Safe Medication Administration IV Calculations Pediatric dosages Reconstitution
- Slides: 45
Safe Medication Administration: IV Calculations, Pediatric dosages, Reconstitution Deborah M. Leveille, RN, MSN, CNL, CCRN
Parenteral Administration IV • Intravenous: Into the vein • Immediate effects, no absorption required • Sites: – – Cephalic vein, Antecubetal, basilic Hand or upper arm Cut-down (central line, VAD, PICC) Never radial, near wrist can cause nerve damage • Needle/gauge size: – 14 -25 gauge depending on size of vein, viscosity, rate of infusion, type of medication (irritating)
Parenteral Administration IV • Aseptic technique when inserting and maintaining IV (always swab port –” scrub the hub”- for 15 seconds before each use i. e. IVP, flushes, IVPB!) • Know rate of administration of drug • Compatability with IVF and other drugs infusing • Monitor for signs and symptoms of : – Phlebitis: inflammation of vein, redness, warmth, pain – Infiltration (extravasation): when the fluid passes into the tissue; pallor, edema, coolness, decreased IV flow
Parenteral Administration: IV (cont. ) • Never push medications through a difficult or clogged IV line • Know facility protocol for changing IV sites and primary tubing (i. e. q 72 hours), 2 nd tubing (or tubing used intermittently) usually 24 hrs • Always make sure tubing is primed • Know which medications need filters: TPN, Lipids, Amiodarone (some facilities require filters with any central line) • Never administer medication that is cloudy/discolored or has precipitate or exceeds expiration date.
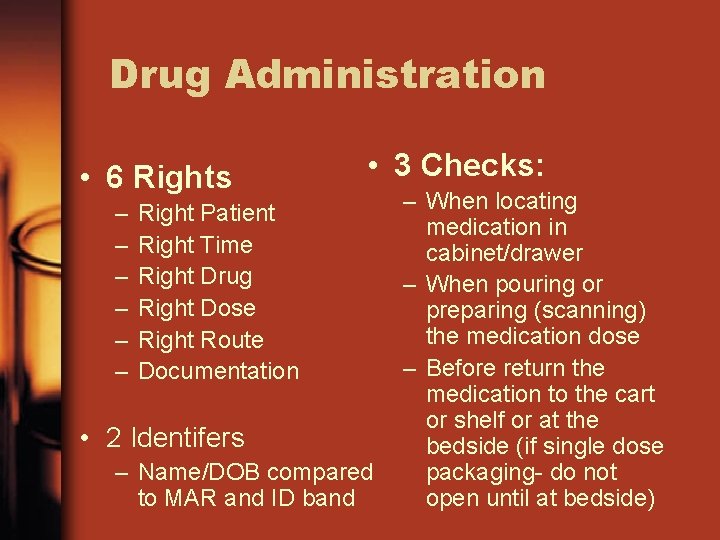
Drug Administration • 6 Rights – – – • 3 Checks: Right Patient Right Time Right Drug Right Dose Right Route Documentation • 2 Identifers – Name/DOB compared to MAR and ID band – When locating medication in cabinet/drawer – When pouring or preparing (scanning) the medication dose – Before return the medication to the cart or shelf or at the bedside (if single dose packaging- do not open until at bedside)
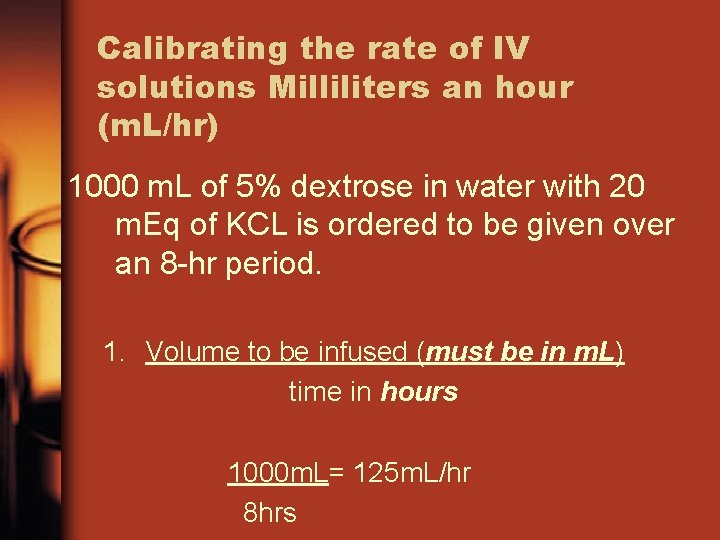
Calibrating the rate of IV solutions Milliliters an hour (m. L/hr) 1000 m. L of 5% dextrose in water with 20 m. Eq of KCL is ordered to be given over an 8 -hr period. 1. Volume to be infused (must be in m. L) time in hours 1000 m. L= 125 m. L/hr 8 hrs
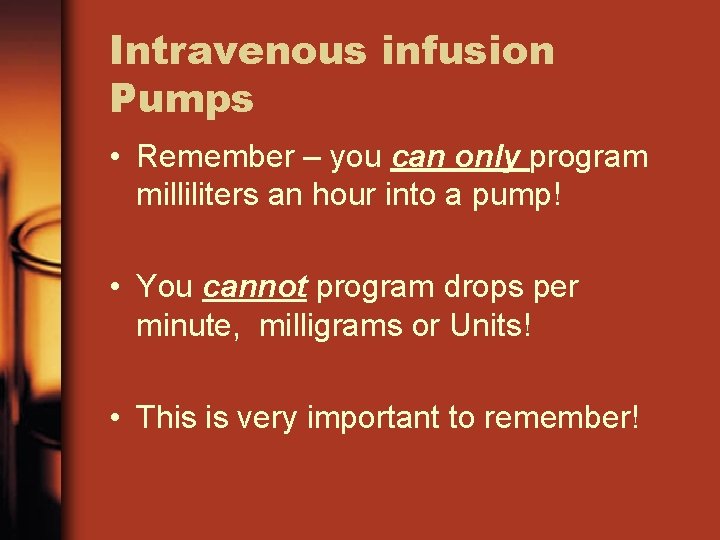
Intravenous infusion Pumps • Remember – you can only program milliliters an hour into a pump! • You cannot program drops per minute, milligrams or Units! • This is very important to remember!
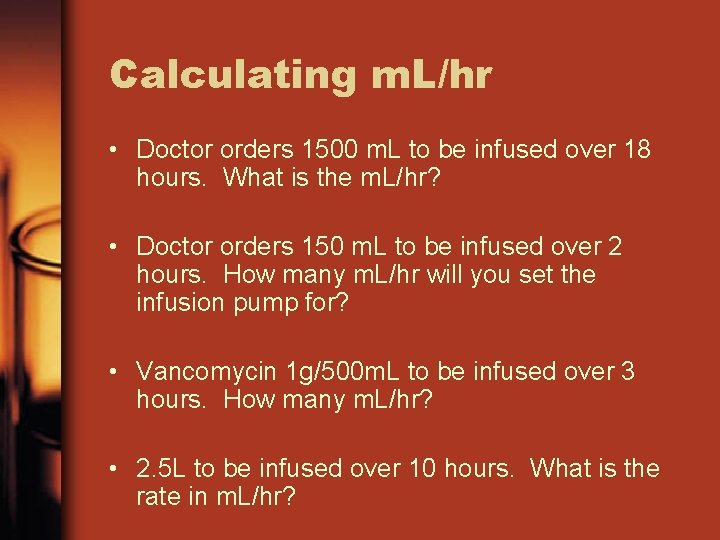
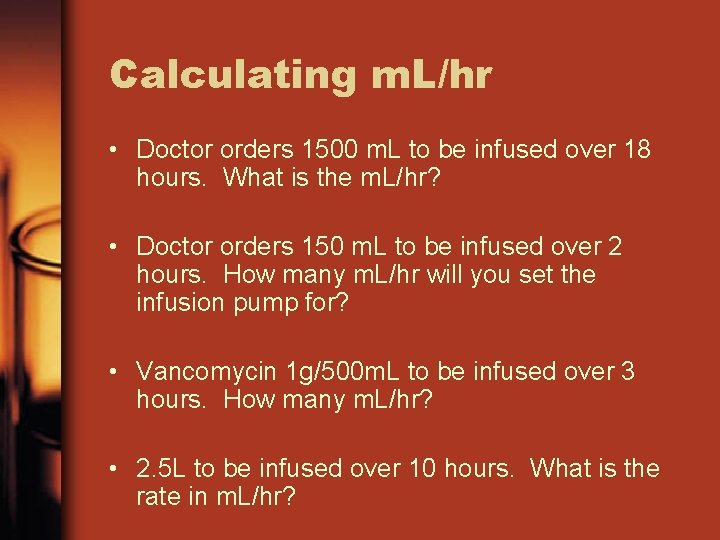
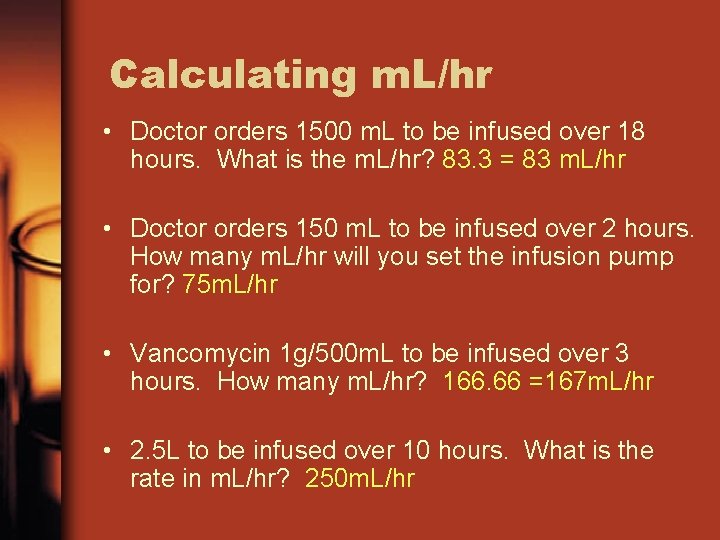
Calculating m. L/hr • Doctor orders 1500 m. L to be infused over 18 hours. What is the m. L/hr? • Doctor orders 150 m. L to be infused over 2 hours. How many m. L/hr will you set the infusion pump for? • Vancomycin 1 g/500 m. L to be infused over 3 hours. How many m. L/hr? • 2. 5 L to be infused over 10 hours. What is the rate in m. L/hr?
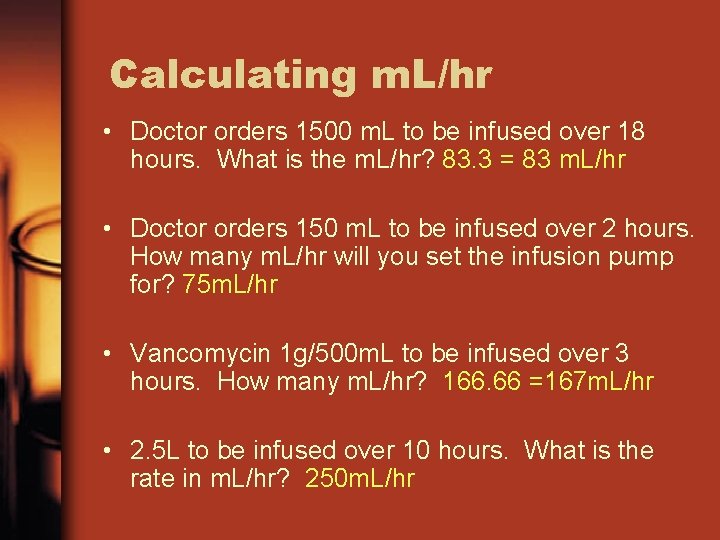
Calculating m. L/hr • Doctor orders 1500 m. L to be infused over 18 hours. What is the m. L/hr? 83. 3 = 83 m. L/hr • Doctor orders 150 m. L to be infused over 2 hours. How many m. L/hr will you set the infusion pump for? 75 m. L/hr • Vancomycin 1 g/500 m. L to be infused over 3 hours. How many m. L/hr? 166. 66 =167 m. L/hr • 2. 5 L to be infused over 10 hours. What is the rate in m. L/hr? 250 m. L/hr
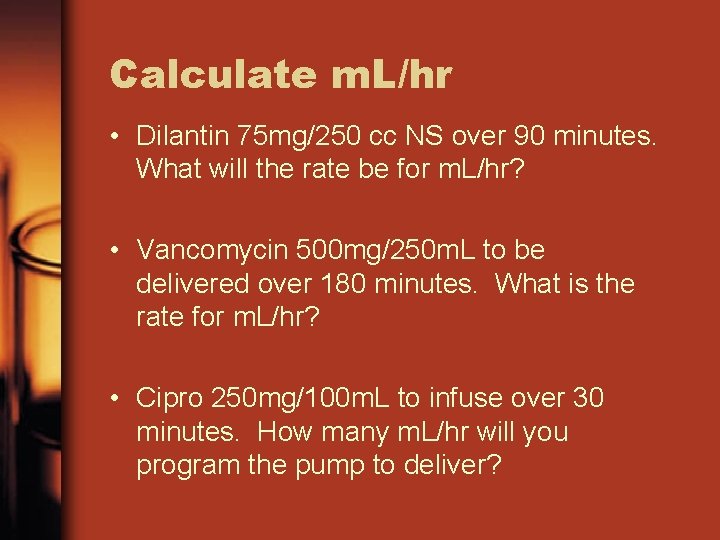
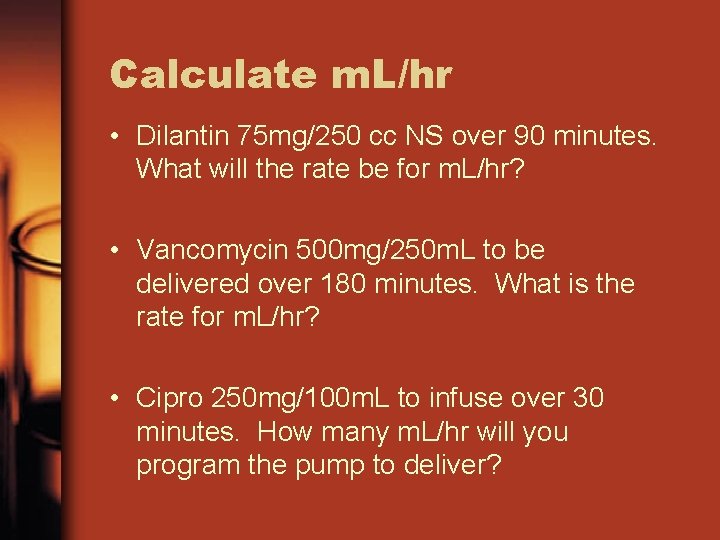
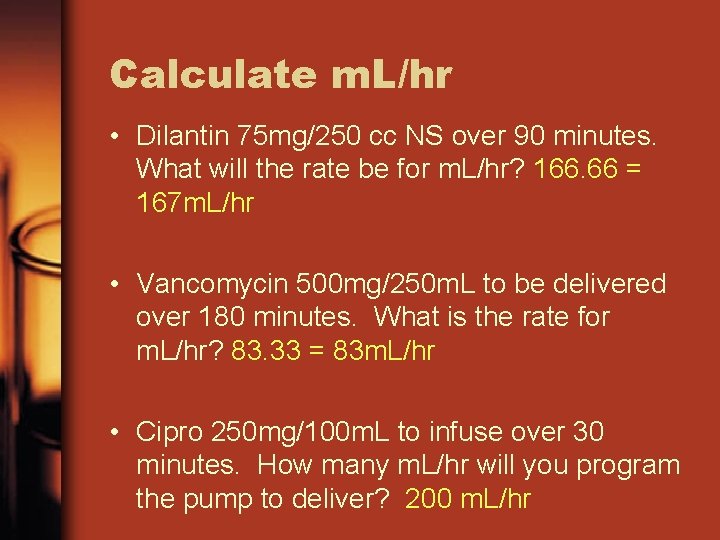
Calculate m. L/hr • Dilantin 75 mg/250 cc NS over 90 minutes. What will the rate be for m. L/hr? • Vancomycin 500 mg/250 m. L to be delivered over 180 minutes. What is the rate for m. L/hr? • Cipro 250 mg/100 m. L to infuse over 30 minutes. How many m. L/hr will you program the pump to deliver?
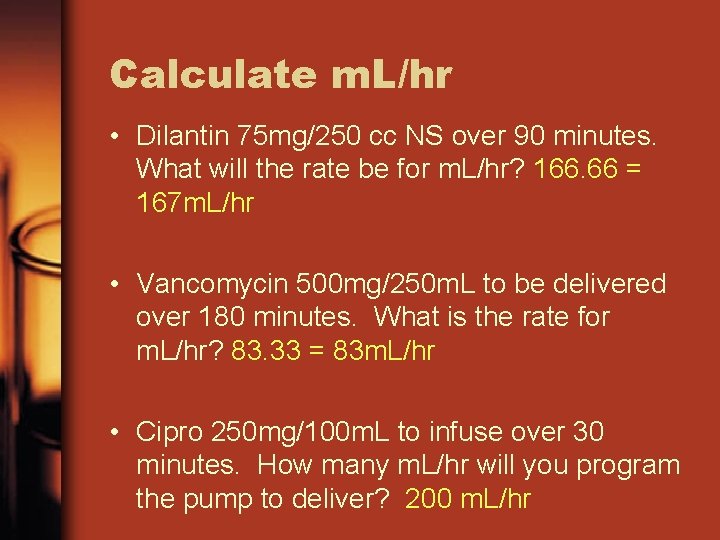
Calculate m. L/hr • Dilantin 75 mg/250 cc NS over 90 minutes. What will the rate be for m. L/hr? 166. 66 = 167 m. L/hr • Vancomycin 500 mg/250 m. L to be delivered over 180 minutes. What is the rate for m. L/hr? 83. 33 = 83 m. L/hr • Cipro 250 mg/100 m. L to infuse over 30 minutes. How many m. L/hr will you program the pump to deliver? 200 m. L/hr
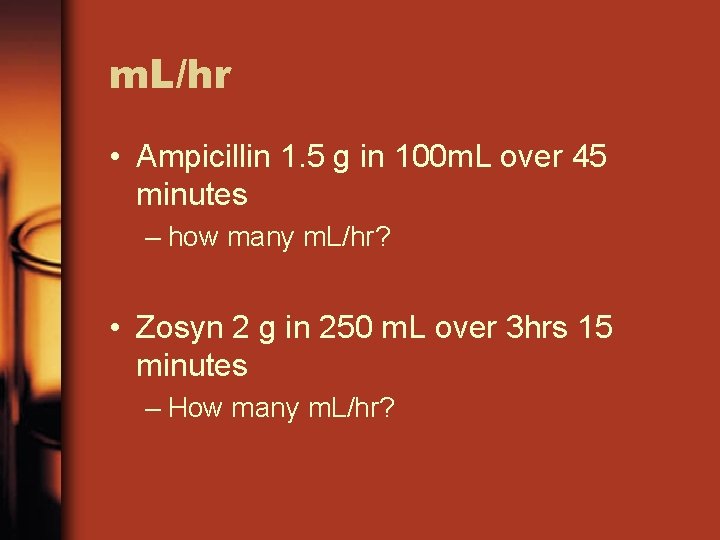
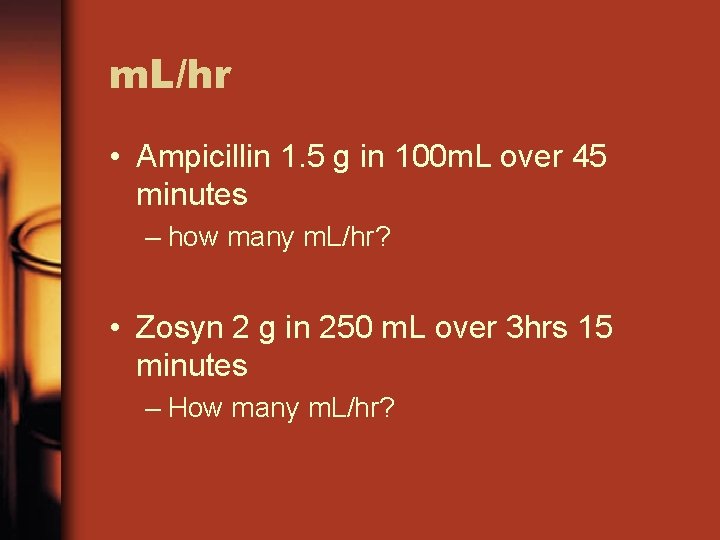
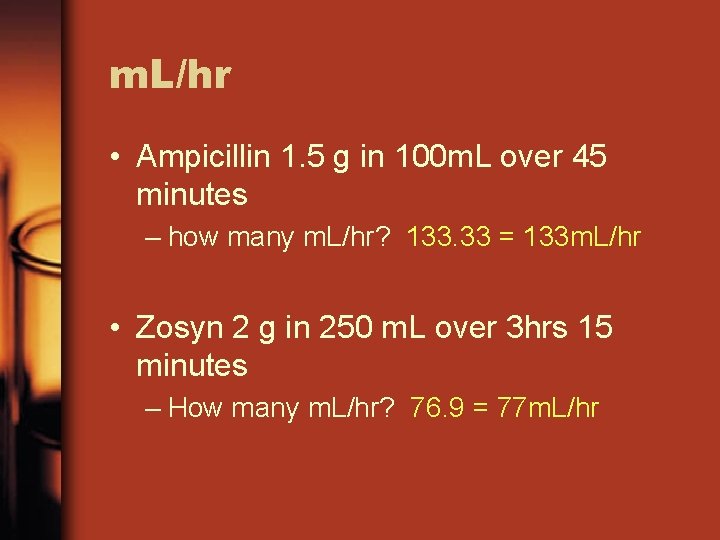
m. L/hr • Ampicillin 1. 5 g in 100 m. L over 45 minutes – how many m. L/hr? • Zosyn 2 g in 250 m. L over 3 hrs 15 minutes – How many m. L/hr?
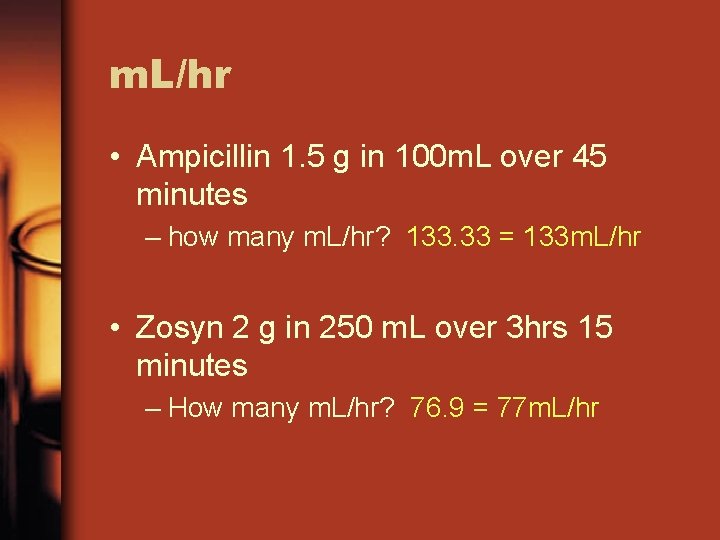
m. L/hr • Ampicillin 1. 5 g in 100 m. L over 45 minutes – how many m. L/hr? 133. 33 = 133 m. L/hr • Zosyn 2 g in 250 m. L over 3 hrs 15 minutes – How many m. L/hr? 76. 9 = 77 m. L/hr
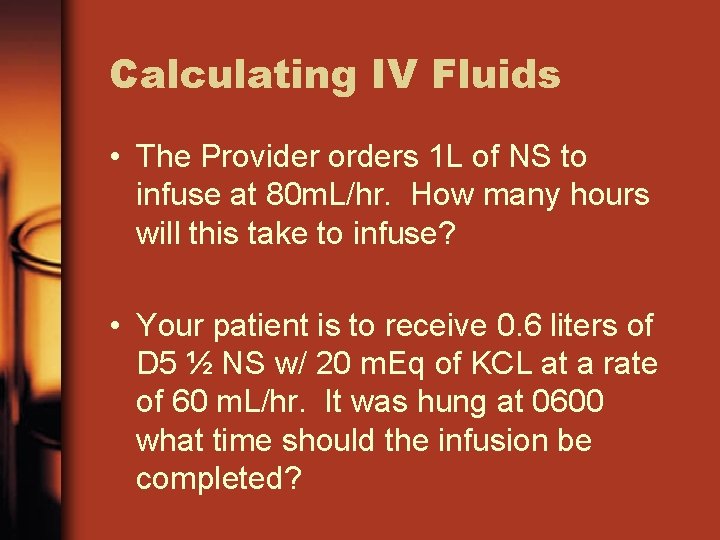
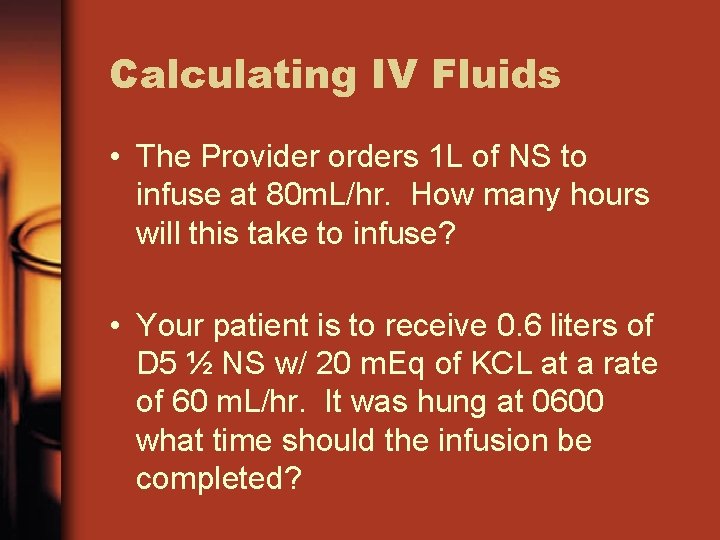
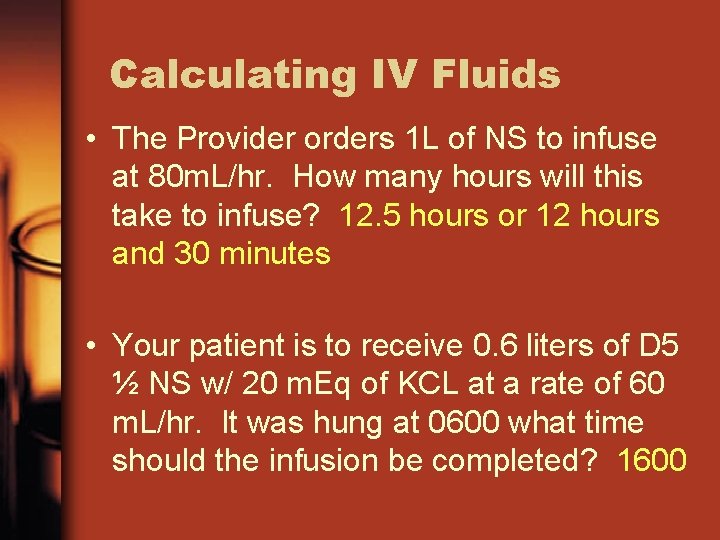
Calculating IV Fluids • The Provider orders 1 L of NS to infuse at 80 m. L/hr. How many hours will this take to infuse? • Your patient is to receive 0. 6 liters of D 5 ½ NS w/ 20 m. Eq of KCL at a rate of 60 m. L/hr. It was hung at 0600 what time should the infusion be completed?
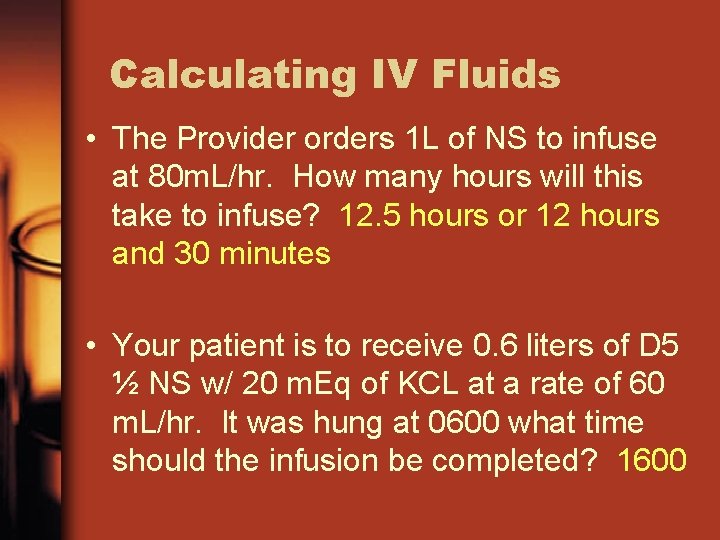
Calculating IV Fluids • The Provider orders 1 L of NS to infuse at 80 m. L/hr. How many hours will this take to infuse? 12. 5 hours or 12 hours and 30 minutes • Your patient is to receive 0. 6 liters of D 5 ½ NS w/ 20 m. Eq of KCL at a rate of 60 m. L/hr. It was hung at 0600 what time should the infusion be completed? 1600
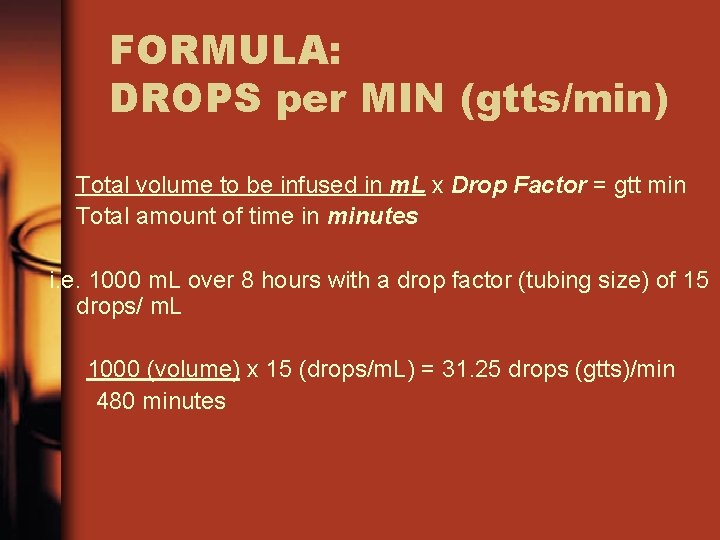
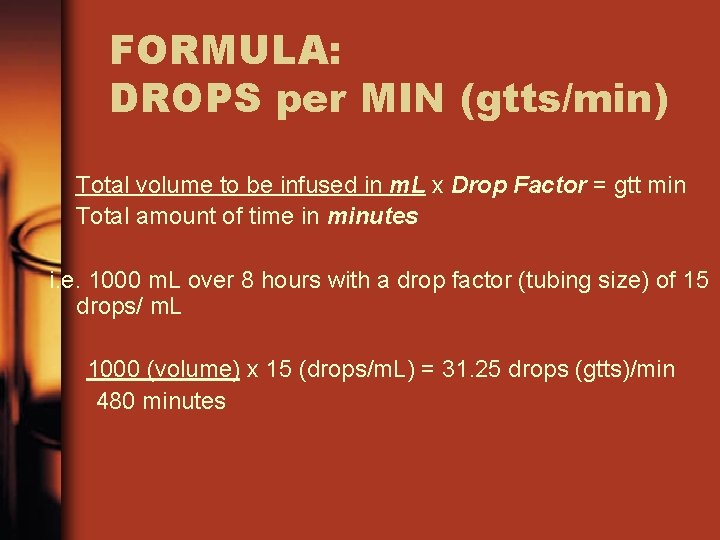
FORMULA: DROPS per MIN (gtts/min) Total volume to be infused in m. L x Drop Factor = gtt min Total amount of time in minutes i. e. 1000 m. L over 8 hours with a drop factor (tubing size) of 15 drops/ m. L 1000 (volume) x 15 (drops/m. L) = 31. 25 drops (gtts)/min 480 minutes
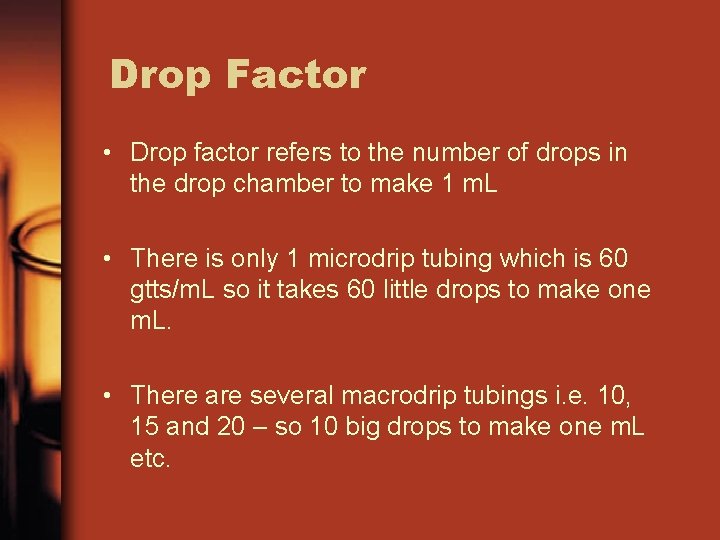
Drop Factor • Drop factor refers to the number of drops in the drop chamber to make 1 m. L • There is only 1 microdrip tubing which is 60 gtts/m. L so it takes 60 little drops to make one m. L. • There are several macrodrip tubings i. e. 10, 15 and 20 – so 10 big drops to make one m. L etc.
Calculating Drops per Min • 500 m. L over 30 minutes with a drop set (tubing size) of 15 drops /m. L • 50 m. L over 15 minutes with a drop set of 15 drops/m. L • 100 m. L over 20 minutes with a drop set of 15 drops/m. L
Calculating Drops per Min • 500 m. L over 30 minutes with a drop set (tubing size) of 15 drops /m. L. How many gtts/min? 250 gtts/min • 50 m. L over 15 minutes with a drop set of 15 drops/m. L. How many gtts/min? 50 gtts/min • 100 m. L over 20 minutes with a drop set of 15 drops/m. L. How many gtts/min? 75 gtts/min
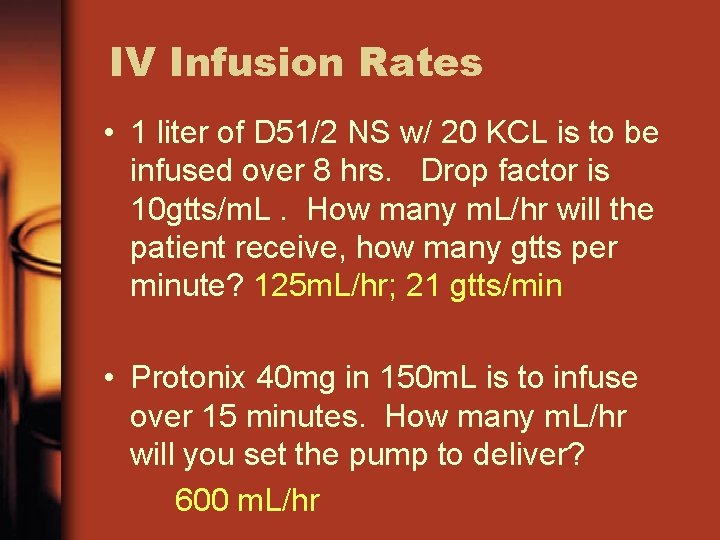
IV Infusion Rates Pretest • 1 liter of D 51/2 NS w/ 20 KCL is to be infused over 8 hrs. Drop factor is 10 gtts/m. L. How many m. L/hr will the patient receive, how many gtts per minute? • Protonix 40 mg in 150 m. L is to infuse over 15 minutes. How many m. L/hr will you set the pump to deliver?
IV Infusion Rates • 1 liter of D 51/2 NS w/ 20 KCL is to be infused over 8 hrs. Drop factor is 10 gtts/m. L. How many m. L/hr will the patient receive, how many gtts per minute? 125 m. L/hr; 21 gtts/min • Protonix 40 mg in 150 m. L is to infuse over 15 minutes. How many m. L/hr will you set the pump to deliver? 600 m. L/hr
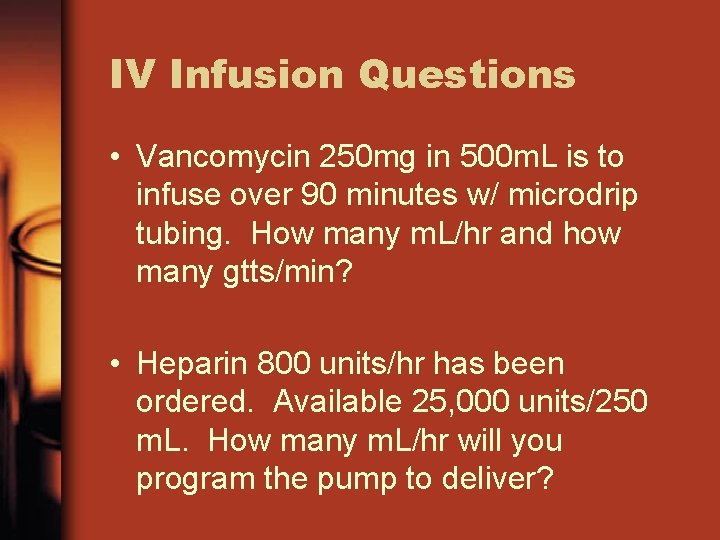
IV Infusion Questions • Vancomycin 250 mg in 500 m. L is to infuse over 90 minutes w/ microdrip tubing. How many m. L/hr and how many gtts/min? • Heparin 800 units/hr has been ordered. Available 25, 000 units/250 m. L. How many m. L/hr will you program the pump to deliver?
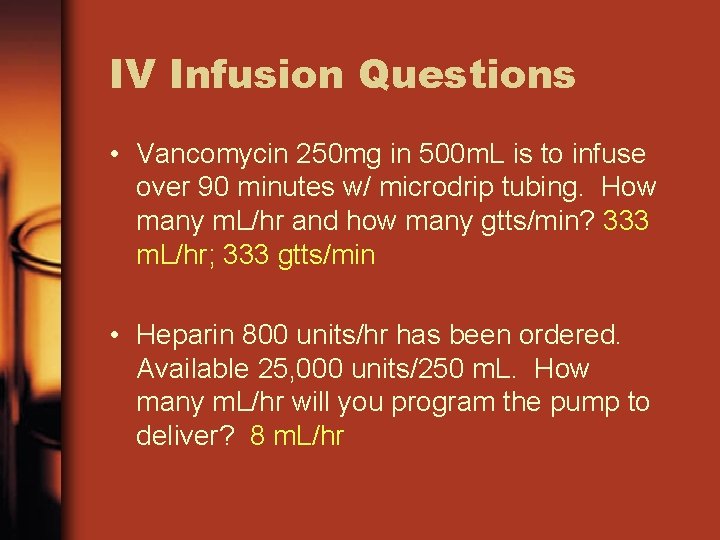
IV Infusion Questions • Vancomycin 250 mg in 500 m. L is to infuse over 90 minutes w/ microdrip tubing. How many m. L/hr and how many gtts/min? 333 m. L/hr; 333 gtts/min • Heparin 800 units/hr has been ordered. Available 25, 000 units/250 m. L. How many m. L/hr will you program the pump to deliver? 8 m. L/hr
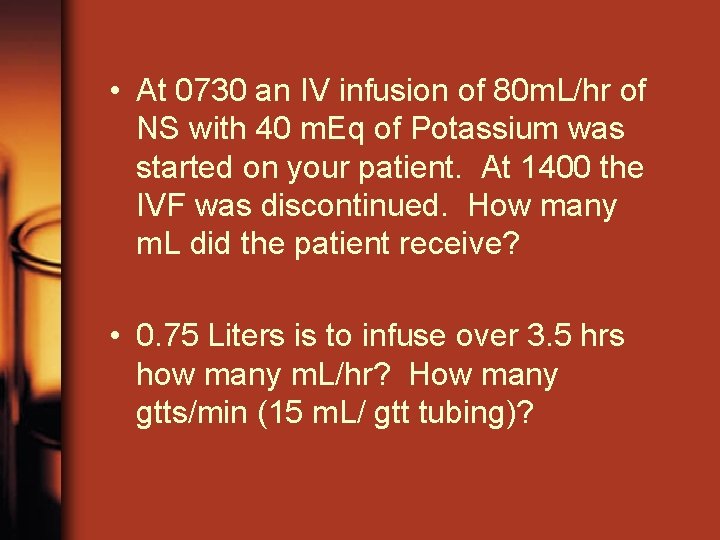
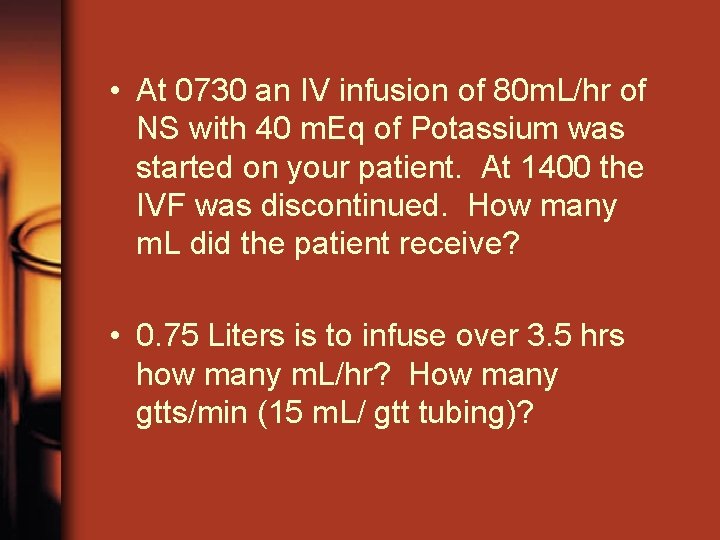
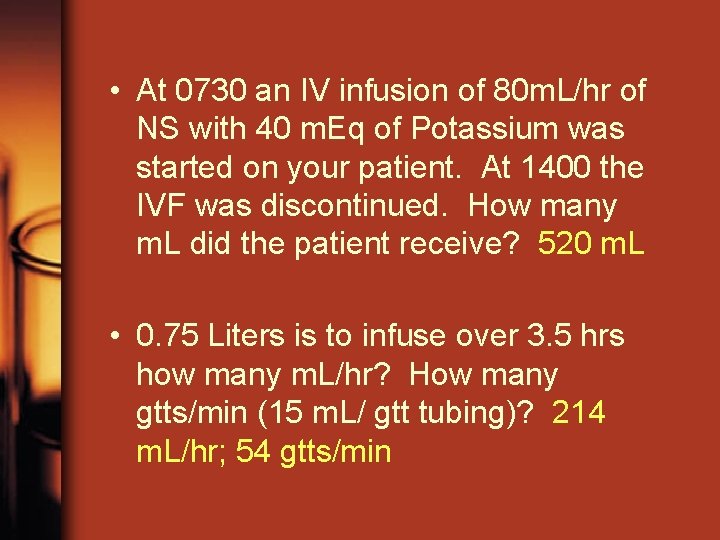
• At 0730 an IV infusion of 80 m. L/hr of NS with 40 m. Eq of Potassium was started on your patient. At 1400 the IVF was discontinued. How many m. L did the patient receive? • 0. 75 Liters is to infuse over 3. 5 hrs how many m. L/hr? How many gtts/min (15 m. L/ gtt tubing)?
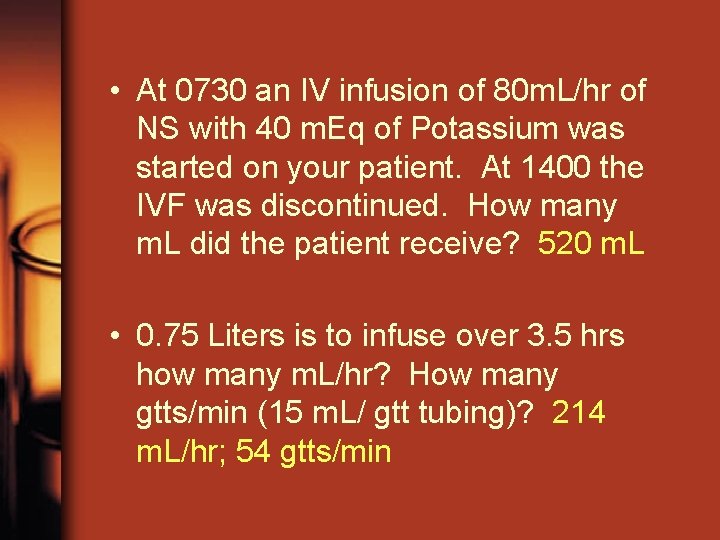
• At 0730 an IV infusion of 80 m. L/hr of NS with 40 m. Eq of Potassium was started on your patient. At 1400 the IVF was discontinued. How many m. L did the patient receive? 520 m. L • 0. 75 Liters is to infuse over 3. 5 hrs how many m. L/hr? How many gtts/min (15 m. L/ gtt tubing)? 214 m. L/hr; 54 gtts/min
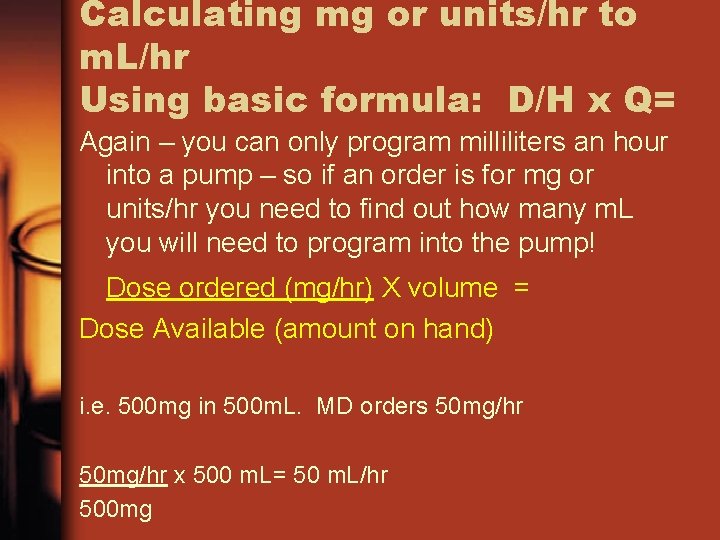
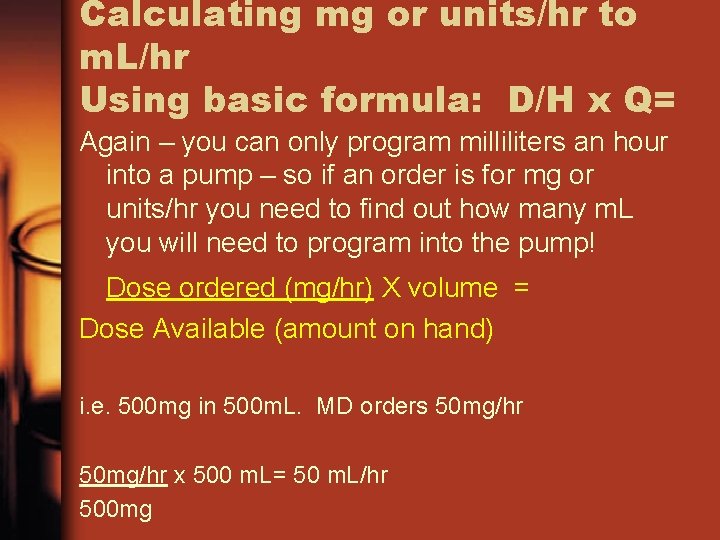
Calculating mg or units/hr to m. L/hr Using basic formula: D/H x Q= Again – you can only program milliliters an hour into a pump – so if an order is for mg or units/hr you need to find out how many m. L you will need to program into the pump! Dose ordered (mg/hr) X volume = Dose Available (amount on hand) i. e. 500 mg in 500 m. L. MD orders 50 mg/hr x 500 m. L= 50 m. L/hr 500 mg
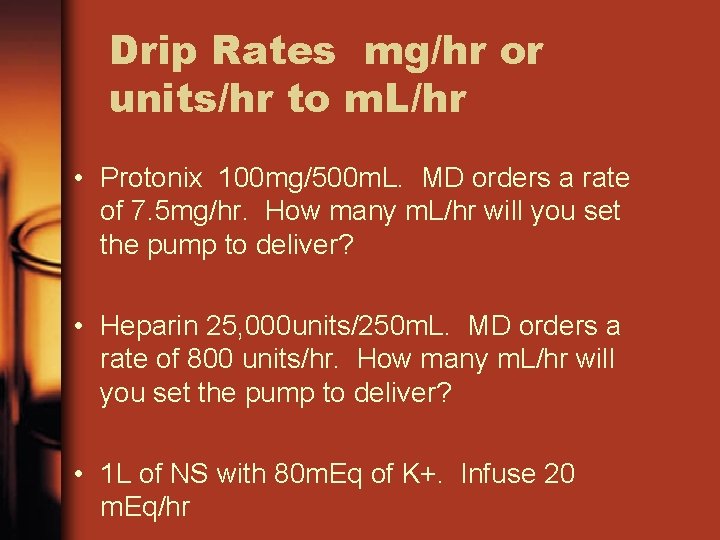
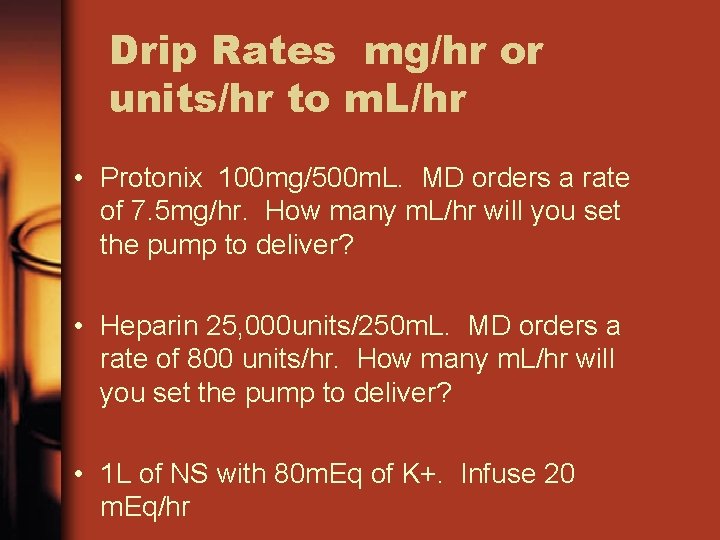
Drip Rates mg/hr or units/hr to m. L/hr • Protonix 100 mg/500 m. L. MD orders a rate of 7. 5 mg/hr. How many m. L/hr will you set the pump to deliver? • Heparin 25, 000 units/250 m. L. MD orders a rate of 800 units/hr. How many m. L/hr will you set the pump to deliver? • 1 L of NS with 80 m. Eq of K+. Infuse 20 m. Eq/hr
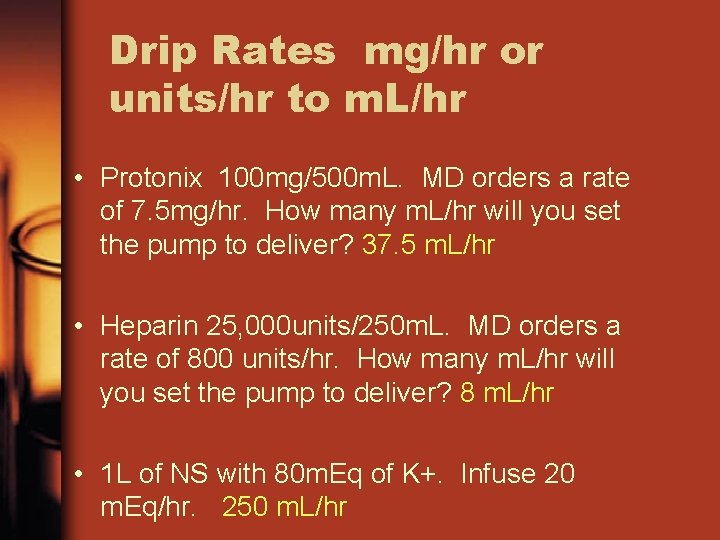
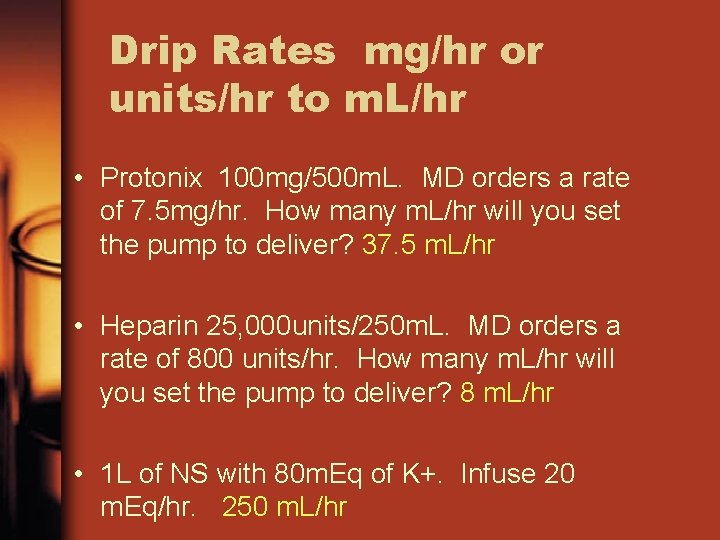
Drip Rates mg/hr or units/hr to m. L/hr • Protonix 100 mg/500 m. L. MD orders a rate of 7. 5 mg/hr. How many m. L/hr will you set the pump to deliver? 37. 5 m. L/hr • Heparin 25, 000 units/250 m. L. MD orders a rate of 800 units/hr. How many m. L/hr will you set the pump to deliver? 8 m. L/hr • 1 L of NS with 80 m. Eq of K+. Infuse 20 m. Eq/hr. 250 m. L/hr
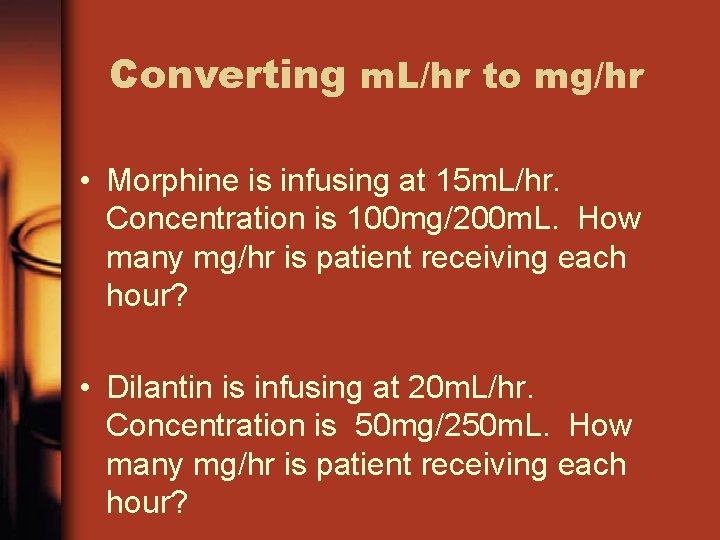
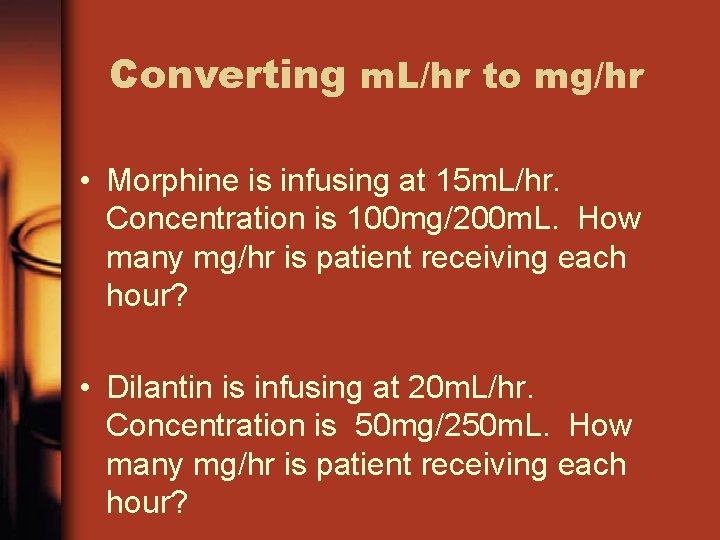
Converting m. L/hr to mg/hr • Morphine is infusing at 15 m. L/hr. Concentration is 100 mg/200 m. L. How many mg/hr is patient receiving each hour? • Dilantin is infusing at 20 m. L/hr. Concentration is 50 mg/250 m. L. How many mg/hr is patient receiving each hour?
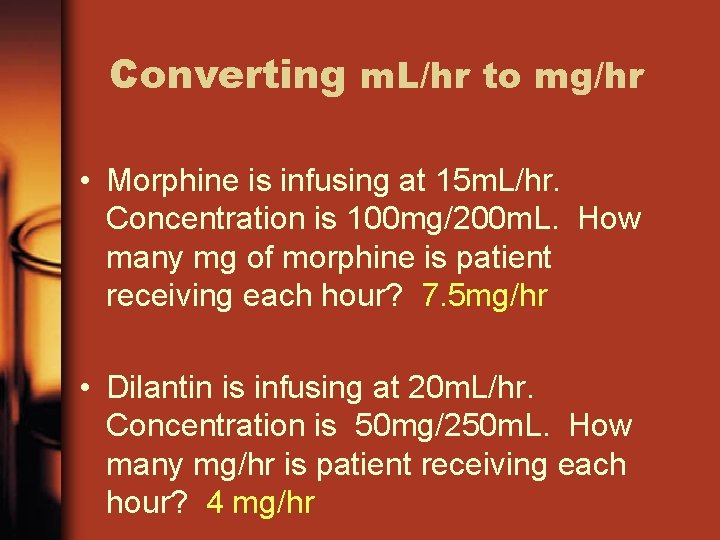
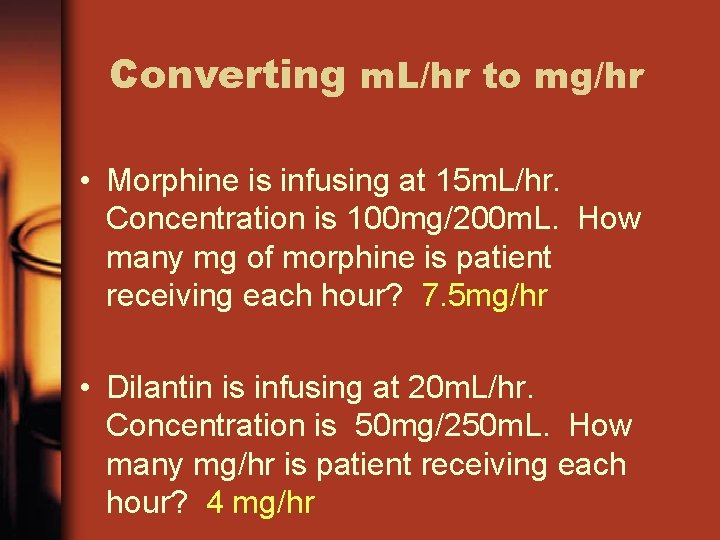
Converting m. L/hr to mg/hr • Morphine is infusing at 15 m. L/hr. Concentration is 100 mg/200 m. L. How many mg of morphine is patient receiving each hour? 7. 5 mg/hr • Dilantin is infusing at 20 m. L/hr. Concentration is 50 mg/250 m. L. How many mg/hr is patient receiving each hour? 4 mg/hr
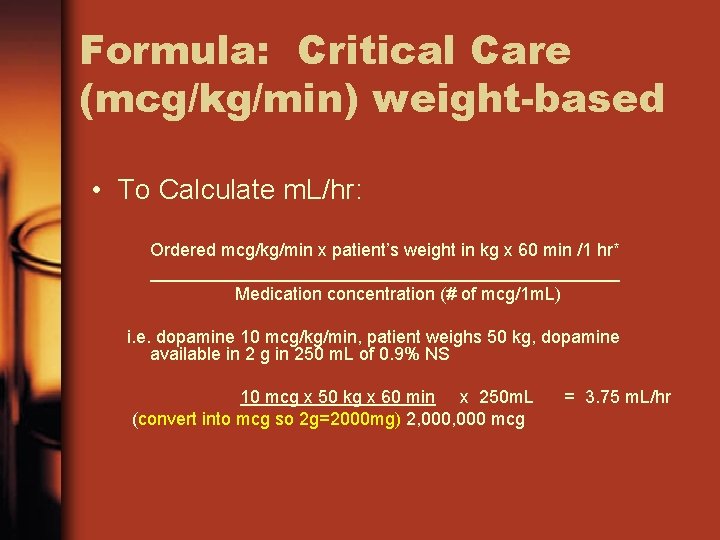
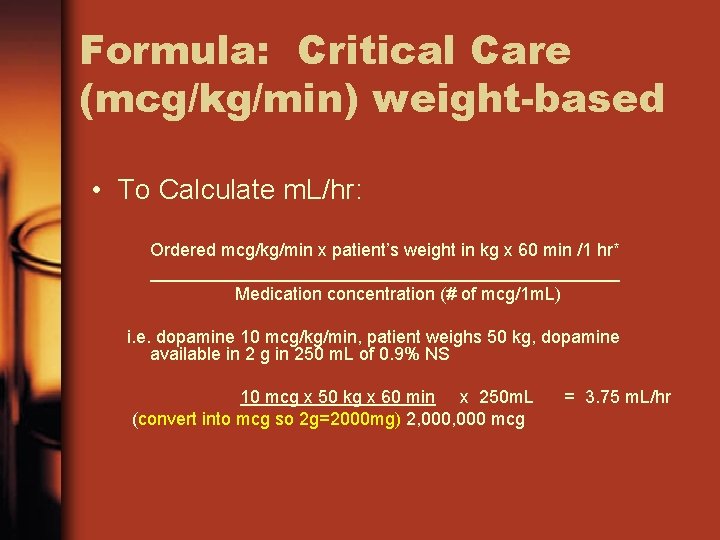
Formula: Critical Care (mcg/kg/min) weight-based • To Calculate m. L/hr: Ordered mcg/kg/min x patient’s weight in kg x 60 min /1 hr* ________________________ Medication concentration (# of mcg/1 m. L) i. e. dopamine 10 mcg/kg/min, patient weighs 50 kg, dopamine available in 2 g in 250 m. L of 0. 9% NS 10 mcg x 50 kg x 60 min x 250 m. L (convert into mcg so 2 g=2000 mg) 2, 000 mcg = 3. 75 m. L/hr
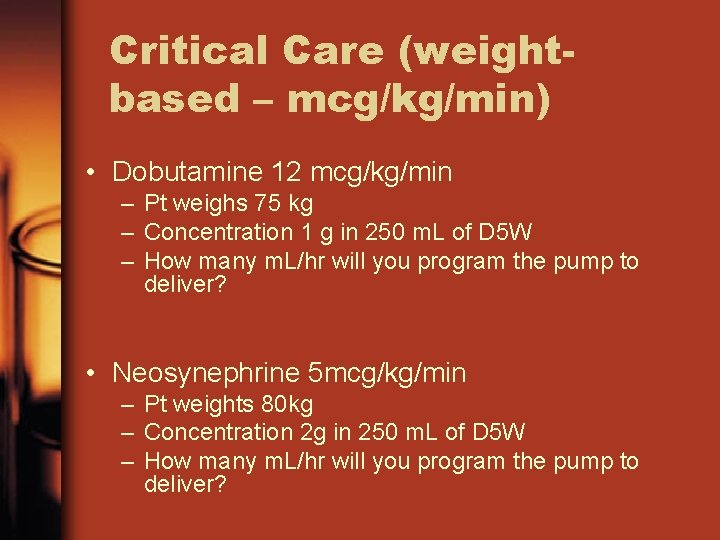
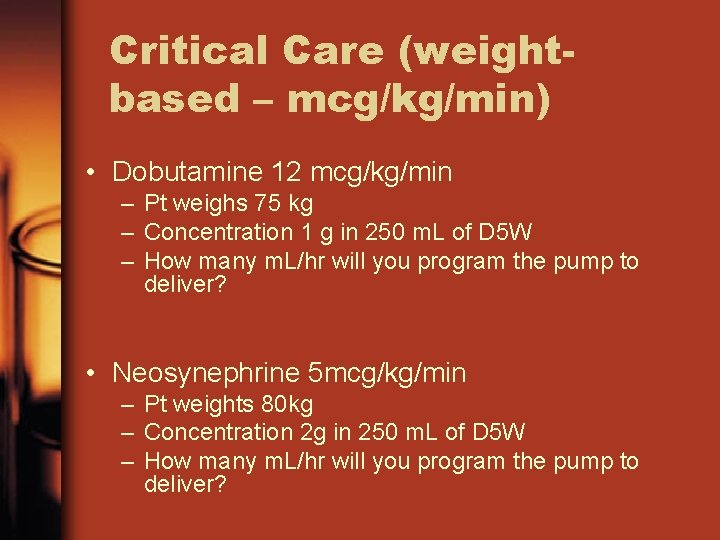
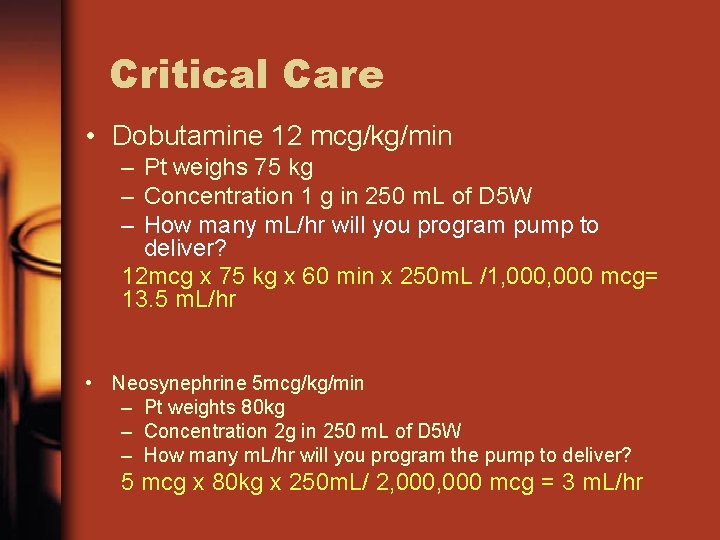
Critical Care (weightbased – mcg/kg/min) • Dobutamine 12 mcg/kg/min – Pt weighs 75 kg – Concentration 1 g in 250 m. L of D 5 W – How many m. L/hr will you program the pump to deliver? • Neosynephrine 5 mcg/kg/min – Pt weights 80 kg – Concentration 2 g in 250 m. L of D 5 W – How many m. L/hr will you program the pump to deliver?
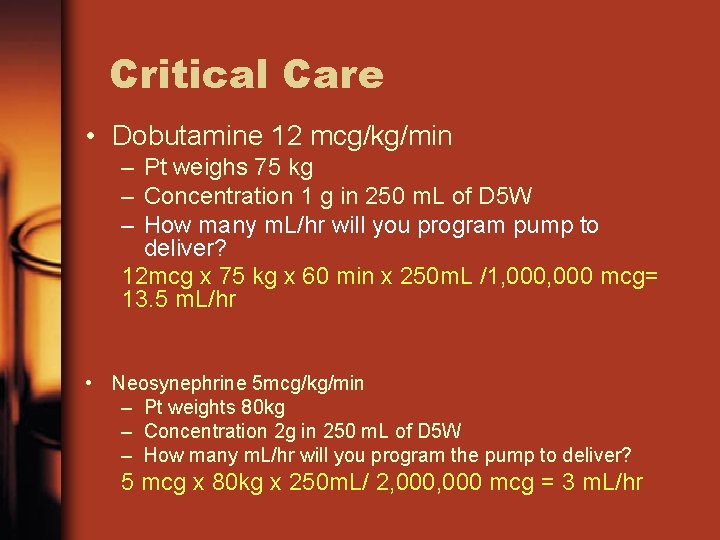
Critical Care • Dobutamine 12 mcg/kg/min – Pt weighs 75 kg – Concentration 1 g in 250 m. L of D 5 W – How many m. L/hr will you program pump to deliver? 12 mcg x 75 kg x 60 min x 250 m. L /1, 000 mcg= 13. 5 m. L/hr • Neosynephrine 5 mcg/kg/min – Pt weights 80 kg – Concentration 2 g in 250 m. L of D 5 W – How many m. L/hr will you program the pump to deliver? 5 mcg x 80 kg x 250 m. L/ 2, 000 mcg = 3 m. L/hr
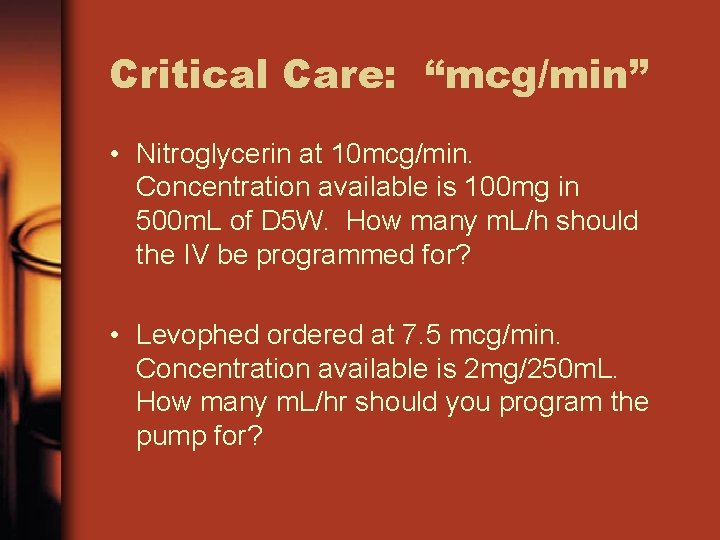
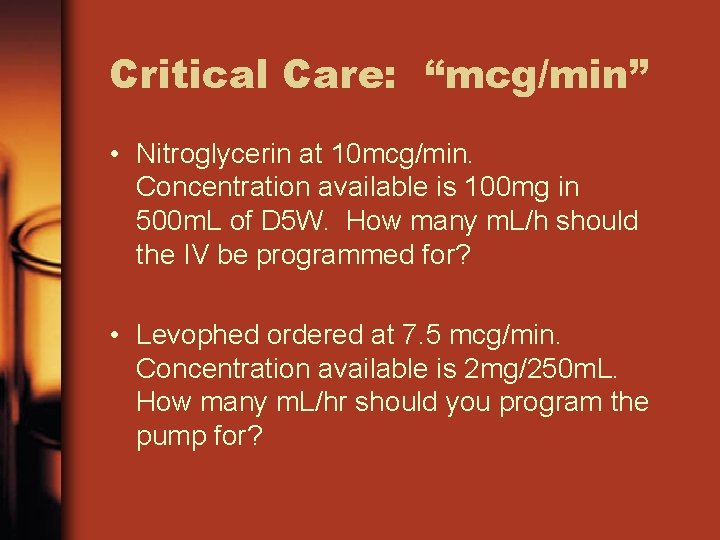
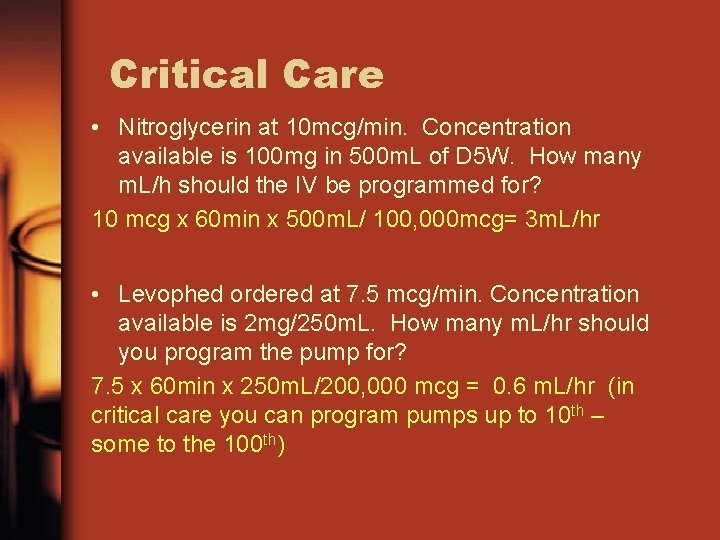
Critical Care: “mcg/min” • Nitroglycerin at 10 mcg/min. Concentration available is 100 mg in 500 m. L of D 5 W. How many m. L/h should the IV be programmed for? • Levophed ordered at 7. 5 mcg/min. Concentration available is 2 mg/250 m. L. How many m. L/hr should you program the pump for?
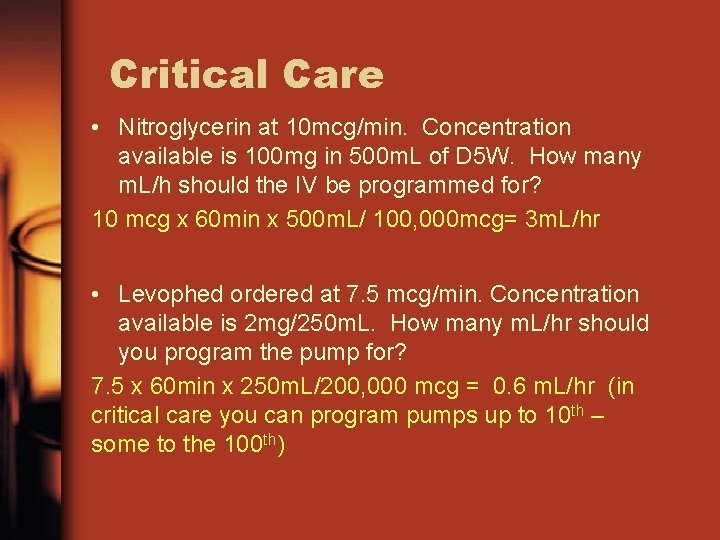
Critical Care • Nitroglycerin at 10 mcg/min. Concentration available is 100 mg in 500 m. L of D 5 W. How many m. L/h should the IV be programmed for? 10 mcg x 60 min x 500 m. L/ 100, 000 mcg= 3 m. L/hr • Levophed ordered at 7. 5 mcg/min. Concentration available is 2 mg/250 m. L. How many m. L/hr should you program the pump for? 7. 5 x 60 min x 250 m. L/200, 000 mcg = 0. 6 m. L/hr (in critical care you can program pumps up to 10 th – some to the 100 th)
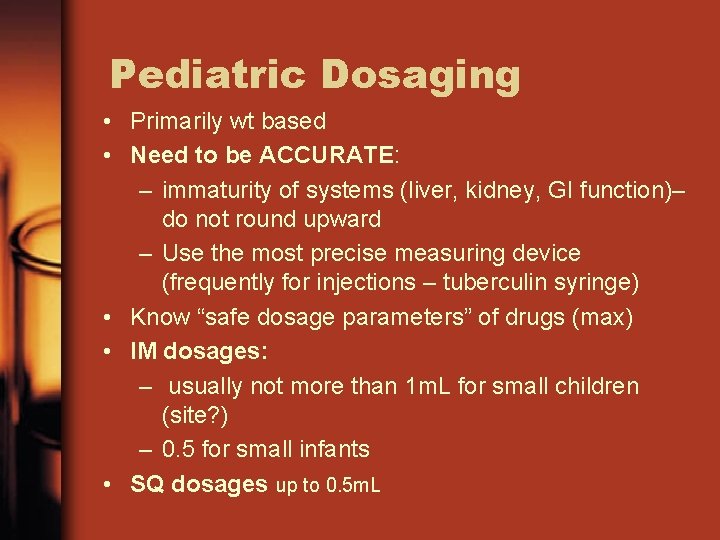
Pediatric Dosaging • Primarily wt based • Need to be ACCURATE: – immaturity of systems (liver, kidney, GI function)– do not round upward – Use the most precise measuring device (frequently for injections – tuberculin syringe) • Know “safe dosage parameters” of drugs (max) • IM dosages: – usually not more than 1 m. L for small children (site? ) – 0. 5 for small infants • SQ dosages up to 0. 5 m. L
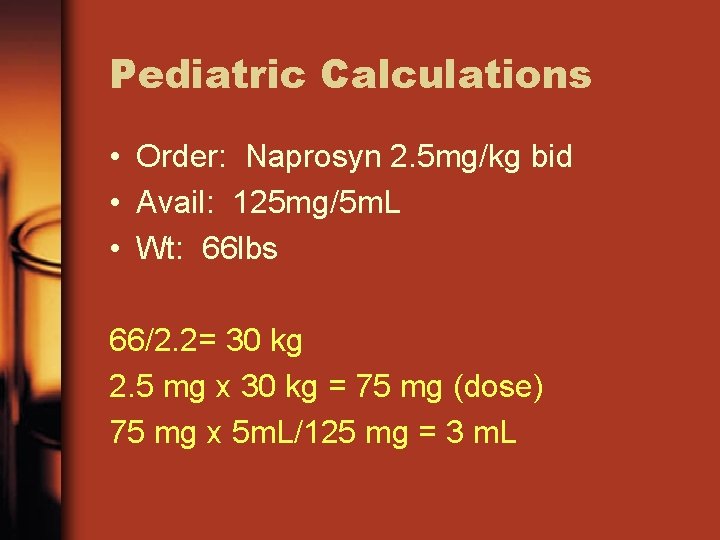
Pediatric Calculations • Order: Naprosyn 2. 5 mg/kg bid • Avail: 125 mg/5 m. L • Wt: 66 lbs
Pediatric Calculations • Order: Naprosyn 2. 5 mg/kg bid • Avail: 125 mg/5 m. L • Wt: 66 lbs 66/2. 2= 30 kg 2. 5 mg x 30 kg = 75 mg (dose) 75 mg x 5 m. L/125 mg = 3 m. L
Background: Reconstitution of Medications • Some medications are stable for only short periods in the liquid state. • Once mixed, a medication is good for only 1 to 14 days. • The mixing process is called “reconstitution. ” • Many facilities reconstitute medications in the pharmacy. • Nurses may have to admix medications just before administration or in the home setting (i. e. Levothyroxine, protonix).
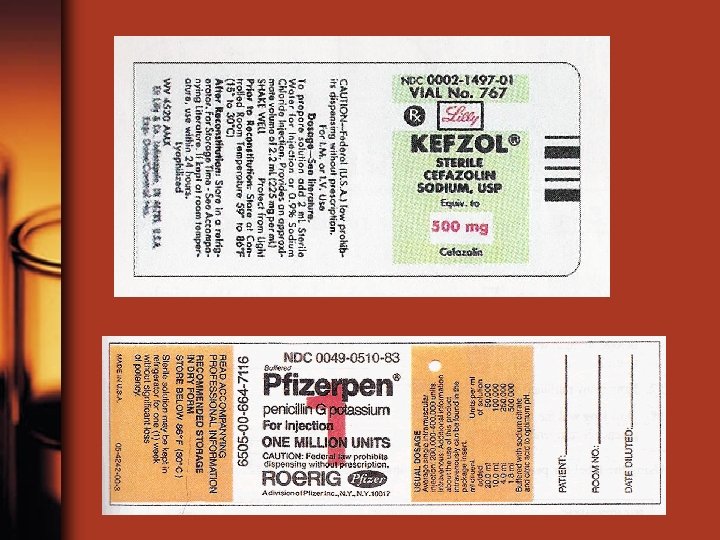
Basic Principles for Reconstitution 1. Manufacturer provides directions – Including m. L, diluent, storage instructions, concentration after admixture 2. Diluents—Check expirations dates before use! – Most common - sterile water or saline – Others: D 5 W, special solution (provided) 3. Must identify the following information: – Type of diluent, amount of diluent – Expiration period after admixture
Basic Principles for Reconstitution (cont’d) 4. 5. If components in item #3 are unavailable, consult PDR (Physician’s Desk Reference), pharmacist or other reliable source. Single dose or multidose after admixture—label clearly – Date and time, mixture strength, expiration date and time – Storage instructions (e. g. , “refrigerate, ” “room temp”) – Nurse’s initials – Apply label so that medication information is not obscured – Discard if labeled inappropriately
Guidelines for Choosing Appropriate Concentrations (cont’d) Multi-dose options: “Respectively” means “in the order given” Example: Reconstitute with 23 m. L, 18 m. L, and 8 m. L to provide concentrations of 200, 000 units per m. L, 250, 000 units per m. L, and 500, 000 units per m. L, respectively: – 23 m. L yields 200, 000 units per m. L – 18 m. L yields 250, 000 units per m. L – 8 m. L yields 500, 000 units per m. L – WRITE THE DOSAGE STRENGTH YOU PREPARED ON VIAL AFTER ADMIXTURE
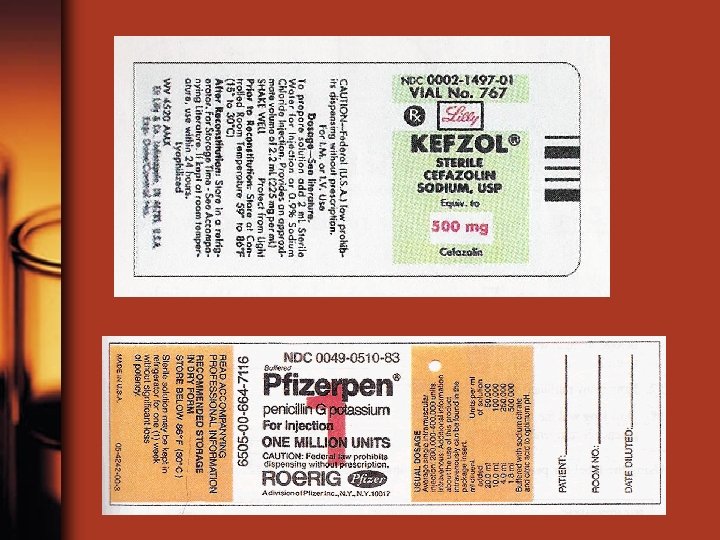
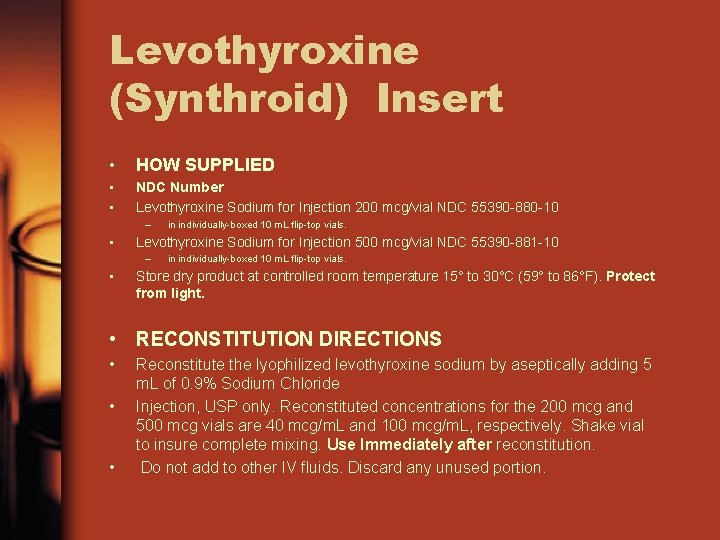
Levothyroxine (Synthroid) Insert • HOW SUPPLIED • • NDC Number Levothyroxine Sodium for Injection 200 mcg/vial NDC 55390 -880 -10 – • Levothyroxine Sodium for Injection 500 mcg/vial NDC 55390 -881 -10 – • in individually-boxed 10 m. L flip-top vials. Store dry product at controlled room temperature 15° to 30°C (59° to 86°F). Protect from light. • RECONSTITUTION DIRECTIONS • • • Reconstitute the lyophilized levothyroxine sodium by aseptically adding 5 m. L of 0. 9% Sodium Chloride Injection, USP only. Reconstituted concentrations for the 200 mcg and 500 mcg vials are 40 mcg/m. L and 100 mcg/m. L, respectively. Shake vial to insure complete mixing. Use Immediately after reconstitution. Do not add to other IV fluids. Discard any unused portion.
References • Asperheim, M. K. (2006). Introduction to Pharmacology, Elsevier Saunders • Pinnell, N. L, (1996). Nursing Pharmacology, W. B. Saunders Co. • Rollant, P. D. , Hill, K. Y. (1996). Nursing Pharmacology, Mosby’s Review Series, St. Louis