Safety and Efficacy of the Hypoglossal Nerve Stimulator
- Slides: 1
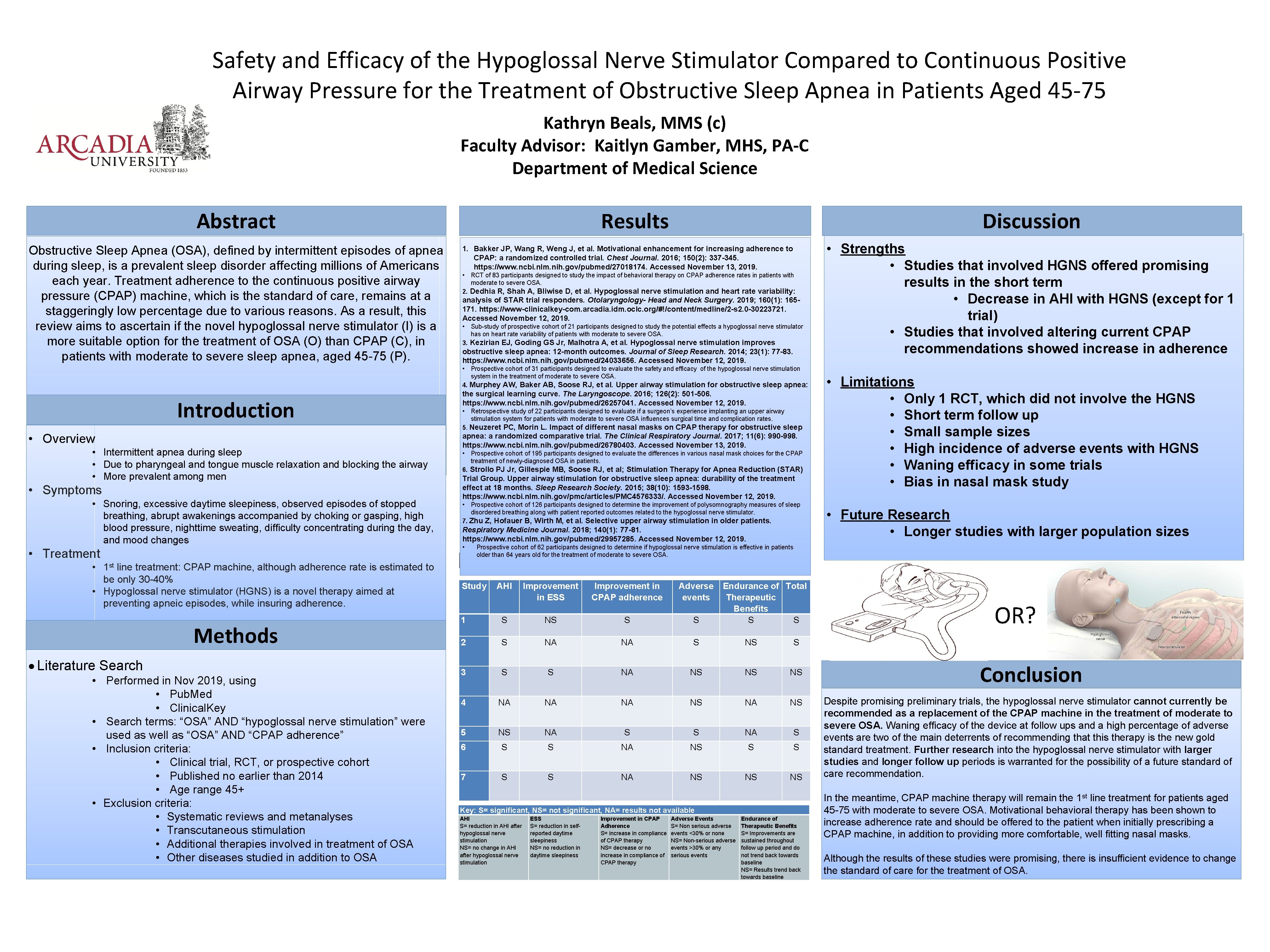
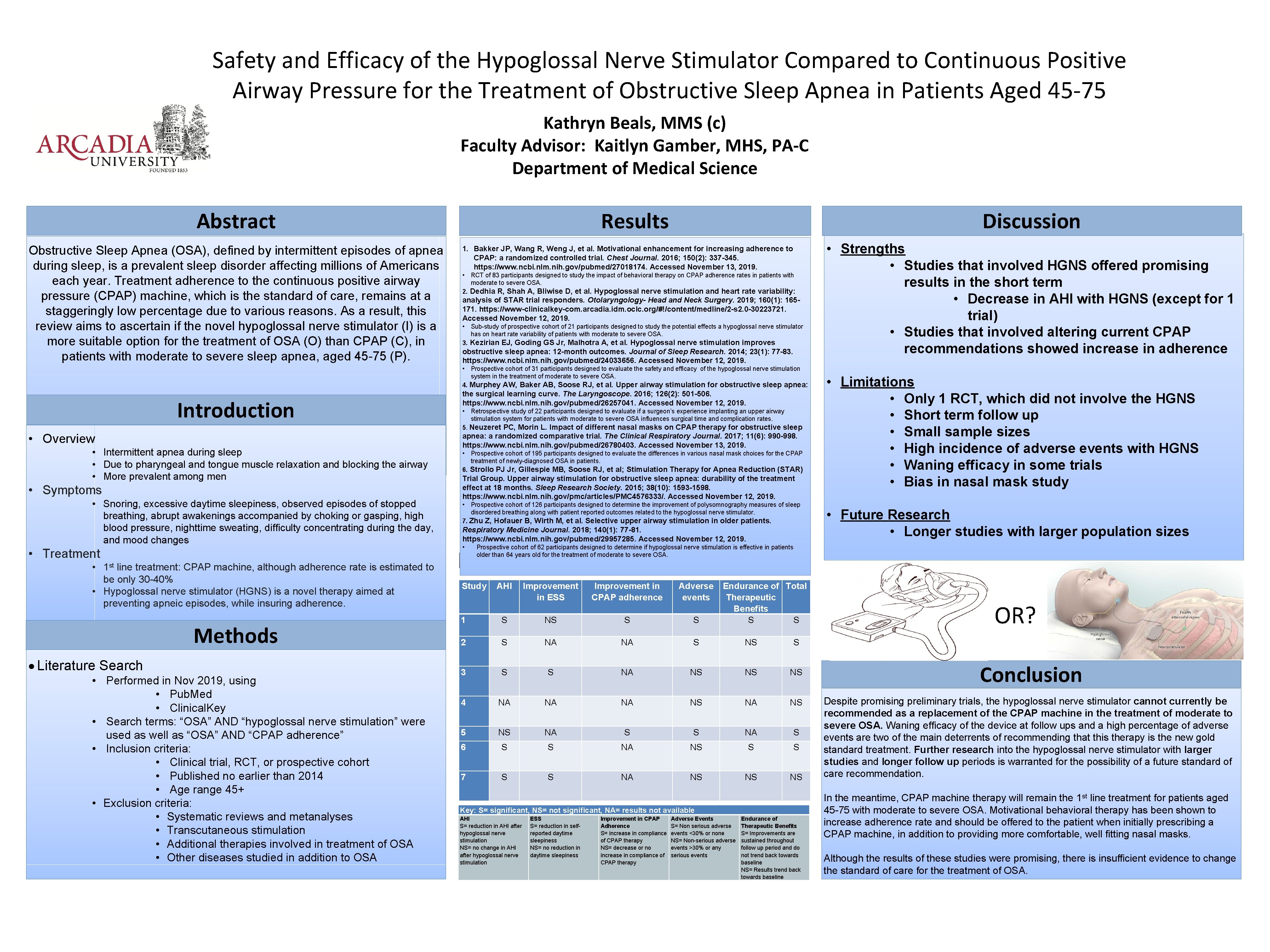
Safety and Efficacy of the Hypoglossal Nerve Stimulator Compared to Continuous Positive Airway Pressure for the Treatment of Obstructive Sleep Apnea in Patients Aged 45 -75 Kathryn Beals, MMS (c) Faculty Advisor: Kaitlyn Gamber, MHS, PA-C Department of Medical Science Abstract Obstructive Sleep Apnea (OSA), defined by intermittent episodes of apnea during sleep, is a prevalent sleep disorder affecting millions of Americans each year. Treatment adherence to the continuous positive airway pressure (CPAP) machine, which is the standard of care, remains at a staggeringly low percentage due to various reasons. As a result, this review aims to ascertain if the novel hypoglossal nerve stimulator (I) is a more suitable option for the treatment of OSA (O) than CPAP (C), in patients with moderate to severe sleep apnea, aged 45 -75 (P). Results Discussion 1. Bakker JP, Wang R, Weng J, et al. Motivational enhancement for increasing adherence to CPAP: a randomized controlled trial. Chest Journal. 2016; 150(2): 337 -345. https: //www. ncbi. nlm. nih. gov/pubmed/27018174. Accessed November 13, 2019. • RCT of 83 participants designed to study the impact of behavioral therapy on CPAP adherence rates in patients with moderate to severe OSA. 2. Dedhia R, Shah A, Bliwise D, et al. Hypoglossal nerve stimulation and heart rate variability: analysis of STAR trial responders. Otolaryngology- Head and Neck Surgery. 2019; 160(1): 165171. https: //www-clinicalkey-com. arcadia. idm. oclc. org/#!/content/medline/2 -s 2. 0 -30223721. Accessed November 12, 2019. • Sub-study of prospective cohort of 21 participants designed to study the potential effects a hypoglossal nerve stimulator has on heart rate variability of patients with moderate to severe OSA. 3. Kezirian EJ, Goding GS Jr, Malhotra A, et al. Hypoglossal nerve stimulation improves obstructive sleep apnea: 12 -month outcomes. Journal of Sleep Research. 2014; 23(1): 77 -83. https: //www. ncbi. nlm. nih. gov/pubmed/24033656. Accessed November 12, 2019. • Prospective cohort of 31 participants designed to evaluate the safety and efficacy of the hypoglossal nerve stimulation system in the treatment of moderate to severe OSA. 4. Murphey AW, Baker AB, Soose RJ, et al. Upper airway stimulation for obstructive sleep apnea: Introduction • Overview • Intermittent apnea during sleep • Due to pharyngeal and tongue muscle relaxation and blocking the airway • More prevalent among men • Symptoms • Snoring, excessive daytime sleepiness, observed episodes of stopped breathing, abrupt awakenings accompanied by choking or gasping, high blood pressure, nighttime sweating, difficulty concentrating during the day, and mood changes • Treatment • 1 st line treatment: CPAP machine, although adherence rate is estimated to be only 30 -40% • Hypoglossal nerve stimulator (HGNS) is a novel therapy aimed at preventing apneic episodes, while insuring adherence. Methods Literature Search • Performed in Nov 2019, using • Pub. Med • Clinical. Key • Search terms: “OSA” AND “hypoglossal nerve stimulation” were used as well as “OSA” AND “CPAP adherence” • Inclusion criteria: • Clinical trial, RCT, or prospective cohort • Published no earlier than 2014 • Age range 45+ • Exclusion criteria: • Systematic reviews and metanalyses • Transcutaneous stimulation • Additional therapies involved in treatment of OSA • Other diseases studied in addition to OSA the surgical learning curve. The Laryngoscope. 2016; 126(2): 501 -506. https: //www. ncbi. nlm. nih. gov/pubmed/26257041. Accessed November 12, 2019. • Retrospective study of 22 participants designed to evaluate if a surgeon’s experience implanting an upper airway stimulation system for patients with moderate to severe OSA influences surgical time and complication rates. 5. Neuzeret PC, Morin L. Impact of different nasal masks on CPAP therapy for obstructive sleep apnea: a randomized comparative trial. The Clinical Respiratory Journal. 2017; 11(6): 990 -998. https: //www. ncbi. nlm. nih. gov/pubmed/26780403. Accessed November 13, 2019. • Prospective cohort of 195 participants designed to evaluate the differences in various nasal mask choices for the CPAP treatment of newly-diagnosed OSA in patients. 6. Strollo PJ Jr, Gillespie MB, Soose RJ, et al; Stimulation Therapy for Apnea Reduction (STAR) Trial Group. Upper airway stimulation for obstructive sleep apnea: durability of the treatment effect at 18 months. Sleep Research Society. 2015; 38(10): 1593 -1598. https: //www. ncbi. nlm. nih. gov/pmc/articles/PMC 4576333/. Accessed November 12, 2019. • Prospective cohort of 126 participants designed to determine the improvement of polysomnography measures of sleep disordered breathing along with patient reported outcomes related to the hypoglossal nerve stimulator. 7. Zhu Z, Hofauer B, Wirth M, et al. Selective upper airway stimulation in older patients. Respiratory Medicine Journal. 2018; 140(1): 77 -81. https: //www. ncbi. nlm. nih. gov/pubmed/29957285. Accessed November 12, 2019. • • Strengths • Studies that involved HGNS offered promising results in the short term • Decrease in AHI with HGNS (except for 1 trial) • Studies that involved altering current CPAP recommendations showed increase in adherence • Limitations • Only 1 RCT, which did not involve the HGNS • Short term follow up • Small sample sizes • High incidence of adverse events with HGNS • Waning efficacy in some trials • Bias in nasal mask study • Future Research • Longer studies with larger population sizes Prospective cohort of 62 participants designed to determine if hypoglossal nerve stimulation is effective in patients older than 64 years old for the treatment of moderate to severe OSA. Table 1. Example Table Study AHI Improvement in ESS Improvement in CPAP adherence Adverse events Endurance of Total Therapeutic Benefits S S 1 S NS S S 2 S NA NA S NS S 3 S S NA NS NS NS 4 NA NA NA NS 5 NS NA S 6 S S NA NS S S 7 S S NA NS NS NS Key: S= significant, NS= not significant, NA= results not available AHI S= reduction in AHI after hypoglossal nerve stimulation NS= no change in AHI after hypoglossal nerve stimulation ESS S= reduction in selfreported daytime sleepiness NS= no reduction in daytime sleepiness Improvement in CPAP Adherence S= increase in compliance of CPAP therapy NS= decrease or no increase in compliance of CPAP therapy Adverse Events S= Non serious adverse events <30% or none NS= Non-serious adverse events >30% or any serious events Endurance of Therapeutic Benefits S= Improvements are sustained throughout follow up period and do not trend back towards baseline NS= Results trend back towards baseline OR? Conclusion Despite promising preliminary trials, the hypoglossal nerve stimulator cannot currently be recommended as a replacement of the CPAP machine in the treatment of moderate to severe OSA. Waning efficacy of the device at follow ups and a high percentage of adverse events are two of the main deterrents of recommending that this therapy is the new gold standard treatment. Further research into the hypoglossal nerve stimulator with larger studies and longer follow up periods is warranted for the possibility of a future standard of care recommendation. In the meantime, CPAP machine therapy will remain the 1 st line treatment for patients aged 45 -75 with moderate to severe OSA. Motivational behavioral therapy has been shown to increase adherence rate and should be offered to the patient when initially prescribing a CPAP machine, in addition to providing more comfortable, well fitting nasal masks. Although the results of these studies were promising, there is insufficient evidence to change the standard of care for the treatment of OSA.