Safe prescribing How to avoid prescribing errors Kevin

Safe prescribing: How to avoid prescribing errors Kevin Gibbs Clinical Pharmacy Manager United Bristol Healthcare Trust
Aims ¡ To provide an awareness of: l l l ¡ Common medication errors How to minimise these National and local resources available to you to aid in safer prescribing To give you some prescribing pointers to look out for in your clinical placements
¡ By the end of the session you should be able to: l l Define a medication error List the ‘Five Rights’ Identify common types of medication errors Begin to think about how to minimise errors by using your knowledge, skills and available resources
During your placements Think about: ¡ What do I need to prescribe in a safe way? l l Patient information ¡ Co-morbid conditions Drug information ¡ Pharmacology Pharmacokinetics and pharmacodynamics ¡ Therapeutics Systems ¡ Policies, guidelines, prescribing aids etc ¡ l
What is an error?
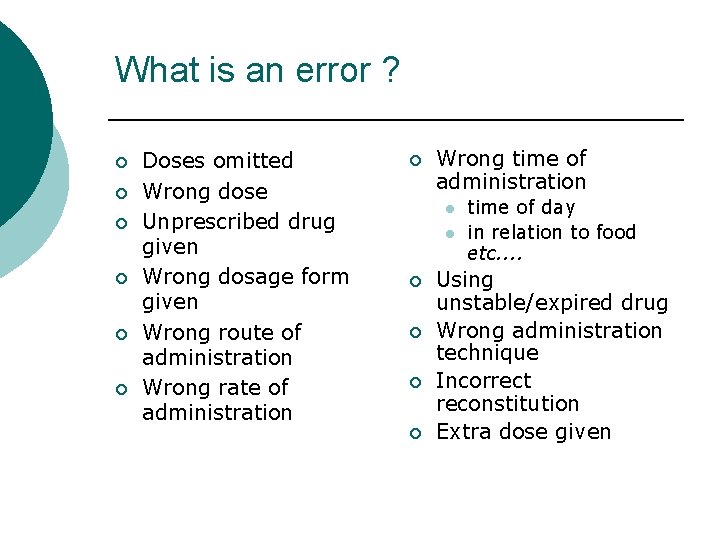
What is an error ? ¡ ¡ ¡ Doses omitted Wrong dose Unprescribed drug given Wrong dosage form given Wrong route of administration Wrong rate of administration ¡ Wrong time of administration l l ¡ ¡ time of day in relation to food etc. . Using unstable/expired drug Wrong administration technique Incorrect reconstitution Extra dose given
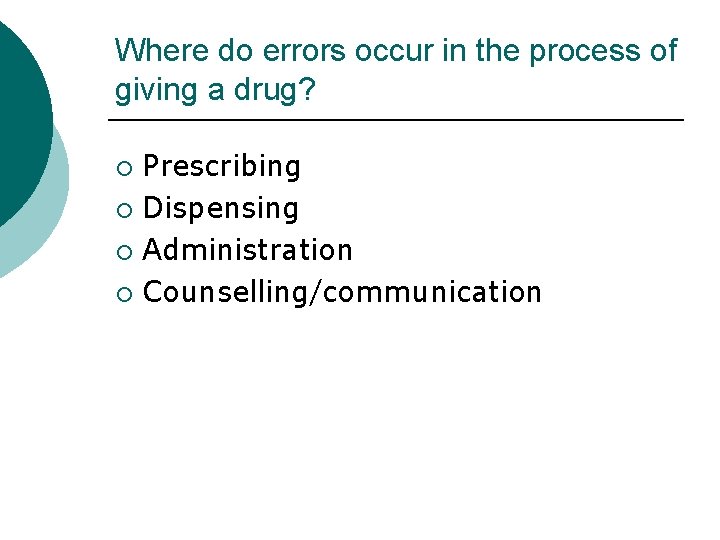
Where do errors occur in the process of giving a drug? Prescribing ¡ Dispensing ¡ Administration ¡ Counselling/communication ¡
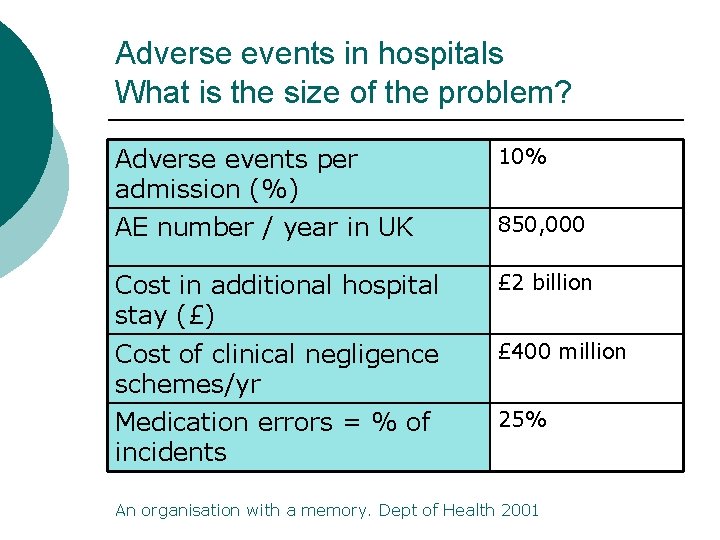
Adverse events in hospitals What is the size of the problem? Adverse events per admission (%) 10% AE number / year in UK 850, 000 Cost in additional hospital stay (£) £ 2 billion Cost of clinical negligence schemes/yr £ 400 million Medication errors = % of incidents 25% An organisation with a memory. Dept of Health 2001
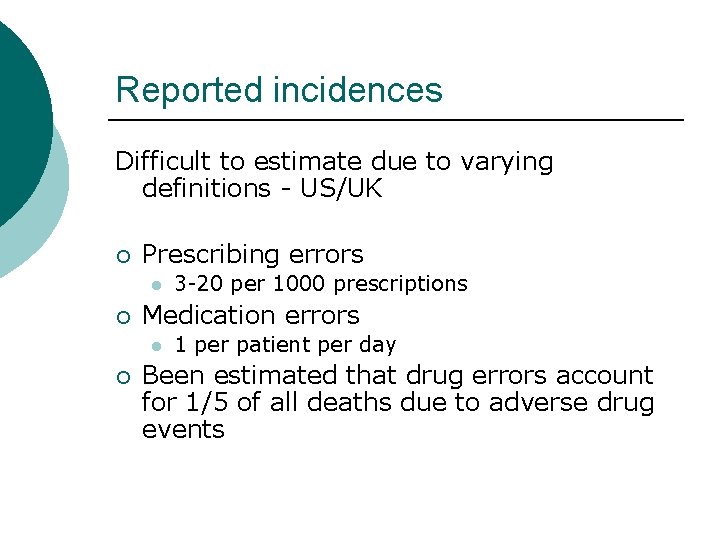
Reported incidences Difficult to estimate due to varying definitions - US/UK ¡ Prescribing errors l ¡ Medication errors l ¡ 3 -20 per 1000 prescriptions 1 per patient per day Been estimated that drug errors account for 1/5 of all deaths due to adverse drug events
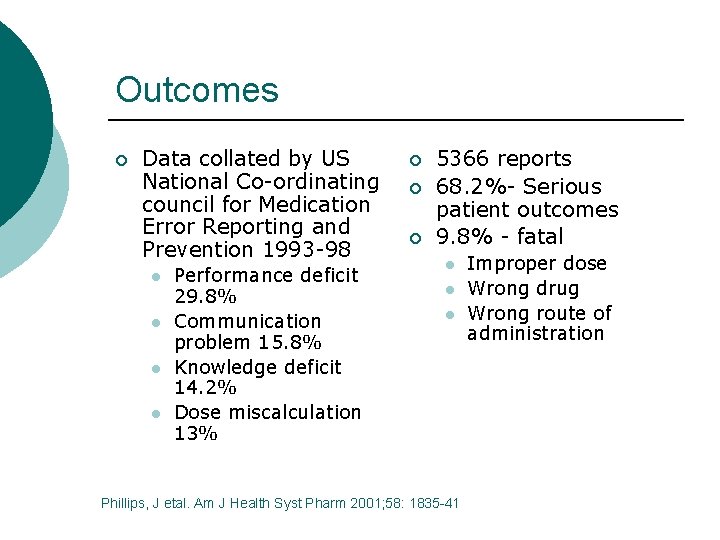
Outcomes ¡ Data collated by US National Co-ordinating council for Medication Error Reporting and Prevention 1993 -98 l l Performance deficit 29. 8% Communication problem 15. 8% Knowledge deficit 14. 2% Dose miscalculation 13% ¡ ¡ ¡ 5366 reports 68. 2%- Serious patient outcomes 9. 8% - fatal l Phillips, J etal. Am J Health Syst Pharm 2001; 58: 1835 -41 Improper dose Wrong drug Wrong route of administration
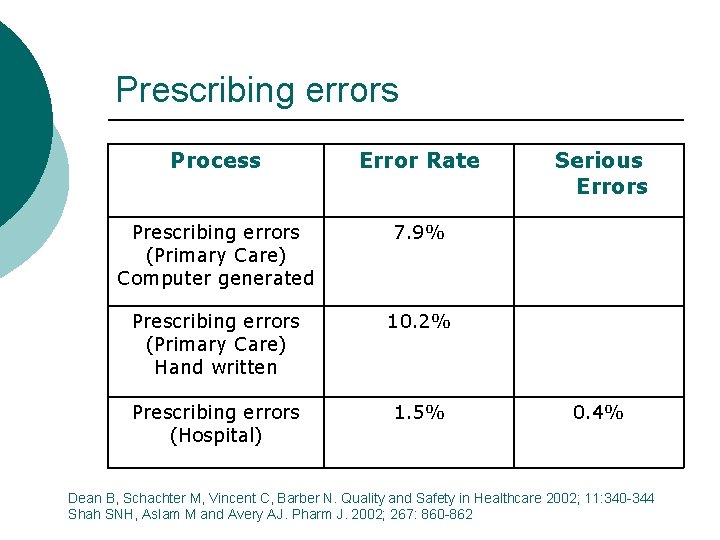
Prescribing errors Process Error Rate Prescribing errors (Primary Care) Computer generated 7. 9% Prescribing errors (Primary Care) Hand written 10. 2% Prescribing errors (Hospital) 1. 5% Serious Errors 0. 4% Dean B, Schachter M, Vincent C, Barber N. Quality and Safety in Healthcare 2002; 11: 340 -344 Shah SNH, Aslam M and Avery AJ. Pharm J. 2002; 267: 860 -862
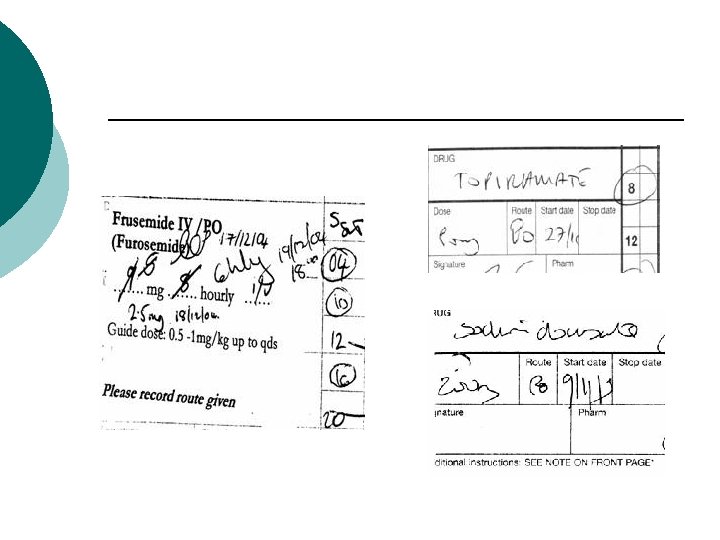
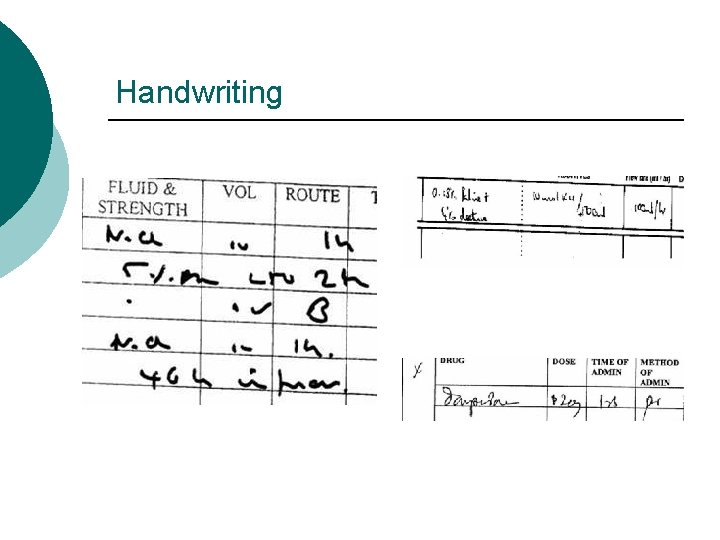
Handwriting
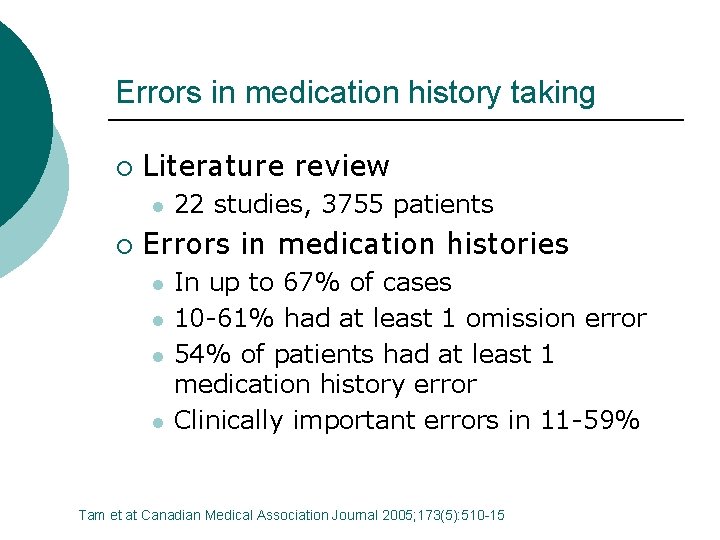
Errors in medication history taking ¡ Literature review l ¡ 22 studies, 3755 patients Errors in medication histories l l In up to 67% of cases 10 -61% had at least 1 omission error 54% of patients had at least 1 medication history error Clinically important errors in 11 -59% Tam et at Canadian Medical Association Journal 2005; 173(5): 510 -15
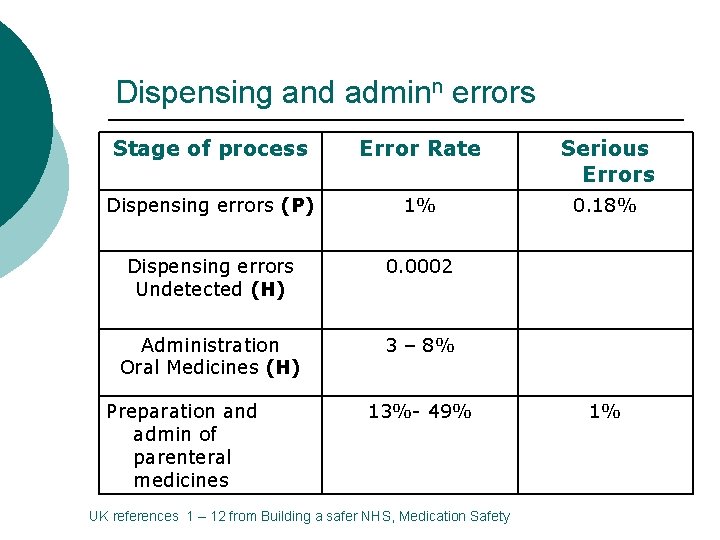
Dispensing and adminn errors Stage of process Error Rate Serious Errors Dispensing errors (P) 1% 0. 18% Dispensing errors Undetected (H) 0. 0002 Administration Oral Medicines (H) 3 – 8% Preparation and admin of parenteral medicines 13%- 49% UK references 1 – 12 from Building a safer NHS, Medication Safety 1%
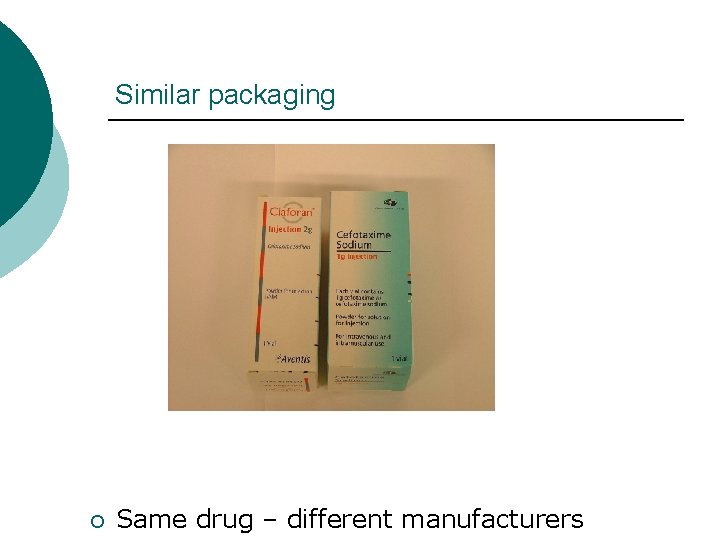
Similar packaging ¡ Same drug – different manufacturers
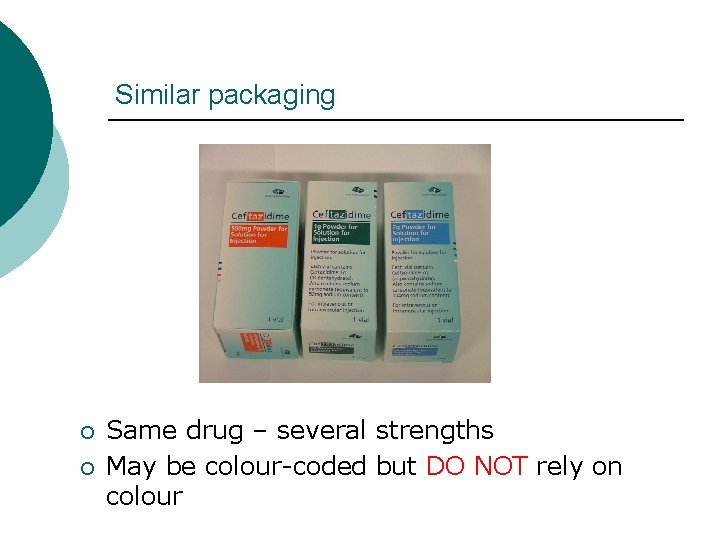
Similar packaging ¡ ¡ Same drug – several strengths May be colour-coded but DO NOT rely on colour
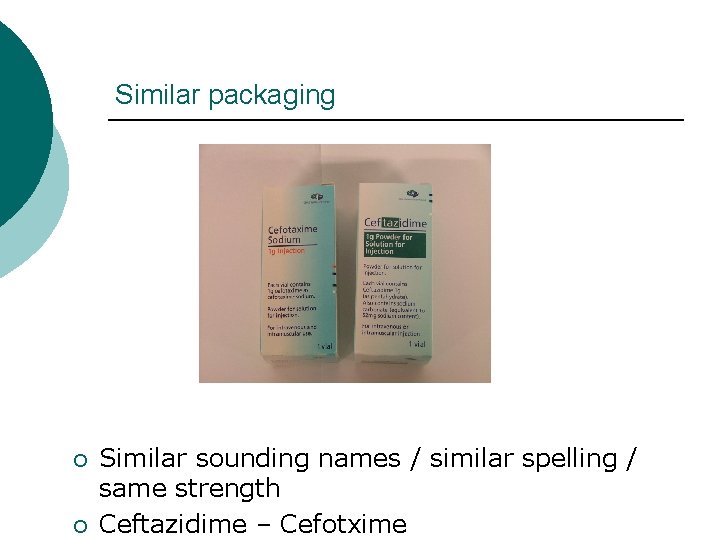
Similar packaging ¡ ¡ Similar sounding names / similar spelling / same strength Ceftazidime – Cefotxime
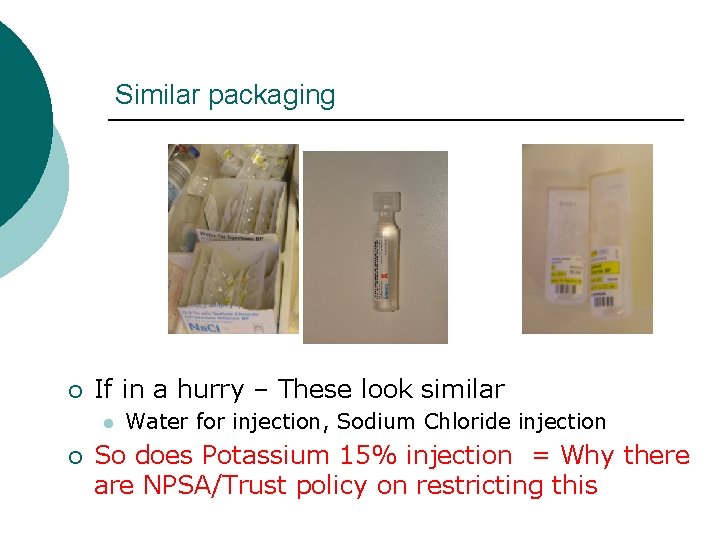
Similar packaging ¡ If in a hurry – These look similar l ¡ Water for injection, Sodium Chloride injection So does Potassium 15% injection = Why there are NPSA/Trust policy on restricting this
Summary: Common error types Wrong patient ¡ Contra-indicated medicine ¡ l Allergy, medical condition, drug-drug interaction Wrong ¡ Wrong ¡ drug / ingredient dose / frequency formulation route of administration quantity
Poor handwriting on Rx ¡ Incorrect IV administration calculations or pump rates ¡ Poor record keeping/checking ¡ l l double doses wrong patient Paediatric doses ¡ Poor administration technique ¡
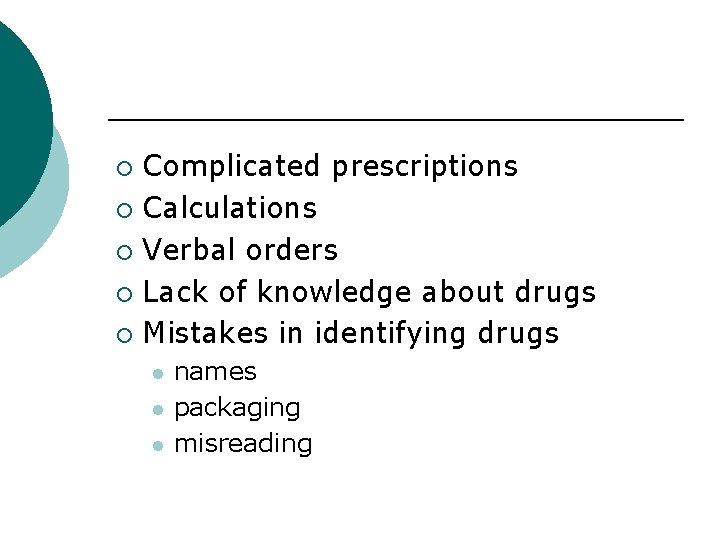
Complicated prescriptions ¡ Calculations ¡ Verbal orders ¡ Lack of knowledge about drugs ¡ Mistakes in identifying drugs ¡ l l l names packaging misreading
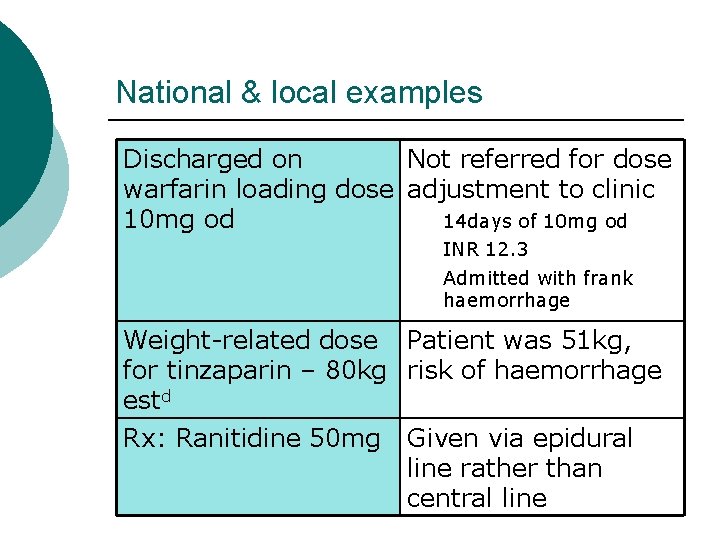
National & local examples Discharged on Not referred for dose warfarin loading dose adjustment to clinic 14 days of 10 mg od INR 12. 3 Admitted with frank haemorrhage Weight-related dose Patient was 51 kg, for tinzaparin – 80 kg risk of haemorrhage estd Rx: Ranitidine 50 mg Given via epidural line rather than central line
Discharged on Not referred for dose warfarin loading dose adjustment to clinic 14 days of 10 mg od INR 12. 3 Admitted with frank haemorrhage Weight-related dose for tinzaparin – 80 kg estd Rx: Ranitidine 50 mg Patient was 51 kg, risk of haemorrhage Given via epidural line rather than central line
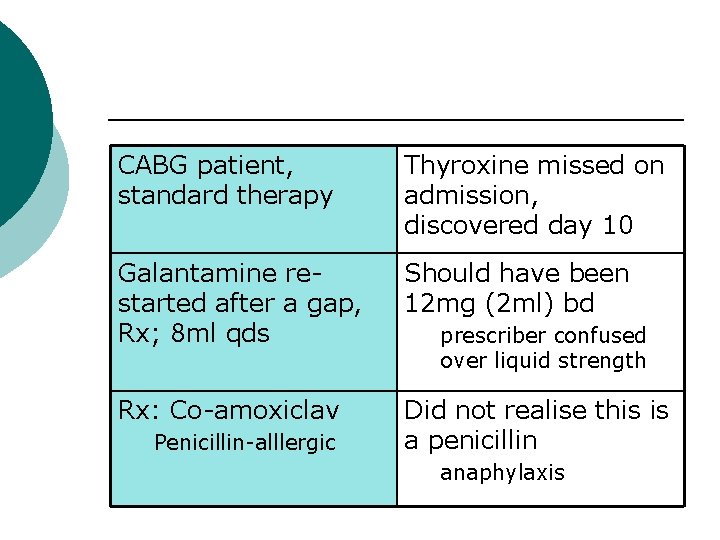
CABG patient, standard therapy Thyroxine missed on admission, discovered day 10 Galantamine restarted after a gap, Rx; 8 ml qds Should have been 12 mg (2 ml) bd Rx: Co-amoxiclav Did not realise this is a penicillin Penicillin-alllergic prescriber confused over liquid strength anaphylaxis
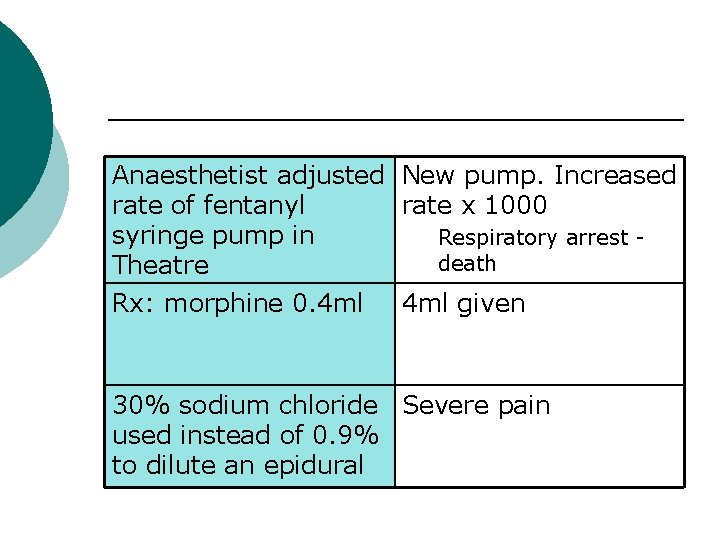
Anaesthetist adjusted New pump. Increased rate of fentanyl rate x 1000 syringe pump in Respiratory arrest death Theatre Rx: morphine 0. 4 ml given 30% sodium chloride Severe pain used instead of 0. 9% to dilute an epidural
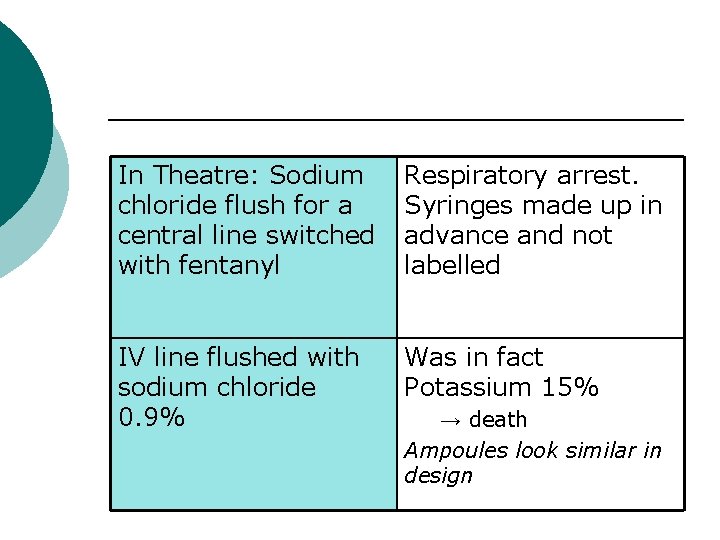
In Theatre: Sodium chloride flush for a central line switched with fentanyl Respiratory arrest. Syringes made up in advance and not labelled IV line flushed with sodium chloride 0. 9% Was in fact Potassium 15% → death Ampoules look similar in design
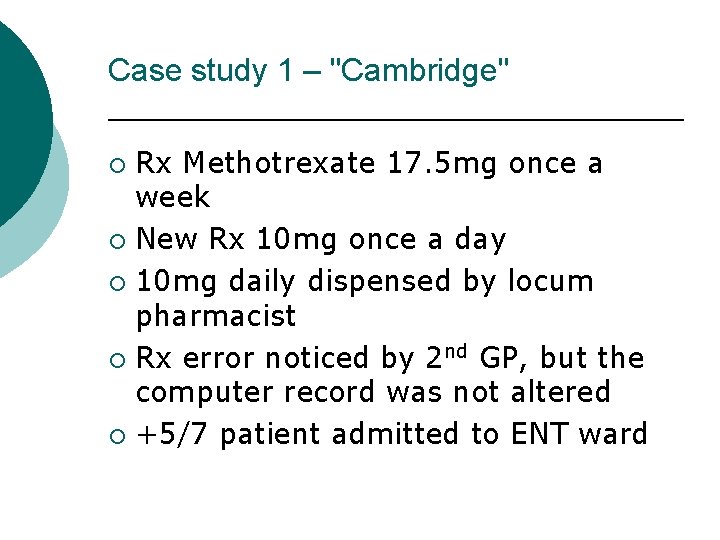
Case study 1 – "Cambridge" Rx Methotrexate 17. 5 mg once a week ¡ New Rx 10 mg once a day ¡ 10 mg daily dispensed by locum pharmacist ¡ Rx error noticed by 2 nd GP, but the computer record was not altered ¡ +5/7 patient admitted to ENT ward ¡
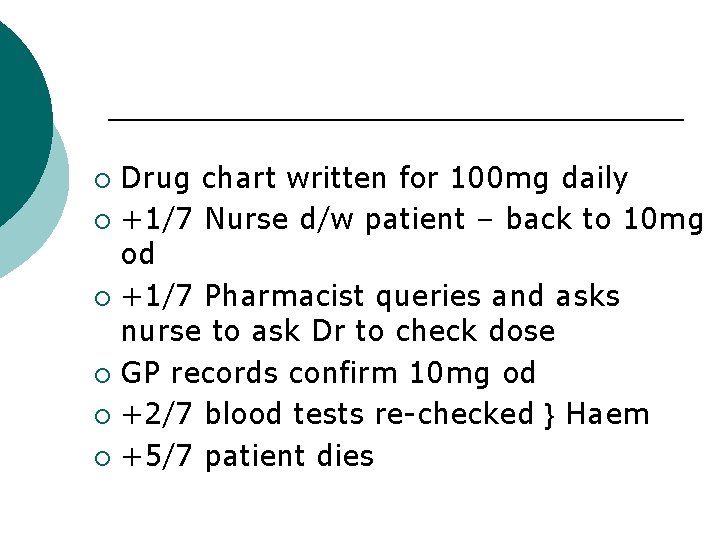
Drug chart written for 100 mg daily ¡ +1/7 Nurse d/w patient – back to 10 mg od ¡ +1/7 Pharmacist queries and asks nurse to ask Dr to check dose ¡ GP records confirm 10 mg od ¡ +2/7 blood tests re-checked } Haem ¡ +5/7 patient dies ¡
Case study 2 – “Nottingham” Rx Intrathecal methotrexate under GA in theatre by Oncology Reg & intravenous vincristine on ward by specialist nurse ¡ "Outlied" on non-specialist ward ¡ Both drugs delivered to theatre from ward ¡ Given food pre-op – op postponed ¡
Orignal Sp. R off-duty now ¡ Cover Sp. R unable to leave ward, anaesthetist to admin intrathecal drug ¡ Aneasthetist had given I/Thecal drugs before but had never given chemotherapy ¡ Methotrexate given intravenously ¡ Vincristine given intrathecally ¡ Patient died ¡
Improving medication safety Department of Health. Jan 2004
Improving medication safety: Main areas of medication error ¡ ¡ ¡ ¡ Anaesthetic practice Anticoagulants Cytotoxic drugs Intravenous infusions Methotrexate Opiate analgesics Potassium chloride
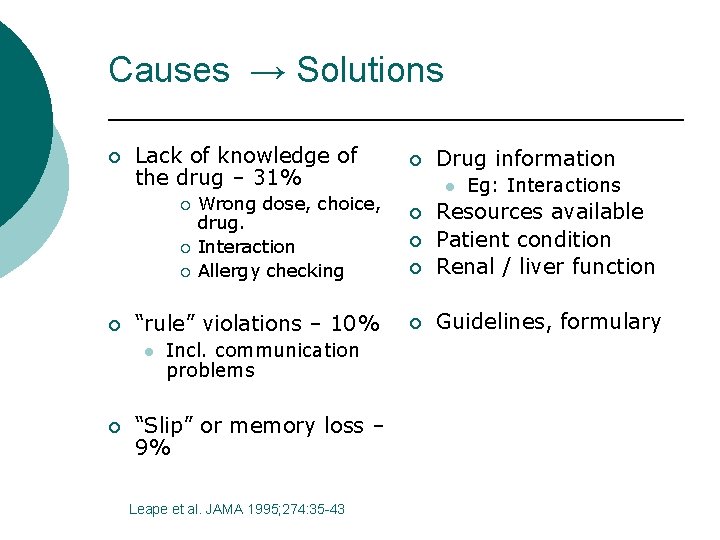
Causes → Solutions ¡ Lack of knowledge of the drug – 31% ¡ ¡ “rule” violations – 10% l ¡ Wrong dose, choice, drug. Interaction Allergy checking Incl. communication problems “Slip” or memory loss – 9% Leape et al. JAMA 1995; 274: 35 -43 ¡ Drug information l Eg: Interactions ¡ Resources available Patient condition Renal / liver function ¡ Guidelines, formulary ¡ ¡
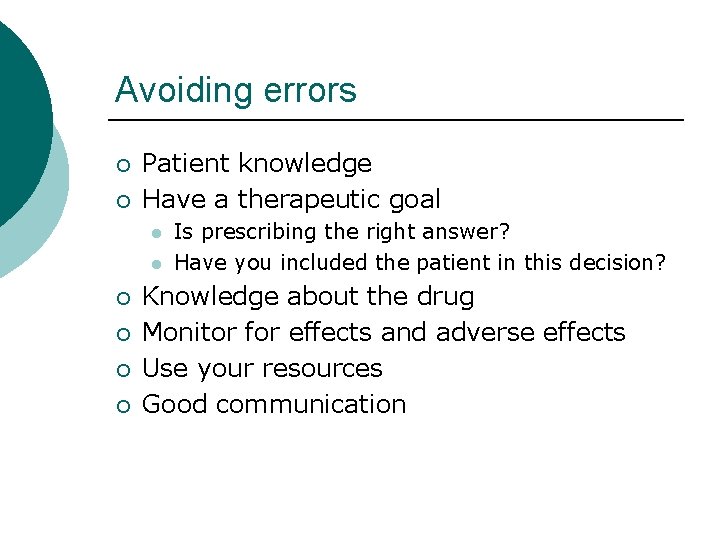
Avoiding errors ¡ ¡ Patient knowledge Have a therapeutic goal l l ¡ ¡ Is prescribing the right answer? Have you included the patient in this decision? Knowledge about the drug Monitor for effects and adverse effects Use your resources Good communication
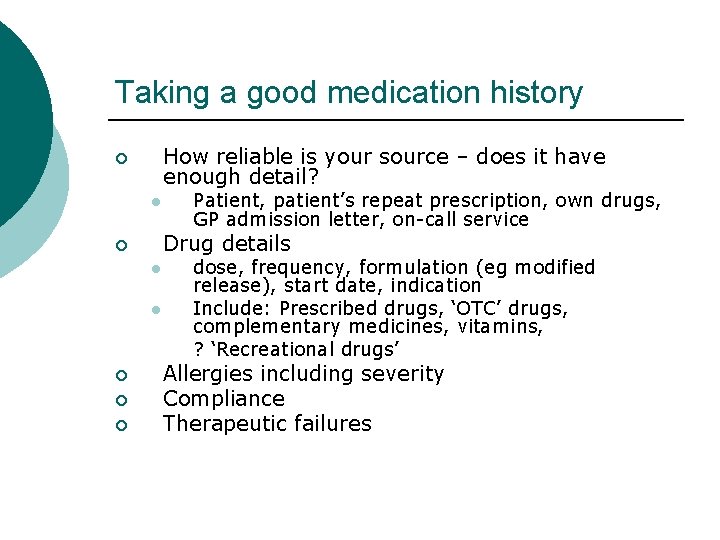
Taking a good medication history How reliable is your source – does it have enough detail? ¡ l Drug details ¡ l l ¡ ¡ ¡ Patient, patient’s repeat prescription, own drugs, GP admission letter, on-call service dose, frequency, formulation (eg modified release), start date, indication Include: Prescribed drugs, ‘OTC’ drugs, complementary medicines, vitamins, ? ‘Recreational drugs’ Allergies including severity Compliance Therapeutic failures
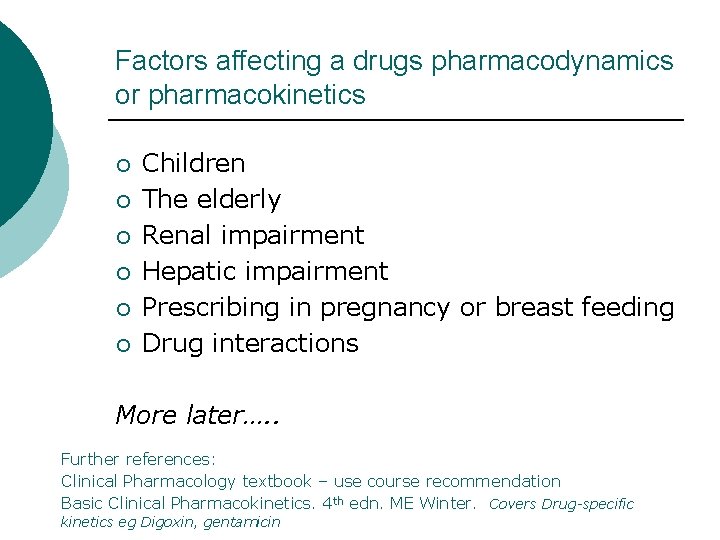
Factors affecting a drugs pharmacodynamics or pharmacokinetics ¡ ¡ ¡ Children The elderly Renal impairment Hepatic impairment Prescribing in pregnancy or breast feeding Drug interactions More later…. . Further references: Clinical Pharmacology textbook – use course recommendation Basic Clinical Pharmacokinetics. 4 th edn. ME Winter. Covers Drug-specific kinetics eg Digoxin, gentamicin
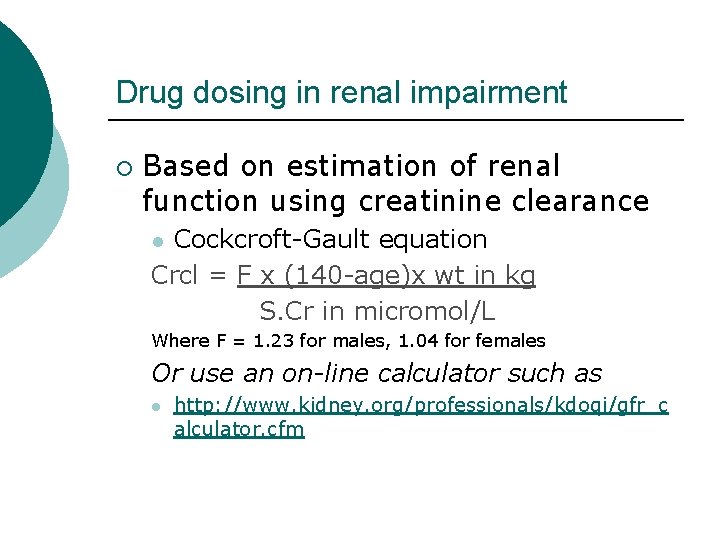
Drug dosing in renal impairment ¡ Based on estimation of renal function using creatinine clearance Cockcroft-Gault equation Crcl = F x (140 -age)x wt in kg S. Cr in micromol/L l Where F = 1. 23 for males, 1. 04 for females Or use an on-line calculator such as l http: //www. kidney. org/professionals/kdoqi/gfr_c alculator. cfm
Drug-drug interactions drug-food interactions ¡ Resources l l BNF Appendix 1 Pharmacy Medicines Information Departments ¡ ¡ Have specialists texts and other resources to help m. Ore in a leter talk
Resources available to you Summary of Product Characteristics for each medicine - e. MC ¡ Pharmacy Medicines Information ¡ On-line ¡ National ¡ Electronic prescribing ¡ Other medical and non-medical prescribers ¡
Pharmacy ¡ Avaliable for help and advice l l l Ward Pharmacist Local Medicines Information department Regional medicines Information ¡ l Mainly Community sector enquiries Out-of-hours: On-call or resident pharmacist
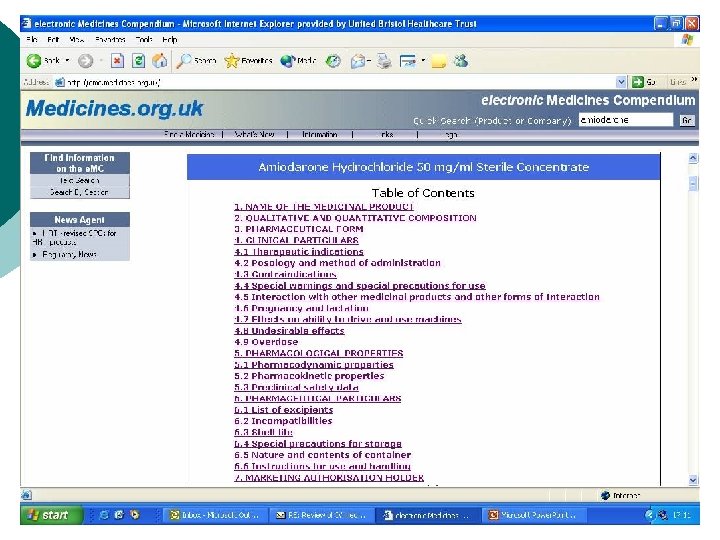
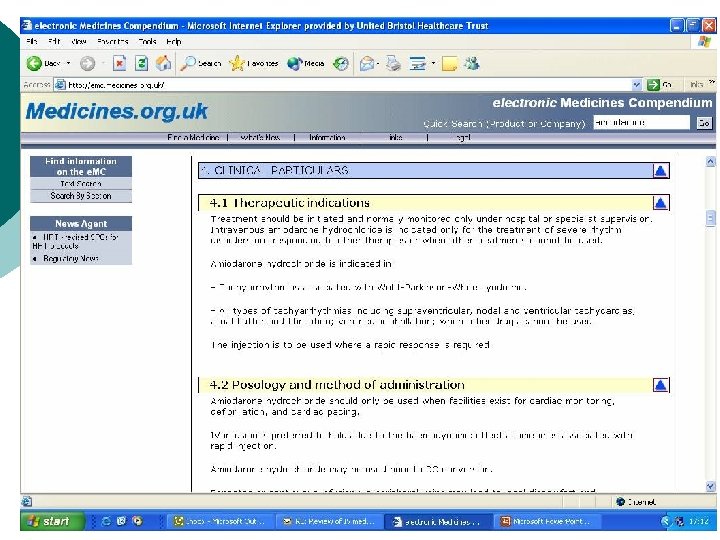
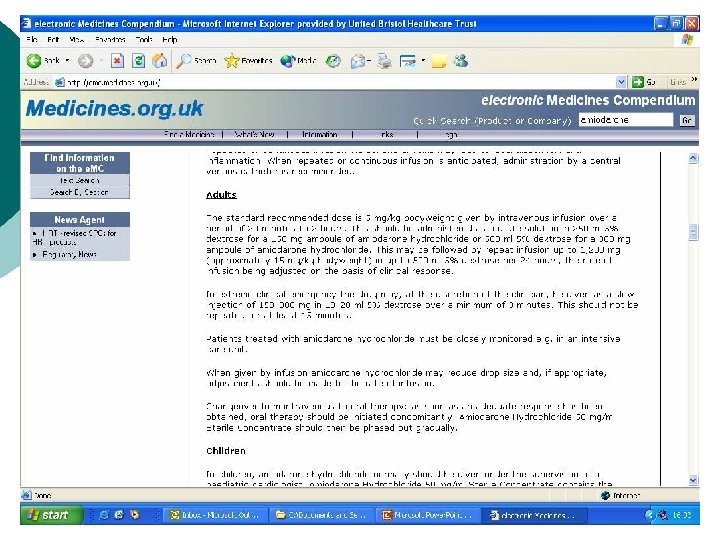
Electronic Medicines Compendium (e. MC) ¡ The e. MC provides up-to-date information on licensed UK medicines http: //emc. medicines. org. uk/ l l ¡ Summary of Product Characteristics (SPCs) Patient Information Leaflets (PILs). SPCs are legal & technical documents with information to help guide on the best way to use a medicine.
In summary
Prescribing responsibilities Drug ¡ Dose ¡ Route ¡ Rate of administration ¡ Duration of treatment ¡ ¡ Checking patient allergies & sensitivities
¡ Providing a prescription that is: l l Legible Legal Signed Giving all information to allow safe administration
Hints ¡ ¡ Clear and unambiguous ¡ Care with units ¡ Legal Approved name ¡ ¡ No abbreviations ¡ Care with IVs Is it weight/BSArelated dosing. Is weight accurate?
¡ ¡ ¡ Clear decimal points 0. 5 ml not. 5 ml Rewrite charts regularly Take time, eg to read labels ¡ ¡ ¡ Avoid abbreviations od / bd / tds / qds Not 250 mg 3
¡ Take particular care if: l l l Impaired renal function Hepatic dysfunction Children The elderly Drug is unknown to you Very new drug
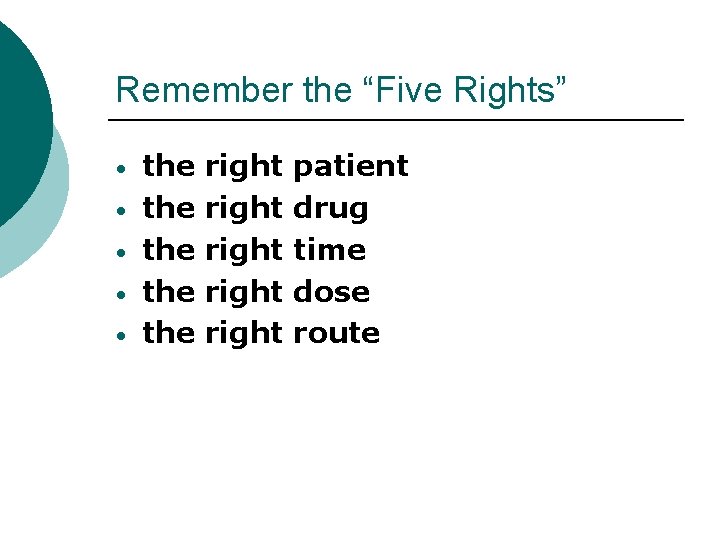
Remember the “Five Rights” • • • the the the right right patient drug time dose route
If in doubt ……. . Ask
Further reading & resources Naylor, R. Medication Errors. Radcliffe Press. ISBN 1857759567 ¡ Department of Health. (2004). Building a safer NHS. Improving medication safety. ¡ l ¡ http: //www. dh. gov. uk/Publications. And. Statist ics/Publications. Policy. And. Guidan ce/Publications. Policy. And. Guidance. Article/fs/e n? CONTENT_ID=4071443&chk=PH 2 s. ST National Patient Safety Agency l Website: http: //www. npsa. nhs. uk/
¡ National Prescribing Centre l ¡ Website: http: //www. ismp. org/ National Electronic Library for Medicines l ¡ http: //www. npc. co. uk/ Institute for Safe Medication Practices (ISMP) (American) l ¡ Website: http: //www. druginfozone. nhs. uk/hom e/default. aspx Aronson & Richards. Oxford Handbook of Practical Drug Therapy. ISBN 0198530072
- Slides: 57