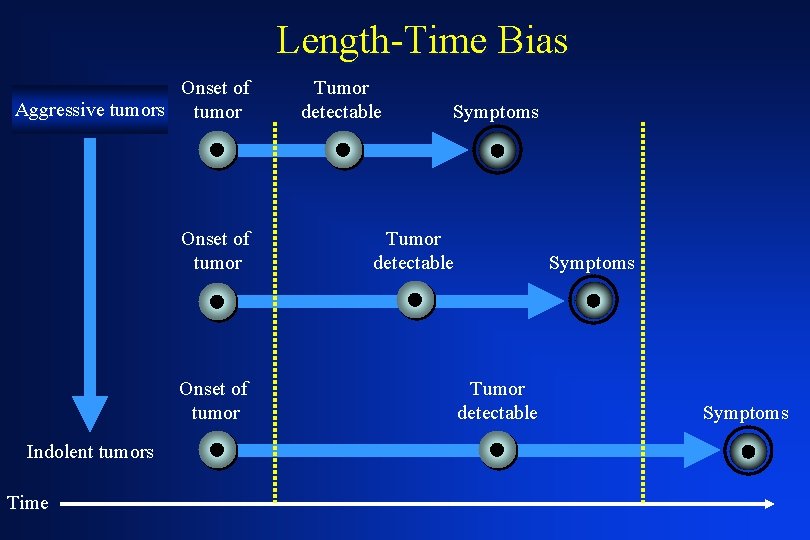
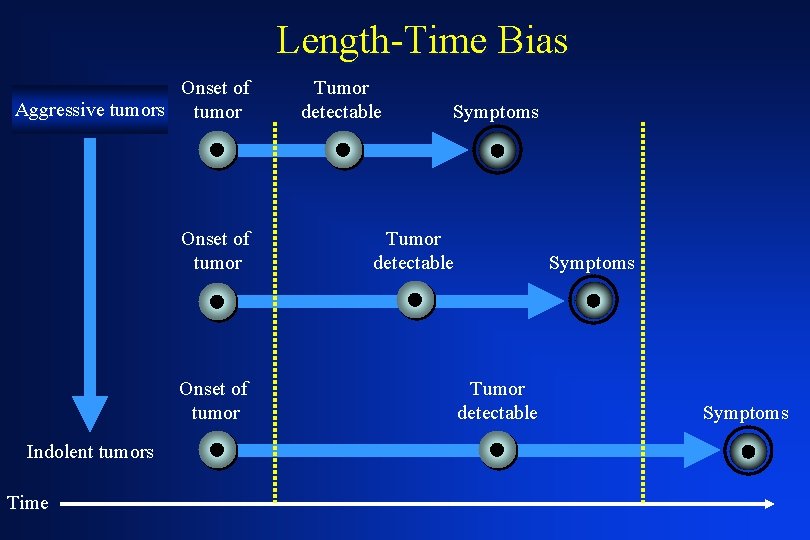
Length-Time Bias Onset of Aggressive tumors tumor Onset of tumor Indolent tumors Time Tumor detectable Symptoms
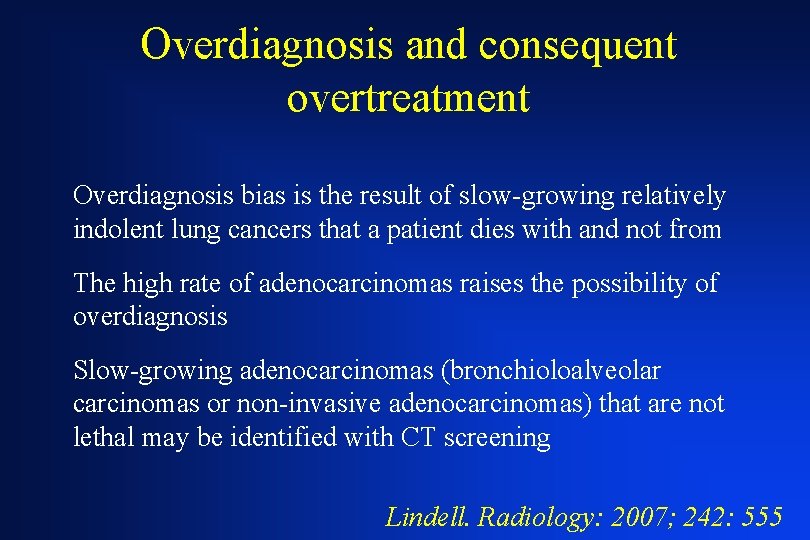
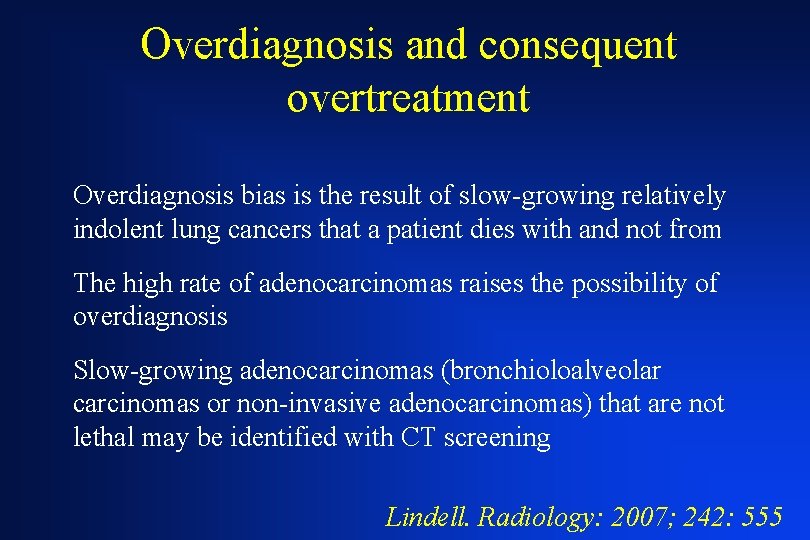
Overdiagnosis and consequent overtreatment Overdiagnosis bias is the result of slow-growing relatively indolent lung cancers that a patient dies with and not from The high rate of adenocarcinomas raises the possibility of overdiagnosis Slow-growing adenocarcinomas (bronchioloalveolar carcinomas or non-invasive adenocarcinomas) that are not lethal may be identified with CT screening Lindell. Radiology: 2007; 242: 555

Non solid nodules: malignant causes Ground glass opacity Adenocarcinoma Bronchioloalveolar cell carcinoma
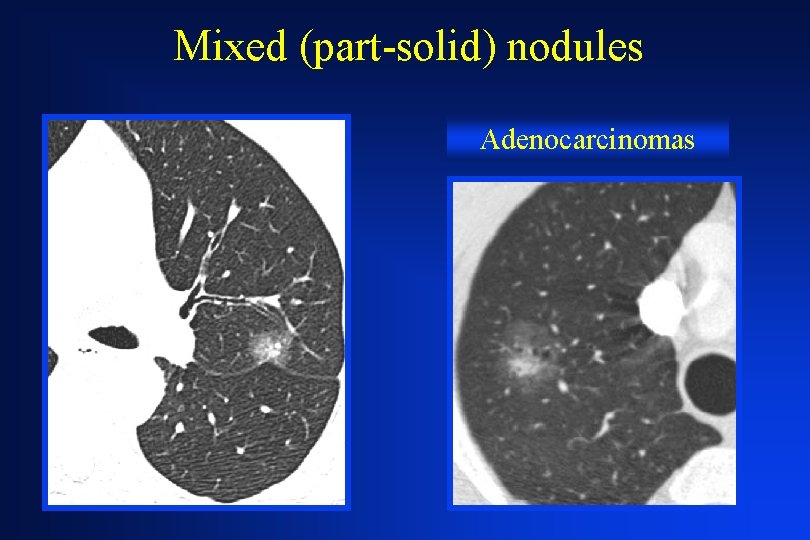
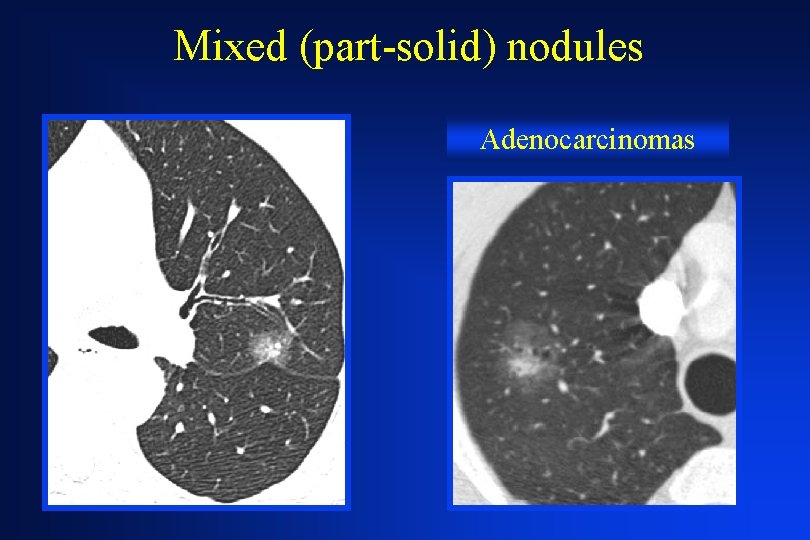
Mixed (part-solid) nodules Adenocarcinomas
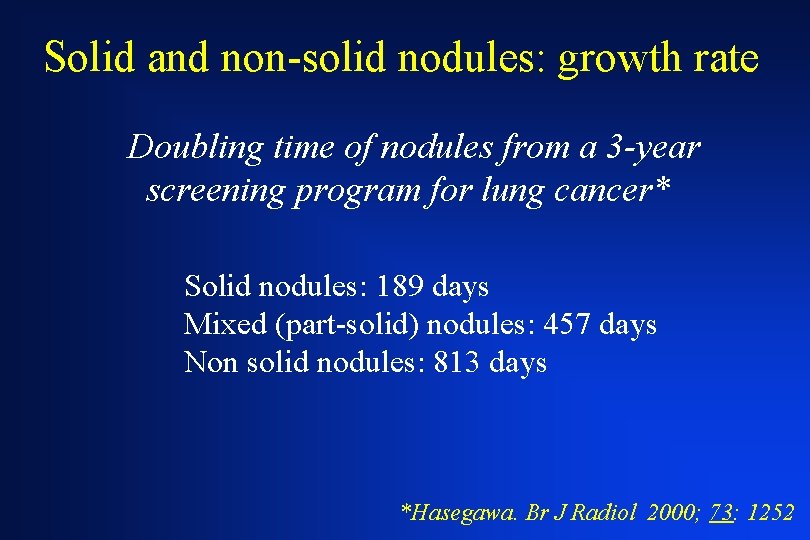
Solid and non-solid nodules: growth rate Doubling time of nodules from a 3 -year screening program for lung cancer* Solid nodules: 189 days Mixed (part-solid) nodules: 457 days Non solid nodules: 813 days *Hasegawa. Br J Radiol 2000; 73: 1252
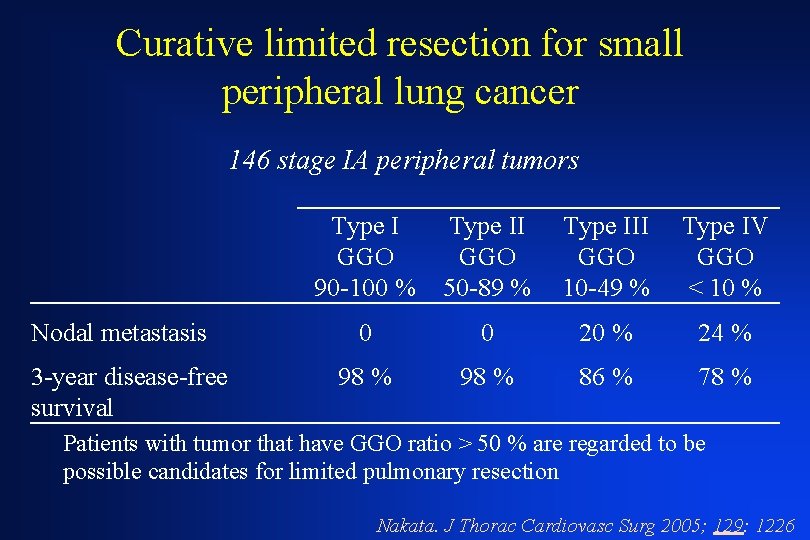
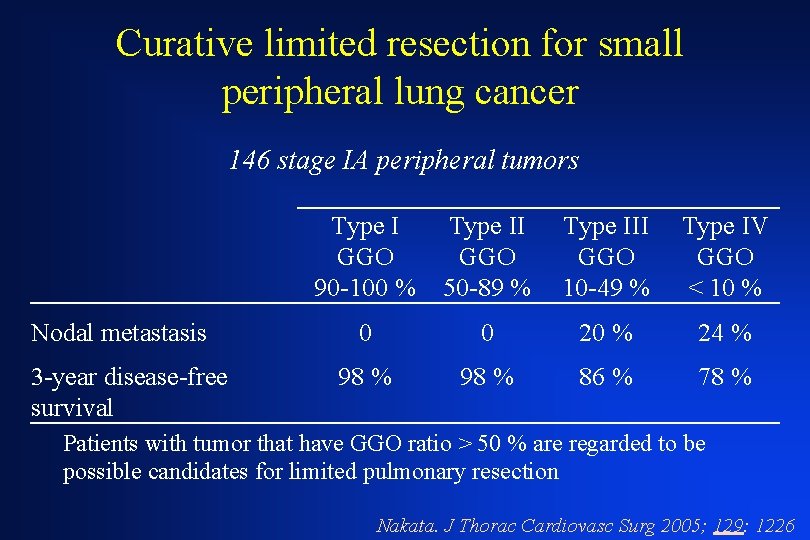
Curative limited resection for small peripheral lung cancer 146 stage IA peripheral tumors Nodal metastasis 3 -year disease-free survival Type I GGO 90 -100 % Type II GGO 50 -89 % Type III GGO 10 -49 % Type IV GGO < 10 % 0 0 20 % 24 % 98 % 86 % 78 % Patients with tumor that have GGO ratio > 50 % are regarded to be possible candidates for limited pulmonary resection Nakata. J Thorac Cardiovasc Surg 2005; 129: 1226

Overdiagnosis: a Substantial Concern in Lung Cancer Screening 61 cancers reviewed and 48 assessed for morphologic change Mean tumor size: 16. 4 mm (5. 5 -52. 5 mm) 74% prevalence, 37% incidence detected lung cancers were adenocarcinomas Mean volume doubling time (VDT) was 518 days 13/48 (27%) cancers had a VDT longer than 400 days (11/13 were in women) Lindell. Radiology: 2007; 242: 555
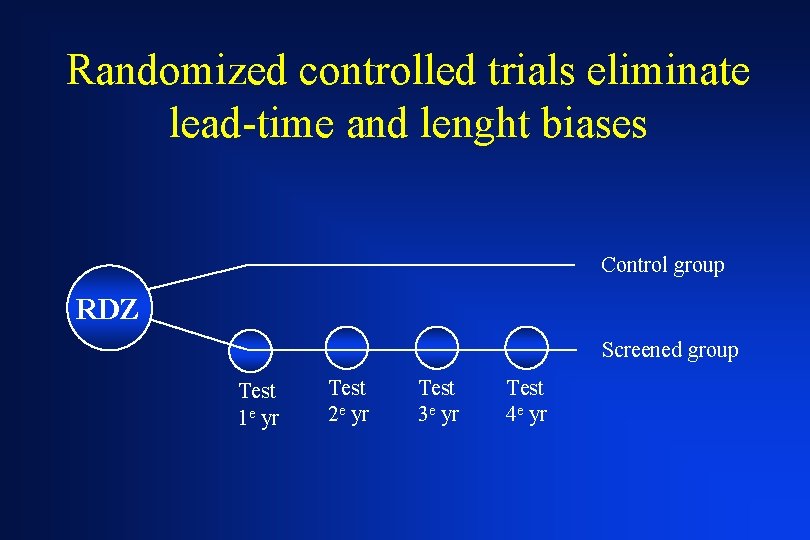
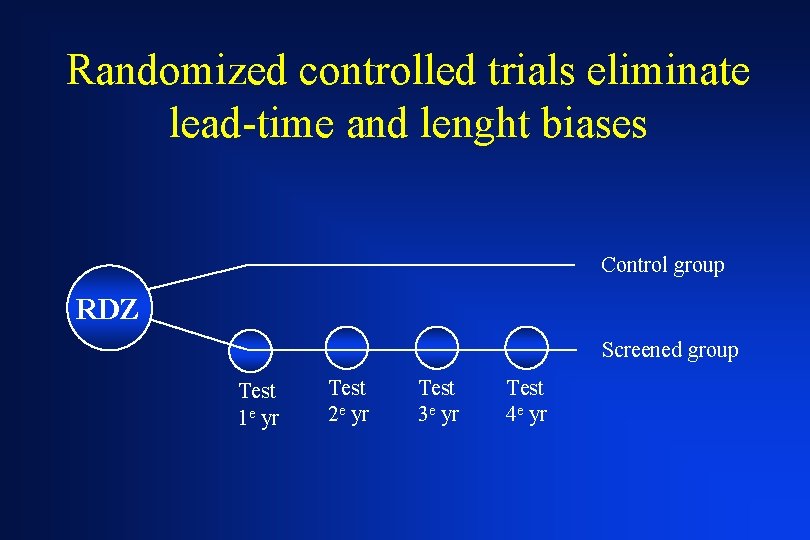
Randomized controlled trials eliminate lead-time and lenght biases Control group RDZ Screened group Test 1 e yr Test 2 e yr Test 3 e yr Test 4 e yr
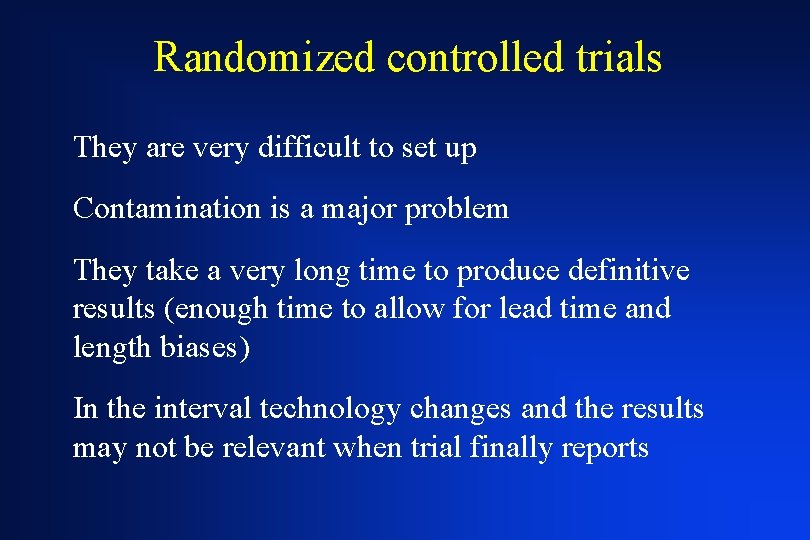
Randomized controlled trials They are very difficult to set up Contamination is a major problem They take a very long time to produce definitive results (enough time to allow for lead time and length biases) In the interval technology changes and the results may not be relevant when trial finally reports
Lung Cancer Study: a randomized controlled trial (LDCT vs CR) 3, 318 tobacco-exposed subjects Compliance at baseline was 96% in the LDCT arm and 93% in the CR arm At year one screening compliance was 86% in the LDCT arm and 80% in the CR arm Gohagan. Chest 2004; 126: 114
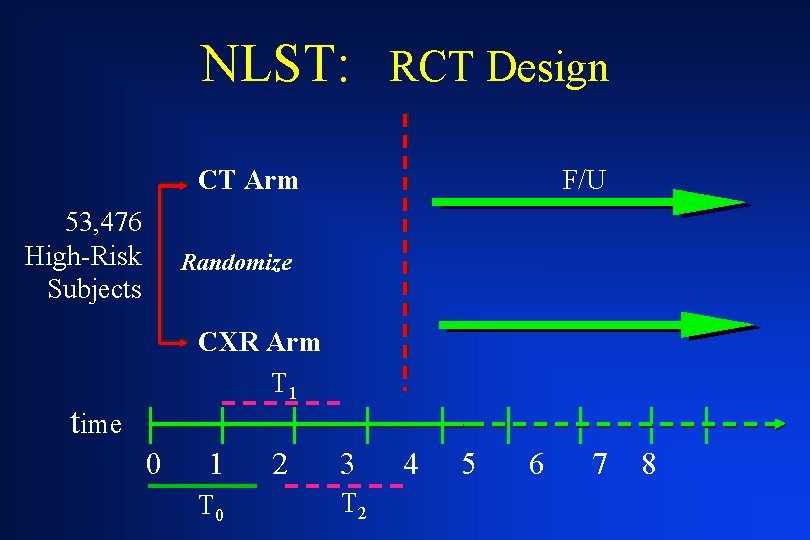
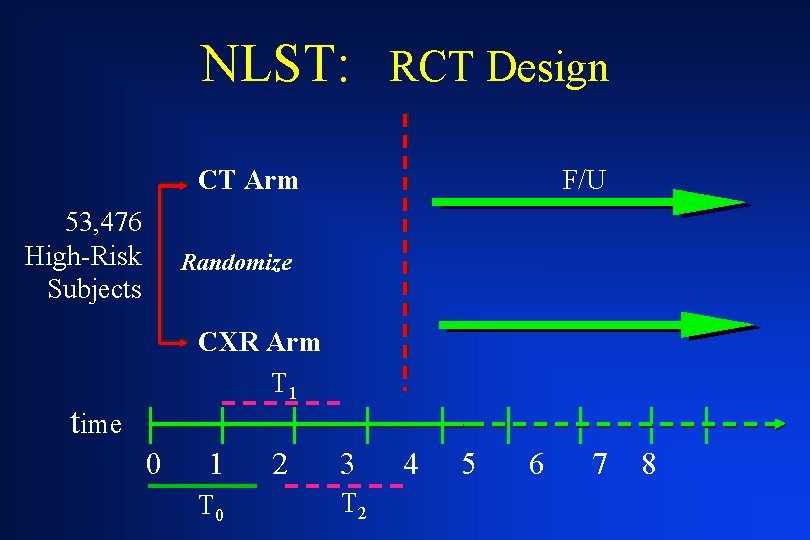
NLST: RCT Design CT Arm 53, 476 High-Risk Subjects F/U Randomize CXR Arm T 1 time 0 1 T 0 2 3 T 2 4 5 6 7 8
The NELSON Trial 15, 428 subjects LDCT screened arm is beeing compared to a control arm without screening Van Iersel. Int J Cancer 2007; 120: 868
Conclusion Screening for lung cancer with LDCT may increase the rate of lung cancer diagnosis and treatment, but may not meaningfully reduce the risk of advanced lung cancer or death from lung cancer Until more conclusive data are available, asymptomatic individuals should not be screened outside of clinical research studies
Conclusion Randomized controlled trials are the only way to reliably determine whether screening does more good than harm Although expensive and time-consuming, rigorous trials of cancer screening are far more cost-effective than widespread adoption of costly screening interventions that cause more harm than good Welch. Arch Intern Med; 2007; 167: 2289
Genetic abnormalities and biomarkers of premalignancy or early malignancy Genomic and proteomic methods may offer a much easier mass screening as the first step of a screening strategy Detection of biomarkers will have profound implications for more precise selection and stratification of population at risk for lung cancer Meyerson. J Clin Oncol. 2005; 23: 3219 Zhong. Am J Respir Crit Care Med. 2005; 172: 1308 Field. J Thorac Oncol. 2006; 1: 497