Salvage Lymph Node Dissection for Prostate Cancer Nodal




- Slides: 42
Salvage Lymph Node Dissection for Prostate Cancer Nodal Recurrence Detected by 11 C-Choline PET/CT RJ Karnes MD, FACS Vice-Chair Associate Professor and Consultant Dept. of Urology/Urologic Oncology Mayo Clinic-Rochester
Introduction • Approximately a third of radical prostatectomy (RP) patients will have a biochemical recurrence (BCR) • BCR can be indicative of a local and/or systemic relapse • 11 C-Choline PET/CT performs well in men with BCR following primary treatment failure • Nodal recurrence
Introduction • 11 C-Choline PET/CT enhances the rate of prostate cancer lesion detection by ~30% over conventional imaging • Mitchell C, et al J Urology, April ’ 13 • FDA NDA 2012 Choline C 11 - Mayo Clinic
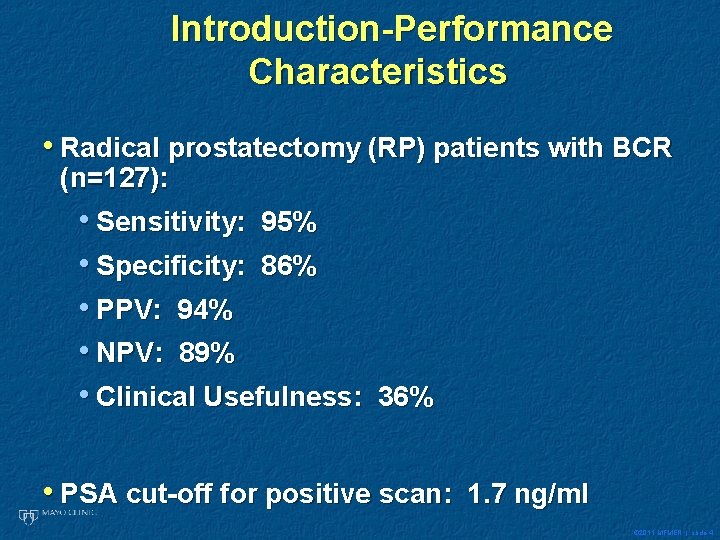
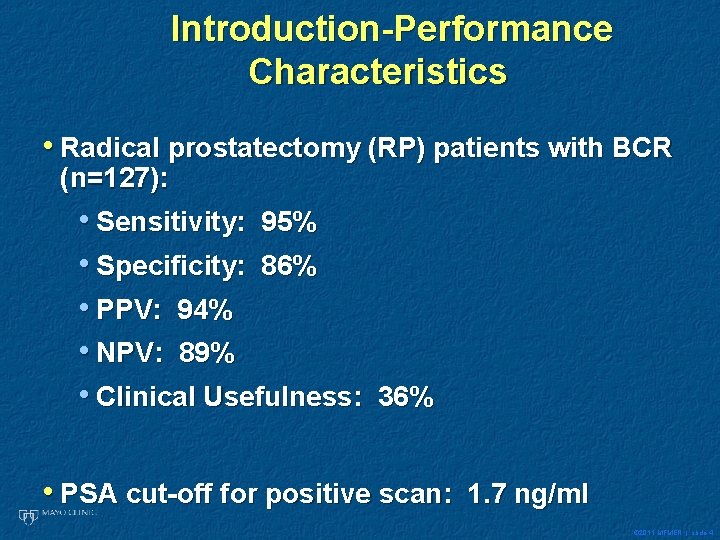
Introduction-Performance Characteristics • Radical prostatectomy (RP) patients with BCR (n=127): • Sensitivity: 95% • Specificity: 86% • PPV: 94% • NPV: 89% • Clinical Usefulness: 36% • PSA cut-off for positive scan: 1. 7 ng/ml © 2011 MFMER | slide-4
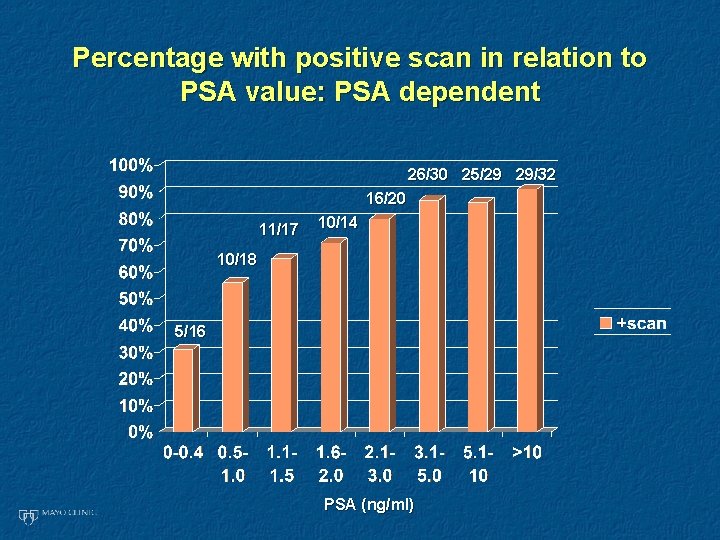
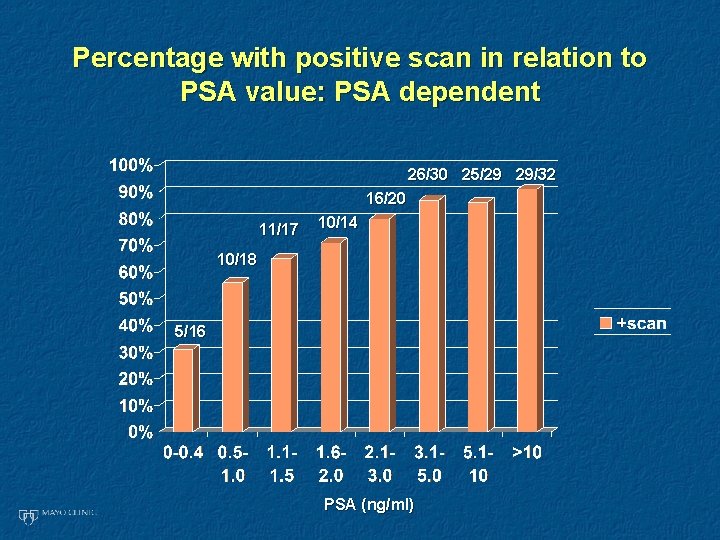
Percentage with positive scan in relation to PSA value: PSA dependent 26/30 25/29 29/32 16/20 11/17 10/14 10/18 5/16 PSA (ng/ml)
PET C 11 Choline Observations • Performs well in men with BCR following primary treatment failure (75% +) • Optimum PSA value for lesion detection is between 1. 7 - 2. 0 ng/ml • PSA kinetics did not matter (high rate of ADT/CRPC) • Generally not recommended for PSA <1 • Over 1/3 of our scans at this level were + • Patient cohort (median PSA 3. 2 at scan; others 0. 8 -2. 15 ng/ml) and higher % of adjuvant/salvage therapies © 2011 MFMER | slide-6
Introduction • In the treatment naïve man, surgery alone can be potentially curative in limited nodal (p. N+) disease • Nodal recurrence tends to have a more favorable prognosis than bone or visceral metastasis • The role of salvage lymph node dissection (s. LND) is optional - EAU guidelines
Introduction • Contemporary role of s. LND was recently reviewed • Delay clinical progression • Postpone hormonal therapy (HT) • Approximately 1/3 free of further BCR at 5 yrs • Abdollah, et al. , Eur Uro, 2014
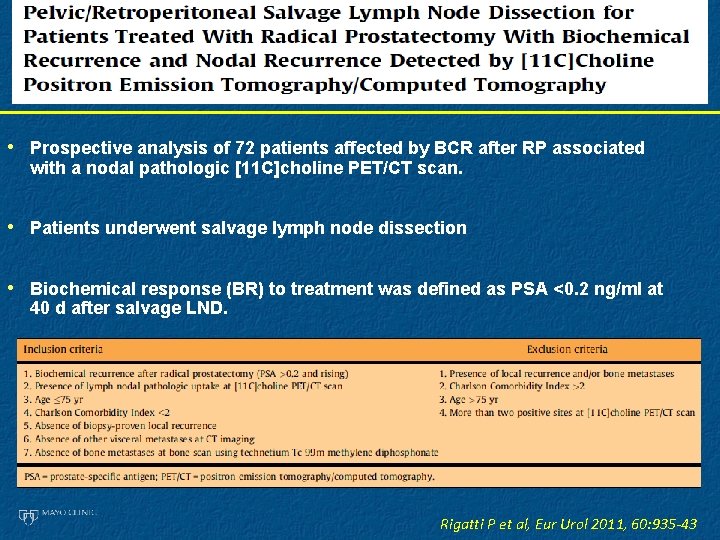
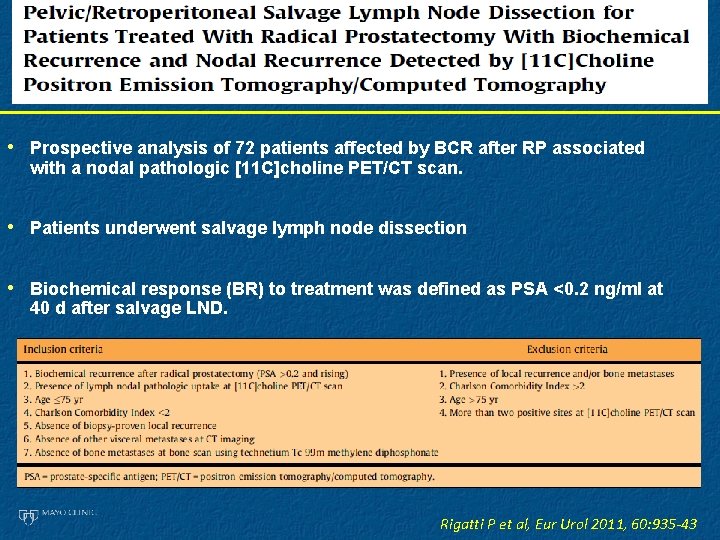
• Prospective analysis of 72 patients affected by BCR after RP associated with a nodal pathologic [11 C]choline PET/CT scan. • Patients underwent salvage lymph node dissection • Biochemical response (BR) to treatment was defined as PSA <0. 2 ng/ml at 40 d after salvage LND. Rigatti P et al, Eur Urol 2011, 60: 935 -43
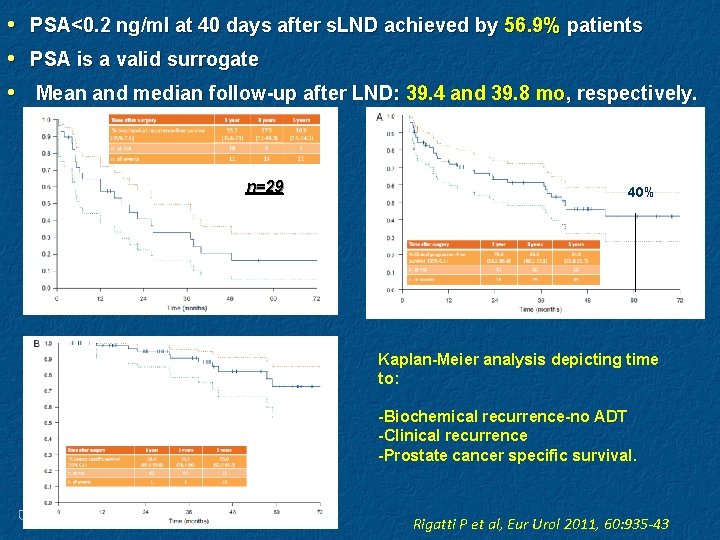
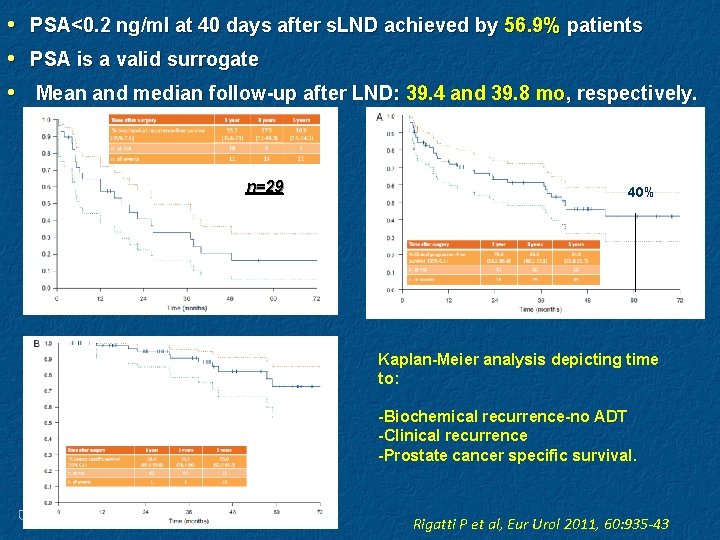
• • • PSA<0. 2 ng/ml at 40 days after s. LND achieved by 56. 9% patients PSA is a valid surrogate Mean and median follow-up after LND: 39. 4 and 39. 8 mo, respectively. n=29 40% Kaplan-Meier analysis depicting time to: -Biochemical recurrence-no ADT -Clinical recurrence -Prostate cancer specific survival. Rigatti P et al, Eur Urol 2011, 60: 935 -43
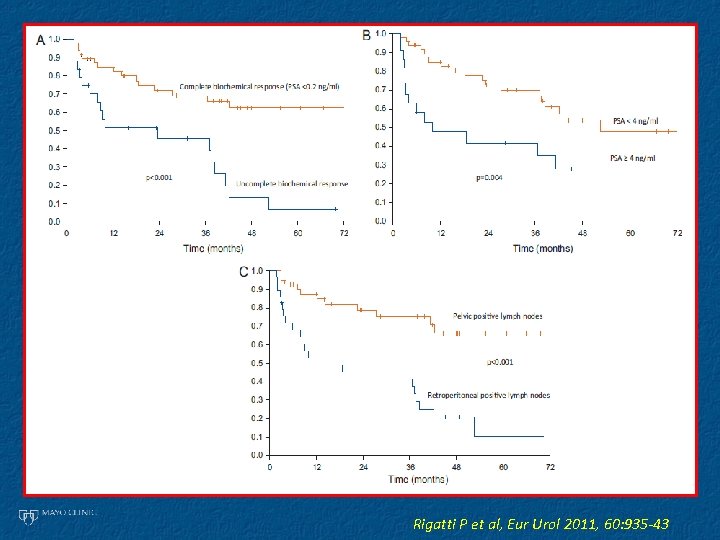
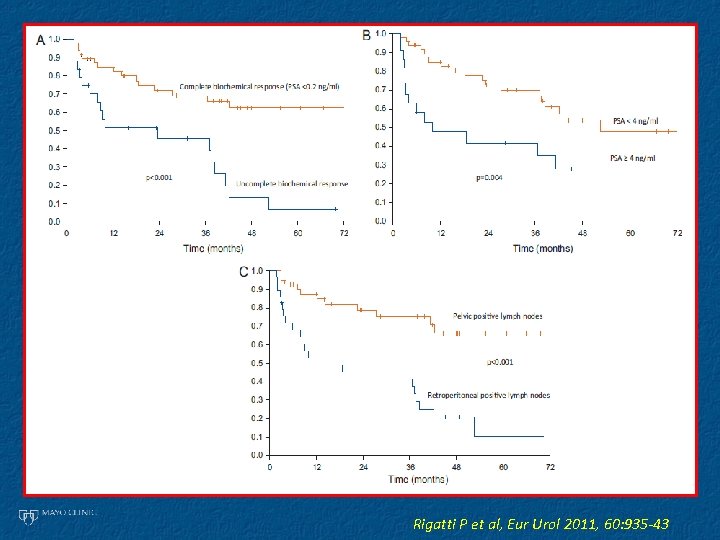
Rigatti P et al, Eur Urol 2011, 60: 935 -43

Studies reporting results of salvage LND Study # pts Mean pre-op. PSA # nodes removed Post-op. PSA < 0. 2 ng/ml Rinnab et al. 15 2. 56 NA 8% Winter et al. 11 3. 02 NA 40% Martini et al. 8 1. 62 11. 6 62% Schilling et al 10 - 7 NA Tilki et al 56 6. 0 21. 3 NA Jilg et al 47 11. 1 23. 3 46% According to the EAU guidelines the role of salvage LND is optional but still experimental, needing to be further tested in prospective clinical trials Mottet et al, Eur Urol, 59: 572 -83, 2011
Case
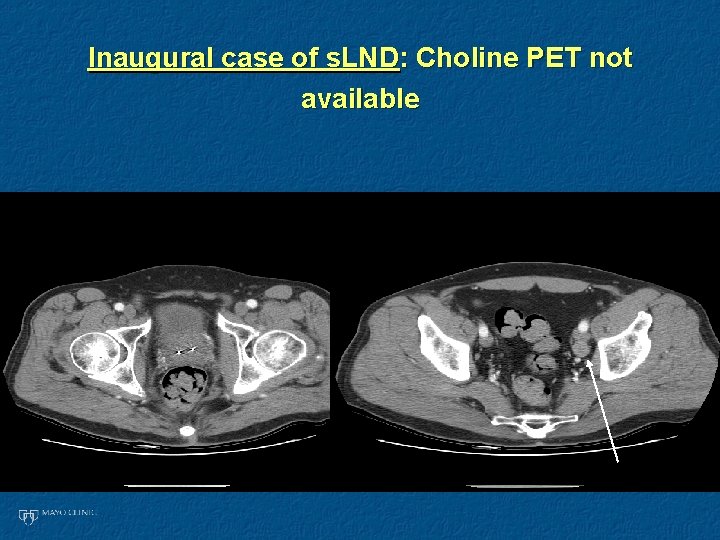
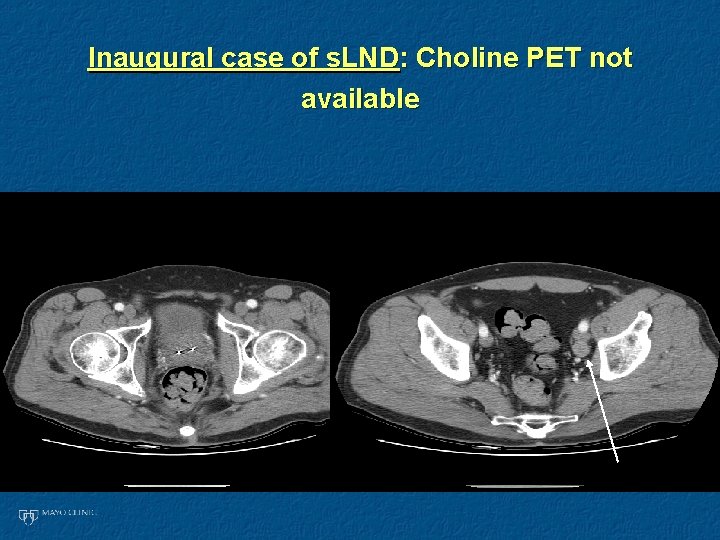
Inaugural case of s. LND: Choline PET not available
Inaugural case s. LND: Metastatectomy/organ sparing surgery for radiation failure • Biopsy of node+ for prostate ACA • One month shot of leuprolide • Refuses and says “take the node out and nothing else” • 2 nodes + for 4+4 at PLND in summer 2007 • PSA stable 0. 1 to 0. 2 to date and CT -
Case
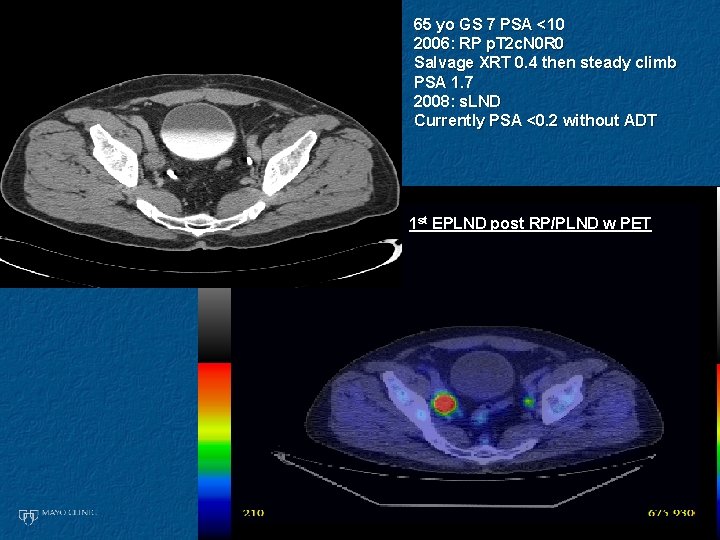
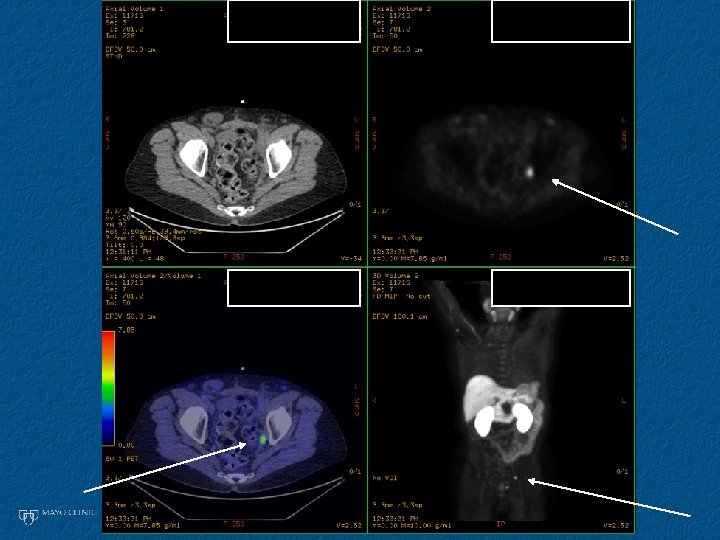
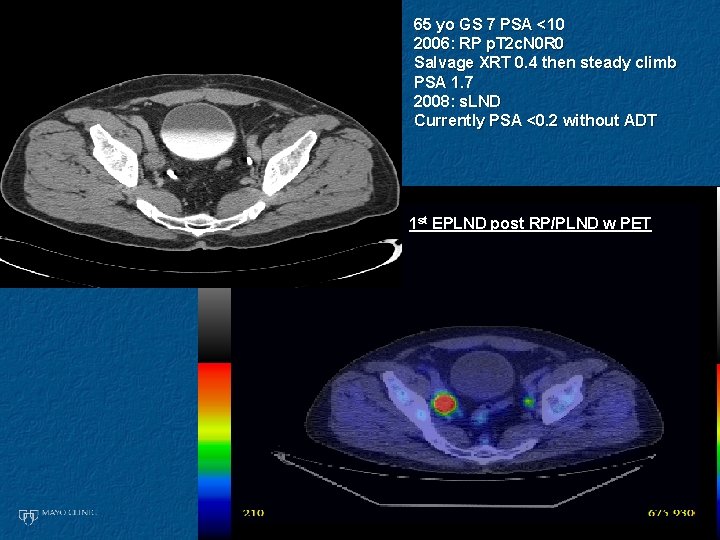
65 yo GS 7 PSA <10 2006: RP p. T 2 c. N 0 R 0 Salvage XRT 0. 4 then steady climb PSA 1. 7 2008: s. LND Currently PSA <0. 2 without ADT 1 st EPLND post RP/PLND w PET
Case

70 yo G 4+5 XRT decade earlier ADT for 6 months 2008: PSA 8. 1 ng/ml Testosterone nl 2008: s. LND Hypogastric region No ADT (metabolic syndrome) 2010: PSA <0. 1 and CT- 1 st EPLND post XRT w PET
Case
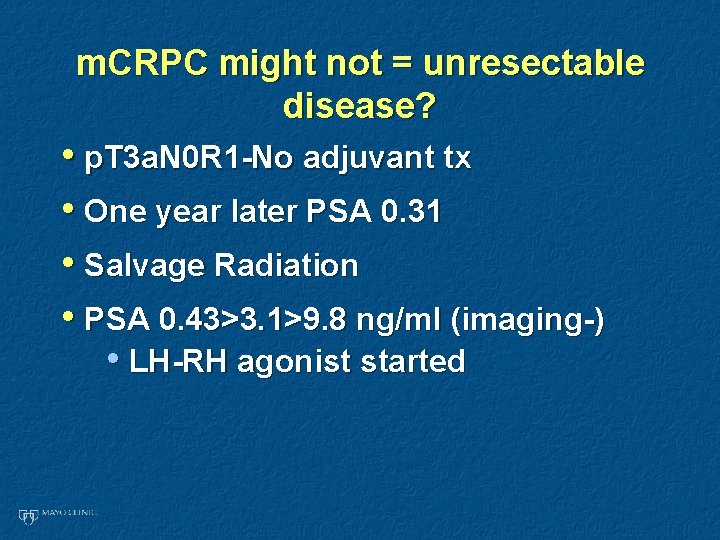
m. CRPC might not = unresectable disease? • p. T 3 a. N 0 R 1 -No adjuvant tx • One year later PSA 0. 31 • Salvage Radiation • PSA 0. 43>3. 1>9. 8 ng/ml (imaging-) • LH-RH agonist started
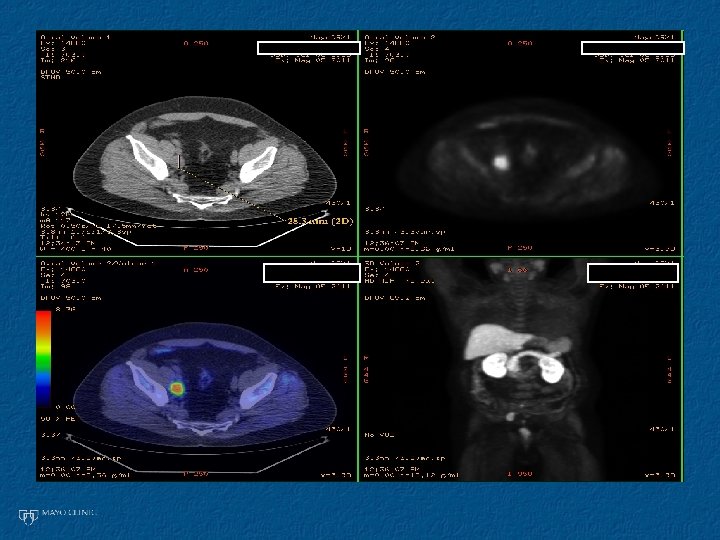
• PSA drops to 3. 2 ng/ml • Starts rising: Secondary hormonal manipulation • Referred to Medical Oncology • CRPC -PSA 14 ng/ml one year later (post ADT) • PET-CT C 11 Choline scan ordered
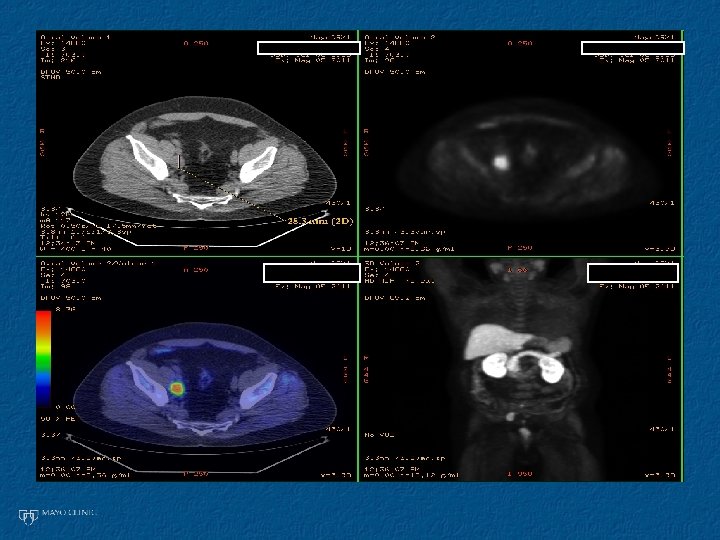
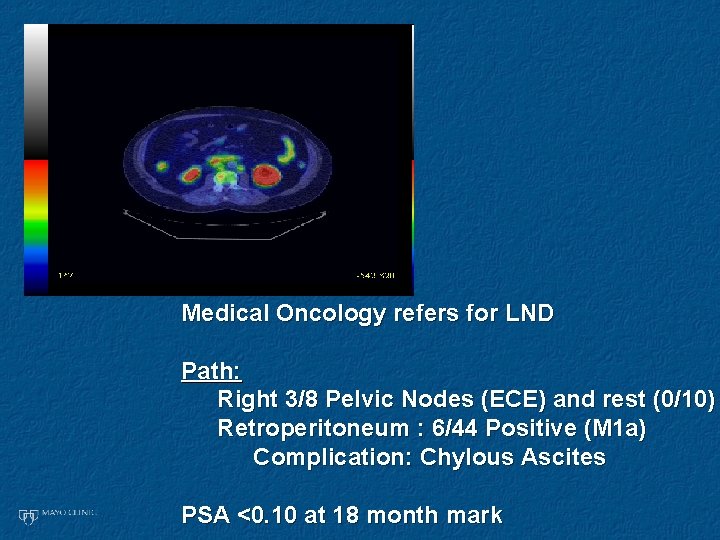
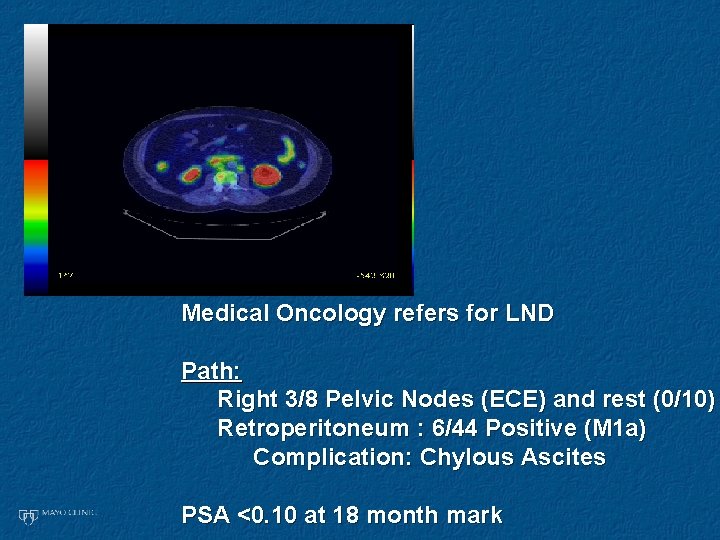
Medical Oncology refers for LND Path: Right 3/8 Pelvic Nodes (ECE) and rest (0/10) Retroperitoneum : 6/44 Positive (M 1 a) Complication: Chylous Ascites PSA <0. 10 at 18 month mark
Case

52 yo s/p dv. P for p. N+: MRI and PET-CT same 2 years CAB PSA 2. 4
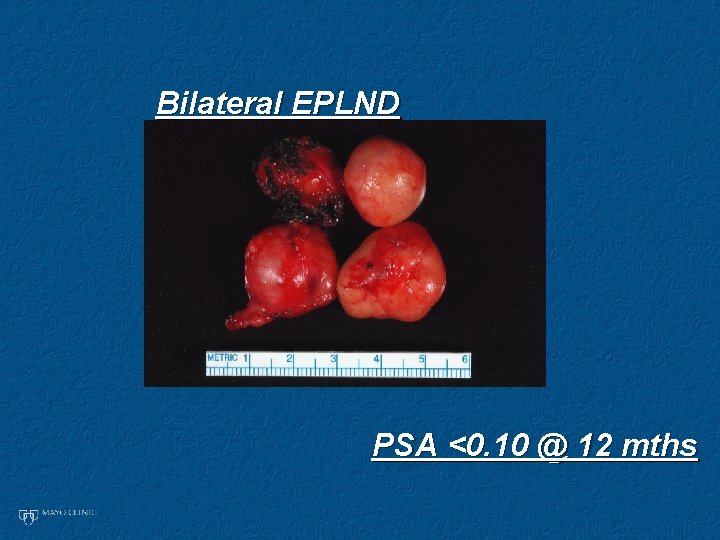
Bilateral EPLND PSA <0. 10 @ 12 mths
Objective • Report the largest series in the U. S. of s. LND targeting 11 C Choline PET avid nodes in the setting of BCR

Methods • Retrospective analysis of a prospectively kept database of bilateral s. LNDs using 11 C Choline PET by a single surgeon (RJK) • Only previously treated RP+/-LND patients were included and the main surgical intent was s. LND • Primary endpoints: BCR and systemic progression • Evaluation by Kaplan Meier analysis
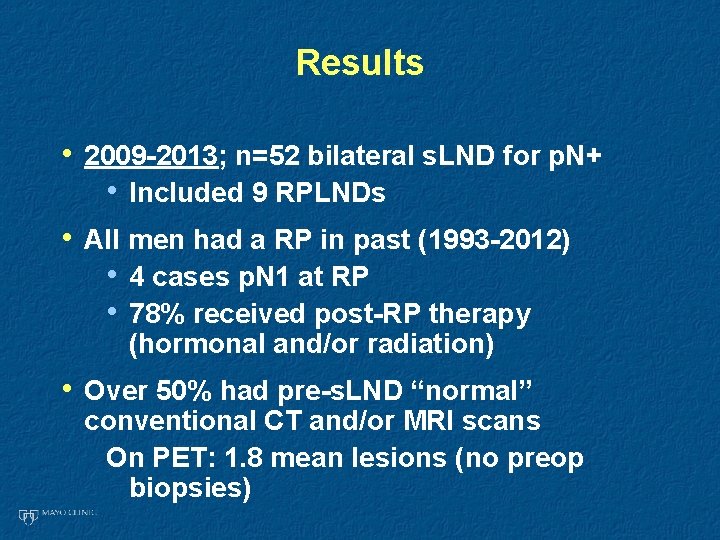
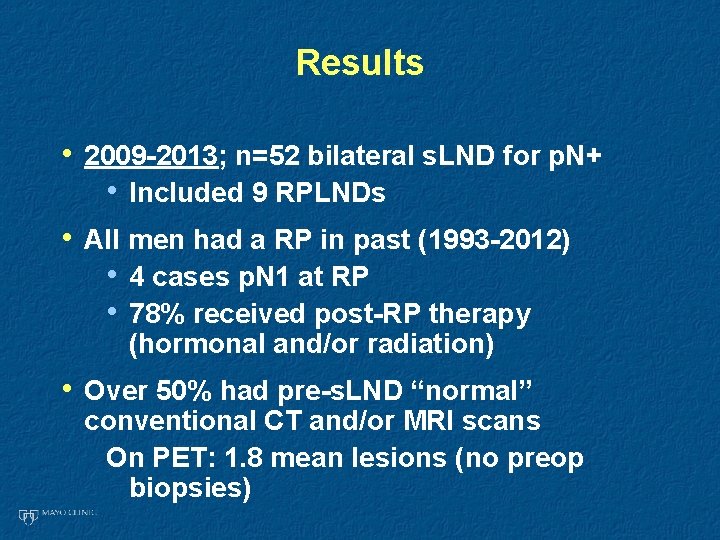
Results • 2009 -2013; n=52 bilateral s. LND for p. N+ • Included 9 RPLNDs • All men had a RP in past (1993 -2012) • 4 cases p. N 1 at RP • 78% received post-RP therapy (hormonal and/or radiation) • Over 50% had pre-s. LND “normal” conventional CT and/or MRI scans On PET: 1. 8 mean lesions (no preop biopsies)
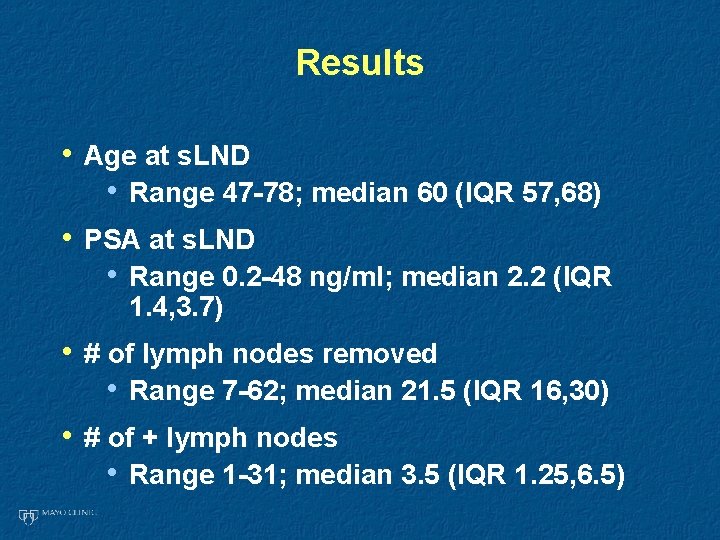
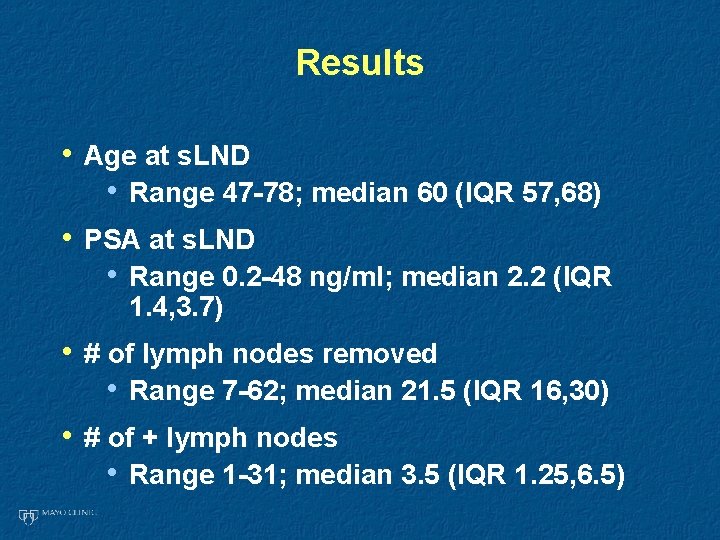
Results • Age at s. LND • Range 47 -78; median 60 (IQR 57, 68) • PSA at s. LND • Range 0. 2 -48 ng/ml; median 2. 2 (IQR 1. 4, 3. 7) • # of lymph nodes removed • Range 7 -62; median 21. 5 (IQR 16, 30) • # of + lymph nodes • Range 1 -31; median 3. 5 (IQR 1. 25, 6. 5)
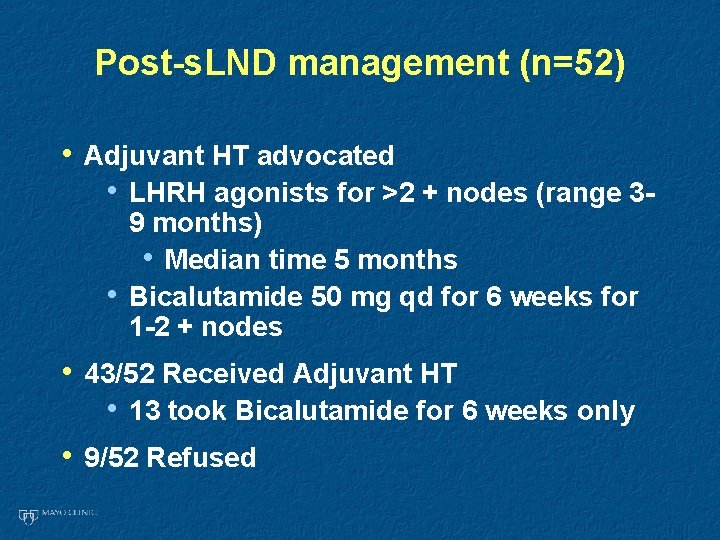
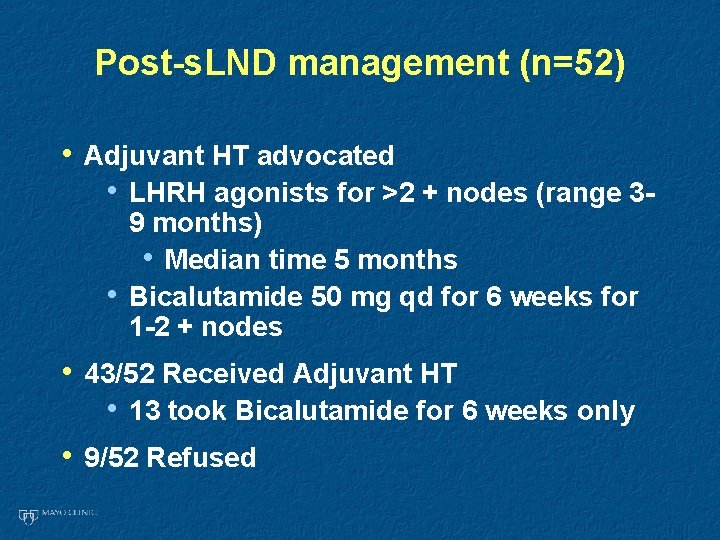
Post-s. LND management (n=52) • Adjuvant HT advocated • LHRH agonists for >2 + nodes (range 3 • 9 months) • Median time 5 months Bicalutamide 50 mg qd for 6 weeks for 1 -2 + nodes • 43/52 Received Adjuvant HT • 13 took Bicalutamide for 6 weeks only • 9/52 Refused
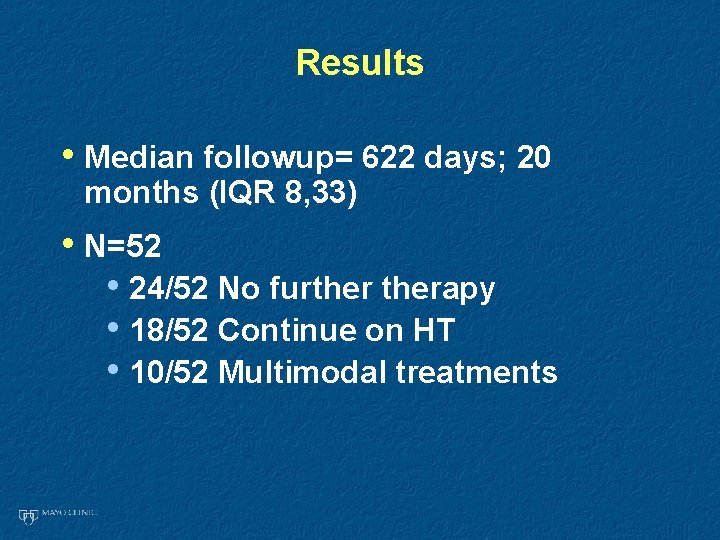
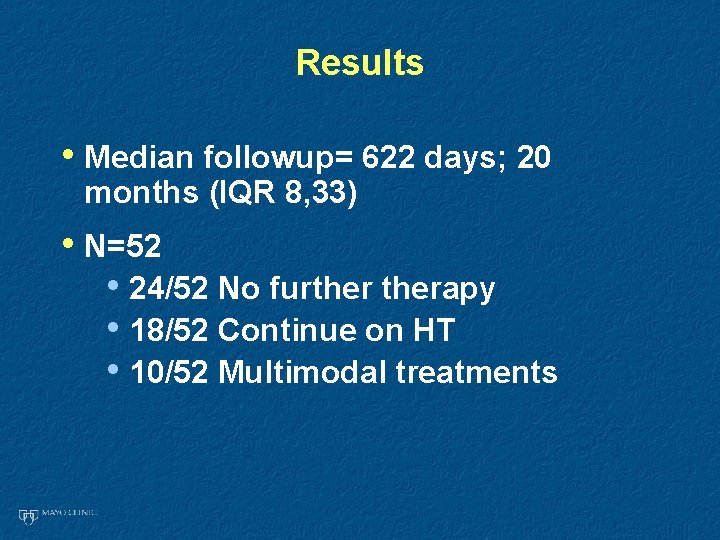
Results • Median followup= 622 days; 20 months (IQR 8, 33) • N=52 • 24/52 No furtherapy • 18/52 Continue on HT • 10/52 Multimodal treatments
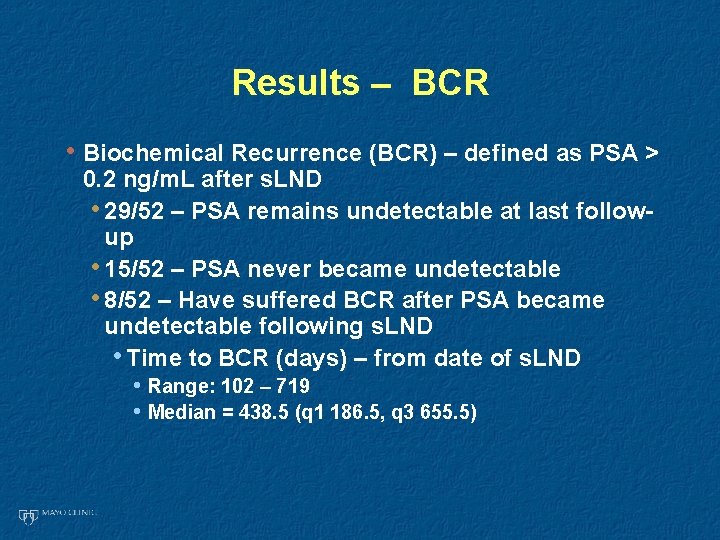
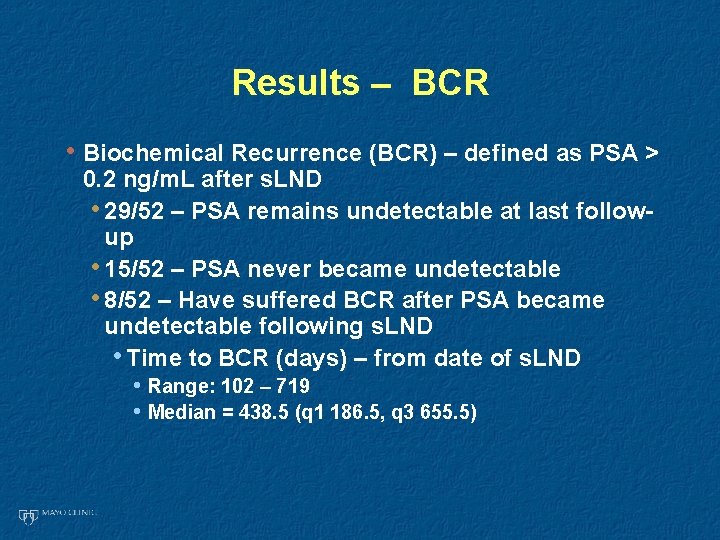
Results – BCR • Biochemical Recurrence (BCR) – defined as PSA > 0. 2 ng/m. L after s. LND • 29/52 – PSA remains undetectable at last followup • 15/52 – PSA never became undetectable • 8/52 – Have suffered BCR after PSA became undetectable following s. LND • Time to BCR (days) – from date of s. LND • Range: 102 – 719 • Median = 438. 5 (q 1 186. 5, q 3 655. 5)
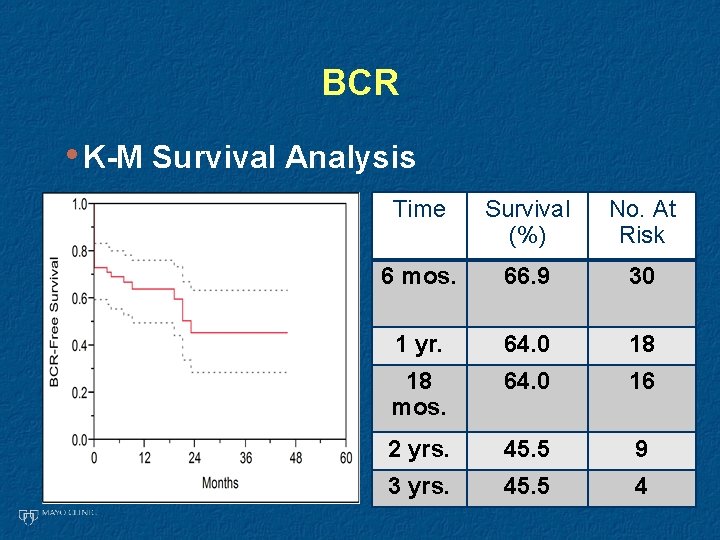
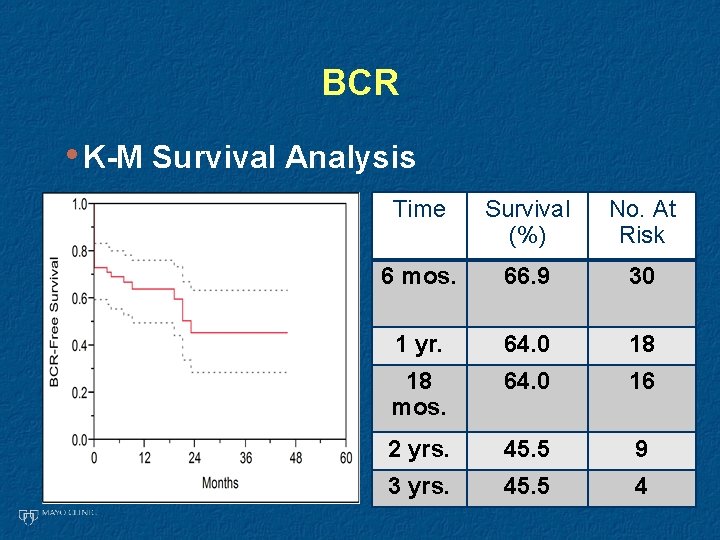
BCR • K-M Survival Analysis Time Survival (%) No. At Risk 6 mos. 66. 9 30 1 yr. 64. 0 18 18 mos. 64. 0 16 2 yrs. 45. 5 9 3 yrs. 45. 5 4
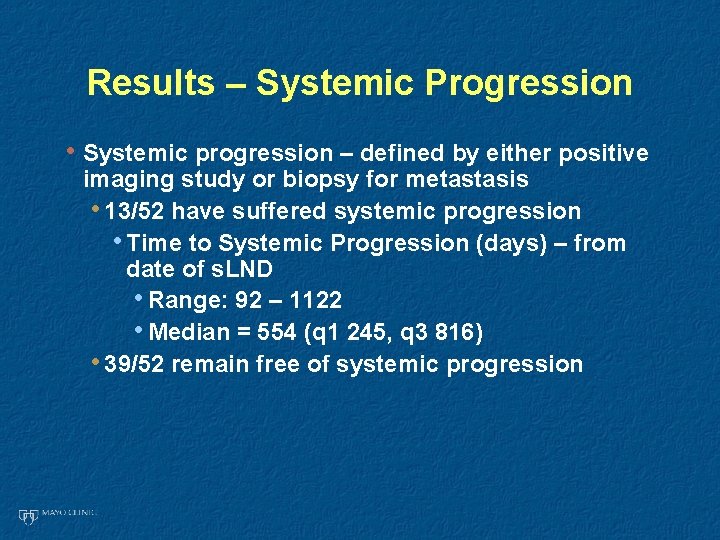
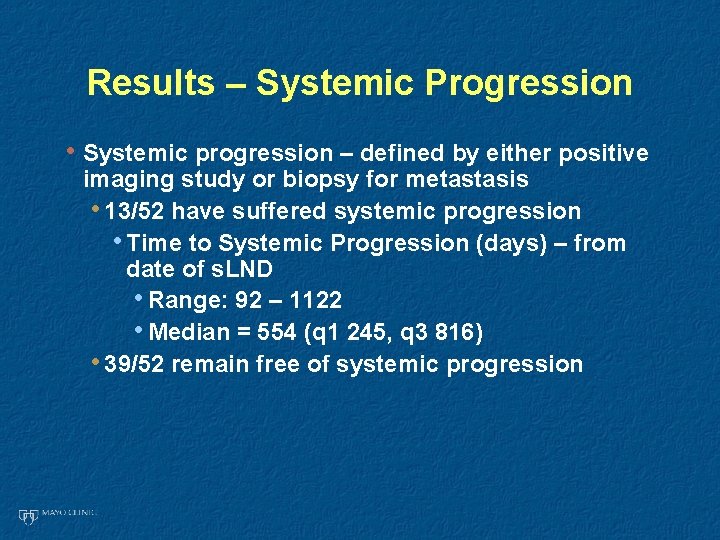
Results – Systemic Progression • Systemic progression – defined by either positive imaging study or biopsy for metastasis • 13/52 have suffered systemic progression • Time to Systemic Progression (days) – from date of s. LND • Range: 92 – 1122 • Median = 554 (q 1 245, q 3 816) • 39/52 remain free of systemic progression
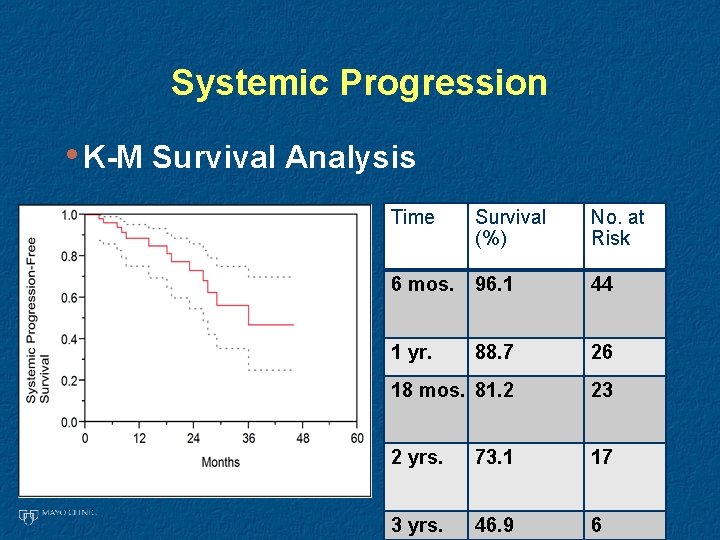
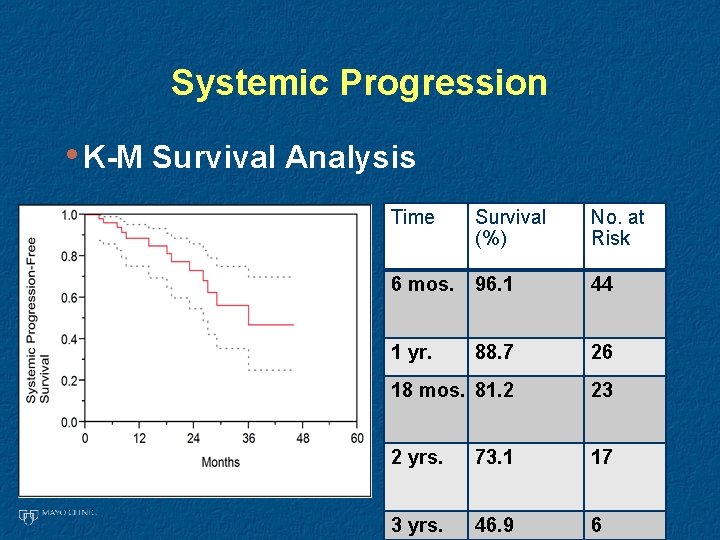
Systemic Progression • K-M Survival Analysis Time Survival (%) No. at Risk 6 mos. 96. 1 44 1 yr. 88. 7 26 18 mos. 81. 2 23 2 yrs. 73. 1 17 3 yrs. 46. 9 6
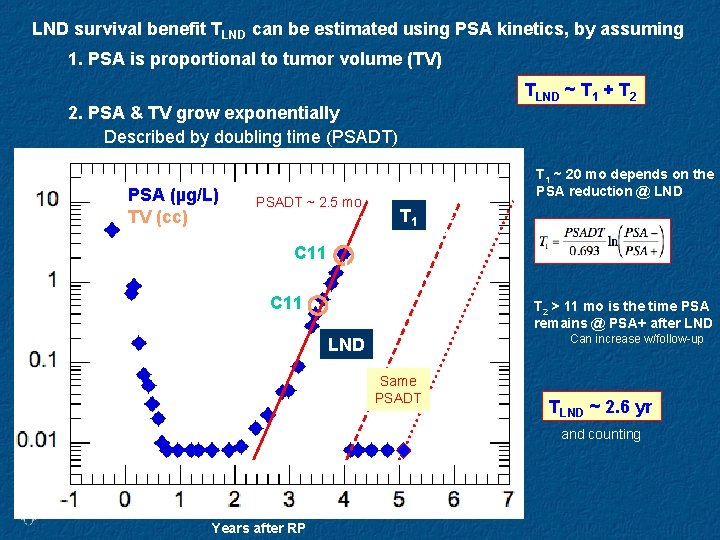
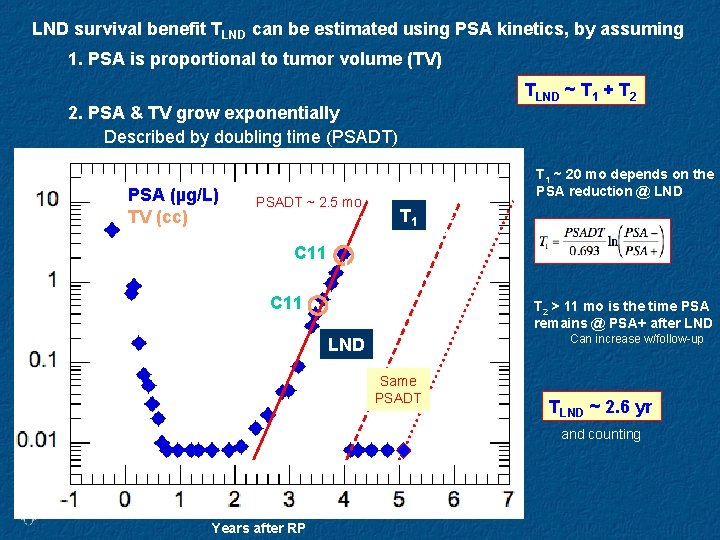
LND survival benefit TLND can be estimated using PSA kinetics, by assuming 1. PSA is proportional to tumor volume (TV) TLND ~ T 1 + T 2 2. PSA & TV grow exponentially Described by doubling time (PSADT) PSA (µg/L) TV (cc) T 1 ~ 20 mo depends on the PSA reduction @ LND PSADT ~ 2. 5 mo C 11 T 1 PSA- C 11 T 2 > 11 mo is the time PSA remains @ PSA+ after LND Can increase w/follow-up LND Same PSADT PSA+ Years after RP T 2 TLND ~ 2. 6 yr and counting
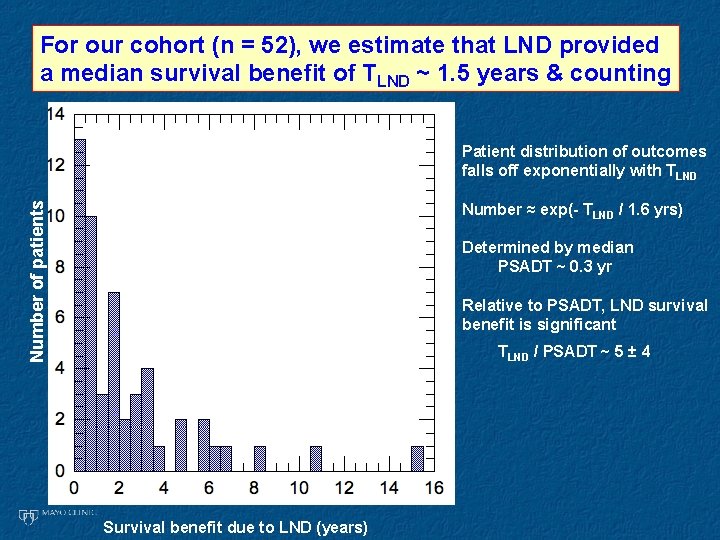
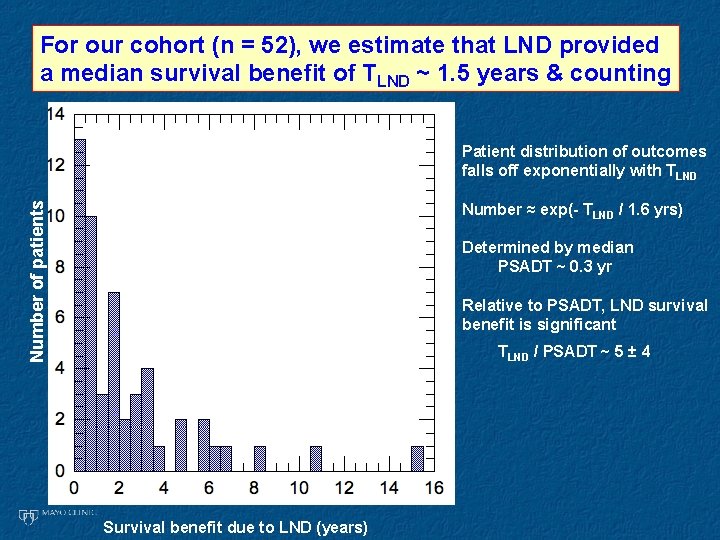
For our cohort (n = 52), we estimate that LND provided a median survival benefit of TLND ~ 1. 5 years & counting Number of patients Patient distribution of outcomes falls off exponentially with TLND Number ≈ exp(- TLND / 1. 6 yrs) Determined by median PSADT ~ 0. 3 yr Relative to PSADT, LND survival benefit is significant TLND / PSADT ~ 5 ± 4 Survival benefit due to LND (years)
Discussion • Univariate: Nothing significant • Heterogenous population • Non-randomized • No comparable control group
Conclusion • Valid treatment option • PSA as surrogate of tumor volume • Most derive some benefit (PSA decreased) • Some derive much (PSA <0. 2) • Deserves further study • Imaging: PET-CT vs other • Ideal patient not yet defined