Scottish Patient Safety Programme in Primary Care SPSP




- Slides: 32
Scottish Patient Safety Programme in Primary Care (SPSP – PC) Implementation & Spread Strategy 2013– 2018
The Who, What and How? • Outline key elements of the SPSP – PC Implementation and Spread strategy, including: • Focus • Programme Aims • What are we spreading? • Rate of spread • Methodology • Infrastructure: • Contractual Levers • NHS Boards • Questions and Feedback
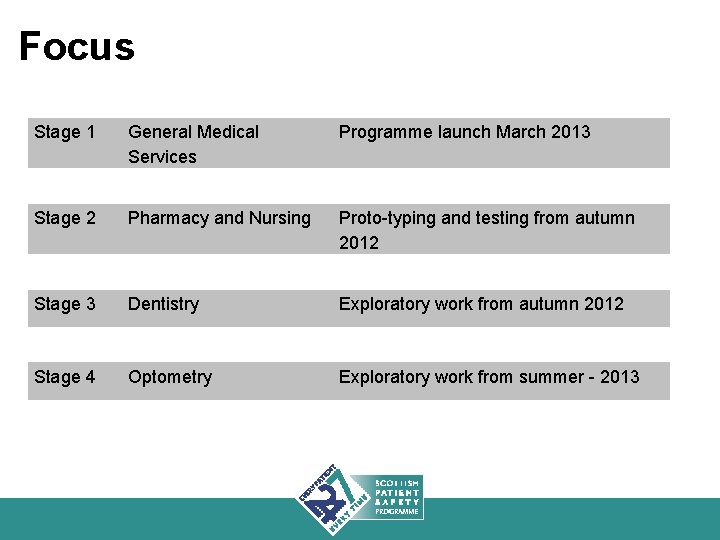
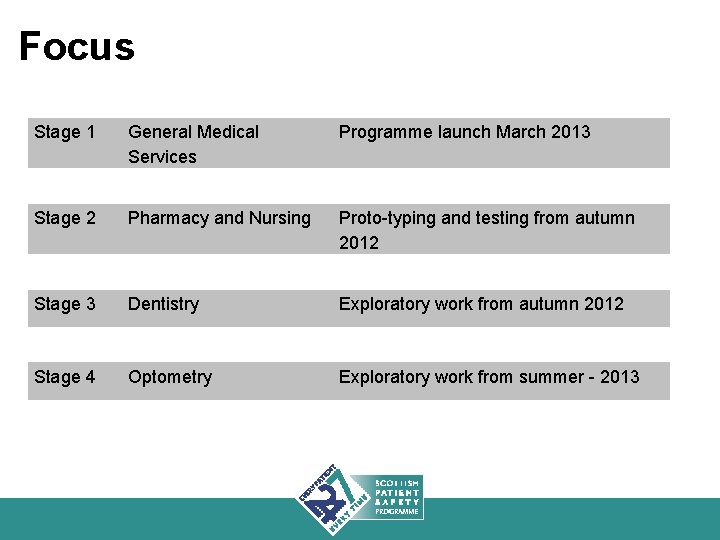
Focus Stage 1 General Medical Services Programme launch March 2013 Stage 2 Pharmacy and Nursing Proto-typing and testing from autumn 2012 Stage 3 Dentistry Exploratory work from autumn 2012 Stage 4 Optometry Exploratory work from summer - 2013
Programme Aims • To reduce the number of events which could cause avoidable harm to people from healthcare delivered in any primary care setting. • All NHS territorial boards and 95% of primary care clinical teams will be developing their safety culture and achieving reliability in 3 high-risk areas by 2018.
What are we spreading? 3 Workstreams: • Safety Culture and Leadership • Safer Medicines • Safe and reliable patient care within practice and across the interface
Safety Culture and Leadership Aim: To develop a safety culture that engages with patients to support the delivery of safe and reliable care in primary care teams. • Increase awareness of safety issues within practice, through practice teams undertaking Safety Climate Survey’s. • Practices identify, reduce and learn from adverse events identified through trigger tool, SEA’s and adverse event reporting. • Safety walkrounds to ensure Safety in Primary Care is embedded within the NHS Board safety agenda.
Safer Medicines Aim: To Provide Safe and Effective Medicines Management in Primary Care • Implement systems for reliable prescribing and monitoring of warfarin, methotrexate and azathioprine. • Practices have safe and reliable systems for medicines reconciliation following discharge. • Implement systems for safe and reliable insulin administration. • Implement systems to support reliable prescribing and monitoring of high risk medications in community pharmacy. • Use existing electronic data to support targeted application of clinical judgment to reduce high risk prescribing.
Safe and reliable patient care within practice and across the interface Aim: To provide safe and reliable patient care across the interface and at home. • GP practices have safe and reliable systems for handling written communication received from external sources • Health Boards and GP practices have safe and reliable results handling systems • • • Reduce harm from pressure ulcers Reduce harm from falls Reduce incidence of catheter-associated urinary tract infection
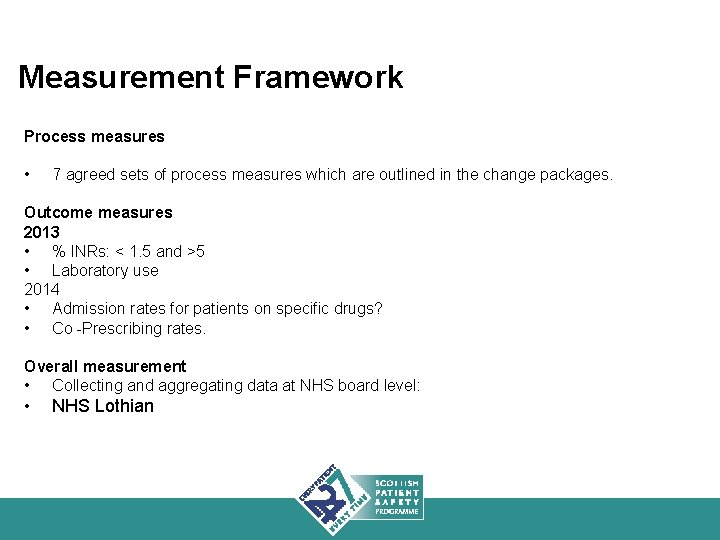
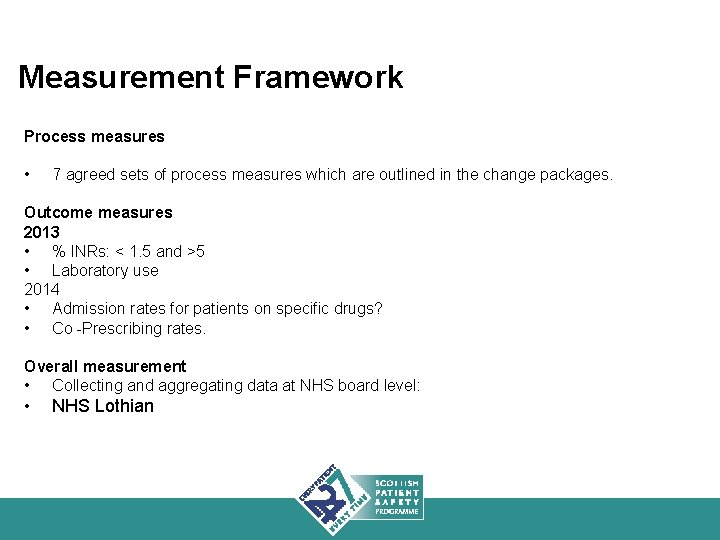
Measurement Framework Process measures • 7 agreed sets of process measures which are outlined in the change packages. Outcome measures 2013 • % INRs: < 1. 5 and >5 • Laboratory use 2014 • Admission rates for patients on specific drugs? • Co -Prescribing rates. Overall measurement • Collecting and aggregating data at NHS board level: • NHS Lothian
Rate of Spread: • Not all at once • Menu • Build over time • Practices and boards prioritise
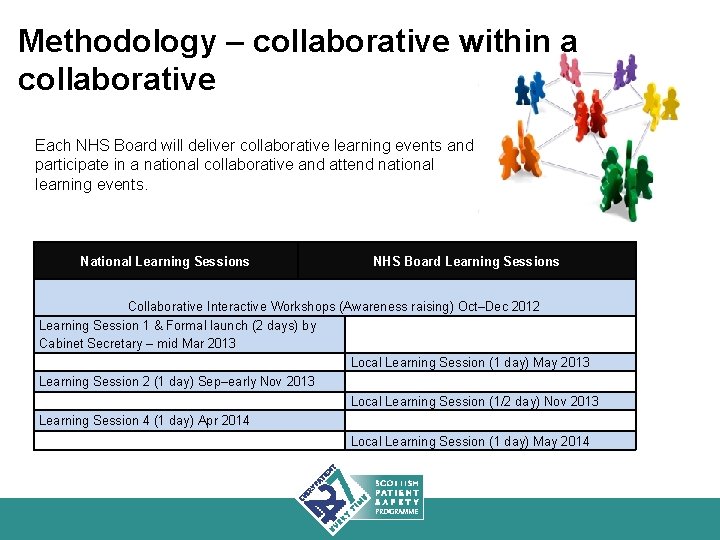
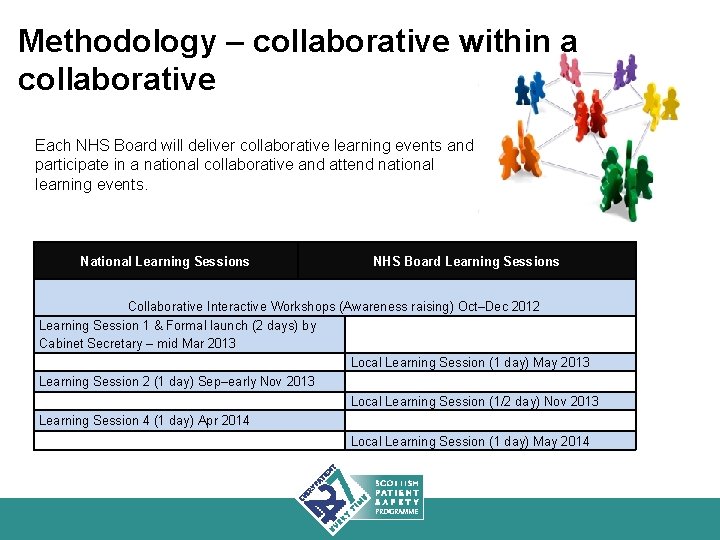
Methodology – collaborative within a collaborative Each NHS Board will deliver collaborative learning events and participate in a national collaborative and attend national learning events. National Learning Sessions NHS Board Learning Sessions Collaborative Interactive Workshops (Awareness raising) Oct–Dec 2012 Learning Session 1 & Formal launch (2 days) by Cabinet Secretary – mid Mar 2013 Local Learning Session (1 day) May 2013 Learning Session 2 (1 day) Sep–early Nov 2013 Local Learning Session (1/2 day) Nov 2013 Learning Session 4 (1 day) Apr 2014 Local Learning Session (1 day) May 2014

Successful implementation needs. . . • Commitment of Boards, HIS and SGHD • Build on the professionalism of front line staff • Prioritised within existing and adapted contracts • Alignment with GP Appraisal and Revalidation
SGHD and HIS Health Boards GP Practices
Healthcare Improvement Scotland will provide: • • • National Leadership and Influence Tools Guidance National collaborative Expertise Support
Boards need to provide … Executive buy in and championing To Prioritise this programme Dedicated programme management, clinical leadership and QI support to: • Run the collaborative • Build knowledge and skills • Support practices
What’s in it for boards? • • Fewer adverse events Fewer Admissions Safe effective prescribing Fewer Falls/ UTIs/Pressure ulcers • Improved Interface working – SPSP • Engagement with Primary care
Adverse events in primary care in NHS Scotland cause: • 39, 000 Admissions pa • 21, 000 pa admissions are drug side effect related • 14, 000 pa preventable • 6, 500 from Warfarin, NSAIDS, Diuretic, Antiplatelets alone Based on 327, 000 acute medical emergency admissions 2010/11 - ISD Howard et al Br J pharmacology 2006 Howard et al qshc 2003
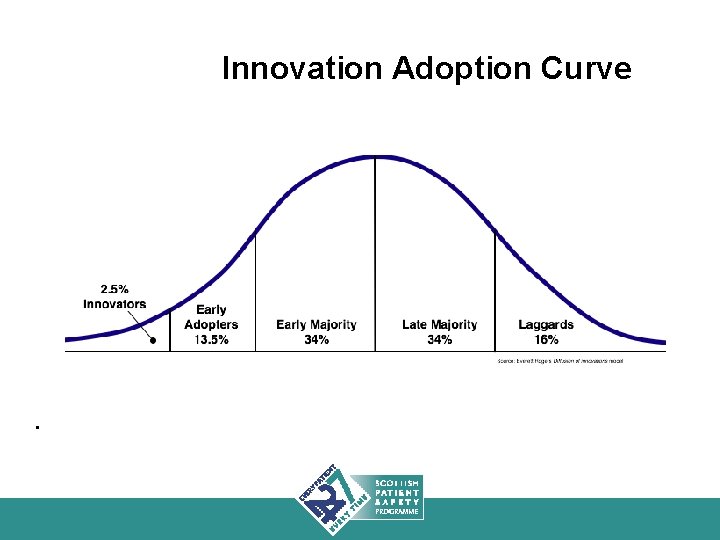
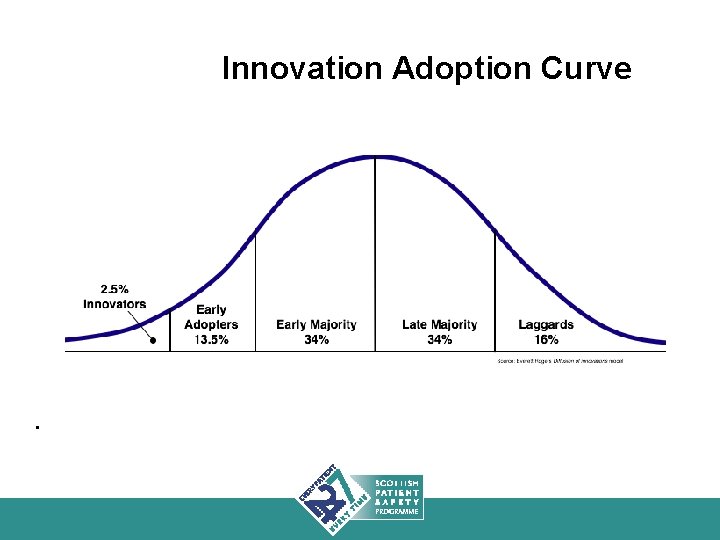
Innovation Adoption Curve .
What’s in it for Clinicians Doing the best for your patients Working better as a team More confidence in your systems Less things going wrong Less stress More Efficient Better Interface working


Revalidation • Safety core to revalidation and GMC guidance • Bundles, Trigger Tool and Climate Survey evidence for GP appraisal
Enhanced Service - 5 years To support Improvement in key areas of the programme • Attending Collaborative Learning Event • Data collection and improvement 1 high risk process per annum • Trigger Tool Review (25 records biannually) • Safety Climate Survey annually Safety as Core in Scottish Focussed Contract
Alignment • • Productive General Practice Medical Defence organisations – MDDUS GP training Prescribing initiatives
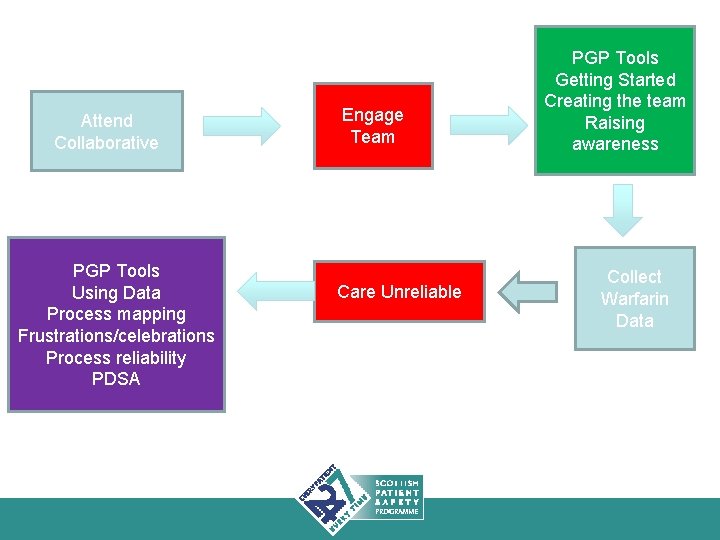
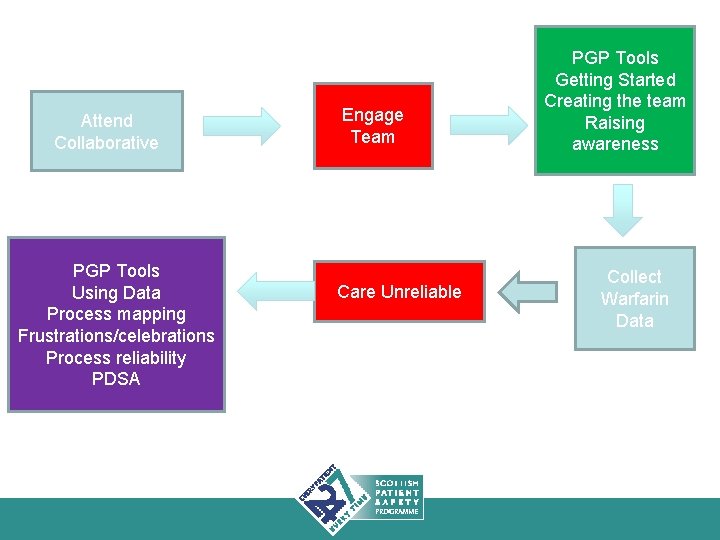
Attend Collaborative PGP Tools Using Data Process mapping Frustrations/celebrations Process reliability PDSA Engage Team Care Unreliable PGP Tools Getting Started Creating the team Raising awareness Collect Warfarin Data
And for Patients… Better Informed Better Understanding More in control of health Actively engaged in improving services More confident in systems More reliable care Less chance of being harmed/ admitted Better QOL

Why wouldn’t we?
Discussion • • What challenges do you anticipate? What benefits do you see? How does this align with: Current board objectives and activities? • Questions?