Sacral Nerve Stimulation Critical Update and Literature Review

- Slides: 48
Sacral Nerve Stimulation: Critical Update and Literature Review Magdy Hassouna MD Ph. D University of Toronto
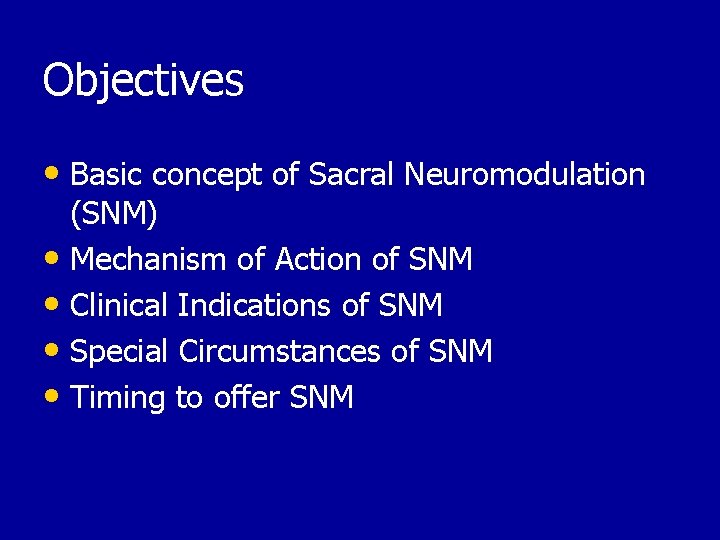
Objectives • Basic concept of Sacral Neuromodulation (SNM) • Mechanism of Action of SNM • Clinical Indications of SNM • Special Circumstances of SNM • Timing to offer SNM
Disclosures • Medtronic • Johnson and Johnson
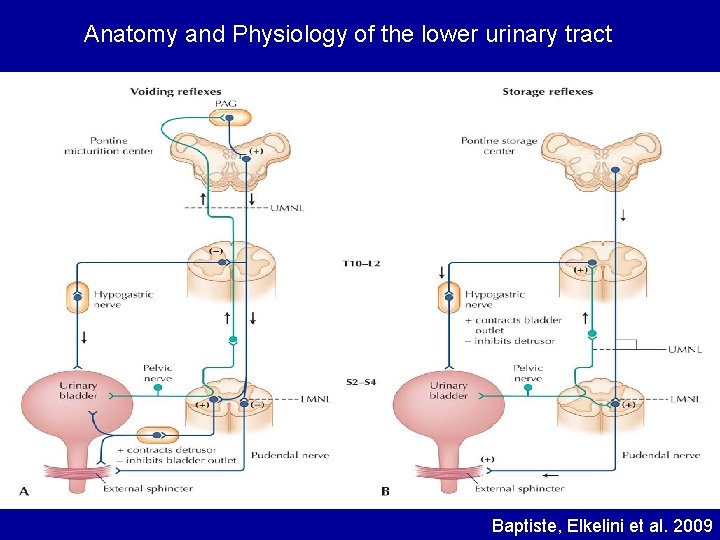
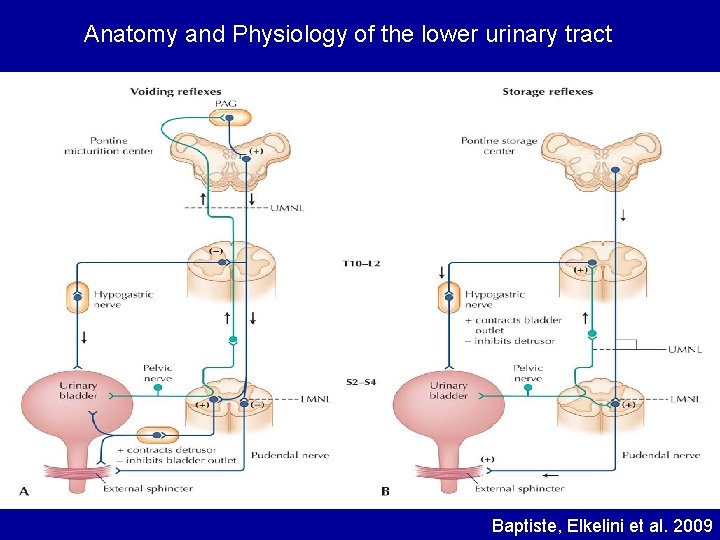
Anatomy and Physiology of the lower urinary tract Baptiste, Elkelini et al. 2009
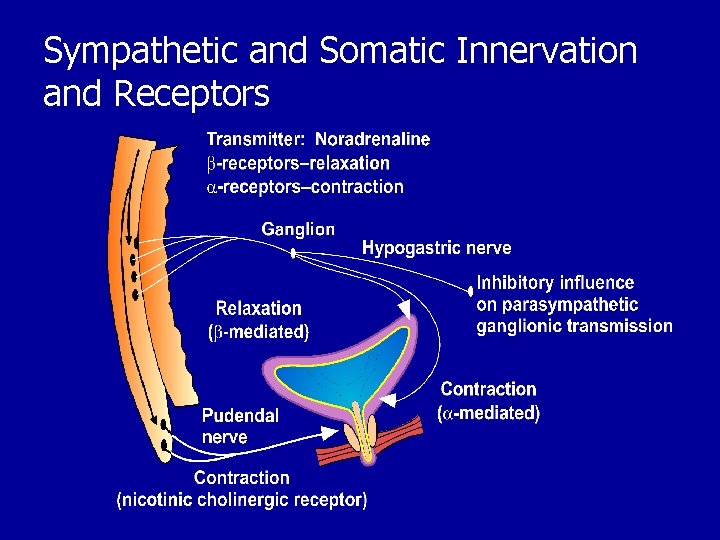
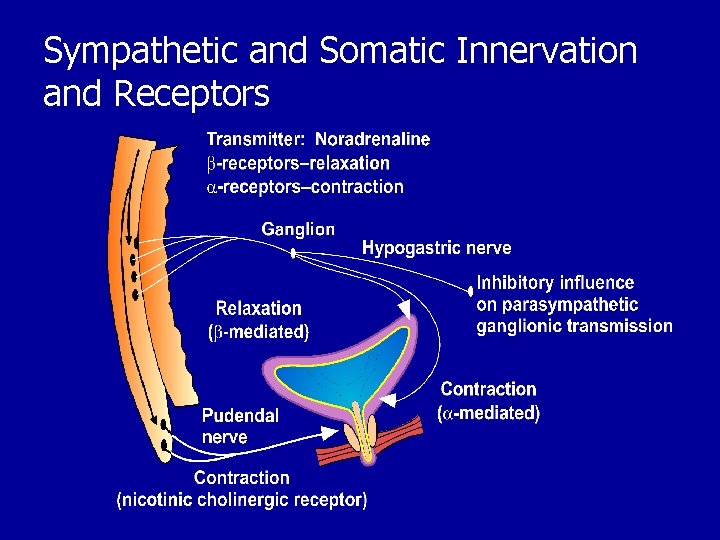
Sympathetic and Somatic Innervation and Receptors
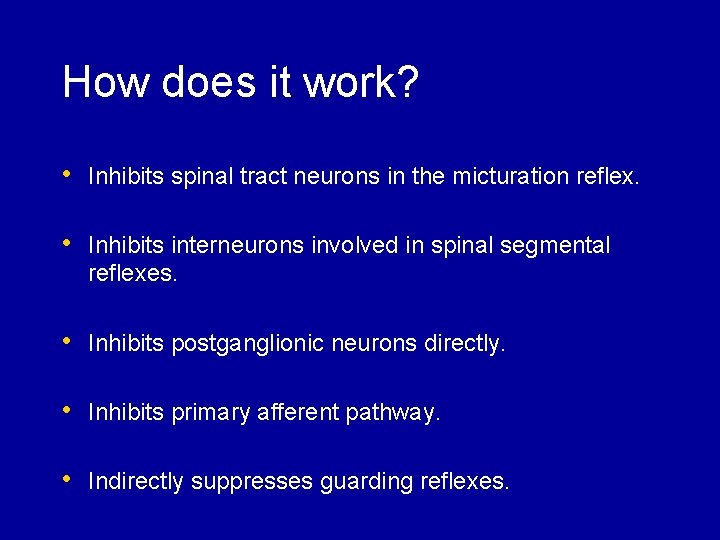
How does it work? • Inhibits spinal tract neurons in the micturation reflex. • Inhibits interneurons involved in spinal segmental reflexes. • Inhibits postganglionic neurons directly. • Inhibits primary afferent pathway. • Indirectly suppresses guarding reflexes.
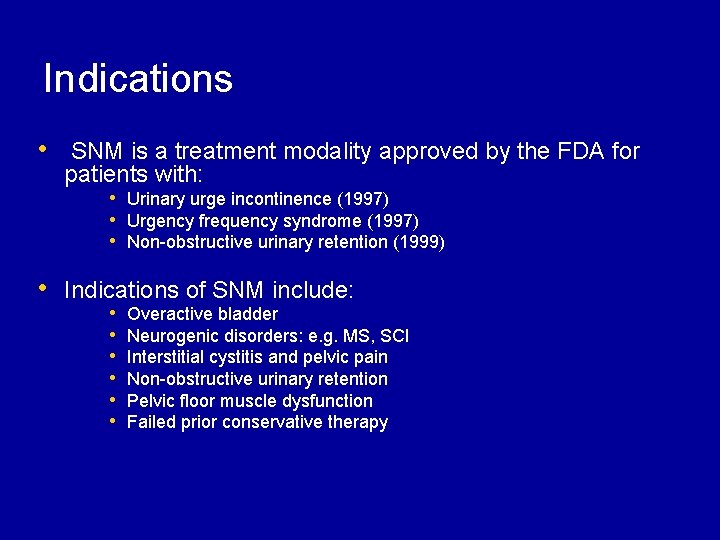
Indications • SNM is a treatment modality approved by the FDA for patients with: • Urinary urge incontinence (1997) • Urgency frequency syndrome (1997) • Non-obstructive urinary retention (1999) • Indications of SNM include: • • • Overactive bladder Neurogenic disorders: e. g. MS, SCI Interstitial cystitis and pelvic pain Non-obstructive urinary retention Pelvic floor muscle dysfunction Failed prior conservative therapy
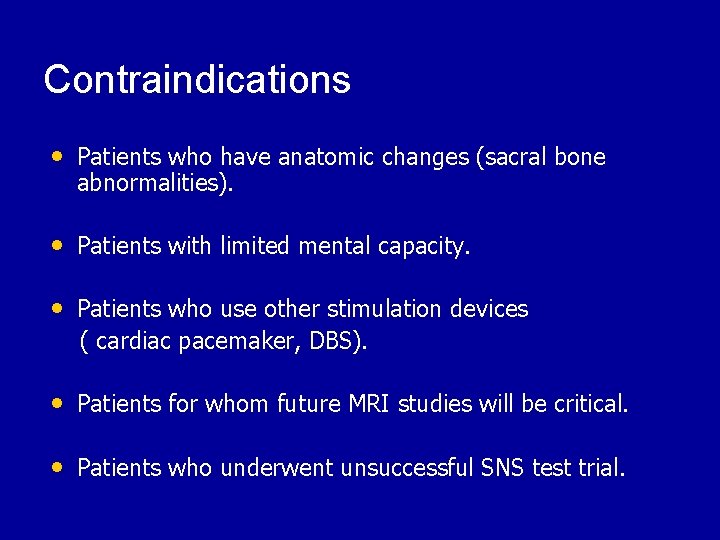
Contraindications • Patients who have anatomic changes (sacral bone abnormalities). • Patients with limited mental capacity. • Patients who use other stimulation devices ( cardiac pacemaker, DBS). • Patients for whom future MRI studies will be critical. • Patients who underwent unsuccessful SNS test trial.
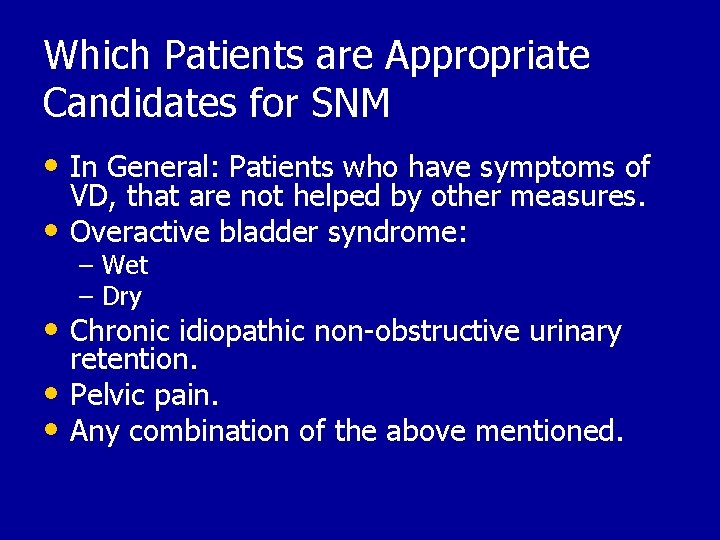
Which Patients are Appropriate Candidates for SNM • In General: Patients who have symptoms of VD, that are not helped by other measures. • Overactive bladder syndrome: – Wet – Dry • Chronic idiopathic non-obstructive urinary retention. • Pelvic pain. • Any combination of the above mentioned.
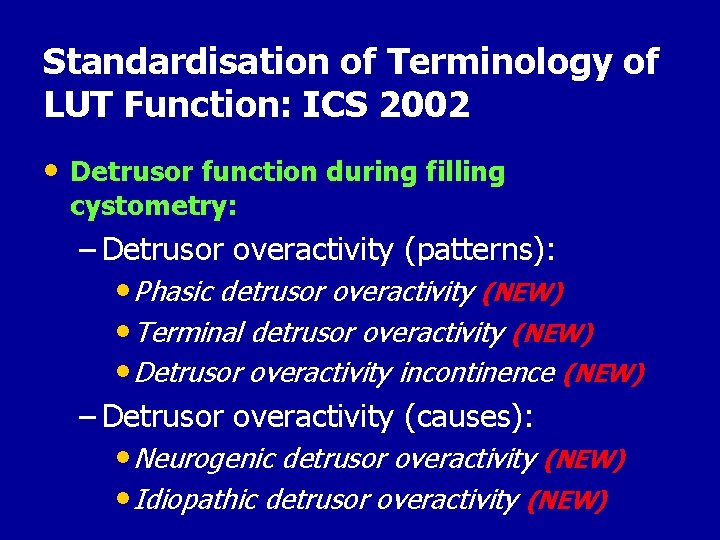
Standardisation of Terminology of LUT Function: ICS 2002 • Detrusor function during filling cystometry: – Detrusor overactivity (patterns): • Phasic detrusor overactivity (NEW) • Terminal detrusor overactivity (NEW) • Detrusor overactivity incontinence (NEW) – Detrusor overactivity (causes): • Neurogenic detrusor overactivity (NEW) • Idiopathic detrusor overactivity (NEW)
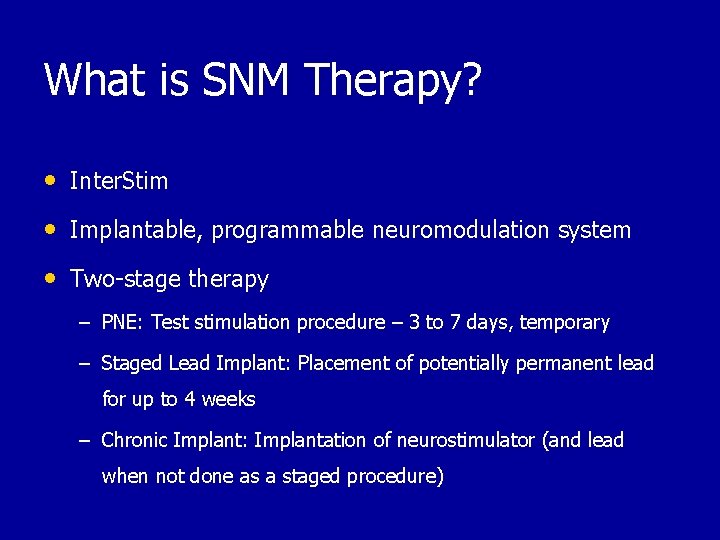
What is SNM Therapy? ® • Inter. Stim • Implantable, programmable neuromodulation system • Two-stage therapy – PNE: Test stimulation procedure – 3 to 7 days, temporary – Staged Lead Implant: Placement of potentially permanent lead for up to 4 weeks – Chronic Implant: Implantation of neurostimulator (and lead when not done as a staged procedure)
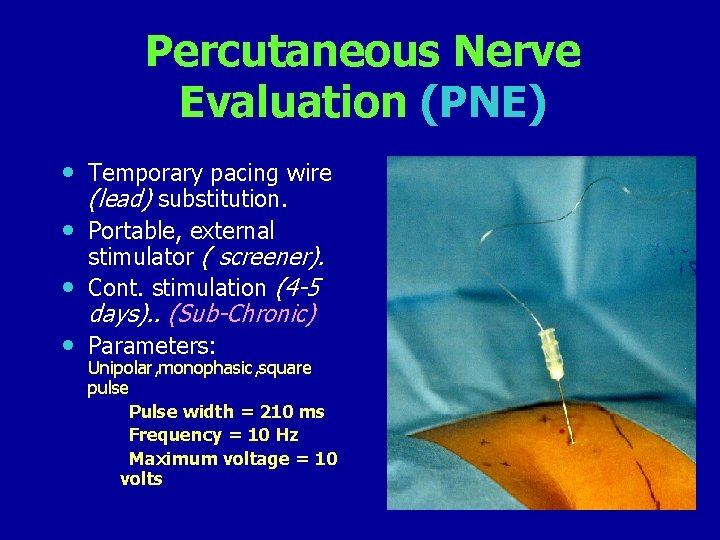
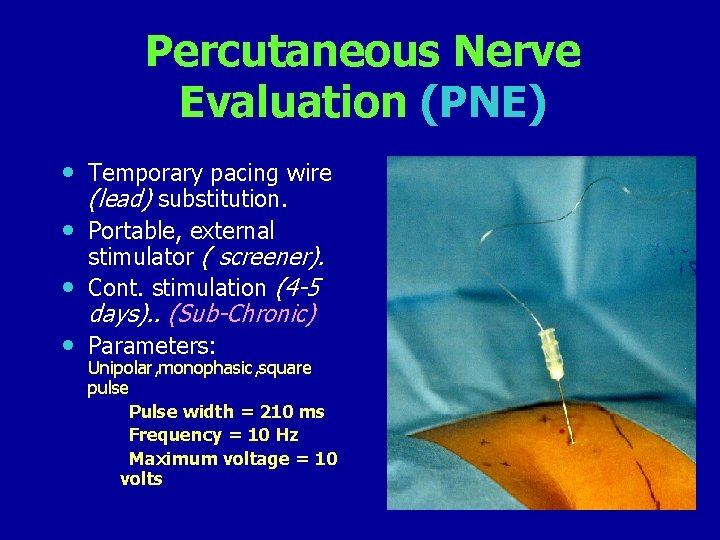
Percutaneous Nerve Evaluation (PNE) • Temporary pacing wire (lead) substitution. • Portable, external • stimulator ( screener). Cont. stimulation (4 -5 days). . (Sub-Chronic) • Parameters: Unipolar, monophasic, square pulse Pulse width = 210 ms Frequency = 10 Hz Maximum voltage = 10 volts
Trial Period • Success equals ≥ 50% improvement • Number of leaks/day • Number of voids/day • Voided volume/void • Degree of urgency
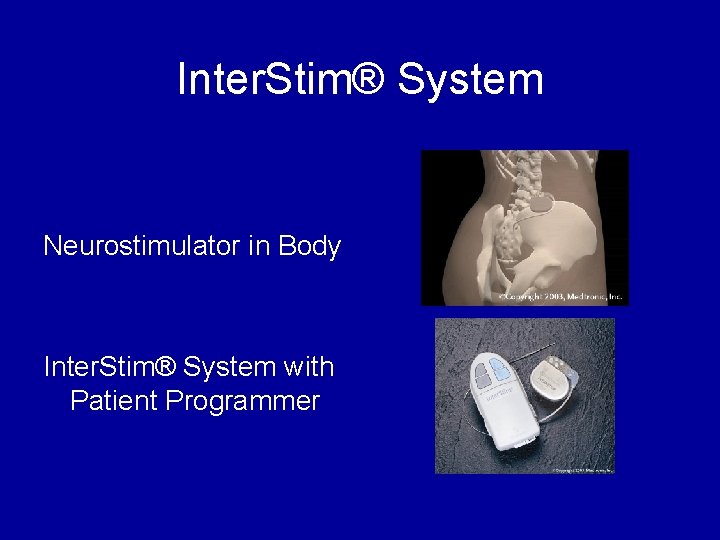
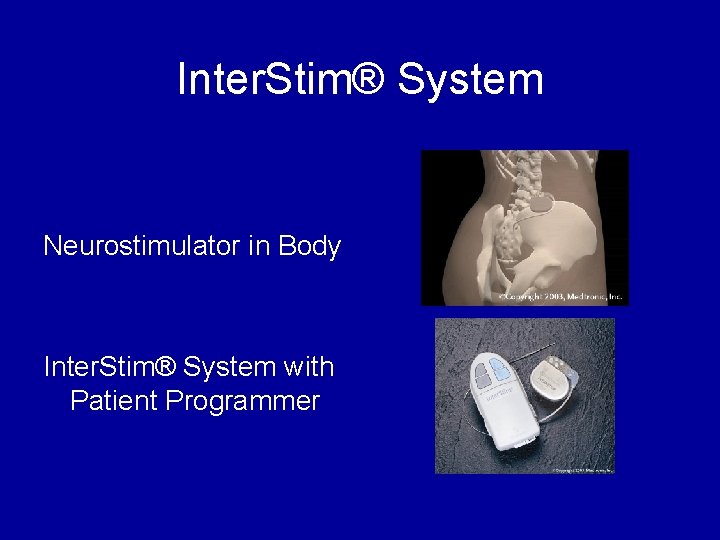
Inter. Stim® System Neurostimulator in Body Inter. Stim® System with Patient Programmer
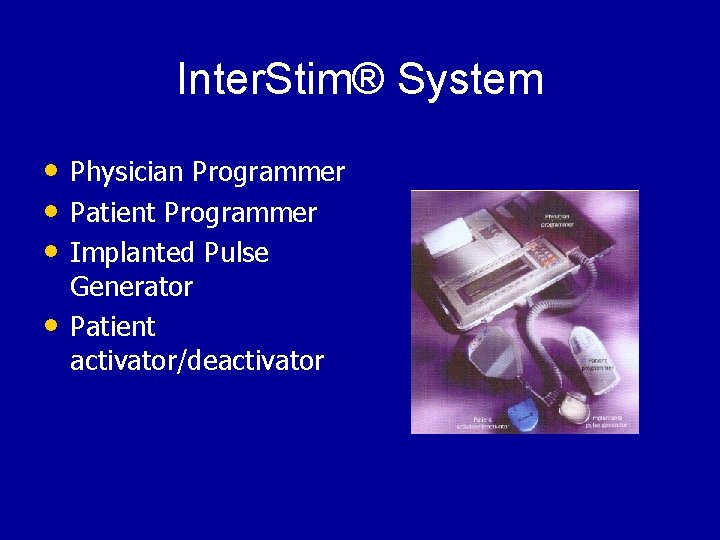
Inter. Stim® System • Physician Programmer • Patient Programmer • Implanted Pulse • Generator Patient activator/deactivator
SNM in Neurogenic Disorders • Multiple Sclerosis ? ? • Spinal Cord Injury ? ? • SNS # CIC / Diversion • Inappropriate Candidates: – Peripheral Neuropathy – Cord lesion – Parkinsonism – Myelodysplasia – MS
SNM and neurogenic disorders • SCI: – In a series of 37 patients with SCI who underwent anterior sacral root stimulation, micturation control was maintained in 87% after 7 years. (Vastenholt ( et al, 2003) – Everaert et al, 1997 reported favourable urodynamic changes in 27 neuromodulation implanted patients with spastic pelvic floor syndrome, bladder neck dysfunction, sphincter hypertonia, sphincter dysfunction, detrusor overdistenstion and hypercontractile detrusor. – Another study on incomplete spinal cord injured patients suffering from lower urinary tract symptoms showed that SNM is effective in 56%(Lombardi and Del, 2009).
SNM in Neurogenic bladder • MS: – In a small series of 5 patients with MS, there was an overall 81. 4% decrease of urgency and frequency with a significant decrease in the number of upper urinary tract infections and fever; there was a slight improvement in bowel function; and overall 51. 8% improvement in the Qol. (Minardi D, Muzzonigro G. , 2005) • Guillain-Barre syndrome: – Wosnitzer et al showed the voiding dysfunction caused by GB syndrome responded to SNM treatment. (Wosnitzer et al, 2009
SNM and PBS (painful bladder syndrome) • Several studies reported improvement in pelvic pain, reduction in narcotic requirements, and improved Qo. L. (Lukban et al, 2002) (Everaert et al, 2001) (Siegel et al, 2001) (Comiter, 2003) • We reported in long term follow-up of 21 female patients with painful bladder syndrome in which 52% showed response to PNE and proceeded for permanent IPG implantation, that an improvement in bladder pain, Qo. L and voiding parameters was maintained after 5 years. (Ghazwani et al, 2011)
SNM and children • In one study, SNM was effective in controlling urinary and fecal incontinence in 33 children with neurogenic voiding dysfunction (Haddad M et al, Journal of Urology, 2010) • Similar results were shown by Humphreys MR et al, and they showed that SNM was effective in the majority of patients with the dysfunctional elimination syndrome. (Humphreys MR et al, Journal of Urology, 2006)
SNM in Children • Another study showed that SNM improved voiding dysfunction after 27 months of prospective follow-up – Urinary incontinence, 88% (14 of 16), – urgency and frequency, 69% (9 of 13), – nocturnal enuresis 89% (8 of 9), – constipation 69% (11 of 16). (Roth TJ et al, Journal of Urology, 2008)
SNS for Bowel Dysfunction • Present indications* – Fecal incontinence – Fecal urgency-frequency (IBS) – Idiopathic chronic constipation • Many patients have both GU/GI symptoms • Often GI improvements most meaningful to patients *Jarret, Br J Surg. 2004; Matzel, Lancet 2004; Kenefic, Br J Surg. 2002
Newer forms of Neuromodulation • Percutaneous tibial nerve stimulation • External urinary sphincter stimulation • Dorsal genital nerve stimulation • Pudendal nerve stimulation
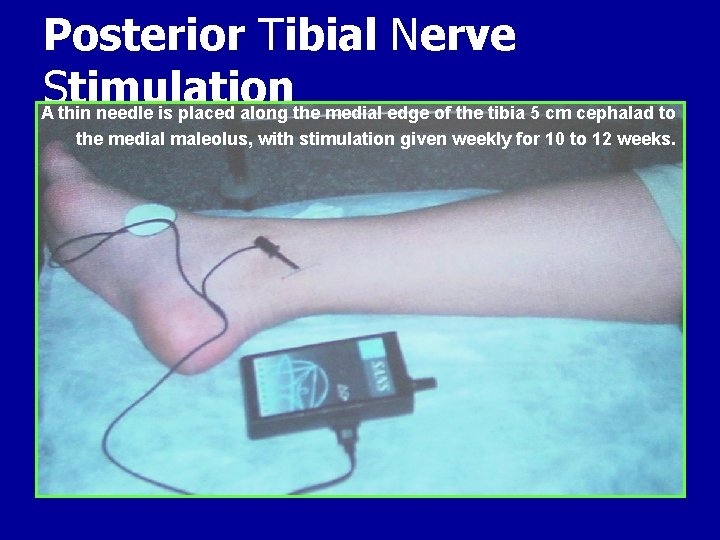
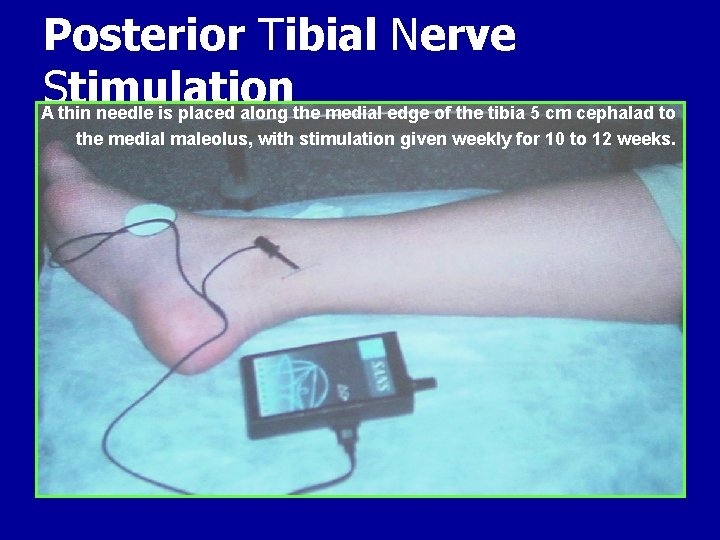
Posterior Tibial Nerve S timulation A thin needle is placed along the medial edge of the tibia 5 cm cephalad to the medial maleolus, with stimulation given weekly for 10 to 12 weeks.
Posterior Tibial Nerve Stimulation • Afferent stimulation provides central • inhibition of the preganglionic bladder motor neurons through a direct route in the sacral cord. Another technique that is less invasive is using disposable, self-adhesive contact electrodes. • Chronic therapy: few long-term series • Marketed commercially as Urgent PC – FDA approved for OAB 2005
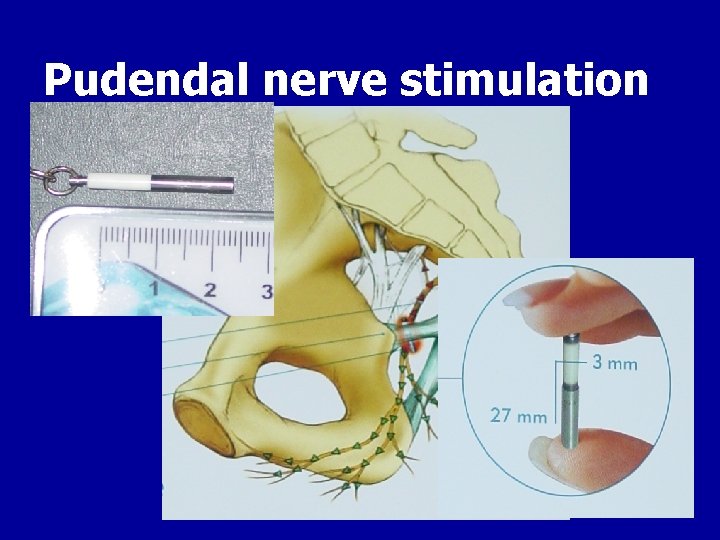
Pudendal Nerve Stimulation • Pudendal nerve stimulation by percutaneously implanting a small pellet close to the pudendal nerve is also currently under investigation. This procedure activates somatic afferent fibers in 3 of the sacral nerves. In contrast, sacral nerve stimulation activates only one sacral nerve, usually S 3.
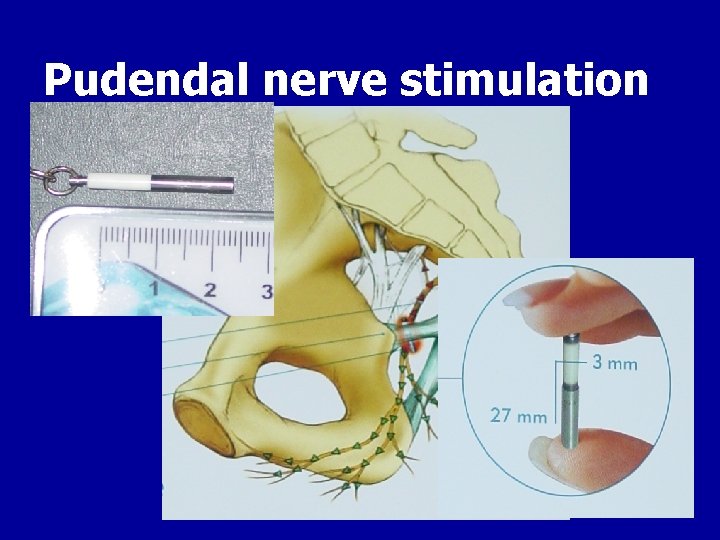
Pudendal nerve stimulation
Dorsal Genital Nerve Stimulation • Target DGN, a sensory branch of pudendal N. • MOA: sensory afferent modulation • Trial: percutaneous lead, office based • Chronic therapy: no information • Not a commercial product
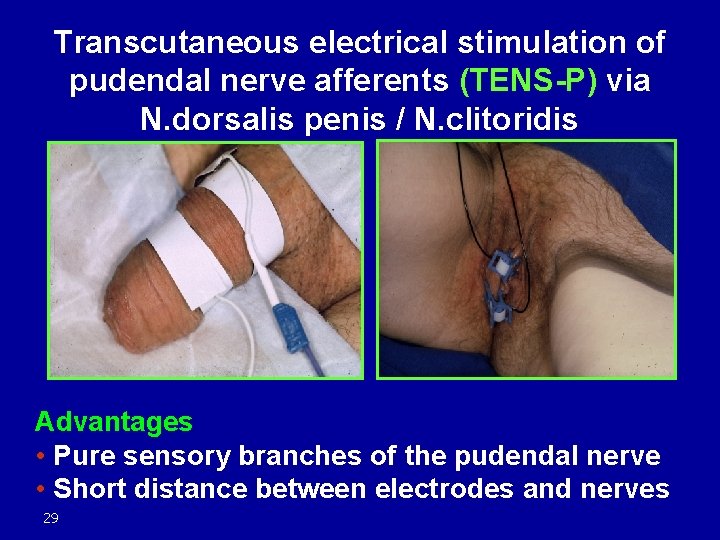
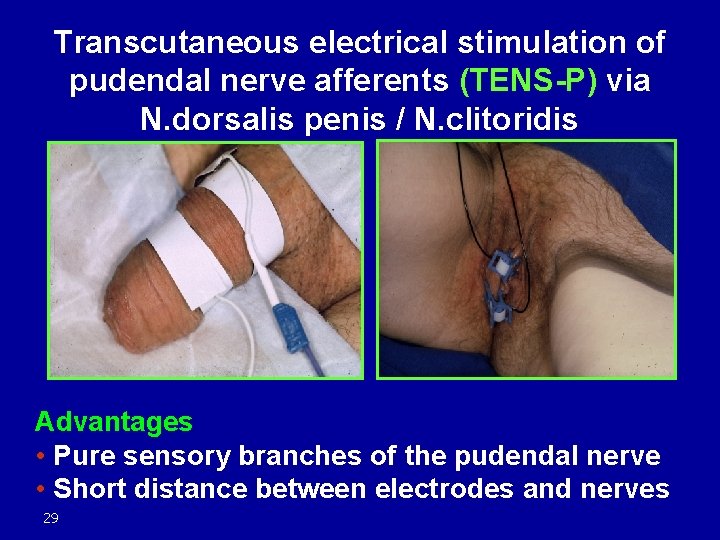
Transcutaneous electrical stimulation of pudendal nerve afferents (TENS-P) via N. dorsalis penis / N. clitoridis Advantages • Pure sensory branches of the pudendal nerve • Short distance between electrodes and nerves 29
External Urinary Sphincter Stimulation • Target EUS • MOA: Activation of efferent fibers cause reflex detrusor relaxation (guarding reflex) • Trial: percutaneous lead, office based • Chronic therapy: limited info available • Not a commercial product
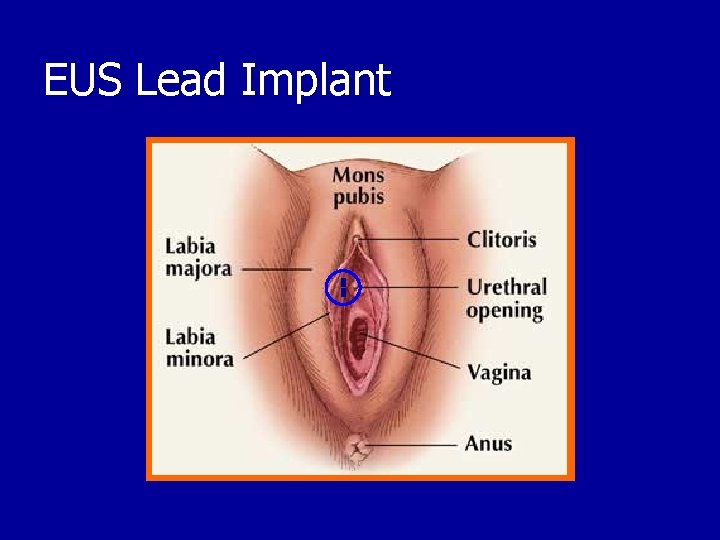
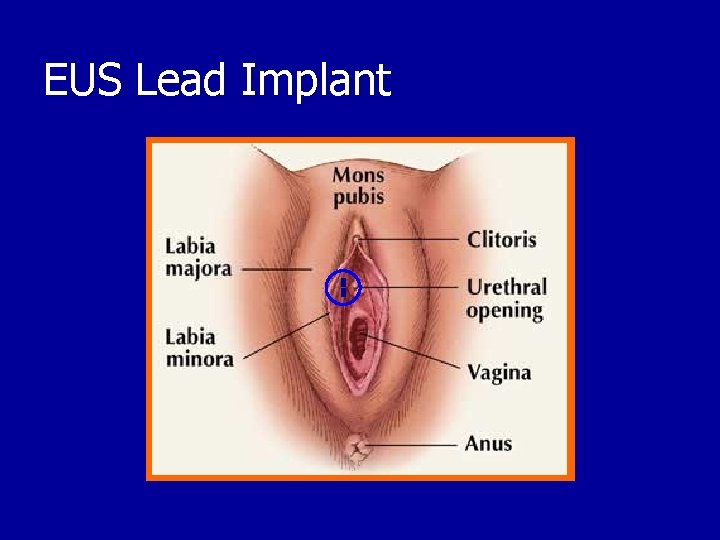
EUS Lead Implant
SNM and Female Sexual Function • Literature is scarce. • One recent study showed that SNM improved sexual functions in patients with OAB. (Paul R, et al 2007) • Another study showed similar results in patients with neurogenic bladder. (Lombardi G, et al 2008)
Effects of sacral neuromodulation on female sexual function • Prospective study. • SNM; December 2009 - July 2012. • Dx: Females with OAB, non-obstructive UR. • Female Sexual Function Index (FSFI): Baseline and Postoperatively at 3 months. Paul R et al, Int Urogynecol J (2007)
Female Sexual Function Index (FSFI): • 19 questions. • Patients must be sexually active for 4 weeks. • Questions are grouped and scored: – – – Libido Arousal Lubrication Orgasm Satisfaction Pain
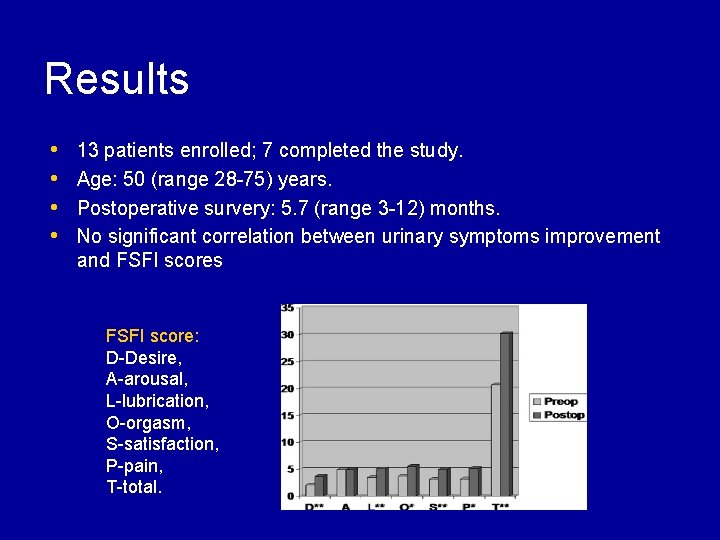
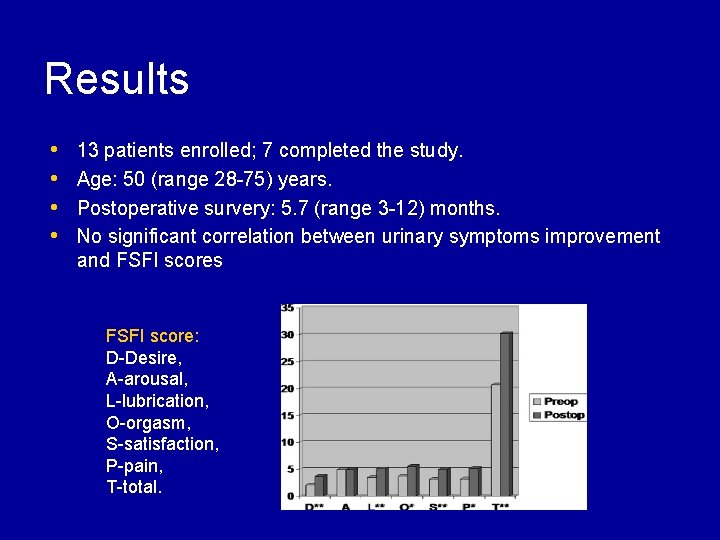
Results • • 13 patients enrolled; 7 completed the study. Age: 50 (range 28 -75) years. Postoperative survery: 5. 7 (range 3 -12) months. No significant correlation between urinary symptoms improvement and FSFI scores FSFI score: D-Desire, A-arousal, L-lubrication, O-orgasm, S-satisfaction, P-pain, T-total.
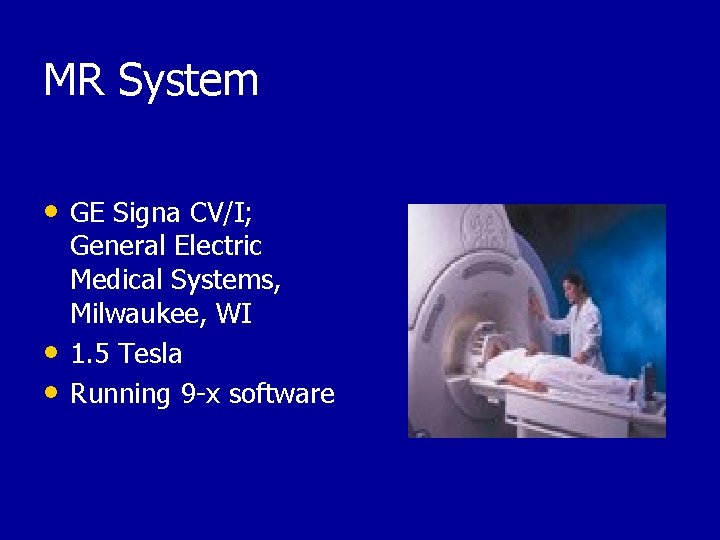
MR System • GE Signa CV/I; • • General Electric Medical Systems, Milwaukee, WI 1. 5 Tesla Running 9 -x software
Reasons to contraindicate MRI include: – Motion and/or dislocation of the Neurostimulator. – Changes to the Neurostimulator program. – Malfunction and damage of the device. – Pain stimulation due to voltages and currents in the Neurostimulator induced by pulsed radiofrequency (RF) fields. – Heating of the Neurostimulator leads due to – electromagnetic RF fields.
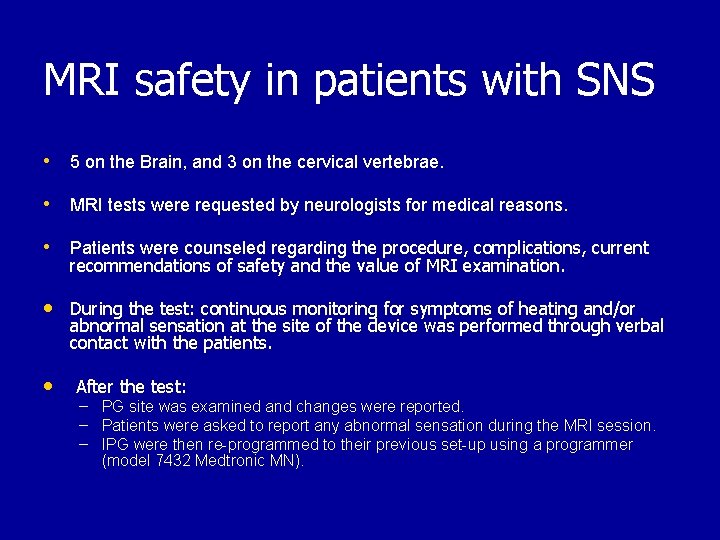
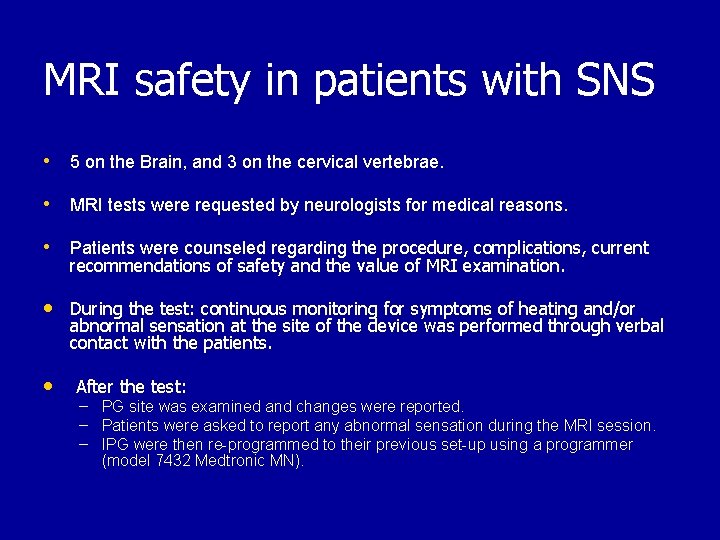
MRI safety in patients with SNS • 5 on the Brain, and 3 on the cervical vertebrae. • MRI tests were requested by neurologists for medical reasons. • Patients were counseled regarding the procedure, complications, current recommendations of safety and the value of MRI examination. • During the test: continuous monitoring for symptoms of heating and/or abnormal sensation at the site of the device was performed through verbal contact with the patients. • After the test: – – – PG site was examined and changes were reported. Patients were asked to report any abnormal sensation during the MRI session. IPG were then re-programmed to their previous set-up using a programmer (model 7432 Medtronic MN).
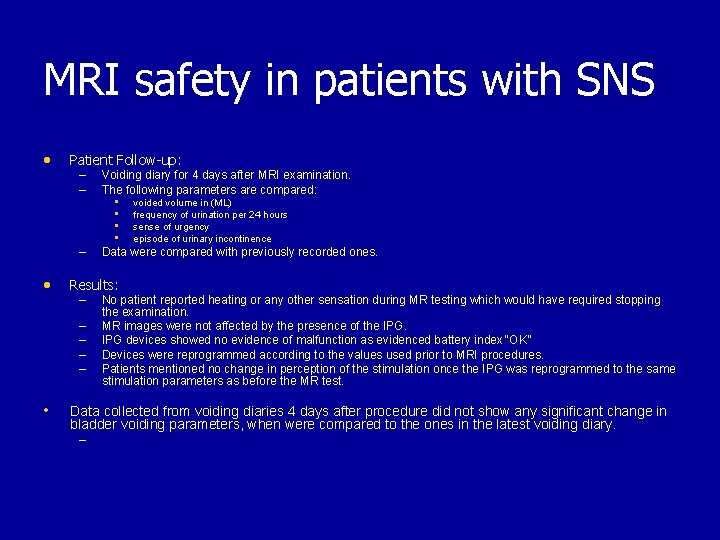
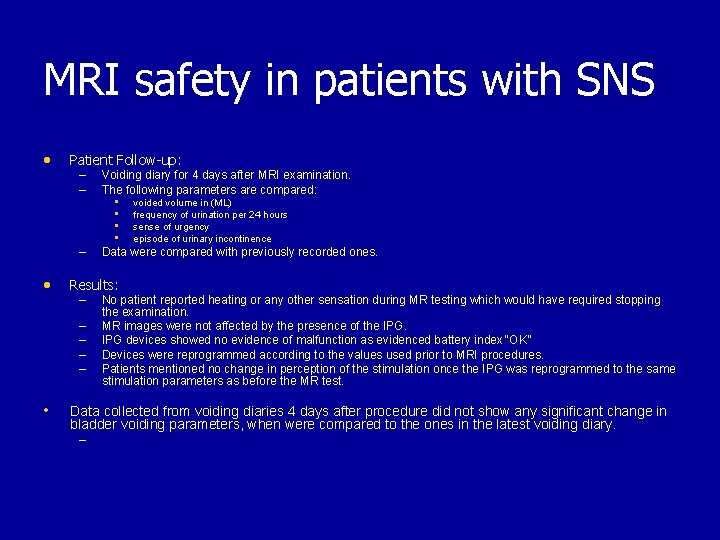
MRI safety in patients with SNS • Patient Follow-up: – – – • Results: – – – • Voiding diary for 4 days after MRI examination. The following parameters are compared: • voided volume in (ML) • frequency of urination per 24 hours • sense of urgency • episode of urinary incontinence Data were compared with previously recorded ones. No patient reported heating or any other sensation during MR testing which would have required stopping the examination. MR images were not affected by the presence of the IPG devices showed no evidence of malfunction as evidenced battery index “OK” Devices were reprogrammed according to the values used prior to MRI procedures. Patients mentioned no change in perception of the stimulation once the IPG was reprogrammed to the same stimulation parameters as before the MR test. Data collected from voiding diaries 4 days after procedure did not show any significant change in bladder voiding parameters, when were compared to the ones in the latest voiding diary. –
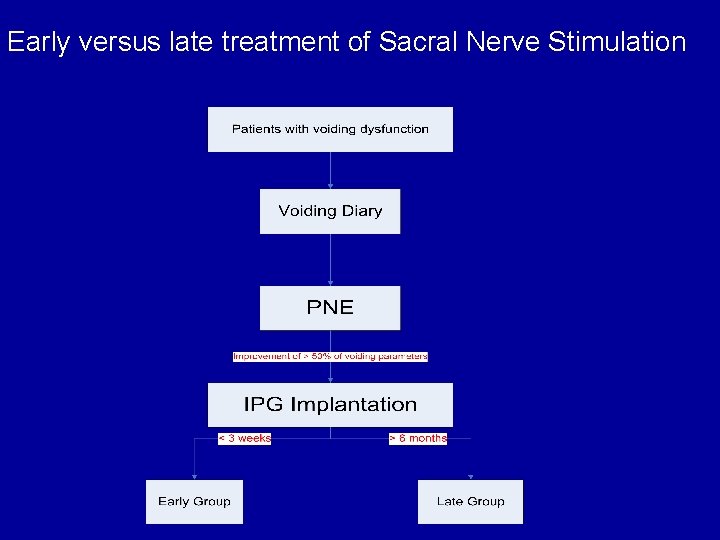
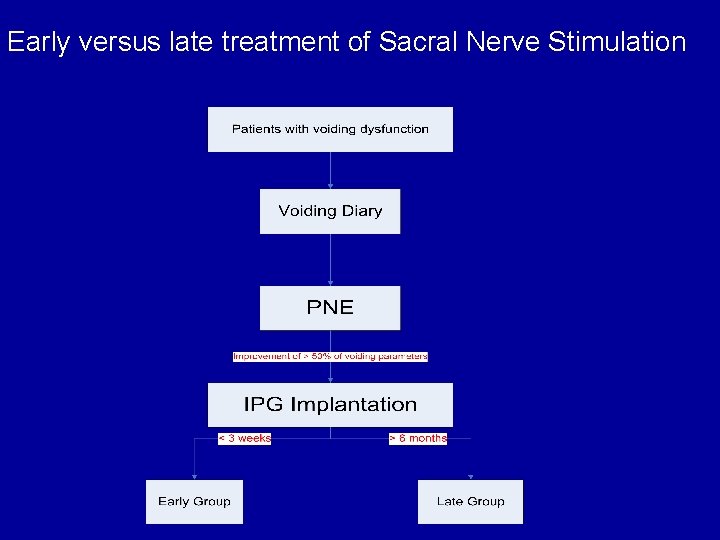
Early versus late treatment of Sacral Nerve Stimulation
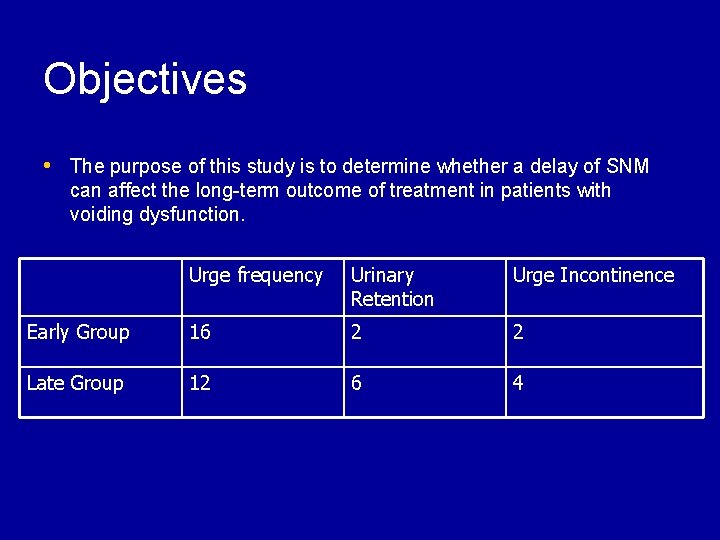
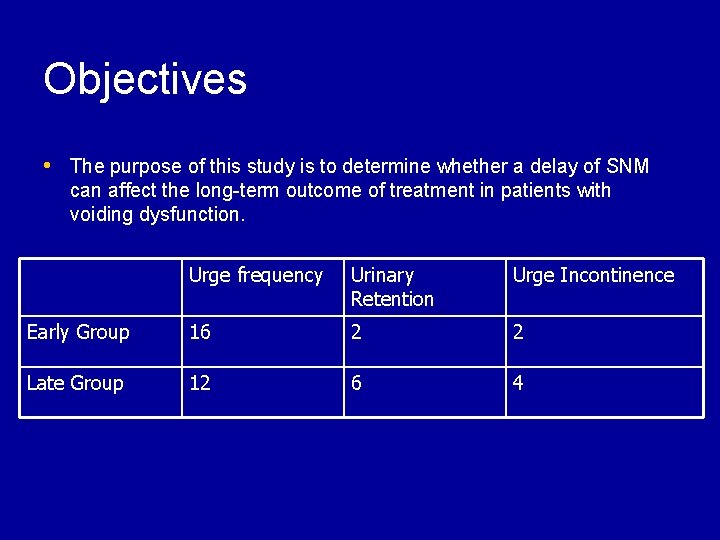
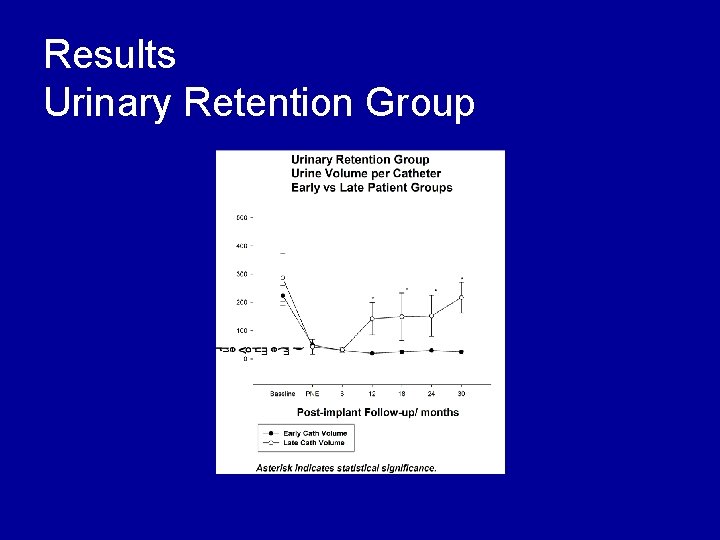
Objectives • The purpose of this study is to determine whether a delay of SNM can affect the long-term outcome of treatment in patients with voiding dysfunction. Urge frequency Urinary Retention Urge Incontinence Early Group 16 2 2 Late Group 12 6 4
Results Patients • Medication intake and co-morbidity were very similar in both study groups • Late patient group: – Mean age at presentation: 40 ± 4. 1 years – Duration of urinary symptoms: 5. 8 ± 2. 6 years • Early patients group: – Mean age at presentation: 42 ± 3. 3 years – Duration of urinary symptoms: 6. 6 ± 1. 3 years
Results Patients • Early group: 16 out of 20 patients (80%) showed good response in their symptoms and overall satisfaction for a follow-up period (mean) 32. 5 months. – 3/20 patients had poor response. – One had the neurostimulator removed due to lack of efficacy. • Late group: 13/22 patients (59%) showed good response in their symptoms and the overall satisfaction. – 7/22 had symptoms less than those in post screening diaries but still better than the baseline diaries. – 2 had the neurostimulator removed due to lack of efficacy.
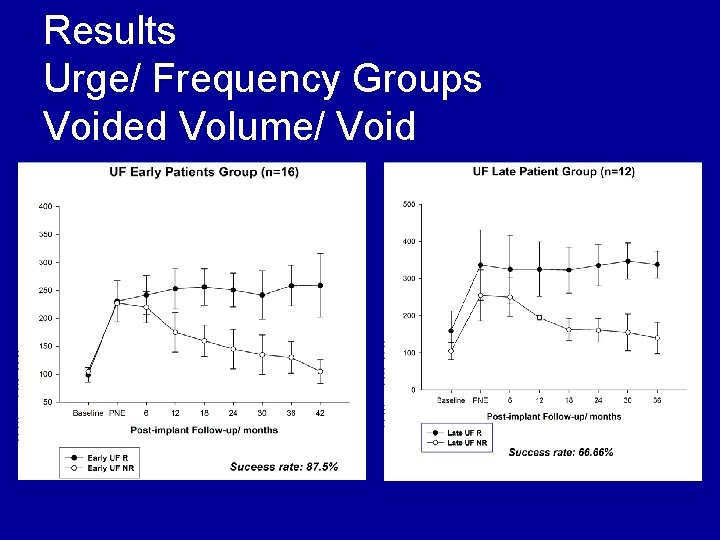
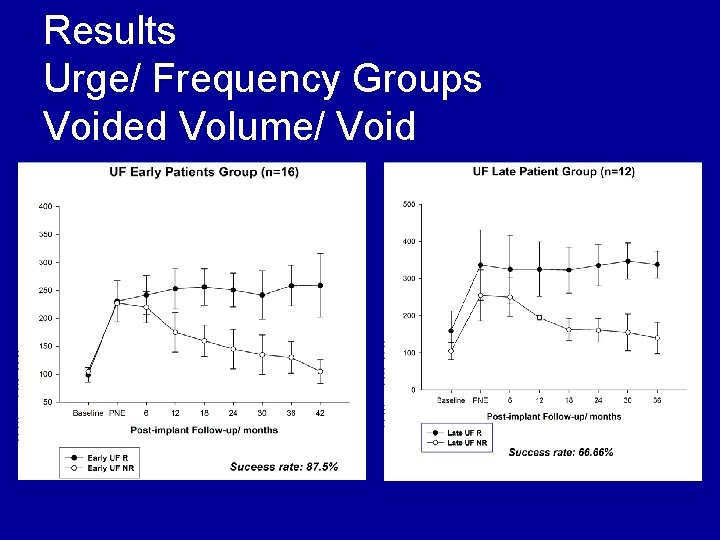
Results Urge/ Frequency Groups Voided Volume/ Void
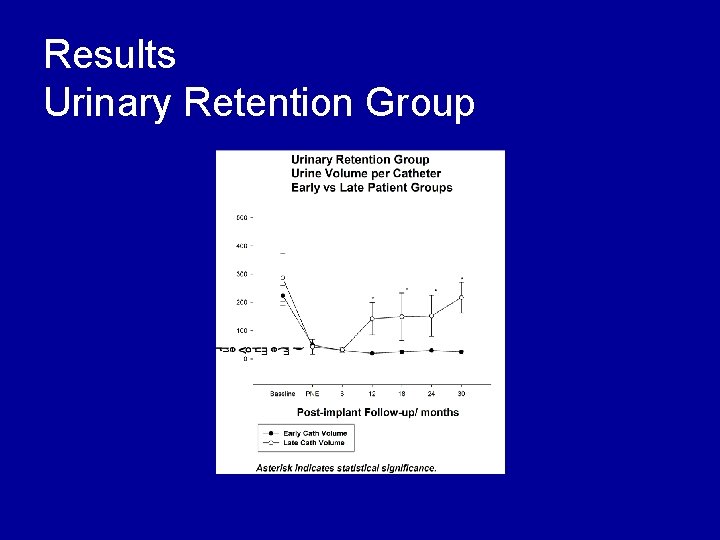
Results Urinary Retention Group
Conclusion • Patients who received SNS implanted • shortly after PNE had shown a better outcome compared to patients who had to wait for 6 months or longer. This study suggests that SNS prevents the progression of the pathophysiologic mechanisms (? ? ) involved in voiding dysfunction.
Conclusion • Newer modalities of SNM are promising • MRI in patients with SNM is feasible • Newer Indications of SNM are emerging

Thank You