Safe Script Training Acknowledgement of country I would














- Slides: 71

Safe. Script Training

Acknowledgement of country I would like to acknowledge the traditional custodians of this land. I would also like to pay my respect to their Elders, past, present and emerging and extend that respect to other Aboriginal people present today. Facilitators
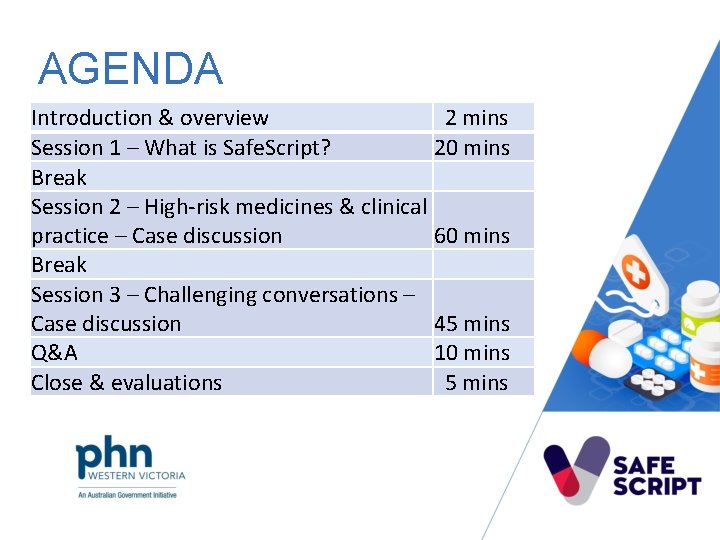
AGENDA Introduction & overview 2 mins Session 1 – What is Safe. Script? 20 mins Break Session 2 – High-risk medicines & clinical practice – Case discussion 60 mins Break Session 3 – Challenging conversations – Case discussion 45 mins Q&A 10 mins Close & evaluations 5 mins
OVERVIEW Safe. Script is a real-time prescription monitoring system that enables prescription records for certain monitored medicines to be stored centrally & accessed by prescribers & pharmacists during a consultation to aid clinical decision making.

SESSION 1 ABOUT SAFESCRIPT Handouts in the satchels References & resources on Safe. Script Hub Slides in satchel & on Hub Case study in satchel
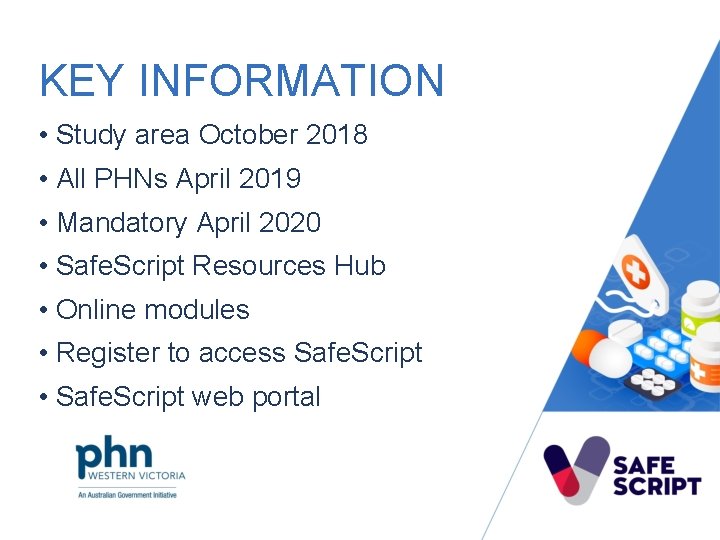
KEY INFORMATION • Study area October 2018 • All PHNs April 2019 • Mandatory April 2020 • Safe. Script Resources Hub • Online modules • Register to access Safe. Script • Safe. Script web portal
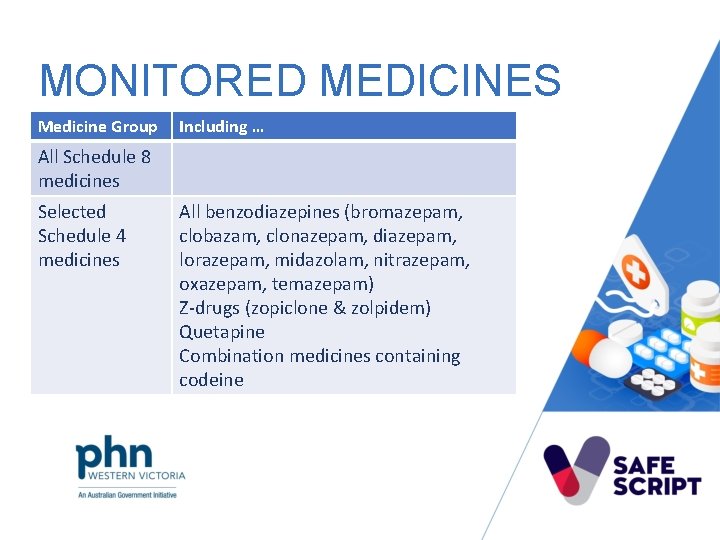
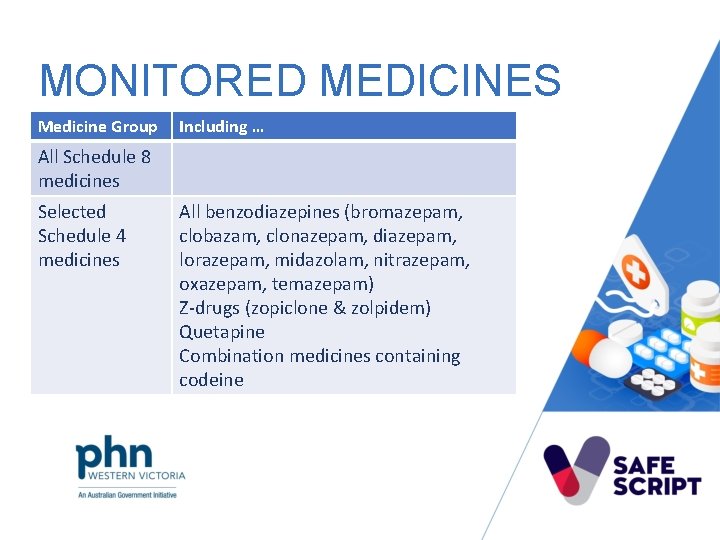
MONITORED MEDICINES Medicine Group Including … All Schedule 8 medicines Selected Schedule 4 medicines All benzodiazepines (bromazepam, clobazam, clonazepam, diazepam, lorazepam, midazolam, nitrazepam, oxazepam, temazepam) Z-drugs (zopiclone & zolpidem) Quetapine Combination medicines containing codeine
WHAT IT MEANS FOR YOU Clinical support tool • Additional clinical information • Does not replace clinical judgement
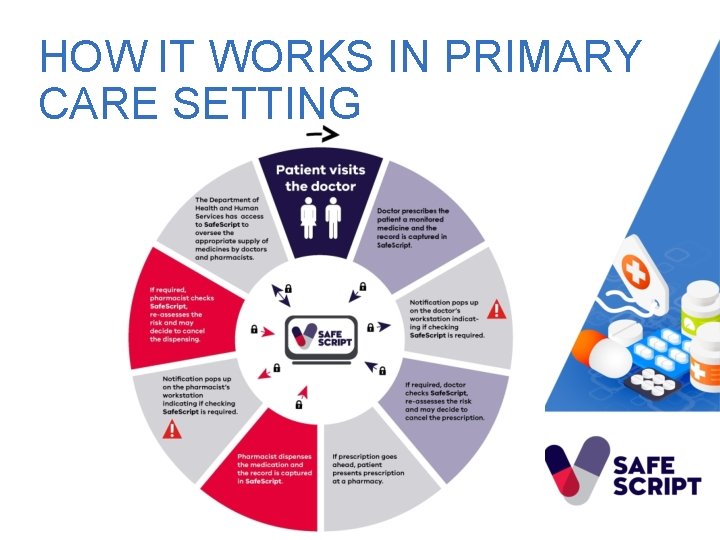
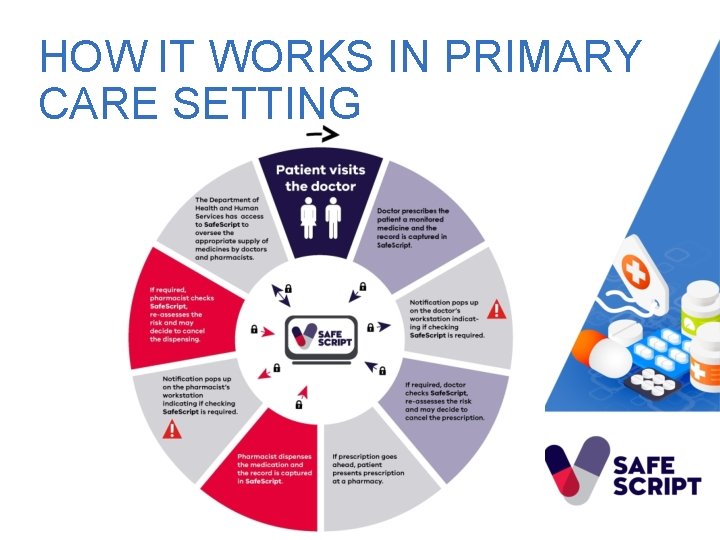
HOW IT WORKS IN PRIMARY CARE SETTING
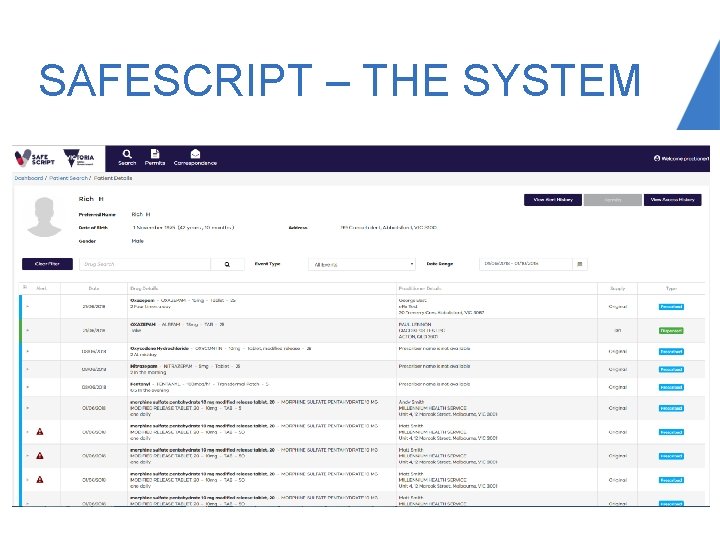
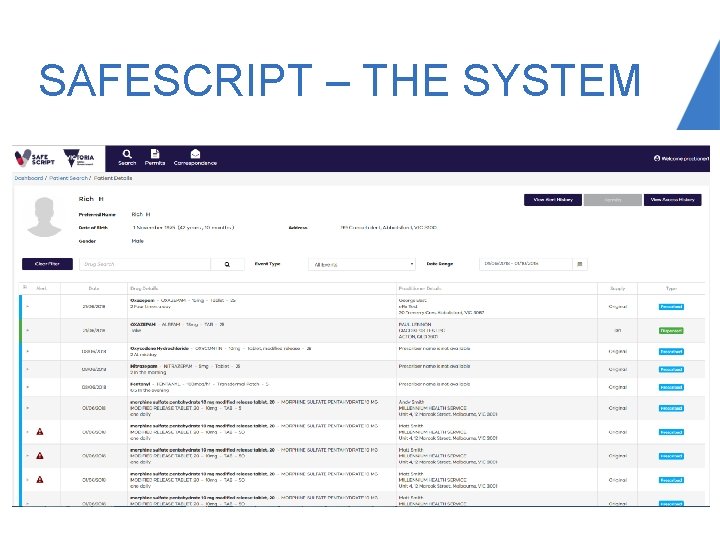
SAFESCRIPT – THE SYSTEM
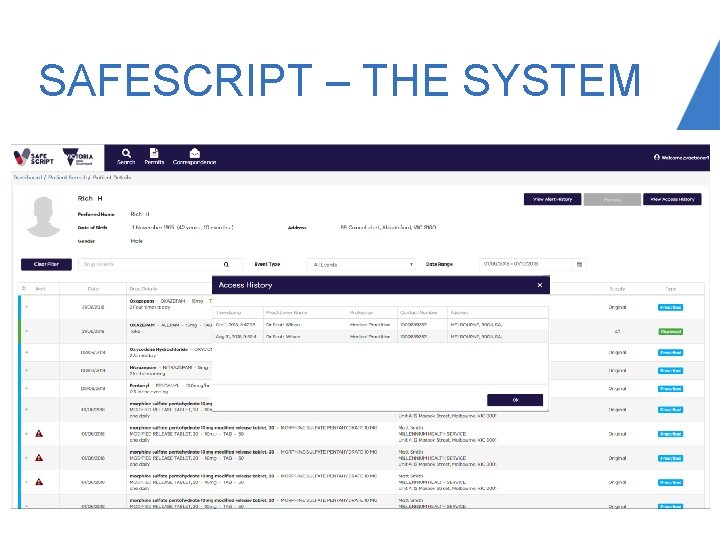
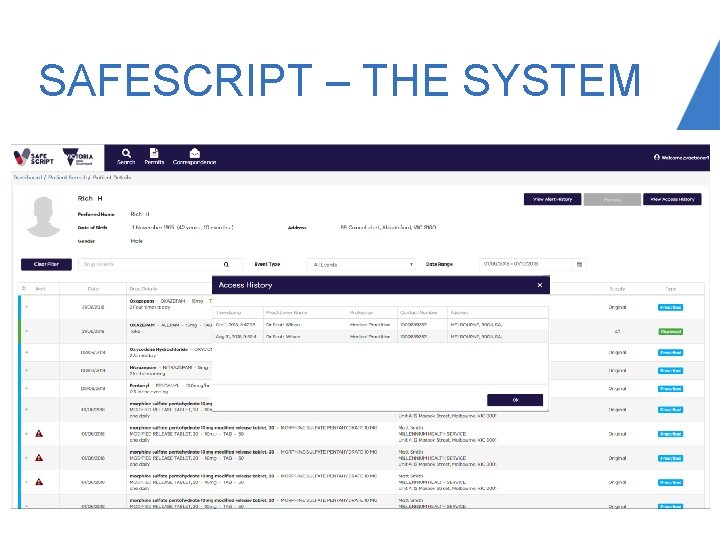
SAFESCRIPT – THE SYSTEM
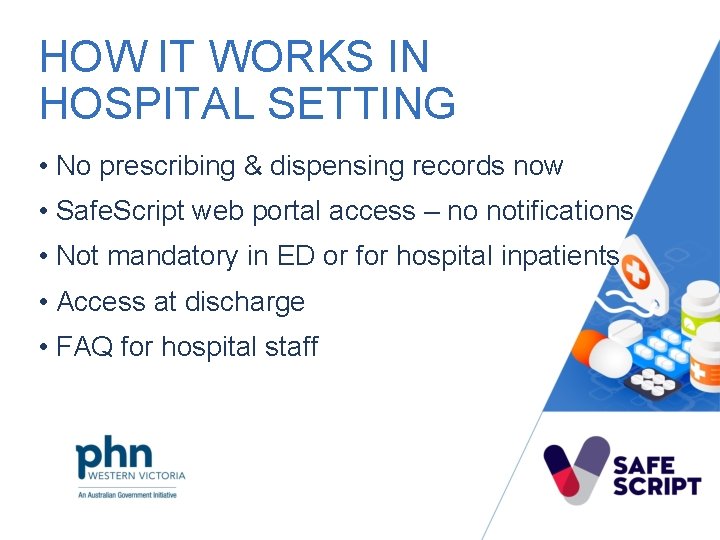
HOW IT WORKS IN HOSPITAL SETTING • No prescribing & dispensing records now • Safe. Script web portal access – no notifications • Not mandatory in ED or for hospital inpatients • Access at discharge • FAQ for hospital staff
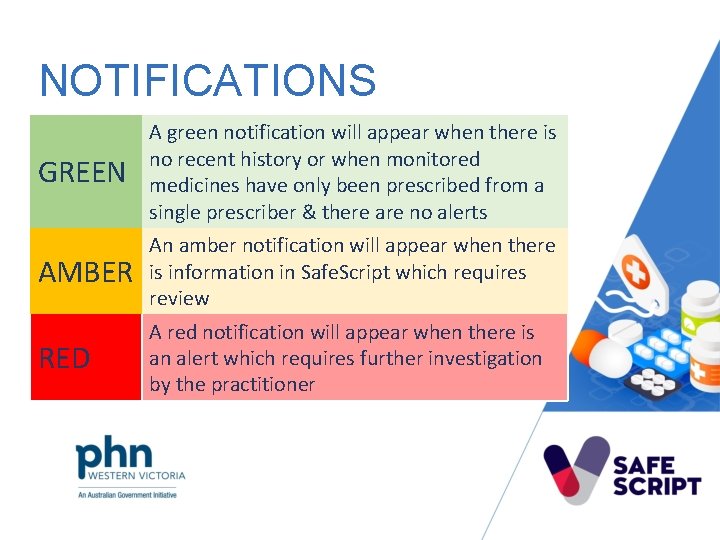
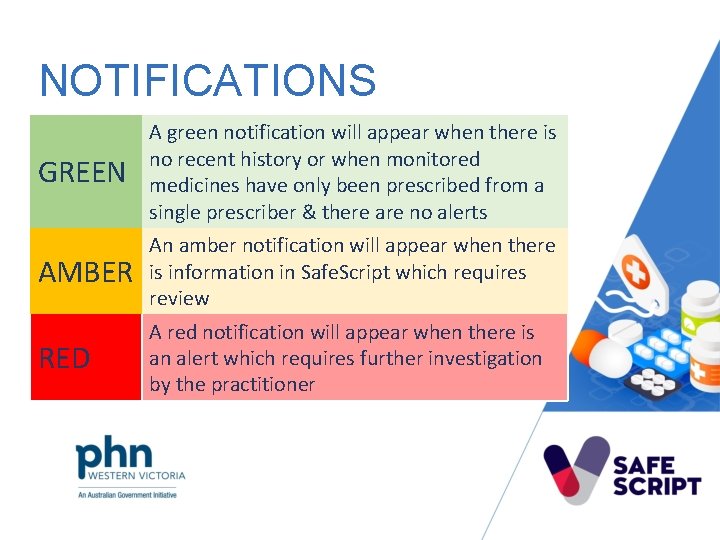
NOTIFICATIONS GREEN A green notification will appear when there is no recent history or when monitored medicines have only been prescribed from a single prescriber & there are no alerts AMBER An amber notification will appear when there is information in Safe. Script which requires review RED A red notification will appear when there is an alert which requires further investigation by the practitioner
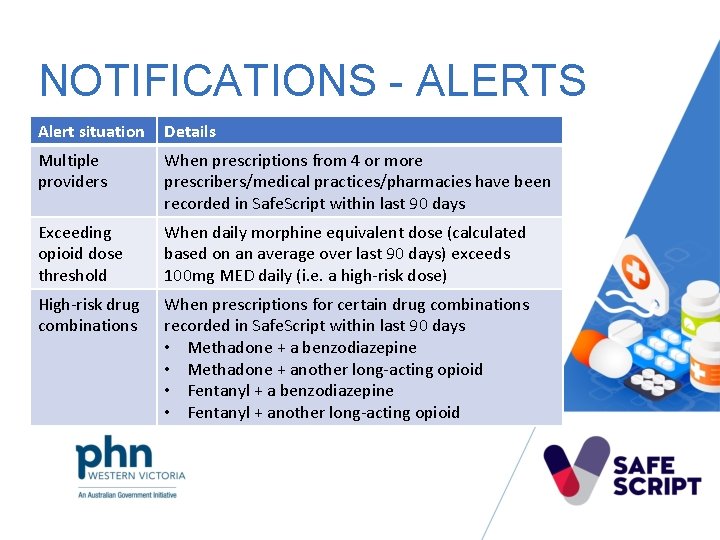
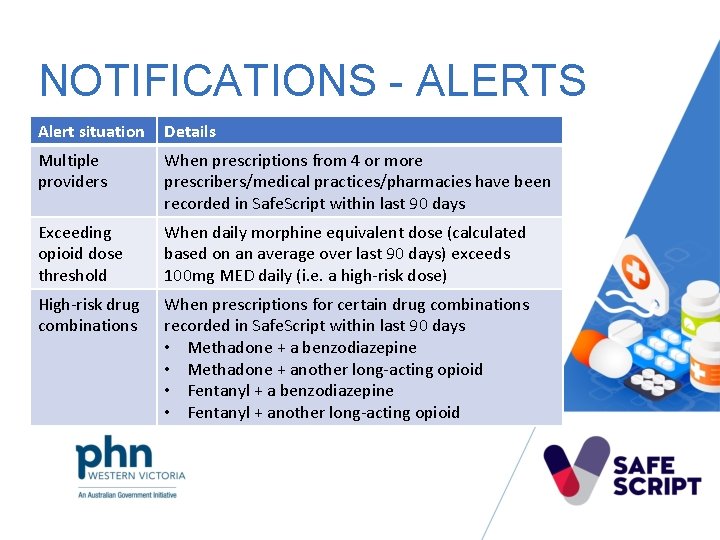
NOTIFICATIONS - ALERTS Alert situation Details Multiple providers When prescriptions from 4 or more prescribers/medical practices/pharmacies have been recorded in Safe. Script within last 90 days Exceeding opioid dose threshold When daily morphine equivalent dose (calculated based on an average over last 90 days) exceeds 100 mg MED daily (i. e. a high-risk dose) High-risk drug combinations When prescriptions for certain drug combinations recorded in Safe. Script within last 90 days • Methadone + a benzodiazepine • Methadone + another long-acting opioid • Fentanyl + a benzodiazepine • Fentanyl + another long-acting opioid
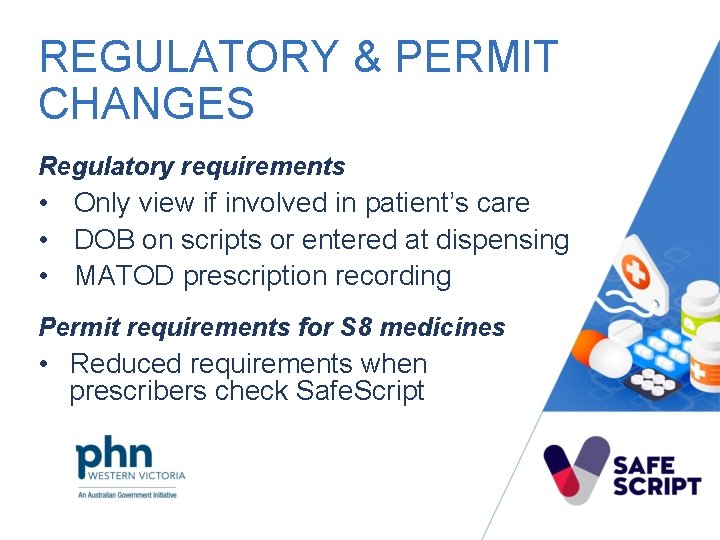
REGULATORY & PERMIT CHANGES Regulatory requirements • Only view if involved in patient’s care • DOB on scripts or entered at dispensing • MATOD prescription recording Permit requirements for S 8 medicines • Reduced requirements when prescribers check Safe. Script
PATIENTS • Only access & disclose information when appropriate • Keep login details confidential • Counsel patients in private • Advise patients to correct data where captured What it means for patients • Patient anxiety • Be respectful • Safety is the focus

BREAK 2 mins
UNDERTAKING CLINICAL ASSESSMENT • Full medicine & illicit drug history • Risk screening • Physical examination
SAFE & APPROPRIATE PRESCRIBING Review patient medicine history • Review all information available (dispensing, prescribing, Safe. Script) • Confirm diagnosis • Drug inxs, disease inxs, contraindications, pregnancy, breastfeeding • Ensure therapeutic need • Non pharmacological approaches • Non high-risk medicines • Supply interval
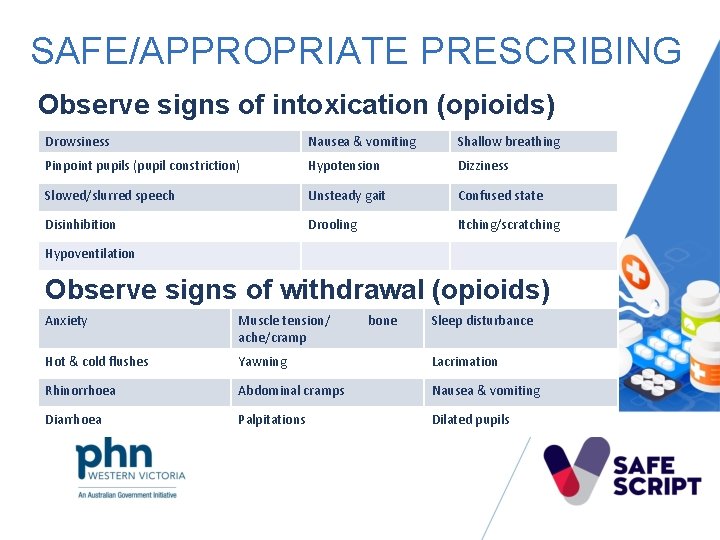
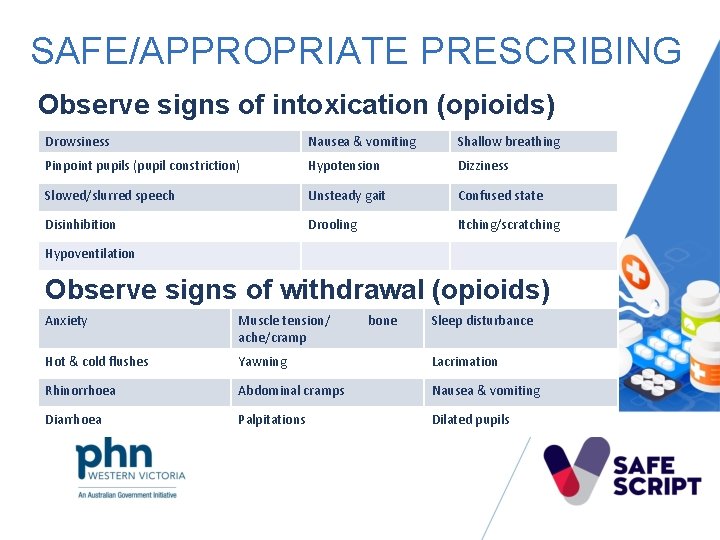
SAFE/APPROPRIATE PRESCRIBING Observe signs of intoxication (opioids) Drowsiness Nausea & vomiting Shallow breathing Pinpoint pupils (pupil constriction) Hypotension Dizziness Disinhibition Drooling Itching/scratching • Slowed/slurred Drowsiness Nausea & vomiting speech Unsteady gait Confused state Hypoventilation Observe signs of withdrawal (opioids) Anxiety Muscle tension/ ache/cramp bone Sleep disturbance Hot & cold flushes Yawning Lacrimation Rhinorrhoea Abdominal cramps Nausea & vomiting Diarrhoea Palpitations Dilated pupils
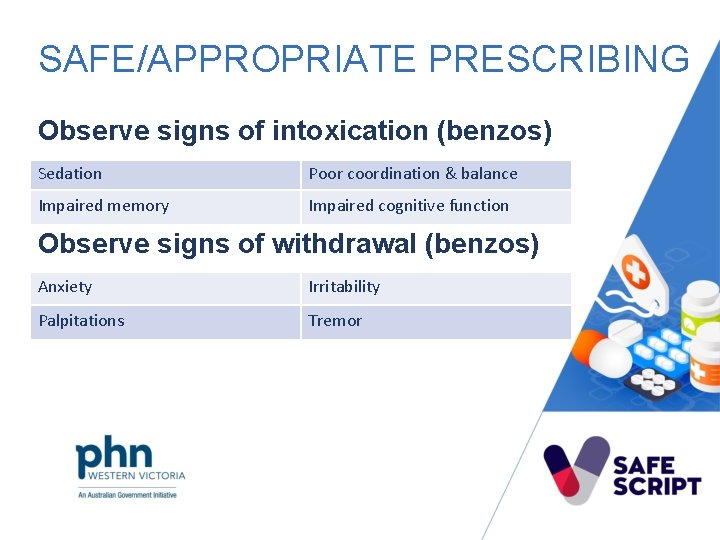
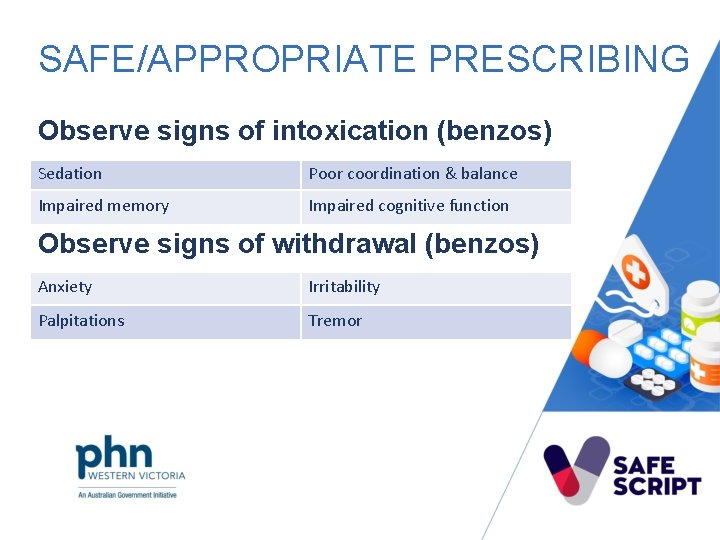
SAFE/APPROPRIATE PRESCRIBING Observe signs of intoxication (benzos) Sedation Poor coordination & balance Impaired memory Impaired cognitive function Observe signs of withdrawal (benzos) Anxiety Irritability Palpitations Tremor
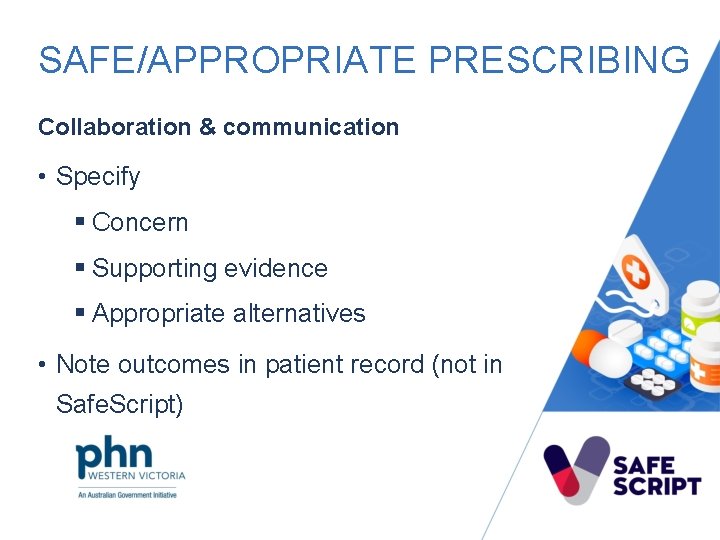
SAFE/APPROPRIATE PRESCRIBING Collaboration & communication • Specify § Concern § Supporting evidence § Appropriate alternatives • Note outcomes in patient record (not in Safe. Script)
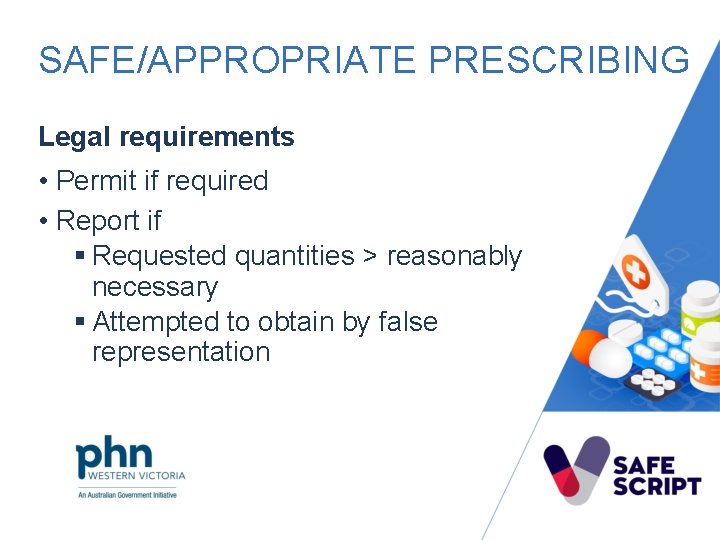
SAFE/APPROPRIATE PRESCRIBING Legal requirements • Permit if required • Report if § Requested quantities > reasonably necessary § Attempted to obtain by false representation
SAFE/APPROPRIATE PRESCRIBING Counsel patient • Specific requirements for the medicine • Applicable warnings • Risk of dependence • Guidance about storage & disposal • Naloxone
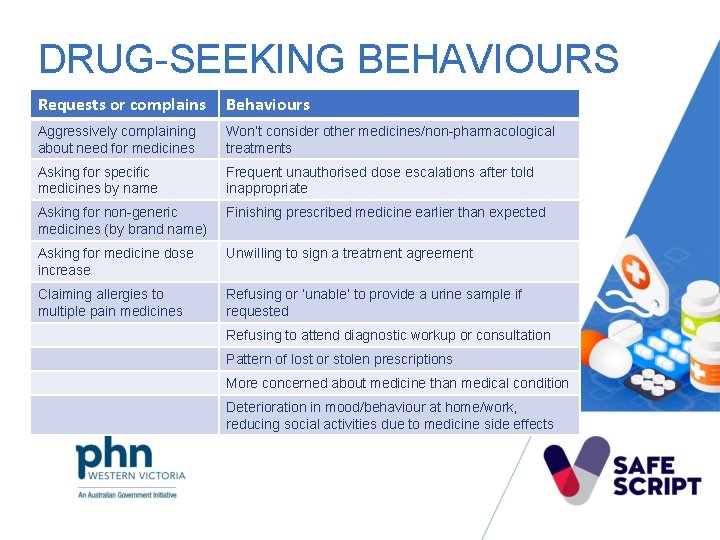
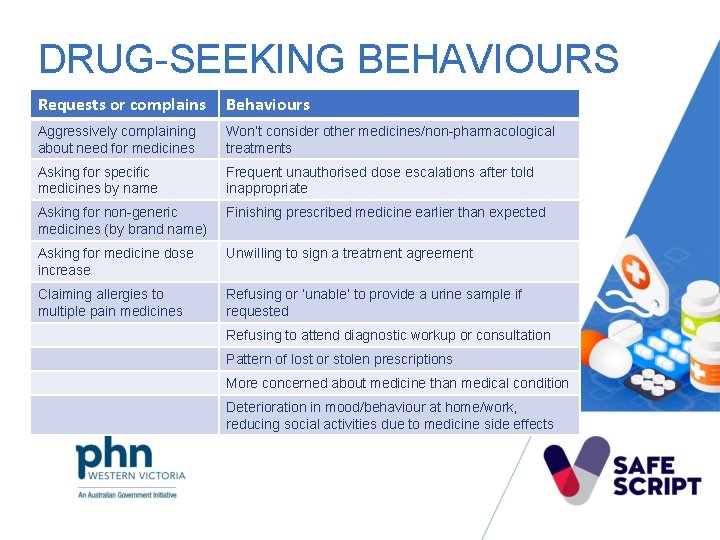
DRUG-SEEKING BEHAVIOURS Requests or complains Behaviours Aggressively complaining about need for medicines Won’t consider other medicines/non-pharmacological treatments Asking for specific medicines by name Frequent unauthorised dose escalations after told inappropriate Asking for non-generic medicines (by brand name) Finishing prescribed medicine earlier than expected Asking for medicine dose increase Unwilling to sign a treatment agreement Claiming allergies to multiple pain medicines Refusing or ‘unable’ to provide a urine sample if requested Refusing to attend diagnostic workup or consultation Pattern of lost or stolen prescriptions More concerned about medicine than medical condition Deterioration in mood/behaviour at home/work, reducing social activities due to medicine side effects
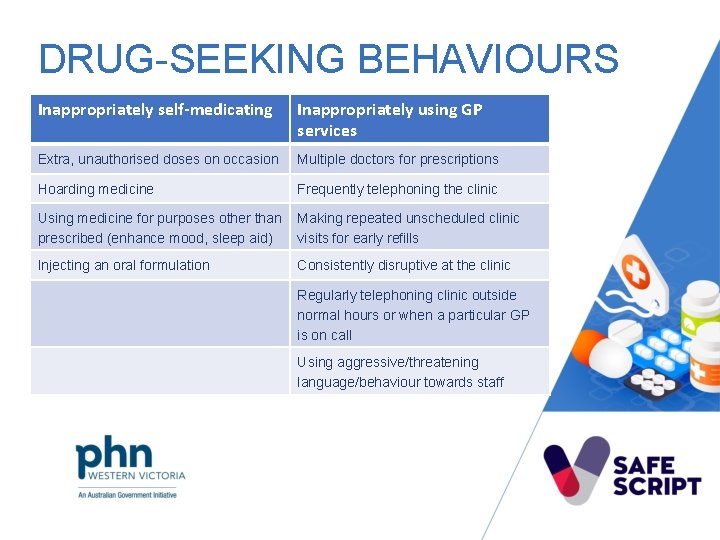
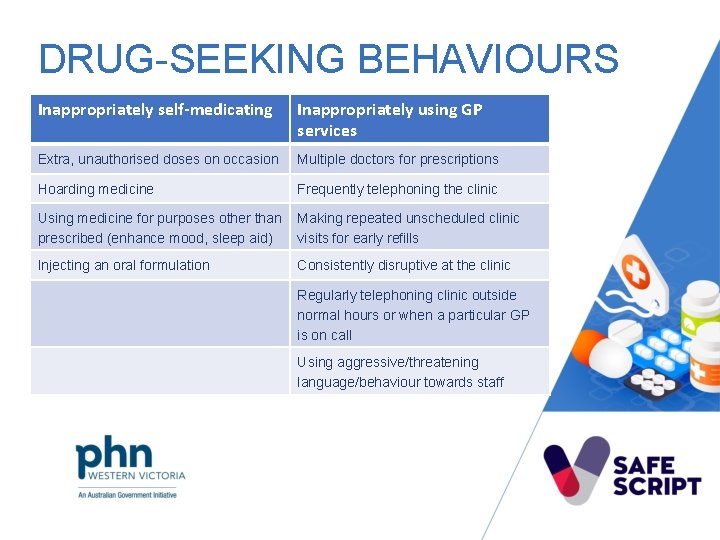
DRUG-SEEKING BEHAVIOURS Inappropriately self-medicating Inappropriately using GP services Extra, unauthorised doses on occasion Multiple doctors for prescriptions Hoarding medicine Frequently telephoning the clinic Using medicine for purposes other than Making repeated unscheduled clinic prescribed (enhance mood, sleep aid) visits for early refills Injecting an oral formulation Consistently disruptive at the clinic Regularly telephoning clinic outside normal hours or when a particular GP is on call Using aggressive/threatening language/behaviour towards staff
HIGH RISK/DEPENDENCE SIGNS • Higher doses than recommended • Length of time • Increase in dose • Withdrawal symptoms
CONSIDER OPTIONS • Help patient recognise the issue • Work with patient to set goals for recovery • Help patient seek appropriate treatment • Consider evidence-based nonpharmacological options • Consider use of other, lower-risk medicines
SAFE & APPROPRIATE PRESCRIBING If supplying • Lowest effective dose for shortest possible time • Regular monitoring • Provide patient information • Consider treatment agreement

STRATEGIES TO MINIMISE PRESCRIBING RISKS & HARMS • One-prescriber, one-practice, one-pharmacy • Smaller quantities • Staged supply • Take-home naloxone • Tapering/discontinuation • Alternatives to high risk medicines • MATOD
NALOXONE
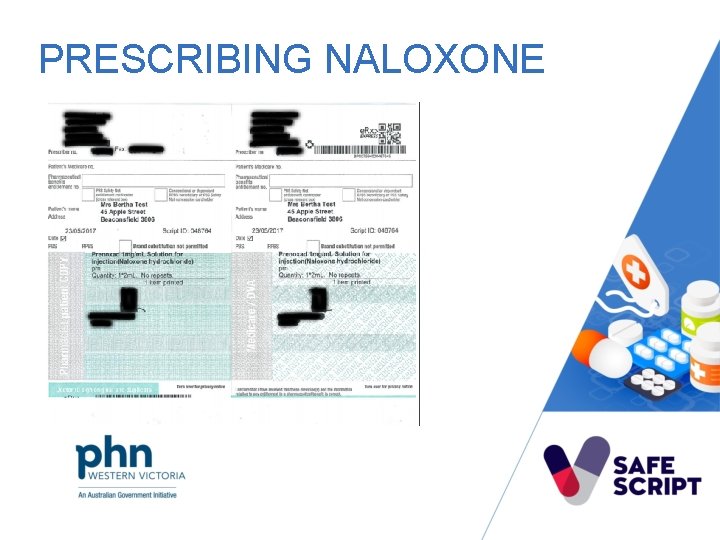
PRESCRIBING NALOXONE
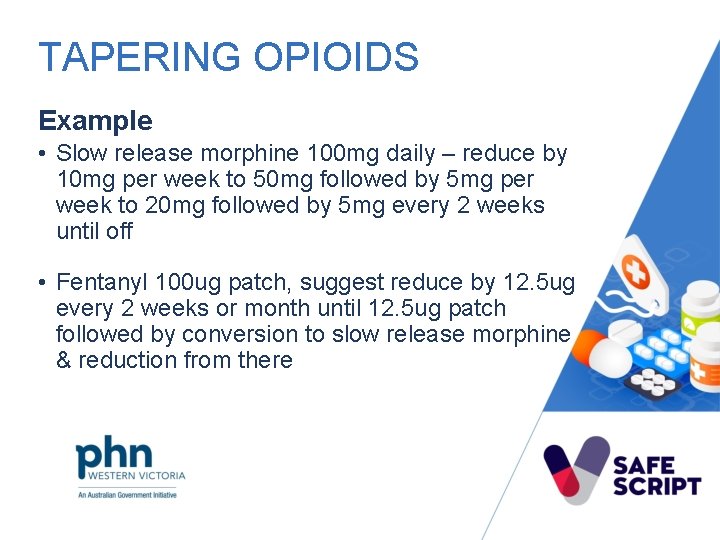
TAPERING OPIOIDS • Controlled release morphine or other long acting opioid • Scheduled doses • Rate can vary § 10% every 2 – 4 weeks • Hold dose if severe withdrawal symptoms • Maintenance dose maybe required
TAPERING OPIOIDS Example • Slow release morphine 100 mg daily – reduce by 10 mg per week to 50 mg followed by 5 mg per week to 20 mg followed by 5 mg every 2 weeks until off • Fentanyl 100 ug patch, suggest reduce by 12. 5 ug every 2 weeks or month until 12. 5 ug patch followed by conversion to slow release morphine & reduction from there

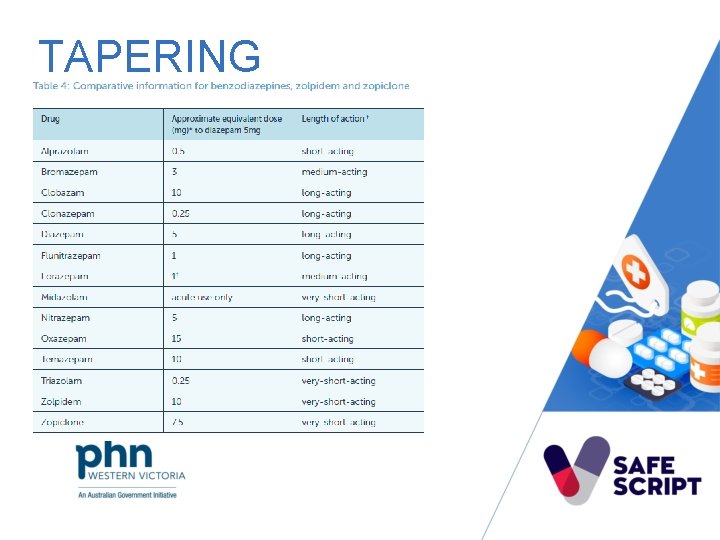
TAPERING
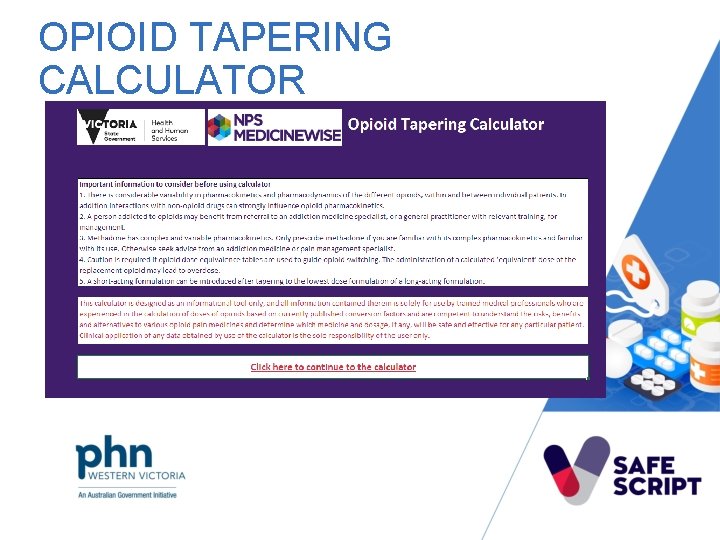
OPIOID TAPERING CALCULATOR
TAPERING BENZODIAZEPINES • Taper 15% of starting dose per week • Titrate against symptoms • Stabilisation of equivalent diazepam before reduction
RECONNEXION BENZODIAZEPINE TOOLKIT
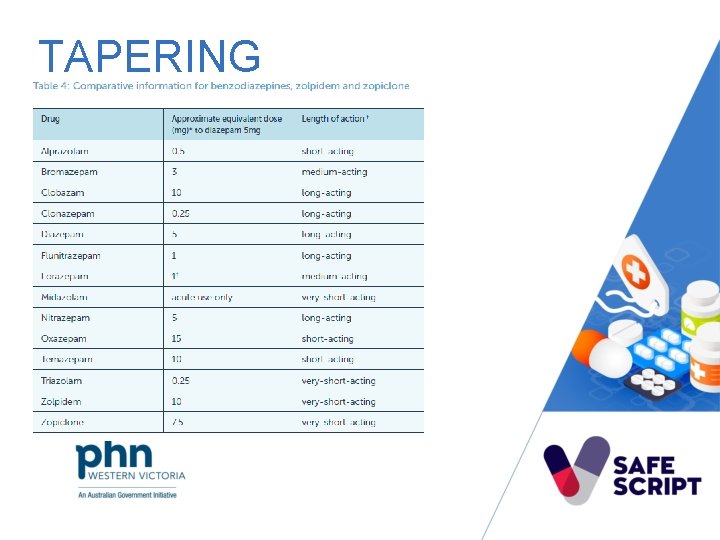
TAPERING
TAPERING QUETIAPINE • Taper if taking for >3 months • Dose reduction of 25%-50% every 1 -2 weeks • Cease after 2 weeks on minimum dose • Slower withdrawal maybe required if prescribed for longer durations

ALTERNATIVES TO HIGH-RISK MEDICINES Link to Brainman video
ALTERNATIVES TO HIGH-RISK MEDICINES • Heat or cold • Referral to other health practitioners • Relaxation techniques • De-sensitisation • Distraction • Aids & appliances • Review of lifestyle factors
ALTERNATIVES - PHARMACOLOGICAL • Simple analgesics § Individually or in combination • Complementary medicines • Analgesic adjuvants

ALTERNATIVES - PACING Link to video on pacing

PAIN MANAGEMENT PLANS
BETTER PAIN MANAGEMENT Link to video
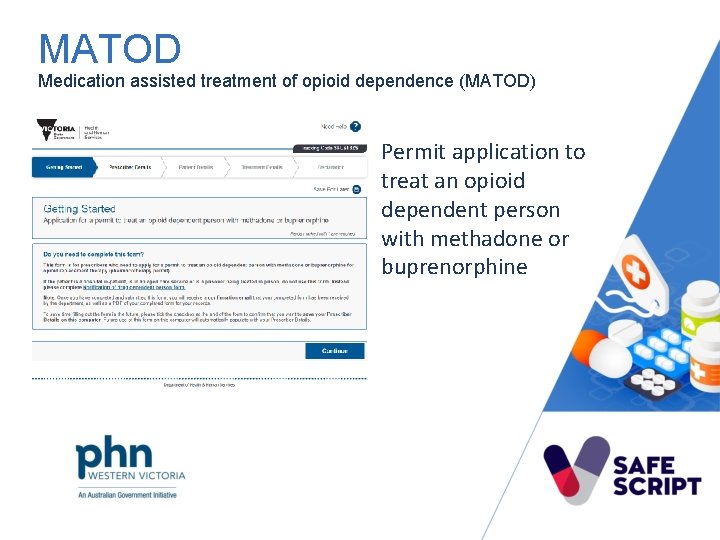
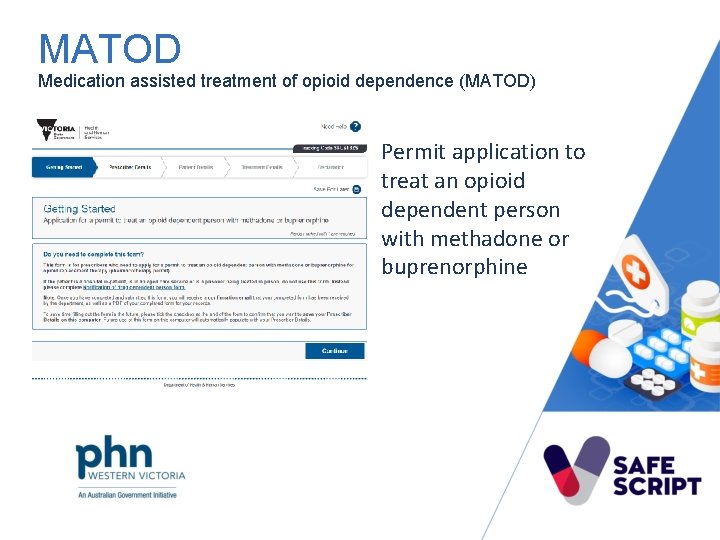
MATOD Medication assisted treatment of opioid dependence (MATOD) Permit application to treat an opioid dependent person with methadone or buprenorphine
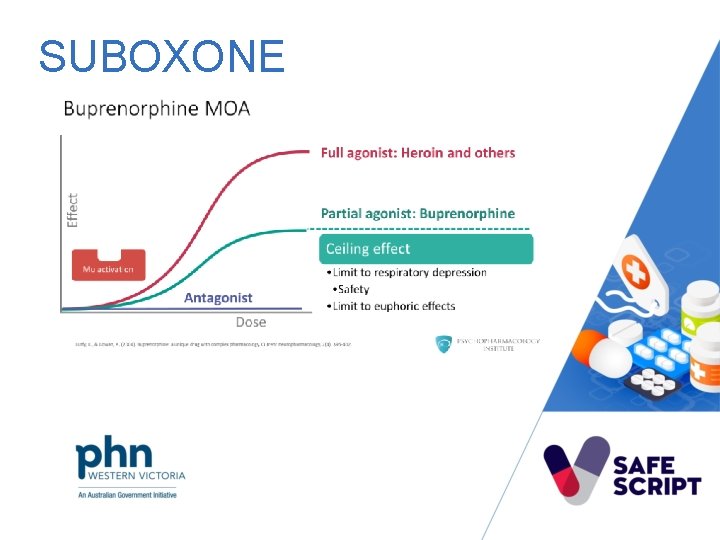
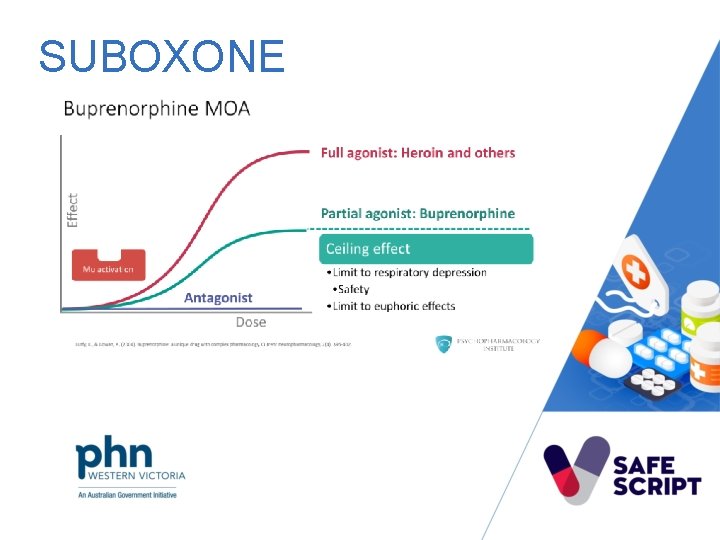
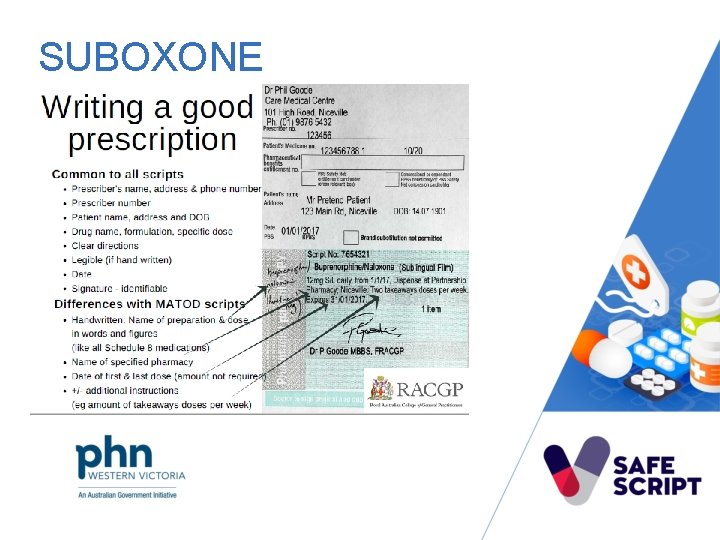
SUBOXONE
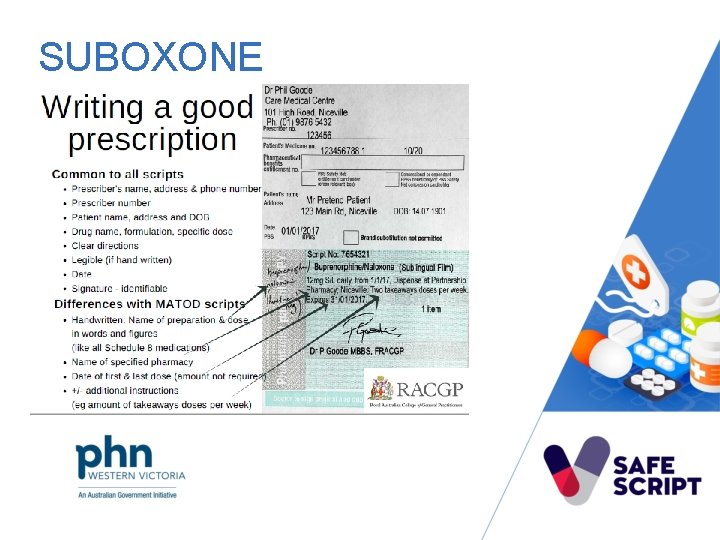
SUBOXONE
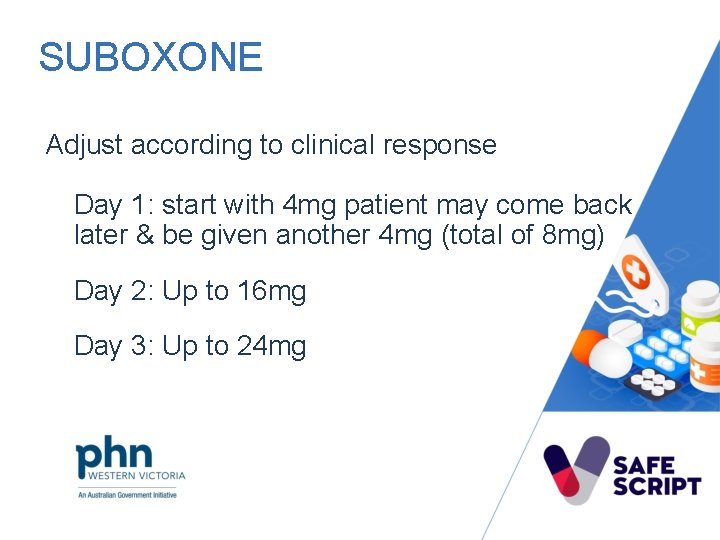
SUBOXONE Adjust according to clinical response Day 1: start with 4 mg patient may come back later & be given another 4 mg (total of 8 mg) Day 2: Up to 16 mg Day 3: Up to 24 mg
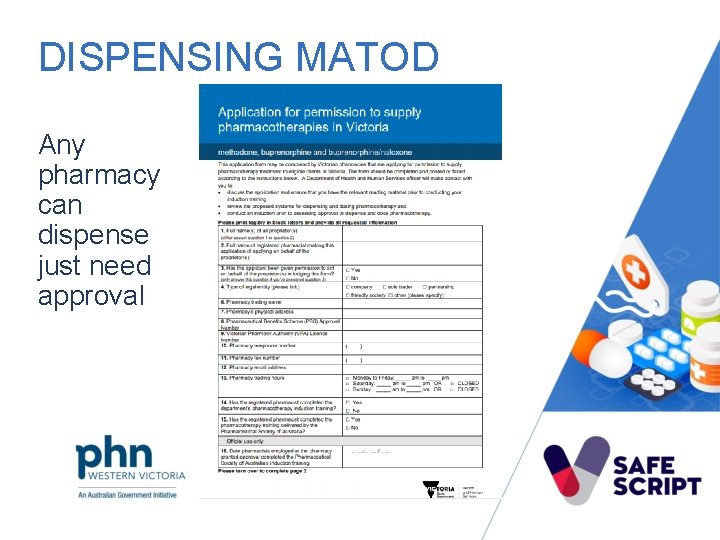
DISPENSING MATOD Any pharmacy can dispense just need approval
SUPPORT • Health. Pathways • Pharmacotherapy Area Based Networks • RAMPS • DACAS • Victorian Opioid Management ECHO
IF NOT PRESCRIBING/DISPENSING • Explain the risks/reasons • Help the patient seek appropriate treatment • Consider evidence-based non-pharmacological options for management • Provide referral options if appropriate • Collaborate with other health professionals • Document • Notify MPR if required

MEET JANET At a medical practice in Maiden Gully Victoria
QUESTIONS 1. To work out how Janet came to obtain prescriptions from multiple prescribers, what steps would you take? 2. Based on the information, if you decide to proceed with prescribing oxycodone, what are some approaches you can discuss with Janet to minimize the risks of prescribing?

JANET Janet presents at a Pharmacy in Maiden Gully Victoria
QUESTIONS 3. To work out how Janet came to obtain prescriptions from multiple prescribers, what next steps would you take? 4. At this stage, what additional information might be required before deciding whether or not to dispense the medicine?
BREAK 5 mins
CHALLENGING CONVERSATIONS • Avoid stigma • Patient-centred, shared-decision making • Patient’s readiness to change • Motivational interviewing
MOTIVATIONAL INTERVIEWING RULE • Resist the righting reflex • Understand the patient’s motivations & own reasons to change • Listen with empathy • Empower your patient
MOTIVATIONAL INTERVIEWING OARS • Open-ended questions • Affirmations • Reflections • Summarise
PATIENT RESISTANCE • Agree on direction • Assess readiness to change • Provide brief information about the effects & risks of substance abuse • Create doubt & evoke concern

MEET JANET At a medical practice in Maiden Gully Victoria
QUESTIONS 5. What approaches might help Janet recognise this issue & help motivate her to change her behaviour?
LET’S CONSIDER… 1. What if Janet had been using oxycontin for chronic pain for 6 -12 months prior to Safe. Script? How will the conversations change? 2. What are the treatment options? 3. What if your patient has been prescribed quetiapine for sleep or anxiety? 4. What if your patient has been taking diazepam for 5 years? 5. What if your patient has been prescribed benzodiazepine & a z-drug?

ACCESS & TRAINING SAFESCRIPT INFORMATION ACCESS • Only prescribers & pharmacists directly involved in the patient’s care • No patient permission required • No patient access to their Safe. Script record • Safe. Script registration SAFESCRIPT TRAINING • Training open to all health professionals • https: //vphna. org. au/safescript-hub/

HEALTHPATHWAYS & REFERRAL PAGES https: //westvic. healthpathways. org. au/
RESOURCES HUB https: //vphna. org. au/safescript-hub/ Links • References used in training development • Supplementary training available • Articles of interest • Health. Pathways sites • DHHS Safe. Script site • …. & more including these slides
ADDITIONAL SUPPORT PABNs – help manage patients & optimise available support - https: //www. pabn. org. au/ • • AMS support – consultations or Opioid Management ECHO GP & pharmacist mentoring Health. Pathways Communities of practice Clinical consultants GP Clinical Advisors DACAS
INFORMATION • Project information - DHHS Safe. Script website - www. health. vic. gov. au/safescript Email - safescript@dhhs. vic. gov. au Phone - 9096 5633 • Pharmacotherapy area based networks • Victorian Opioid Management ECHO
• QUESTIONS? ? • EVALUATION • CPD – CERIFICATES • ACRRM activity # 13949 – 2 core points • RACGP activity # 135060 – 4 Cat. 2 points • APC pending THANK YOU