Salivary Gland Diseases DEPARTMENT OF ORAL MEDICINE RADIOLOGY



- Slides: 60
Salivary Gland Diseases DEPARTMENT OF ORAL MEDICINE & RADIOLOGY Dentistry Explorer
Introduction • Most common presentation of salivary gland disease – dry mouth Dentistry Explorer
Classification • Developmental abnormalities – Aplasia/agenesis • • Hemifacial microstomia Treacher Collin’s syndrome Lacrimo-auriculo-dento-digital syndrome Heriditary ectodermal dysplasia – Staphne’s cyst • Accessary salivary duct • Diverticuli – pouch protruding from the wall of a duct – recurrent sailadenitis • Darier’s Disease Dentistry Explorer
Classification • Sialolithiasis – Hydroxyapatite • Calcium phosphate & carbon • Mucoceles • Extravasation • Retention – Ranula Dentistry Explorer
Classification • Inflammatory and Reactive Lesions – Necrotizing sialometaplasia • Benign self-limiting reactive inflammatory disorder of salivary tissue – Kuttner’s Tumour • Chronic sclerosing sialadenitis – Radiation Induced Pathology • External • Internal Dentistry Explorer
Classification • Allergic Sialadenitis – Allergens • • Ethambutol Heavy metals Iodine Phenobarbital – Acute enlargement • Bacterial and viral Sialadenitis Dentistry Explorer
Classification • Systemic conditions with salivary gland involvement: • • • Diabetes Mellitus Anorexia Nervosa Chronic alcoholism Dehydration Drugs – – – Tricyclic antidepressants Anticholinergics Antihistamines Antihypertensives Cytotoxic agents Antiseizure medications Dentistry Explorer
Classification • Systemic conditions with salivary gland involvement: • Mikulicz’s disease • Sjogren’s syndrome • Granulomatous conditions – Tuberculosis – Sarcoidosis Dentistry Explorer
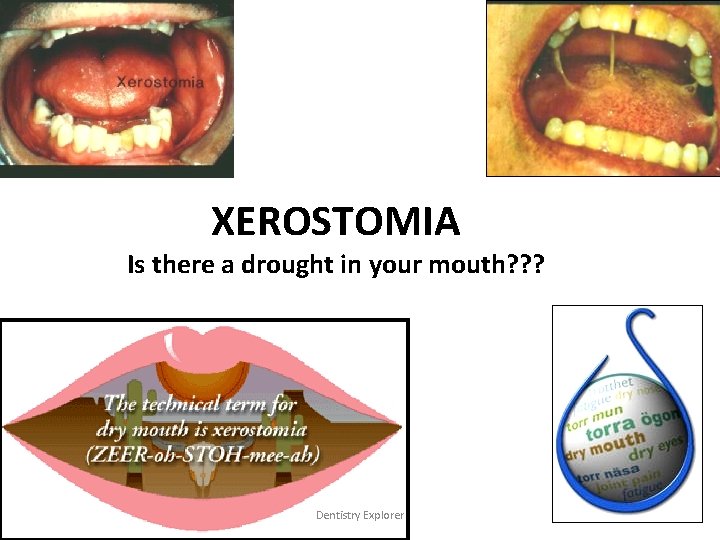
XEROSTOMIA Is there a drought in your mouth? ? ? Dentistry Explorer
• Subjective feeling of dryness • The dental term “xerostomia” means dryness of mouth due to decreased function of the glands that produce saliva Dentistry Explorer
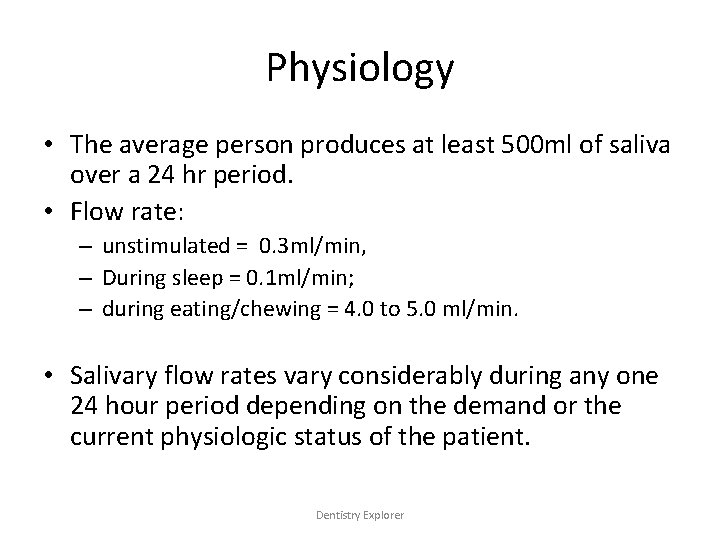
Physiology • The average person produces at least 500 ml of saliva over a 24 hr period. • Flow rate: – unstimulated = 0. 3 ml/min, – During sleep = 0. 1 ml/min; – during eating/chewing = 4. 0 to 5. 0 ml/min. • Salivary flow rates vary considerably during any one 24 hour period depending on the demand or the current physiologic status of the patient. Dentistry Explorer
Pathophysiology • Salivary gland secretion is mainly under autonomic nervous control, but various hormones may also modulate salivary composition. 1. Parasympathetic nerve fibers → release of Ach, substance P → act on alpha receptors → increases Calcium ions in serous acinar cells → profuse secretion with decreased amylase(watery). 2. Sympathetic nerve fibers → release of norepinephrine, vasoactive intestinal polypeptides → act on beta receptors → increases cyclic Adenosine monophosphate in acinar cells → secretion rich in amylase(thick). • Dentistry Explorer
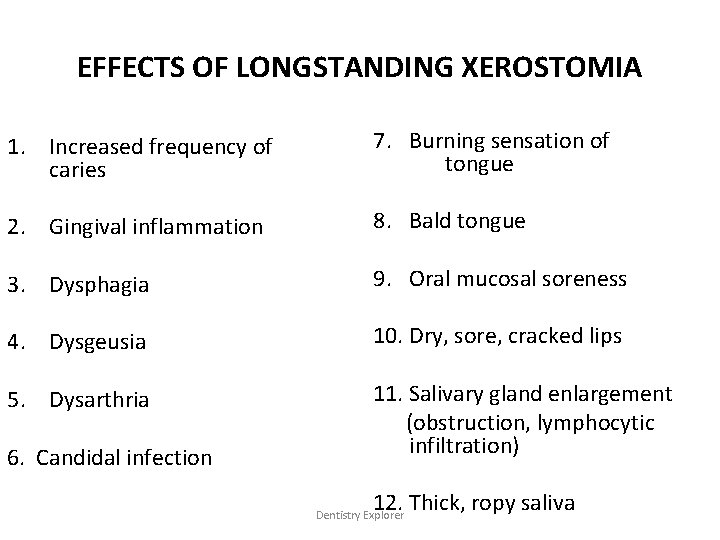
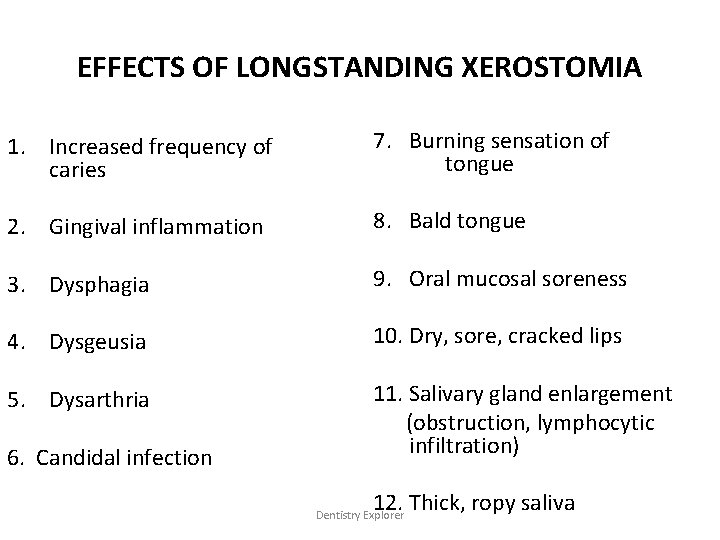
EFFECTS OF LONGSTANDING XEROSTOMIA 1. Increased frequency of caries 7. Burning sensation of tongue 2. Gingival inflammation 8. Bald tongue 3. Dysphagia 9. Oral mucosal soreness 4. Dysgeusia 10. Dry, sore, cracked lips 5. Dysarthria 11. Salivary gland enlargement (obstruction, lymphocytic infiltration) 6. Candidal infection 12. Thick, ropy saliva Dentistry Explorer

Dentistry Explorer
DIAGNOSIS • HISTORY • CLINICAL EXAMINATION • INVESTIGATIONS Dentistry Explorer
HISTORY • Medical condition and medication • History of radiotherapy • Dryness of other parts of body • Pain in joints. Dentistry Explorer
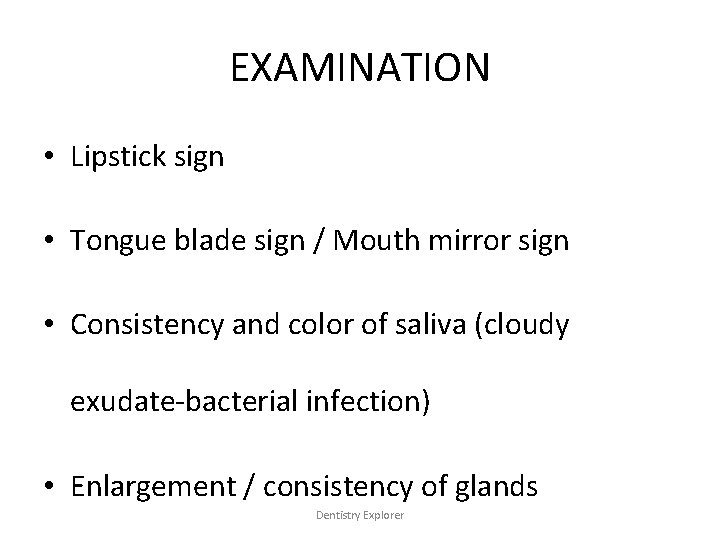
EXAMINATION • Lipstick sign • Tongue blade sign / Mouth mirror sign • Consistency and color of saliva (cloudy exudate-bacterial infection) • Enlargement / consistency of glands Dentistry Explorer
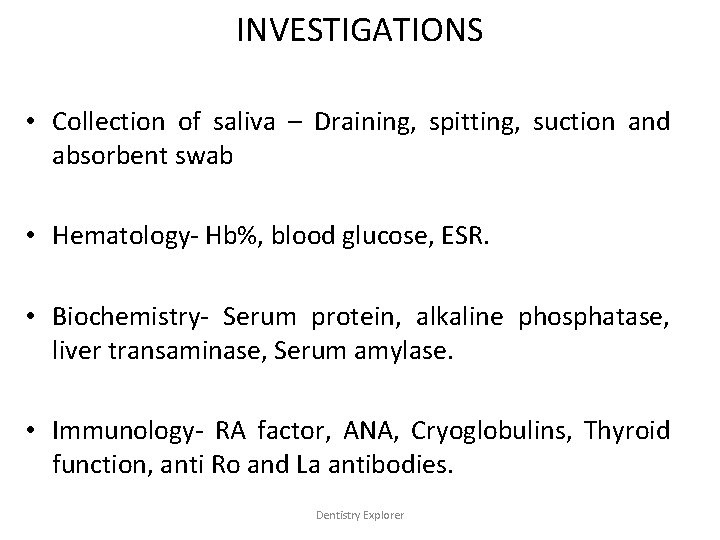
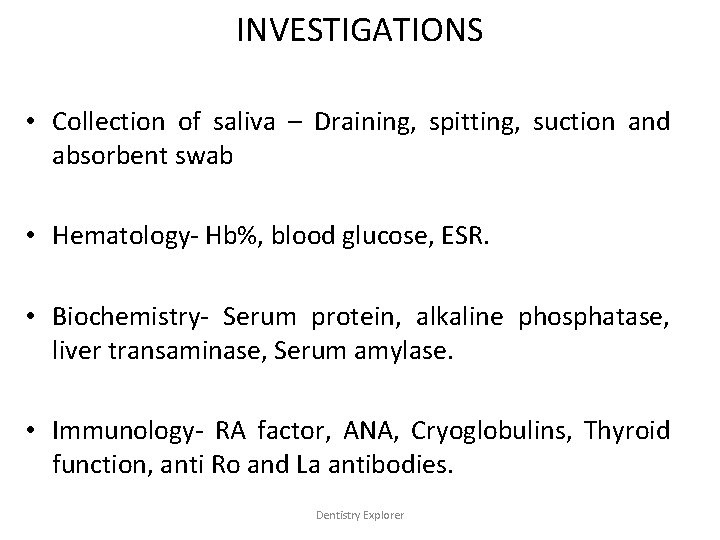
INVESTIGATIONS • Collection of saliva – Draining, spitting, suction and absorbent swab • Hematology- Hb%, blood glucose, ESR. • Biochemistry- Serum protein, alkaline phosphatase, liver transaminase, Serum amylase. • Immunology- RA factor, ANA, Cryoglobulins, Thyroid function, anti Ro and La antibodies. Dentistry Explorer

INVESTIGATIONS • Histopathology of minor salivary gland tissue. • Sialometry-salivary flow • Sialochemistry- Saliva can be collected either by spitting, suction, draining or absorbent method. Carlson Crittenden collector & Lashley’s cup are used to collect parotid saliva and Segregator is used to collect submandibular saliva (BY ASPIRATING). • Miscellaneous tests like Schirmer’s test, Rose Bengal dye test, Break up time test. Dentistry Explorer
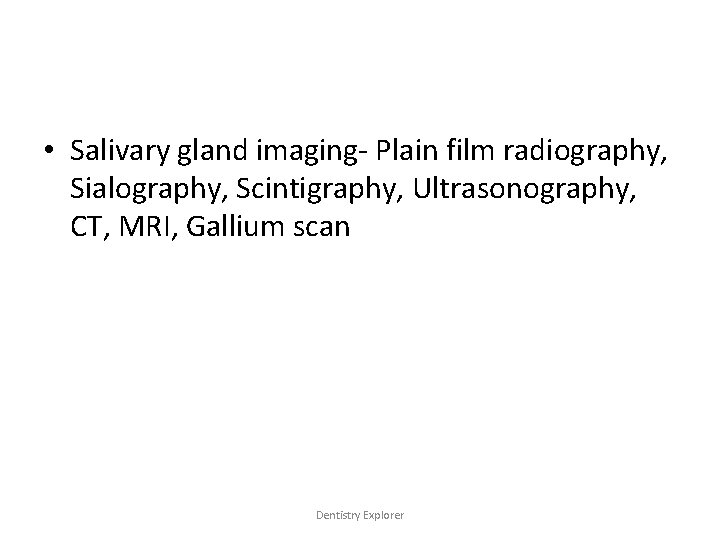
• Salivary gland imaging- Plain film radiography, Sialography, Scintigraphy, Ultrasonography, CT, MRI, Gallium scan Dentistry Explorer
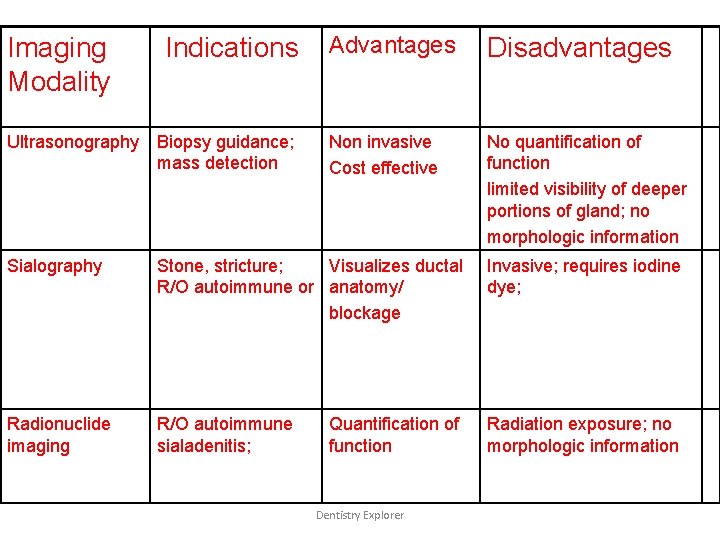
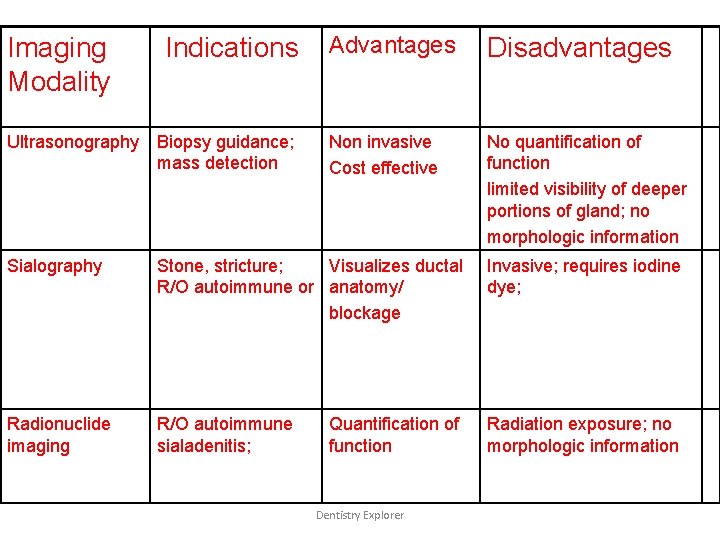
Imaging Modality Indications Ultrasonography Biopsy guidance; mass detection Advantages Disadvantages Non invasive Cost effective No quantification of function limited visibility of deeper portions of gland; no morphologic information Sialography Stone, stricture; Visualizes ductal R/O autoimmune or anatomy/ blockage Invasive; requires iodine dye; Radionuclide imaging R/O autoimmune sialadenitis; Radiation exposure; no morphologic information Quantification of function Dentistry Explorer
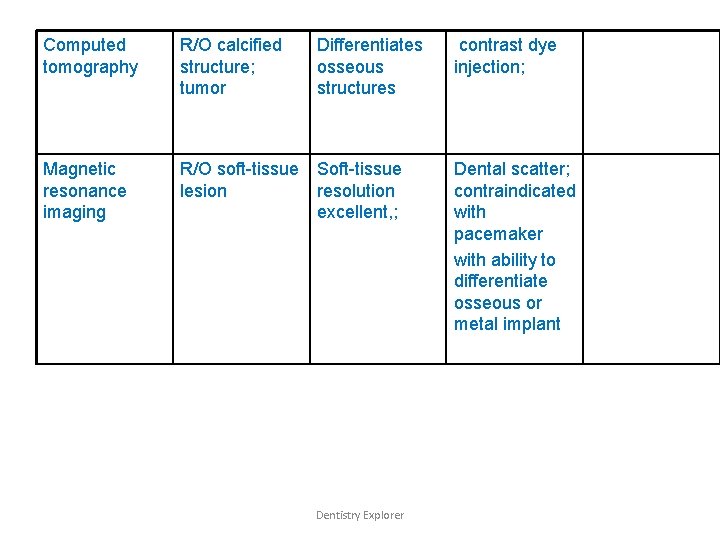
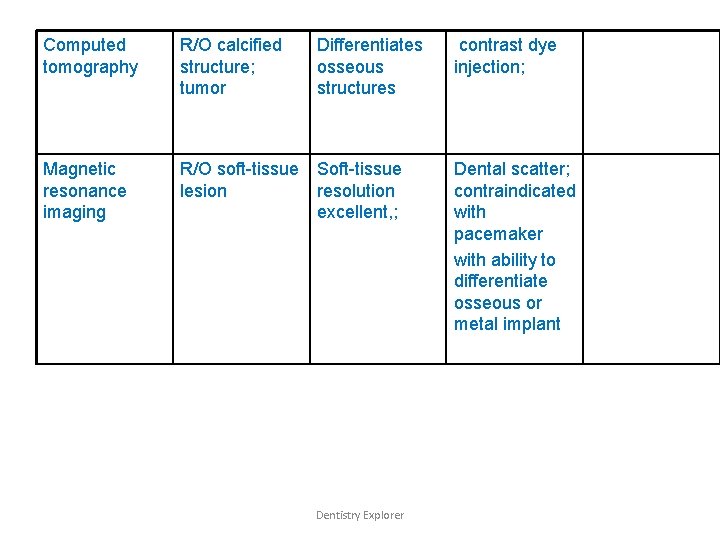
Computed tomography R/O calcified structure; tumor Differentiates osseous structures Magnetic resonance imaging R/O soft-tissue Soft-tissue lesion resolution excellent, ; Dentistry Explorer contrast dye injection; Dental scatter; contraindicated with pacemaker with ability to differentiate osseous or metal implant
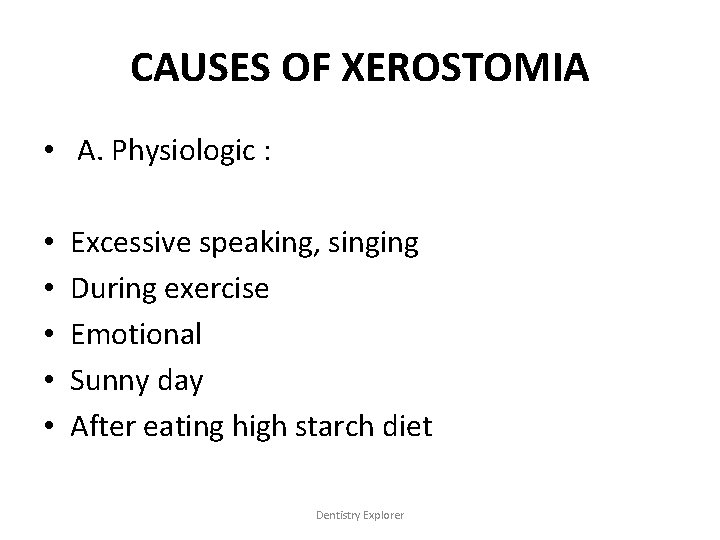
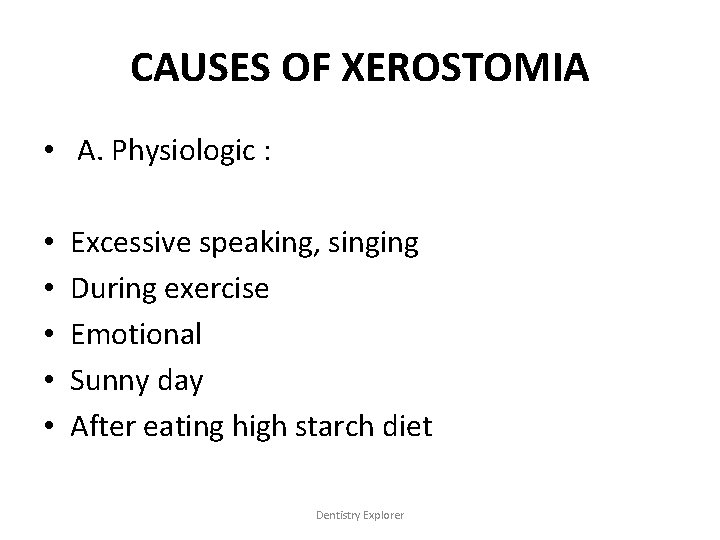
CAUSES OF XEROSTOMIA • A. Physiologic : • • • Excessive speaking, singing During exercise Emotional Sunny day After eating high starch diet Dentistry Explorer
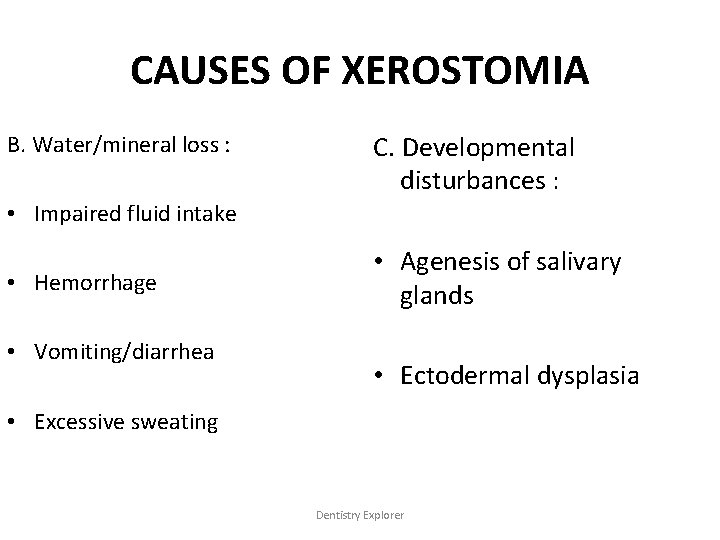
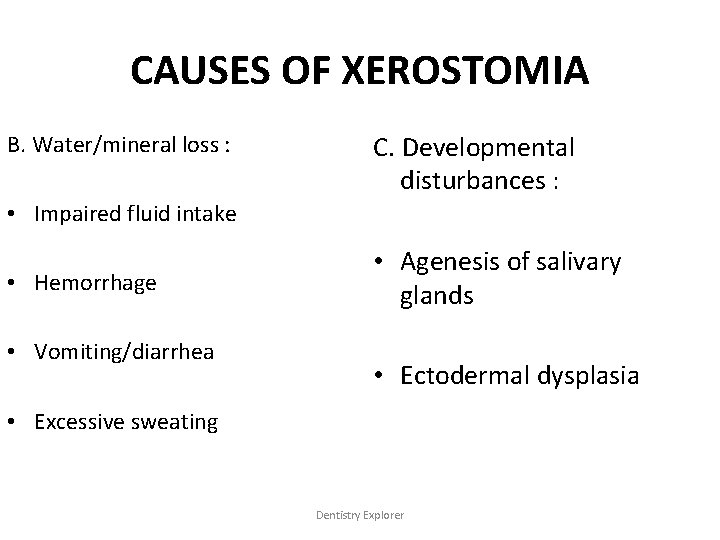
CAUSES OF XEROSTOMIA B. Water/mineral loss : C. Developmental disturbances : • Impaired fluid intake • Hemorrhage • Vomiting/diarrhea • Agenesis of salivary glands • Ectodermal dysplasia • Excessive sweating Dentistry Explorer
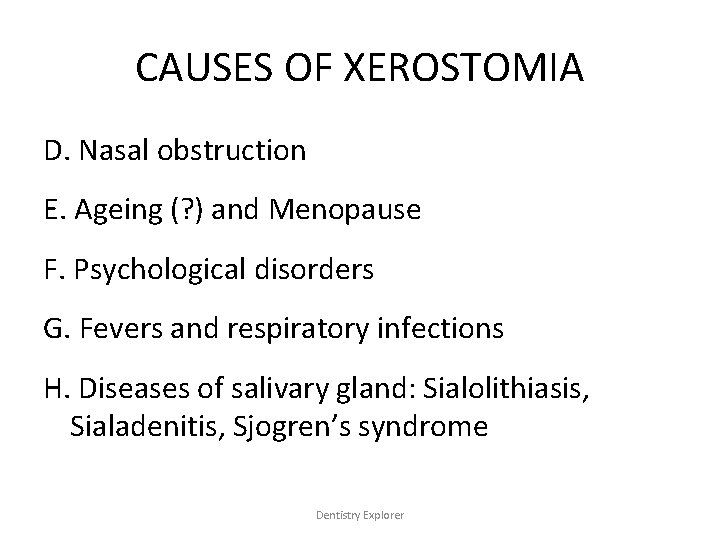
CAUSES OF XEROSTOMIA D. Nasal obstruction E. Ageing (? ) and Menopause F. Psychological disorders G. Fevers and respiratory infections H. Diseases of salivary gland: Sialolithiasis, Sialadenitis, Sjogren’s syndrome Dentistry Explorer
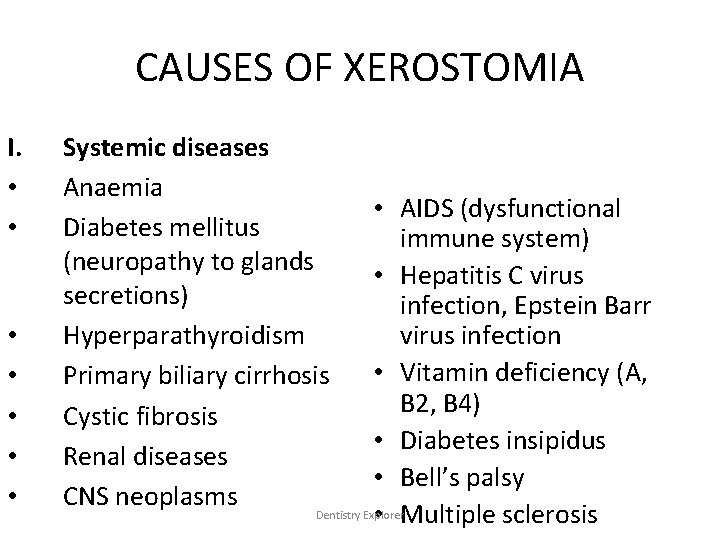
CAUSES OF XEROSTOMIA I. • • Systemic diseases Anaemia • AIDS (dysfunctional Diabetes mellitus immune system) (neuropathy to glands • Hepatitis C virus secretions) infection, Epstein Barr Hyperparathyroidism virus infection • Vitamin deficiency (A, Primary biliary cirrhosis B 2, B 4) Cystic fibrosis • Diabetes insipidus Renal diseases • Bell’s palsy CNS neoplasms Dentistry Explorer • Multiple sclerosis
CAUSES OF XEROSTOMIA J. Iatrogenic : • Drugs (antihypertensives, antiasthmatics, antihistami ne, antipsychotic, sedatives, diuretics) • Radiation therapy • Chemotherapy (makes saliva thicker causing dry mouth) Dentistry Explorer
CAUSES OF XEROSTOMIA K. Rarities : • Amyloidosis • Wegener’s disease • Hemochromatosis L. Local factors : • Smoking • Decreased mastication Dentistry Explorer
Dentistry Explorer
Dentistry Explorer
MANAGEMENT • Topical therapies: – Water, – Sugar free gum, – candies and liquids, – sugar free lemon drops, – glycerine swabs, – lubricating gels (aloe vera, vitamin E), – mouth washes, – lozenges, – tooth pastes Dentistry Explorer
MANAGEMENT • Topical therapy: – salivary stimulant pastilles, – mucin spray, – humidifiers, – saliva substitute placed in intraoral device, – artificial saliva ( carboxy methyl cellulose, gastrin, mucins, water, bicarbonates). Dentistry Explorer
MANAGEMENT • Systemic agents: – Pilocarpine (15 mg/d), – Bethanechol (75 -200 mg/d in divided dose), – Cevimeline, – Interferon ά, – Carbacholine, – Bromhexine, – Pyridostigmine, – Corticosteroids, Dentistry Explorer
MANAGEMENT • Systemic agents: – hydroxychloroquine, – vitamins, – electrostimulation, – evening primrose oil, – Acupuncture Dentistry Explorer
MANAGEMENT • Amifostine – administered IV before irradiation lessens the severity of radiation induced xerostomia. • Pyridostigmine – benefits the treatment of drug related xerostomia. • Interferon ά – augments the transcription and production of aquaporin -5, which, in vitro, is a membrane-bound protein important in lacrimal and salivary gland function. Dentistry Explorer
MANAGEMENT • Supportive therapy : – Topical fluoride (0. 05%) mouthwashes, – Chlorhexidine mouthwashes, – Antifungals • nystatin pastilles, • amphoterecin lozenges, • miconazole gels, – dietary advice, – proper denture fit and instructions, – pit & fissure sealants. Dentistry Explorer
Sialorrea • Excessive secretion of saliva • Hypersalivation • Causes • Increase in saliva production • Decrease in salivary clearance • Medications – – – Pilocarpine Cevimeline Lithium Nitrazepam Clozapine Dentistry Explorer
• Causes – Hyperhydration – Infant teething – Secretory phase of menstruation – Heavy metal Poisoning – GERD – Obstructive esophagitis – Neurological changes eg: cerebral vascular accidents – Neuromuscular diseases – Minor hypersalivation • Apthous ulcers • Ill-fitting oral prosthesis Dentistry Explorer
Clinical Features • Drooling- impaired quality of life • Partial or total blockage of airway – aspiration of oral contents • Perioral irritation & traumatic ulceration – secondarily infected with fungus & Bacteria Dentistry Explorer
Diagnosis • Exact History of hypersalivation and past medical history • Systematic oral evaluation – • • • salivary gland enlargement, oral ulceration, orofacial mass, neuromuscular function, condition of prosthesis Dentistry Explorer
Diagnosis • 2 major issues: – Clearance – Production - swallowing study - salivary flow rate • Blood samples – Heavy metals – Organophosphate pesticides • CT scan – If onset is acute – CVA Dentistry Explorer

Treatment • 3 major therapy – Physical therapy – Medicinal therapy – Surgery • Physical Therapy – To improve neuromuscular control – Speech & swallowing therapy Dentistry Explorer
Treatment • Medicinal Therapy – Depending on etiology – If medicine induced - Alternative medication – If due to chronic nausea (chemotherapy) – antiemetic drug – If due to systemic condition – treat the cause Dentistry Explorer
Treatment • Xerostomic agents • • • Atropine Glycopyrrolate Diphenhydramine hydrochloride Scopalamine transdermal patch Propantheline Benztropine Dentistry Explorer
Treatment • Surgical Therapy – Redirection of submandibular & parotid ducts posterior to tonsillar pillars – Bilateral tympanic neuronectomy – Redirection of submandibular duct and excision of sublingual gland – Ductal Ligation of all major submandibular/sublingual ducts Dentistry Explorer
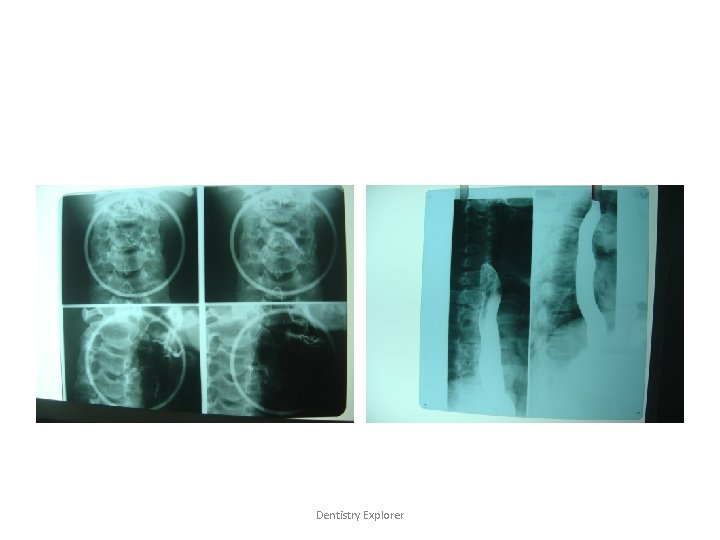
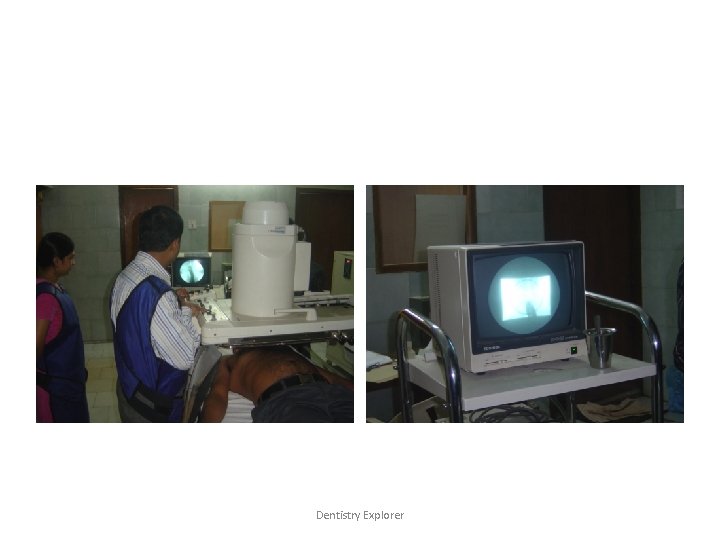
SIALOGRAPHY Dentistry Explorer
INTRODUCTION • Radiographic visualization of salivary gland following retrograde instillation of soluble contrast material into the ducts • Glands are cannulated and filled with a radiopaque contrast to make them visible in the radiograph Dentistry Explorer
INTRODUCTION • Reveals the location and integrity of gland • Indicates the presence of diseases that change the internal architecture Dentistry Explorer
Indications • Detection of calculi/foreign bodies • Determination of extent of destruction of gland secondary to obstructing calculi • Detection of fistula, diverticuli, strictures • Diagnosis of recurrent swellings and inflammatory processes • Demonstration of tumour • Selection of a site for biopsy • Therapeutic purpose Dentistry Explorer
Contraindications • Patients with sensitivity to iodine compounds • Asthmatic patients/anaphylaxis • Acute inflammation • Thyroid function test – to be done prior sialography Dentistry Explorer
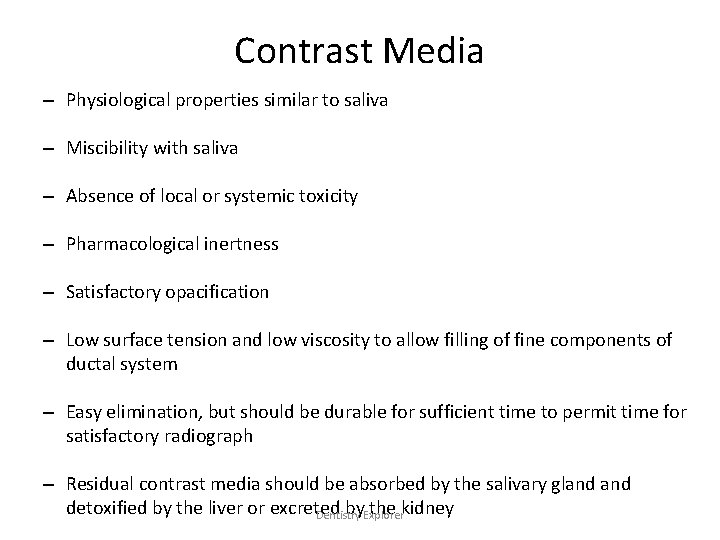
Contrast Media – Physiological properties similar to saliva – Miscibility with saliva – Absence of local or systemic toxicity – Pharmacological inertness – Satisfactory opacification – Low surface tension and low viscosity to allow filling of fine components of ductal system – Easy elimination, but should be durable for sufficient time to permit time for satisfactory radiograph – Residual contrast media should be absorbed by the salivary gland detoxified by the liver or excreted by. Explorer the kidney Dentistry
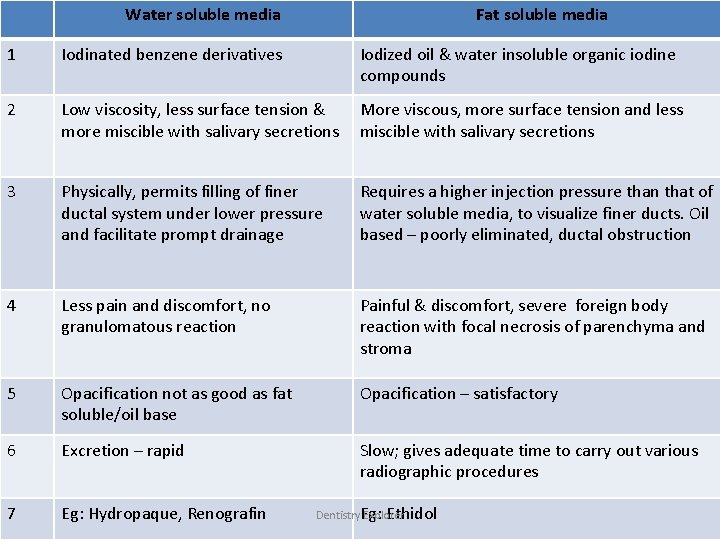
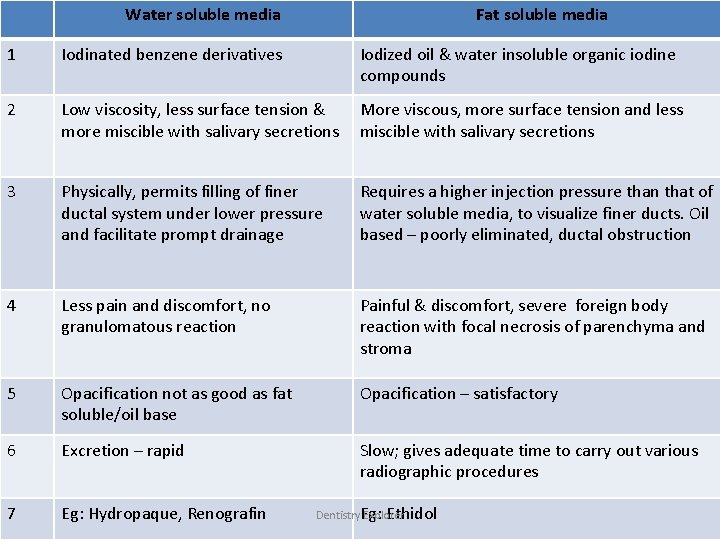
Water soluble media Fat soluble media 1 Iodinated benzene derivatives Iodized oil & water insoluble organic iodine compounds 2 Low viscosity, less surface tension & more miscible with salivary secretions More viscous, more surface tension and less miscible with salivary secretions 3 Physically, permits filling of finer ductal system under lower pressure and facilitate prompt drainage Requires a higher injection pressure than that of water soluble media, to visualize finer ducts. Oil based – poorly eliminated, ductal obstruction 4 Less pain and discomfort, no granulomatous reaction Painful & discomfort, severe foreign body reaction with focal necrosis of parenchyma and stroma 5 Opacification not as good as fat soluble/oil base Opacification – satisfactory 6 Excretion – rapid Slow; gives adequate time to carry out various radiographic procedures 7 Eg: Hydropaque, Renografin Ethidol Dentistry. Eg: Explorer
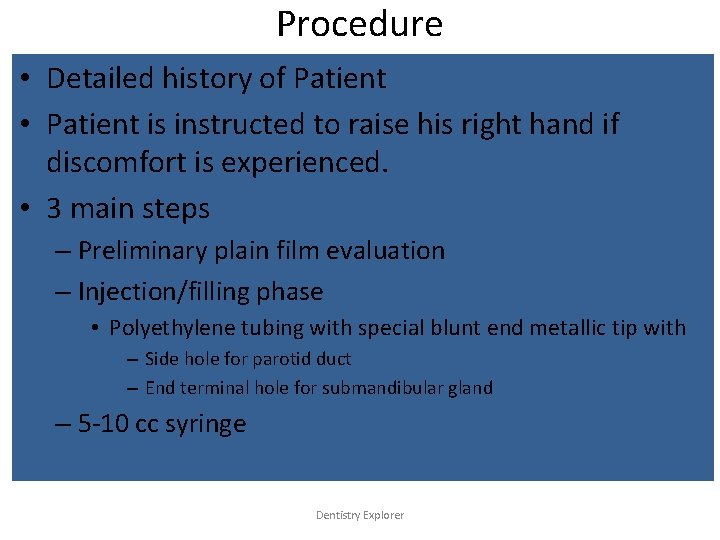
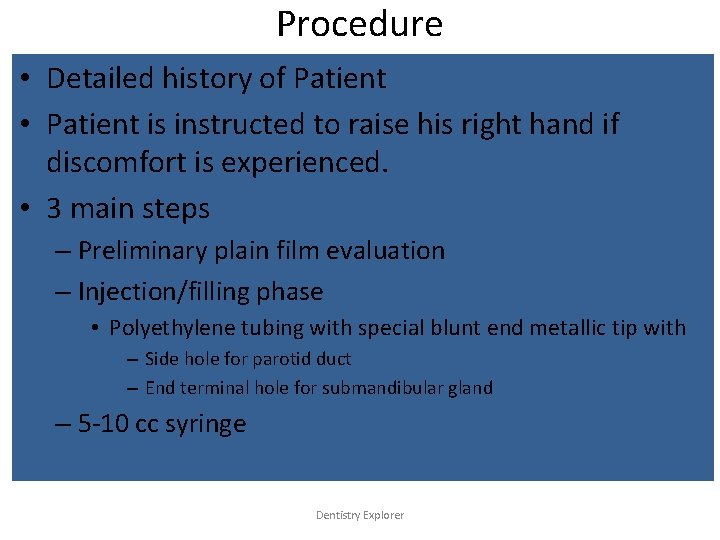
Procedure • Detailed history of Patient • Patient is instructed to raise his right hand if discomfort is experienced. • 3 main steps – Preliminary plain film evaluation – Injection/filling phase • Polyethylene tubing with special blunt end metallic tip with – Side hole for parotid duct – End terminal hole for submandibular gland – 5 -10 cc syringe Dentistry Explorer
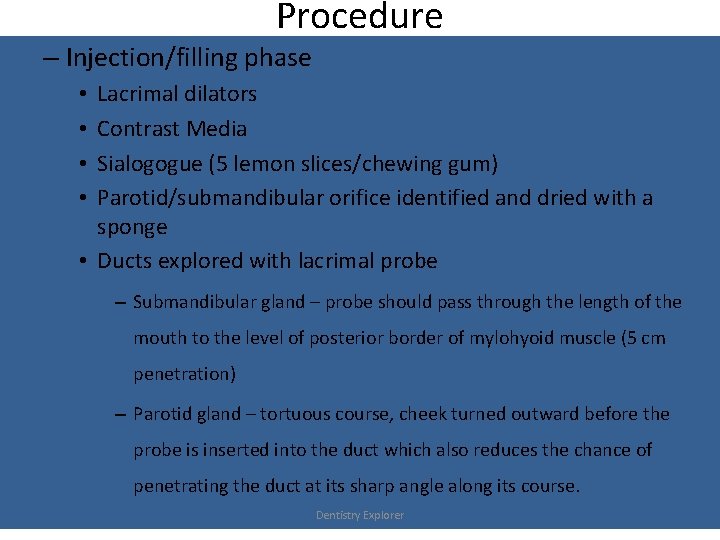
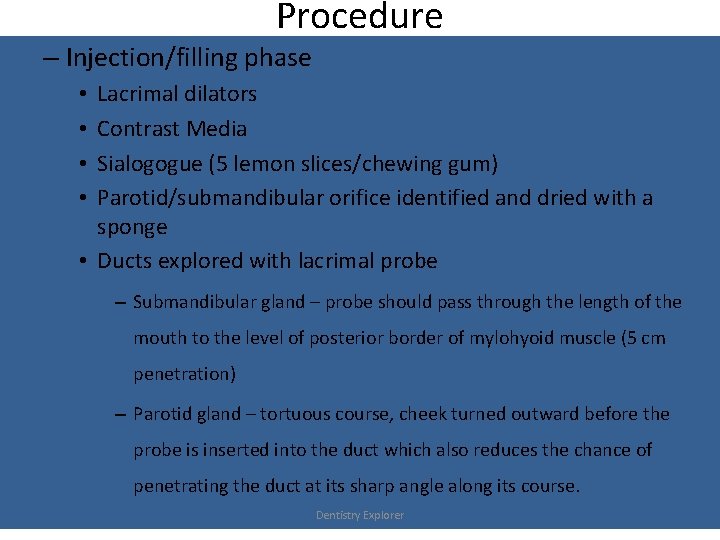
Procedure – Injection/filling phase Lacrimal dilators Contrast Media Sialogogue (5 lemon slices/chewing gum) Parotid/submandibular orifice identified and dried with a sponge • Ducts explored with lacrimal probe • • – Submandibular gland – probe should pass through the length of the mouth to the level of posterior border of mylohyoid muscle (5 cm penetration) – Parotid gland – tortuous course, cheek turned outward before the probe is inserted into the duct which also reduces the chance of penetrating the duct at its sharp angle along its course. Dentistry Explorer
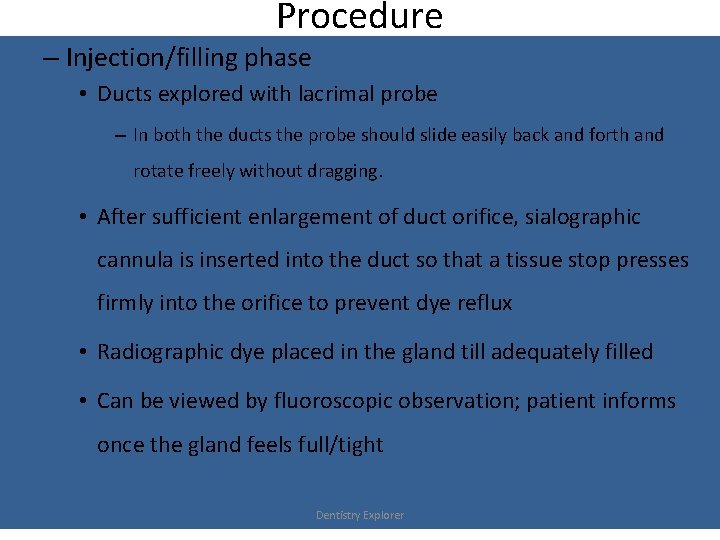
Procedure – Injection/filling phase • Ducts explored with lacrimal probe – In both the ducts the probe should slide easily back and forth and rotate freely without dragging. • After sufficient enlargement of duct orifice, sialographic cannula is inserted into the duct so that a tissue stop presses firmly into the orifice to prevent dye reflux • Radiographic dye placed in the gland till adequately filled • Can be viewed by fluoroscopic observation; patient informs once the gland feels full/tight Dentistry Explorer
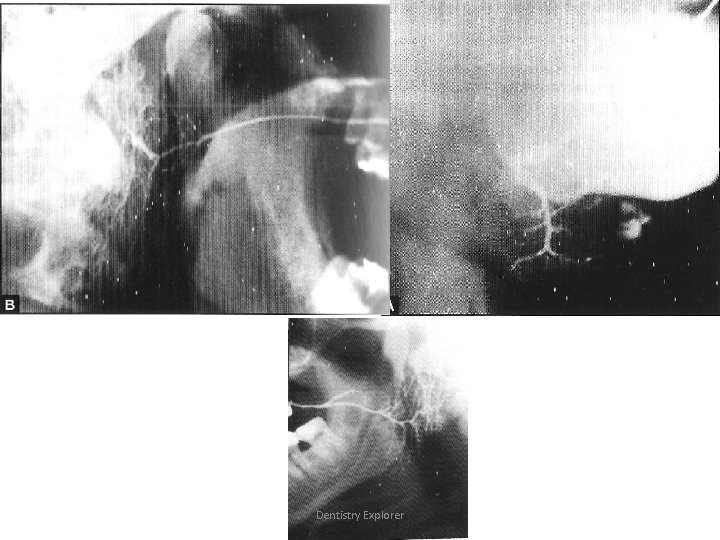
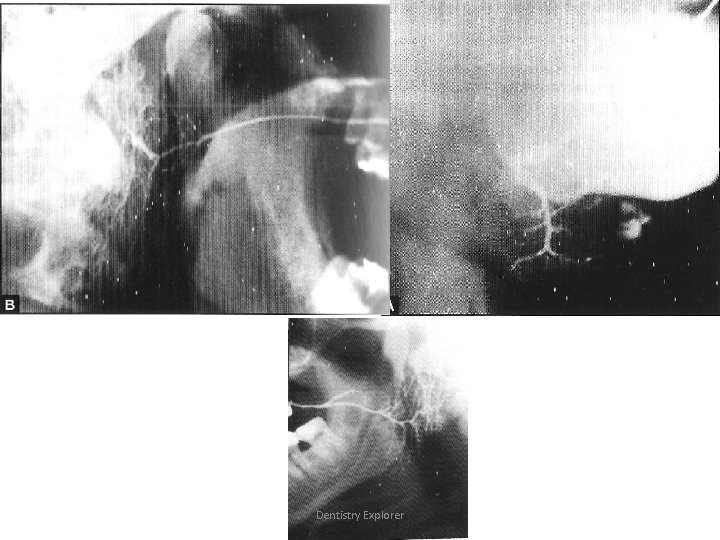
– Injection/filling phase • Volume required: – Parotid – 0. 76 -1 ml – Submandibular – 0 -0. 75 ml • If dye overfills, discomfort is noticed • Radiographic projections – Patients placed in supine position – Dentures removed – Several radiographs obtained to monitor filling phase & degree of filling – Lateral oblique projection (duct pattern is not distorted) or mandibular occlusal view- sialilith detected (submandibular gland) – AP view: medial and lateral gland structures viewed » Parotid – mouth should be kept open (reduces superimposition of mandible on parotid gland) Dentistry Explorer
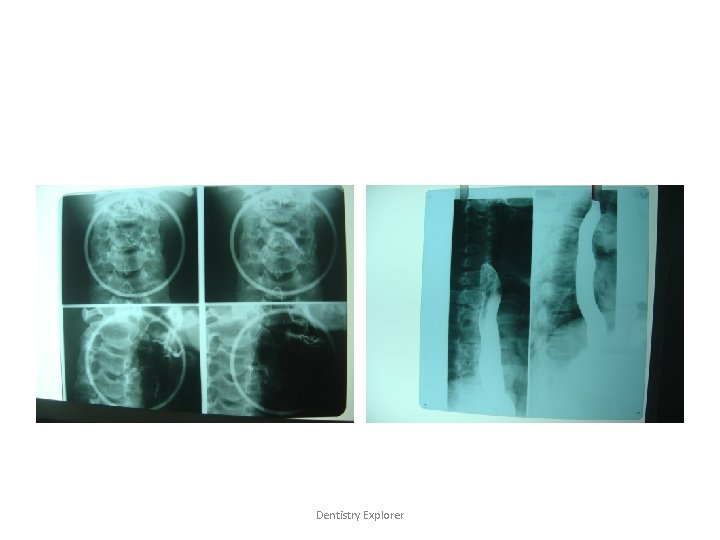
Dentistry Explorer
Procedure – Injection/filling phase • Radiographic projections – OPG » to detect the erosion of bone » Destruction of mandible salivary tumours – Other views » Reverse basilar view to demonstrate deep parotid » Puffed cheek view – superficial portion of stenson’s duct » RG with mouth open – reduces superimposition of mandible on parotid gland Dentistry Explorer
Procedure – Parenchymal phase • After final view, cannula removed from duct orifice • Patient instructed to chew gum/lemon slice and rinse to stimulate the gland cause excretion of the dye • Repeat radiographs taken every 5 minutes after cannula removal • Normal gland excretes 100% contrast media within 5 mins. of removal of cannula Dentistry Explorer
Advancements • Interventional sialography – Balloon catheters and small Dormia basket under fluoroscopic guidance – Balloon catheter is inflated and produce dilation of ductal strictures – Dormia basket – to retrieve mobile ductal stones. – Major advantage – no need of surgery Dentistry Explorer
 Oral disease
Oral disease Warthin tumor
Warthin tumor Types of salivary glands
Types of salivary glands Warthin's tumor
Warthin's tumor Cylindroma slideshare
Cylindroma slideshare Gland histology
Gland histology Salivary gland histology
Salivary gland histology Warthin's tumor
Warthin's tumor Pathogenesis of pleomorphic adenoma
Pathogenesis of pleomorphic adenoma Oncocytoma salivary gland
Oncocytoma salivary gland Weber's gland
Weber's gland Simple branched acinar
Simple branched acinar Basal cell adenoma
Basal cell adenoma Salivary gland
Salivary gland Functions of bile juice
Functions of bile juice Salivary gland disorders classification
Salivary gland disorders classification Pleomorphic adenoma
Pleomorphic adenoma Pineal gland pituitary gland
Pineal gland pituitary gland Pituitary gland and pineal gland spiritual
Pituitary gland and pineal gland spiritual American academy of oral and maxillofacial radiology
American academy of oral and maxillofacial radiology Cholecystolithiasis
Cholecystolithiasis Oral pathology
Oral pathology Dentobuff strip system
Dentobuff strip system Salivary amylase digestion of starch
Salivary amylase digestion of starch Dysphagia terminology
Dysphagia terminology Phadebas paper
Phadebas paper Basal cell adenoma
Basal cell adenoma Pancreas organ
Pancreas organ Types of salivary glands
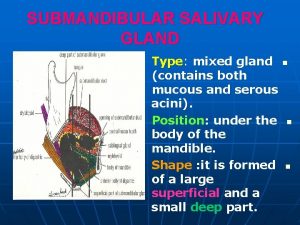
Types of salivary glands Sialography
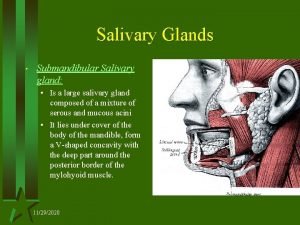
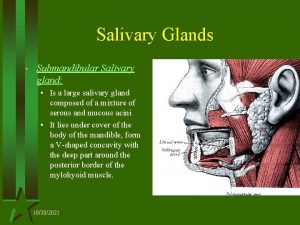
Sialography Sialography
Sialography Saliva formation
Saliva formation Lactobacillus colony count test
Lactobacillus colony count test Minor salivary glands
Minor salivary glands Colon
Colon Department of medicine solna
Department of medicine solna Department of medicine mcgill
Department of medicine mcgill Ellis curve x ray
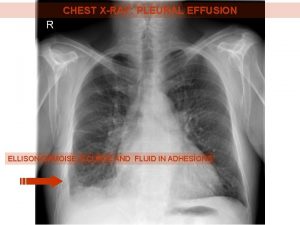
Ellis curve x ray Empty notch sign radiology
Empty notch sign radiology El camino college radiology
El camino college radiology Silicosis radiology
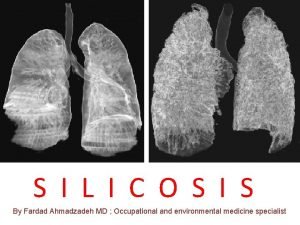
Silicosis radiology Gonad shielding
Gonad shielding Radiology alert system
Radiology alert system Statdx elsevier
Statdx elsevier Hlc accreditation
Hlc accreditation Magnetic resonance timisoara
Magnetic resonance timisoara Oid in radiology
Oid in radiology X ray mastoid towns view
X ray mastoid towns view Varicocele grading radiology assistant
Varicocele grading radiology assistant Fruit laden tree appearance
Fruit laden tree appearance Linear energy transfer
Linear energy transfer Karisma medical software
Karisma medical software Angiofibroma nasofaring
Angiofibroma nasofaring Radiolysis of water ppt
Radiolysis of water ppt Lens
Lens Radiology st1 competition ratio
Radiology st1 competition ratio Tennis elbow radiology
Tennis elbow radiology Darkroom infection control guidelines
Darkroom infection control guidelines Ellis s curve pleural effusion
Ellis s curve pleural effusion Topographic occlusal projection
Topographic occlusal projection Oklahoma state radiology residency
Oklahoma state radiology residency