SARCOIDOSIS AHMAD BASEEM AHMAD AMER QOLA GHASI SARCOIDOSIS
SARCOIDOSIS AHMAD BASEEM AHMAD AMER QOLA GHASI
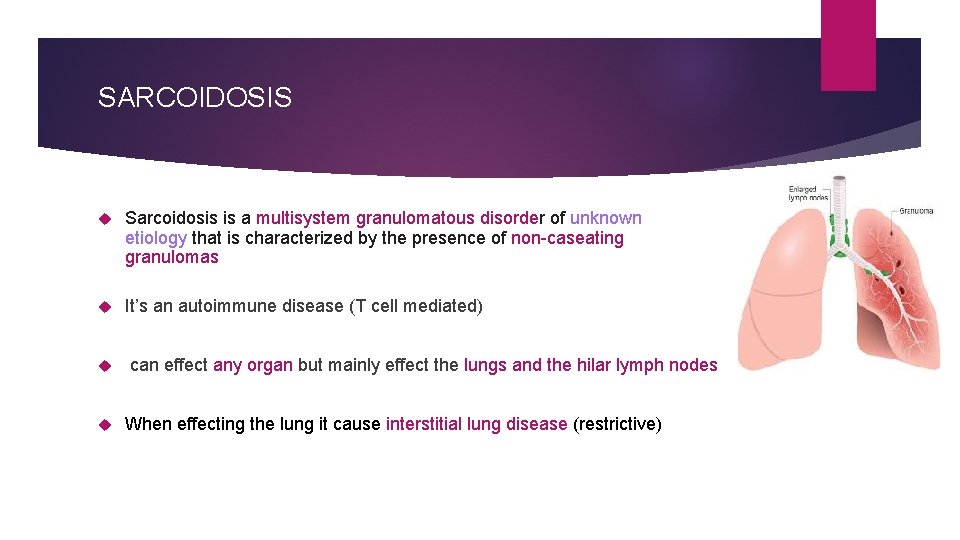
SARCOIDOSIS Sarcoidosis is a multisystem granulomatous disorder of unknown etiology that is characterized by the presence of non-caseating granulomas It’s an autoimmune disease (T cell mediated) can effect any organ but mainly effect the lungs and the hilar lymph nodes When effecting the lung it cause interstitial lung disease (restrictive)
epidemiology Occurs most often in the African American population, especially women! 75% of cases occur when the individual is under 40 years of age. Eskimos, Arabs and Chinese are rarely affected The tendency for sarcoid to present in the spring and summer has led to speculation about the role of infective agents (next slide) Sarcoidosis occurs less frequently in Smokers
etiology Etiology is unknown ! several lines of evidence suggest that it is a disease of disordered immune regulation in genetically predisposed individuals exposed to certain environmental agents Genetic susceptibility is supported by familial clustering; a range of class II HLA alleles confer protection from, or susceptibility (HLA-DRB 1) to the condition. Micro organisms (environmental agents) that their antigens are thought to have a role: v M. Tuberculosis v Borrelia Burgdorferi (Lyme Disease) v Human Herpes Virus 8 (HHV 8) v Proprionibacterium Acne
pathophysiology normally the dendritic cells and macrophages (antigen presenting cells) represent the pathogen antigen to naive CD 4+ T cell and release cytokines which stimulate the activation and proliferation of the naive T cells to CD 4+ TH 1 cells which will release more IL-2 for further proliferation and IFN-γ resulting in macrophages activation (T cell mediated immune response ) In sarcoidosis, the CD 4+ T cell response to unknown antigen, the T cell meditated immune response will lead to form small nodules (non-caseating granulomas) in any organ and trigger an inflammation in heathy tissue (autoimmune disease) HLA II gene polymorphism (HLA-DRB 1) with environmental factors (discussed earlier ) are thought to have a role
Non-caseating granulomas non-caseating granulomas are different from the “caseating”(e. g. TB) by the absences of necrotic tissue in the center The center is formed by large multinucleated cell /giant cell (fused macrophages)and epithelioid cells. Inclusion “ asteroid bodies” and schaumann bodies are seen within. And it’s surrounded by fibroblast, mast cells, monocytes and lymphocytes (the outer layer ) The giant cells release 1 -alpha hydroxylase Ca absorption hypercalcemia. activated vitamin D
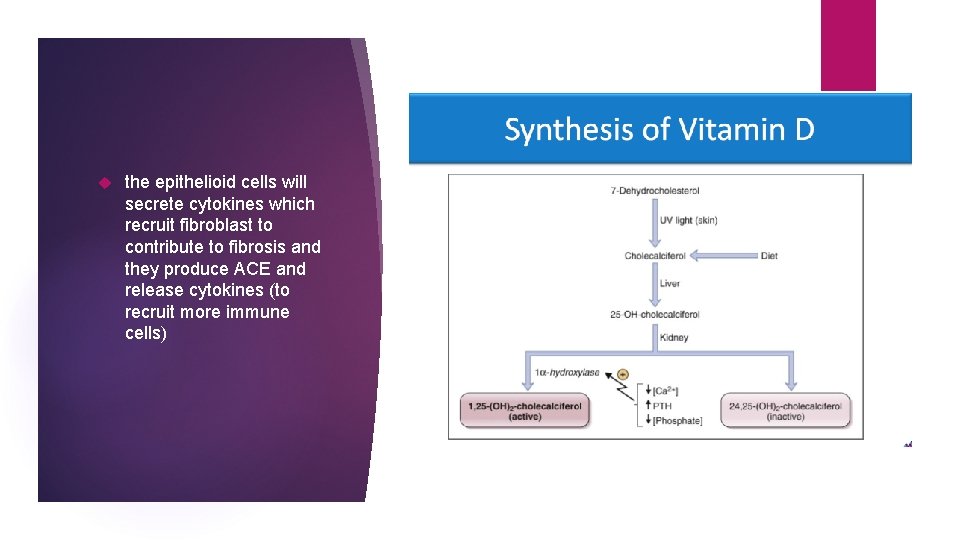
the epithelioid cells will secrete cytokines which recruit fibroblast to contribute to fibrosis and they produce ACE and release cytokines (to recruit more immune cells)
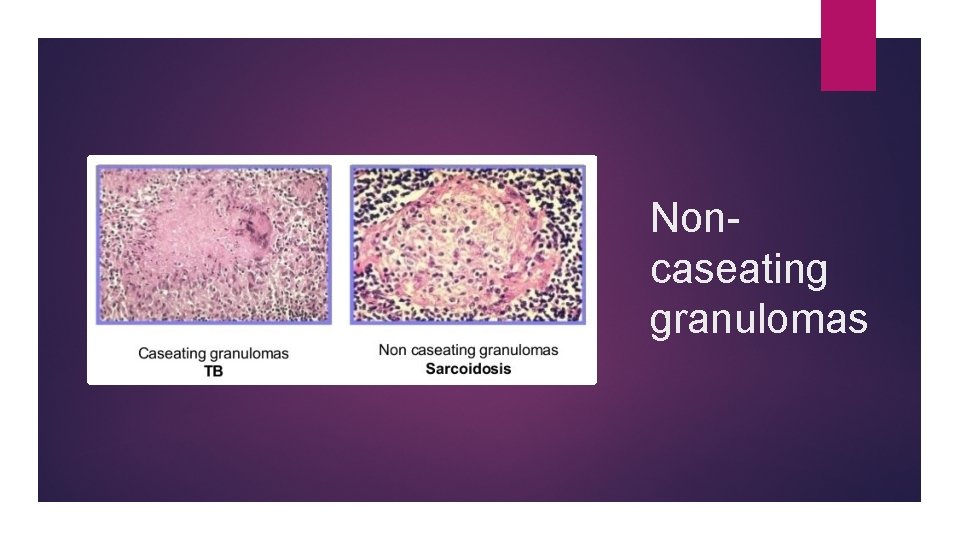
Noncaseating granulomas
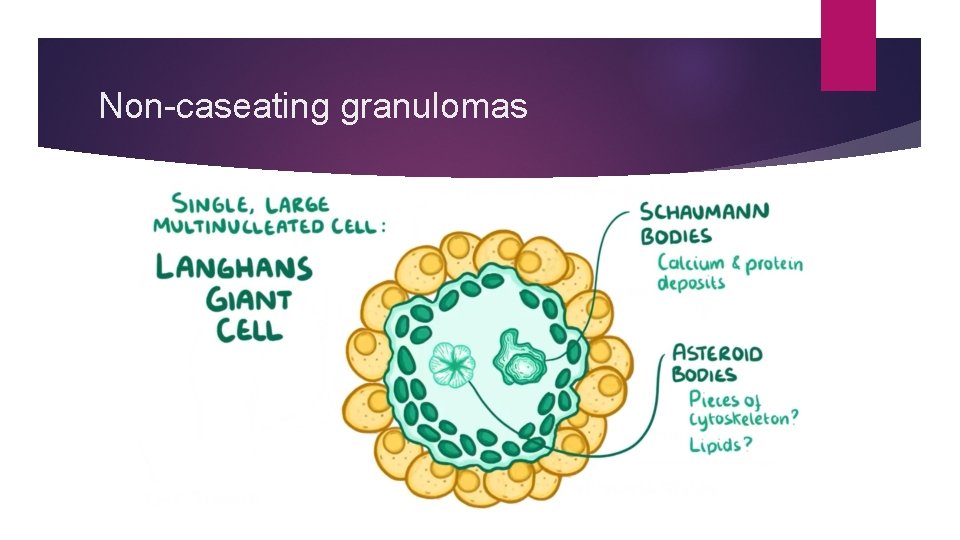
Non-caseating granulomas
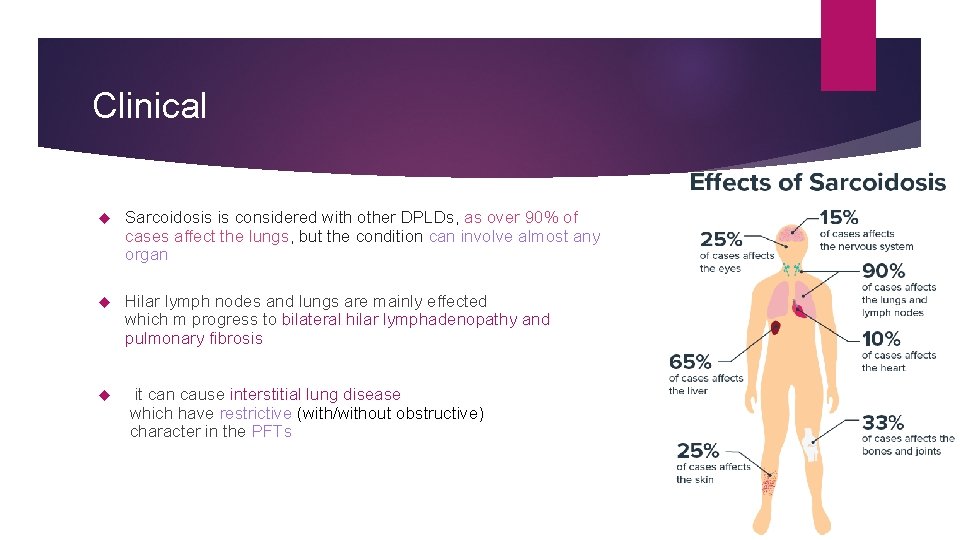
Clinical Sarcoidosis is considered with other DPLDs, as over 90% of cases affect the lungs, but the condition can involve almost any organ Hilar lymph nodes and lungs are mainly effected which m progress to bilateral hilar lymphadenopathy and pulmonary fibrosis it can cause interstitial lung disease which have restrictive (with/without obstructive) character in the PFTs
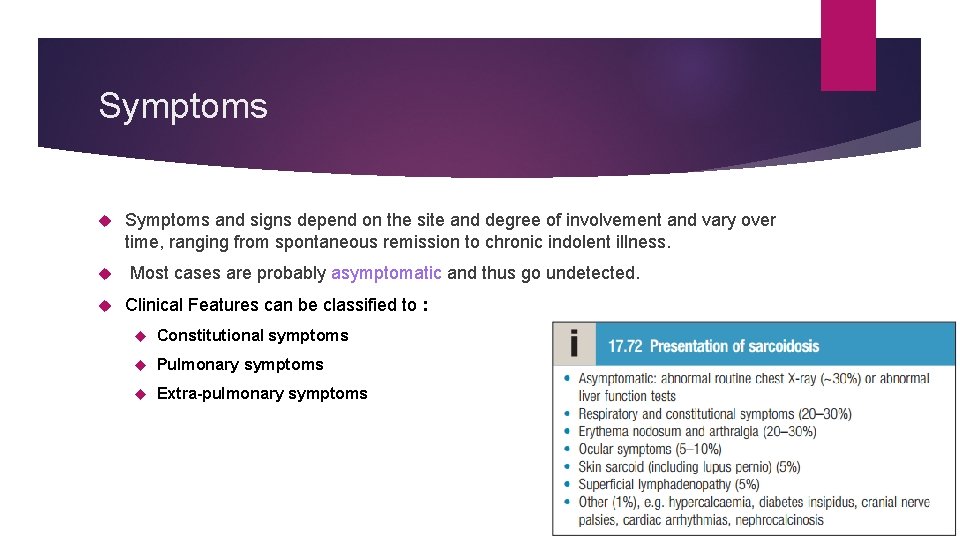
Symptoms and signs depend on the site and degree of involvement and vary over time, ranging from spontaneous remission to chronic indolent illness. Most cases are probably asymptomatic and thus go undetected. Clinical Features can be classified to : Constitutional symptoms Pulmonary symptoms Extra-pulmonary symptoms
Constitutional symptoms Malaise fever anorexia weight loss
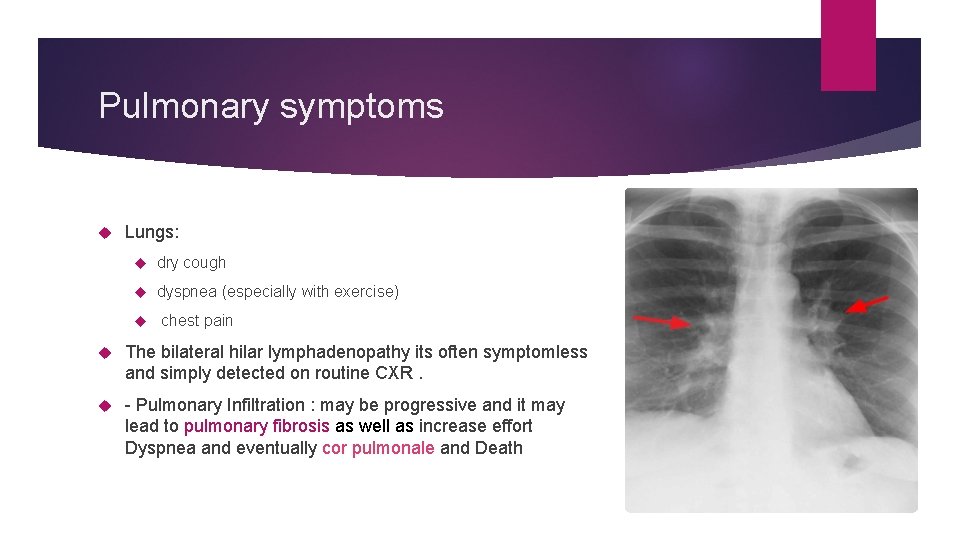
Pulmonary symptoms Lungs: dry cough dyspnea (especially with exercise) chest pain The bilateral hilar lymphadenopathy its often symptomless and simply detected on routine CXR. - Pulmonary Infiltration : may be progressive and it may lead to pulmonary fibrosis as well as increase effort Dyspnea and eventually cor pulmonale and Death
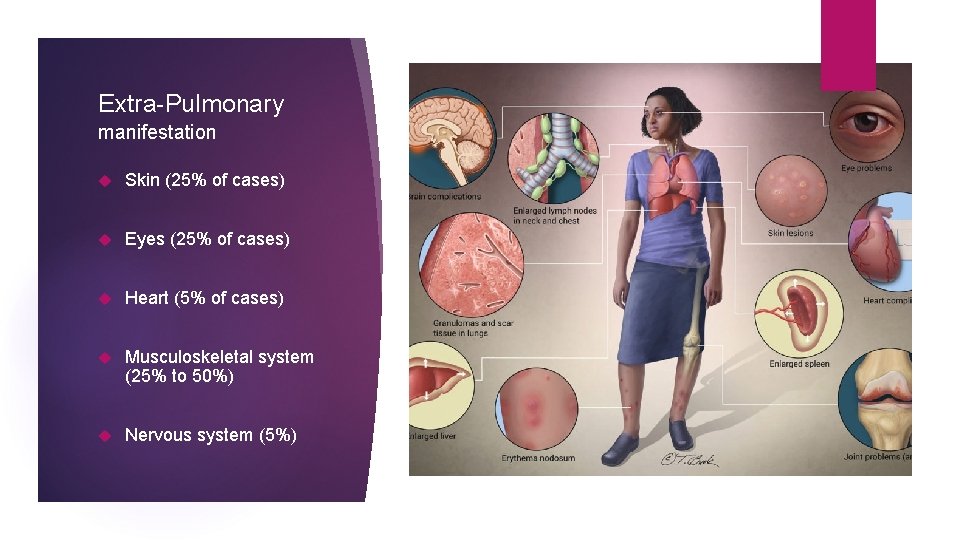
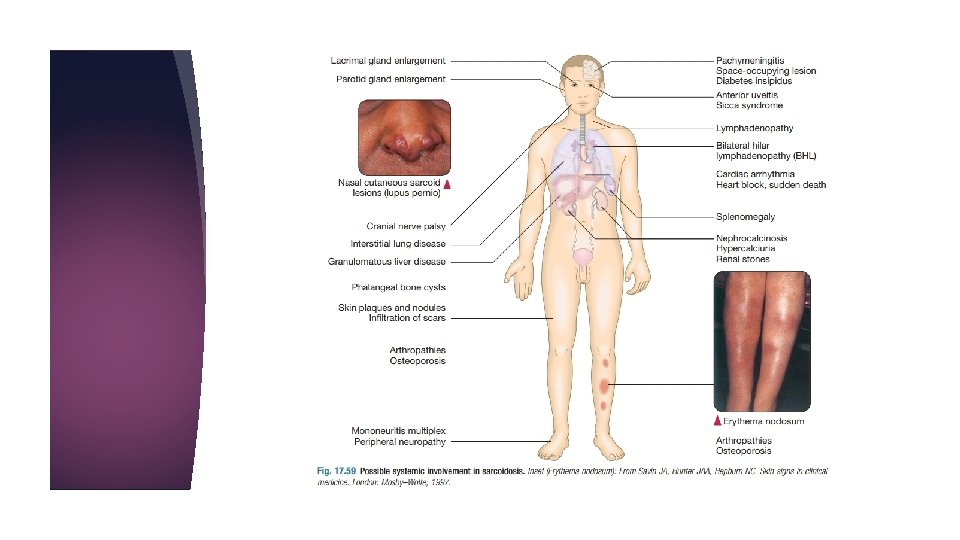
Extra-Pulmonary manifestation Skin (25% of cases) Eyes (25% of cases) Heart (5% of cases) Musculoskeletal system (25% to 50%) Nervous system (5%)
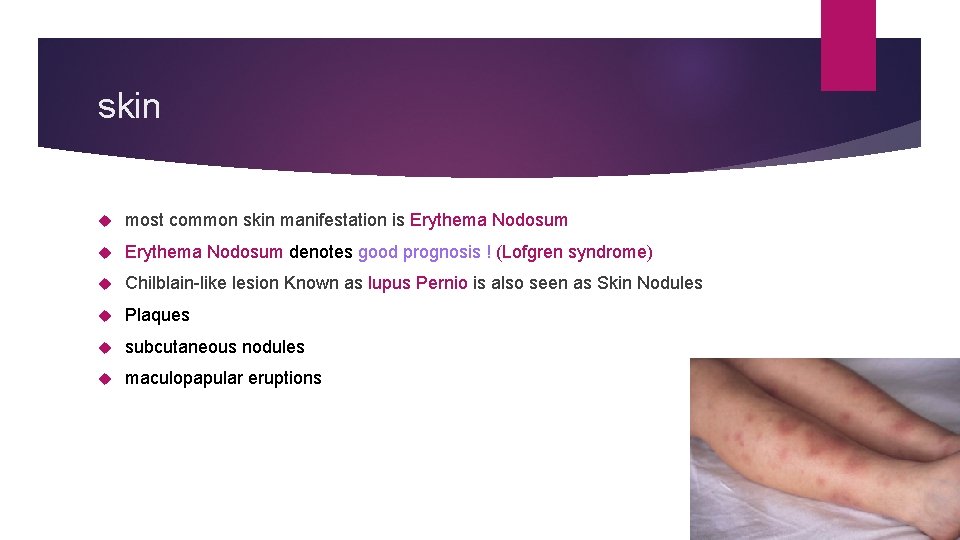
skin most common skin manifestation is Erythema Nodosum denotes good prognosis ! (Lofgren syndrome) Chilblain-like lesion Known as lupus Pernio is also seen as Skin Nodules Plaques subcutaneous nodules maculopapular eruptions
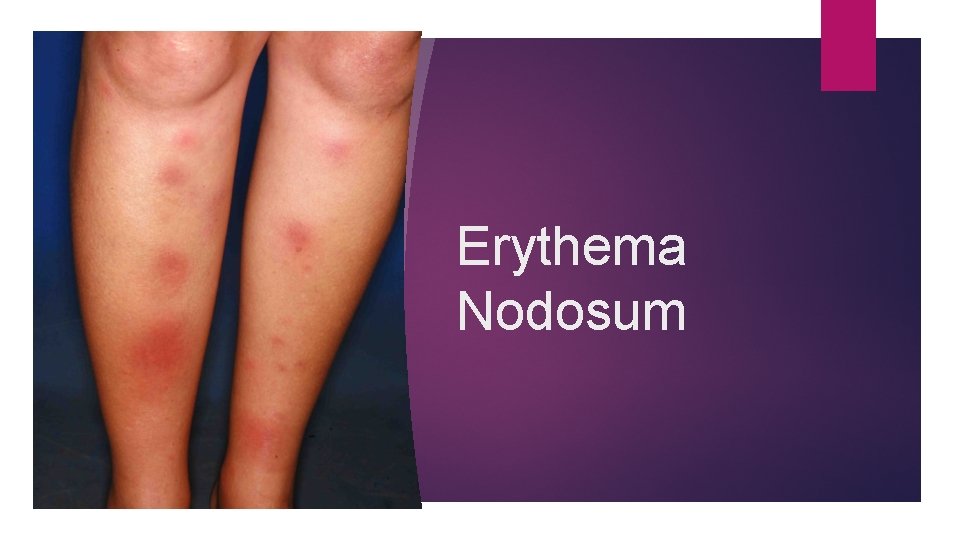
Erythema Nodosum

lupus Pernio
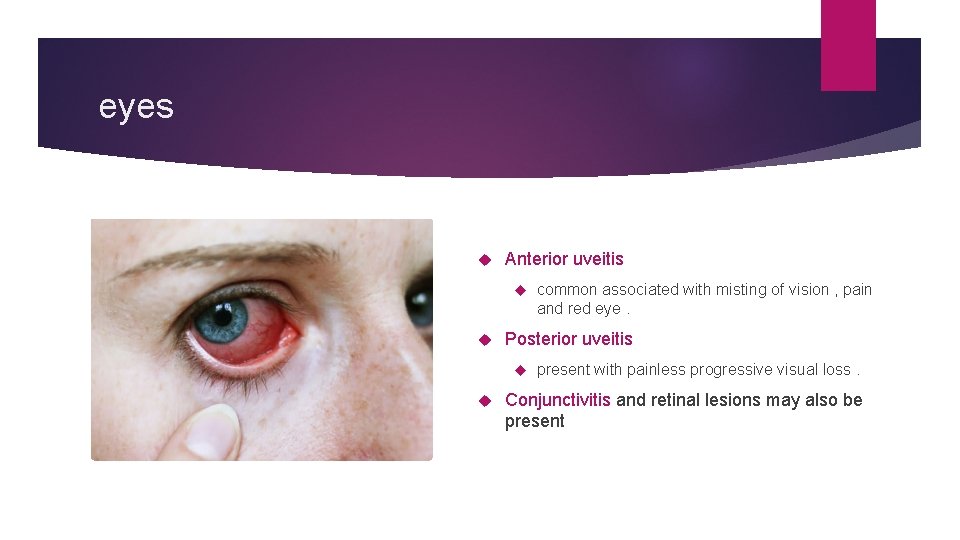
eyes Anterior uveitis Posterior uveitis common associated with misting of vision , pain and red eye. present with painless progressive visual loss. Conjunctivitis and retinal lesions may also be present
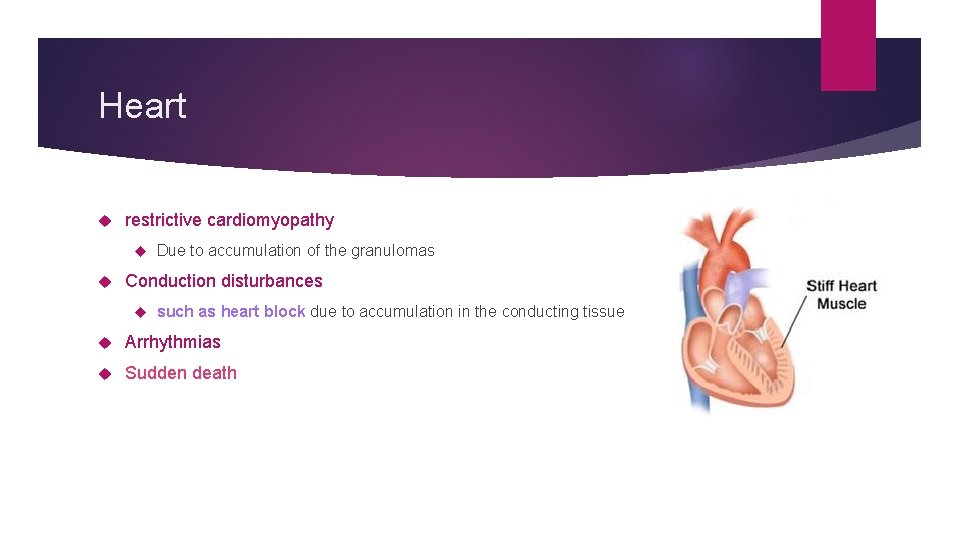
Heart restrictive cardiomyopathy Due to accumulation of the granulomas Conduction disturbances such as heart block due to accumulation in the conducting tissue Arrhythmias Sudden death
Extra-Pulmonary symptoms (count. ) Liver and spleen Hepatosplenomegaly Bone and joint Arthalgia and arthritis resembles R. A Usually bilateral involvement of the ankle joints Bone lesions Kidney nephrosclerosis and formation of renal calculi due to hypercalcemia
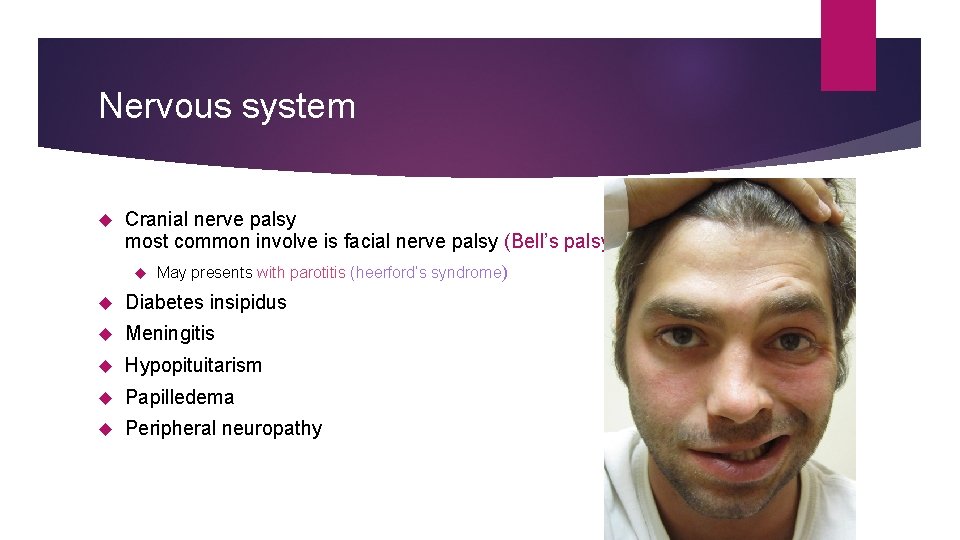
Nervous system Cranial nerve palsy most common involve is facial nerve palsy (Bell’s palsy) May presents with parotitis (heerford’s syndrome) Diabetes insipidus Meningitis Hypopituitarism Papilledema Peripheral neuropathy
Löfgren syndrome Subtypes and variants heerford’s syndrome
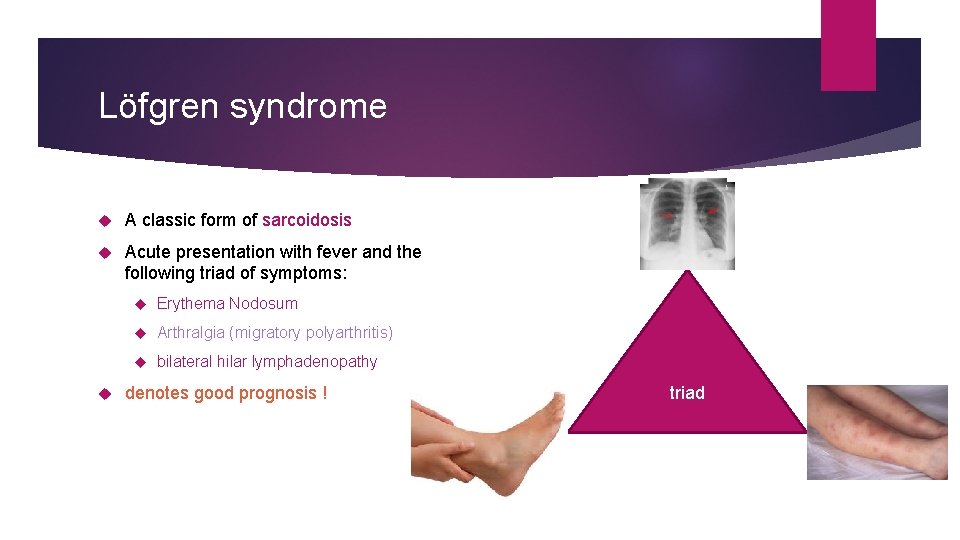
Löfgren syndrome A classic form of sarcoidosis Acute presentation with fever and the following triad of symptoms: Erythema Nodosum Arthralgia (migratory polyarthritis) bilateral hilar lymphadenopathy denotes good prognosis ! triad
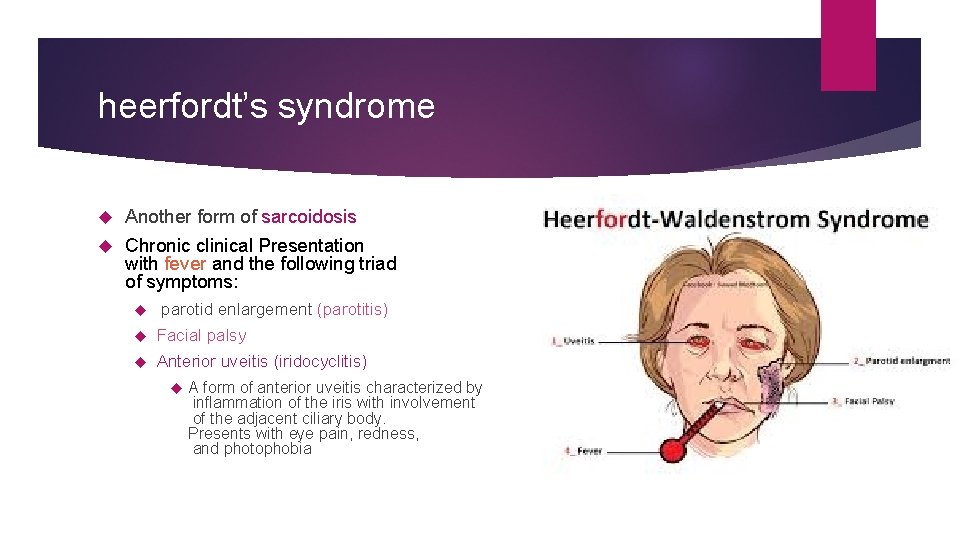
heerfordt’s syndrome Another form of sarcoidosis Chronic clinical Presentation with fever and the following triad of symptoms: parotid enlargement (parotitis) Facial palsy Anterior uveitis (iridocyclitis) A form of anterior uveitis characterized by inflammation of the iris with involvement of the adjacent ciliary body. Presents with eye pain, redness, and photophobia
Diagnosis Sarcoidosis is partly a diagnosis of exclusion. It is imperative to exclude the other granulomatous diseases like hypersensitivity pneumonitis (i. e. using BAL the CD 4/CD 8 helper/ suppressor ratio >4: 1 while in hypersensitivity pneumonitis the ratio <1) While ensuring the absence of organisms and negative culture Definitive diagnosis requires transbronchial biopsy (gold standard) Must see noncaseating granulomas By itself is not diagnostic because noncaseating granulomas are found in other diseases Must be used in the context of clinical presentation In Classic forms of sarcoidosis like Löfgren syndrome, biopsy confirmation is not necessary Other laboratory and radiographic findings could be helpful (next slides)
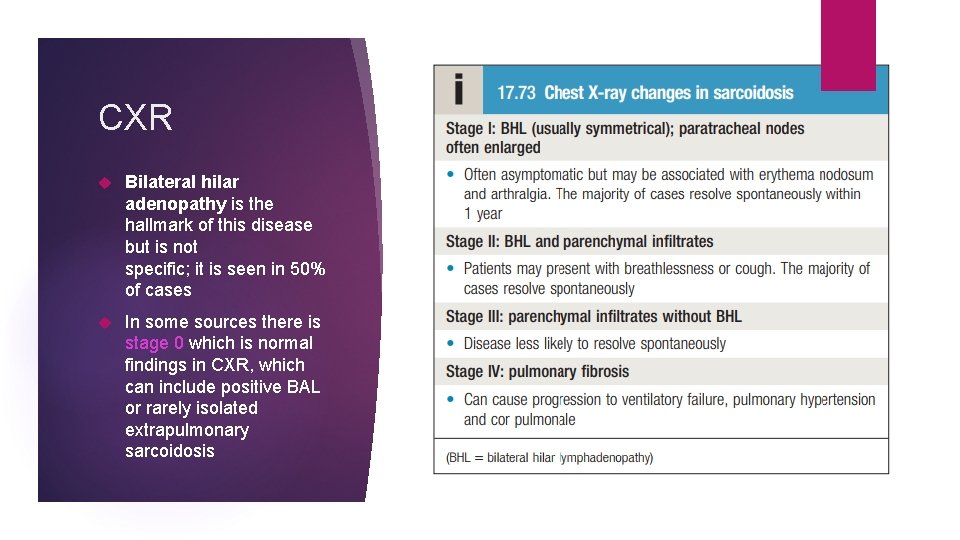
CXR Bilateral hilar adenopathy is the hallmark of this disease but is not specific; it is seen in 50% of cases In some sources there is stage 0 which is normal findings in CXR, which can include positive BAL or rarely isolated extrapulmonary sarcoidosis
Sarcoidosis stages
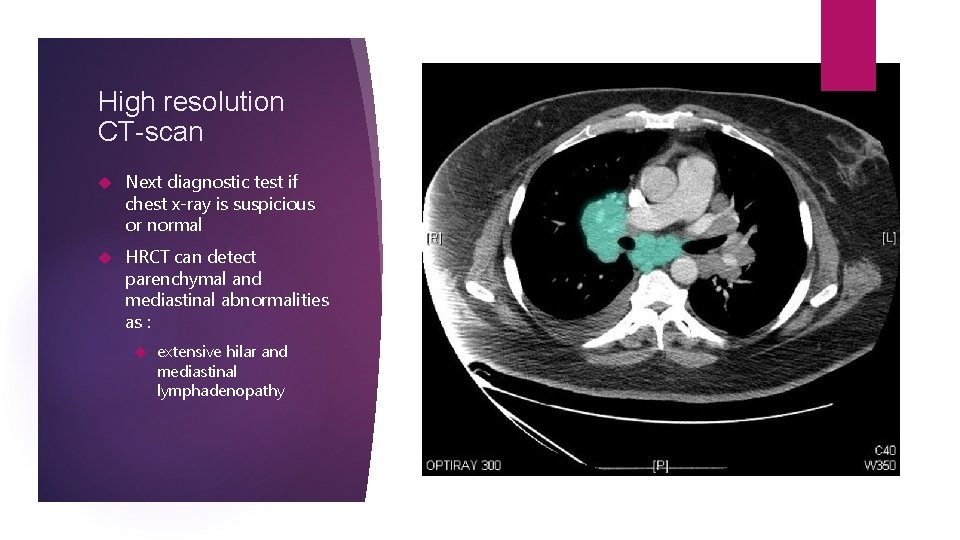
High resolution CT-scan Next diagnostic test if chest x-ray is suspicious or normal HRCT can detect parenchymal and mediastinal abnormalities as : extensive hilar and mediastinal lymphadenopathy
Laboratory Angiotensin-converting enzyme (ACE) is elevated in serum in about 50% to 80% of patients. This test helps support the diagnosis. However, other pulmonary diseases may cause an elevation in this enzyme (lacks sensitivity and specificity). Hypercalciuria and hypercalcemia are common. PFTs: decreased lung volumes (VC and TLC) – restrictive character decreased DLCO (diffusing capacity for carbon monoxide) decreased or normal FEV 1/FVC ratio – obstructive character
treatment Most cases resolve or significantly improve spontaneously in 2 years and do not require treatment. however Patients who present with acute illness and erythema nodosum should receive NSAIDs for symptomatic relief Systemic corticosteroids are the treatment of choice. The indications for treatment are unclear. However, patients who are symptomatic or have active lung disease, pulmonary function deterioration, conduction disturbances, or severe skin or eye involvement should be treated. Methotrexate or other immunosuppressive agents can be used in patients with progressive disease refractory to corticosteroids.
Recourses Davidson’s Principles and Practice of Medicine 23 rd edition Robbins Basic pathology 10 th edition Med. Study internal medicine core 18 th edition Step-up to medicine 5 th edition Herold G. Internal Medicine. Cologne, Germany: Herold G; 2014 Mayo Clinic Internal Medicine
- Slides: 33