ROOT CANAL FILLING MATERIALS INTRODUCTION w Bacteria Apical
ROOT CANAL FILLING MATERIALS
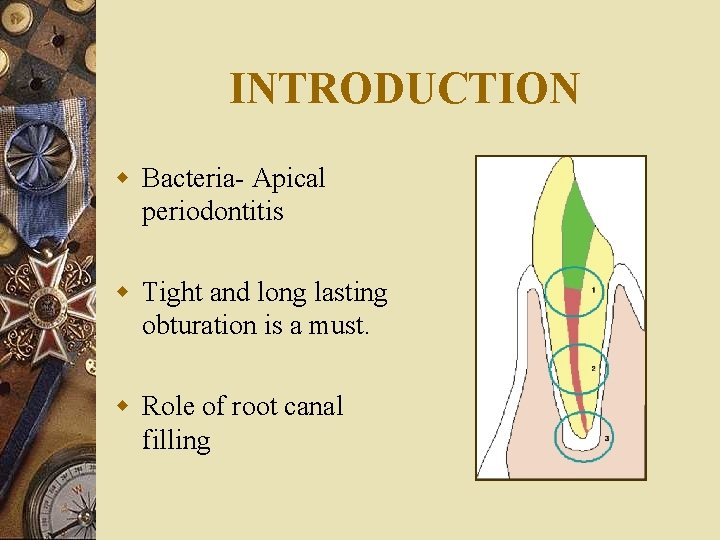
INTRODUCTION w Bacteria- Apical periodontitis w Tight and long lasting obturation is a must. w Role of root canal filling
HISTORY 200 B. C. - bronze wire found in the root canal in the skull of a Nabatean warrior 1825 - Gold foil by Edward Hudson Other material 1847 - Hill developed first gutta –percha material known as Hill’s stopping
1848 - G. P. was patented and first used as insulation for undersea cables 1867 - Bowman, 1 st use of gutta percha for canal filling in an extracted first molar 1883 - Perry claimed the use of Pointed gold wire wrapped with some soft G. P.
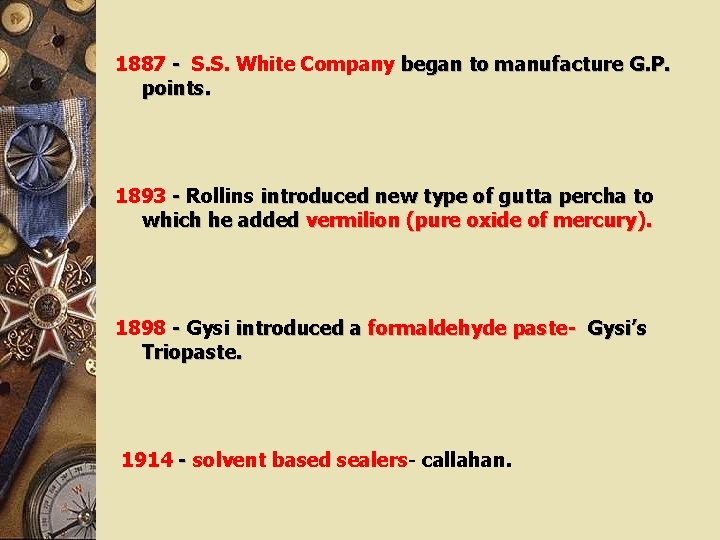
1887 - S. S. White Company began to manufacture G. P. points. 1893 - Rollins introduced new type of gutta percha to which he added vermilion (pure oxide of mercury). 1898 - Gysi introduced a formaldehyde paste- Gysi’s Triopaste. 1914 - solvent based sealers- callahan.
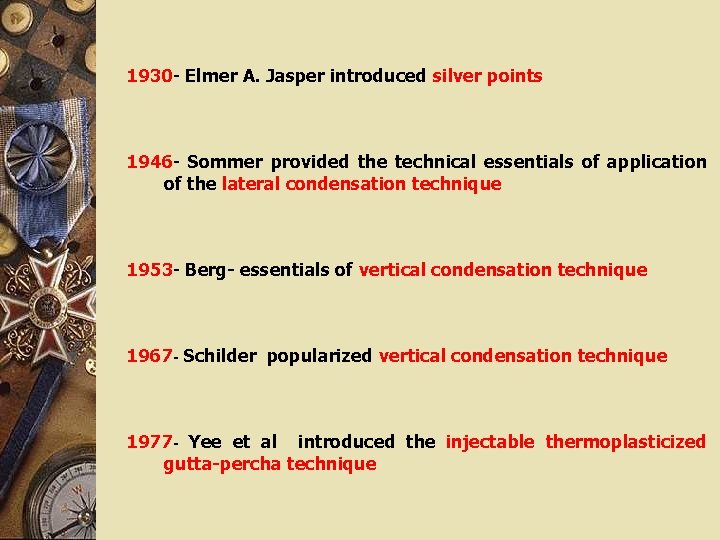
1930 - Elmer A. Jasper introduced silver points 1946 - Sommer provided the technical essentials of application of the lateral condensation technique 1953 - Berg- essentials of vertical condensation technique 1967 - Schilder popularized vertical condensation technique 1977 - Yee et al introduced the injectable thermoplasticized gutta-percha technique
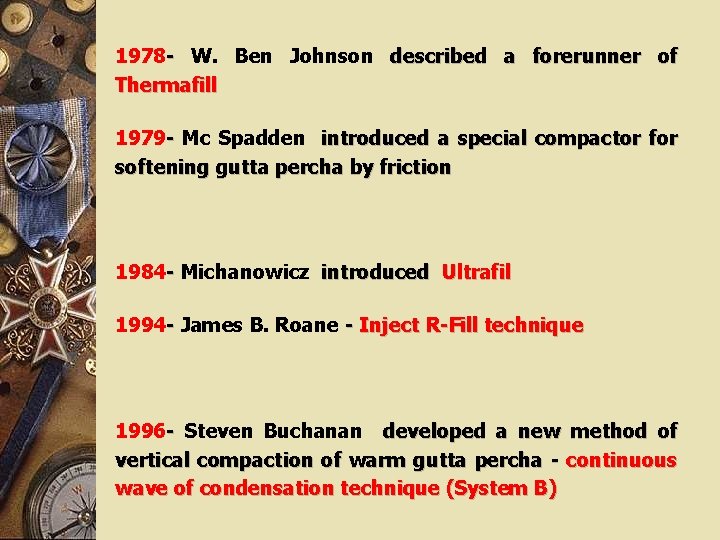
1978 - W. Ben Johnson described a forerunner of Thermafill 1979 - Mc Spadden introduced a special compactor for softening gutta percha by friction 1984 - Michanowicz introduced Ultrafil 1994 - James B. Roane - Inject R-Fill technique 1996 - Steven Buchanan developed a new method of vertical compaction of warm gutta percha - continuous wave of condensation technique (System B)
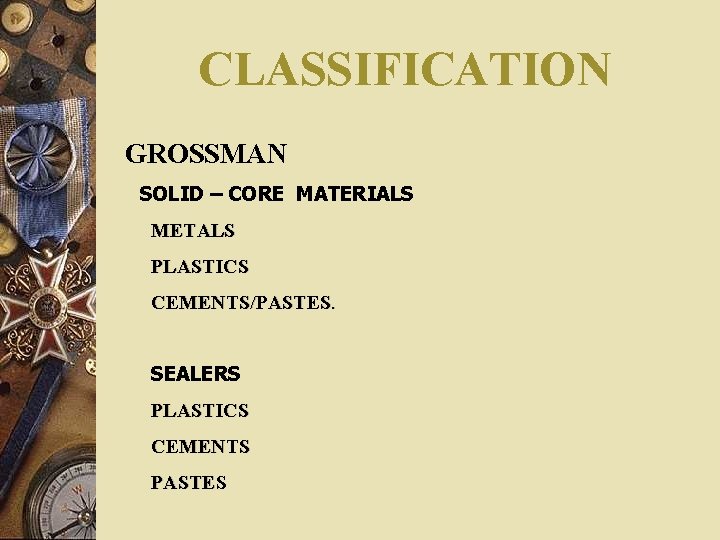
CLASSIFICATION GROSSMAN SOLID – CORE MATERIALS METALS PLASTICS CEMENTS/PASTES. SEALERS PLASTICS CEMENTS PASTES
GUNNAR CONES SEALERS COMBINATION OF TWO

INGLE SOLID CORE FILLING MATERIALS SEMI- SOLID CORE FILLING MATERIALS PASTE FILLING MATERIALS
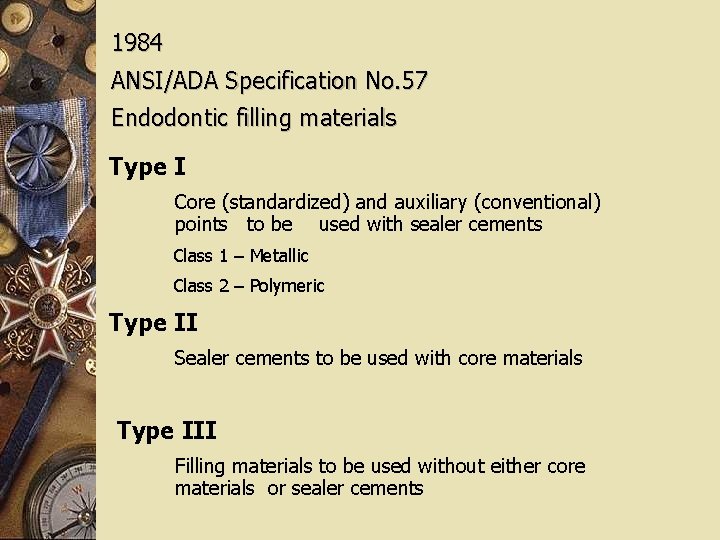
1984 ANSI/ADA Specification No. 57 Endodontic filling materials Type I Core (standardized) and auxiliary (conventional) points to be used with sealer cements Class 1 – Metallic Class 2 – Polymeric Type II Sealer cements to be used with core materials Type III Filling materials to be used without either core materials or sealer cements
REVISED CLASSIFICATION (1993 &1994) Endodontic obturation points- ADA NO. 78 Endodontic sealing materials- ADA NO. 57
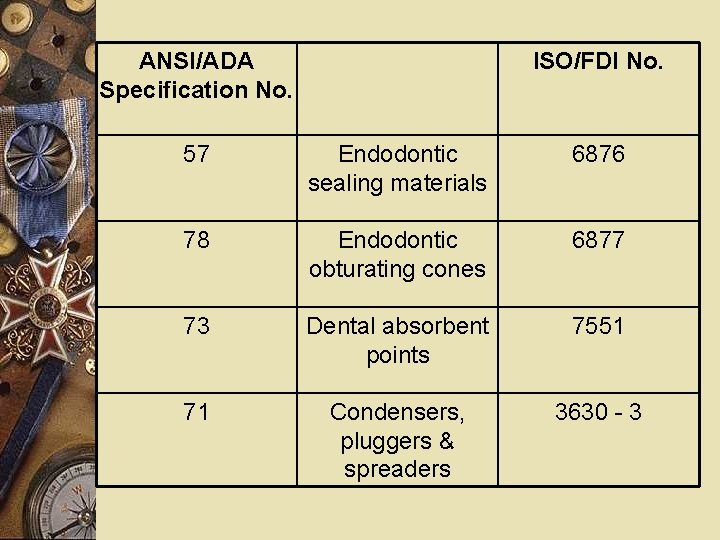
ANSI/ADA Specification No. ISO/FDI No. 57 Endodontic sealing materials 6876 78 Endodontic obturating cones 6877 73 Dental absorbent points 7551 71 Condensers, pluggers & spreaders 3630 - 3
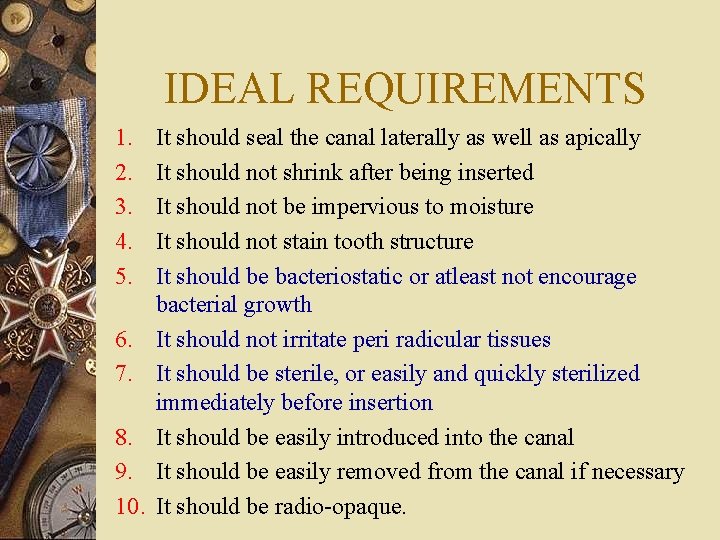
IDEAL REQUIREMENTS 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. It should seal the canal laterally as well as apically It should not shrink after being inserted It should not be impervious to moisture It should not stain tooth structure It should be bacteriostatic or atleast not encourage bacterial growth It should not irritate peri radicular tissues It should be sterile, or easily and quickly sterilized immediately before insertion It should be easily introduced into the canal It should be easily removed from the canal if necessary It should be radio-opaque.
SILVER POINTS w Introduced by. . w Advantages w Disadvantages w Not bieng used today

GUTTAPERCHA w History Mazer wood -1600 Guttapercha -1840 Best known use- “gutties”
w SOURCE Natural guttapercha- Taban tree other sources w CHEMISTRY Natural rubber - 1, 4 - cispolyisoprene Guttapercha – 1, 4 - trans polyisoprene


CRYSTALLINE FORMS w α ---- runny, tacky and sticky (lower viscosity- good flow) w β ---- solid, compactible and elongatible (higher viscosity)

COMPOSITION w Guttapercha - 18 -22% w Zinc oxide - 59 - 79% w Heavy metal salts- 1 -17% w Waxes & resins - 1 -4%
CURRENT FORMS w Solid core Gutta-percha points Standardized Non standardized w Thermo mechanical compactible Gutta-percha w Thermo plasticized Gutta-percha w Carrier based Gutta-percha w Medicated Gutta-percha

THERMO PLASTICIZED GUTTAPERCHA w Concept – yee et al w Used w Classified

OBTURA SYSTEM

ELEMENTS CALAMUS

ULTRAFIL Low temp. system 3 viscosities
THERMO MECHANICAL COMPACTIBLE GUTTA-PERCHA w Concept- Mc Spadden w Original- Mc Spadden w Later – Microseal system
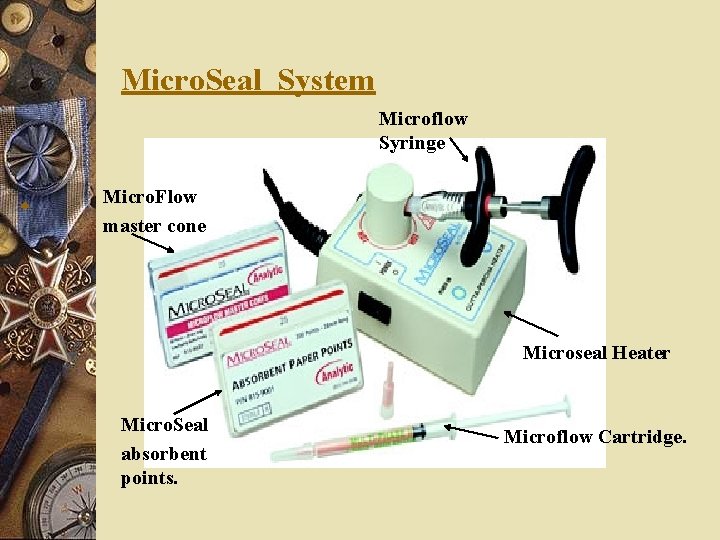
HERMOMECHANICAL COMPACTION Micro. Seal System Microflow Syringe Micro. Flow w master cone Microseal Heater Micro. Seal absorbent points. Microflow Cartridge.

TECHNIQUE
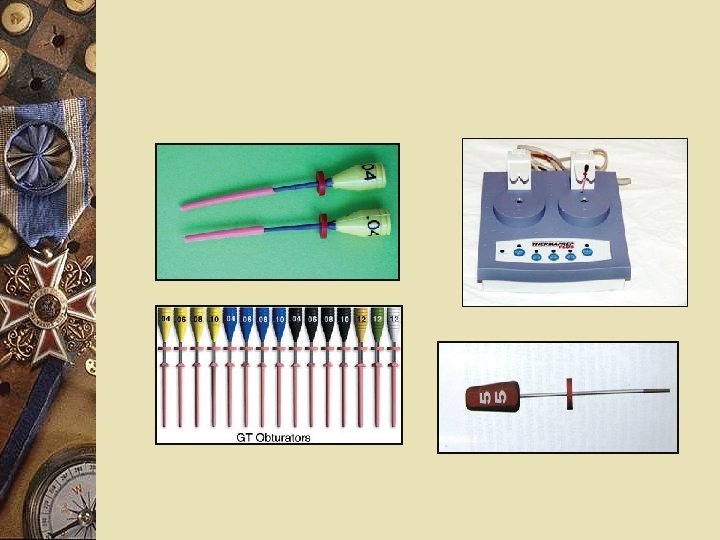
CARRIER BASED GUTTAPERCHA w Concept- Johnson w Products Thermafil plus obturators G T obturators Protaper obturators Densfil Soft core

w Iodoform G. P. with Ca. OH w Activ point
w Rejuvenation of G. P. w Sterilization of G. P. Most practical method of disinfection 5. 25% Na. OCL.
PROPERTIES w TECHNICAL PROPERTIES / LEAKAGE w BIOLOGICAL PROPERTIES Seltzer- overextension/overfilling-severe inf. reaction Sjogren- size of g. p. particles- intensity of inf. response Concerns regarding cross-reactivity between g. p. & natural rubber latex.

w ANTIMICROBIAL PROPERTIES w HANDLING PROPERTIES
GUTTAFLOW Composition: Gutta-percha powder Poly-dimethylsiloxane Silicone oil Paraffin oil Platinum catalyst Nano-silver Coloring agents
Capsule Gutta. Flow® consists of two components (paste-system) special capsule for single use each capsule can fill 3 -4 canals Canal Tip for a fast, easy and safe application uses a luer lock design flexible, for easy delivery of product
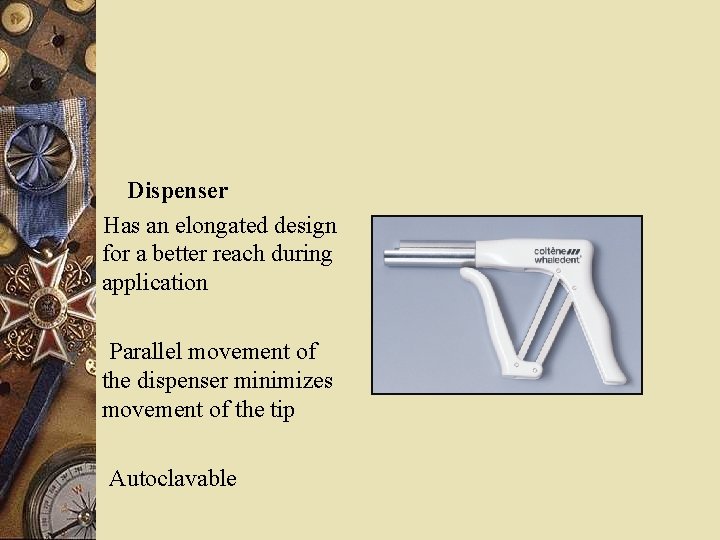
Dispenser Has an elongated design for a better reach during application Parallel movement of the dispenser minimizes movement of the tip Autoclavable
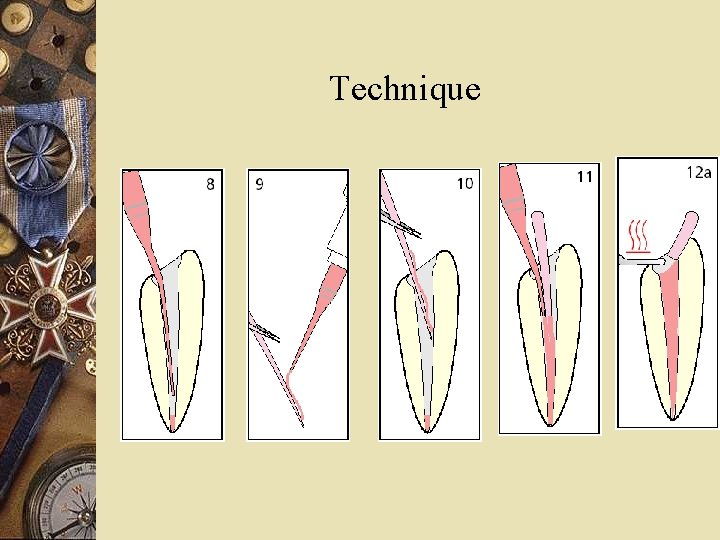
Technique

w Advantages w Disadvantages

RESILON w Resilon system Primer Sealer Core material Thinning agent
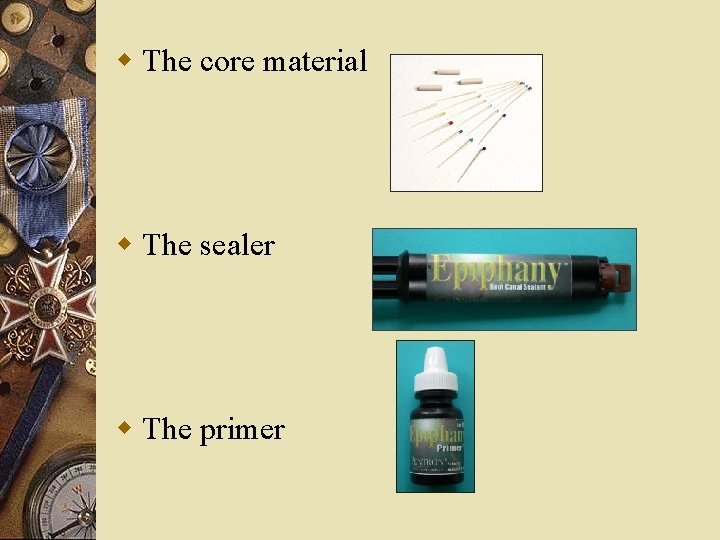
w The core material w The sealer w The primer
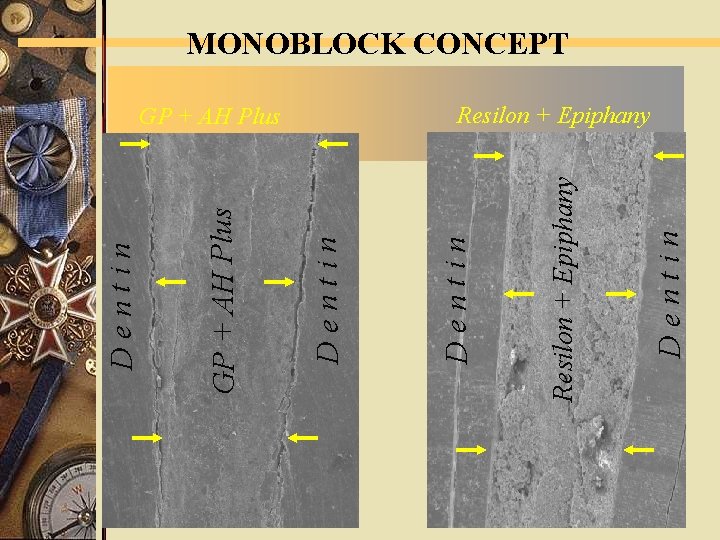
D e n t i n Resilon + Epiphany GP + AH Plus D e n t i n MONOBLOCK CONCEPT Resilon + Epiphany

USING Real. Seal™ WITH SYSTEM B Set the temperature to 150° C and the power to 10. USING Real. Seal™ WITH THE OBTURA GUN • For the 25 gauge needle tips, set the temperature to 160° C. • For the 23 gauge needle tips, set the temperature to 140° C. • For the 20 gauge needle tips, set the temperature to 120130° C.
Studies on resilon w Nielsen & Baumgartner examined depth of Ni-Ti spreader penetration in root canals having 0. 04 preparation size using. 02 and. 04 taper master GP and Resilion points. w A significant diff was noticed. w The depth of penetration is greatest for. 02 taper Resilon followed by. 02 taper GP then. 04 taper Resilon and. 04 taper GP
w Shipper et al investigated resistance to bacterial penetration of GP with AH 26 sealer, GP with Epiphany and Resilon with epiphany. w Lateral and vertical condensation techniques were used for obturation. w The resilon group had least leakage irrespective of the technique used.
w Resilon had been reported to reinforce root canal system. A study was conducted to compare cohesive strength and stiffness of Resilon and GP. w They found that both Resilon and GP did not have enough stiffness so that they could reinforce the roots.

w Tay et al evaluated biodegradation of Resilon and GP, polycaprolactone disc to hydrolytic enzymes of saliva, enzyme secretion by bacteria. w GP showed weight gain with enzyme lipase polysaccharide and cholesterol esterase. But Resilon and polycaprolactone showed extensive weight loss and glass filler particles were exposed leading to rough surface.
PASTE FILLING MATERIALS w Types Zinc-oxide & eugenol + other additives Plastics w Placement w Adv & Disadv.

MTA • Developed by. . • COMPOSITION

CLINICAL APPLICATIONS OF MTA Pulp capping Perforation repair Root resorption Root end filling Apexification
TECHNICAL PROPERTIES w MTA has outstanding sealing ability. This has been verified in many studies using MTA as a root- end filling material. Torabinejad et al. using an aqueous solution of rhodamine B fluorescent dye found MTA leaked significantly less than amalgam or ethoxybenzoic acid (Supper EBA) as a root- end filling material. w In another dye study, Torabinejad et al. found MTA sealed better as a root- end filling material than amalgam, intermediate restorative material (IRM), or Super EBA, even in the presence of blood contamination.

BIOCOMPATIBILITY w Cell culture studies have demonstrated that the cytotoxicity of MTA was significantly less than that of IRM or Super EBA. w Implantation of MTA into tibias and mandibles of guinea pigs resulted in a tissue reaction considered favorable and slightly milder than that of Super EBA. w Koh et al. found favourable biologic responses to MTA from human osteoblasts, and favourable cellular response to MTA.
w MTA is also reported to have qualities that may provide an environment for repair and regeneration of periapical tissues. w MTA has shown an inductive effect on cementoblasts in dogs and monkeys. w Zhu et al. showed osteoblasts attaching and spreading on MTA. w Regan et al. demonstrated that both MTA and Diaket can support almost complete regeneration of the periradicular periodontium when used as a root- end filling material on teeth that are not infected. w Back et al. found that MTA showed the most favorable periapical tissue response and that there was neoformation of cemental coverage over MTA.
w. ANTIMICROBIAL PROPERTIES w. MTA has some effect on a few facultative bacteria, which may be due to the high p. H. (Torabinejad et al, 1995) w MTA also demonstrates an antifungal effect against Candida albicans.
HANDLING PROPERTIES The MTA powder is mixed with sterile water at a ratio of 3: 1. It can be mixed on a glass slab or a paper pad, with the help of a plastic or a metal spatula
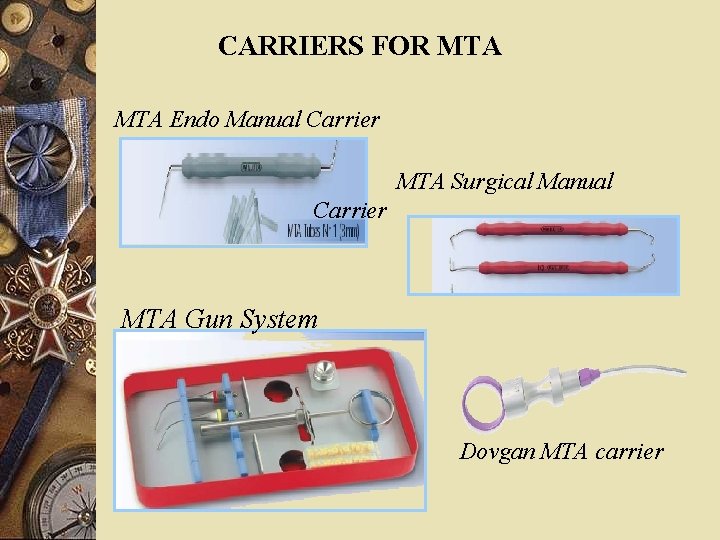
CARRIERS FOR MTA Endo Manual Carrier MTA Surgical Manual Carrier MTA Gun System Dovgan MTA carrier
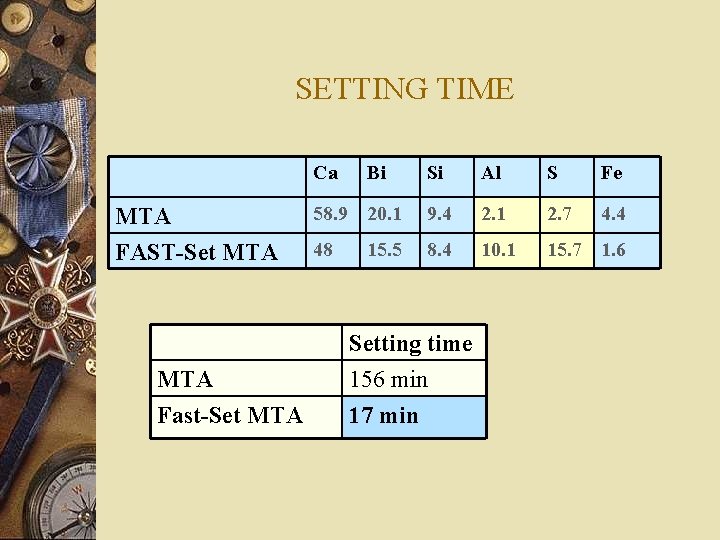
SETTING TIME Ca MTA FAST-Set MTA Fast-Set MTA Bi Si Al S Fe 58. 9 20. 1 9. 4 2. 1 2. 7 4. 4 48 8. 4 10. 1 15. 7 1. 6 15. 5 Setting time 156 min 17 min

ROOT CANAL SEALERS

w Definition w Functions
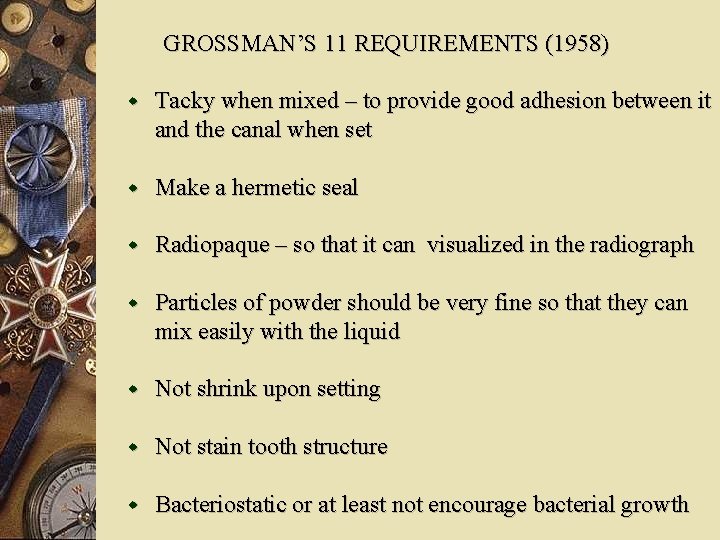
GROSSMAN’S 11 REQUIREMENTS (1958) w Tacky when mixed – to provide good adhesion between it and the canal when set w Make a hermetic seal w Radiopaque – so that it can visualized in the radiograph w Particles of powder should be very fine so that they can mix easily with the liquid w Not shrink upon setting w Not stain tooth structure w Bacteriostatic or at least not encourage bacterial growth

w Set slowly w Insoluble in tissue fluids w Tissue tolerant i. e. , nonirritating to periradicular tissue w Soluble in a common solvent if it is necessary to remove the root canal filling ADDITIONAL REQUIREMENTS w Not provoke an immune response in periradicular tissue w Neither mutagenic nor carcinogenic
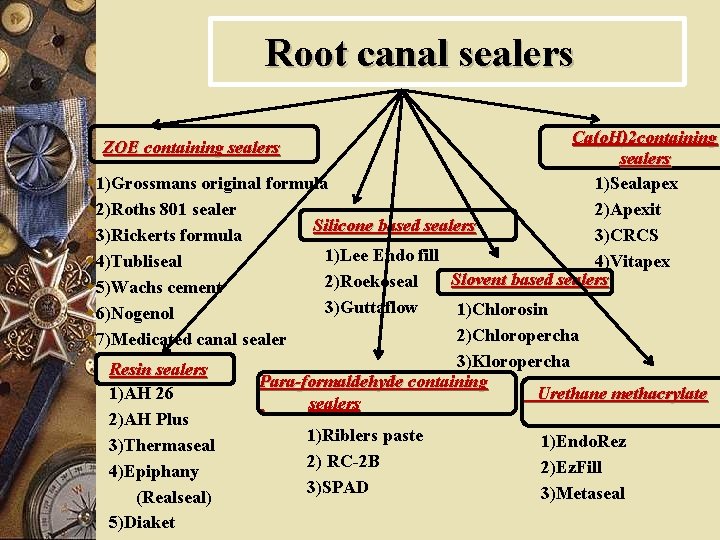
Root canal sealers Ca(o. H)2 containing sealers w 1)Grossmans original formula 1)Sealapex w 2)Roths 801 sealer 2)Apexit Silicone based sealers w 3)Rickerts formula 3)CRCS 1)Lee Endo fill w 4)Tubliseal 4)Vitapex Slovent based sealers 2)Roekoseal w 5)Wachs cement ZOE containing sealers Resin sealers 1)AH 26 2)AH Plus 3)Thermaseal 4)Epiphany (Realseal) 5)Diaket 3)Guttaflow 1)Chlorosin 2)Chloropercha 3)Kloropercha Para-formaldehyde containing Urethane methacrylate sealers w 6)Nogenol w 7)Medicated canal sealer 1)Riblers paste 2) RC-2 B 3)SPAD 1)Endo. Rez 2)Ez. Fill 3)Metaseal
COHEN’S TYPE I CLASS 1 CLASS 2 CLASS 3 TYPE II CLASS 1 CLASS 2 CLASS 3 CLASS 4.
HARTY F. J Zinc-oxide eugenol based. Resin based. GP based. Dentin adhesive materials. Materials to which medicaments have been added. a) to reduce post op pain. b) to induce cementogenesis.
CLARK Absorbable. Kerr pcs Grossman’s sealer Roth Tubliseal Non-absorbable A H 26 Diaket
ZINC OXIDE EUGENOL SEALERS
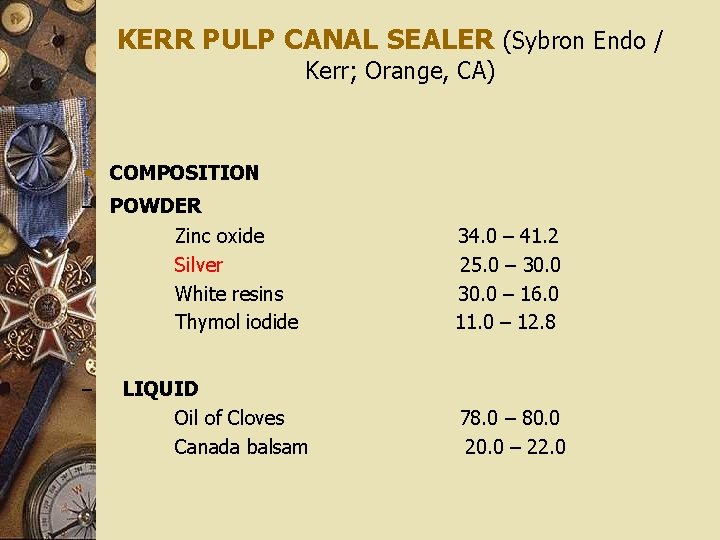
KERR PULP CANAL SEALER (Sybron Endo / Kerr; Orange, CA) w COMPOSITION – POWDER Zinc oxide Silver White resins Thymol iodide – LIQUID Oil of Cloves Canada balsam 34. 0 – 41. 2 25. 0 – 30. 0 – 16. 0 11. 0 – 12. 8 78. 0 – 80. 0 20. 0 – 22. 0

2 versions w Regular Pulp Canal Sealer w Pulp Canal Sealer EWT – Working time IS 6 hrs.

TUBLI – SEAL (Kerr Dental) TWO Paste system Base paste Catalyst paste Zinc oxide Polypale resin Barium sulphate eugenol Mineral oil thymol iodide Corn starch Lecithin ADV & DIS ADV

GROSSMAN’S SEALER/ROTH 801 GROSSMAN’S ORIGINAL FORMULA Powder: Zinc oxide Stabelite resin Bismuth subcarbonate Barium sulphate Liquid: Eugenol Oil of sweet almond

w ADVANTAGES w DISADVANTAGES
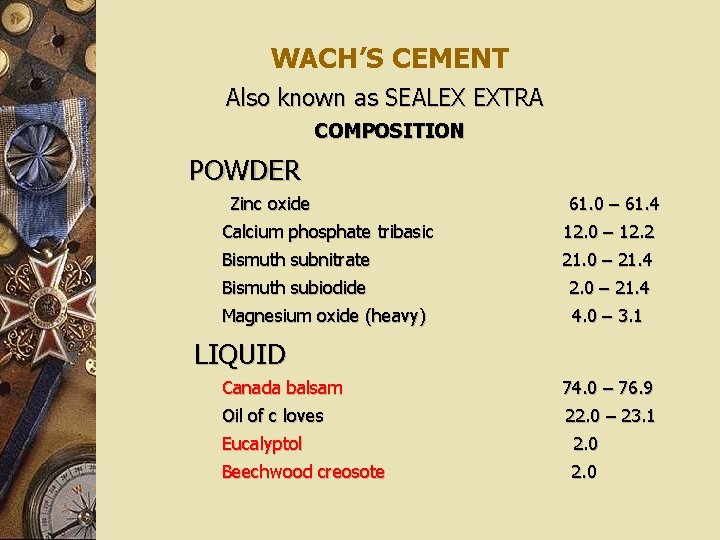
WACH’S CEMENT Also known as SEALEX EXTRA COMPOSITION POWDER Zinc oxide 61. 0 – 61. 4 Calcium phosphate tribasic 12. 0 – 12. 2 Bismuth subnitrate 21. 0 – 21. 4 Bismuth subiodide 2. 0 – 21. 4 Magnesium oxide (heavy) 4. 0 – 3. 1 LIQUID Canada balsam 74. 0 – 76. 9 Oil of c loves 22. 0 – 23. 1 Eucalyptol 2. 0 Beechwood creosote 2. 0
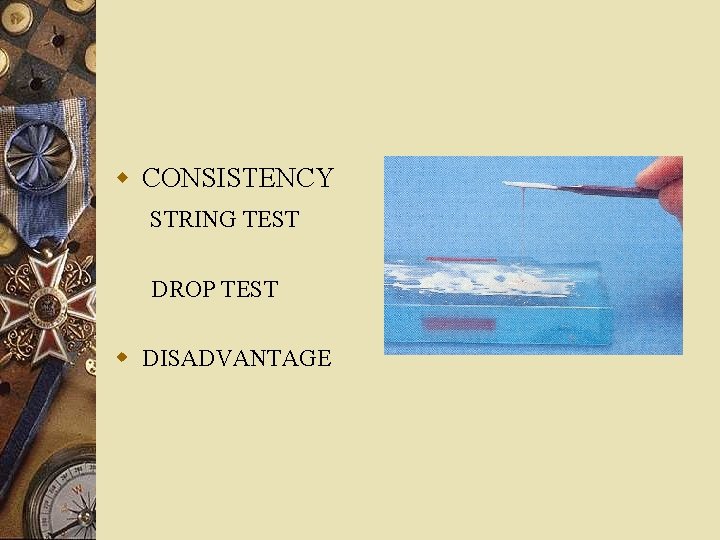
w CONSISTENCY STRING TEST DROP TEST w DISADVANTAGE
PROCOSOL By Grossman 1936 Properties similar to Wachs pastes Developed with the purpose of increasing the working time INDICATIONS

NOGENOL (G – C America) COMPOSITION BASE Zinc oxide Barium sulfate ACCELERATOR Hydrogenated rosin Methyl abietate Lauric acid Chlorothymol Salicylic acid
MEDICATED CANAL SEALER Developed by martin Contains iodoform Used with MGP

PROPERTIES w Technical properties w Biological properties w Antimicrobial w Handling
RESIN BASED SEALERS

DIAKET w Widely used in Europe either with gutta percha or alone as a paste fill material. w Supply. w Setting reaction. w Known for its resistance to absorption.
COMPOSITION POWDER Zinc oxide Bismuth phosphate LIQUID 2, 2’ Dihydroxy – 5, 5’ dichlorodiphenye methane Proprionylacetophenone (B-diketone) Triethanolamine Caproic acid Copolymers of vinylacetate, vinyl chloride and vinyl isobutyl ether

PROPERTIES w Technical properties w Biological properties. w Handling
A H 26 Derives its name from A- Aethoxylinharz (German) for ethoxyline base H- Hexamethylene tetramine 26 - Was the test number Developed by. .
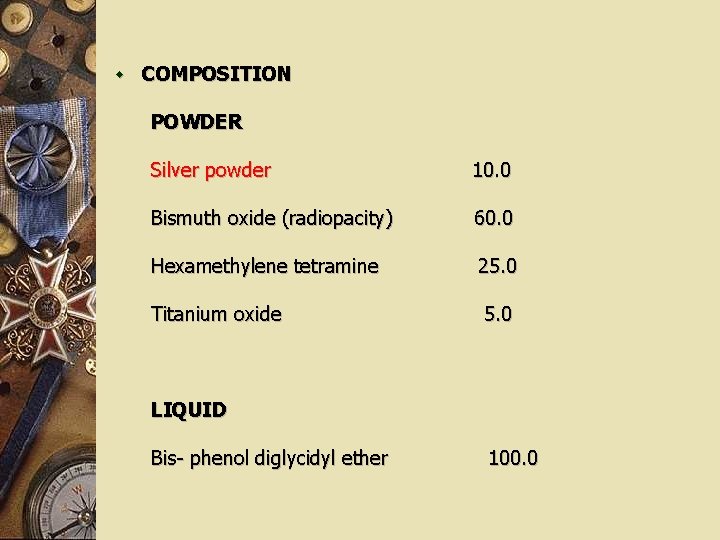
w COMPOSITION POWDER Silver powder 10. 0 Bismuth oxide (radiopacity) 60. 0 Hexamethylene tetramine 25. 0 Titanium oxide 5. 0 LIQUID Bis- phenol diglycidyl ether 100. 0

PROPERTIES w Technical properties w Biological properties. w Handling w Disadvantages

A H PLUS Epoxy Paste Amine Paste Epoxy Resin Amines Calcium tungstate Zirconium oxide Silica Iron oxide Silicone oil Advantages over AH 26
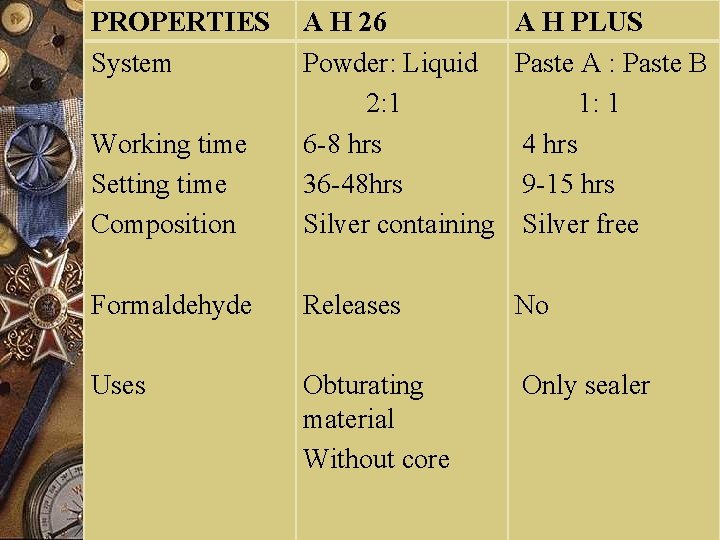
PROPERTIES System Working time Setting time Composition A H 26 Powder: Liquid 2: 1 6 -8 hrs 36 -48 hrs Silver containing A H PLUS Paste A : Paste B 1: 1 4 hrs 9 -15 hrs Silver free Formaldehyde Releases No Uses Obturating material Without core Only sealer

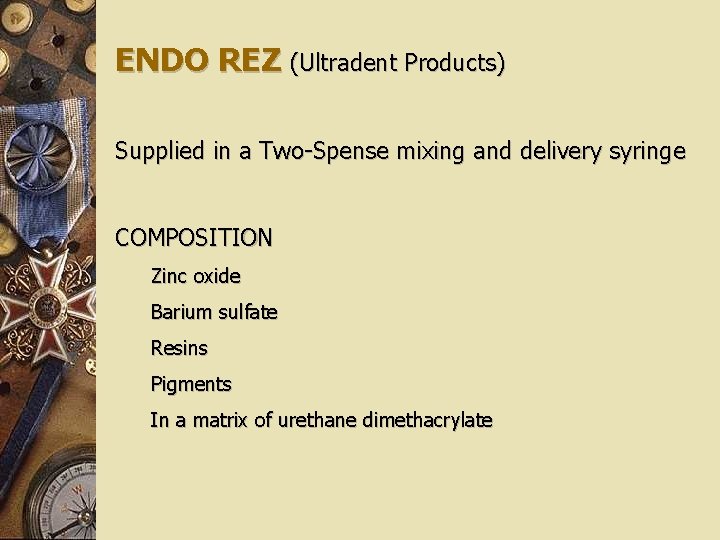
ENDO REZ (Ultradent Products) Supplied in a Two-Spense mixing and delivery syringe COMPOSITION Zinc oxide Barium sulfate Resins Pigments In a matrix of urethane dimethacrylate
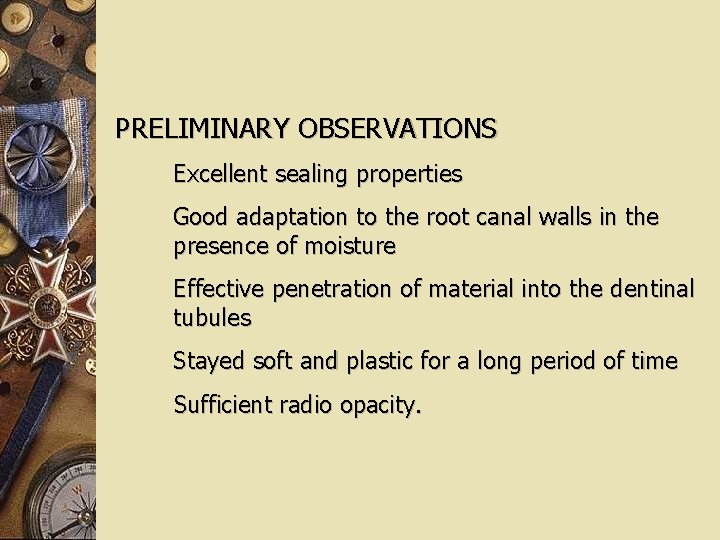
PRELIMINARY OBSERVATIONS Excellent sealing properties Good adaptation to the root canal walls in the presence of moisture Effective penetration of material into the dentinal tubules Stayed soft and plastic for a long period of time Sufficient radio opacity.
FIBREFILL ROOT CANAL SEALANT (Jeneric/ Pentron Wallingford) COMPOSITION Mixture of UDMA, PEGDMA, HDDMA and BIS-GMA resins Treated barium borosilicate glasses Barium sulfate Silica Calcium hydroxide Calcium phosphates Stabilizers Pigments Benzoyl peroxide Used in combination with a self - cured primer (Fibrefill Primer A&B)

EPIPHANY ROOT CANAL SEALANT (Pentron Clinical Technologies) is a dual-curing, hydrophilic resin sealer dispensed from a double barrel, auto-mix syringe. Matrix & fillers coronal seal curing within the root canal shrinkage on polymerization.
CALCIUM HYDROXIDE SEALERS

SEALAPEX ( Sybron Endo/ Kerr, Orange, CA) COMPOSITION BASE Zinc oxide Calcium hydroxide Butyl benzene Sulfonamide Zinc stearate CATALYST Barium sulfate Titanium dioxide Isobutyl salicylate ( proprietary resin) Aerocil R 972
CRCS ( Coltene/ Whaledent Hygenic, USA) Zinc oxide - eugenol -eucalyptol base. COMPOSITION POWDER Zinc oxide Calcium hydroxide Barium sulfate Bismuth subcarbonate Hydrogenated resin ester LIQUID Eugenol Euclayptol
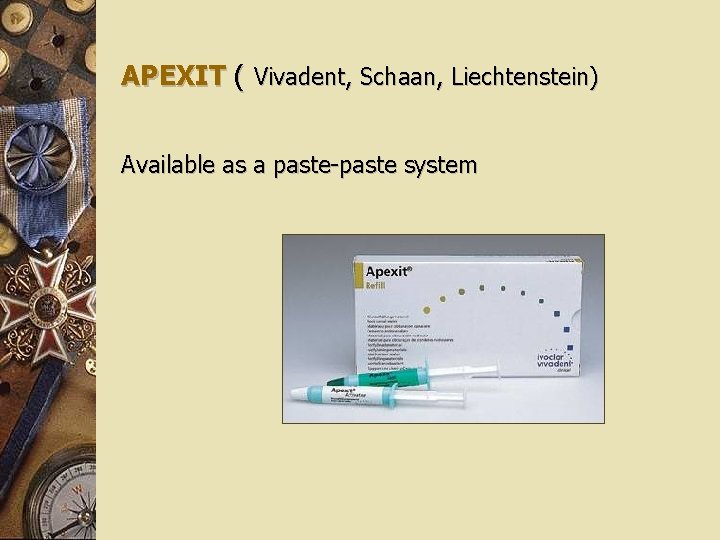
APEXIT ( Vivadent, Schaan, Liechtenstein) Available as a paste-paste system
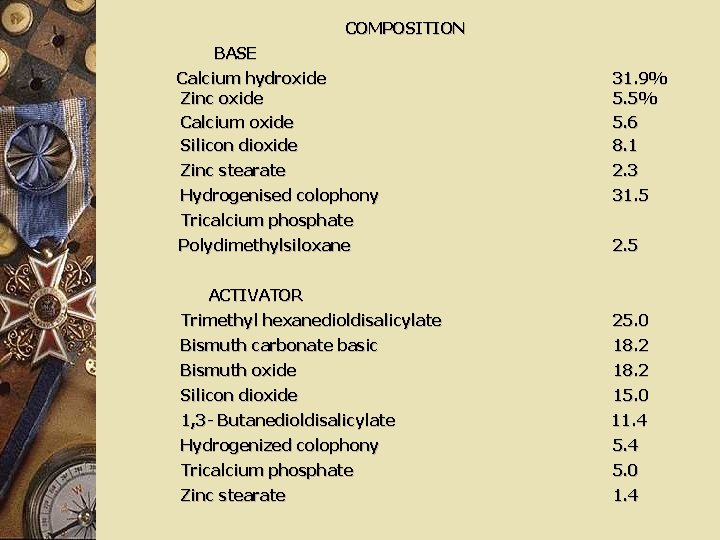
COMPOSITION BASE Calcium hydroxide Zinc oxide Calcium oxide Silicon dioxide 31. 9% 5. 5% 5. 6 8. 1 Zinc stearate 2. 3 Hydrogenised colophony 31. 5 Tricalcium phosphate Polydimethylsiloxane 2. 5 ACTIVATOR Trimethyl hexanedioldisalicylate 25. 0 Bismuth carbonate basic 18. 2 Bismuth oxide 18. 2 Silicon dioxide 15. 0 1, 3 - Butanedioldisalicylate 11. 4 Hydrogenized colophony 5. 4 Tricalcium phosphate 5. 0 Zinc stearate 1. 4

PROPERTIES w Technical properties w Biological properties w Antimicrobial w Root end closure

GLASS – I 0 N 0 MER SEALERS

KETAC-ENDO (3 M, ESPE, Minneapolis, US) Introduced by Ray & Seltzer in 1991 w Technical properties w Biological properties w Antimicrobial w Handling
FORMALDEHYDE CONTAINING SEALERS

N 2 COMPOSITION POWDER Zinc oxide Bismuth subcarbonate Bismuth subnitrate Paraformaldehyde Titanium dioxide Phenylmercuric borate Lead tetroxide LIQUID Eugenol Peanut oil Rose oil

ENDOMETHASONE ( Specialities, Septodont, France) POWDER Zinc oxide Bismuth subnitrate Dexamethasone Hydrocortisone acetate Thymol iodide Paraformaldehyde LIQUID Eugenol Peppermint oil Anise oil
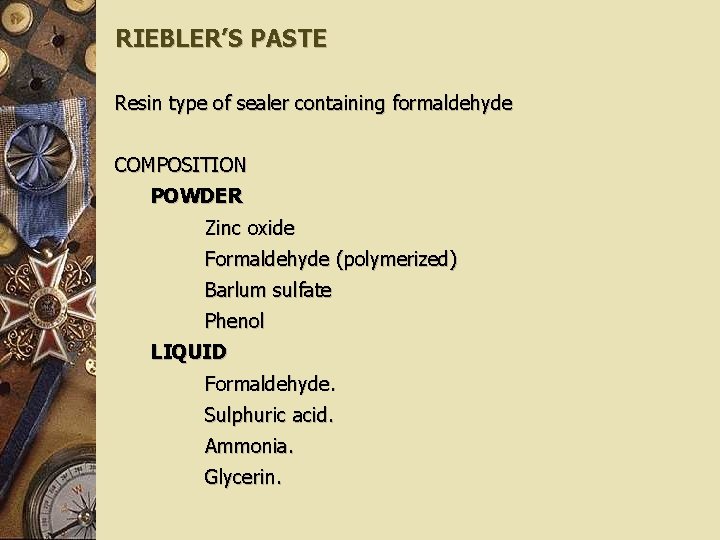
RIEBLER’S PASTE Resin type of sealer containing formaldehyde COMPOSITION POWDER Zinc oxide Formaldehyde (polymerized) Barlum sulfate Phenol LIQUID Formaldehyde. Sulphuric acid. Ammonia. Glycerin.

PROPERTIES w Technical properties w Biological properties w Handling
SOLVENT BASED SEALERS
CHLOROPERCHA (Moyco, Union Broach, York PA) Gutta – percha – 9. 0 Chloroform – 91. 0 Advantages Disadvantages
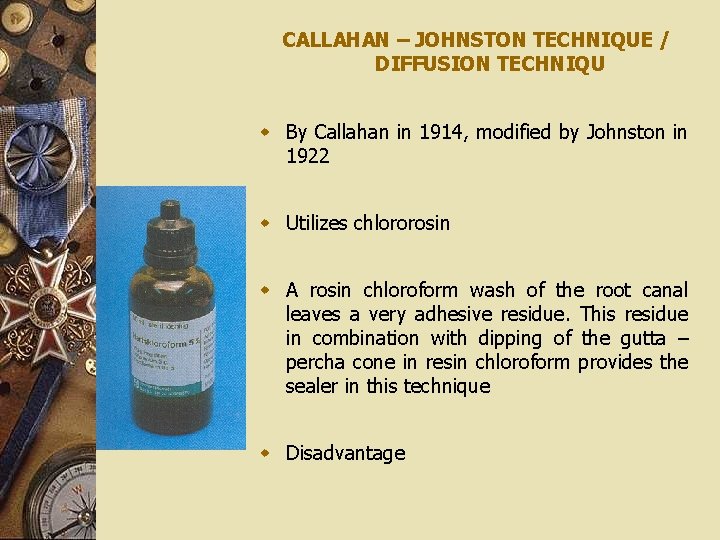
CALLAHAN – JOHNSTON TECHNIQUE / DIFFUSION TECHNIQU w By Callahan in 1914, modified by Johnston in 1922 w Utilizes chlororosin w A rosin chloroform wash of the root canal leaves a very adhesive residue. This residue in combination with dipping of the gutta – percha cone in resin chloroform provides the sealer in this technique w Disadvantage
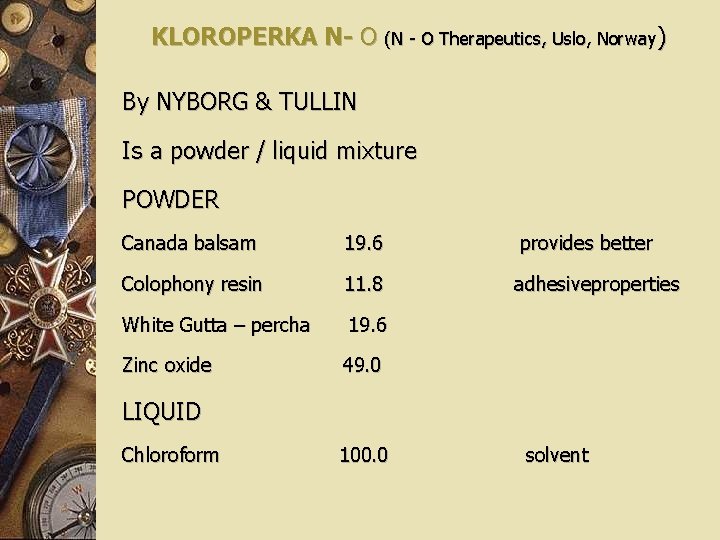
KLOROPERKA N- O (N - O Therapeutics, Uslo, Norway) By NYBORG & TULLIN Is a powder / liquid mixture POWDER Canada balsam 19. 6 provides better Colophony resin 11. 8 adhesiveproperties White Gutta – percha 19. 6 Zinc oxide 49. 0 LIQUID Chloroform 100. 0 solvent
EUCAPERCHA By Buckley Eucalyptol does not dissolve gutta percha rapidly as does chloroform Is a paste made by softening surface of gutta – percha in warm oil of eucalyptus (eucalyptol) DIS ADVANTAGES

SILICONE BASED SEALERS
LEE ENDOFILL Active ingredients. Hydroxyl terminated dimethyl polysiloxane. Undecylenic acid. Benzyl alcohol. Hydrophobic amorphous silica (10 -30µ particle size). Properties Paste is pale pink Low viscosity Disadvantages

ROEKO SEAL w Is a polyvinyl siloxane w Properties w Advantage
NEWER SEALERS
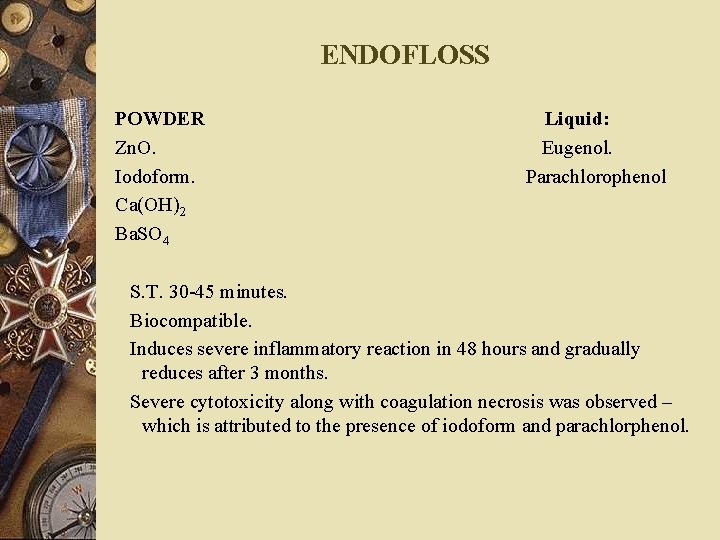
ENDOFLOSS POWDER Zn. O. Iodoform. Ca(OH)2 Ba. SO 4 Liquid: Eugenol. Parachlorophenol S. T. 30 -45 minutes. Biocompatible. Induces severe inflammatory reaction in 48 hours and gradually reduces after 3 months. Severe cytotoxicity along with coagulation necrosis was observed – which is attributed to the presence of iodoform and parachlorphenol.
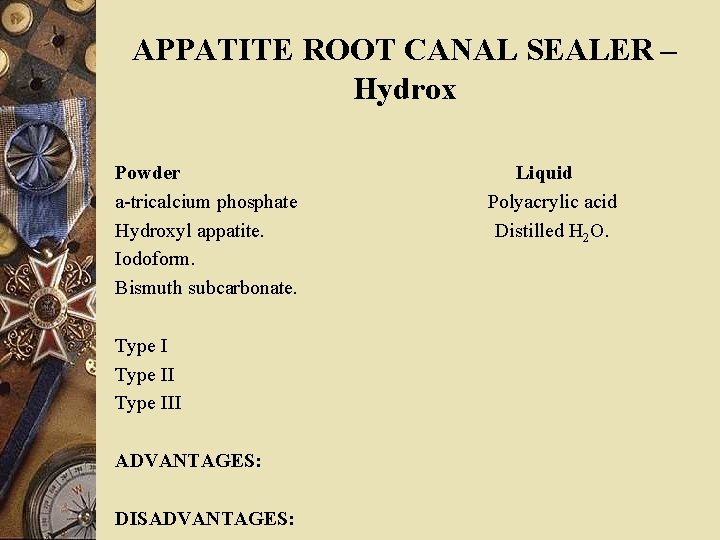
APPATITE ROOT CANAL SEALER – Hydrox Powder a-tricalcium phosphate Hydroxyl appatite. Iodoform. Bismuth subcarbonate. Type III ADVANTAGES: DISADVANTAGES: Liquid Polyacrylic acid Distilled H 2 O.
NEWLY DEVELOPED Ca. PO 4 TYPE SEALERS Tetra calcium phosphate (Te. CP). Diacalcium phosphate dihydrate (DCPD) TDM-S-Buffer solution + 2. 6% chondrotin sulphate. Composition: TDM-S Powder: Tetracalcium phosphate. Dibasic Ca phosphate. Liquid: Citric acid. Dibasic Na. PO 4. Chondrotin sulphate. Distilled H 2 O. Biocompatible. No peri-apical inflammatory reaction. Chondrotin and other ingredients said to promote wound healing.
CONCLUSION As new materials are introduced to fill the root canal system, it is important to remember Grossman’s tenets and to remember the proven success of many of the materials currently in use. With advances in materials and other aspects of endodontics, one cannot imagine materials that will be available to use in root canal syatems in the future. They, no doubt, will be much more biocompatible and one might hope, may promote regeneration of tissues within the tooth and bone.
REFERENCES w TEXT BOOK OF ENDODONTICS…BY INGLE… 5 TH AND 6 TH EDITION w ENDODONTICTHERAPY…. BY WEINE… 4 TH, 5 TH, 6 TH EDITION w PATHWAYS OF THE PULP…COHEN 9 TH AND 10 TH EDITION w GROSSMAN 11 TH EDITION w NICHOLAS w GULABIVALA w HARTYS
- Slides: 118