Safe Patient Handling and Movement Assessing Facility Patient

- Slides: 38
Safe Patient Handling and Movement Assessing Facility & Patient Needs Towards Appropriate Selection of Safe-Lift Equipment Dana L. Root, MS, PT, CPE Regional Ergonomics Coordinator Chicago, IL 312 -353 -2220 414 -297 -3315 root. dana@dol. gov
Terminology n Caregivers: – RNs, LPNs, CNAs – PTs, PTAs, OTAs – Aides – Transporters – Family members – Etc.
Where To Start Step 1: Collect Baseline Data Step 2: Identify High-Risk Units Step 3: Gather Data About High-Risk Units Step 4: Identify High-Risk Tasks Step 5: Conduct Team Assessments of These Tasks Step 6: Analyze the Risk Step 7: Involve the Caregiver and Patient in Selecting the Equipment Step 8: Determine Recommendations Step 9: Implement Recommendations Step 10: Monitor Results
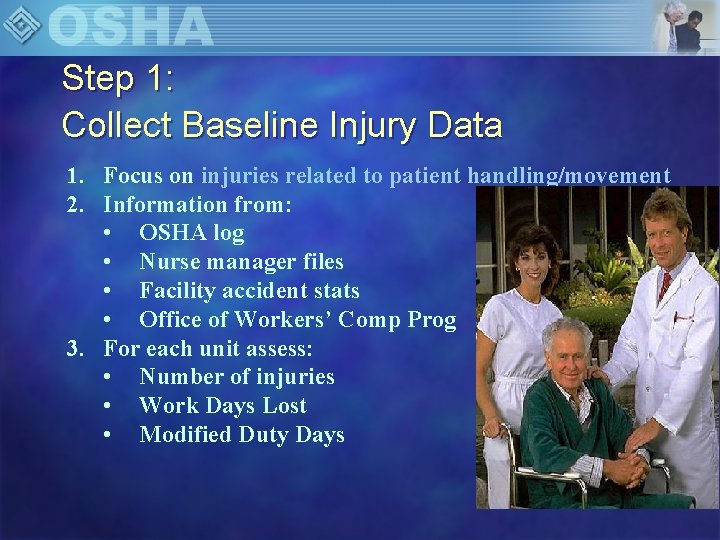
Step 1: Collect Baseline Injury Data 1. Focus on injuries related to patient handling/movement 2. Information from: • OSHA log • Nurse manager files • Facility accident stats • Office of Workers’ Comp Prog 3. For each unit assess: • Number of injuries • Work Days Lost • Modified Duty Days
Step 2: Identify High-Risk Units 1. How? • Using baseline data on the incidence and severity of injuries 2. Why? • Allows you to prioritize time and resources.
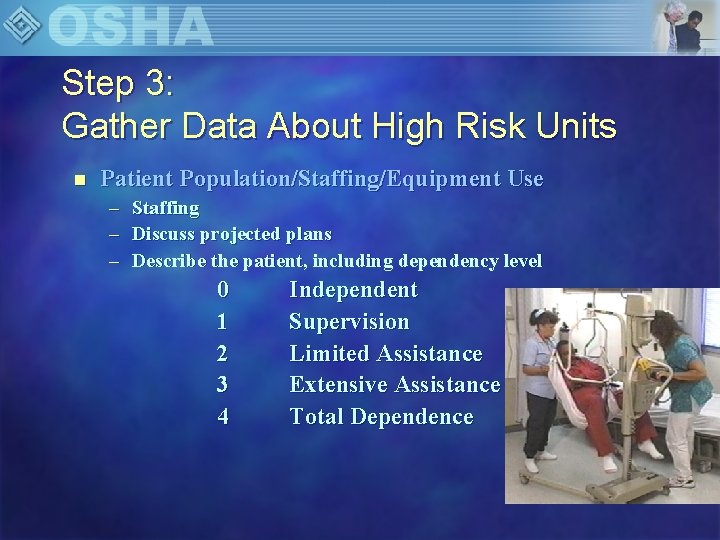
Step 3: Gather Data About High Risk Units n Patient Population/Staffing/Equipment Use – Staffing – Discuss projected plans – Describe the patient, including dependency level 0 1 2 3 4 Independent Supervision Limited Assistance Extensive Assistance Total Dependence
Step 3: Gather Data About High Risk Units Space considerations n n n General facility layout Doorway width Angles and turns Storage Dining rooms n n Hallway – Railings Visiting rooms Activity rooms Common bathrooms
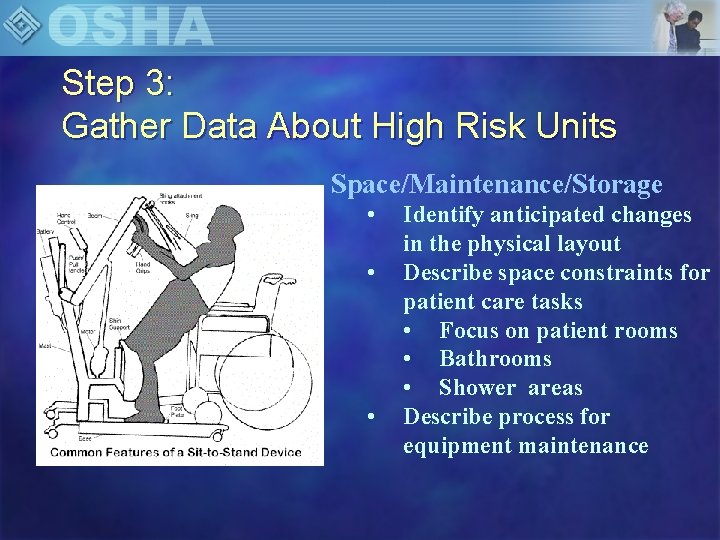
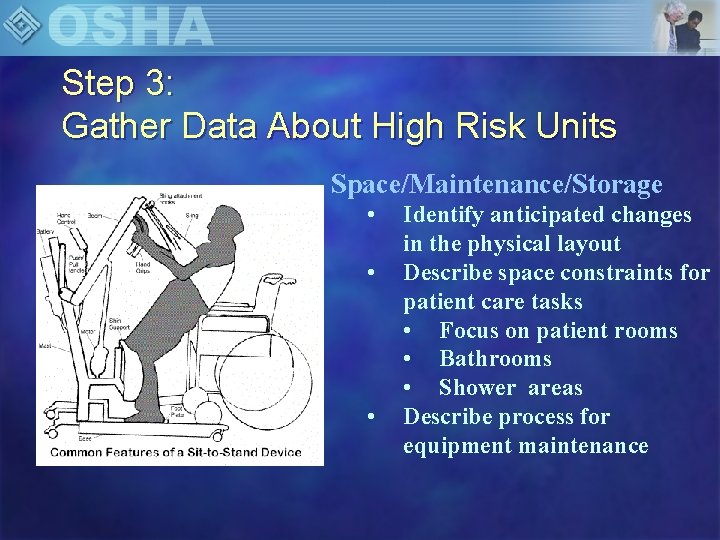
Step 3: Gather Data About High Risk Units Space/Maintenance/Storage • • • Identify anticipated changes in the physical layout Describe space constraints for patient care tasks • Focus on patient rooms • Bathrooms • Shower areas Describe process for equipment maintenance
Step 3: Gather Data about High Risk Units 1. Inventory of all patient care equipment 2. Describe working condition 3. How frequently equipment is used 4. Perception of problem areas
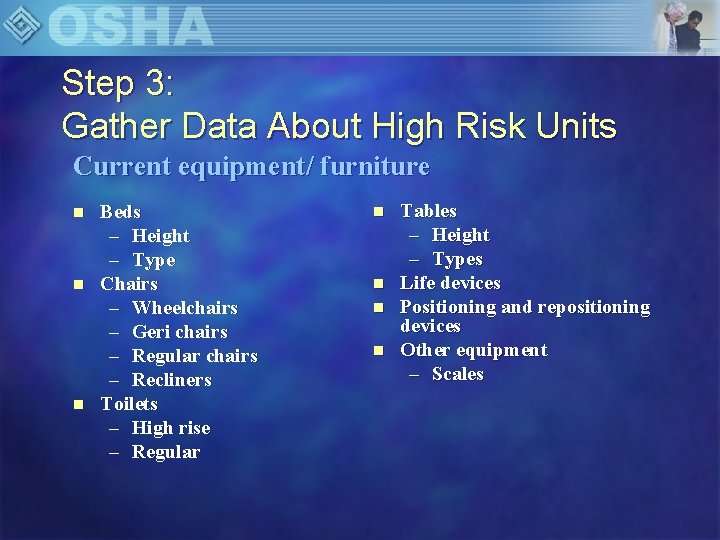
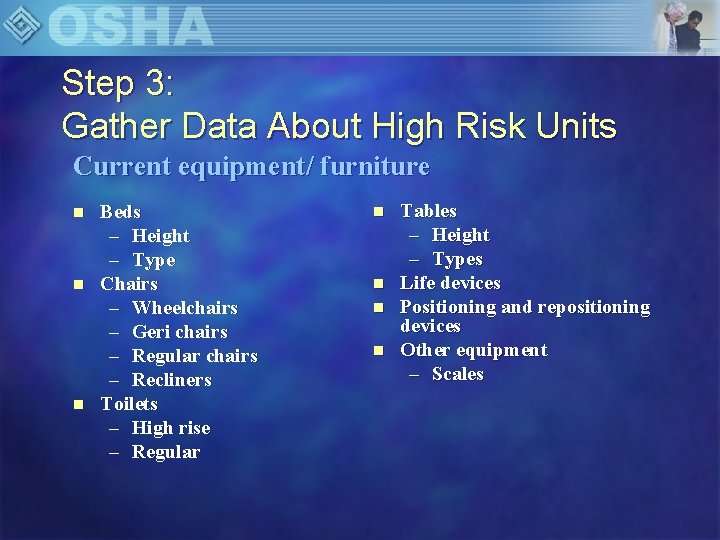
Step 3: Gather Data About High Risk Units Current equipment/ furniture n n n Beds – Height – Type Chairs – Wheelchairs – Geri chairs – Regular chairs – Recliners Toilets – High rise – Regular n n Tables – Height – Types Life devices Positioning and repositioning devices Other equipment – Scales

Step 4: Identify High Risk Tasks • Identify and assess nursing staff perceptions of high-risk tasks. • Identify variation between units • Patient characteristics • Availability of equipment • Physical layout • Work organization
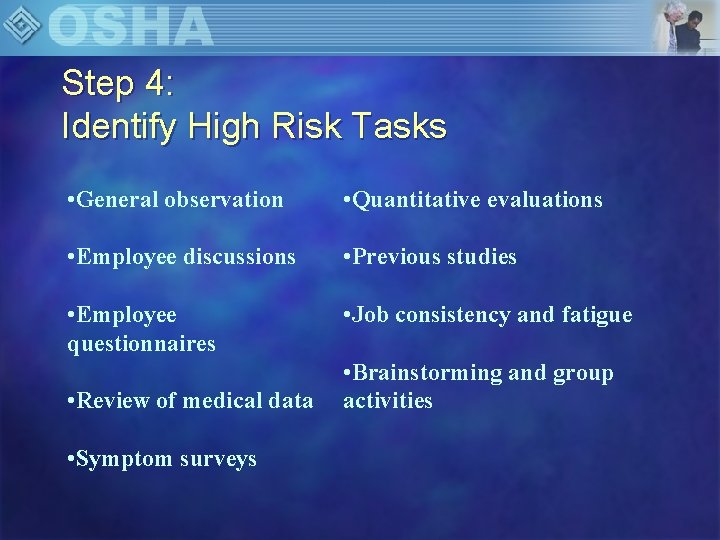
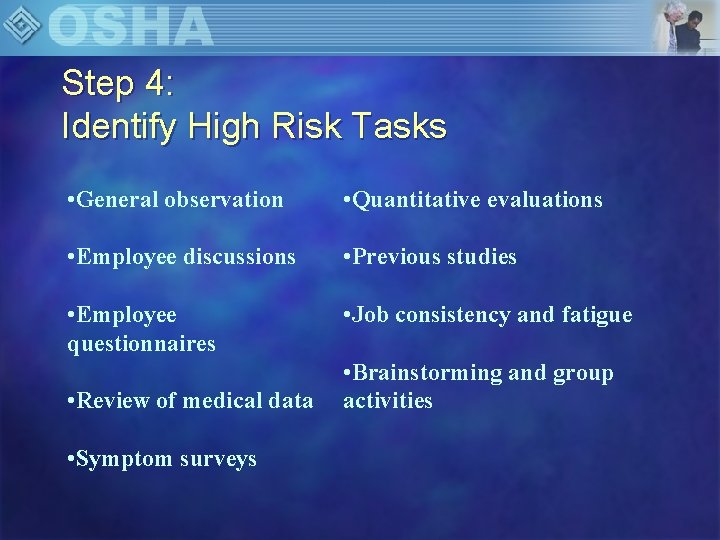
Step 4: Identify High Risk Tasks • General observation • Quantitative evaluations • Employee discussions • Previous studies • Employee questionnaires • Job consistency and fatigue • Review of medical data • Symptom surveys • Brainstorming and group activities
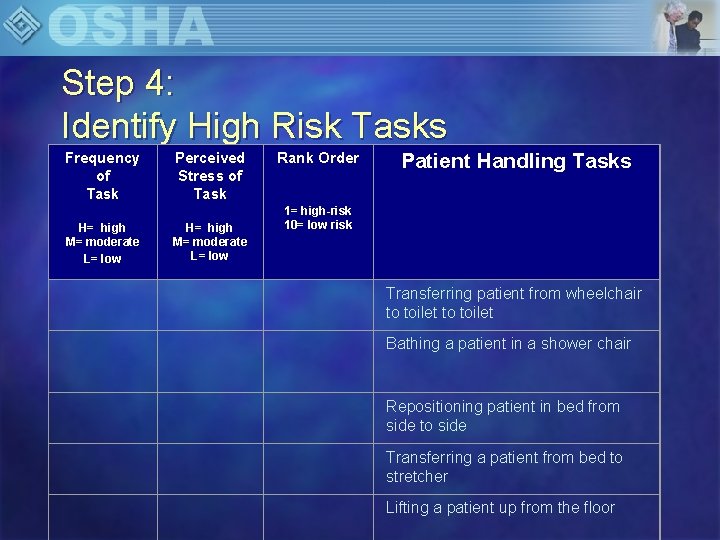
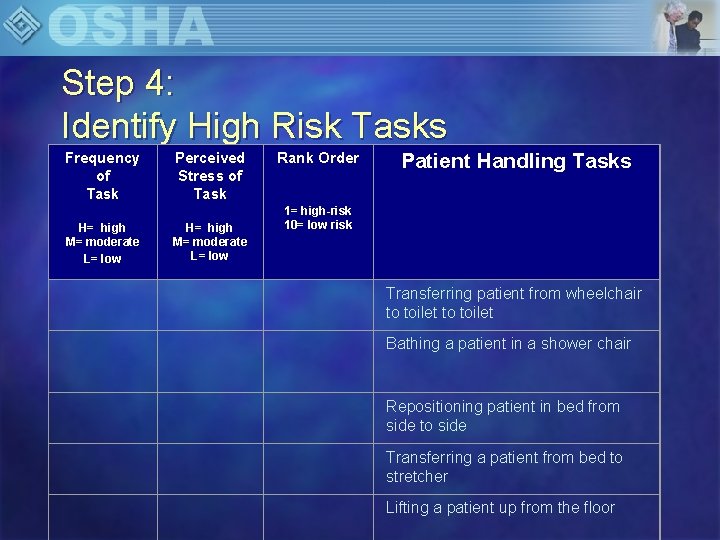
Step 4: Identify High Risk Tasks Frequency of Task H= high M= moderate L= low Perceived Stress of Task H= high M= moderate L= low Rank Order Patient Handling Tasks 1= high-risk 10= low risk Transferring patient from wheelchair to toilet Bathing a patient in a shower chair Repositioning patient in bed from side to side Transferring a patient from bed to stretcher Lifting a patient up from the floor
Step 5: Conduct Assessment by the team Purpose: • Include staff input in assessment and solutions. • Recognize the many direct and indirect factors that may contribute to potential risk • Identify potential solutions that will serve to minimize risk of injury to the caregivers and patients
Step 6: Risk Analysis 1. Review data for each unit: • Baseline injury data • Other data • Staffing • Equipment inventory • Anticipated changes • Rank high risk tasks • Frequency • Stress • Observation data 2. Identify problem areas 3. Set priorities
Step 7: Involve Healthcare Provider & Patient in Selecting Equipment ✲Obtain Patient & Healthcare Provider Buy-In ✲ Purpose: To enhance effectiveness by increasing acceptance and adherence.
Step 7: Involve Healthcare Provider & Patient in Selecting Equipment n Two end user groups: 1. Caregiver 2. Patient n Both participate in the decision making process – Equipment fairs – Trial sessions
Step 7: Involve Healthcare Provider & Patient in Selecting Equipment Patients can rate/rank the equipment using surveys n Family members can have input to selection n
Step 8: Determine Recommendations 1. Achievable and simple 2. Constraints 3. Costs
Step 8: Implement Recommendations 4. Approaches • Engineering Controls • Reduce or eliminate hazard • Equipment • Furniture • Tools • Administrative Controls • Work practices changes • Management policies • Staffing levels • Staff needed for each type of transfer • Lifting schedules • Lifting teams
EQUIPMENT SELECTION: Engineering Controls 1. Eliminate the need to do the hazardous activity 2. Redesign the activity to reduce the hazard or minimize the hazard 3. Formal equipment selection and evaluation process 4. Selected at equipment fairs
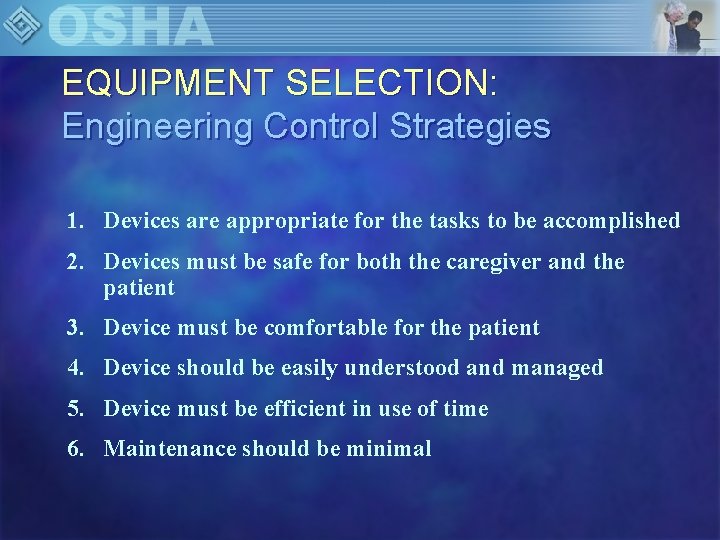
EQUIPMENT SELECTION: Engineering Control Strategies 1. Devices are appropriate for the tasks to be accomplished 2. Devices must be safe for both the caregiver and the patient 3. Device must be comfortable for the patient 4. Device should be easily understood and managed 5. Device must be efficient in use of time 6. Maintenance should be minimal
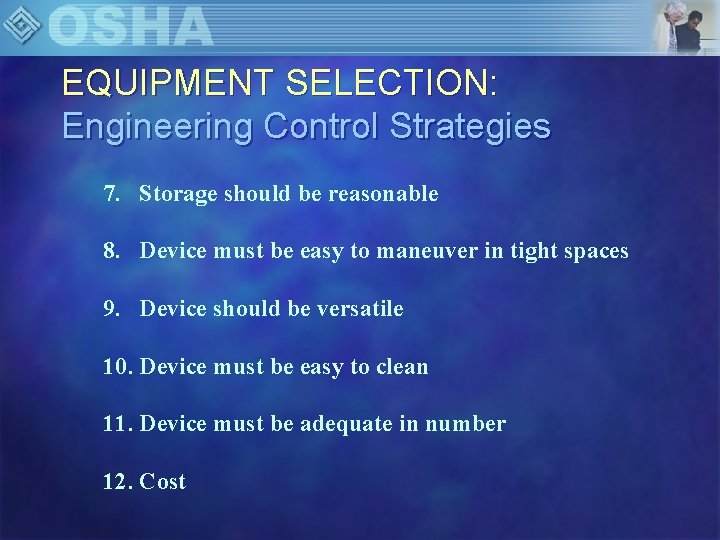
EQUIPMENT SELECTION: Engineering Control Strategies 7. Storage should be reasonable 8. Device must be easy to maneuver in tight spaces 9. Device should be versatile 10. Device must be easy to clean 11. Device must be adequate in number 12. Cost
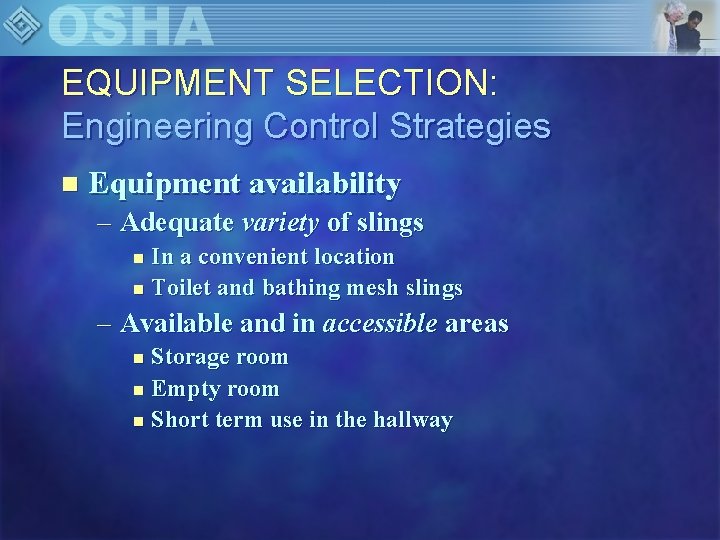
EQUIPMENT SELECTION: Engineering Control Strategies n Equipment availability – Adequate variety of slings In a convenient location n Toilet and bathing mesh slings n – Available and in accessible areas Storage room n Empty room n Short term use in the hallway n
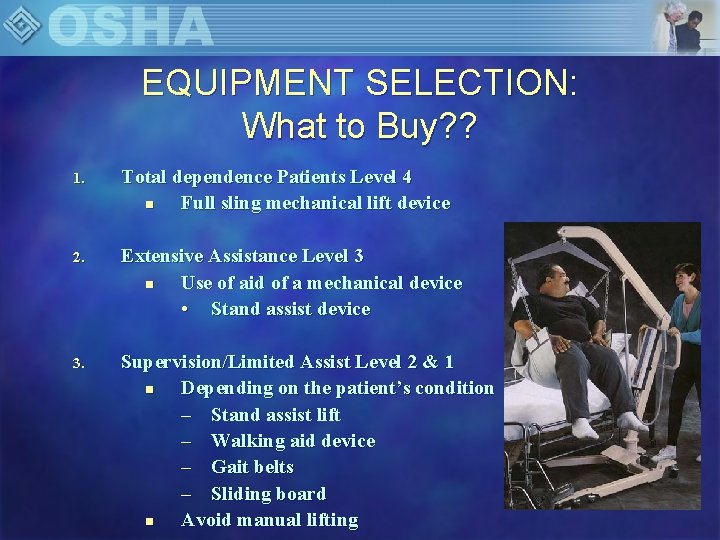
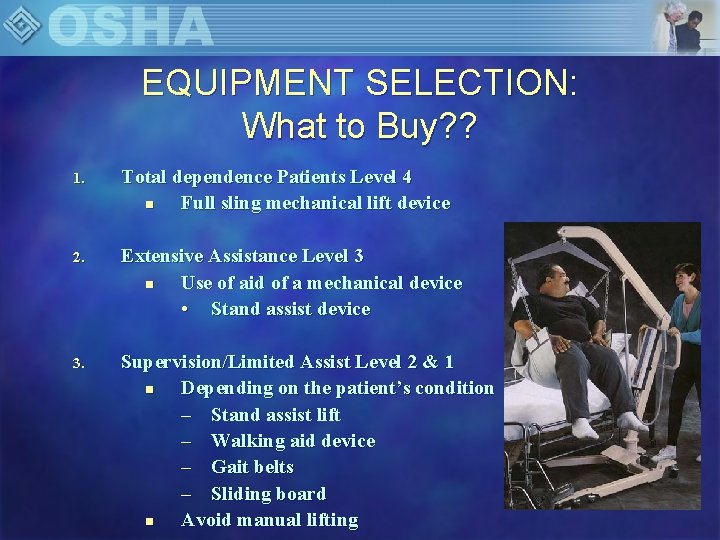
EQUIPMENT SELECTION: What to Buy? ? 1. Total dependence Patients Level 4 n Full sling mechanical lift device 2. Extensive Assistance Level 3 n Use of aid of a mechanical device • Stand assist device 3. Supervision/Limited Assist Level 2 & 1 n Depending on the patient’s condition – Stand assist lift – Walking aid device – Gait belts – Sliding board n Avoid manual lifting
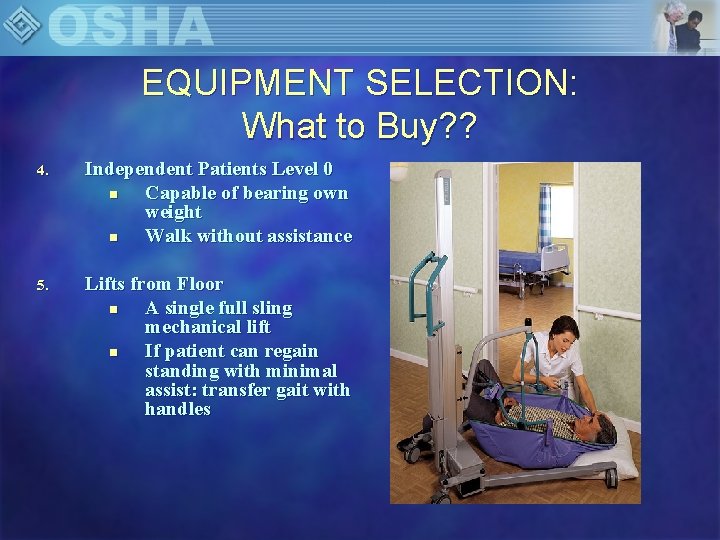
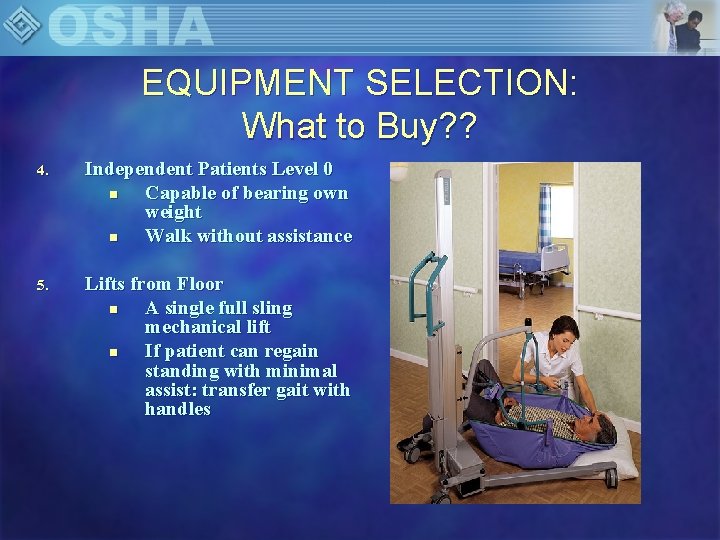
EQUIPMENT SELECTION: What to Buy? ? 4. Independent Patients Level 0 n Capable of bearing own weight n Walk without assistance 5. Lifts from Floor n A single full sling mechanical lift n If patient can regain standing with minimal assist: transfer gait with handles
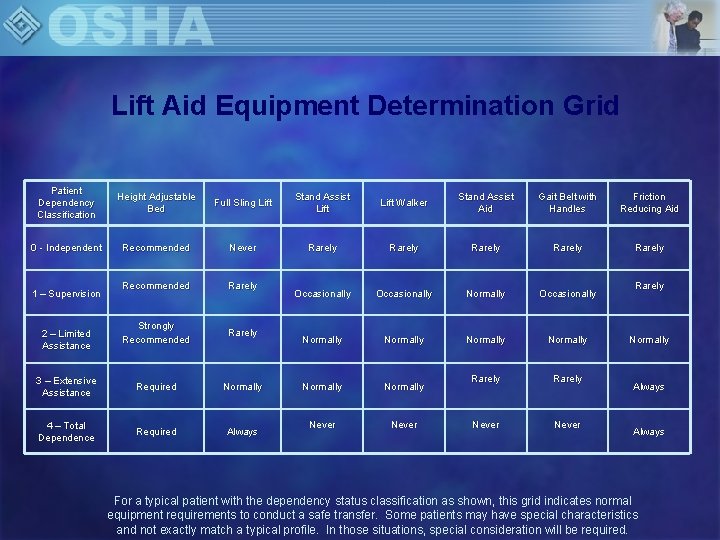
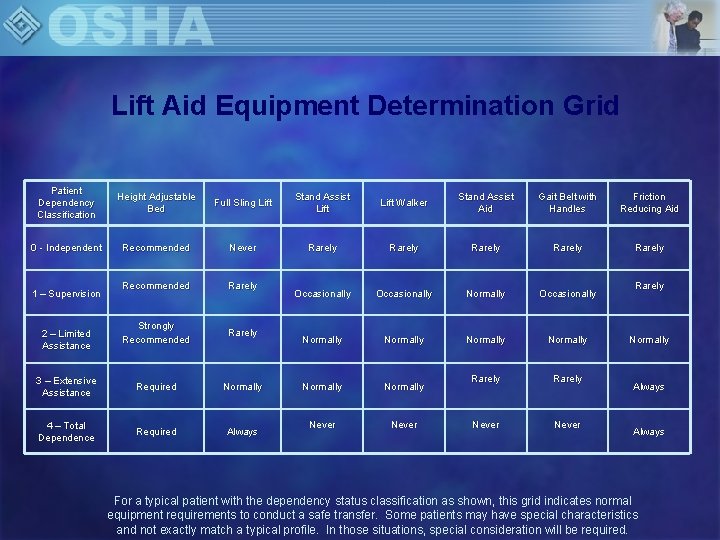
Lift Aid Equipment Determination Grid Patient Dependency Classification Height Adjustable Bed Full Sling Lift Stand Assist Lift Walker Stand Assist Aid Gait Belt with Handles Friction Reducing Aid 0 - Independent Recommended Never Rarely Rarely Recommended Rarely Occasionally Normally Occasionally Strongly Recommended Rarely Normally 3 – Extensive Assistance Required Normally Rarely 4 – Total Dependence Required Always Never 1 – Supervision 2 – Limited Assistance Rarely Normally Always For a typical patient with the dependency status classification as shown, this grid indicates normal equipment requirements to conduct a safe transfer. Some patients may have special characteristics and not exactly match a typical profile. In those situations, special consideration will be required.
EQUIPMENT SELECTION: What to Buy? ? 6. Repositioning – Bed: • Bed controls utilized • Trendelenberg positioning • Friction reducing devices – Chair: • Stand assist lift • Gait Belts • Hand slings
EQUIPMENT SELECTION: What to Buy? ? 7. Special Situations Devices • Bariatric patients ⇒ special equipment • Transfer chairs ⇒ stretcher chairs • Mechanical friction reducing • Sliding boards • Transfer belts • Special training
EQUIPMENT SELECTION: What to Buy? ? 8. Combative & Mentally Impaired Patients n n Use the appropriate lifting aid device Additional care providers as needed
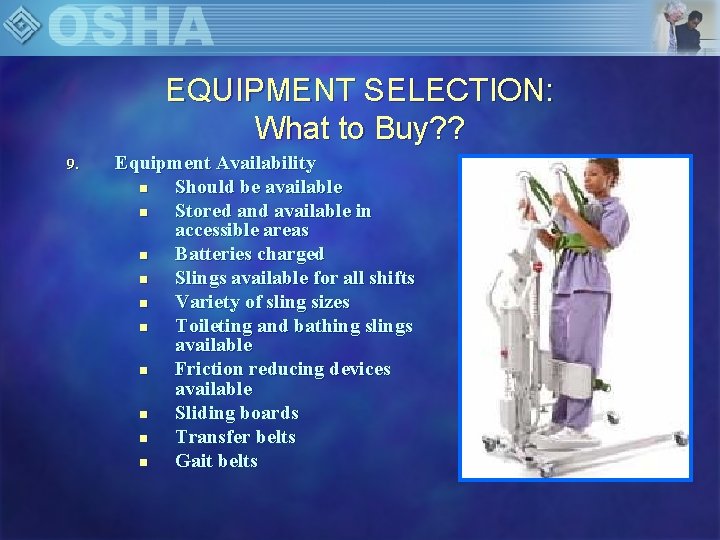
EQUIPMENT SELECTION: What to Buy? ? 9. Equipment Availability n Should be available n Stored and available in accessible areas n Batteries charged n Slings available for all shifts n Variety of sling sizes n Toileting and bathing slings available n Friction reducing devices available n Sliding boards n Transfer belts n Gait belts
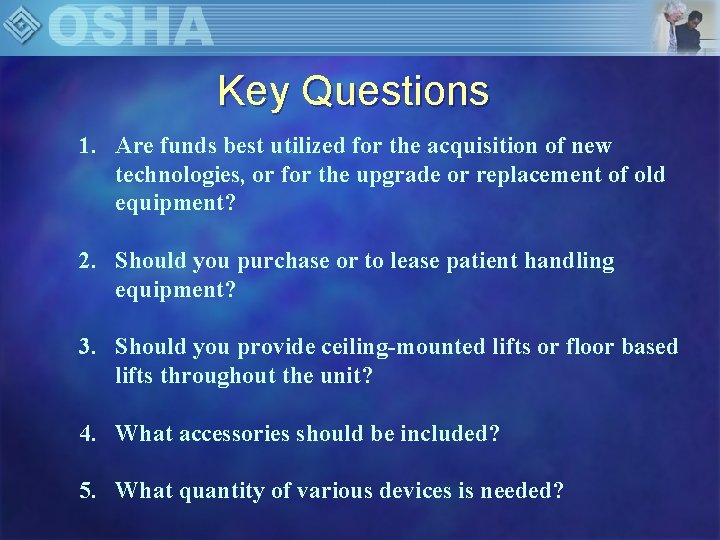
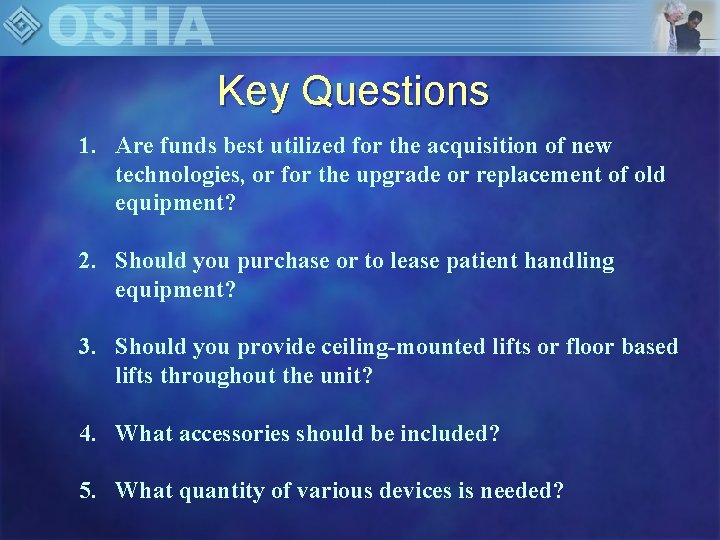
Key Questions 1. Are funds best utilized for the acquisition of new technologies, or for the upgrade or replacement of old equipment? 2. Should you purchase or to lease patient handling equipment? 3. Should you provide ceiling-mounted lifts or floor based lifts throughout the unit? 4. What accessories should be included? 5. What quantity of various devices is needed?
SAFE PATIENT HANDLING EQUIPMENT • Sliding Boards • Air Assisted lateral sliding aids • Friction reducing devices • Mechanical lateral transfer aids • Transfer chairs • Gait belts with handles • Powered full body sling lifts
SAFE PATIENT HANDLING EQUIPMENT • Powered standing assist and repositioning lifts • Standing assist and repositioning aids • Bed Improvements to support transfers • Dependency Chairs • Other ergonomic transfer devices
Monitor Results n Ongoing success of process – Established key indicators – Established time line
Information on OSHA’s Website – www. osha. gov OSHA Home Page OSHA Hospital/Nursing Home Pages OSHA Ergonomics Page
Other Resources Patient Safety Center Patient Care Ergonomics Resource Guide: Safe Patient Handling and Movement www. visn 8. med. va. gov/patientsafetycenter n CDC/NIOSH Safe Lifting and Movement of Nursing Home Residents, publication #2006 -117 www. cdc. gov/niosh n
QUESTIONS……………