Salvage of Speech with Secondary Tissue Augmenting Furlow
- Slides: 1
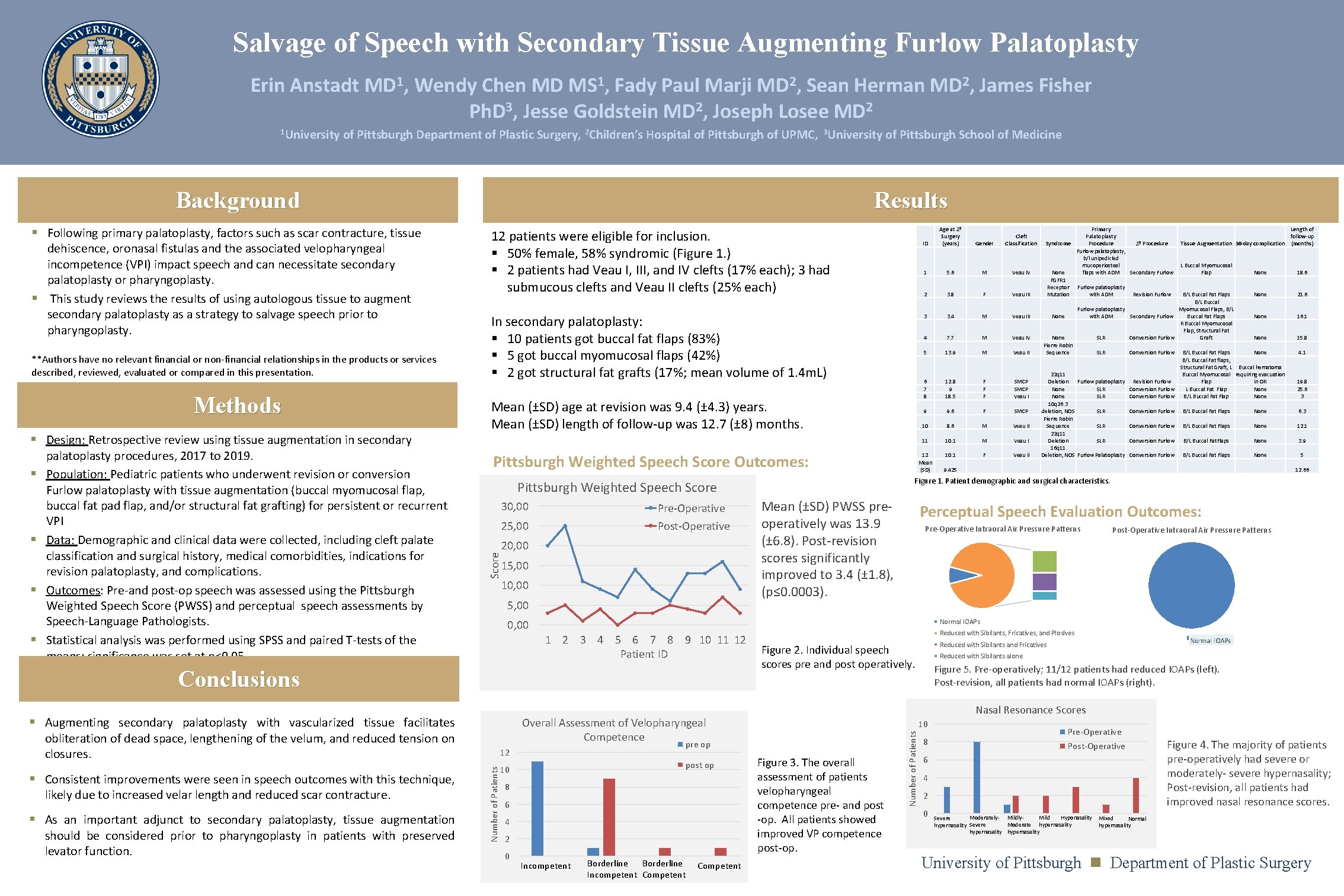
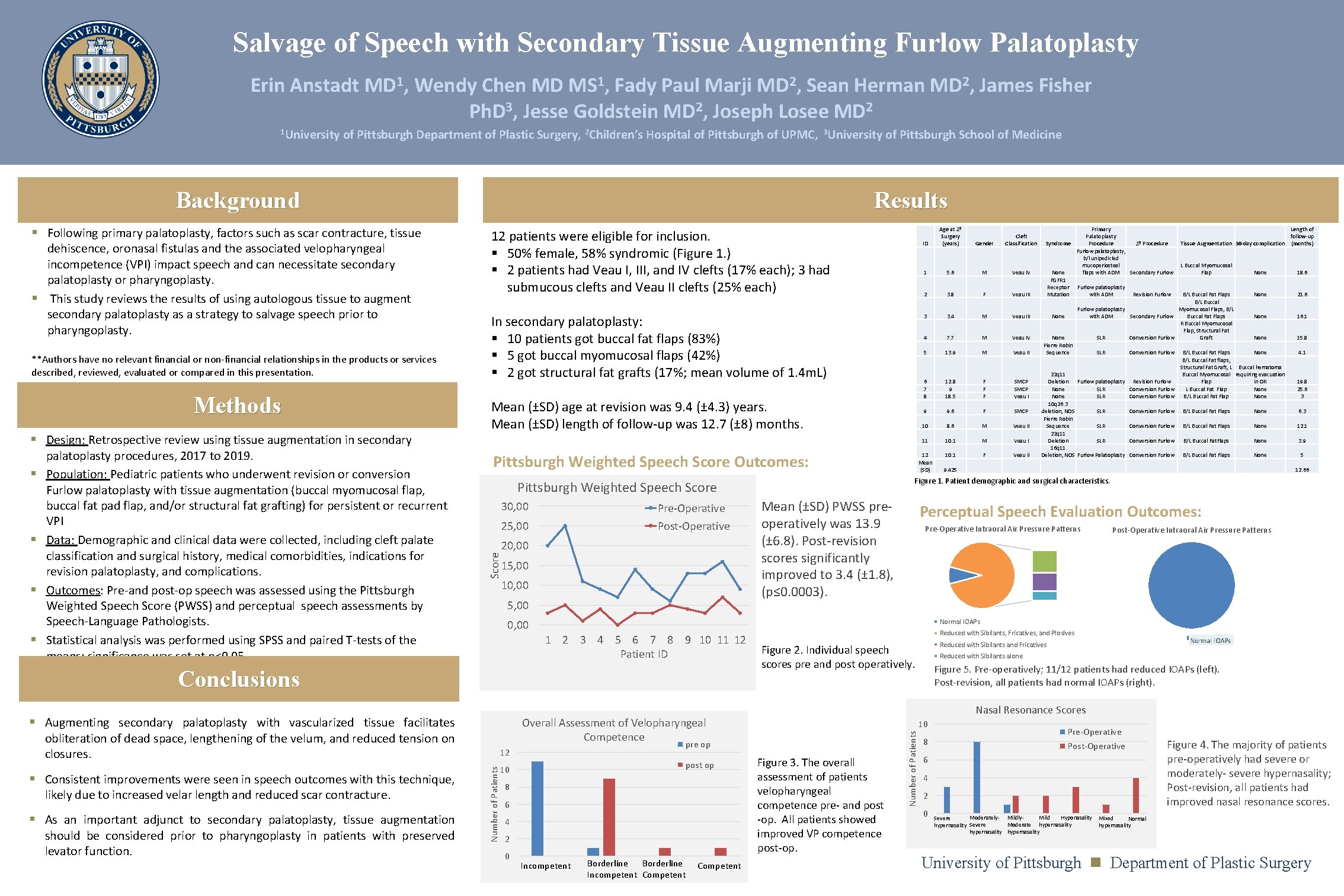
Salvage of Speech with Secondary Tissue Augmenting Furlow Palatoplasty Erin Anstadt MD 1, Wendy Chen MD MS 1, Fady Paul Marji MD 2, Sean Herman MD 2, James Fisher Ph. D 3, Jesse Goldstein MD 2, Joseph Losee MD 2 of Pittsburgh Department of Plastic Surgery, 2 Children’s Hospital of Pittsburgh of UPMC, 3 University of Pittsburgh School of Medicine Background dehiscence, oronasal fistulas and the associated velopharyngeal incompetence (VPI) impact speech and can necessitate secondary palatoplasty or pharyngoplasty. § This study reviews the results of using autologous tissue to augment secondary palatoplasty as a strategy to salvage speech prior to pharyngoplasty. **Authors have no relevant financial or non-financial relationships in the products or services described, reviewed, evaluated or compared in this presentation. Methods § Design: Retrospective review using tissue augmentation in secondary § § palatoplasty procedures, 2017 to 2019. Population: Pediatric patients who underwent revision or conversion Furlow palatoplasty with tissue augmentation (buccal myomucosal flap, buccal fat pad flap, and/or structural fat grafting) for persistent or recurrent VPI Data: Demographic and clinical data were collected, including cleft palate classification and surgical history, medical comorbidities, indications for revision palatoplasty, and complications. Outcomes: Pre-and post-op speech was assessed using the Pittsburgh Weighted Speech Score (PWSS) and perceptual speech assessments by Speech-Language Pathologists. Statistical analysis was performed using SPSS and paired T-tests of the means; significance was set at p<0. 05 12 patients were eligible for inclusion. § 50% female, 58% syndromic (Figure 1. ) § 2 patients had Veau I, III, and IV clefts (17% each); 3 had submucous clefts and Veau II clefts (25% each) In secondary palatoplasty: § 10 patients got buccal fat flaps (83%) § 5 got buccal myomucosal flaps (42%) § 2 got structural fat grafts (17%; mean volume of 1. 4 m. L) Mean (±SD) age at revision was 9. 4 (± 4. 3) years. Mean (±SD) length of follow-up was 12. 7 (± 8) months. Pittsburgh Weighted Speech Score Outcomes: 30, 00 Pre-Operative Post-Operative 25, 00 20, 00 15, 00 10, 00 5, 00 should be considered prior to pharyngoplasty in patients with preserved levator function. 1 5. 6 M Veau IV 2 3. 8 F Veau III 3 3. 4 M Veau III None 4 7. 7 M Veau IV 5 13. 9 M Veau II None Pierre Robin Sequence 6 7 8 12. 8 9 18. 5 F F F SMCP Veau I 9 9. 6 F SMCP 10 8. 6 M Veau II 11 10. 1 M Veau I 12 Mean (SD) 10. 1 F Veau ii post op 10 8 6 4 2 0 Length of follow-up Tissue Augmentation 30 -day complication (months) L Buccal Myomucosal Flap B/L Buccal Fat Flaps B/L Buccal Furlow palatoplasty Myomucosal Flaps, B/L with ADM Secondary Furlow Buccal Fat Flaps R Buccal Myomucosal Flap, Structural Fat SLR Conversion Furlow Graft SLR Conversion Furlow 22 q 11 Deletion Furlow palatoplasty None SLR 10 q 26. 3 deletion, NOS SLR Pierre Robin Sequence SLR 22 q 11 Deletion SLR 16 q 11 Deletion, NOS Furlow Palatoplasty Revision Furlow Conversion Furlow None 18. 6 None 21. 6 None 16. 1 None 15. 8 B/L Buccal Fat Flaps None B/L Buccal Fat flaps, Structural Fat Graft, L Buccal hematoma Buccal Myomucosal requiring evacuation Flap in OR L Buccal Fat Flap None B/L Buccal Fat Flap None 4. 1 19. 8 25. 6 3 Conversion Furlow B/L Buccal Fat Flaps None 6. 3 Conversion Furlow B/L Buccal Fat Flaps None 12. 1 Conversion Furlow B/L Buccal Fat. Flaps None 3. 9 Conversion Furlow B/L Buccal Fat Flaps None 5 9. 425 12. 66 Perceptual Speech Evaluation Outcomes: Pre-Operative Intraoral Air Pressure Patterns Post-Operative Intraoral Air Pressure Patterns . Reduced with Sibilants, Fricatives, and Plosives Incompetent Borderline Incompetent Competent 1 Reduced with Sibilants and Fricatives Figure 2. Individual speech scores pre and post operatively. Reduced with Sibilants alone Figure 5. Pre-operatively; 11/12 patients had reduced IOAPs (left). Post-revision, all patients had normal IOAPs (right). Nasal Resonance Scores 10 pre op 12 Number of Patients § As an important adjunct to secondary palatoplasty, tissue augmentation Mean (±SD) PWSS preoperatively was 13. 9 (± 6. 8). Post-revision scores significantly improved to 3. 4 (± 1. 8), (p≤ 0. 0003). Overall Assessment of Velopharyngeal Competence obliteration of dead space, lengthening of the velum, and reduced tension on closures. Primary Palatoplasty Syndrome Procedure 2º Procedure Furlow palatoplasty, b/l unipedicled mucoperiosteal None flaps with ADM Secondary Furlow FGFR 1 Receptor Furlow palatoplasty Mutation with ADM Revision Furlow Normal IOAPs 1 2 3 4 5 6 7 8 9 10 11 12 Patient ID § Augmenting secondary palatoplasty with vascularized tissue facilitates likely due to increased velar length and reduced scar contracture. Gender Cleft Classification 0, 00 Conclusions § Consistent improvements were seen in speech outcomes with this technique, ID Age at 2º Surgery (years) Figure 1. Patient demographic and surgical characteristics. Pittsburgh Weighted Speech Score § Following primary palatoplasty, factors such as scar contracture, tissue Results Figure 3. The overall assessment of patients velopharyngeal competence pre- and post -op. All patients showed improved VP competence post-op. Number of Patients 1 University Pre-Operative Post-Operative 8 6 4 2 0 Moderately- Mildly. Hyponasality Mild Severe hypernasality Moderate hypernasality Figure 4. The majority of patients pre-operatively had severe or moderately- severe hypernasality; Post-revision, all patients had improved nasal resonance scores. Mixed Normal hypernasality : University of Pittsburgh Department of Plastic Surgery