Saltatory pattern with wide variability The oscillations of
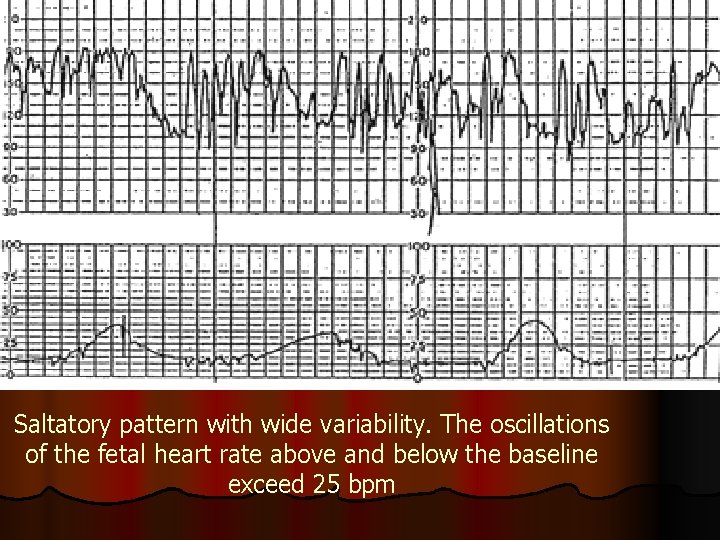
Saltatory pattern with wide variability. The oscillations of the fetal heart rate above and below the baseline exceed 25 bpm
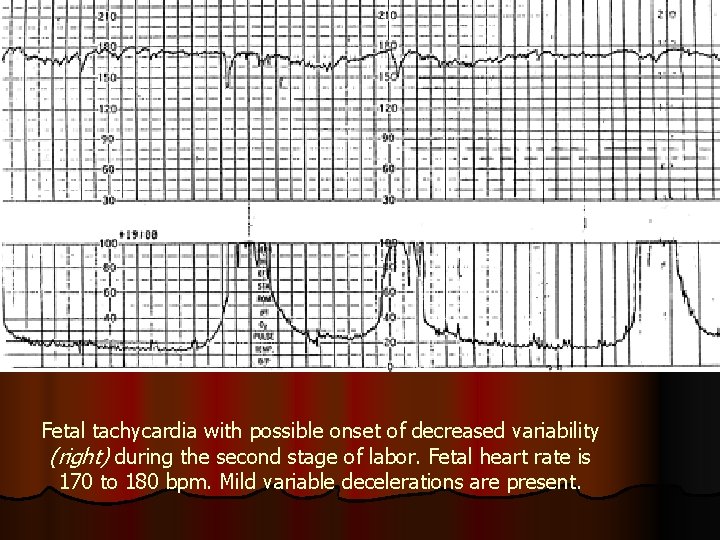
Fetal tachycardia with possible onset of decreased variability (right) during the second stage of labor. Fetal heart rate is 170 to 180 bpm. Mild variable decelerations are present.
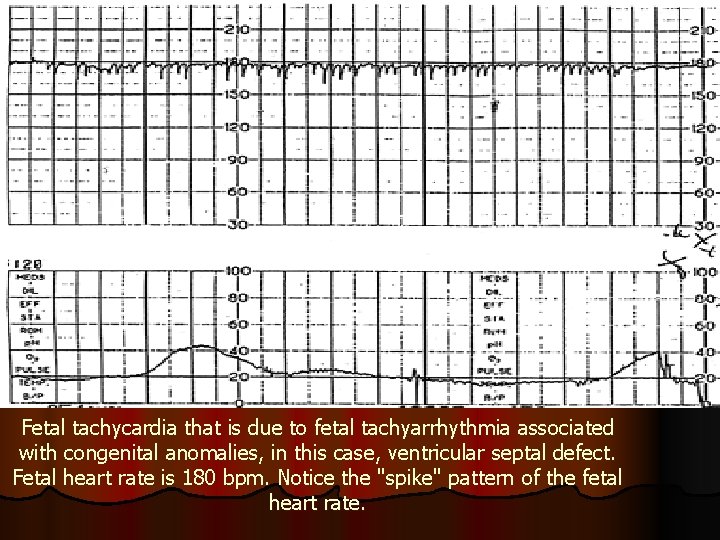
Fetal tachycardia that is due to fetal tachyarrhythmia associated with congenital anomalies, in this case, ventricular septal defect. Fetal heart rate is 180 bpm. Notice the "spike" pattern of the fetal heart rate.
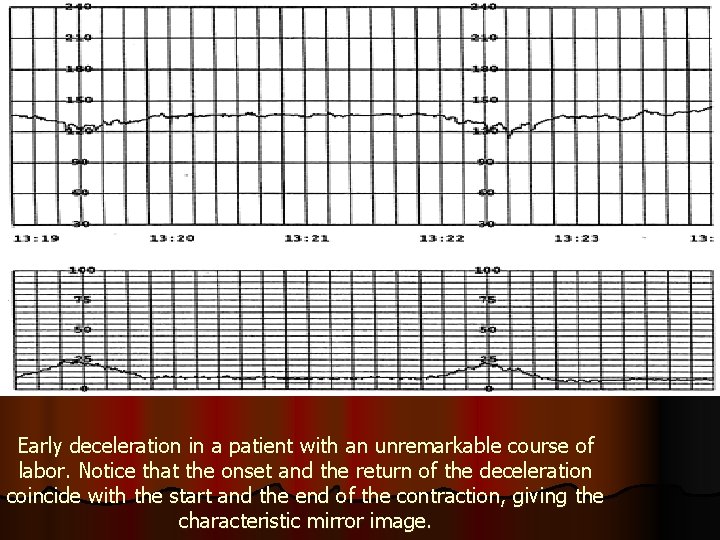
Early deceleration in a patient with an unremarkable course of labor. Notice that the onset and the return of the deceleration coincide with the start and the end of the contraction, giving the characteristic mirror image.
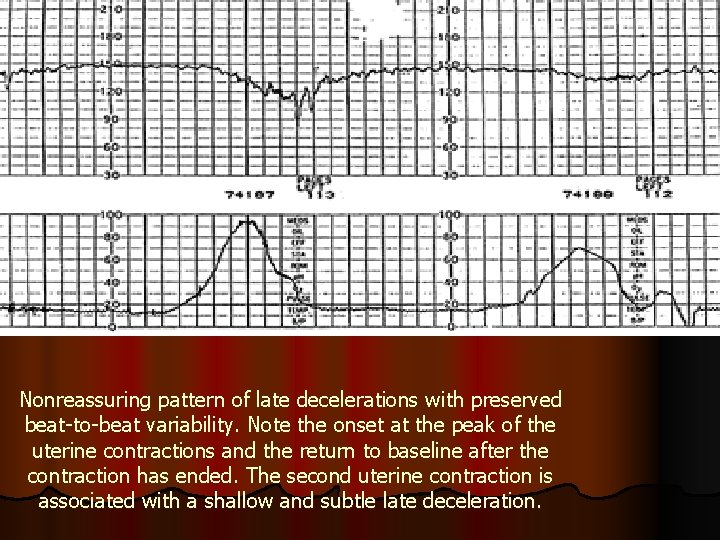
Nonreassuring pattern of late decelerations with preserved beat-to-beat variability. Note the onset at the peak of the uterine contractions and the return to baseline after the contraction has ended. The second uterine contraction is associated with a shallow and subtle late deceleration.
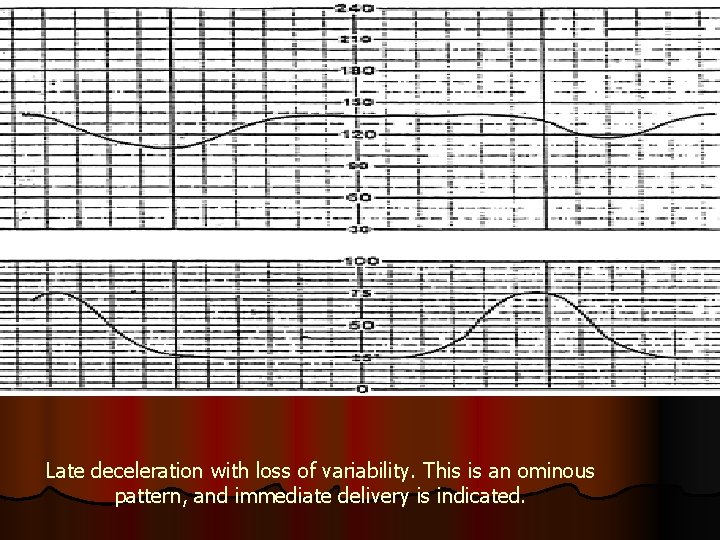
Late deceleration with loss of variability. This is an ominous pattern, and immediate delivery is indicated.
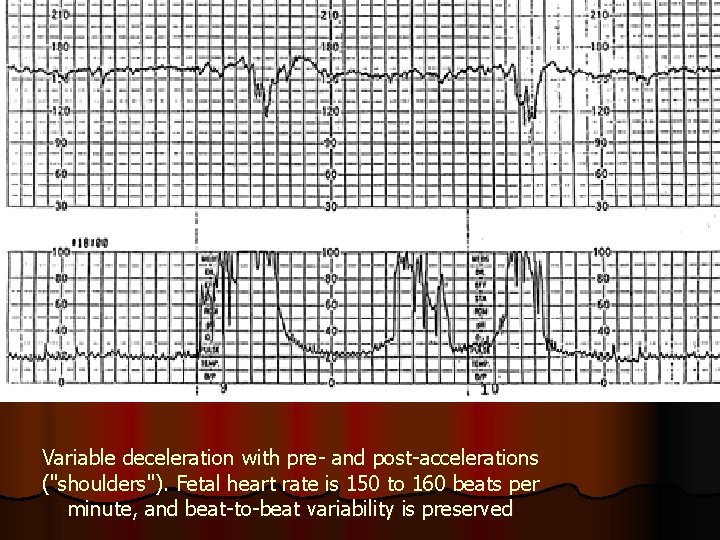
Variable deceleration with pre- and post-accelerations ("shoulders"). Fetal heart rate is 150 to 160 beats per minute, and beat-to-beat variability is preserved
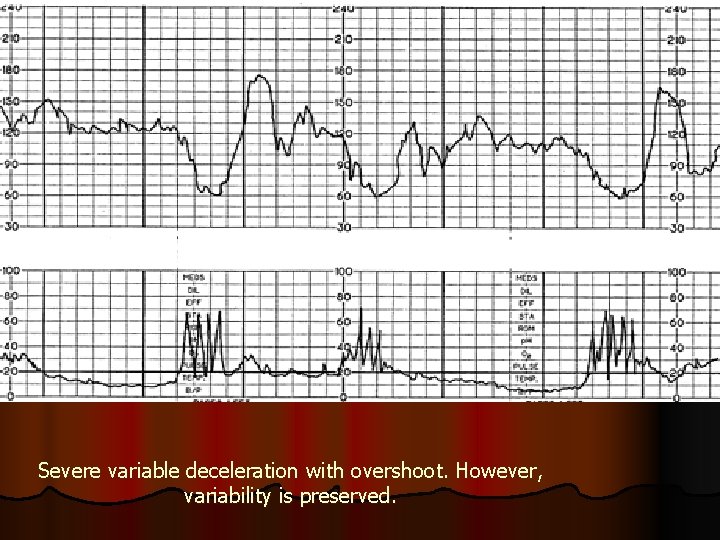
Severe variable deceleration with overshoot. However, variability is preserved.
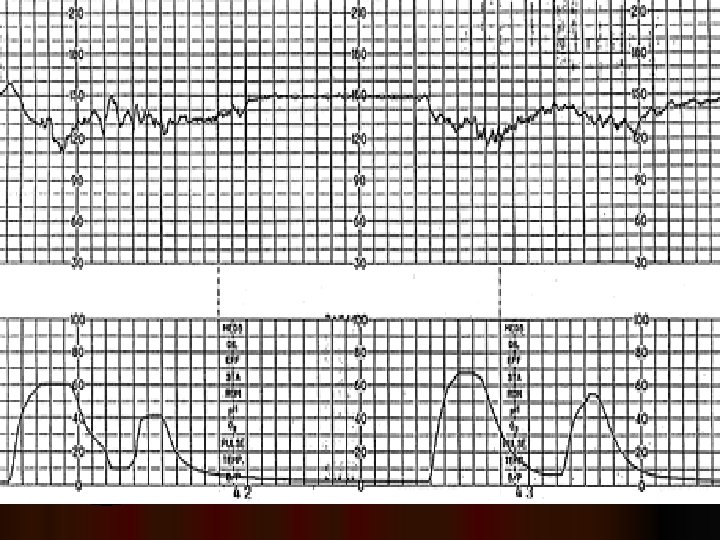
l Late deceleration related to bigeminal contractions. Beat-to-beat variability is preserved. Note the prolonged contraction pattern with elevated uterine tone between the peaks of the contractions, causing hyperstimulation and uteroplacental insufficiency. Management should include treatment of the uterine hyperstimulation. This deceleration pattern also may be interpreted as a variable deceleration with late return to the baseline based on the early onset of the deceleration in relation to the uterine contraction, the presence of an acceleration before the deceleration (the "shoulder") and the relatively sharp descent of the deceleration. However, late decelerations and variable decelerations with late return have the same clinical significance and represent nonreassuring patterns. This tracing probably represents cord compression and uteroplacental insufficiency.
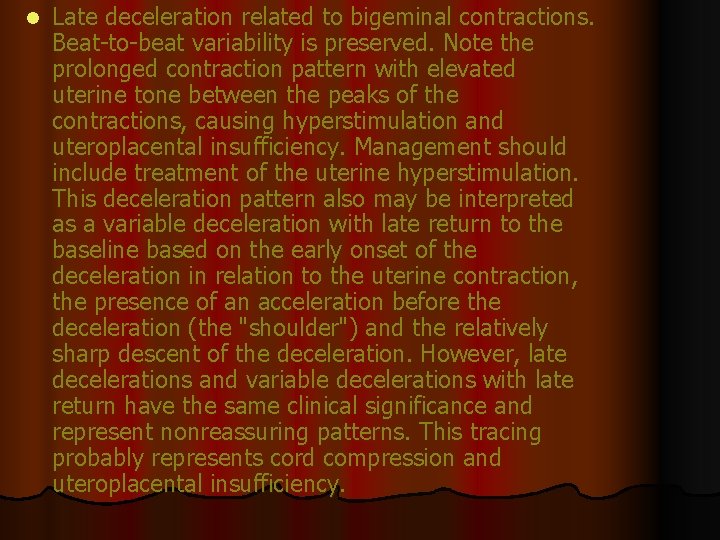
Pseudosinusoidal pattern. Note the decreased regularity and the preserved beat-to-beat variability
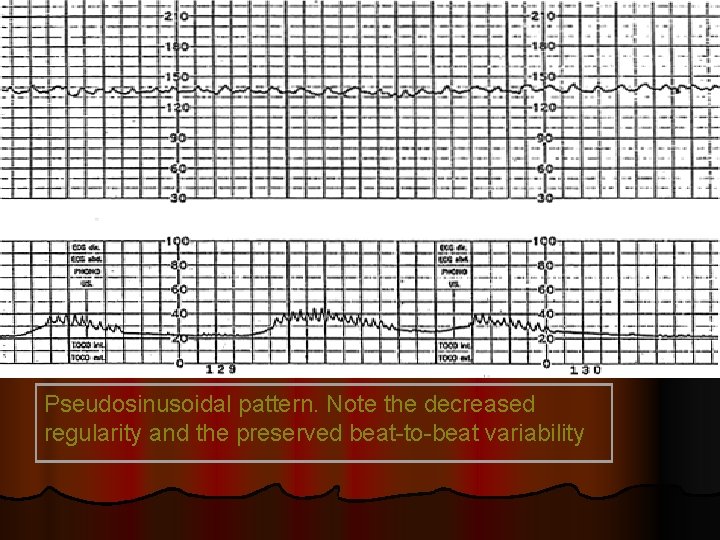
a true sinusoidal pattern
l List 6 Causes of Severe Fetal Bradycardia ? l Prolonged cord compression l Cord prolapse l Tetanic uterine contractions l Paracervical block l Epidural and spinal anesthesia l Maternal seizures l Rapid descent l Vigorous vaginal examination
l list 6 Causes of Severe Fetal Bradycardia ? l Prolonged cord compression l Cord prolapse l Tetanic uterine contractions l Paracervical block l Epidural and spinal anesthesia l Maternal seizures l Rapid descent l Vigorous vaginal examination
l l l l l What is the Signs of Nonreassuring Variable Decelerations that Indicate Hypoxemia ? Increased severity of the deceleration Late onset and gradual return phase Loss of "shoulders" on FHR recording A blunt acceleration or "overshoot" after severe deceleration Unexplained tachycardia Saltatory variability Late decelerations or late return to baseline Decreased variability
l what is the Nonreassuring patterns in the CTG? l Fetal tachycardia l Fetal bradycardia l Saltatory variability l Variable decelerations associated with a nonreassuring pattern l Late decelerations with preserved beat-to-beat variability
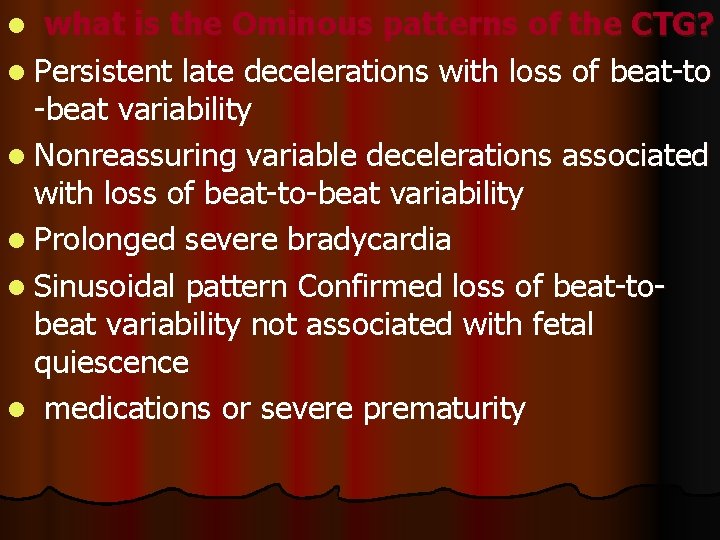
l what is the Ominous patterns of the CTG? l Persistent late decelerations with loss of beat-to -beat variability l Nonreassuring variable decelerations associated with loss of beat-to-beat variability l Prolonged severe bradycardia l Sinusoidal pattern Confirmed loss of beat-tobeat variability not associated with fetal quiescence l medications or severe prematurity
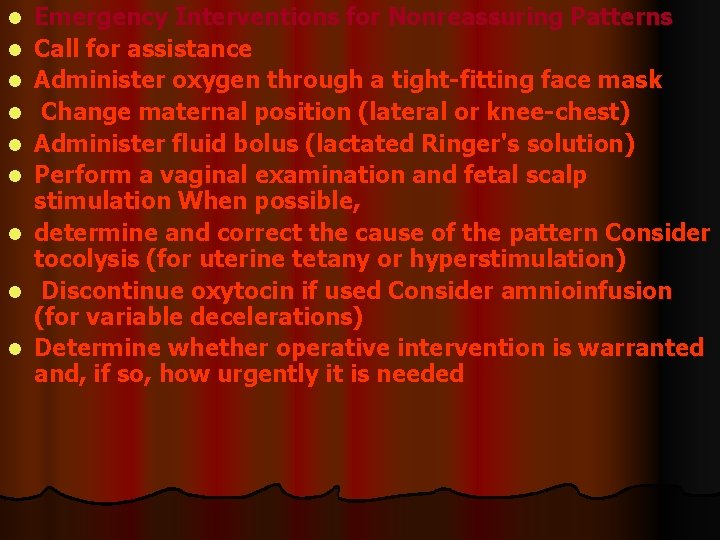
l l l l l Emergency Interventions for Nonreassuring Patterns Call for assistance Administer oxygen through a tight-fitting face mask Change maternal position (lateral or knee-chest) Administer fluid bolus (lactated Ringer's solution) Perform a vaginal examination and fetal scalp stimulation When possible, determine and correct the cause of the pattern Consider tocolysis (for uterine tetany or hyperstimulation) Discontinue oxytocin if used Consider amnioinfusion (for variable decelerations) Determine whether operative intervention is warranted and, if so, how urgently it is needed
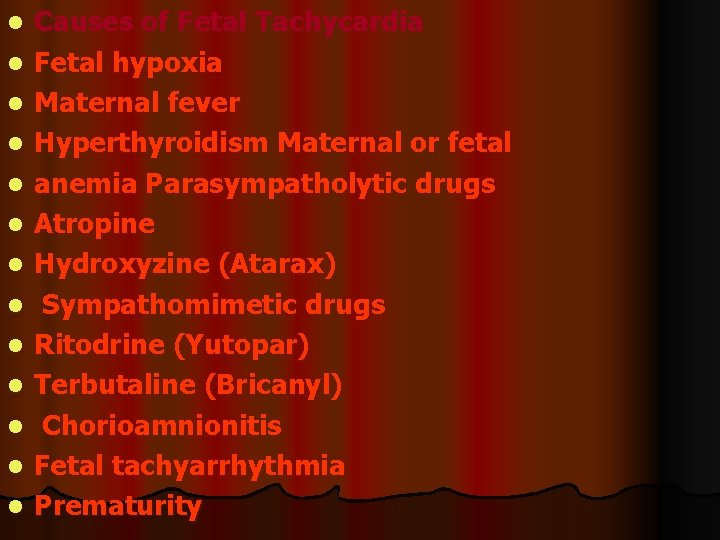
l l l l Causes of Fetal Tachycardia Fetal hypoxia Maternal fever Hyperthyroidism Maternal or fetal anemia Parasympatholytic drugs Atropine Hydroxyzine (Atarax) Sympathomimetic drugs Ritodrine (Yutopar) Terbutaline (Bricanyl) Chorioamnionitis Fetal tachyarrhythmia Prematurity
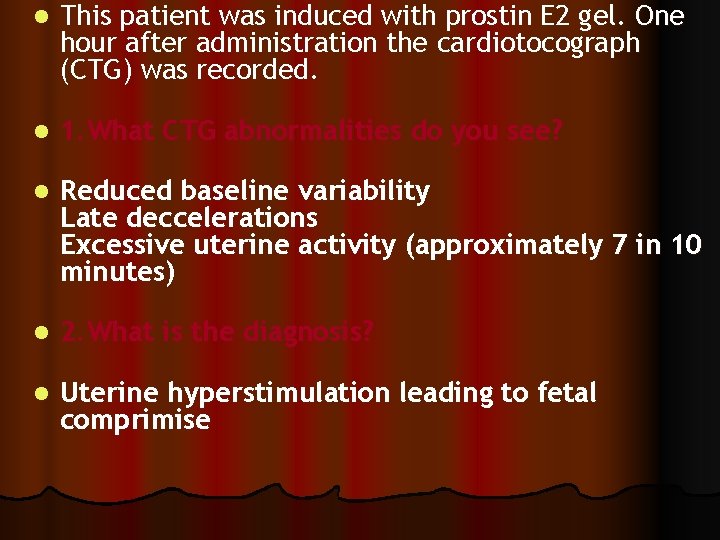
l This patient was induced with prostin E 2 gel. One hour after administration the cardiotocograph (CTG) was recorded. l 1. What CTG abnormalities do you see? l Reduced baseline variability Late deccelerations Excessive uterine activity (approximately 7 in 10 minutes) l 2. What is the diagnosis? l Uterine hyperstimulation leading to fetal comprimise
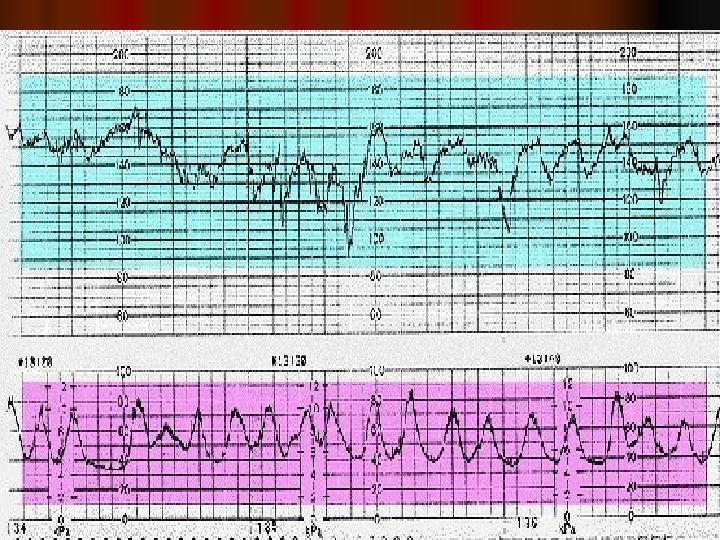
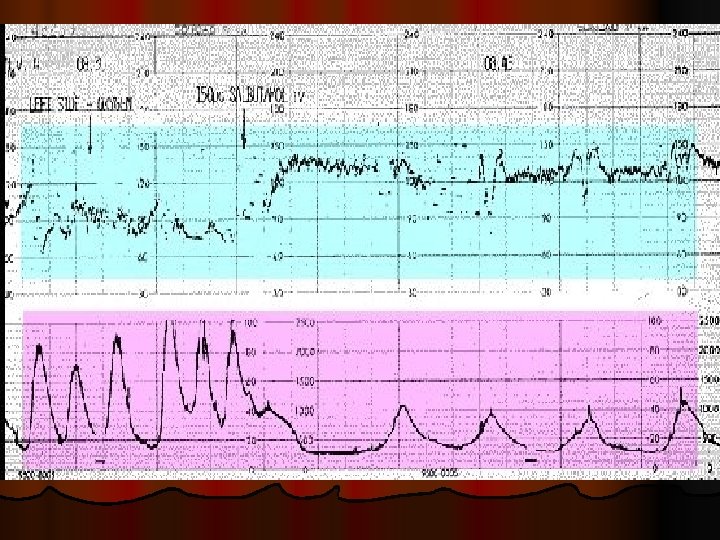
3. What is your management? Move the patient onto her left side to reduce the risk of aortocaval compression. Facial oxygen may improve fetal oxygenation. Use of an intravenous tocolytic agent will reduce the uterine activity. Suitable drugs include salbutamol or ritodrine, both of which are beta-2 agonists. The resulting CTG is shown below.
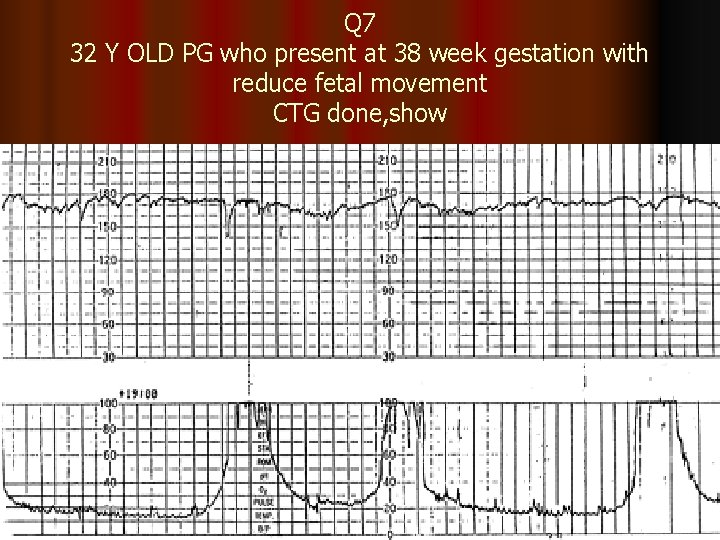
Q 7 32 Y OLD PG who present at 38 week gestation with reduce fetal movement CTG done, show
l 1. What abnormality are shown in the CTG? l 2. What will be the most likely plan of management? l 3. further CTG show persistent of this pattern what will you advice? l 4. if she went into labour , what must you do?
l l l l 1. What abnormality are shown in the CTG? 1. Fetal tachycardia with possible onset of decreased variability 2. What will be the most likely plan of management? Admit into the labour word with continuous monitoring 3. further CTG show persistent of this pattern what will you advice? Delivery by CS if cervix un favorable or. ARM if cervix favorable, and thin start syntocinon 4. if she went into labour , what must you do? Ensure that fetus monitored continuously and perform a fetal blood sample if this pattern persist
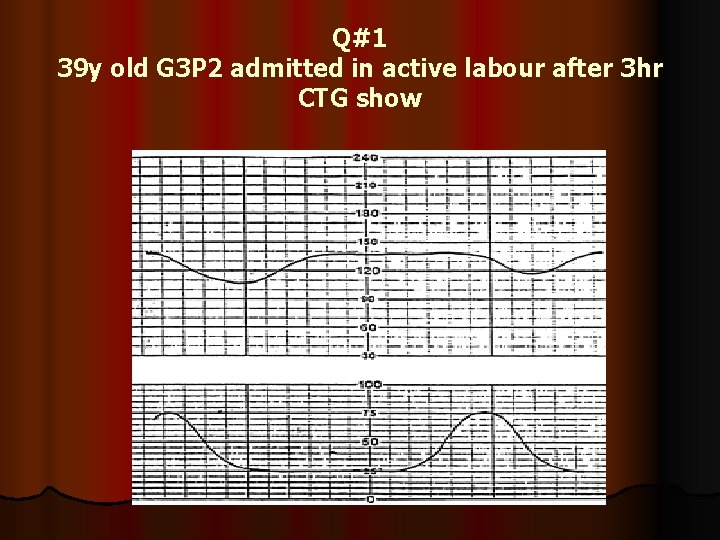
Q#1 39 y old G 3 P 2 admitted in active labour after 3 hr CTG show
l 1. Describe the CTG finding? l 2. what is the next action you will do? l 3. on examination cervix was fully dilated head at +2 station with caput ++ CTG persist the same. how you are going to manage this patient? 4. What other indication for its use? 5. What 6 condition must be fulfilled before the application of this instrument? 6. what 4 complication may arise from use of this instrument?
1. Describe the CTG finding? l Late deceleration with loss of variability. This is an ominous pattern, and immediate delivery is indicated l 2. what is the next action you will do? l Put the patient in lateral side , give oxygen , fast iv drip , and examine the patient to decide about the mode of the delivery l 3. on examination cervix was fully dilated head at +2 station with caput ++ CTG persist the same. how you are going to manage this patient? Immediate delivery is indicated , forceps delivery is appropriate for this pt l
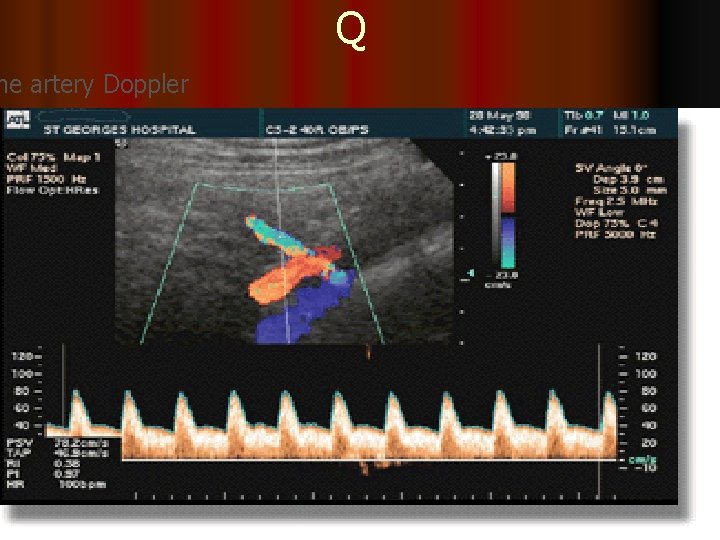
Q ne artery Doppler
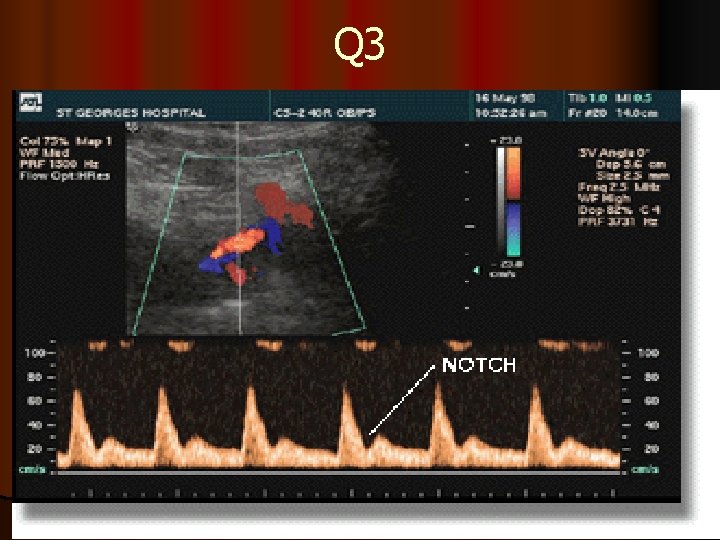
Q 3
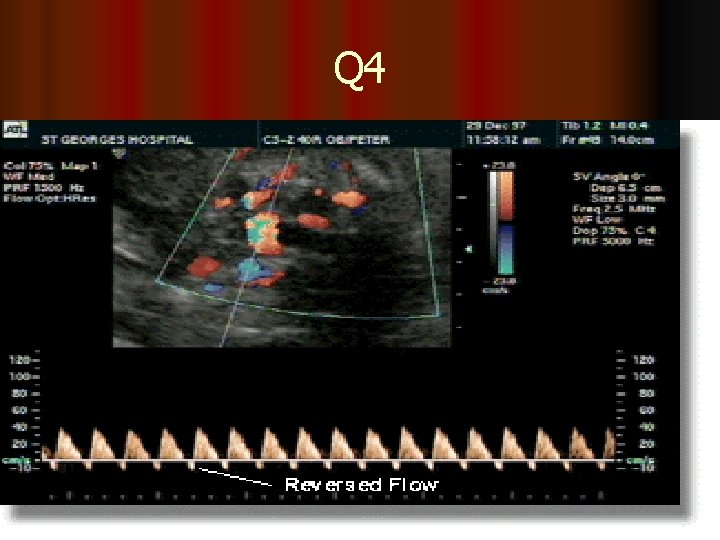
Q 4
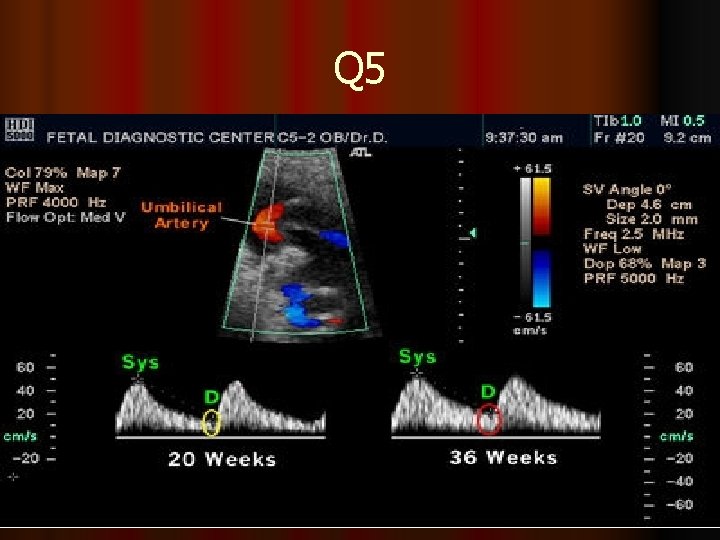
Q 5
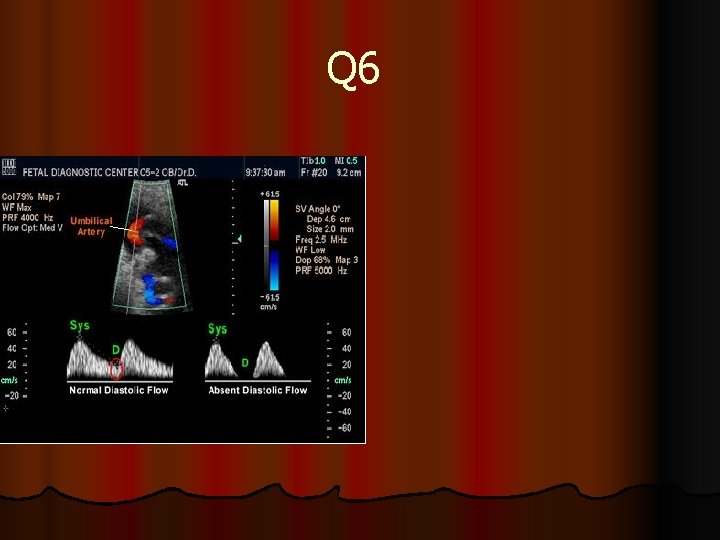
Q 6

Q 7
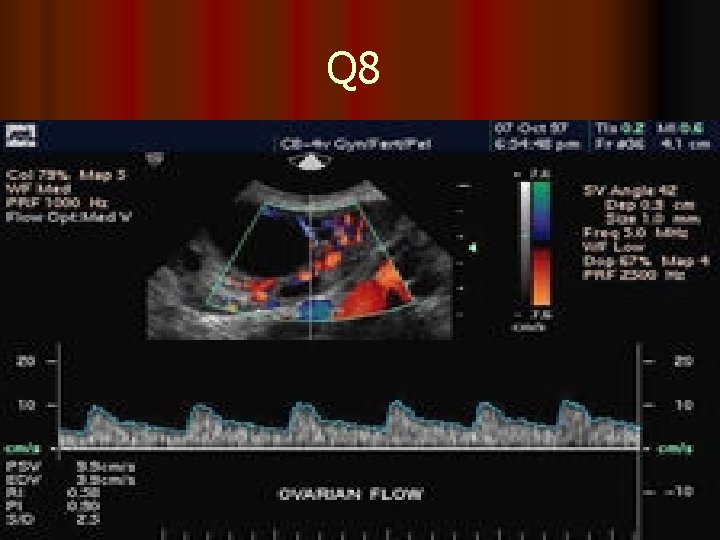
Q 8
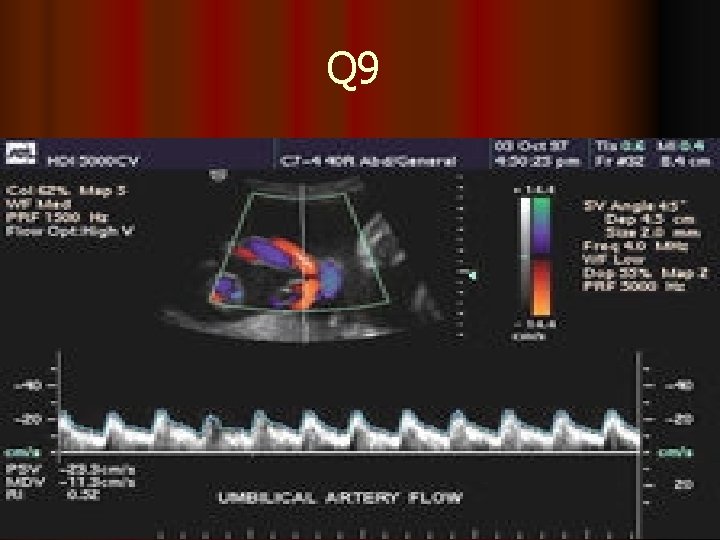
Q 9
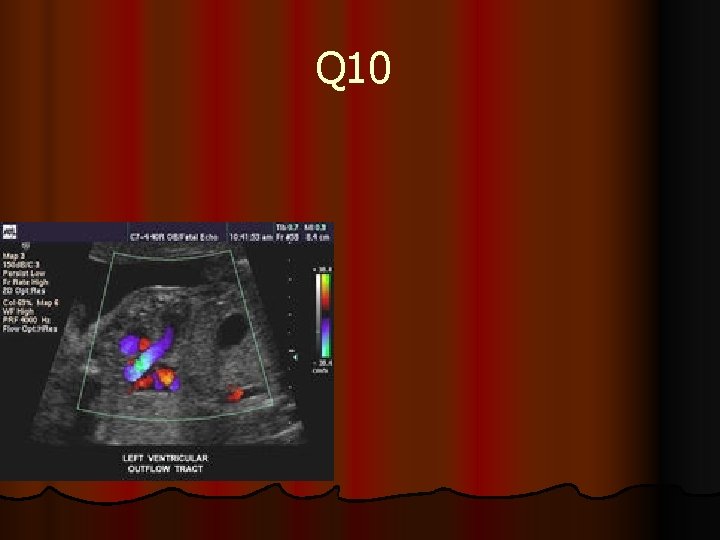
Q 10
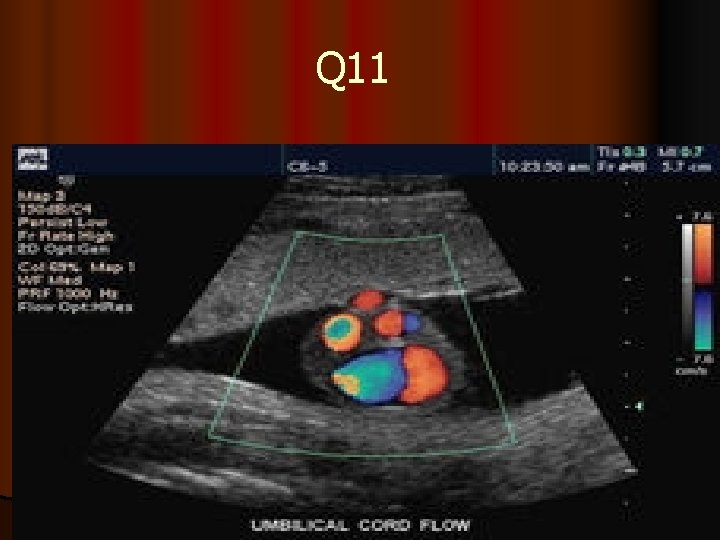
Q 11
2. Uterine artery Doppler is a promising technique for assessment of the level of risk of preeclampsia and IUGR. Doppler ultrasound provides a non-invasive method of assessing the utero-placental circulation. In normal pregnancy , impedance to flow in the uterine artery decreases with gestation and this presumably reflects the trophablastic invasion of the spiral ateries and their change into low resistance vessels. The uterine artery is a branch of the internal iliac artery close to the bifurcation of the common iliac. Colour flow Doppler is the method of choice for accurate screening of uterine artery waveforms.
The resistance index (RI) is the most commonly used index to measure the uterine artery flow as it is unlikely to have absent or reverse end Diastolic (EDF) flow. Although the pulsatility index (PI) can also be used 3. High resistance waveforms in the uterine artery with early diastolic notching in the second trimester are asssociated with the later development of preeclampsia, IUGR, placental abruption and intrauterine death. 4. notches of the uterine artery waveform with a high RI, hold the most risk of complicated pregnancies, although it is still to be established wether the notch or the high RI is the best indicator of poor outcome 5. Systole (Sys) and diastole (D) are identified in green Note that diastole is less at 20 weeks (yellow ellipse) than at 36 weeks (red ellipse). 6. This illustrates absent diastolic flow during diastole. When this occurs there is abnormal resistance in the placenta which results in a marked decrease in blood flow from the fetus to the placenta.
7. Color Doppler of umbilical cord insertion 8. Color Doppler and spectral Doppler of ovarian artery 9. Color Doppler and spectral Doppler of umbilical artery 10. Color Doppler of left ventricular outflow tract 11. Color Doppler of umbilical cord 12. Chromosome pattern of a person with Down's syndrome. Arrow points to an extra chromosome No. 21 l l l l l
l l l l l What is the Signs of Nonreassuring Variable Decelerations that Indicate Hypoxemia ? Increased severity of the deceleration Late onset and gradual return phase Loss of "shoulders" on FHR recording A blunt acceleration or "overshoot" after severe deceleration Unexplained tachycardia Saltatory variability Late decelerations or late return to baseline Decreased variability
l what is the Nonreassuring patterns in the CTG? l Fetal tachycardia l Fetal bradycardia l Saltatory variability l Variable decelerations associated with a nonreassuring pattern l Late decelerations with preserved beat-to-beat variability
l what is the Ominous patterns of the CTG? l Persistent late decelerations with loss of beat-to -beat variability l Nonreassuring variable decelerations associated with loss of beat-to-beat variability l Prolonged severe bradycardia l Sinusoidal pattern Confirmed loss of beat-tobeat variability not associated with fetal quiescence l medications or severe prematurity
l l l l l Emergency Interventions for Nonreassuring Patterns Call for assistance Administer oxygen through a tight-fitting face mask Change maternal position (lateral or knee-chest) Administer fluid bolus (lactated Ringer's solution) Perform a vaginal examination and fetal scalp stimulation When possible, determine and correct the cause of the pattern Consider tocolysis (for uterine tetany or hyperstimulation) Discontinue oxytocin if used Consider amnioinfusion (for variable decelerations) Determine whether operative intervention is warranted and, if so, how urgently it is needed
l l l l Causes of Fetal Tachycardia Fetal hypoxia Maternal fever Hyperthyroidism Maternal or fetal anemia Parasympatholytic drugs Atropine Hydroxyzine (Atarax) Sympathomimetic drugs Ritodrine (Yutopar) Terbutaline (Bricanyl) Chorioamnionitis Fetal tachyarrhythmia Prematurity
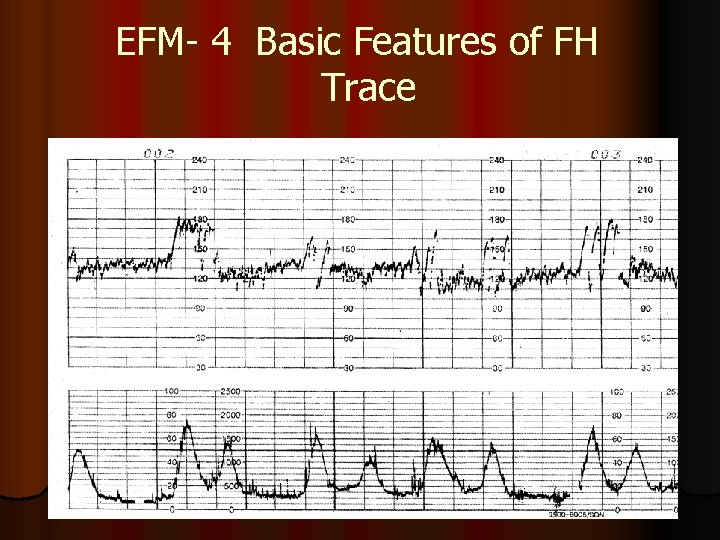
EFM- 4 Basic Features of FH Trace
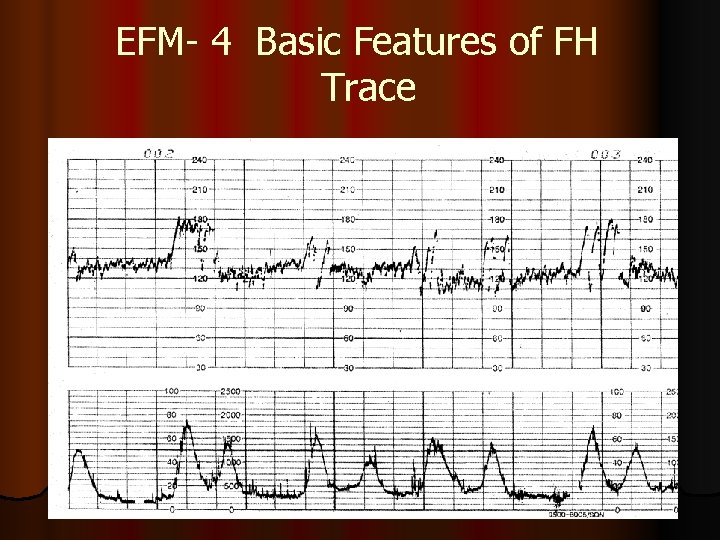
EFM- 4 Basic Features of FH Trace
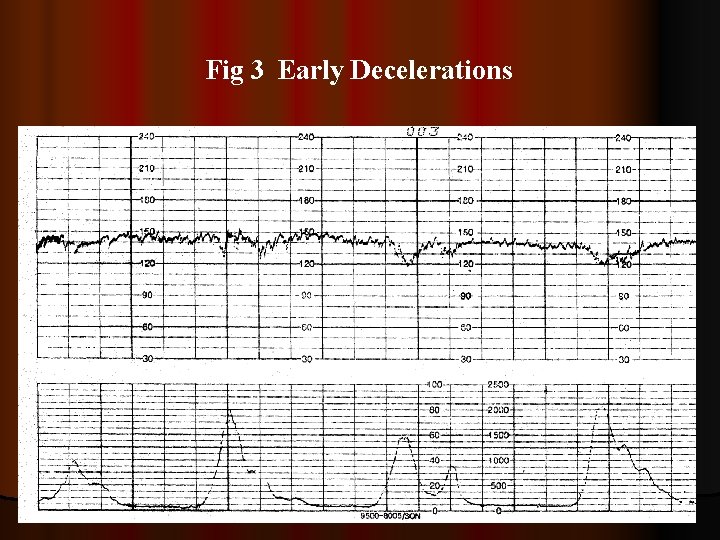
Fig 3 Early Decelerations
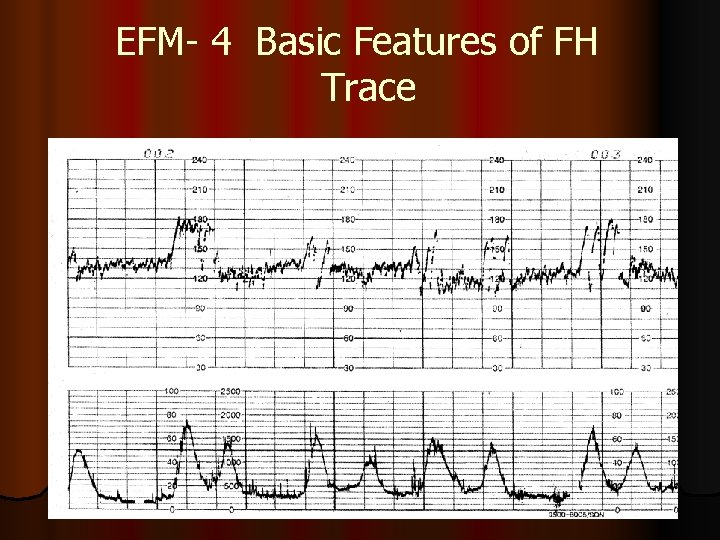
EFM- 4 Basic Features of FH Trace
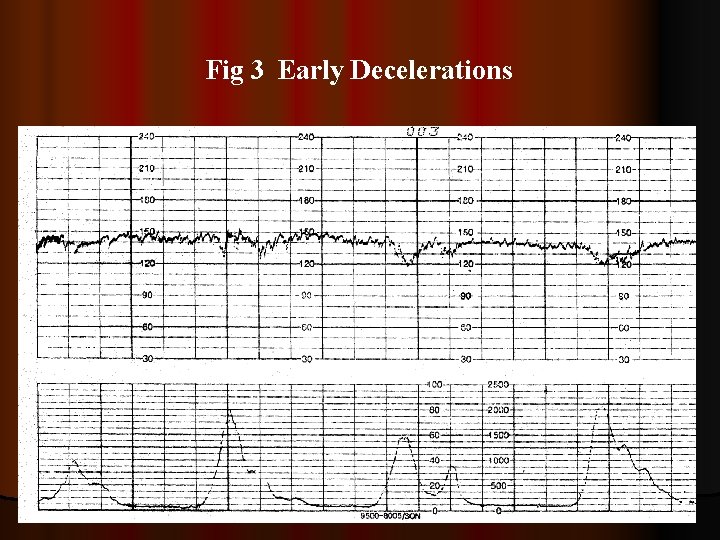
Fig 3 Early Decelerations
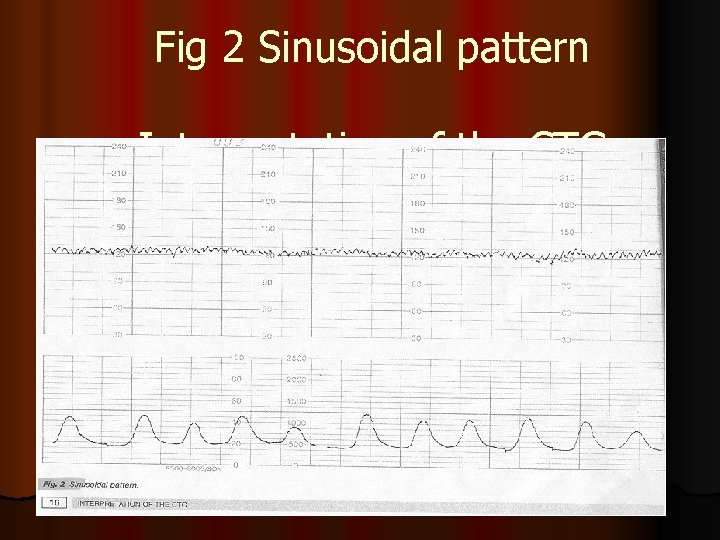
Fig 2 Sinusoidal pattern Interpretation of the CTG
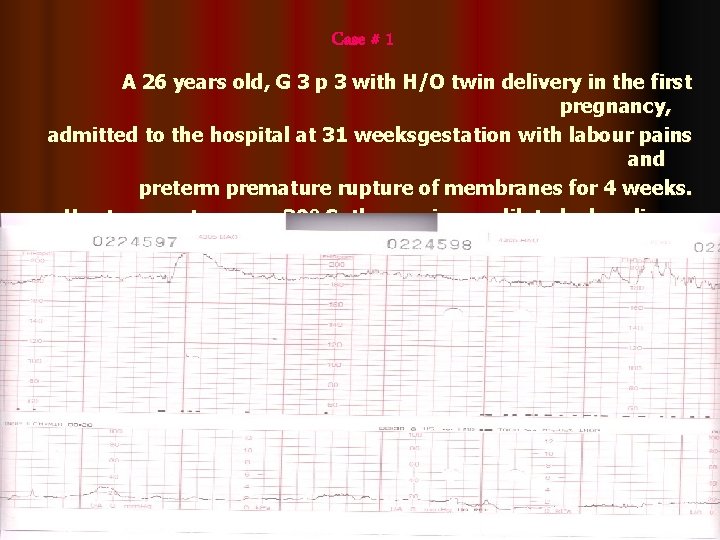
Case # 1 A 26 years old, G 3 p 3 with H/O twin delivery in the first pregnancy, admitted to the hospital at 31 weeksgestation with labour pains and preterm premature rupture of membranes for 4 weeks. Her temperature was 39º C, the cervix cm dilated, clear liquor draining. The WBCs were 25 x 109
Sinus Tachycardia Actions High vaginal swab for bacterial culture and sensitivity test (yes) Parentral antibiotics(yes) Antipyretics and review after 2 hours (no) Adjust tocodynamometer and review (yes) Cesarean section immediately (no) Fetal blood sampling for PH(no) Course and Outcome Labour was augmented with syntocinon, and intravenous triple antibiotics were given. After 5 hours, the patient had normal vaginal delivery of a baby boy weighing 1. 9 kg. Apgar score was 5 at one minute and 8 at five minutes. Cord blood PH was 7. 061, PO 2 11. 3, PCO 2 61 , base excess – 13. 9, and O 2 saturation
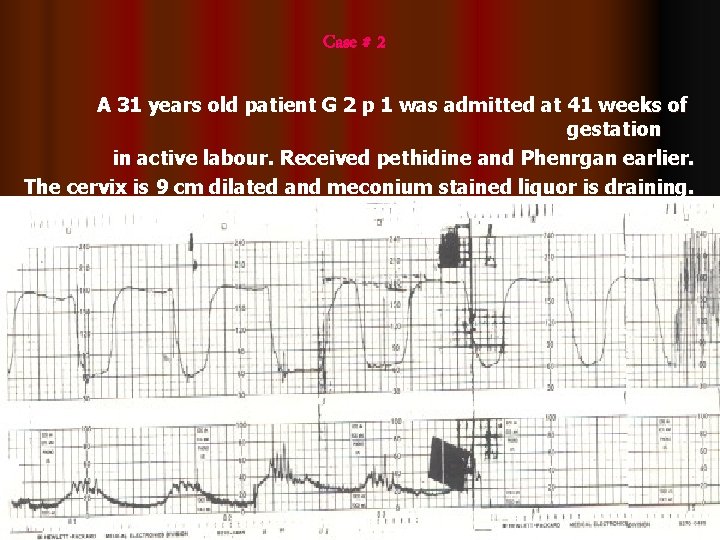
Case # 2 A 31 years old patient G 2 p 1 was admitted at 41 weeks of gestation in active labour. Received pethidine and Phenrgan earlier. The cervix is 9 cm dilated and meconium stained liquor is draining.
Sinus Tachycardia With Deceleration And No Variability: Mixed Pattern Actions Wait and review after 30 minutes(no) Change the position of the patient (yes) Fetal scalp blood sampling(no) Immediate cesarean section (yes) Give naloxone (no) Explain and reassure the patient (yes) Course and Outcome Cesarean section was carried out. A baby girl weighing 3898 gm was delivered from vertex presentation. Apgar score was 1/5 at one and five minutes. The position of the cord was not
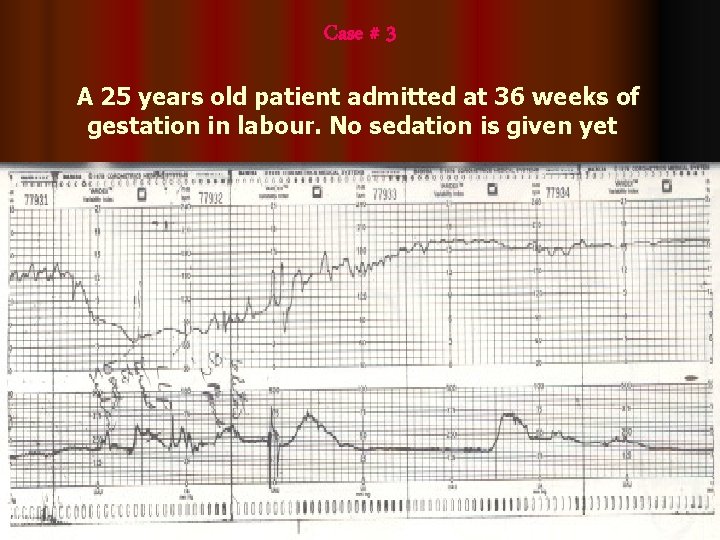
Case # 3 A 25 years old patient admitted at 36 weeks of gestation in labour. No sedation is given yet
Rebound Tachycardia Actions Facial oxygen(no) Give sedation (no) Fetal scalp blood sampling for PH (yes) Augmentation of labour with syntocinon (no) Cesarean section (no) Maternal hydration (no) Course and Outcome After recovery from prolonged deceleration, scalp PH were 7. 28, 7. 36 and 7. 36. the patient had normal vaginal delivery of baby girl weighing 2070 gm(small for age).
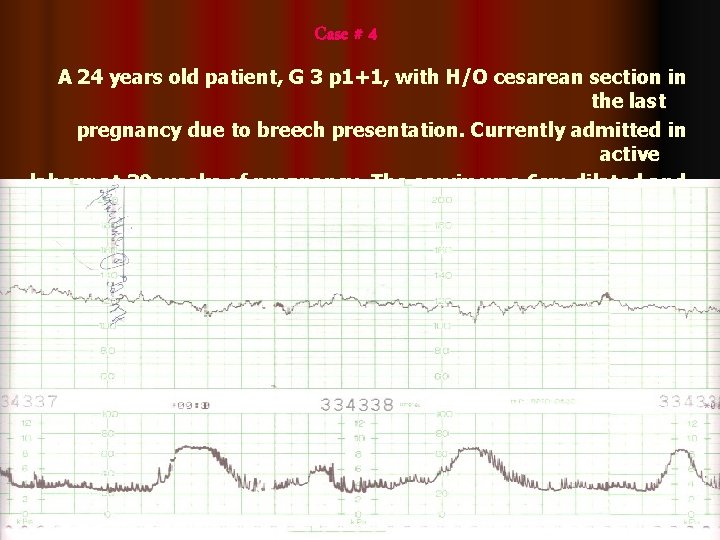
Case # 4 A 24 years old patient, G 3 p 1+1, with H/O cesarean section in the last pregnancy due to breech presentation. Currently admitted in active labour at 39 weeks of pregnancy. The cervix was 6 cm dilated and the head was at 0 station 2 hours prior to this trace
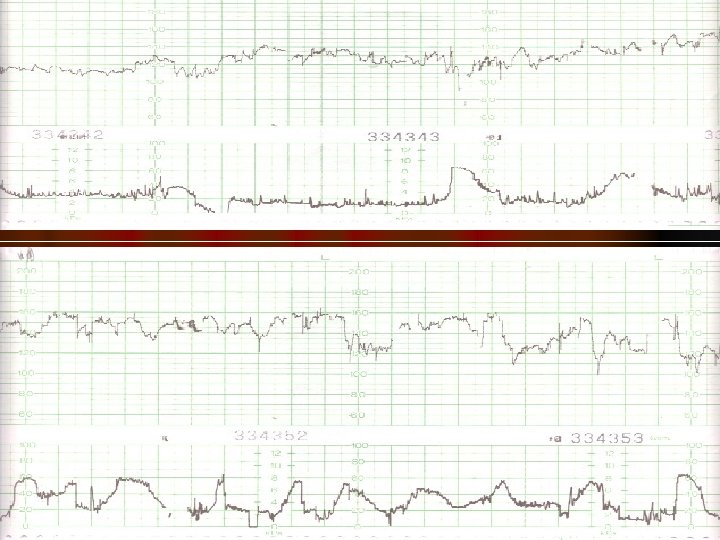
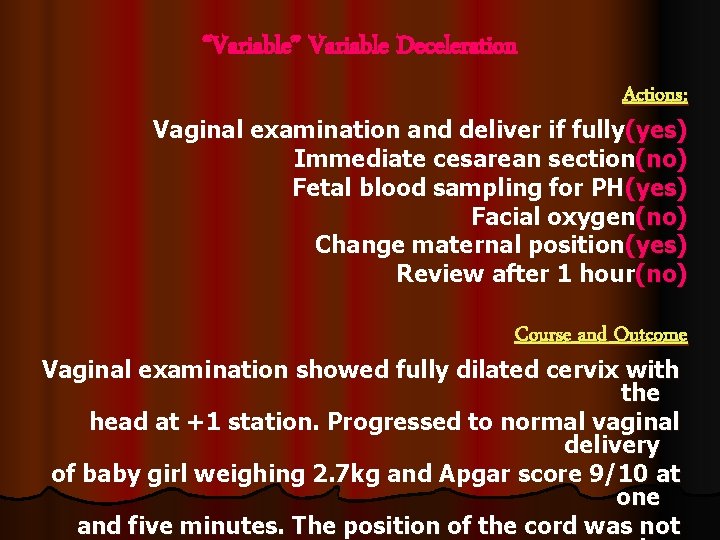
“Variable” Variable Deceleration Actions: Vaginal examination and deliver if fully(yes) Immediate cesarean section(no) Fetal blood sampling for PH(yes) Facial oxygen(no) Change maternal position(yes) Review after 1 hour(no) Course and Outcome Vaginal examination showed fully dilated cervix with the head at +1 station. Progressed to normal vaginal delivery of baby girl weighing 2. 7 kg and Apgar score 9/10 at one and five minutes. The position of the cord was not
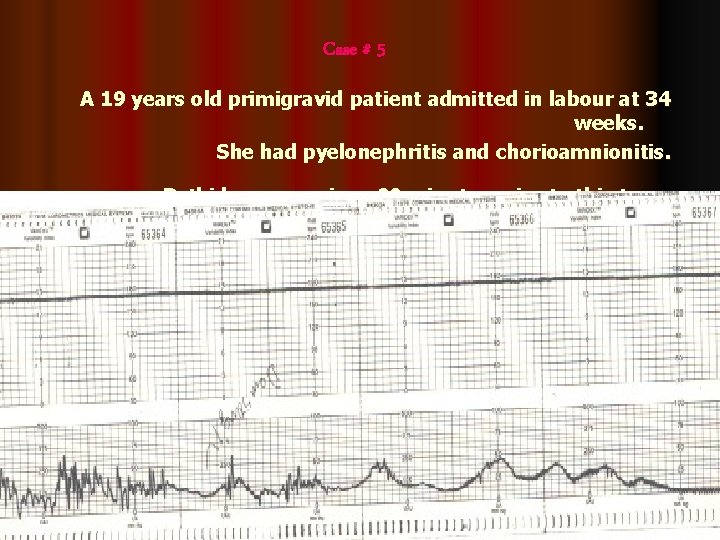
Case # 5 A 19 years old primigravid patient admitted in labour at 34 weeks. She had pyelonephritis and chorioamnionitis. Pethidene was given 90 minutes prior to this trace.
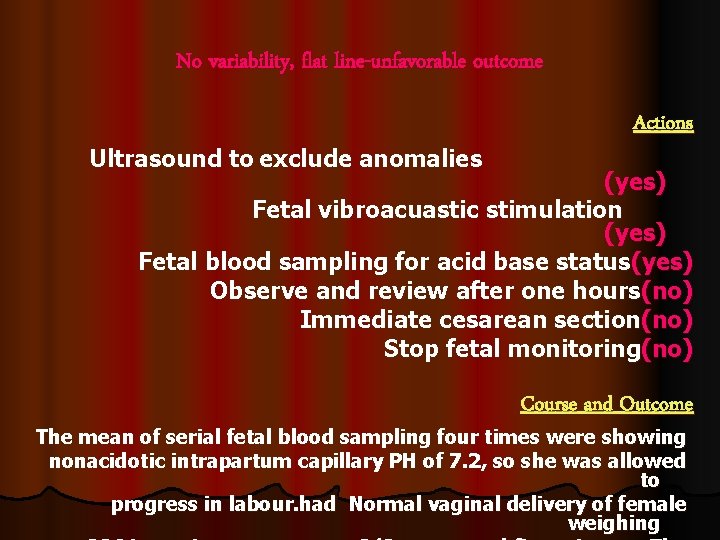
No variability, flat line-unfavorable outcome Actions Ultrasound to exclude anomalies (yes) Fetal vibroacuastic stimulation (yes) Fetal blood sampling for acid base status(yes) Observe and review after one hours(no) Immediate cesarean section(no) Stop fetal monitoring(no) Course and Outcome The mean of serial fetal blood sampling four times were showing nonacidotic intrapartum capillary PH of 7. 2, so she was allowed to progress in labour. had Normal vaginal delivery of female weighing
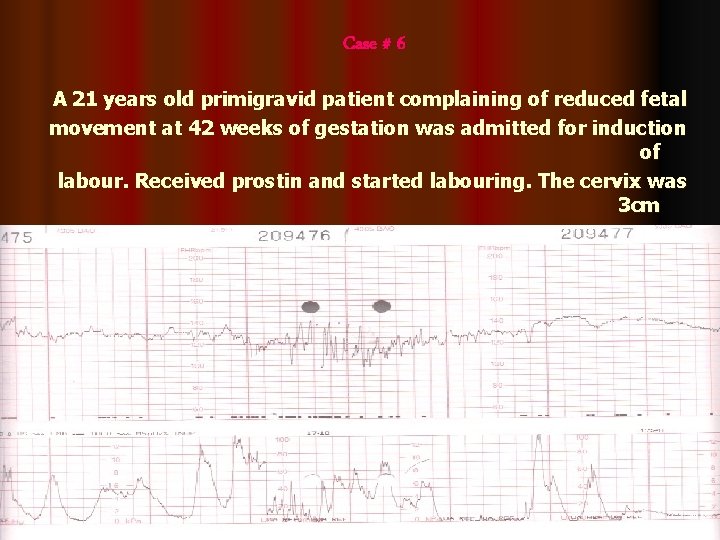
Case # 6 A 21 years old primigravid patient complaining of reduced fetal movement at 42 weeks of gestation was admitted for induction of labour. Received prostin and started labouring. The cervix was 3 cm dilated, so amniotomy was done and liquor was clear. Syntocinon infusion was started 30 minutes ago
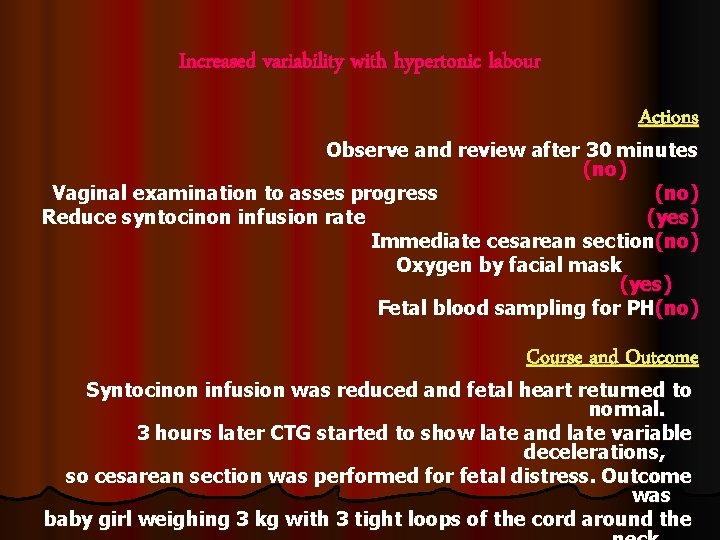
Increased variability with hypertonic labour Actions Observe and review after 30 minutes (no) Vaginal examination to asses progress (no) Reduce syntocinon infusion rate (yes) Immediate cesarean section(no) Oxygen by facial mask (yes) Fetal blood sampling for PH(no) Course and Outcome Syntocinon infusion was reduced and fetal heart returned to normal. 3 hours later CTG started to show late and late variable decelerations, so cesarean section was performed for fetal distress. Outcome was baby girl weighing 3 kg with 3 tight loops of the cord around the
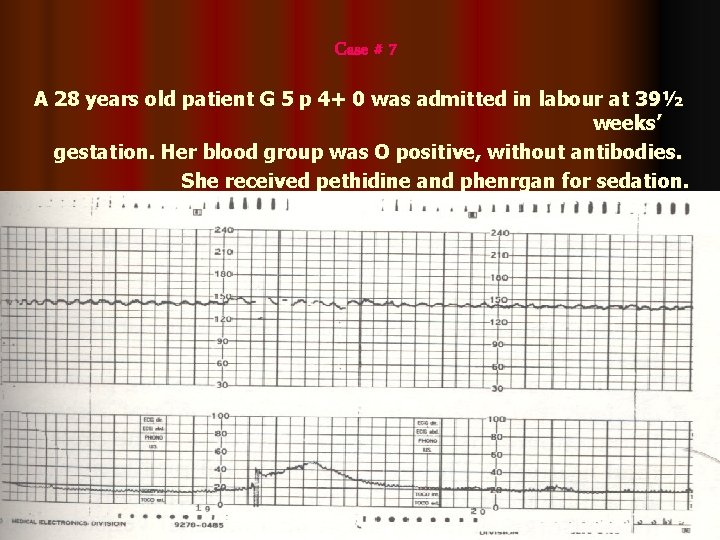
Case # 7 A 28 years old patient G 5 p 4+ 0 was admitted in labour at 39½ weeks’ gestation. Her blood group was O positive, without antibodies. She received pethidine and phenrgan for sedation.
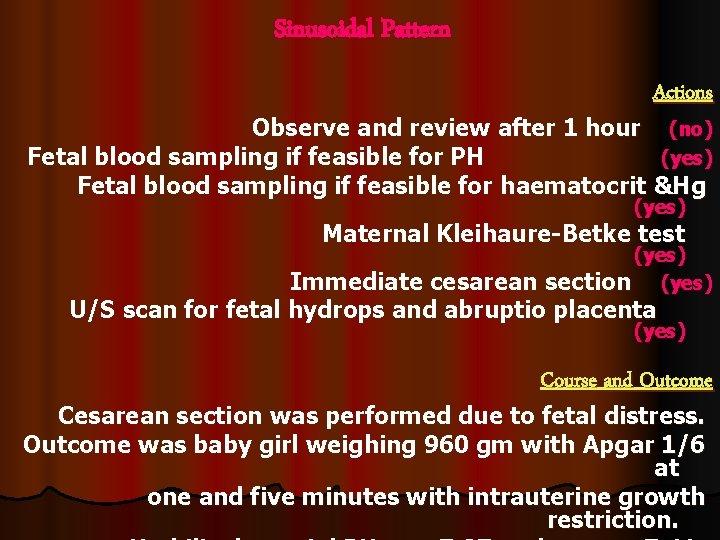
Sinusoidal Pattern Actions Observe and review after 1 hour (no) Fetal blood sampling if feasible for PH (yes) Fetal blood sampling if feasible for haematocrit &Hg (yes) Maternal Kleihaure-Betke test (yes) Immediate cesarean section (yes) U/S scan for fetal hydrops and abruptio placenta (yes) Course and Outcome Cesarean section was performed due to fetal distress. Outcome was baby girl weighing 960 gm with Apgar 1/6 at one and five minutes with intrauterine growth restriction.
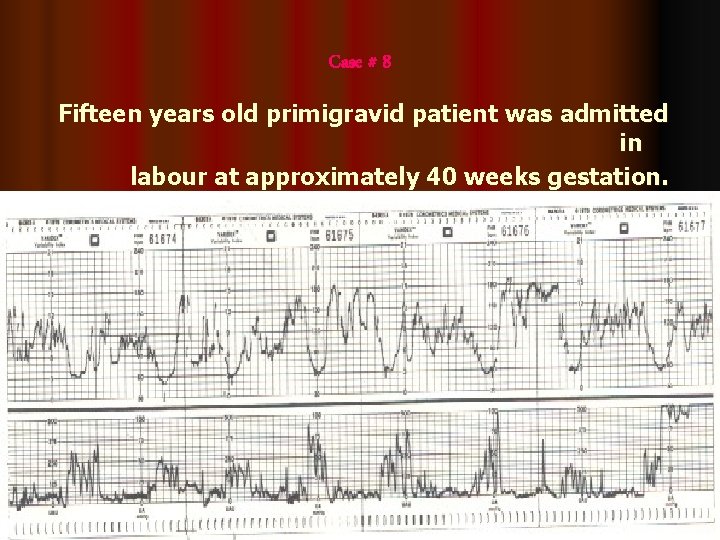
Case # 8 Fifteen years old primigravid patient was admitted in labour at approximately 40 weeks gestation. She received epidural anesthesia
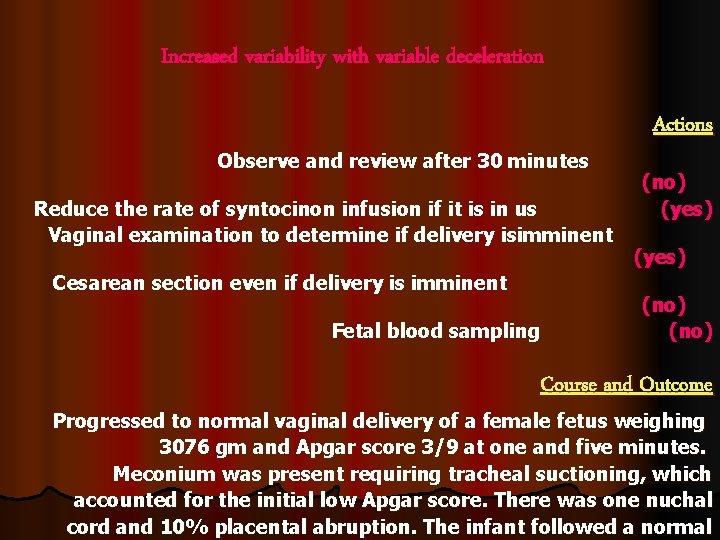
Increased variability with variable deceleration Actions Observe and review after 30 minutes (no) Reduce the rate of syntocinon infusion if it is in us (yes) Vaginal examination to determine if delivery isimminent (yes) Cesarean section even if delivery is imminent (no) Fetal blood sampling (no) Course and Outcome Progressed to normal vaginal delivery of a female fetus weighing 3076 gm and Apgar score 3/9 at one and five minutes. Meconium was present requiring tracheal suctioning, which accounted for the initial low Apgar score. There was one nuchal cord and 10% placental abruption. The infant followed a normal
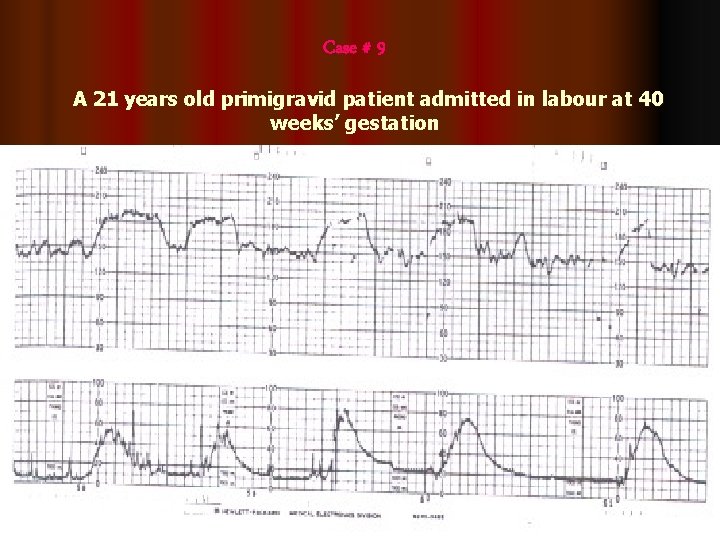
Case # 9 A 21 years old primigravid patient admitted in labour at 40 weeks’ gestation
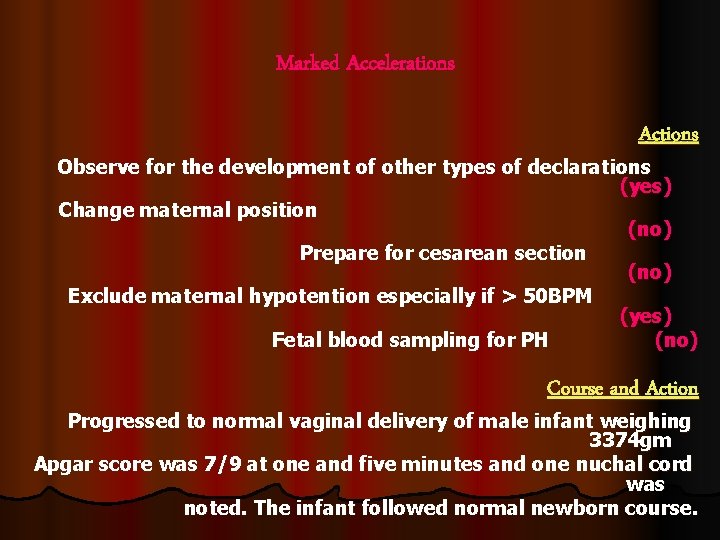
Marked Accelerations Actions Observe for the development of other types of declarations (yes) Change maternal position (no) Prepare for cesarean section (no) Exclude maternal hypotention especially if > 50 BPM (yes) Fetal blood sampling for PH (no) Course and Action Progressed to normal vaginal delivery of male infant weighing 3374 gm Apgar score was 7/9 at one and five minutes and one nuchal cord was noted. The infant followed normal newborn course.
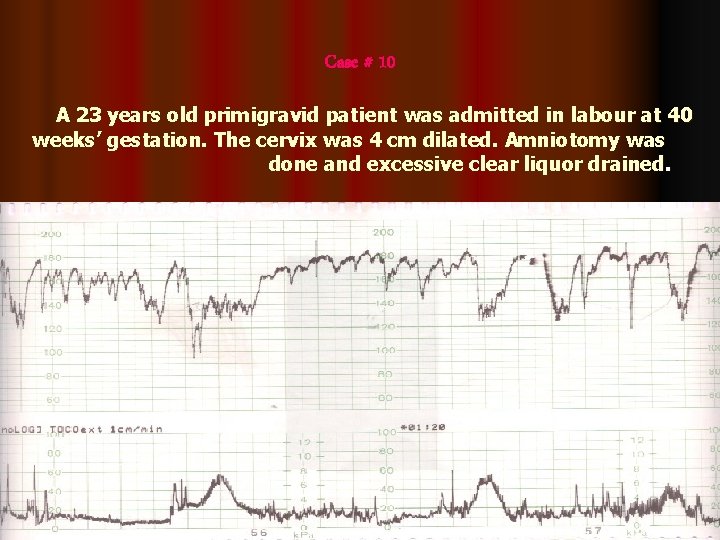
Case # 10 A 23 years old primigravid patient was admitted in labour at 40 weeks’ gestation. The cervix was 4 cm dilated. Amniotomy was done and excessive clear liquor drained.
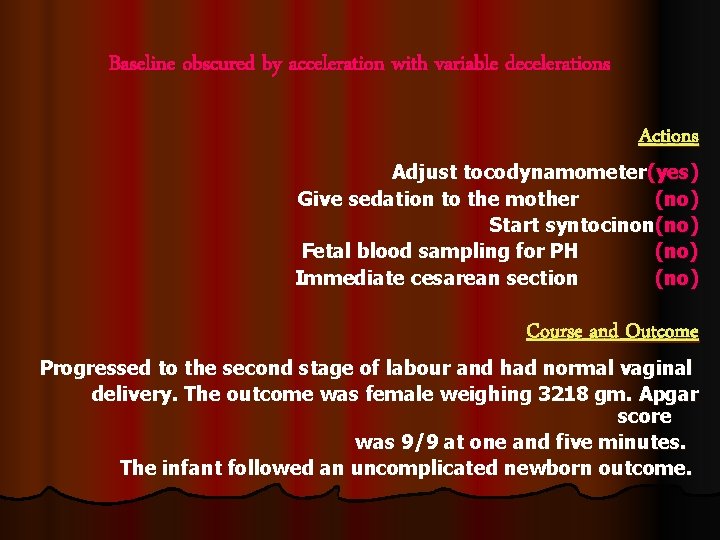
Baseline obscured by acceleration with variable decelerations Actions Adjust tocodynamometer(yes) Give sedation to the mother (no) Start syntocinon(no) Fetal blood sampling for PH (no) Immediate cesarean section (no) Course and Outcome Progressed to the second stage of labour and had normal vaginal delivery. The outcome was female weighing 3218 gm. Apgar score was 9/9 at one and five minutes. The infant followed an uncomplicated newborn outcome.
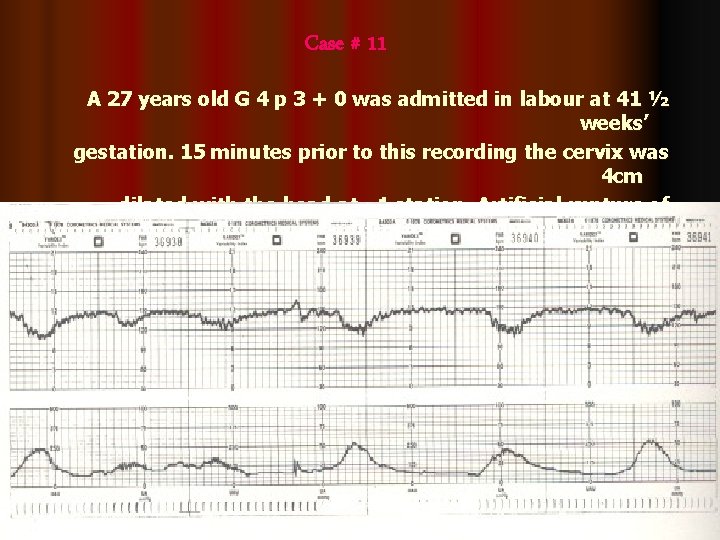
Case # 11 A 27 years old G 4 p 3 + 0 was admitted in labour at 41 ½ weeks’ gestation. 15 minutes prior to this recording the cervix was 4 cm dilated with the head at – 1 station. Artificial rupture of membranes was performed and clear liquor drained.
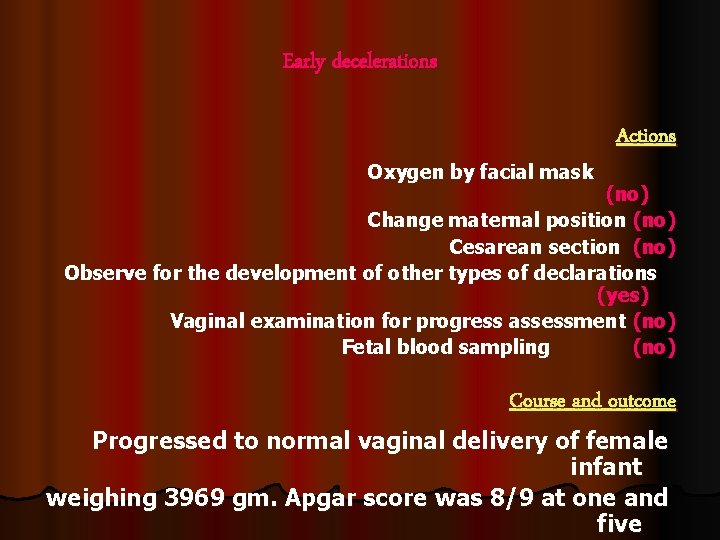
Early decelerations Actions Oxygen by facial mask (no) Change maternal position (no) Cesarean section (no) Observe for the development of other types of declarations (yes) Vaginal examination for progress assessment (no) Fetal blood sampling (no) Course and outcome Progressed to normal vaginal delivery of female infant weighing 3969 gm. Apgar score was 8/9 at one and five
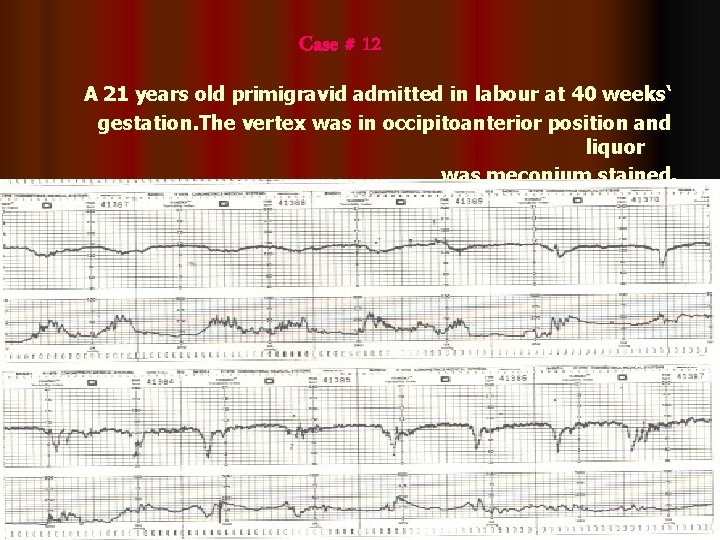
Case # 12 A 21 years old primigravid admitted in labour at 40 weeks‘ gestation. The vertex was in occipitoanterior position and liquor was meconium stained.
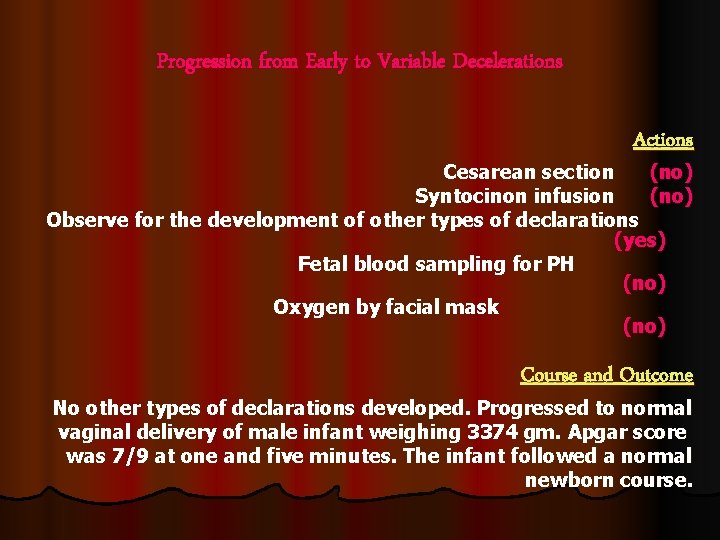
Progression from Early to Variable Decelerations Actions Cesarean section (no) Syntocinon infusion (no) Observe for the development of other types of declarations (yes) Fetal blood sampling for PH (no) Oxygen by facial mask (no) Course and Outcome No other types of declarations developed. Progressed to normal vaginal delivery of male infant weighing 3374 gm. Apgar score was 7/9 at one and five minutes. The infant followed a normal newborn course.
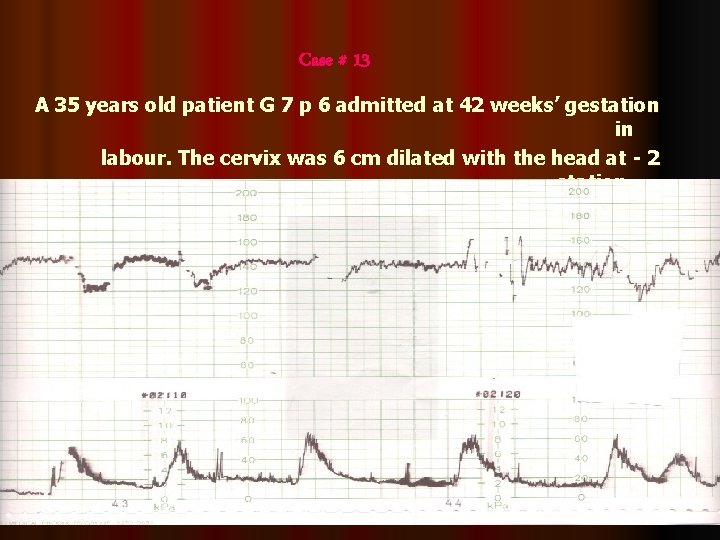
Case # 13 A 35 years old patient G 7 p 6 admitted at 42 weeks’ gestation in labour. The cervix was 6 cm dilated with the head at - 2 station, liquor was stained with meconium.
Late decelerations Actions Observe and review after 1 hour (no) Cesarean section unless the fetus is about to be delivered (yes) Correct maternal hypotention if present (yes) Fetal scalp blood for PH (no) Maternal Kleihaure-Betke test (yes) Course and Outcome Cesarean section was done. The outcome was male baby weighing 3100 gm. Apgar score was 2/8 at one and five minutes. The infant had meconium aspiration.
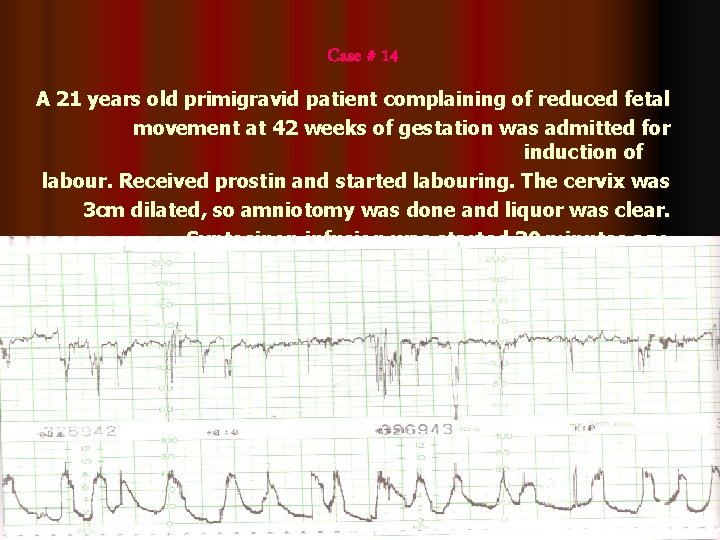
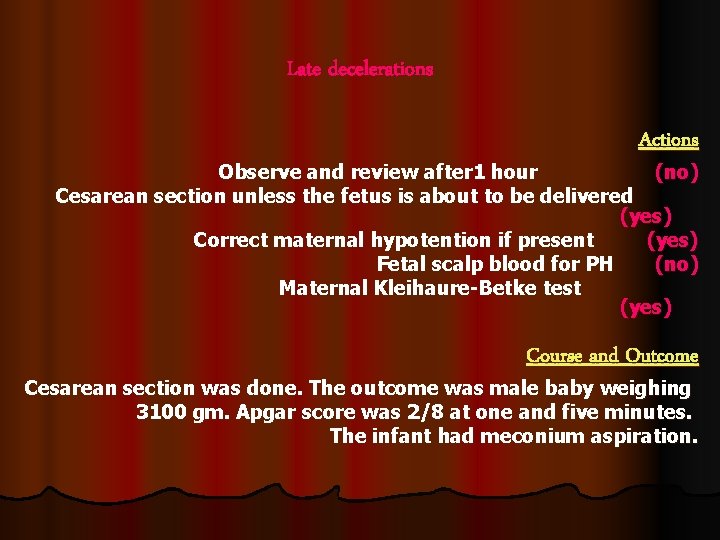
Case # 14 A 21 years old primigravid patient complaining of reduced fetal movement at 42 weeks of gestation was admitted for induction of labour. Received prostin and started labouring. The cervix was 3 cm dilated, so amniotomy was done and liquor was clear. Syntocinon infusion was started 30 minutes ago.
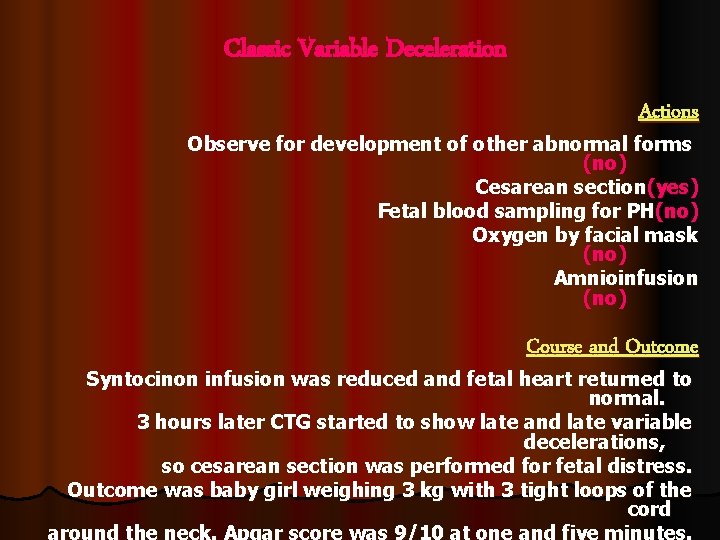
Classic Variable Deceleration Actions Observe for development of other abnormal forms (no) Cesarean section(yes) Fetal blood sampling for PH(no) Oxygen by facial mask (no) Amnioinfusion (no) Course and Outcome Syntocinon infusion was reduced and fetal heart returned to normal. 3 hours later CTG started to show late and late variable decelerations, so cesarean section was performed for fetal distress. Outcome was baby girl weighing 3 kg with 3 tight loops of the cord around the neck. Apgar score was 9/10 at one and five minutes.
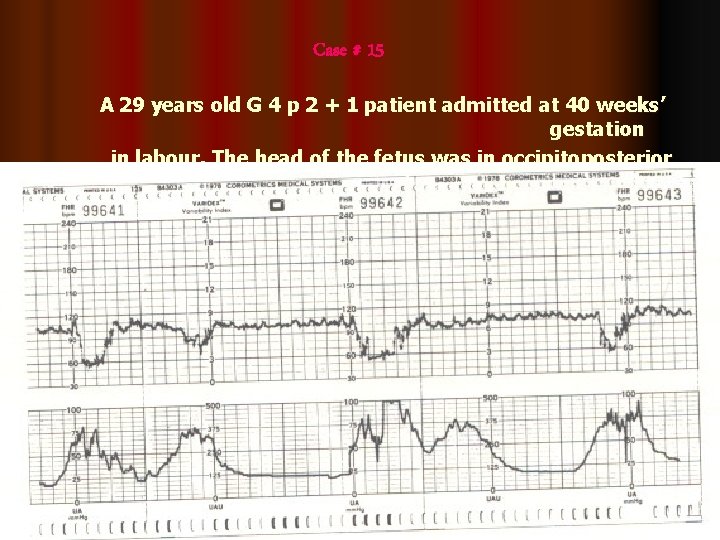
Case # 15 A 29 years old G 4 p 2 + 1 patient admitted at 40 weeks’ gestation in labour. The head of the fetus was in occipitoposterior position.
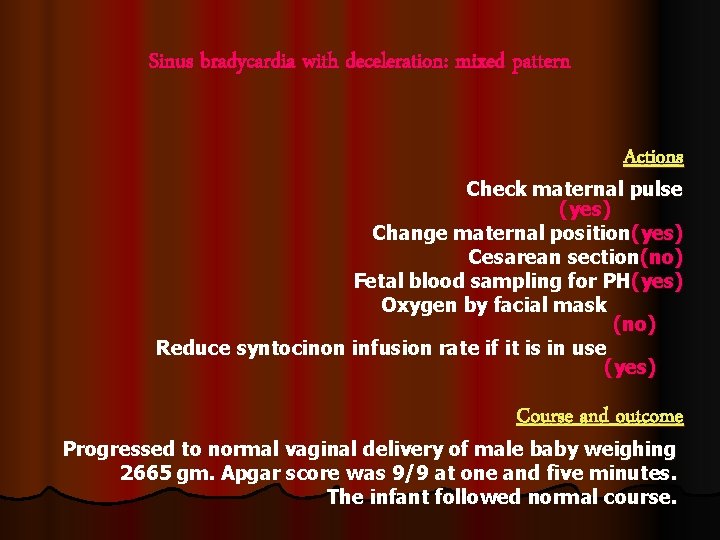
Sinus bradycardia with deceleration: mixed pattern Actions Check maternal pulse (yes) Change maternal position(yes) Cesarean section(no) Fetal blood sampling for PH(yes) Oxygen by facial mask (no) Reduce syntocinon infusion rate if it is in use (yes) Course and outcome Progressed to normal vaginal delivery of male baby weighing 2665 gm. Apgar score was 9/9 at one and five minutes. The infant followed normal course.
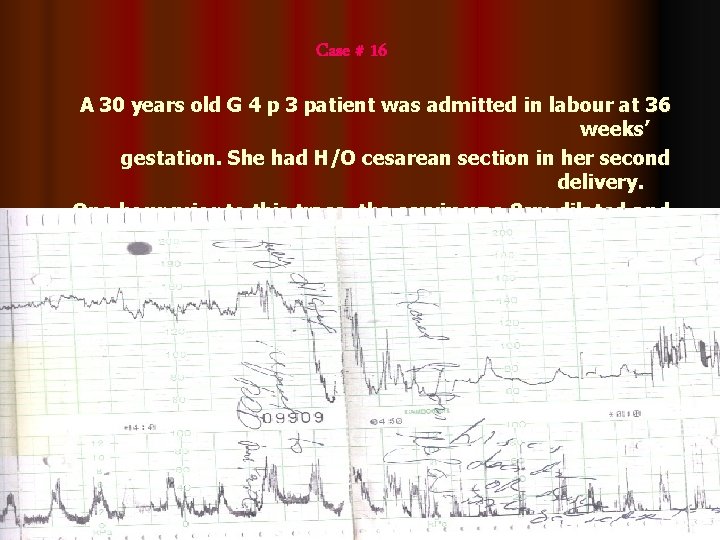
Case # 16 A 30 years old G 4 p 3 patient was admitted in labour at 36 weeks’ gestation. She had H/O cesarean section in her second delivery. One hour prior to this trace, the cervix was 8 cm dilated and clear liquor was draining
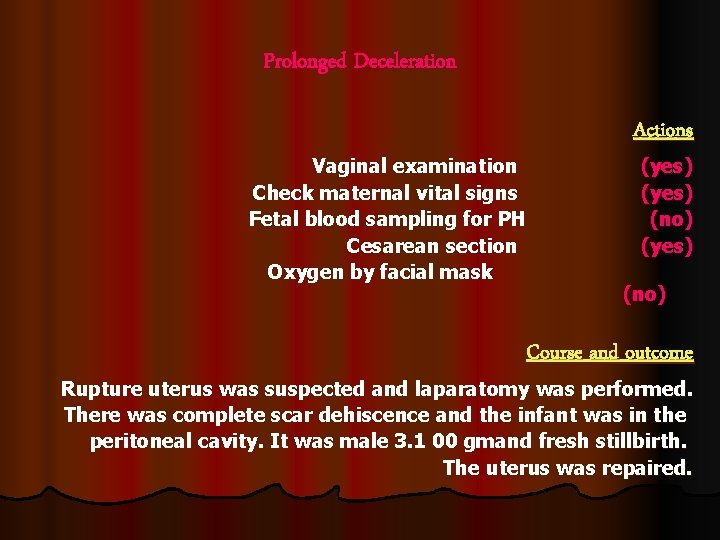
Prolonged Deceleration Actions Vaginal examination (yes) Check maternal vital signs (yes) Fetal blood sampling for PH (no) Cesarean section (yes) Oxygen by facial mask (no) Course and outcome Rupture uterus was suspected and laparatomy was performed. There was complete scar dehiscence and the infant was in the peritoneal cavity. It was male 3. 1 00 gmand fresh stillbirth. The uterus was repaired.
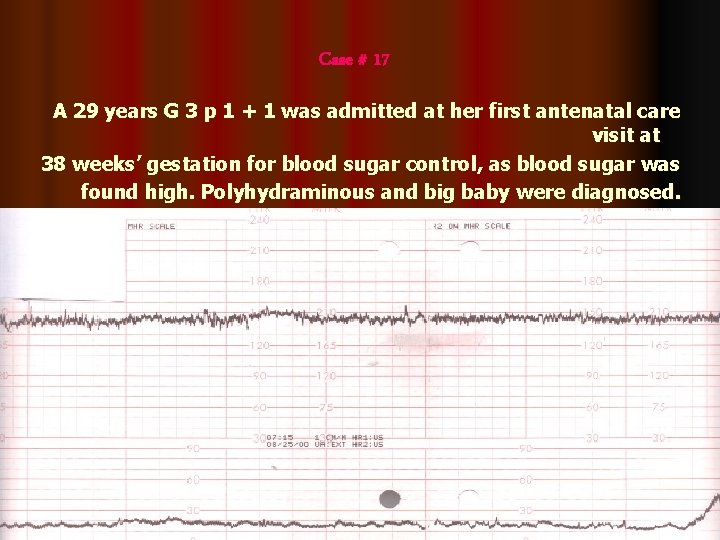
Case # 17 A 29 years G 3 p 1 + 1 was admitted at her first antenatal care visit at 38 weeks’ gestation for blood sugar control, as blood sugar was found high. Polyhydraminous and big baby were diagnosed. She started to complain of labour pains
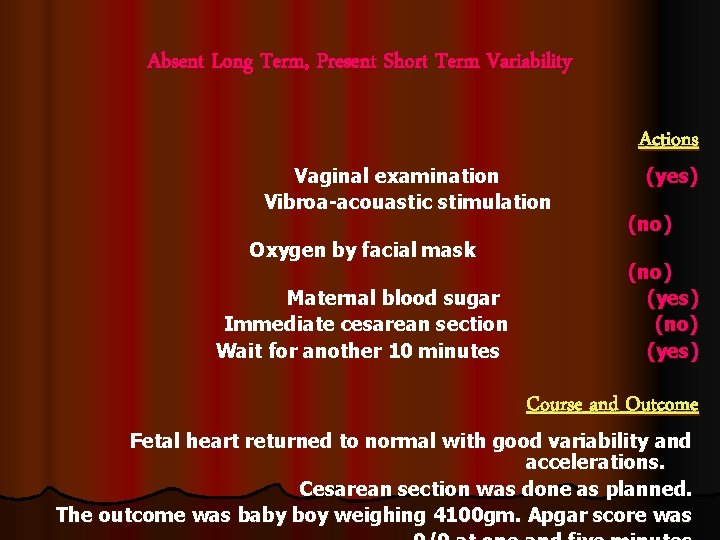
Absent Long Term, Present Short Term Variability Actions Vaginal examination (yes) Vibroa-acouastic stimulation (no) Oxygen by facial mask (no) Maternal blood sugar (yes) Immediate cesarean section (no) Wait for another 10 minutes (yes) Course and Outcome Fetal heart returned to normal with good variability and accelerations. Cesarean section was done as planned. The outcome was baby boy weighing 4100 gm. Apgar score was
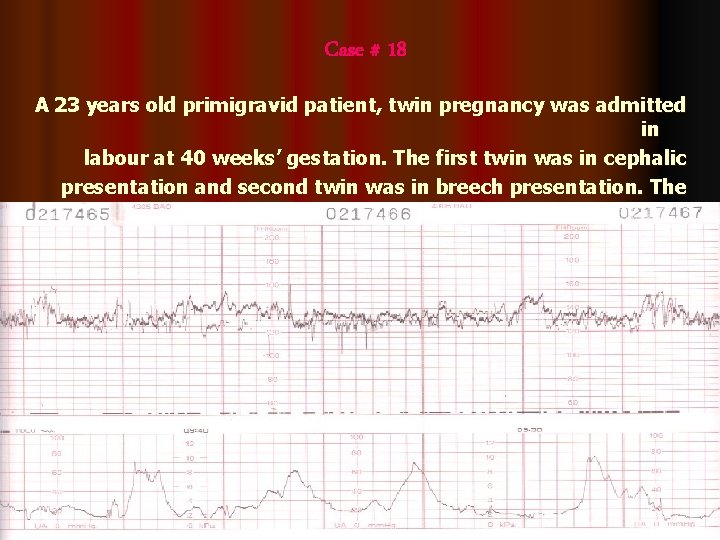
Case # 18 A 23 years old primigravid patient, twin pregnancy was admitted in labour at 40 weeks’ gestation. The first twin was in cephalic presentation and second twin was in breech presentation. The cervix was 3 cm dilated with intact membranes one hour earlier
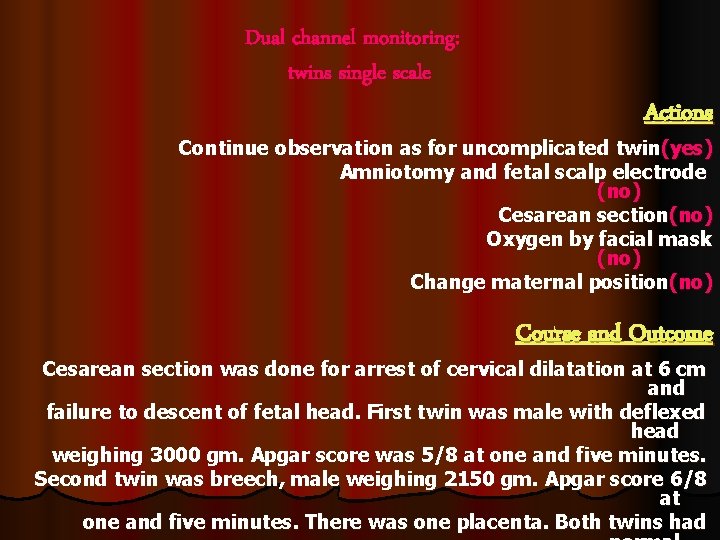
Dual channel monitoring: twins single scale Actions Continue observation as for uncomplicated twin(yes) Amniotomy and fetal scalp electrode (no) Cesarean section(no) Oxygen by facial mask (no) Change maternal position(no) Course and Outcome Cesarean section was done for arrest of cervical dilatation at 6 cm and failure to descent of fetal head. First twin was male with deflexed head weighing 3000 gm. Apgar score was 5/8 at one and five minutes. Second twin was breech, male weighing 2150 gm. Apgar score 6/8 at one and five minutes. There was one placenta. Both twins had
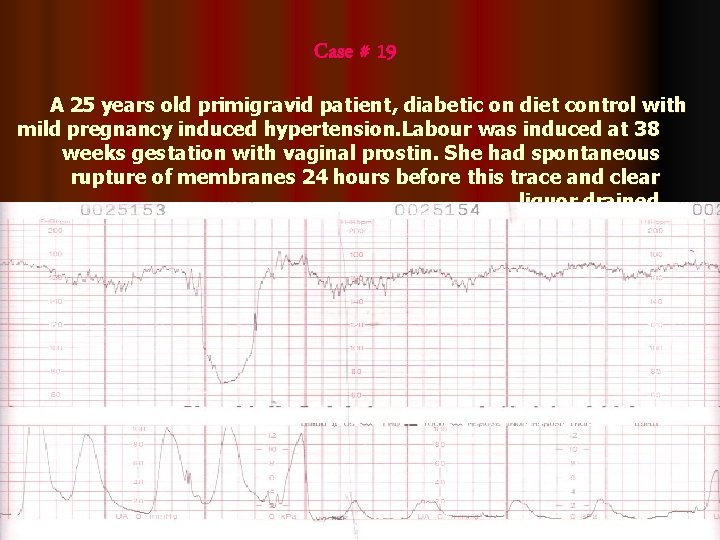
Case # 19 A 25 years old primigravid patient, diabetic on diet control with mild pregnancy induced hypertension. Labour was induced at 38 weeks gestation with vaginal prostin. She had spontaneous rupture of membranes 24 hours before this trace and clear liquor drained.
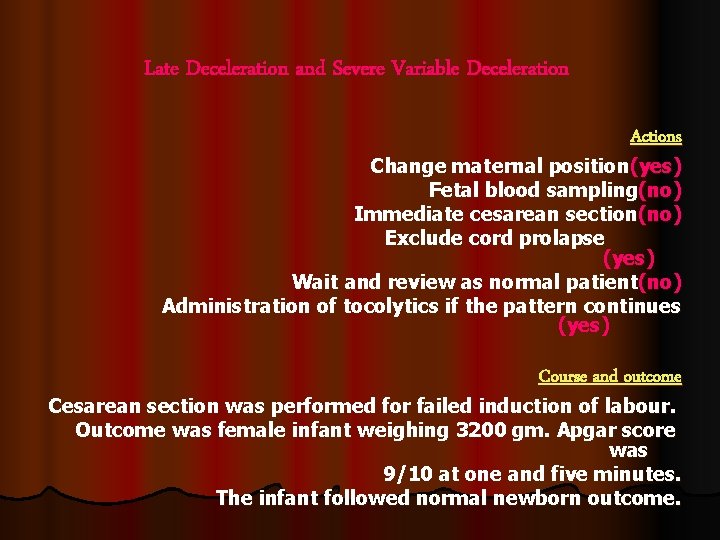
Late Deceleration and Severe Variable Deceleration Actions Change maternal position(yes) Fetal blood sampling(no) Immediate cesarean section(no) Exclude cord prolapse (yes) Wait and review as normal patient(no) Administration of tocolytics if the pattern continues (yes) Course and outcome Cesarean section was performed for failed induction of labour. Outcome was female infant weighing 3200 gm. Apgar score was 9/10 at one and five minutes. The infant followed normal newborn outcome.
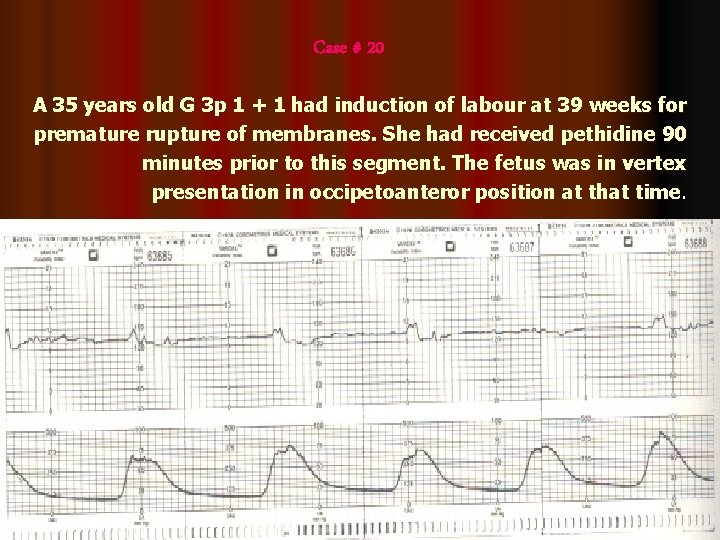
Case # 20 A 35 years old G 3 p 1 + 1 had induction of labour at 39 weeks for premature rupture of membranes. She had received pethidine 90 minutes prior to this segment. The fetus was in vertex presentation in occipetoanteror position at that time.
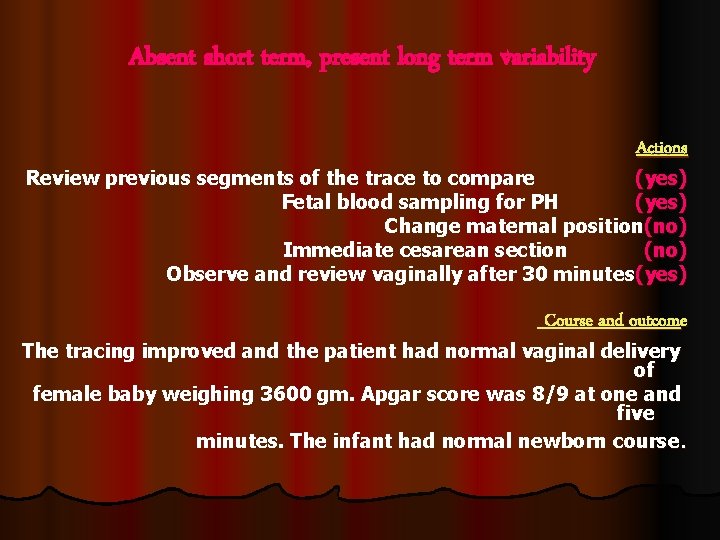
Absent short term, present long term variability Actions Review previous segments of the trace to compare (yes) Fetal blood sampling for PH (yes) Change maternal position(no) Immediate cesarean section (no) Observe and review vaginally after 30 minutes(yes) Course and outcome The tracing improved and the patient had normal vaginal delivery of female baby weighing 3600 gm. Apgar score was 8/9 at one and five minutes. The infant had normal newborn course.
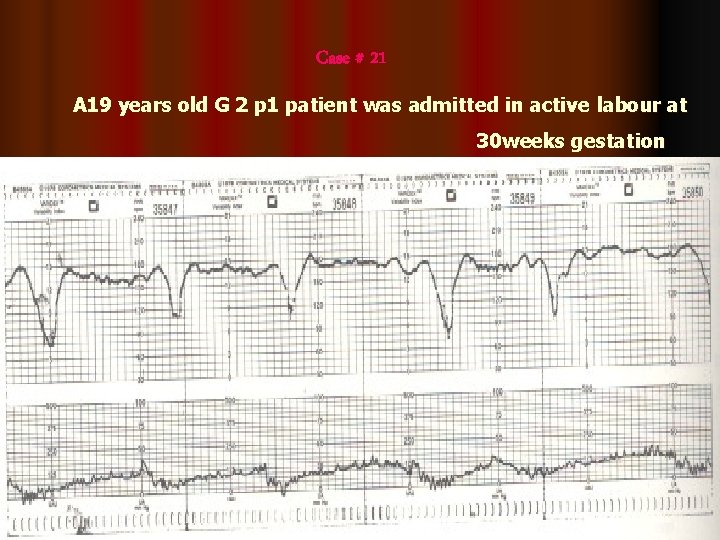
Case # 21 A 19 years old G 2 p 1 patient was admitted in active labour at 30 weeks gestation
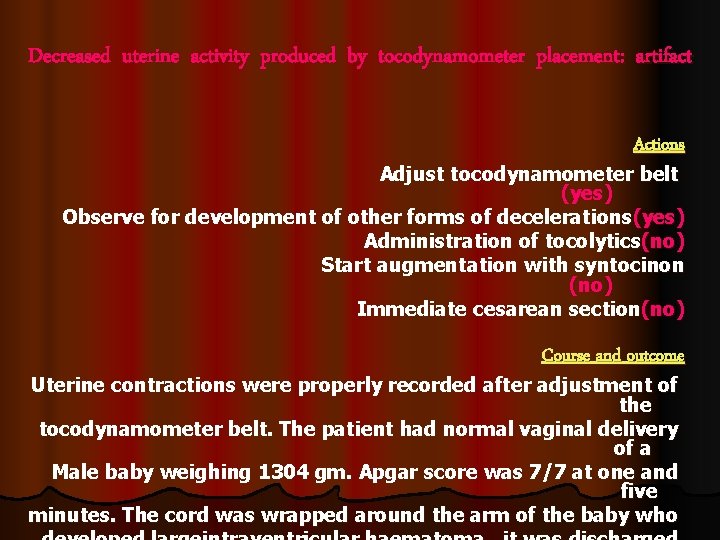
Decreased uterine activity produced by tocodynamometer placement: artifact Actions Adjust tocodynamometer belt (yes) Observe for development of other forms of decelerations (yes) Administration of tocolytics(no) Start augmentation with syntocinon (no) Immediate cesarean section(no) Course and outcome Uterine contractions were properly recorded after adjustment of the tocodynamometer belt. The patient had normal vaginal delivery of a Male baby weighing 1304 gm. Apgar score was 7/7 at one and five minutes. The cord was wrapped around the arm of the baby who
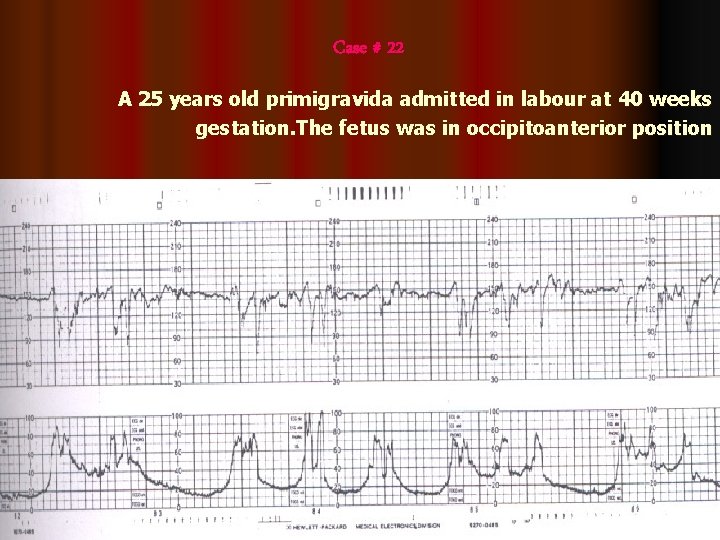
Case # 22 A 25 years old primigravida admitted in labour at 40 weeks gestation. The fetus was in occipitoanterior position
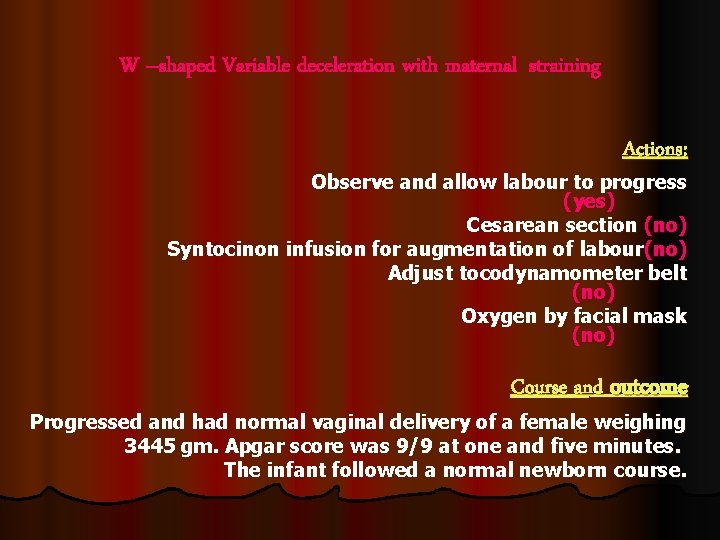
W –shaped Variable deceleration with maternal straining Actions: Observe and allow labour to progress (yes) Cesarean section (no) Syntocinon infusion for augmentation of labour(no) Adjust tocodynamometer belt (no) Oxygen by facial mask (no) Course and outcome Progressed and had normal vaginal delivery of a female weighing 3445 gm. Apgar score was 9/9 at one and five minutes. The infant followed a normal newborn course.

- Slides: 99