SBAR Communication Model Situation Background Assessment and Recommendation
SBAR Communication Model Situation, Background, Assessment, and Recommendation Dagmar Raica, DNP, RN, NEA-BC (Revised: March, 2016) © DRaica
Objectives • List & define what SBAR stands for. • List 3 reasons why SBAR is important to use. • Describe how SBAR affects patient safety. • Describe the difference between assertiveness and aggressiveness. • Verbalize appropriate responses in practice scenarios.
SBAR Ineffective communication poses a significant threat to the safety of hospitalized patients. SBAR is a useful and effective communication tool that allows healthcare professionals to share concise but important information in a short amount of time.
Michael Leonard, physician leader for patient safety at Kaiser Permanente introduced SBAR that was modified for use in health care from the method used in the aviation industry to reduce communication errors among crew members Nurses are often taught to report in a narrative form. Physicians are taught to communicate using brief “bullet points” that provide key information.
SBAR – why it is important to use According to the Joint Commission, communication issues are the leading cause of sentinel events in hospitals. Improving the exchange of information between nurses and physicians have been cited as a key element to preventing medical errors and promoting a safe environment. (Manning, 2006) Miscommunication leads to patient safety issues. (HCPro, 2004)
SBAR Communication Model Easy to remember tool that provides a structured, orderly approach to improve effective communication of accurate, relevant information. The goal is to deliver your message in 1 to 1 ½ minutes. Helps limit the jargon, keeps the message clear, and removes the influence of hierarchy and personality.
SBAR broken down… SITUATION: State what is happening at the present time that has warranted the SBAR communication. (State your name & unit, what patient you are calling about, & what the problem is) Example: Hello Dr. ______, this is ____, from ____unit. I am calling about __(pt name & room #)___. The patient’s code status is ____. I have just assessed the patient myself. I am concerned about ________. (Examples can be BP over or under parameters, pulse over 140 or less than 50, respirations less than 5 or over 40, elevated temp or many other situations). Note: These are examples, your hospital or physician may have established parameters to call about.
SBAR broken down cont’d… BACKGROUND: Explain circumstances leading up to this situation. (State admission diagnosis, date of admission, brief pertinent medical history, and treatment to date) Example: The patient’s mental status is ______, vital signs are _____, skin is _____, O 2 is (not on) or on at ___, oximeter reading is at ___, the patient complains of _______.
SBAR broken down, cont’d…. ASSESSMENT: Indicate what you think the problem is (Provide last vital signs, oxygen if being used, & any changes from prior assessment: vital signs, heart rhythm, pain, wound drainage, neuro changes, etc. Example: I believe the problem is: (state what you believe the problem is, i. e. cardiac, infection, neurologic, respiratory, other). OR: I don’t know what the problem is but the patient is deteriorating. OR: The patient seems to be unstable.
SBAR broken down cont’d…. RECOMMENDATION: Express what you believe the patient needs or what order specifically you want i. e. give fluids, order labs, x-ray, have the physician come see the patient, transfer the patient to ICU, ask for a consulting physician to see the patient, etc. Example: I suggest/request/recommend that you _____ (see immediately, transfer the patient to ICU, ask the hospitalist/resident to see the patient now, talk to family about code status, etc. OR: Suggest tests/interventions that would be needed (Chest x-ray, ABG’s, EKG, CBC, BMP, give additional fluids, pain meds, etc. ) If no improvement, when should we call again?
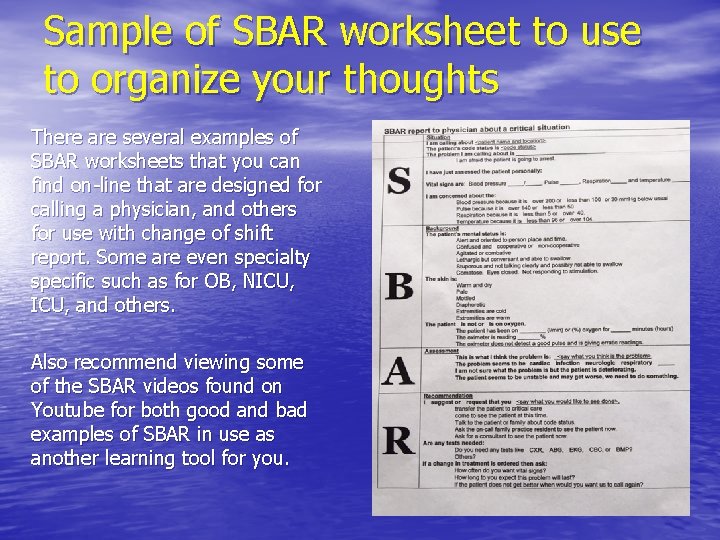
Sample of SBAR worksheet to use to organize your thoughts There are several examples of SBAR worksheets that you can find on-line that are designed for calling a physician, and others for use with change of shift report. Some are even specialty specific such as for OB, NICU, and others. Also recommend viewing some of the SBAR videos found on Youtube for both good and bad examples of SBAR in use as another learning tool for you.
Practice example of making a recommendation: The “R” in SBAR: Which is better? A. The nurse picks up the chart & notices that the physician did not order labs despite a low hematocrit. The nurse says “excuse me, did you want to order labs today? ” B. The nurse says “I noticed that Mrs. Smith’s hct was 26 yesterday, what about repeating the hematcrit? ”
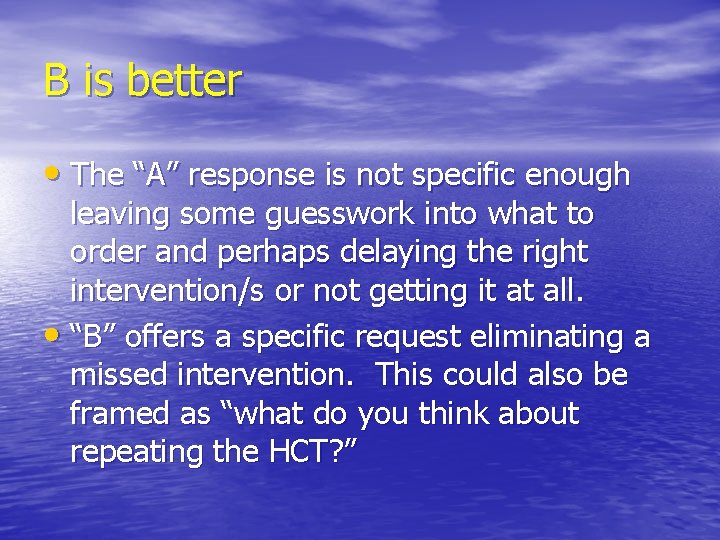
B is better • The “A” response is not specific enough leaving some guesswork into what to order and perhaps delaying the right intervention/s or not getting it at all. • “B” offers a specific request eliminating a missed intervention. This could also be framed as “what do you think about repeating the HCT? ”
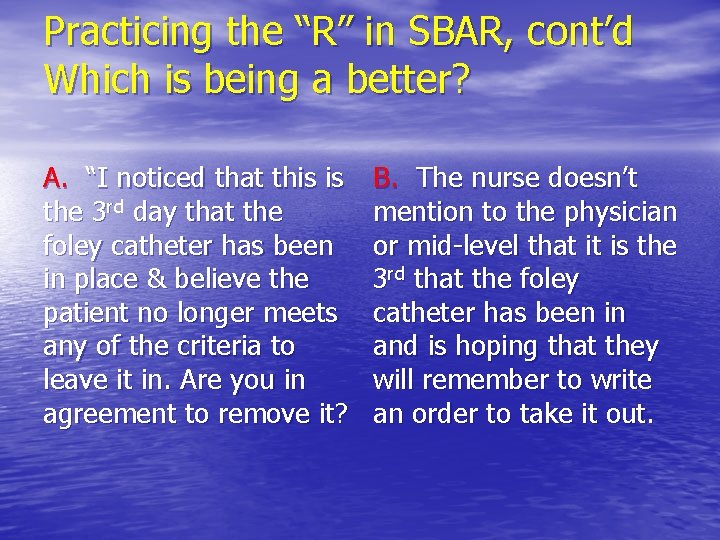
Practicing the “R” in SBAR, cont’d Which is being a better? A. “I noticed that this is the 3 rd day that the foley catheter has been in place & believe the patient no longer meets any of the criteria to leave it in. Are you in agreement to remove it? B. The nurse doesn’t mention to the physician or mid-level that it is the 3 rd that the foley catheter has been in and is hoping that they will remember to write an order to take it out.
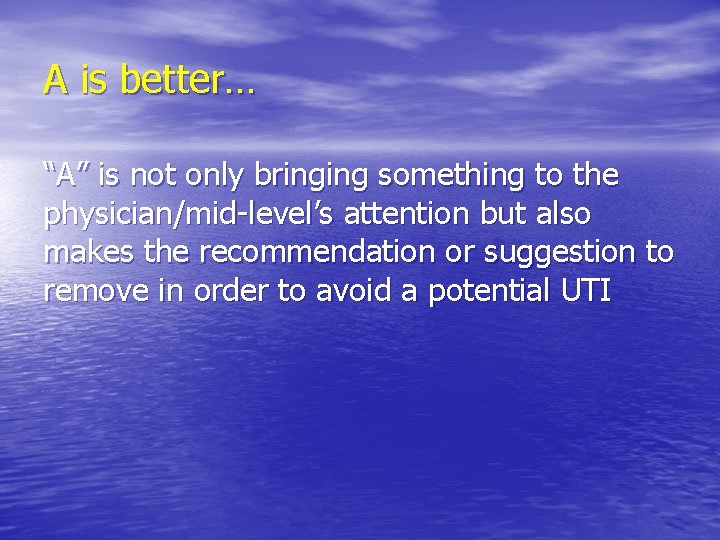
A is better… “A” is not only bringing something to the physician/mid-level’s attention but also makes the recommendation or suggestion to remove in order to avoid a potential UTI
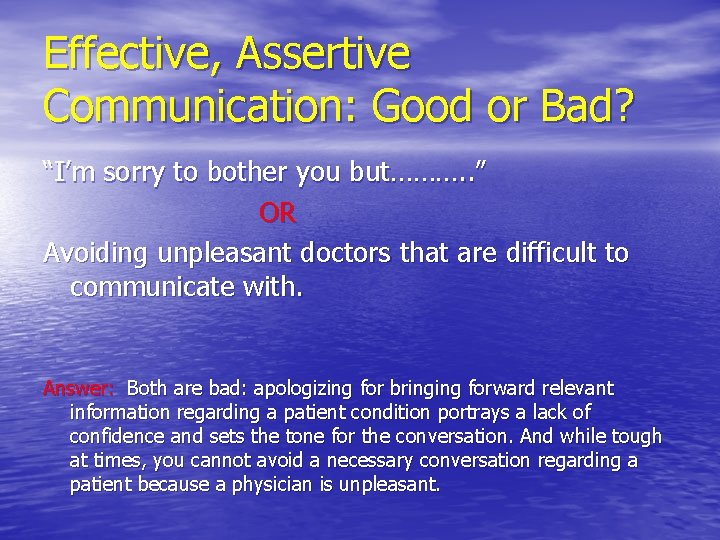
Effective, Assertive Communication: Good or Bad? “I’m sorry to bother you but………. . ” OR Avoiding unpleasant doctors that are difficult to communicate with. Answer: Both are bad: apologizing for bringing forward relevant information regarding a patient condition portrays a lack of confidence and sets the tone for the conversation. And while tough at times, you cannot avoid a necessary conversation regarding a patient because a physician is unpleasant.
Importance of Effective Communication Nurses are the front-line care givers responsible for notifying physicians of patient care issues, acting as the patient advocate, & protecting the patient from further harm, yet current nursephysician relationships & cultures often do not empower nurses to communicate effectively with physicians.
Ways to Improve Communication • Work at developing relationships • • • with a personal connection, ask about their weekend, family, etc. Don’t be afraid to use humor in your communications as you develop relationships based on mutual respect Be prepared with all relevant information before making the call or starting the conversation And, most importantly, utilize a succinct communication model such as SBAR when providing patient information
Improving Communication, cont’d • Assume that you and the physician are on the same • • team & that you have the same broad goals for the patient. Stressing again to be ready with patient data before you call or communicate with the physician. Communicate clearly your title & your relationship with the patient, example primary nurse, wound care nurse, etc. Connecting on a human level can be a powerful catalyst. Utilize appropriate assertiveness (not aggressive) as you advocate for your patient.
Characteristics of an Assertive Nurse (versus aggressive) • Appears self-confident & composed • Maintains eye contact • Uses clear, concise speech • Speaks firmly & positively • Is non-apologetic • Takes initiative to guide situations • Gives the same message verbally & nonverbally • Speaks genuinely, without sarcasm (Communication in Nursing, 2004)
Dealing with Difficult Physicians or Other Healthcare team members • Connecting on a human level can • • be a powerful catalyst. Do not be afraid to express what you think and believe about this patient. Have a memorized response to fall back on so you can respond when caught off guard by an inappropriate comment or behavior.
Examples of a response to have prepared in your mind when caught off guard by rude behavior • “I am almost through, and would like to finish my • • thought. ” “Please don’t yell at me, I am here to do what is best for the patient. ” “You are being rude and inappropriate, it is not helping us take care of the patient. ” Take 5 minutes right now and come up with a comment that you can memorize and have available
Dealing with difficult physicians & others on the healthcare team Remember: Nobody benefits if the nurse doesn’t assert themselves under certain conditions. This does get easier with practice and being prepared!
Summary • Use of SBAR to organize the exchange of information has • • demonstrated effectiveness in reducing communication errors (Beyea, 2004) Promoting nurses’ confident use of SBAR has great potential to decrease miscommunication and increase patient safety Nurses may experience discomfort using SBAR because it moves beyond the traditional approaches of merely reporting information into newer territory of joint decision making which includes providing opinions and making recommendations
Summary, cont’d • Commit to practicing using the SBAR model until it becomes your normal routine • Role playing in the context of communicating with a difficult physician (and using your memorized statement) may also be helpful to improving your ability to communicate effectively
Conclusion STAND IN AWE OF WHAT YOU DO AND RECOGNIZE YOUR TREMENDOUS VALUE
References Beyea, S. C. (2004). Improving verbal communication in clinical care. AORN Journal, 79(5), 1053 -1057. HCPro, (2004). Get in gear. Six road-tested ways to communicate critical test results. Briefings on Patient Safety, 5(11), 2 -6. Manning, M. L. (2006). Improving clinical communication through structured conversation. Nursing Economics, 24(5), 268 -271. Raica, D. A. (2009). Effect of action-oriented communication training on nurses’ communication self-efficacy. Med. Surg Nursing, 18(6), 343 -356, 360.
- Slides: 27