School of Health Sciences Disability and Social Inclusion
School of Health Sciences Disability and Social Inclusion seminar The role of peer workers in mental health services: opportunities and challenges Steve Gillard steven. gillard@city. ac. uk Professor of Mental Health Research School of Health Sciences City, University London
Overview • What is peer support? • Peer support and mental health services • The evidence base for peer support • Challenges of implementing peer support into practice • The ENRICH trial of peer support for discharge • Implications for practice and research…
Peer support is something that occurs naturally; it is what many people do when they recognise a shared experience of adversity and come together to support each other. (Pinto da Costa et al. 2019)
The organisation of peer support Alcoholics Anonymous and other 12 -step programmes (Ferri et al. 2006) • ‘Helper therapy principle’ (Reissman 1965) Service user/ survivor movement • 1970 s → citizen advocacy and campaigning (Mead & Macneil 2005) Self-help movement • E. g. Hearing Voices network (Dillon & Longden 2011)
Peer support in the voluntary sector From peer-led peer support… • Leeds Survivor Led Crisis Service www. lslcs. org. uk/ • Canerows user-led ward visiting and post-discharge support https: //canerows. co. uk/ … to large national providers • Together for Mental Wellbeing www. together-uk. org/peer -support/ • Mind www. mind. org. uk/information-support/drugs-andtreatments/peer-support/

What is peer support? Strong values base to peer support that makes it distinctive from other forms of mental health support • Intentional Peer Support (Mead 2008) 1. both parties ‘invited to learn and grow’ 2. focus on relationship and community rather than individual change alone • O’Hagan et al (2009) 1. equal power relationships (choice and control over engaging with peer support) 2. identification with each other (sense of mutuality) 3. confirming the validity of personal experience
Peer support in mental health services, why now? Rationale (recovery + economics) • Peer support workers, role-modelling living well with mental illness and embodying hope in the future for others, improve the ‘recovery focus’ of mental health services (Repper and Carter 2011) • Economic solution - reflects wider shift in HICs away from professional healthcare workforce • Globally, peer support seen as untapped resource in LMICs (Puschner 2018) to address ‘treatment gap’ between size of population and size of economy
Peer support in mental health services, why now? • DHSC (2011) No Health Without Mental Health • NHS England (2016) The Five Year Forward View for Mental Health: A report from the independent Mental Health Taskforce to the NHS in England • Kaufman et al. (2014) Peer Specialist Training and Certification Programs: A National Overview • Council of Australia Governments (2017) The Fifth National Mental Health and Suicide Prevention Plan
Peer support in the NHS • Peer Support Workers: Arizona → Nottingham • Implementing Recovery through Organisational Change (Im. ROC) • Repper et al. (2013) Peer Support Workers: Theory and Practice. Centre for Mental Health and Mental Health Network, NHS Confederation
Peer support in the NHS • HEE (2017) Stepping forward to 2020/21: The mental health workforce plan for England • HEE (2020) The Competence Framework for Mental Health Peer Support Workers • October 2020 £ 2. 7 M tender to provide training for peer workers and their supervisors
Peer support: a thousand flowers blooming Modality • One-to-one; group; online; hybrid Function • Peer HCA; recovery coach; navigator; self-management Settings • Inpatient; community; primary care; public health Diagnostic group • Depression; psychosis; complex emotional needs Population • Gender; culture; sexuality; young people; carers; refugees Faulkner (2013) Mental health peer support in England: Piecing together the jigsaw. London, MIND
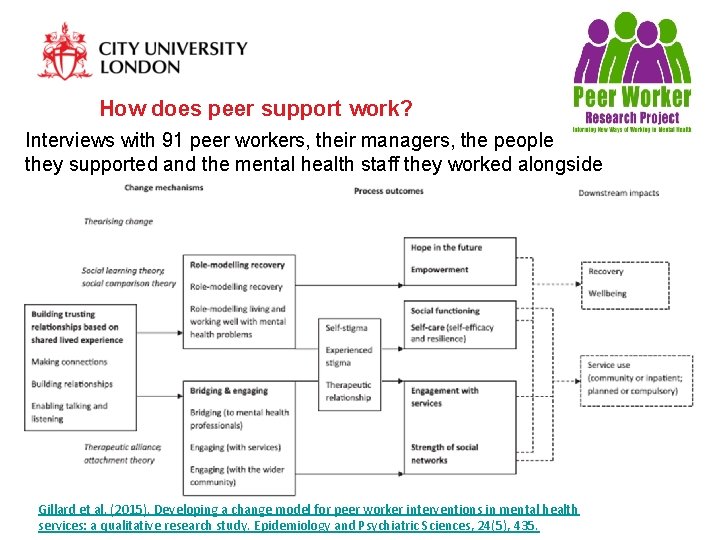
How does peer support work? Interviews with 91 peer workers, their managers, the people they supported and the mental health staff they worked alongside Gillard et al. (2015). Developing a change model for peer worker interventions in mental health services: a qualitative research study. Epidemiology and Psychiatric Sciences, 24(5), 435.
Impacts of peer support For the people being supported (Repper & Carter 2011) • Individual recovery • Hope • Empowerment For peer workers • Confidence, self-esteem, social network (Walker & Bryant 2013) • Employment opportunities +/ • Stress and burnout (Ahmed et al 2015; Park et al 2016) For services • Hospitalisation (Lawn et al 2008) • Cost-effectiveness (Trachtenburg et al 2013)
Peer support and the multi-disciplinary team Peer workers act as a ‘bridge’ between the service user and the clinical team (Simpson et al 2013; Watson 2017) • ‘Translation’ • Relationship based on mutuality and trust enables disclosure Peer workers bring different insight; expertise based on experiential knowledge (Oborn et al 2019) • New approaches to ‘holding risk’ in the team (Holley et al. 2015) Peer workers act as cultural changes agents within teams • Challenging causal use of stigmatising language (Gillard et al 2015)
Evidence base for peer support Early systematic reviews (Pitt et al. 2013; Lloyd Evans et al. 2014) tell us: • Peer support ‘no better or worse’ than support provided by other mental health workers • Large variation in peer support intervention, modality, population and outcomes measured • Lack of description of peer support and how it brings about change • Trials generally low quality (randomisation and blinding procedures not specified, selective reporting of outcomes)
Recent, more focused reviews… Peer support for depression (Pfeiffer et al 2011) • 7 RCTs • No effect on depressive symptoms Peer support for psychosis (Chien et al 2019) • 13 RCTs • No effect on relapse or hospitalisation Digital peer support for people with serious mental illness (Fortuna et al 2020) • Mixed study designs, with and without control • Some evidence in improvement in a range of outcomes Reviews combine one-to-one and group peer support
Challenges of implementing peer support into practice If peer support is experienced as beneficial by so many people, why isn’t the research clearer? Implementation of new roles always challenging (Dierdorff & Morgenson, 2007): 1. 2. 3. 4. 5. Need for new expertise to be clearly defined New workers enabled to use that expertise Leadership Clarity of expectation Issues of professional jurisdiction
Challenges of implementing peer support into practice Evidence suggests that the distinctive contribution that peer support might make can be diluted when good organisational support isn’t in place, including: 1. Shared expectations of the role (especially around peer workers disclosing and using their experiences) 2. Peer support-specific training 3. Supervision (from a peer perspective) 4. Appropriate accommodations 5. Preparation of clinical teams 6. Supportive and enabling leadership 7. Career progression (valuing peer support) Gillard et al. (2013). Introducing peer worker roles into UK mental health service teams: a qualitative analysis of the organisational benefits and challenges. BMC health services Research, 13(1), 1 -13.
Challenges of implementing peer support into practice • Can the values that underpin peer support can be maintained in a highly regulated environment like an NHS Trust (Stewart et al 2008)? • Or will the role inevitably become ‘professionalised’ – standardised training, risk procedures, note-taking – and no longer offer an ‘authentic’ peer support (Faulkner & Kalathil 2012)? • Call for international standards to protect the values of peer support (Stratford et al 2017) • And for fidelity measures that assess delivery of peer support against those values and standards (King & Bender-Simmons 2018)
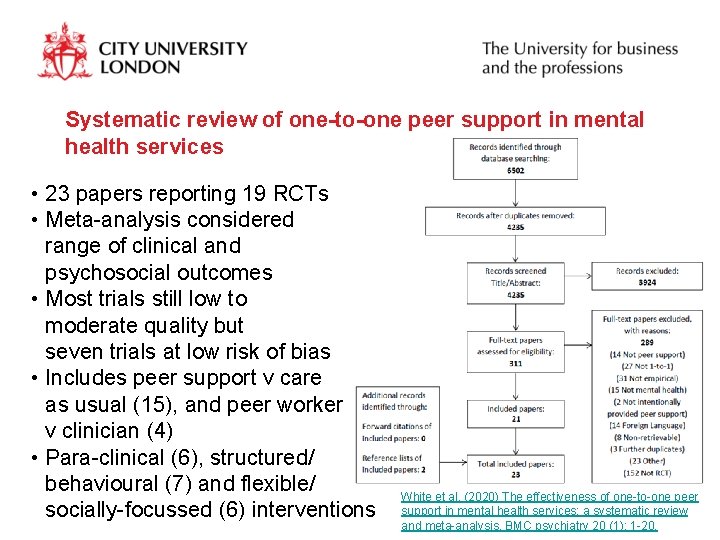
Systematic review of one-to-one peer support in mental health services • 23 papers reporting 19 RCTs • Meta-analysis considered range of clinical and psychosocial outcomes • Most trials still low to moderate quality but seven trials at low risk of bias • Includes peer support v care as usual (15), and peer worker v clinician (4) • Para-clinical (6), structured/ behavioural (7) and flexible/ socially-focussed (6) interventions White et al. (2020) The effectiveness of one-to-one peer support in mental health services: a systematic review and meta-analysis. BMC psychiatry 20 (1): 1 -20.
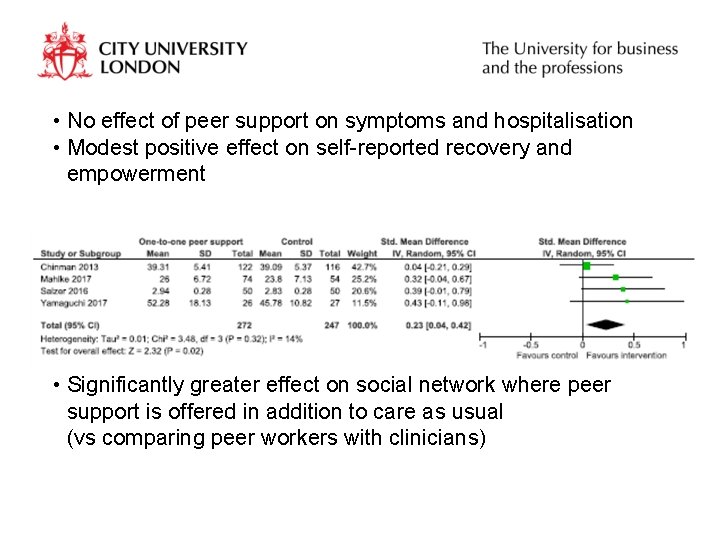
• No effect of peer support on symptoms and hospitalisation • Modest positive effect on self-reported recovery and empowerment • Significantly greater effect on social network where peer support is offered in addition to care as usual (vs comparing peer workers with clinicians)
What the research seems to be telling us… Where peer workers are not supported to work in a distinctive way… … and are asked to do similar work to other mental health workers … (to take on a para-clinical role) … outcomes are no better or worse than ‘care as usual’ (no effect on symptoms or service use) BUT Where peer workers are invited and supported to work in a distinctive, more relational capacity … … the potential exists for impact on psycho-social outcomes… …and on the culture of mental health service provision
Enhanced discharge from inpatient to community mental health care (ENRICH): a programme of applied research to manualise, pilot and trial a Peer Worker intervention • 5 year programme of research funded by UK National Institute of Health Research • 590 participants across 7 sites randomised to peer support for discharge vs care as usual • Eligibility: previous admission; not primary dx LD, ED, D&A • Trial hypothesis Peer support for discharge will reduce readmissions in the year post discharge compared to care as usual • Secondary outcomes • Severity of symptoms; hope; social network; quality of life • Time to readmission; type of admission; DNAs; use of crisis team, A&E Gillard et al. (2020). Peer support for discharge from inpatient to community mental health services: Study protocol clinical trial (SPIRIT Compliant). Medicine, 99(10).

Total of 32 peer workers across 7 sites Surrey & Borders South West London Sussex BDF East London Bradford BMS Central & NW London CNW SAB SWL Birmingham ELN SSX
• Challenge To ensure that the values that make peer support distinctive – building equitable relationships, learning from each other, strengthening social connections – underpin the intervention and trial • Response To integrate experiential knowledge of peer support throughout the research process
Our approach… • Lived experience in the research team • Service user researchers working at all study sites • Local and national Lived Experience Advisory Panels 1. Development of peer support intervention and evaluation process informed by Principles of Peer Support framework 2. Principles-based fidelity index to assess the extent to which a distinctive peer support is being evaluated
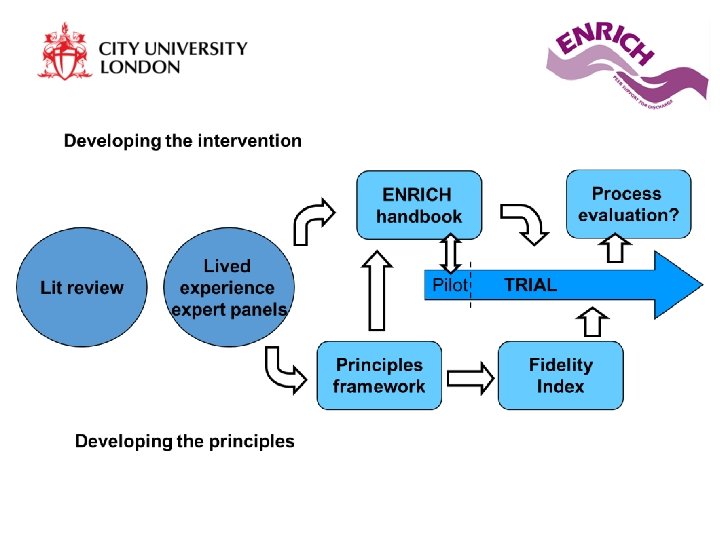
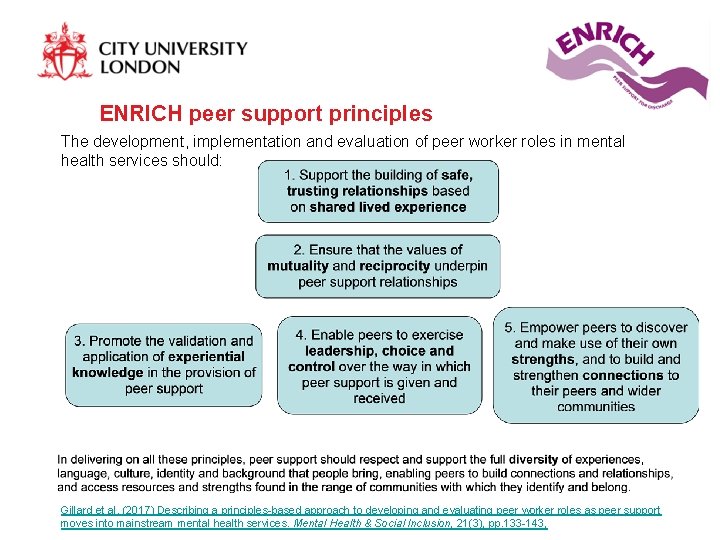
ENRICH peer support principles The development, implementation and evaluation of peer worker roles in mental health services should: Gillard et al. (2017) Describing a principles-based approach to developing and evaluating peer worker roles as peer support moves into mainstream mental health services. Mental Health & Social Inclusion, 21(3), pp. 133 -143,
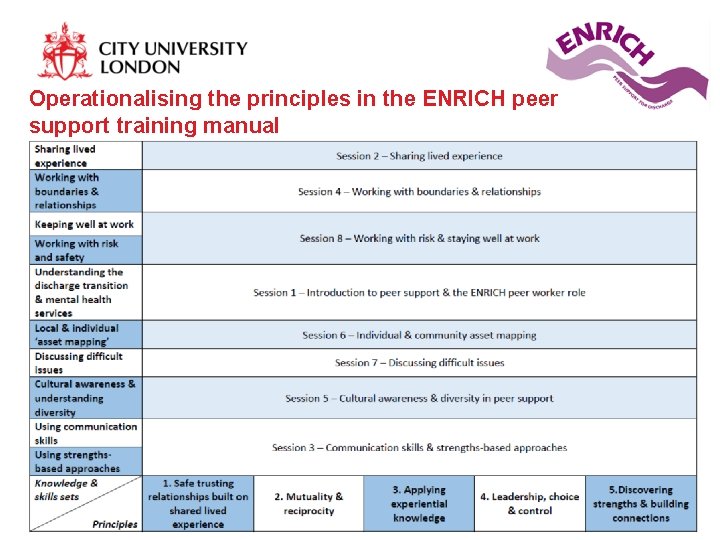
Operationalising the principles in the ENRICH peer support training manual
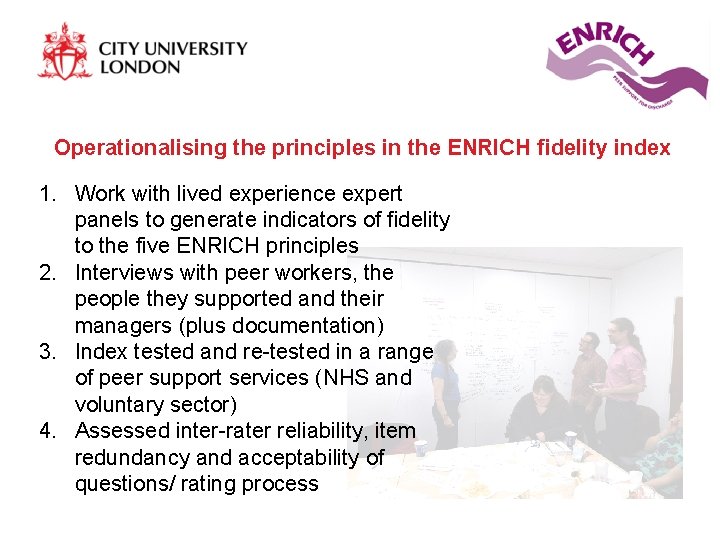
Operationalising the principles in the ENRICH fidelity index 1. Work with lived experience expert panels to generate indicators of fidelity to the five ENRICH principles 2. Interviews with peer workers, the people they supported and their managers (plus documentation) 3. Index tested and re-tested in a range of peer support services (NHS and voluntary sector) 4. Assessed inter-rater reliability, item redundancy and acceptability of questions/ rating process
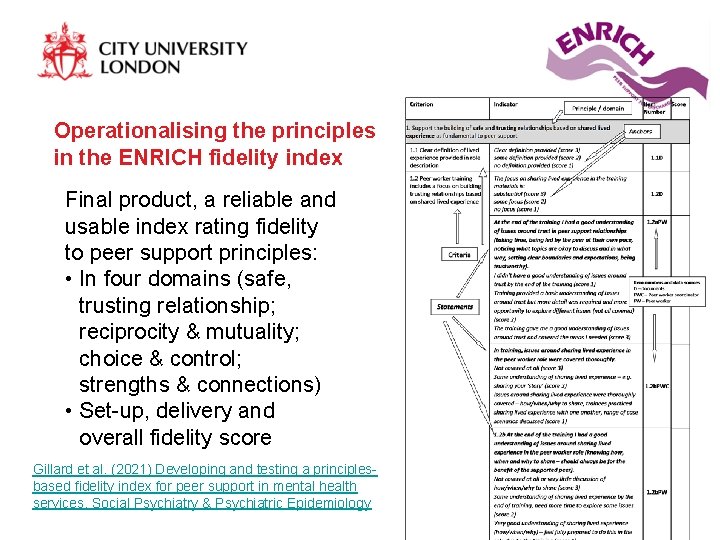
Operationalising the principles in the ENRICH fidelity index Final product, a reliable and usable index rating fidelity to peer support principles: • In four domains (safe, trusting relationship; reciprocity & mutuality; choice & control; strengths & connections) • Set-up, delivery and overall fidelity score Gillard et al. (2021) Developing and testing a principlesbased fidelity index for peer support in mental health services. Social Psychiatry & Psychiatric Epidemiology
Final results, watch this space… The ENRICH programme is funded by the National Institute of Health Research (NIHR), Programme Grants for Applied Research programme, UK. The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR PGf. AR programme, NIHR, NHS or the Department of Health.
Added value: peer support and health inequalities Peer support offers community-driven solutions to persistent inequalities in mental health care • Canerows (Mama Lows Kitchen) • Dial House @ Touchstone Connection based on a wider sense of shared experience relating to culture and community • Validating diversity of understandings of mental health and peer support • ‘Dancing to our own Tunes’ (Kalathil 2011) Potential to come together over complex experiences of marginalisation (Hope & Ali 2019) • mental health and racism; refugees and sexuality
Peer support and culture Challenges • Terminology of peer support and mental health alienating for some • Opportunities of peer support can be limited by language • Formal training, NHS policies and procedures can exclude people with difficult experiences of mental health services • Some preference for peer support from outside of the community (attitudes)
Peer support and culture Need for better understanding needed of the possibilities of both culturally-specific peer support, and peer support provided across difference, in the NHS and in the community: • Peer support, culture and community study funded by City SHS HEIF fund with Bromley by Bow Centre • Peer support, diversity and culture in the NHS workstream in NIHR Programme Development Grant
Implications for peer support in the NHS… Evidence that peer support should be commissioned to reduce hospitalisation and improve symptoms limited • Peer workers as para-clinicians ‘no better or worse’ Potential benefits to psychosocial outcomes if the peer worker role is properly supported/ focused • Peer support in addition to usual care, doing things that optimise the distinctive, relational nature of peer support Potential benefits to MDT skills mix? Implications of current plans for standardised, competenciesbased training not clear?
Implications for research… Research that is focused on specific clinical settings, populations and peer support interventions • including focused systematic reviews Better understanding of the challenges and potentials for peer support in different cultural contexts Need to explore relationship between implementation (support for peer support) and outcomes • including impact of new standardised training • peer support in the MDT Better understanding of how peer support in the voluntary sector and peer-led organisations complements NHS care Post-covid evaluation of remote and online peer support
Thank you Any questions? steven. gillard@city. ac. uk
- Slides: 38