Safe Surgery Checklist Revised for 2013 Shannon Hein
- Slides: 23
Safe Surgery Checklist Revised for 2013 Shannon Hein RN, CPN(C)
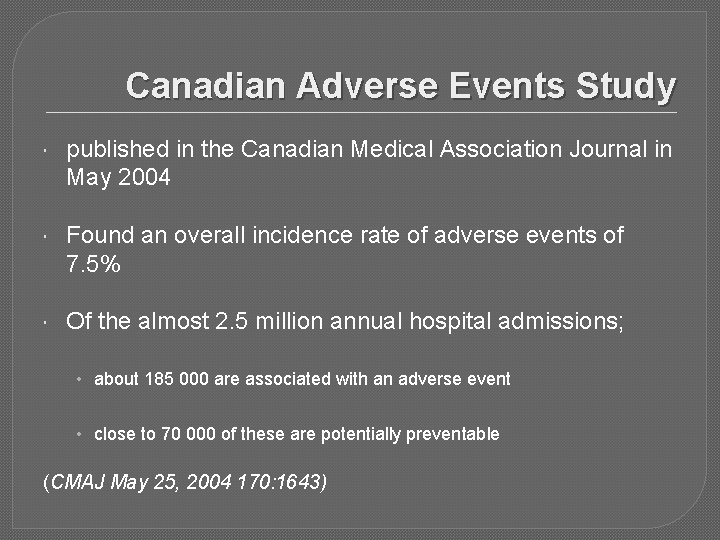
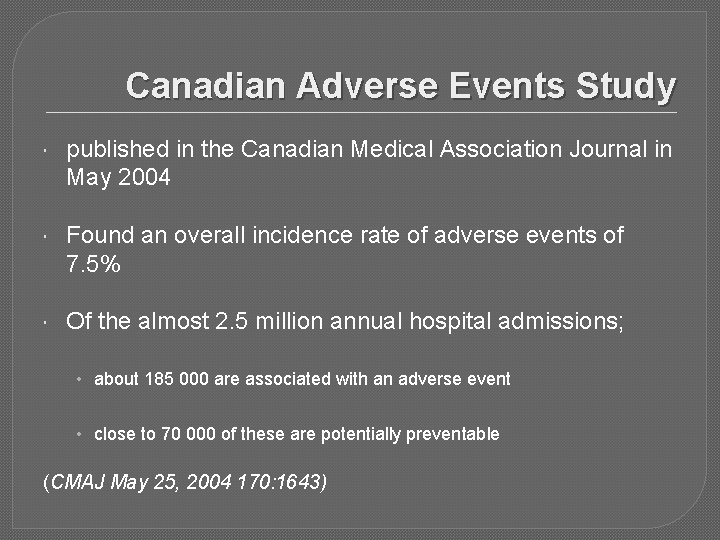
Canadian Adverse Events Study published in the Canadian Medical Association Journal in May 2004 Found an overall incidence rate of adverse events of 7. 5% Of the almost 2. 5 million annual hospital admissions; • about 185 000 are associated with an adverse event • close to 70 000 of these are potentially preventable (CMAJ May 25, 2004 170: 1643)
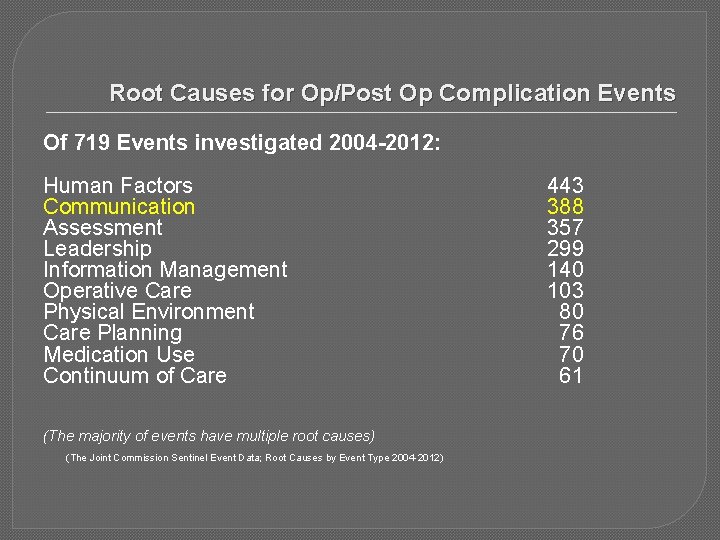
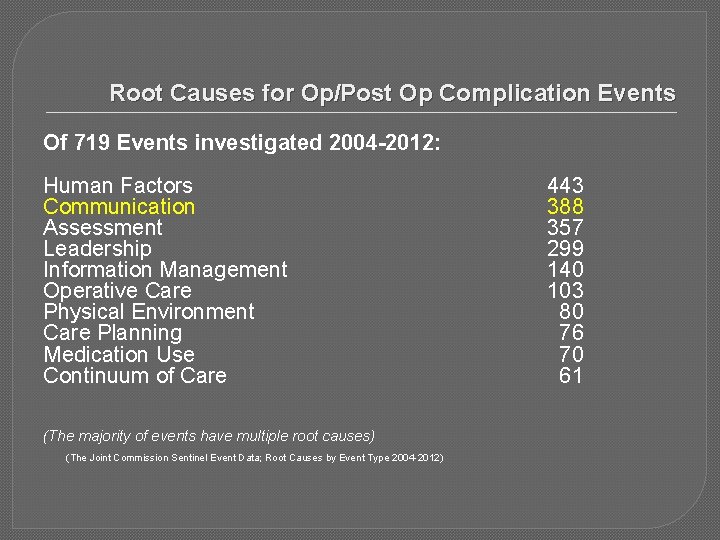
Root Causes for Op/Post Op Complication Events Of 719 Events investigated 2004 -2012: Human Factors Communication Assessment Leadership Information Management Operative Care Physical Environment Care Planning Medication Use Continuum of Care (The majority of events have multiple root causes) (The Joint Commission Sentinel Event Data; Root Causes by Event Type 2004 -2012) 443 388 357 299 140 103 80 76 70 61
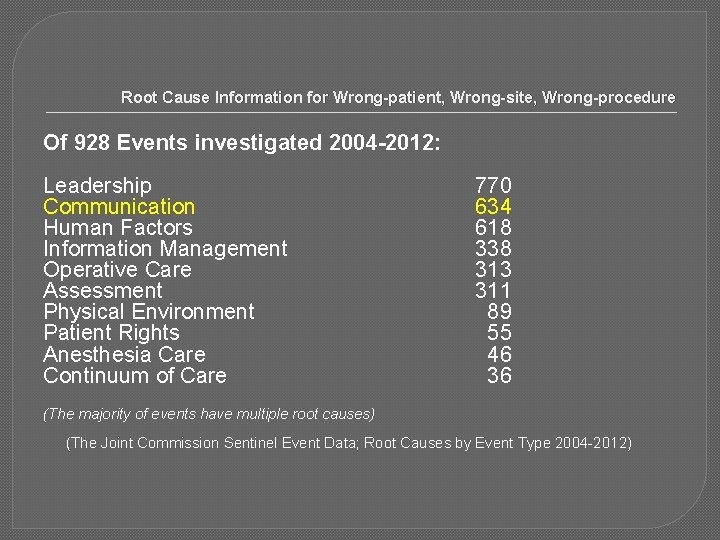
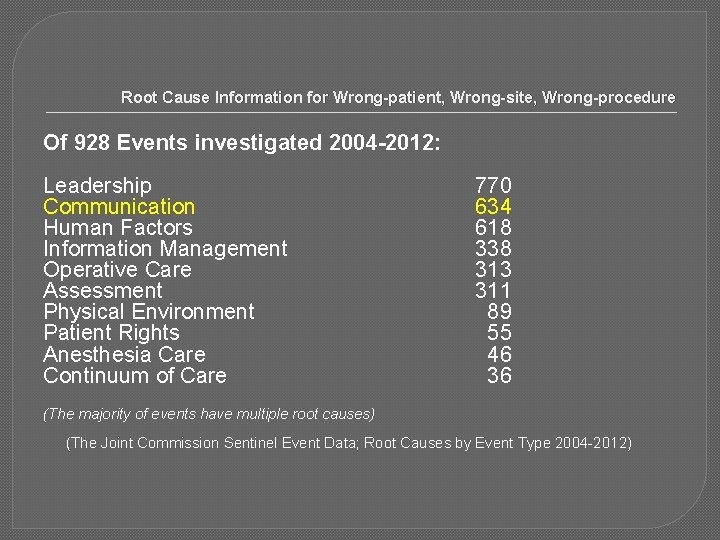
Root Cause Information for Wrong-patient, Wrong-site, Wrong-procedure Of 928 Events investigated 2004 -2012: Leadership Communication Human Factors Information Management Operative Care Assessment Physical Environment Patient Rights Anesthesia Care Continuum of Care 770 634 618 338 313 311 89 55 46 36 (The majority of events have multiple root causes) (The Joint Commission Sentinel Event Data; Root Causes by Event Type 2004 -2012)
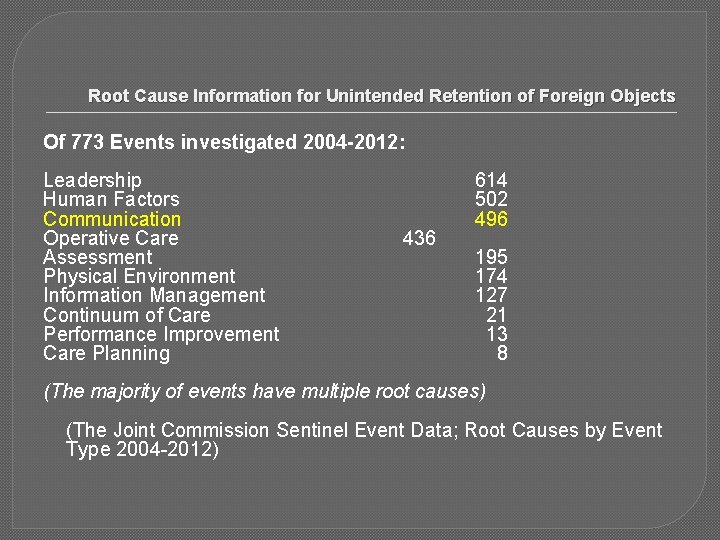
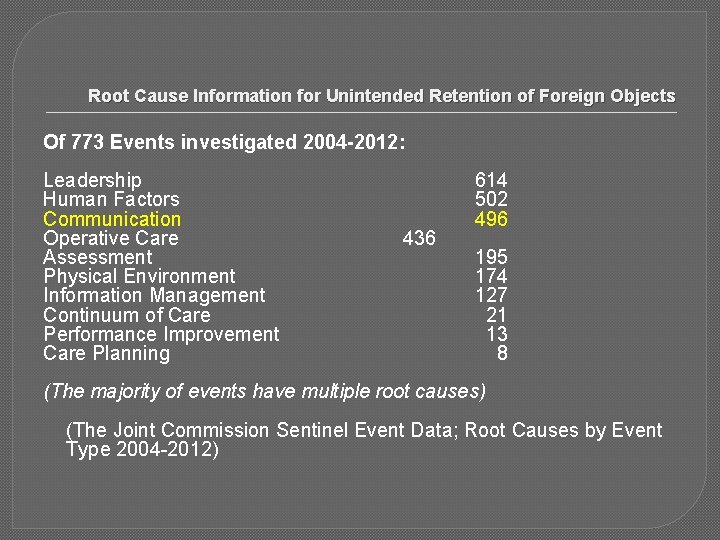
Root Cause Information for Unintended Retention of Foreign Objects Of 773 Events investigated 2004 -2012: Leadership Human Factors Communication Operative Care Assessment Physical Environment Information Management Continuum of Care Performance Improvement Care Planning 436 614 502 496 195 174 127 21 13 8 (The majority of events have multiple root causes) (The Joint Commission Sentinel Event Data; Root Causes by Event Type 2004 -2012)
Safe Surgery Checklist � communication tool intended to be used by clinicians to improve the safety and quality of patient care during surgical procedures � shown to reduce (>30%) the number of preventable complications / mortality associated with surgery by ensuring critical information is shared with all members of the surgical team (NEJM 2009; 360: 491 -499) � Now >3900 hospitals worldwide (122 countries) …more than 90% of the world’s population (WHO)
New England Journal of Medicine Jan. 2009 � “A Surgical Safety Checklist to Reduce Morbidity and Mortality in a Global Population” � Between October 2007 and September 2008, eight hospitals in eight cities collected data on 3733 patients “Pre” Safe Surgery Checklist and 3955 “Post” Safe Surgery Checklist � The rate of death was 0. 9% before the checklist was introduced and declined to 0. 6% afterward (high income sites Toronto, Auckland, London, Seattle) � Inpatient complications occurred in 10. 3% of patients at baseline and in 7. 1% after introduction of the checklist (at high income sites) � Checklist adherence was measured and tight correlations were found between the use of the checklist and achieving these results.
Safe Surgery Checklist Current State A modified version of the WHO Safe Surgery Checklist was introduced to AHS in January 2010 The method of delivery has varied from site to site, with compliance also varying Recognizing that many staff work at multiple sites………. .
The Changes The Safe Surgery Checklist was modified and standardized to ensure that all sites across Alberta are completing the necessary steps After 2013, Safe Surgery Checklist becomes an Accreditation Canada requirement The Covenant Health Safe Surgery Checklist Policy…….
Safe Surgery Checklist Policy � Safe Surgery Checklist Required for all surgical interventions � All steps must be completed by the appropriate people � Required � If to be documented on patient’s health record Briefing is not completed, the case does not proceed � Surgeon and Anesthesiologist: must be staff or Fellow
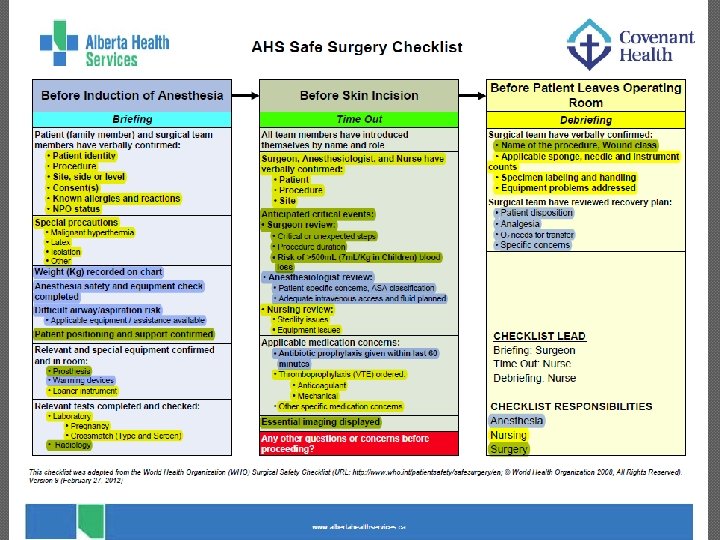
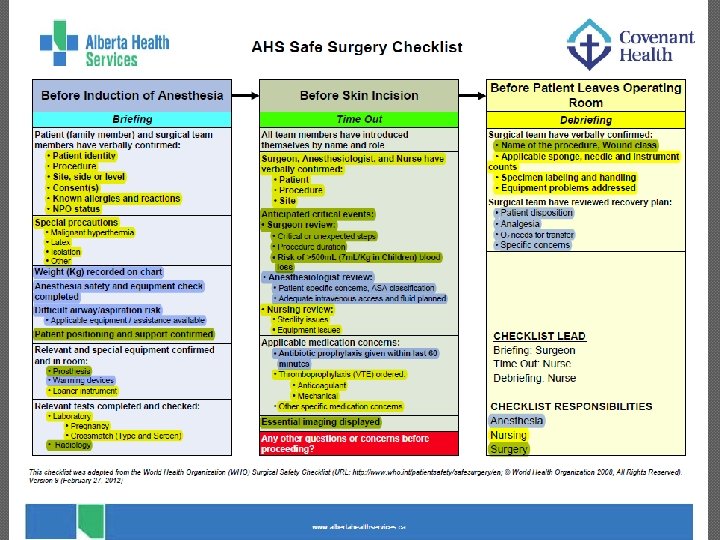
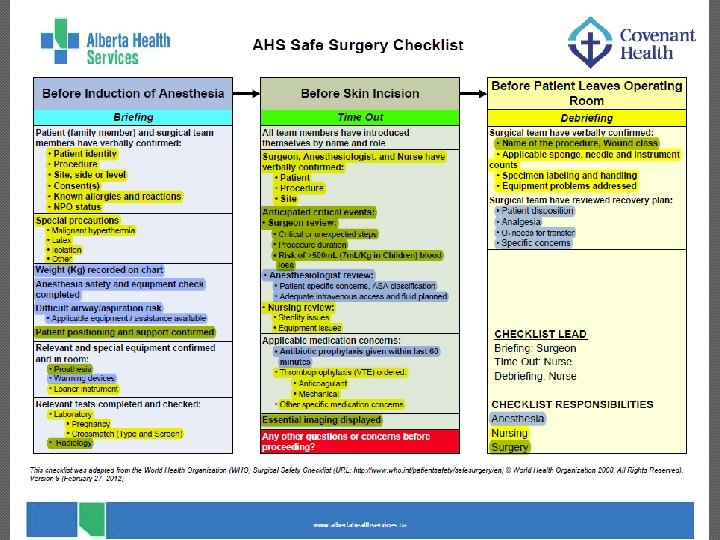
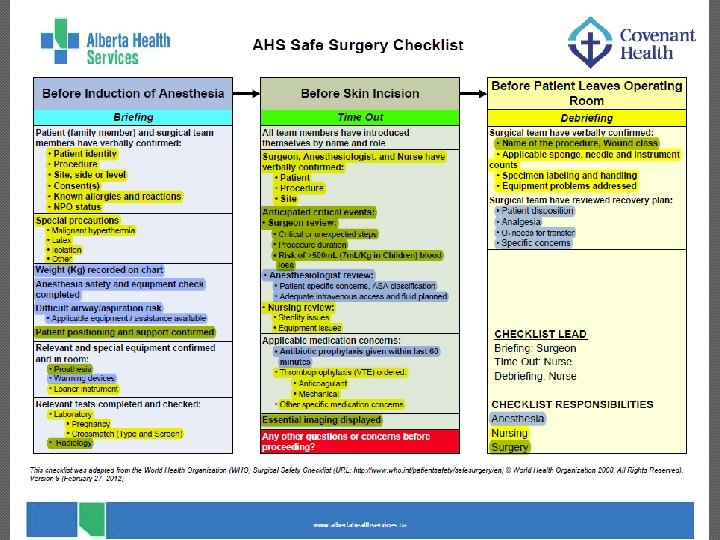
Checklist Lead The Checklist Lead ensures the completion of each section of the Checklist. All steps in each section must be complete before proceeding Briefing: Surgeon Time Out: Nurse Debriefing: Nurse
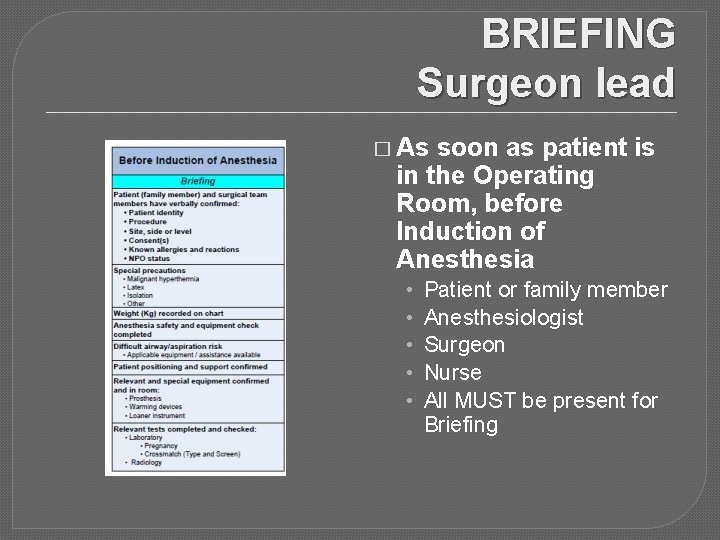
BRIEFING Surgeon lead � As soon as patient is in the Operating Room, before Induction of Anesthesia • • • Patient or family member Anesthesiologist Surgeon Nurse All MUST be present for Briefing
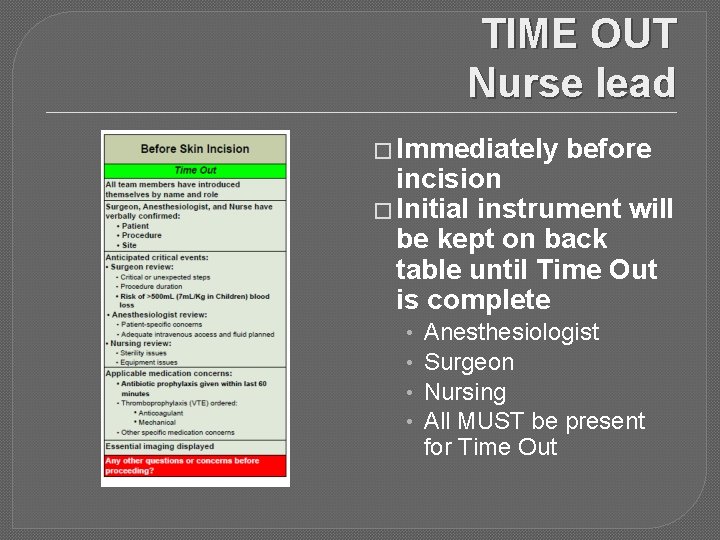
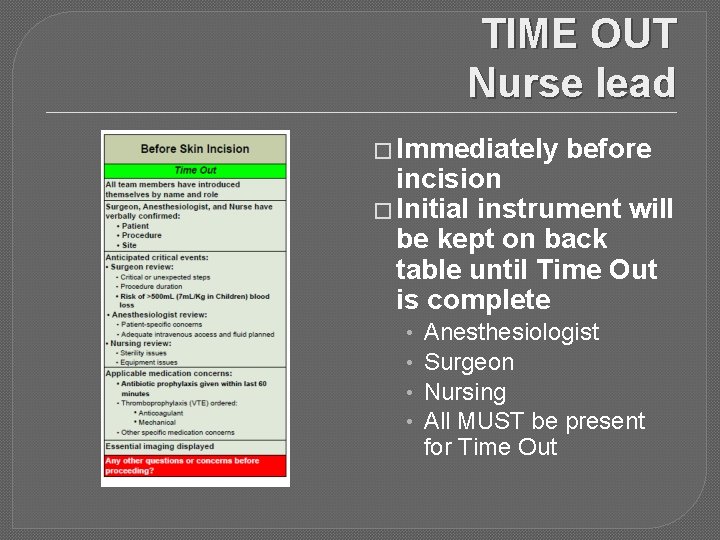
TIME OUT Nurse lead � Immediately before incision � Initial instrument will be kept on back table until Time Out is complete • • Anesthesiologist Surgeon Nursing All MUST be present for Time Out
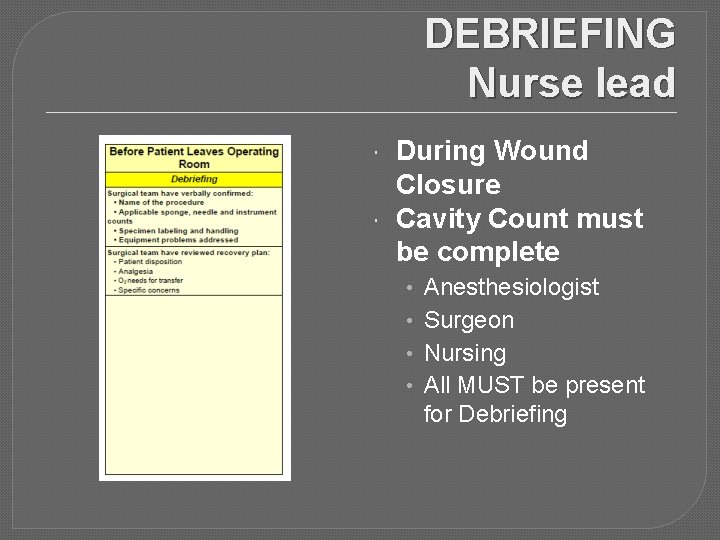
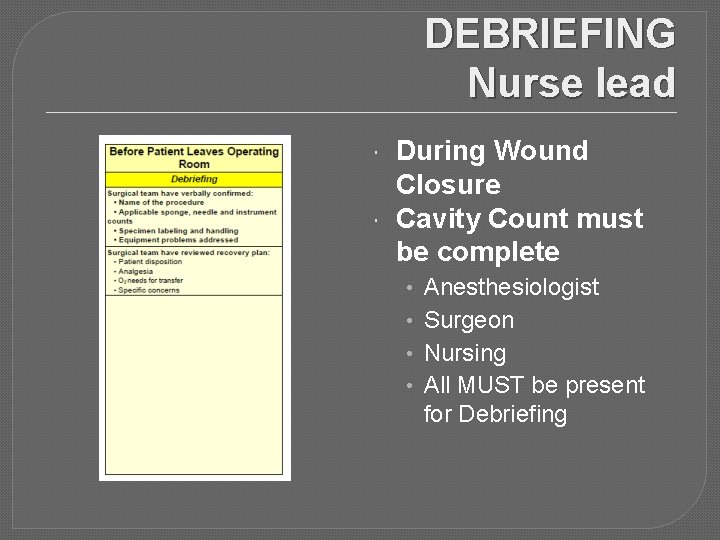
DEBRIEFING Nurse lead During Wound Closure Cavity Count must be complete • • Anesthesiologist Surgeon Nursing All MUST be present for Debriefing
Charting Safe Surgery Checklist will be part of the chart Each section (Briefing, Time Out and Debriefing) will be represented The Checklist Lead ensures these sections are complete Each section is then signed off on the chart
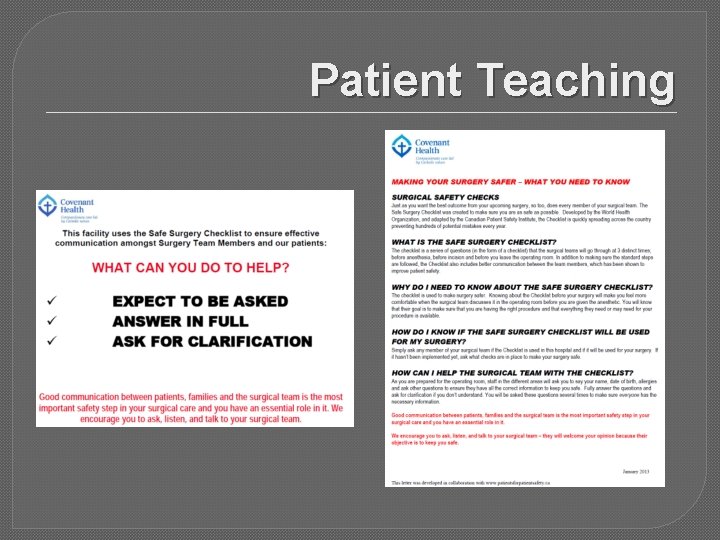
Patient Teaching
FAQ Where is it done? All three sections will be done in the Operating Room. In the event that a patient has an interpreter or cannot represent themselves, the Briefing will take place in the Pre Operative Holding area. Why the changes? To ensure that all hospitals across Alberta are doing the same standardized Checklist. Is this going to slow things down? In the beginning, this may have its growing pains. But, it has actually been proven to save time in many situations
FAQ Can a Resident do the Checklist in place of the Physician? No. The AHS and Covenant Health policies require the Surgeon and Anesthesiologist to be either Staff or Clinical Fellow. Is this for all surgeries? Yes What are the other hospitals doing? All hospitals in Alberta are doing the Safe Surgery Checklist and are required to meet all of the steps and criteria. Is this part of the patient chart? Yes
FAQ Does the Checklist have to be done in an Emergency situation? The Most Responsible Health Practitioner will use discretion in determining which sections of the Checklist will be completed. Documentation of this will go in the patient’s Health Record. What if the patient is undergoing multiple procedures? The Surgeon or alternative surgeon, Anesthesiologist or alternative anesthesiologist and nurse must be present for Briefing and Time Out for each distinct procedure. Upon completion of all procedures, the most responsible surgeon, the anesthesiologist and nurse must ALL be present for debriefing.
FAQ What if the patient needs an interpreter or cannot represent themselves, how do we do the Briefing section? If an interpreter or representative/family member is present, complete the Briefing section in the Pre Operative Holding Area with Circulating Nurse, Anesthesia, and Surgeon present.
References � The Canadian Adverse Events Study Baker GR, Norton P, Flintoft V, et al. The Canadian adverse events study: the incidence of adverse events among hospital patients in Canada. CMAJ. 2004; 170 (11): 1678 - 1686. � Impact of using the checklist at the eight WHO pilot sites Haynes AB, Weiser TG, Berry WB, et al. A surgical safety checklist to reduce morbidity and mortality in a global population. New England Journal of Medicine. 2009 Jan 14; [Epub ahead of print]. � The Joint Commission Sentinel Event Data; Root Causes by Event Type 2004 -2012 � Alberta Health Services Safe Surgery Checklist Provincial Measurement Strategy September 17, 2012