SAQ 9 SAQ 9 A 24 yo man
- Slides: 12
SAQ 9
SAQ 9 A 24 yo man with a 6 yr Hx of Crohns disease presents with 12 hrs of worsening abdominal pain, fever and vomiting. BP 90/60 HR 120 Temp 38. 7
a. List 6 possible causes for this presentation a. List 5 abdominal complications of Crohns disease b. List & Justify 5 investigations in this pt a. Compare Crohns disease & Ulcerative Colitis
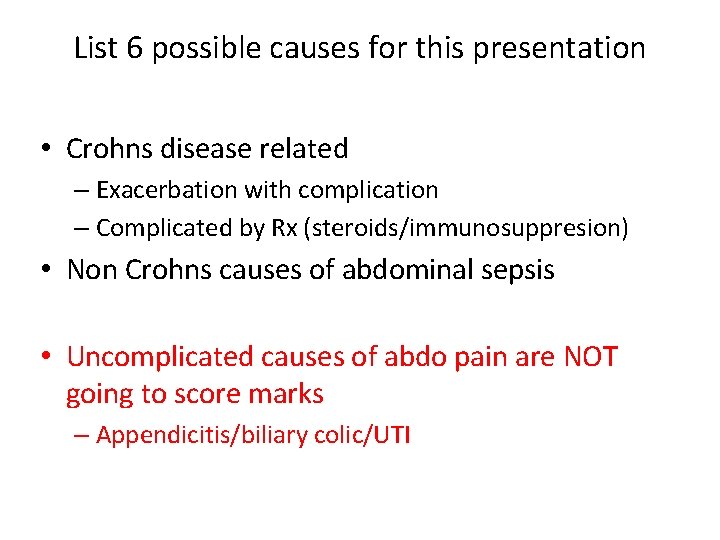
List 6 possible causes for this presentation • Crohns disease related – Exacerbation with complication – Complicated by Rx (steroids/immunosuppresion) • Non Crohns causes of abdominal sepsis • Uncomplicated causes of abdo pain are NOT going to score marks – Appendicitis/biliary colic/UTI
List 6 possible causes for this presentation All the differentials should relate to the STEM if possible Only if you have exhausted abdominal causes should you venture away from the abdomen.
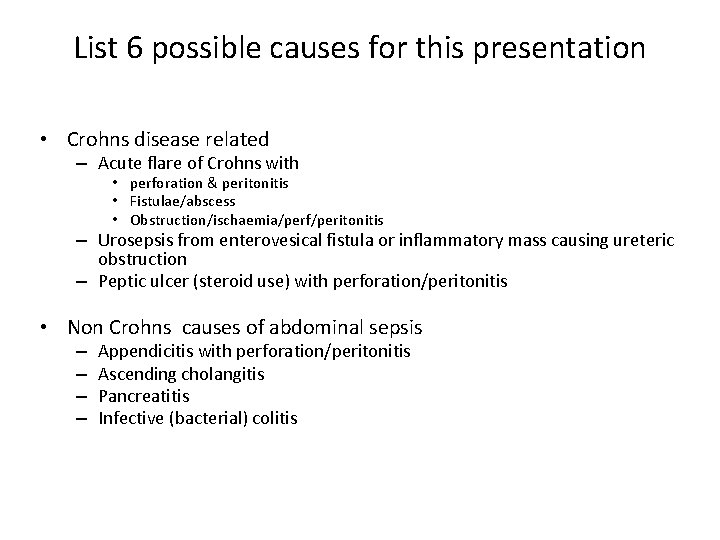
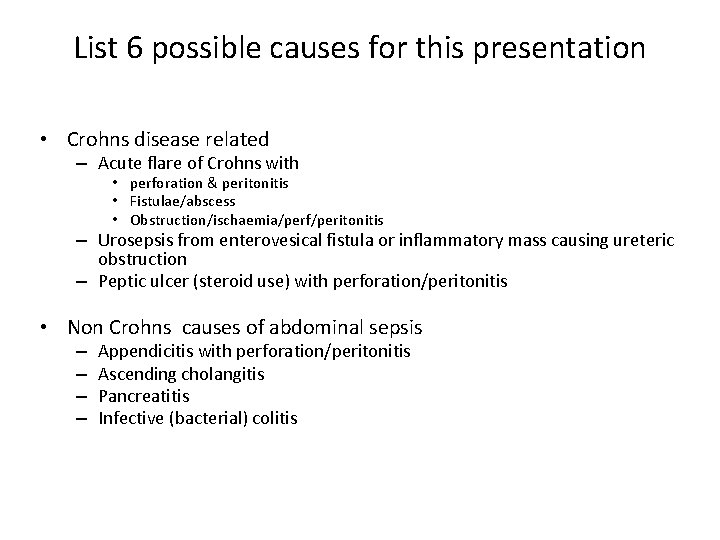
List 6 possible causes for this presentation • Crohns disease related – Acute flare of Crohns with • perforation & peritonitis • Fistulae/abscess • Obstruction/ischaemia/perf/peritonitis – Urosepsis from enterovesical fistula or inflammatory mass causing ureteric obstruction – Peptic ulcer (steroid use) with perforation/peritonitis • Non Crohns causes of abdominal sepsis – – Appendicitis with perforation/peritonitis Ascending cholangitis Pancreatitis Infective (bacterial) colitis
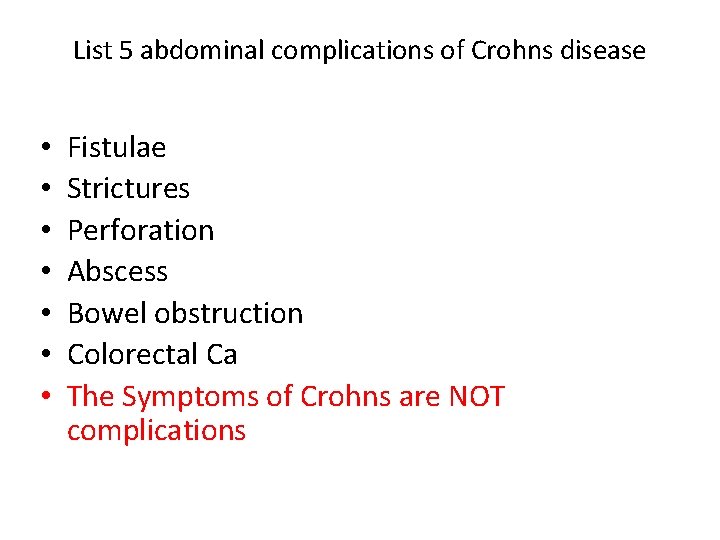
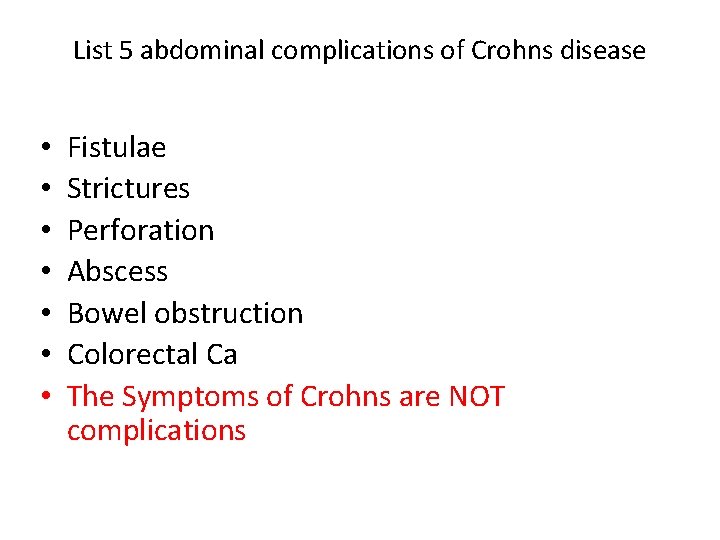
List 5 abdominal complications of Crohns disease • • Fistulae Strictures Perforation Abscess Bowel obstruction Colorectal Ca The Symptoms of Crohns are NOT complications
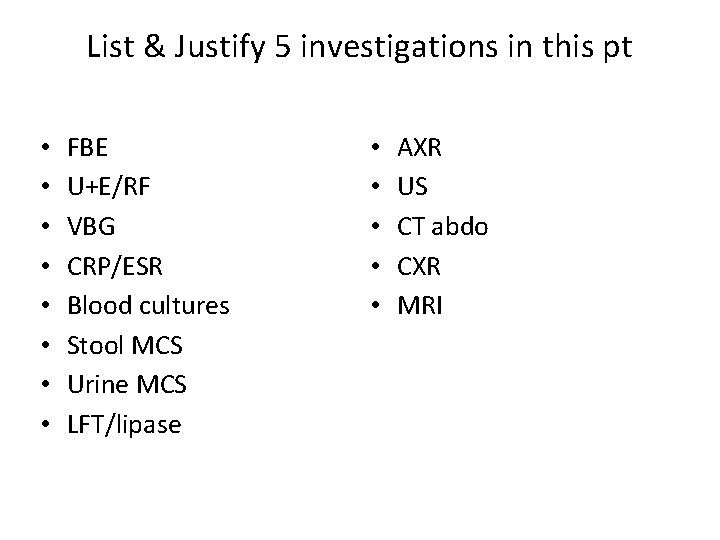
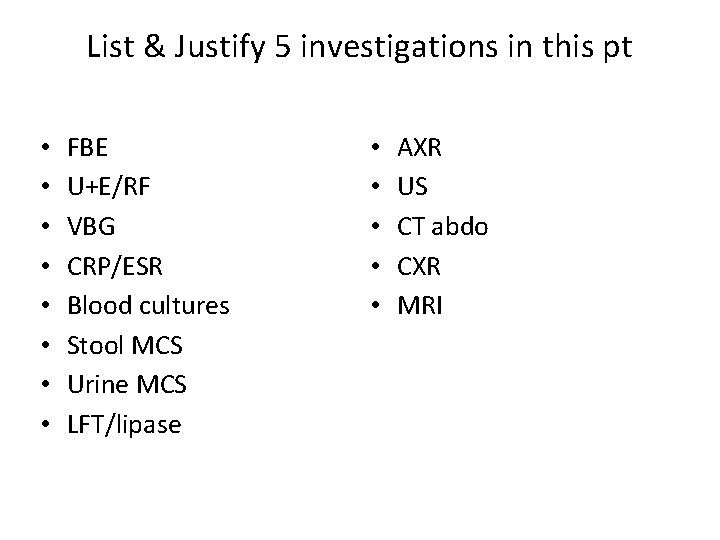
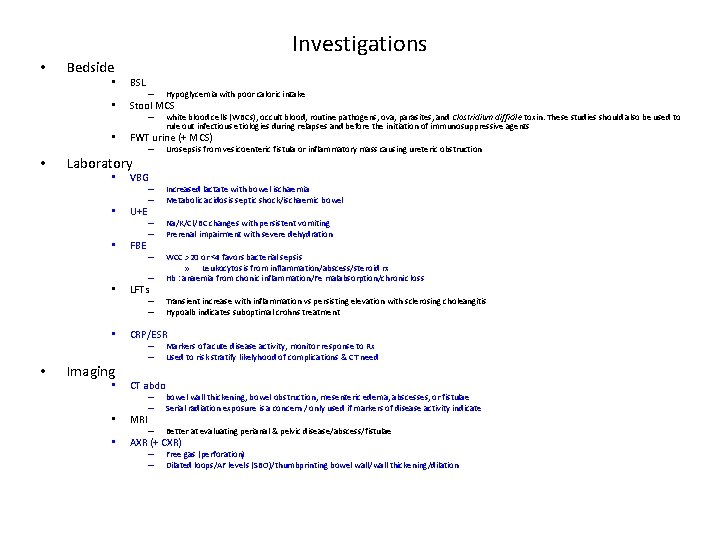
List & Justify 5 investigations in this pt • • FBE U+E/RF VBG CRP/ESR Blood cultures Stool MCS Urine MCS LFT/lipase • • • AXR US CT abdo CXR MRI
Points to consider when asked to justify or provide a satisfactory rationale – when and why you would perform the test(s) – What you would be looking for – Test utility/ or likely yield – Clinically relevant information
Features of an unsuccessful answering – Investigtion without adequate explanation • Eg FBE signs of infection – Listing investigations in a self evident fashion • Eg U+ E to check for electrolyte abnormalities • CRP/ESR – inflammatory markers – Investigations showing no clinical perspective • Eg CXR for pneumonia in this pt – Omitting key investigations – Writing “Baseline” as justification for investigations
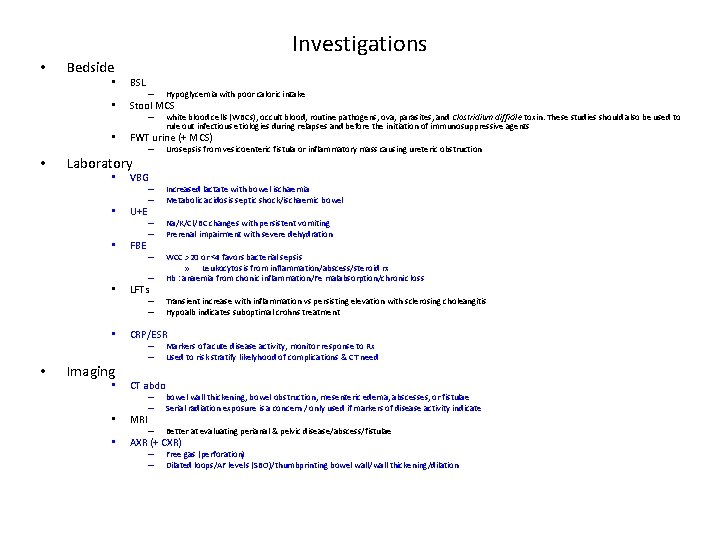
Investigations • Bedside • BSL • Stool MCS • • Imaging • Hypoglycemia with poor caloric intake – white blood cells (WBCs), occult blood, routine pathogens, ova, parasites, and Clostridium difficile toxin. These studies should also be used to rule out infectious etiologies during relapses and before the initiation of immunosuppressive agents FWT urine (+ MCS) Laboratory • – – VBG U+E FBE Urosepsis from vesicoenteric fistula or inflammatory mass causing ureteric obstruction – – Increased lactate with bowel ischaemia Metabolic acidosis septic shock/ischaemic bowel – – Na/K/Cl/BC changes with persistent vomiting Prerenal impairment with severe dehydration – – WCC >20 or <4 favors bacterial sepsis » Leukocytosis from inflammation/abscess/steroid rx Hb : anaemia from chonic inflammation/Fe malabsorption/chronic loss – – Transient increase with inflammation vs persisting elevation with sclerosing choleangitis Hypoalb indicates suboptimal crohns treatment LFTs CRP/ESR – – Markers of acute disease activity, monitor response to Rx Used to risk stratify likelyhood of complications & CT need CT abdo – – bowel wall thickening, bowel obstruction, mesenteric edema, abscesses, or fistulae Serial radiation exposure is a concern / only used if markers of disease activity indicate – Better at evaluating perianal & pelvic disease/abscess/fistulae – – Free gas (perforation) Dilated loops/AF levels (SBO)/thumbprinting bowel wall/wall thickening/dilation • MRI • AXR (+ CXR)
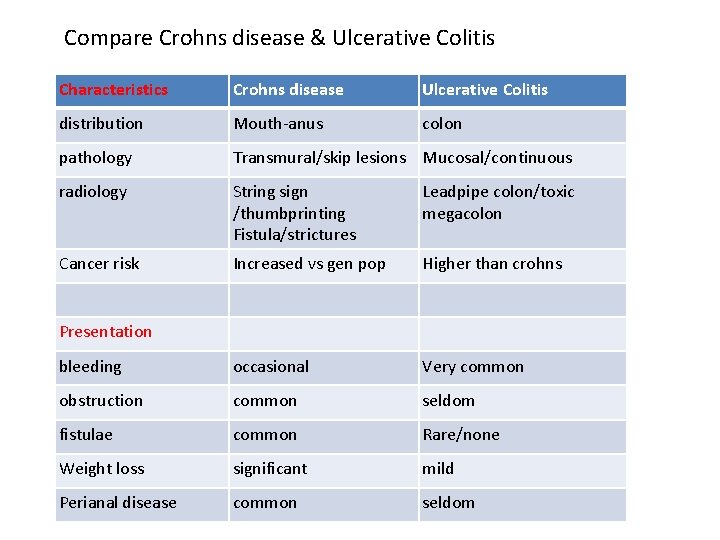
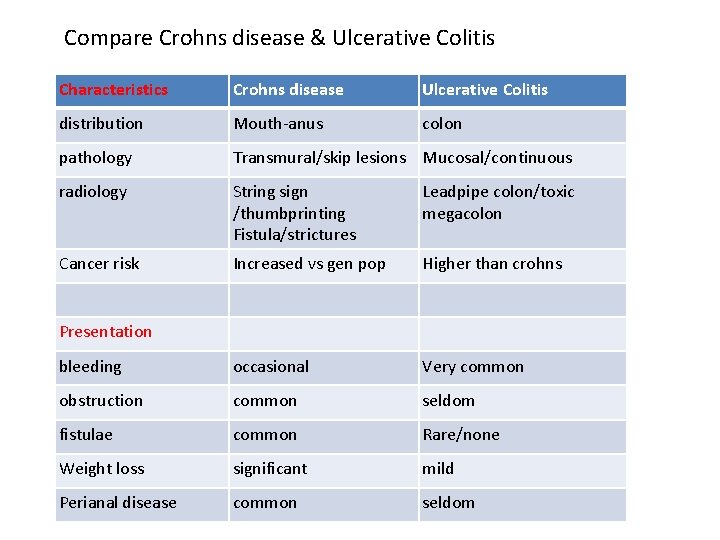
Compare Crohns disease & Ulcerative Colitis Characteristics Crohns disease Ulcerative Colitis distribution Mouth-anus colon pathology Transmural/skip lesions Mucosal/continuous radiology String sign /thumbprinting Fistula/strictures Leadpipe colon/toxic megacolon Cancer risk Increased vs gen pop Higher than crohns bleeding occasional Very common obstruction common seldom fistulae common Rare/none Weight loss significant mild Perianal disease common seldom Presentation