RT CASE OF THE SWOLLEN LEG Cimi Achiam


- Slides: 23
RT: CASE OF THE SWOLLEN LEG Cimi Achiam MD, DTMH, FRCPC
FIRST VISIT: SEPT 14, 2011 12: 25: � 50 yr male cc: L leg swelling 6 days of L leg swelling Transient SOBOE w/ mildly pleuritic chest pain yesterday, but completely resolved on presentation � PMHx: L DVT Jan 2011 Precipitated by flight to Hawaii Tx w/ 6/12 of Warfarin D/C in mid June � No meds currently � Family Hx: nil
VISIT 1 O/E: T 37. 2 HR 70 BP 145/78 RR 20 Sat 96% RA � Chest: GAEBL, clear � CVS: S 1 S 2 N, no murmur � Abdo: Soft NT, not distended � Neuro: Normal � L Leg: proximal swelling

VIST 1 INVESTIGATIONS 6 Pack: - D dimer: 646 Troponin: -
VISIT 1: IMAGING CTPA: � no PE, mildly prominent R hilar node of uncertain clinical significance CT Abdo/Pelvis: � � � No large pelvic mass causing obstruction of veins No acute intra-abdominal abnormality Questionable narrowing of the left common iliac vein at the level of the overlying right common illiac artery ? May-Thurner syndrome. Recommend Interventional Radiology consult. If there is still significant clinical concern, an MRV could be attempted or a CTV could be reattempted with a longer delay between contrast and imaging Doppler US: � � � - DVT, deep venous system widely patent No residual thrombus identified Normal waveforms, phasicity, augmentation, and compression were obtained
VISIT 1 Given high clinical concern for DVT, case was discussed with radiologist and plan was made for MR venogram next day Pt was tx in the mean time with Enoxaparin 1. 5 mg/kg SC
VISIT 2: SEPT 16, 2011 13: 42: Return for MRI results � Patient’s leg re-examined: Pt looks well, no pedal swelling, good circulation to L foot � MR Venogram of Pelvis & Thighs: Negative MR venogram with no evidence of DVT in the pelvis and LE to just above the knees Pt instructed to return on an as needed basis
VISIT 3: SEPT 20, 2011 Patient represented with progressive swelling of his L leg, non- painful, no paraesthesias. No CP or SOB currently or since last evaluation O/E: � Abdomen: Soft NT, no masses or inguinal lymphadenopathy � LE: non-pitting edema from foot to mid thigh, no erythema, normal pedal pulses and motor exam
VISIT 3 Given multiple investigations on previous visits case was discussed with radiology Repeat Doppler U/S planned Doppler U/S report: Occlusive thrombus seen within the left external iliac vein Non-occlusive thrombus within one branch of both of the duplicated superficial femoral, and popliteal veins ? May Thurner’s syndrome
VISIT 3 On suggestion of radiology, interventional radiology consulted re: possibility of thrombolysis/stenting Vascular surgery consult Was informed would have to consult vascular surgery and that they would consult IR if required Pt was admitted anticoagulated with IV heparin protocol Sept 21/11: � Pt underwent thrombolysis & stenting of his left iliac vein � Pt advised to restart IV heparin and continue coumadin x 6 mo minimum
PATHOPHYSIOLOGY OF MAY THURNER SYNDROME
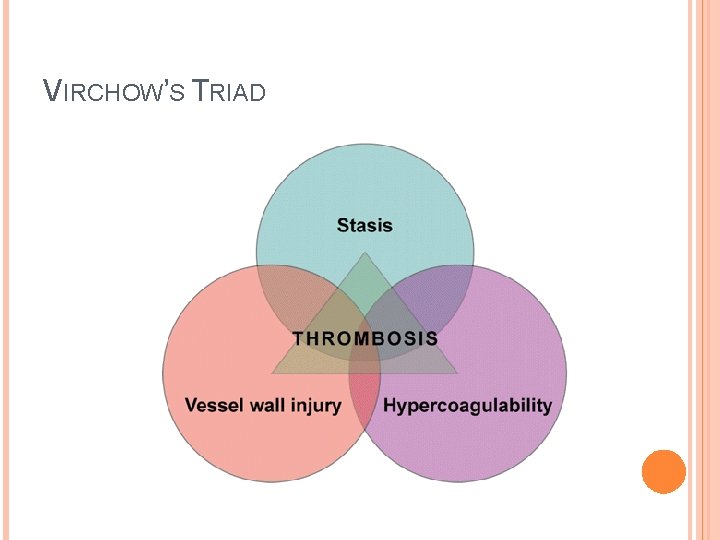
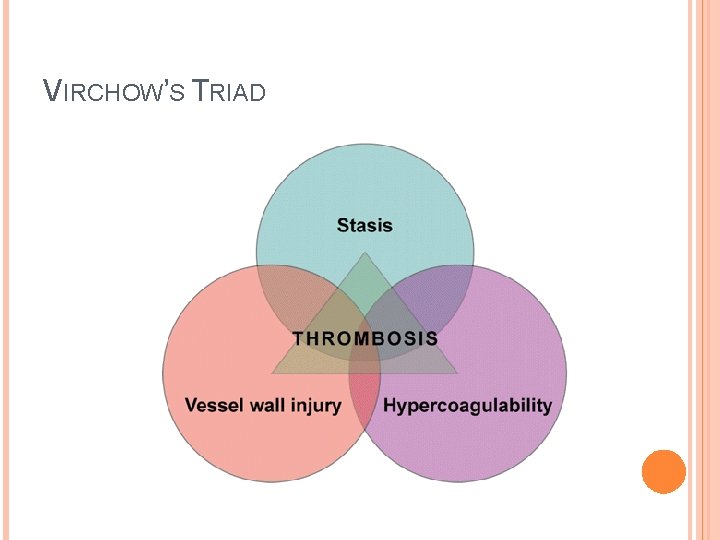
VIRCHOW’S TRIAD
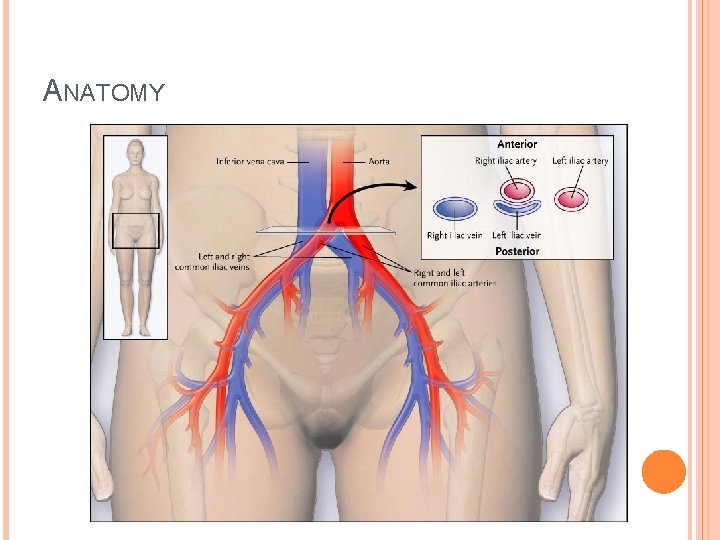
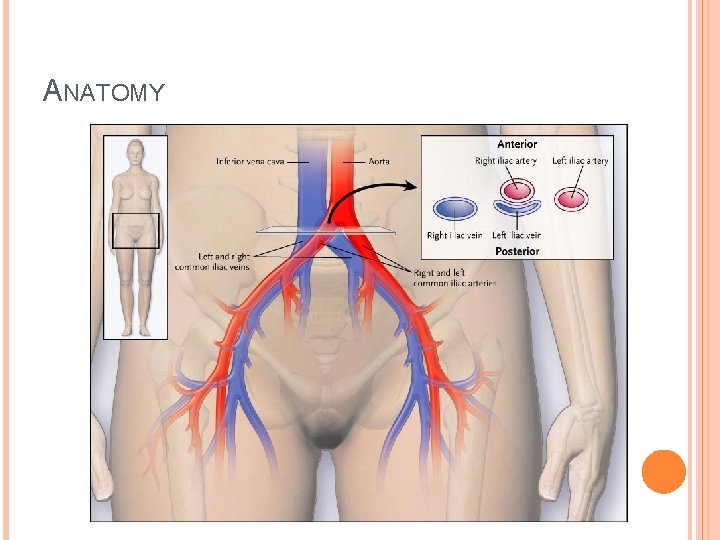
ANATOMY
MAY THURNER SYNDROME Most commonly seen in women between 20 -50 yrs Episodes of DVT may be recurrent and/or poorly responsive to treatment with anticoagulation alone � May require: Catheter-directed thrombolysis Venous angioplasty and/or intravascular stenting Visualization of a clot this high in the pelvis may be difficult to detect using ultrasound of LE � If DVT is strongly suspected, further testing should be performed
DIAGNOSIS OF SUSPECTED DVT OFLE Only a minority of patients (17 and 32 % in two large series) actually have the disease Accurate diagnosis is essential � Potential risk of fatal PE in untreated proximal LE DVTs � Potential risk of fatal bleeding due to anticoagulating a patient who does not have a DVT Birdwell BG, et al. Ann Intern Med 1998; 128: 1 -5 Huisman MV, et al. N Engl J Med 1986; 314: 823
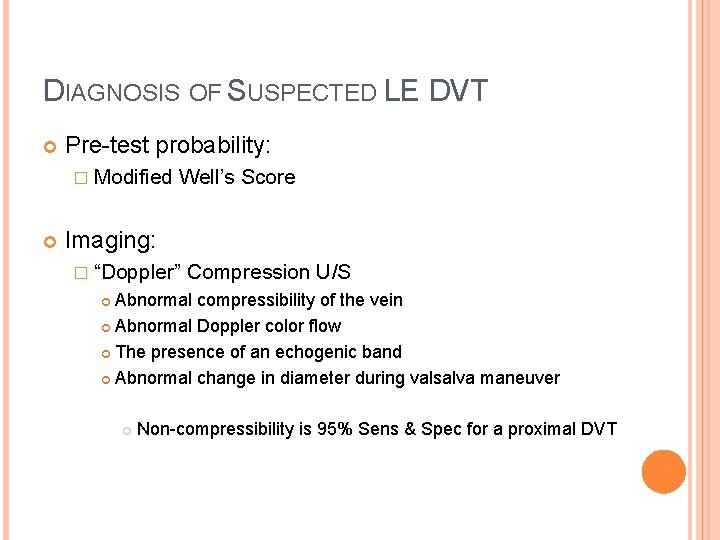
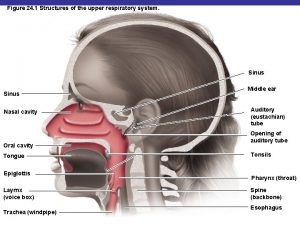
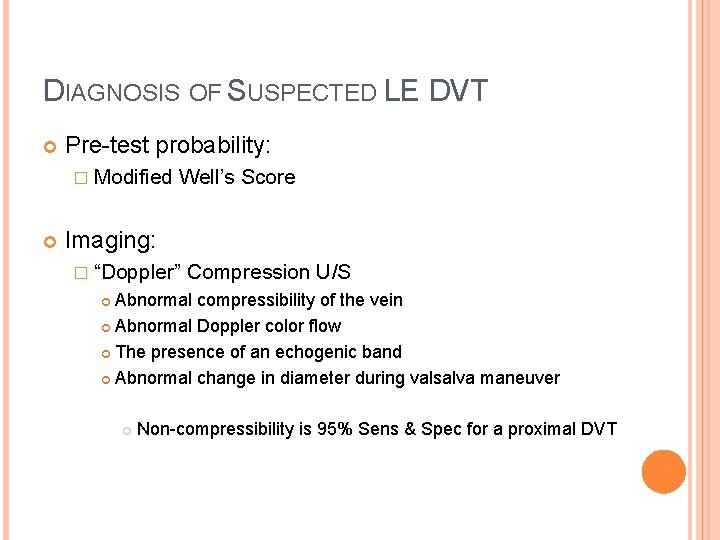
DIAGNOSIS OF SUSPECTED LE DVT Pre-test probability: � Modified Well’s Score Imaging: � “Doppler” Compression U/S Abnormal compressibility of the vein Abnormal Doppler color flow The presence of an echogenic band Abnormal change in diameter during valsalva maneuver Non-compressibility is 95% Sens & Spec for a proximal DVT
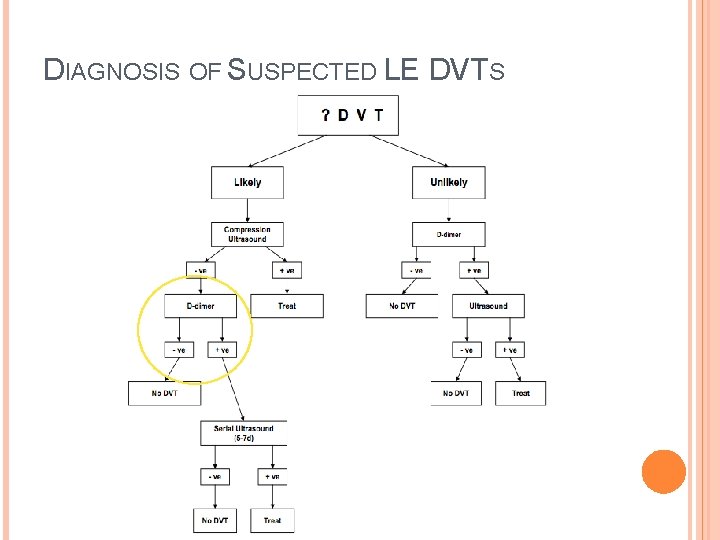
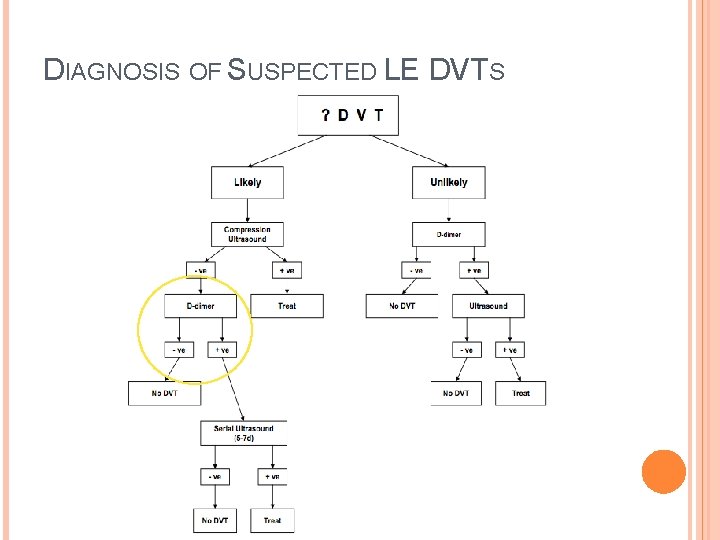
DIAGNOSIS OF SUSPECTED LE DVTS
DIAGNOSTIC IMAGING MODALITIES: BEYOND U/S Contrast Venography Non-invasive Tests: � Impedance Sensitivity 91%; Specificity 96 % � MRI Plethysmography Venography Sens 100%; Spec 96% � CT Venography

AT RCH: HIGH SUSPICION & -DOPPLER U/S Options: Order D-dimer: if positive bring patient back for repeat U/S in 5 -7 days Order more imaging: CT Venogram � May be best option to rule out causes of pelvis compression ie mass and to assess iliac vessels MR Venogram Repeat U/S in 1 week without D-dimer
MANAGEMENT OF DVTS: BEYOND ANTICOAGULATION Thrombolytics Surgical thrombectomy Percutaneous mechanical thrombectomy Potential indications: � Hemodynamically unstable PE � Massive iliofemoral thrombosis � May Thurner syndrome
THROMBOLYTICS May result in more rapid and complete lysis of LE DVT & less post-thrombotic syndrome However, seldom used because: � Clinical relevance of achieving earlier relief of venous obstruction is uncertain � Increased risk of major bleeding � Low risk of death and early recurrence if anticoagulants are started promptly at an appropriate dose � Increased risk of catastrophic bleeding may not be worth preventing post-thrombotic syndrome
THROMBOLYTICS Indications: � Massive proximal LE or iliofemoral thrombosis PLUS Severe symptomatic swelling or Limb-threatening ischemia (phlegmasia cerulea dolens)
TAKE HOME POINTS In patients with recurrent left sided DVT consider May Thurner syndrome In patients with a high probability of DVT a single negative U/S study may be insufficient � Repeat the U/S in 5 -7 days or � Consider adding a D-dimer at the time of the initial workup or � Consider other imaging modalities ie CT venogram
 Right hypotenuse leg
Right hypotenuse leg Licence pro cimi
Licence pro cimi Yengeç çimi
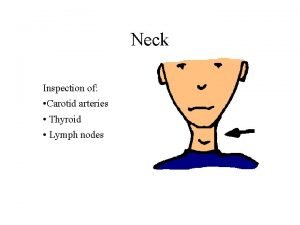
Yengeç çimi Carotid node
Carotid node Tiny glow worm tenderness
Tiny glow worm tenderness Thirotoxicosis
Thirotoxicosis Infraclavicular node
Infraclavicular node Epitrochlear lymph node
Epitrochlear lymph node Cimi el limonar
Cimi el limonar Swollen lymph nodes
Swollen lymph nodes Fox landing cimi
Fox landing cimi Whose name means “swollen foot”?
Whose name means “swollen foot”? Where is your thyroid
Where is your thyroid What is cimi
What is cimi Best worst and average case
Best worst and average case Tư thế ngồi viết
Tư thế ngồi viết Bảng số nguyên tố
Bảng số nguyên tố đặc điểm cơ thể của người tối cổ
đặc điểm cơ thể của người tối cổ Các châu lục và đại dương trên thế giới
Các châu lục và đại dương trên thế giới Cách giải mật thư tọa độ
Cách giải mật thư tọa độ Thang điểm glasgow
Thang điểm glasgow ưu thế lai là gì
ưu thế lai là gì Thẻ vin
Thẻ vin Cái miệng bé xinh thế chỉ nói điều hay thôi
Cái miệng bé xinh thế chỉ nói điều hay thôi