S S E B A C S abscess

S S E B A C S
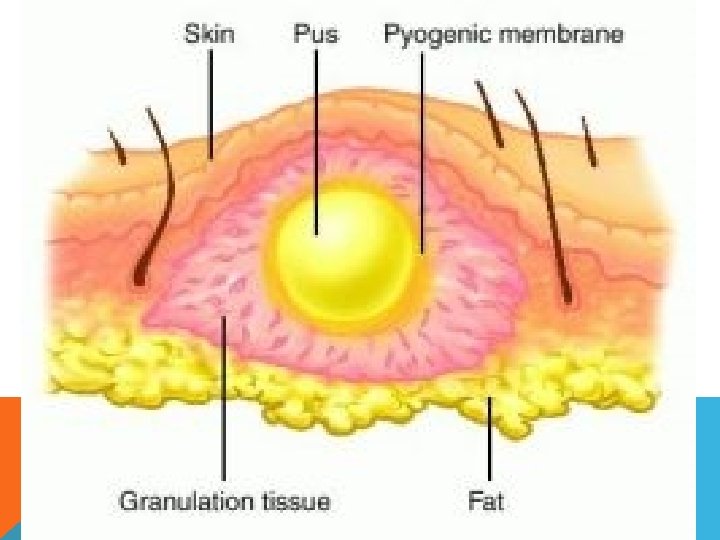
abscess n An abscess is a cavity filled with pus and lined by a pyogenic membrane. This pyogenic membrane consists of dead tissue cells and a wall of granulation tissue consisting for the most part
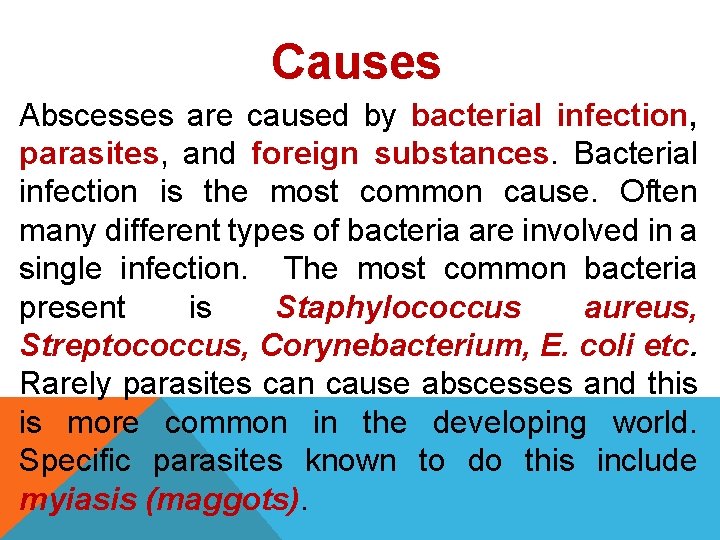
Causes Abscesses are caused by bacterial infection, parasites, and foreign substances. Bacterial infection is the most common cause. Often many different types of bacteria are involved in a single infection. The most common bacteria present is Staphylococcus aureus, Streptococcus, Corynebacterium, E. coli etc. Rarely parasites can cause abscesses and this is more common in the developing world. Specific parasites known to do this include myiasis (maggots).

Signs and symptoms Abscesses may occur in any kind of solid tissue but most frequently on skin surface (where they may be superficial pustules (boils) or deep skin abscesses), in the lungs, brain, teeth, kidneys and tonsils. Major complications are spreading of the abscess material to adjacent or remote tissues and extensive regional tissue death (gangrene). The main symptoms and signs of a skin abscess are redness, heat, swelling, pain and loss of function. There may also be high temperature (fever) and chills.
Internal abscess is more difficult to identify, but signs include pain in the affected area, a high temperature, and generally feeling unwell. Internal abscesses rarely heal themselves, so prompt medical attention is indicated if such an abscess is suspected. An abscess could potentially be fatal (although this is rare) if it compresses vital structures such as the trachea in the context of a deep neck abscess. If superficial, abscesses may be fluctuant when palpated. This is a wave-like motion which is caused by movement of the pus inside the abscess.
Abscess Symptoms Most often, an abscess becomes a painful, compressible mass that is red, warm to touch, and tender. • As some abscesses progress, they may "point" and come to a head so you can see the material inside and then spontaneously open (rupture). • Most will continue to get worse without care. The infection can spread to the tissues under the skin and even into the bloodstream. • If the infection spreads into deeper tissue, you may develop a fever and begin to feel ill.
Classification of Abscesses may be classified (generally) as either skin abscesses or internal abscesses. Skin abscesses are common; internal abscesses tend to be harder to diagnose, and more serious. Skin abscesses are also called cutaneous or subcutaneous abscess. Abscess can be classified into : Ø Acute abscess(hot). Ø Chronic abscess(cold). Ø Superficial abscess. Ø Deep abscess.
DIFFERENTIAL DIAGNOSIS ØTumor ØCyst ØHygroma ØHematoma ØHernia
Treatment The basic principle of treatment of an abscess are: n to drain the pus; n to send a sample of pus for culture and sensitivity test; n to give proper antibiotic
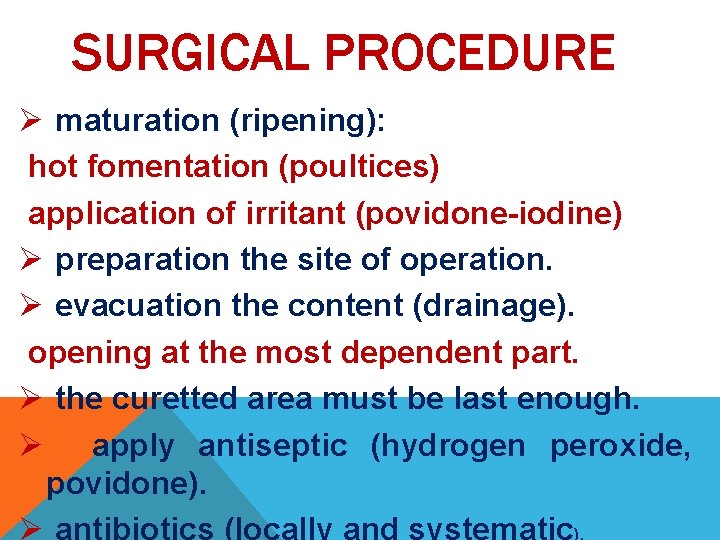
SURGICAL PROCEDURE Ø maturation (ripening): hot fomentation (poultices) application of irritant (povidone-iodine) Ø preparation the site of operation. Ø evacuation the content (drainage). opening at the most dependent part. Ø the curetted area must be last enough. Ø apply antiseptic (hydrogen peroxide, povidone).

S I F U T A L
FISTULA Abnormal epithelial-lined communication between two anatomical structure, most commonly seen between two internal organs, or between an internal organ and the surface of the body as a rectal fistula, bronchopleural fistula, cutaneous fistula etc.
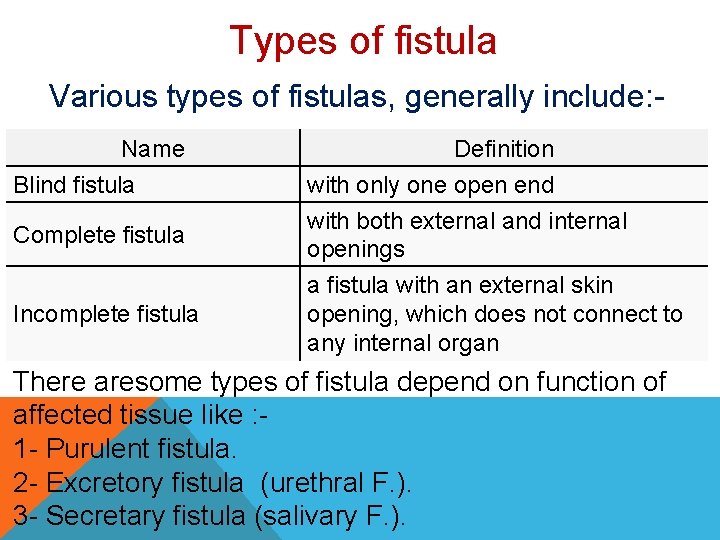
Types of fistula Various types of fistulas, generally include: Name Blind fistula Complete fistula Incomplete fistula Definition with only one open end with both external and internal openings a fistula with an external skin opening, which does not connect to any internal organ There aresome types of fistula depend on function of affected tissue like : 1 - Purulent fistula. 2 - Excretory fistula (urethral F. ). 3 - Secretary fistula (salivary F. ).
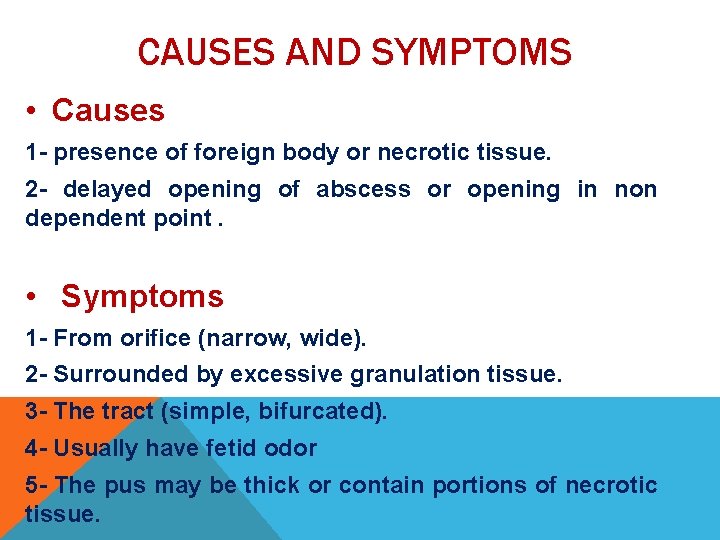
CAUSES AND SYMPTOMS • Causes 1 - presence of foreign body or necrotic tissue. 2 - delayed opening of abscess or opening in non dependent point. • Symptoms 1 - From orifice (narrow, wide). 2 - Surrounded by excessive granulation tissue. 3 - The tract (simple, bifurcated). 4 - Usually have fetid odor 5 - The pus may be thick or contain portions of necrotic tissue.
TREATMENT 1. Identify the internal opening 2. Incision at inter sphincter groove 3. Dissection through inter sphincter plane to find intersphincteric fistula tract 4. Secure suture ligation of intersphincteric fistula tract 5. Remove the fistula tract by caustic agents or surgically 6. Curette fistula tract from external opening 7. Suture closure of external sphincter muscle defect 8. Closure of intersphincteric wound

A T A H M E M O
HAEMATOMA A hematoma is an abnormal collection of blood outside of a blood vessel. It occurs because the wall of a blood vessel wall, artery, vein, or capillary, has been damaged and blood has leaked into tissues where it does not belong. The hematoma may be tiny, with just a dot of blood, or it can be large and cause significant swelling.
Hematoma Symptoms depend upon their location and whether the size of the hematoma or the associated swelling and inflammation cause nearby structures to be affected. The common symptoms of inflammation include: • redness, • pain, and • swelling. Hematomas tend to resolve over time. • The initial firm texture of the blood clot gradually becomes more spongy and soft as the clot is broken down by the body.
PREVENTION OF HEMATOMA Simple therapies at home may be utilized in treating superficial (under the skin) hematomas. Most injuries and bruises can be treated with resting, icing, compression, and elevating the area. This is remembered by the acronym RICE. These measures usually help to reduce inflammation and diminish its symptoms. • Rest • Ice (Apply the ice or cold pack for 20 minutes at a time, 4 to 8 times a day. ) • Compress (Compression can be achieved by using elastic bandages. ) • Elevate (Elevation of the injured area above the level of the heart is recommended. )
Treatment Medical care and definitive treatment of a hematoma depends upon its location, what body parts are affected, and what symptoms are present. For example 1 - Small hematoma was disappeared by application of iodine ointment to induce the absorption of the fluid contents of the swelling (hematoma).
2 - large hematoma: ØAfter 7 -10 days from occurrence of hematoma must be evacuated by incision of it. ØWashing the cavity of incised hematoma with antiseptic and swabbed with tincture iodine. ØPack the cavity with sterile gauze.

E N A G G N E R
GANGRENE is a condition that occurs when body tissue dies. It is caused by a loss of blood supply due to an underlying illness, injury, and/or infection. Fingers, toes, and limbs are most often affected, but gangrene can also occur inside the body, damaging organs and muscles. There are different types of gangrene and all require immediate medical attention.
GANGRENE CAUSES • • • Blood plays a very important role in your health. Not only does it transport oxygen and nutrients throughout your body to feed cells, it delivers disease-fighting antibodies that protect your body from infection. When blood cannot travel freely throughout the body, your cells cannot survive, infection can develop, and tissue can die from gangrene. Any condition that affects blood flow increases your risk of gangrene, including: Diabetes Atherosclerosis Peripheral arterial disease Trauma or serious injury Raynaud's phenomenon (a condition in which the blood vessels that supply the skin become intermittently narrowed
Gangrene Types There are two main types of gangrene: 1 - Dry gangrene: More common in people with diabetes and autoimmune diseases, dry gangrene usually affects the hands and feet. It develops when blood flow to the affected area is impaired, usually as a result of poor circulation. In this type, the tissue dries up and may be brown to purplish-blue to black in color and often falls off. Unlike other types of gangrene, infection is typically not present in dry gangrene. However, dry gangrene can lead to wet gangrene if it becomes infected.
2 - Wet gangrene: Unlike dry gangrene, wet gangrene almost always involves an infection. Injury from burns or trauma where a body part is crushed or squeezed can rapidly cut off blood supply to the affected area, causing tissue death and increased risk of infection. The tissue swells and blisters and is called "wet" because of pus. Infection from wet gangrene can spread quickly throughout the body, making wet gangrene a very serious and potentially life-threatening condition if not treated quickly.
Types of wet gangrene 2 -A-Internal gangrene: If gangrene occurs inside the body due to blocked blood flow to an internal organ, then it is referred to as internal gangrene. This is usually related to an infected organ such as the appendix or colon.
2 -B- Gas gangrene : Gas gangrene is rare but dangerous. It occurs when infection develops deep inside the body, such as inside muscles or organs, usually as a result of trauma. The bacteria that causes gangrene, called clostridia, release dangerous toxins or poisons that wreak havoc throughout the body, along with gas which can be trapped within body tissue. As the condition progresses, the skin may become pale and gray, and make a crackling sound when pressed, due to the gas within the tissue. Gas gangrene warrants immediate medical treatment. Without treatment, death can occur within 48 hours.
2 -C-Fournier's gangrene: Also a rare condition, Fournier's gangrene is caused by an infection in the genital area. Men are affected more often than women. If the infection gets into the bloodstream, a condition called sepsis, it can be life-threatening.
Gangrene Symptoms You may notice the following symptoms at the site of the dry gangrene: • Dry and shriveled skin that changes color from blue to black and eventually sloughs off • Cold and numb skin • Pain may or may not be present
Symptoms of wet gangrene may include: • Swelling and pain at the site of infection • Change in skin color from red to brown to black • Blisters or sores that produce a bad-smelling discharge (pus) • Fever and feeling unwell • A crackling noise that comes from the affected area when pressed
Treatments Treatment for gangrene involves removing the dead tissue, treating and preventing the spread of infection, and treating the condition that caused gangrene to develop. Surgery. Also called debridement, the dead tissue is surgically removed to prevent the spread of infection. In some situations, amputation (removal of the affected limb, finger or toe) may be required.




C T S Y
Cysts are closed capsule or saclike structures, typically filled with liquid, semisolid or gaseous material - very much like a blister. Cysts occur within tissue, and can affect any part of the body. They vary in size from microscopic to the size of some large cysts can displace internal organs.
CAUSES Common causes of cysts include: • Tumors • Genetic conditions • Infections • A fault in an organ of a developing embryo • A defect in the cells • Chronic inflammatory conditions • Blockages of ducts in the body which cause a fluid build-up • A parasite • Impact injury that breaks a vessel.
CLASSIFICATION OF CYST 1 - Congenital cyst. 2 - Acquired cysts : • Retention cyst. • Distention cyst. • Parasitic cyst. • Degenerative cyst.
TREATMENT 1 - puncture of cyst by trocar and canular or seton needle (siphon) to evacute the content and the lining tissue is swabbed with irritant substance like iodine or carbolic acid to destroy it and leading to obliteration of the cavity. Small cyst may be incised along its entire length. 2 - Excision of the cyst – specially in tumor.

U R E C L
DEFINITION A lesion of the skin or of a mucous membrane, such as the one lining the stomach or duodenum, that is accompanied by formation of pus and necrosis of surrounding tissue, usually resulting from inflammation or ischemia
CLASSIFICATION OF ULCER 1 - Non- specific ulcers: - are caused by trauma or pyogenic bacteria. 2 - Specific ulcers: - are found in the course of certain specific disease such as ulcerative lymphangitis and tuberculosis. 3 - Malignant ulcers such as rodent ulcer, epitheliomatous and fungating.
ETIOLOGY 1 - Repeated irritation of a wound. 2 - Presence of foreign body or necrotic tissue in the wound. 3 - loss of innervation. 4 - lack of blood supply.
TREATMENT Ø Removal of the causative agent. Ø In case of septic inflammatory ulcer application of warm antiseptic fomentation. Ø Use of thermocautery for destroying callous tissue and promoting normal granulation and circulation.
- Slides: 46