Role of recurrent disease for late allograft loss







- Slides: 32

Role of recurrent disease for late allograft loss Fernando G. Cosio Mayo Clinic, Rochester MN 10 th Banff conference on allograft pathology
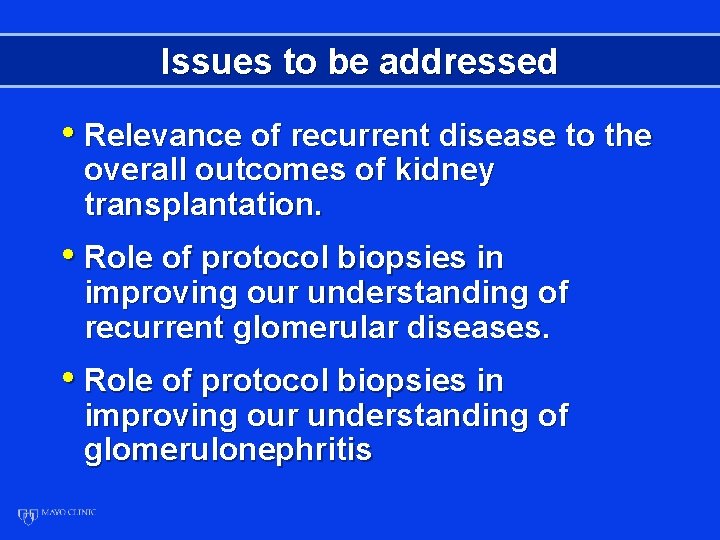
Issues to be addressed • Relevance of recurrent disease to the overall outcomes of kidney transplantation. • Role of protocol biopsies in improving our understanding of recurrent glomerular diseases. • Role of protocol biopsies in improving our understanding of glomerulonephritis
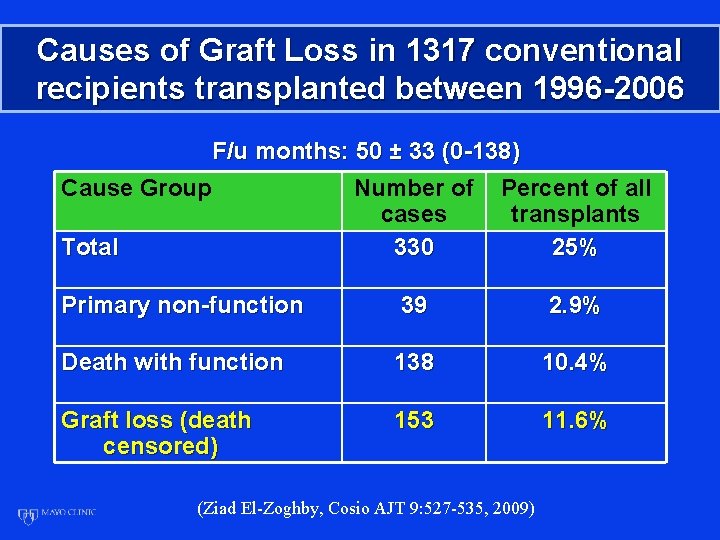
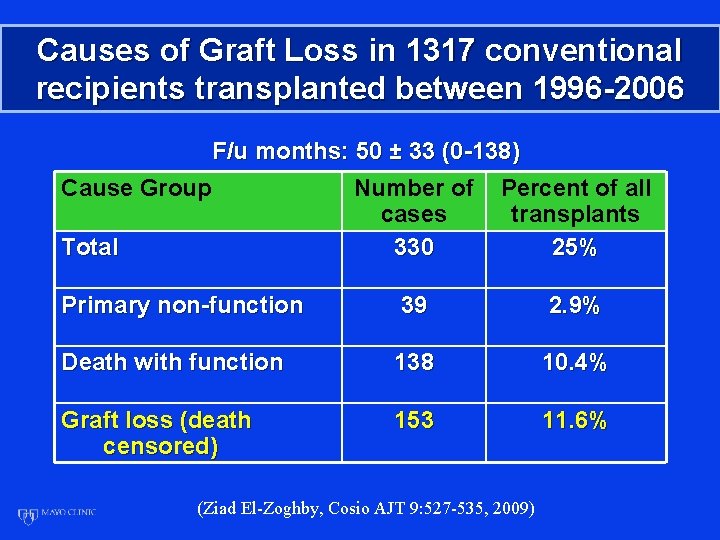
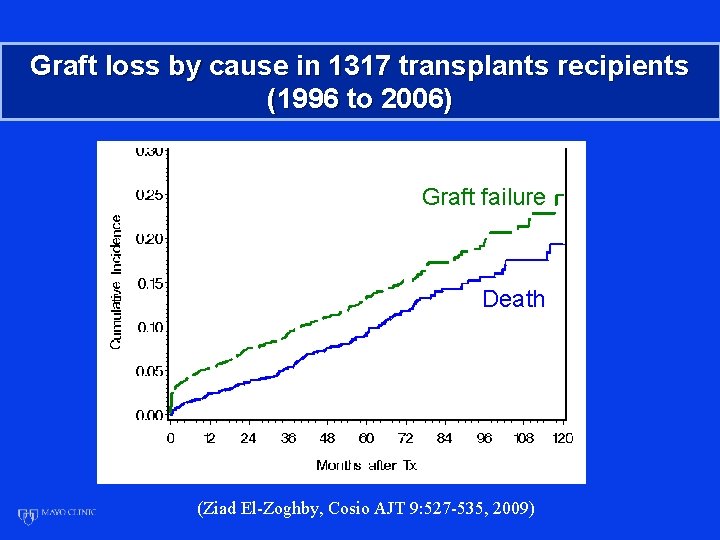
Causes of Graft Loss in 1317 conventional recipients transplanted between 1996 -2006 F/u months: 50 ± 33 (0 -138) Cause Group Number of cases 330 Percent of all transplants 25% Primary non-function 39 2. 9% Death with function 138 10. 4% Graft loss (death censored) 153 11. 6% Total (Ziad El-Zoghby, Cosio AJT 9: 527 -535, 2009)

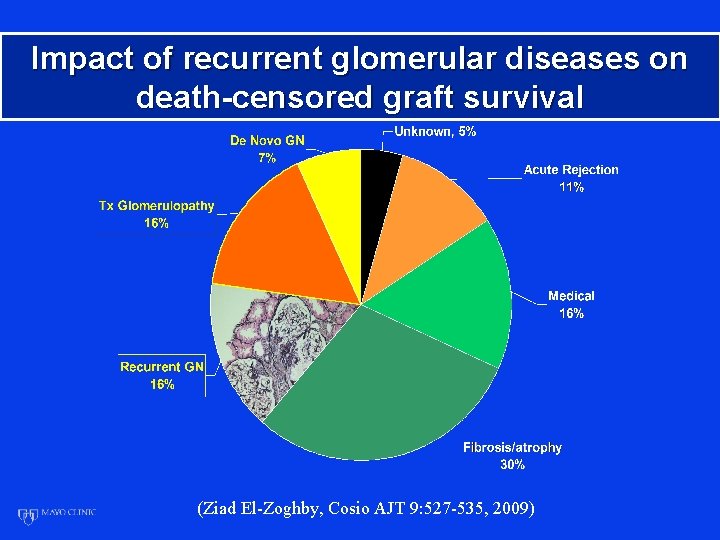
Mechanisms of death-censored kidney graft loss (1996 -2006) 1317 transplants 153 losses Cell-mediated Antibody-mediated (Ziad El-Zoghby, Cosio et al AJT 9: 527 -535, 2009)
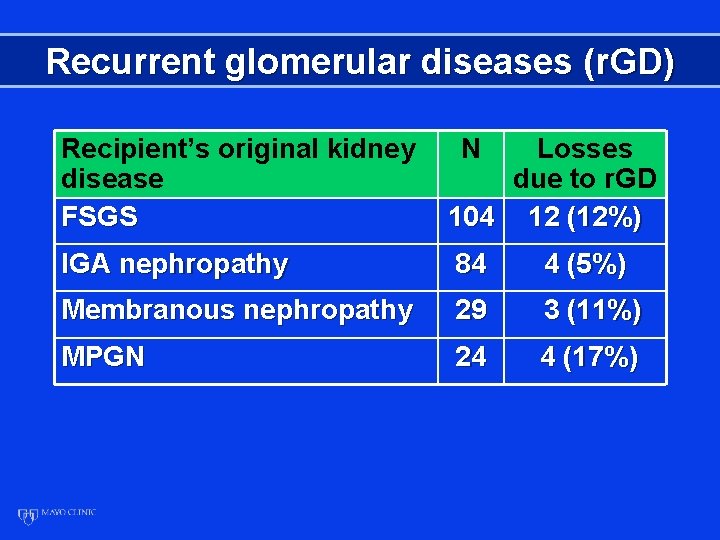
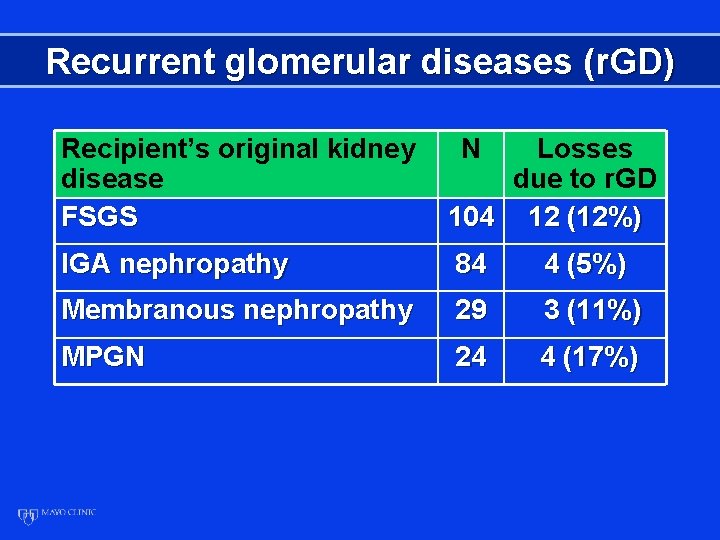
Recurrent glomerular diseases (r. GD) Recipient’s original kidney disease FSGS N Losses due to r. GD 104 12 (12%) IGA nephropathy 84 4 (5%) Membranous nephropathy 29 3 (11%) MPGN 24 4 (17%)
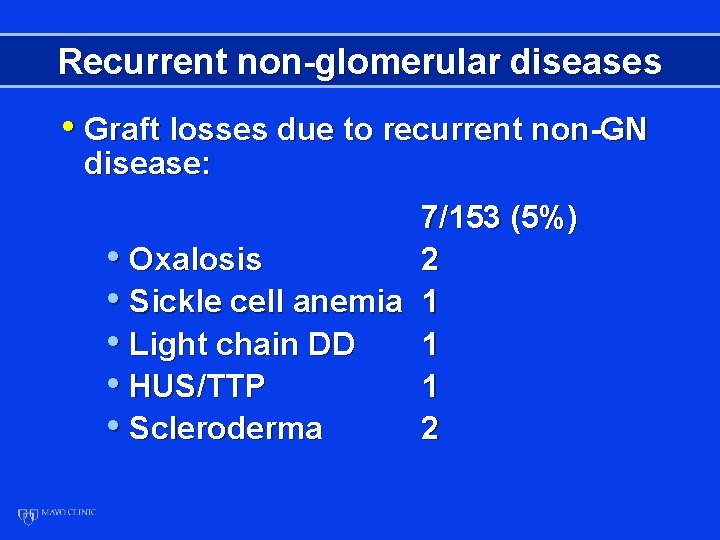
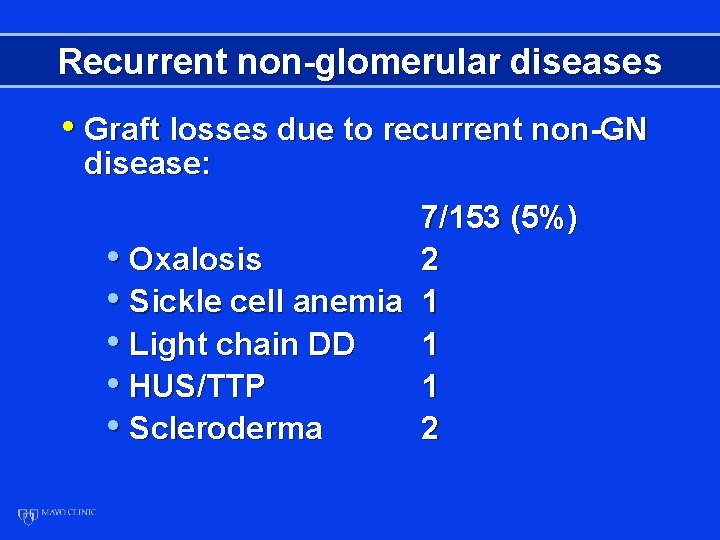
Recurrent non-glomerular diseases • Graft losses due to recurrent non-GN disease: 7/153 (5%) • Oxalosis 2 • Sickle cell anemia 1 • Light chain DD 1 • HUS/TTP 1 • Scleroderma 2
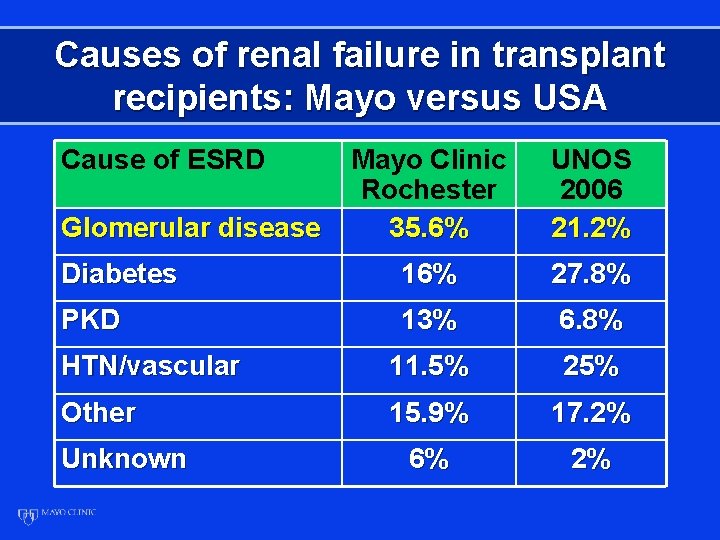
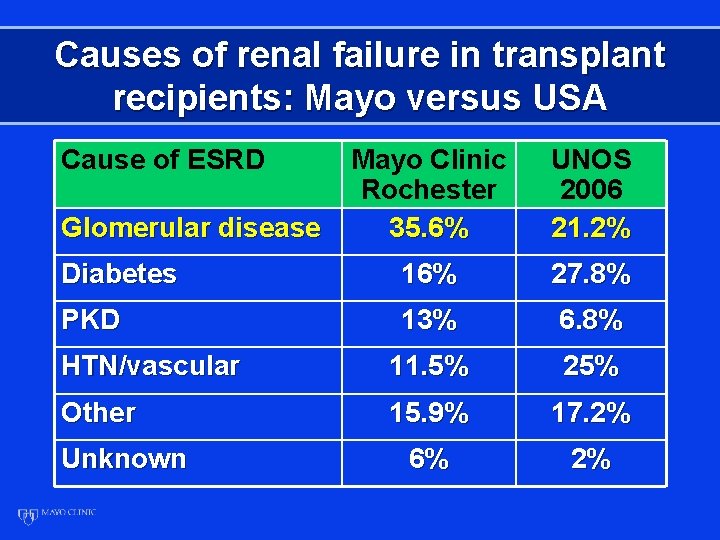
Causes of renal failure in transplant recipients: Mayo versus USA Cause of ESRD Mayo Clinic Rochester 35. 6% UNOS 2006 21. 2% Diabetes 16% 27. 8% PKD 13% 6. 8% HTN/vascular 11. 5% 25% Other 15. 9% 17. 2% 6% 2% Glomerular disease Unknown
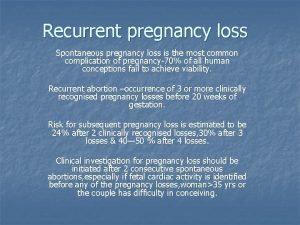
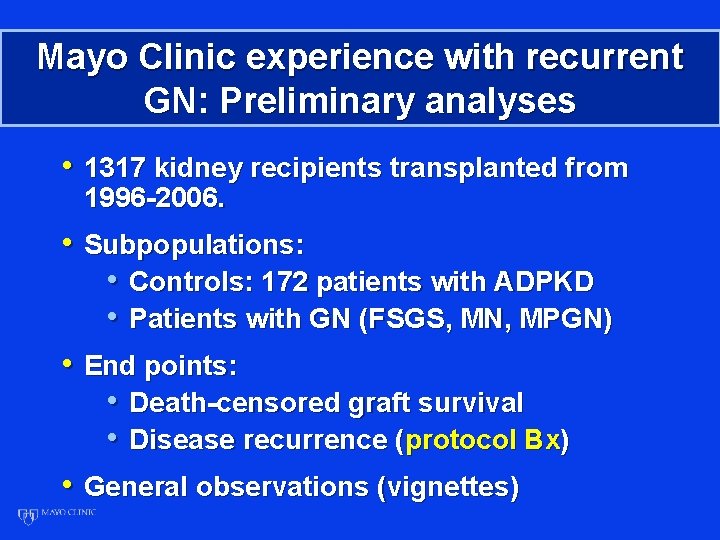
Mayo Clinic experience with recurrent GN: Preliminary analyses • 1317 kidney recipients transplanted from 1996 -2006. • Subpopulations: • Controls: 172 patients with ADPKD • Patients with GN (FSGS, MN, MPGN) • End points: • Death-censored graft survival • Disease recurrence (protocol Bx) • General observations (vignettes)
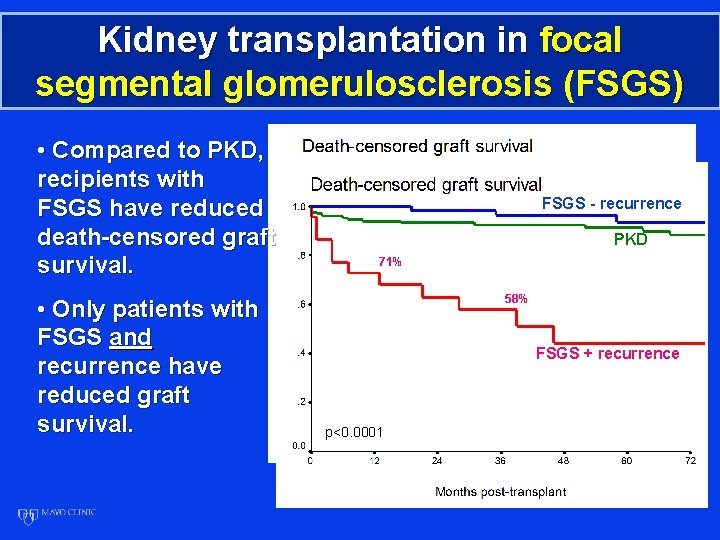
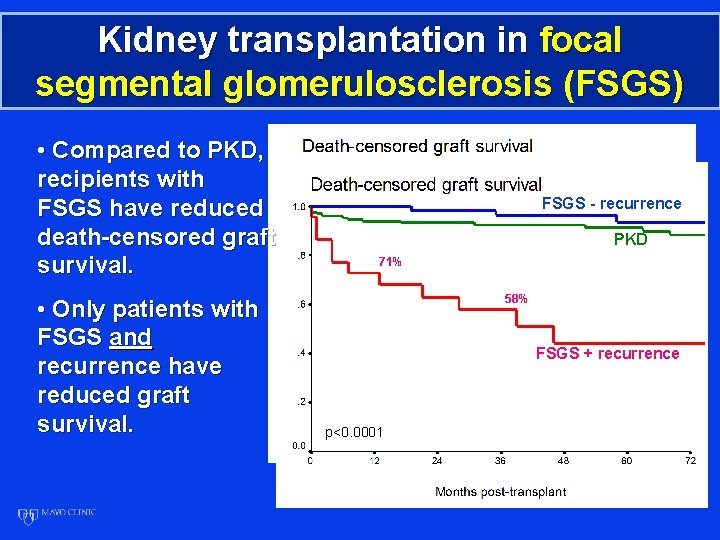
Kidney transplantation in focal segmental glomerulosclerosis (FSGS) • Compared to PKD, recipients with FSGS have reduced death-censored graft survival. • Only patients with FSGS and recurrence have reduced graft survival. PKD, N=172 FSGS - recurrence PKD 71% 58% FSGS, N=103 FSGS + recurrence p=0. 0048 p<0. 0001
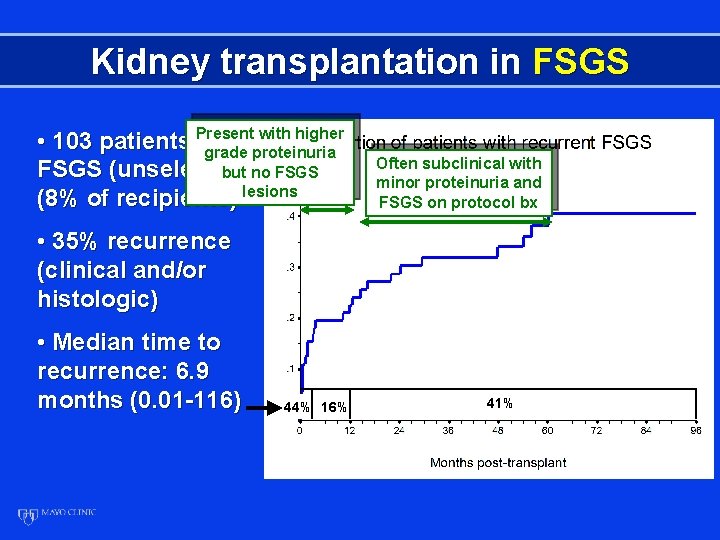
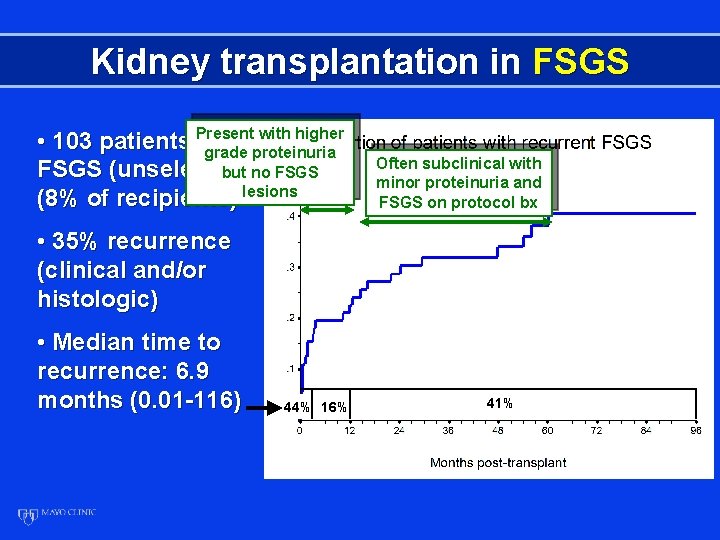
Kidney transplantation in FSGS with higher • 103 patients Present with grade proteinuria FSGS (unselected but)no FSGS (8% of recipients) lesions Often subclinical with minor proteinuria and FSGS on protocol bx • 35% recurrence (clinical and/or histologic) • Median time to recurrence: 6. 9 months (0. 01 -116) 44% 16% 41%
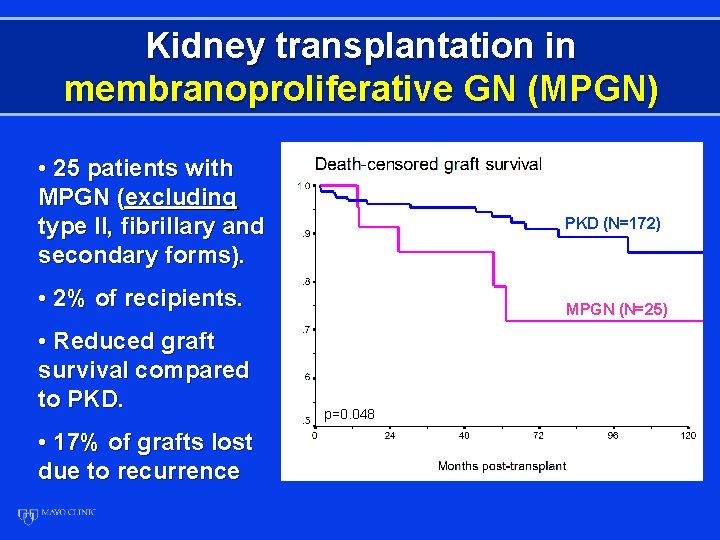
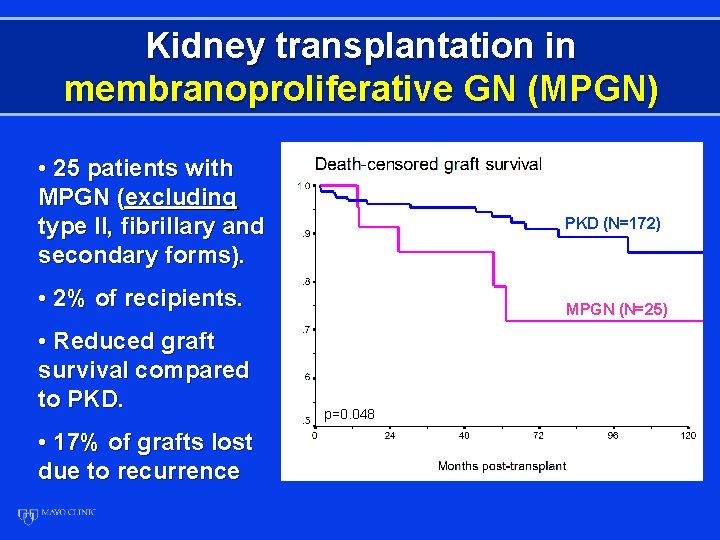
Kidney transplantation in membranoproliferative GN (MPGN) • 25 patients with MPGN (excluding type II, fibrillary and secondary forms). PKD (N=172) • 2% of recipients. • Reduced graft survival compared to PKD. • 17% of grafts lost due to recurrence MPGN (N=25) p=0. 048
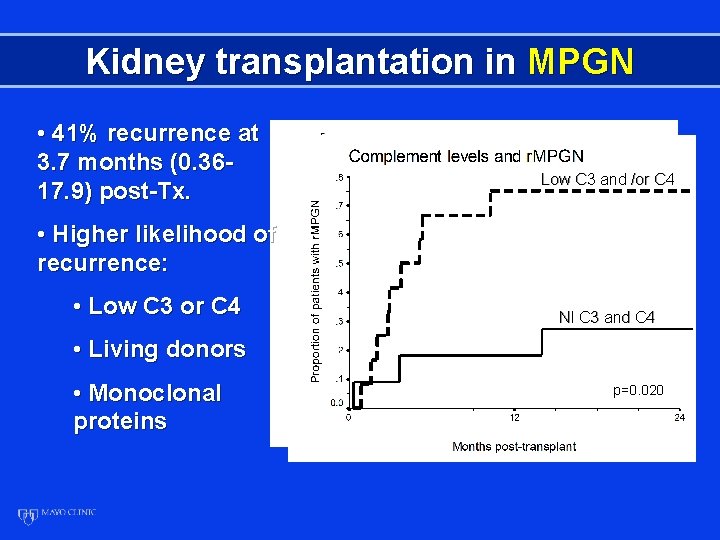
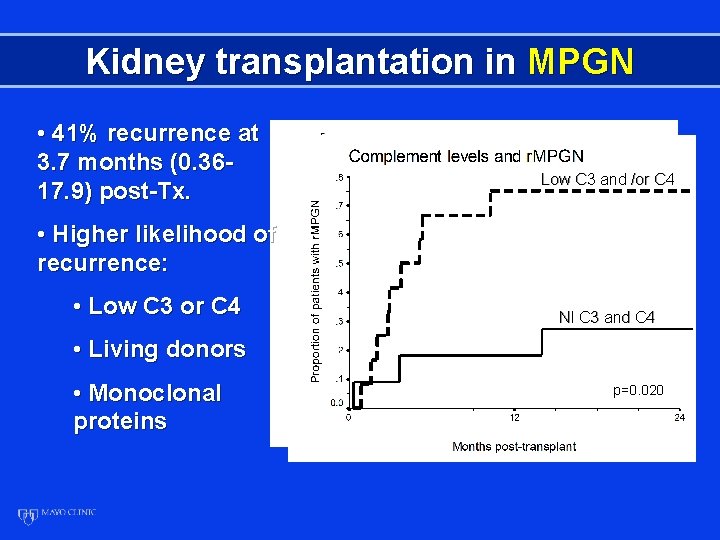
Kidney transplantation in MPGN • 41% recurrence at 3. 7 months (0. 3617. 9) post-Tx. Low C 3 and /or C 4 • Higher likelihood of recurrence: • Low C 3 or C 4 Nl C 3 and C 4 • Living donors • Monoclonal proteins p=0. 020
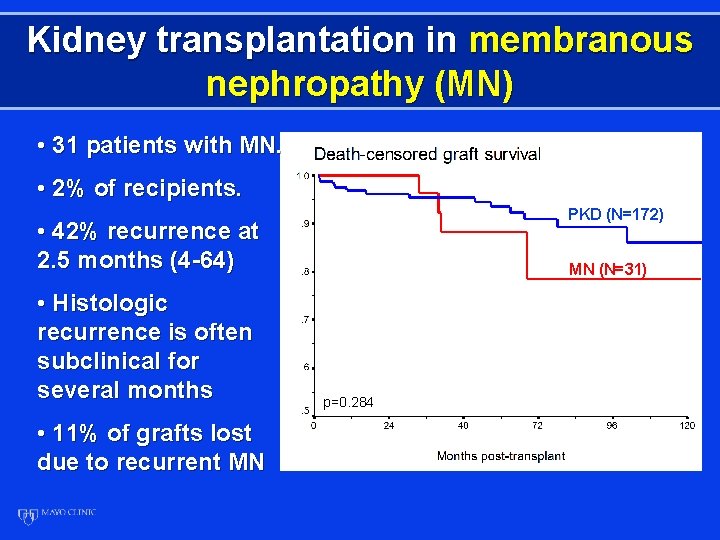
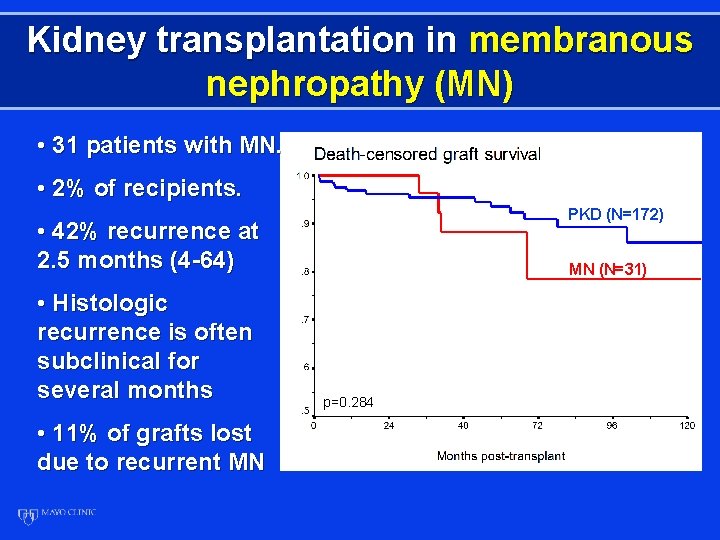
Kidney transplantation in membranous nephropathy (MN) • 31 patients with MN. • 2% of recipients. PKD (N=172) • 42% recurrence at 2. 5 months (4 -64) • Histologic recurrence is often subclinical for several months • 11% of grafts lost due to recurrent MN MN (N=31) p=0. 284
Protocol biopsies and recurrent disease: Postulates 1. Protocol biopsies may allow early diagnosis of recurrent GN before it is clinically apparent. 2. The earliest histologic changes of GN may give us clues about the pathogenesis of these diseases. 3. Early histologic diagnosis may allow more effective treatment.
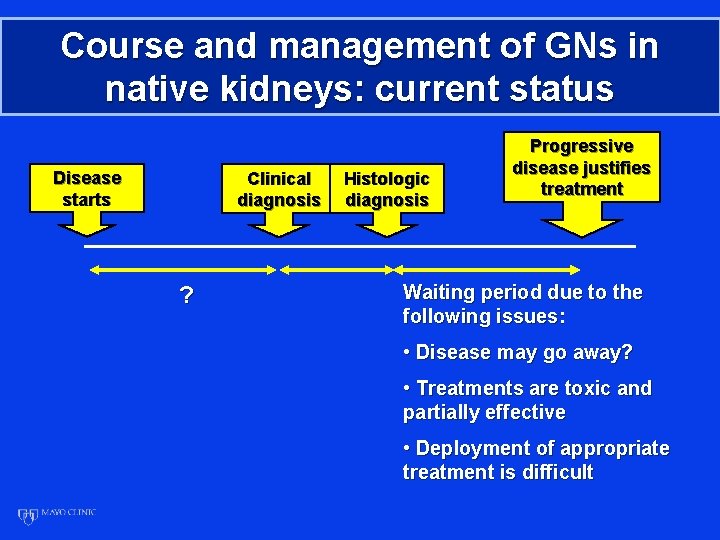
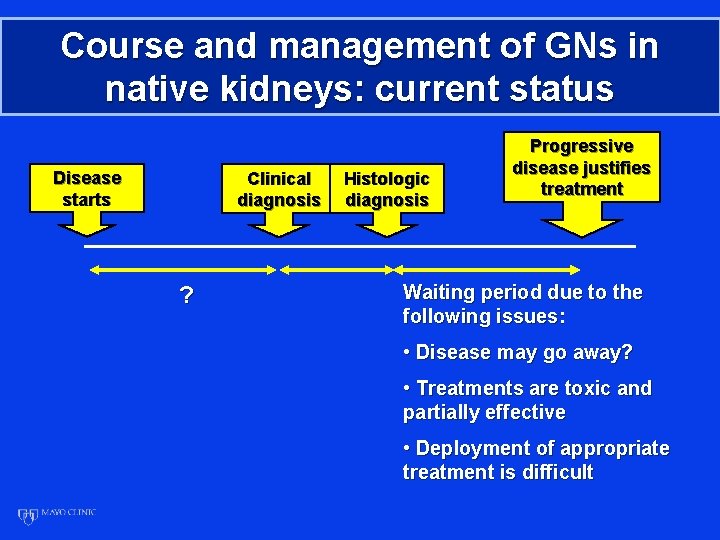
Course and management of GNs in native kidneys: current status Disease starts Clinical diagnosis ? Histologic diagnosis Progressive disease justifies treatment Waiting period due to the following issues: • Disease may go away? • Treatments are toxic and partially effective • Deployment of appropriate treatment is difficult
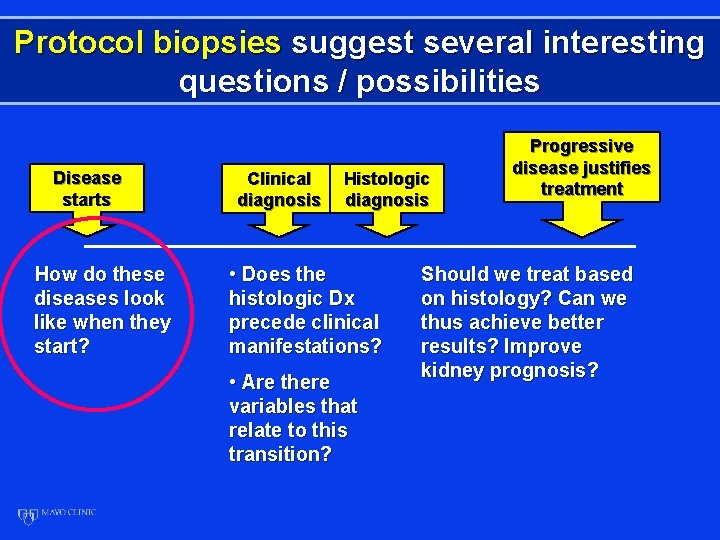
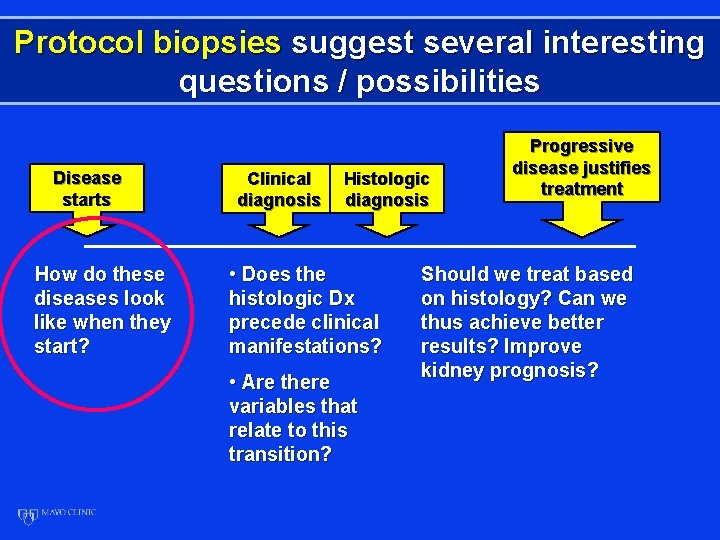
Protocol biopsies suggest several interesting questions / possibilities Disease starts How do these diseases look like when they start? Clinical diagnosis Histologic diagnosis • Does the histologic Dx precede clinical manifestations? • Are there variables that relate to this transition? Progressive disease justifies treatment Should we treat based on histology? Can we thus achieve better results? Improve kidney prognosis?
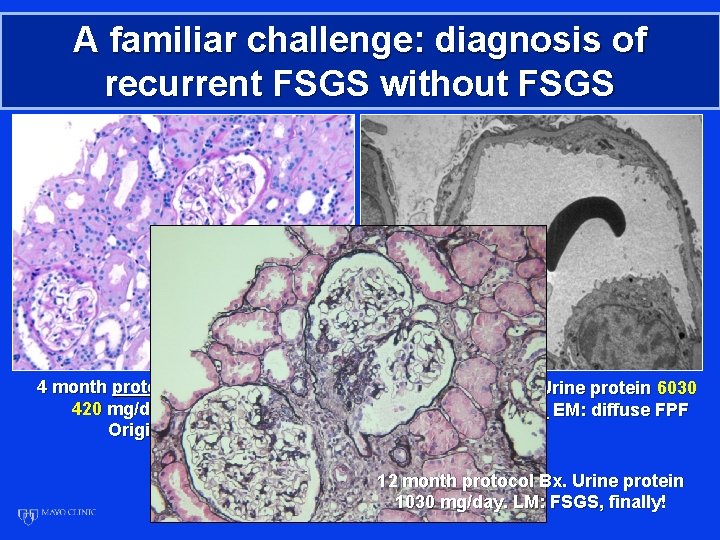
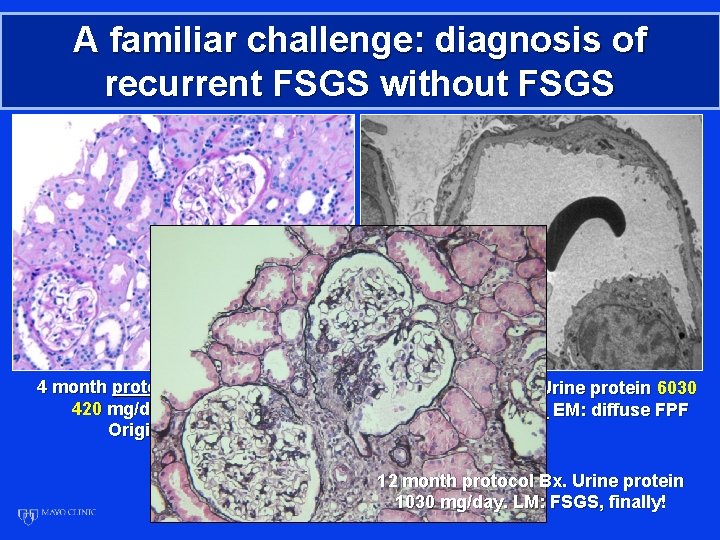
A familiar challenge: diagnosis of recurrent FSGS without FSGS 4 month protocol Bx. Urine protein 420 mg/day. EM: focal FPF Original Dx: FSGS 5 month clinical Bx. Urine protein 6030 mg/day. LM: normal. EM: diffuse FPF 12 month protocol Bx. Urine protein 1030 mg/day. LM: FSGS, finally!
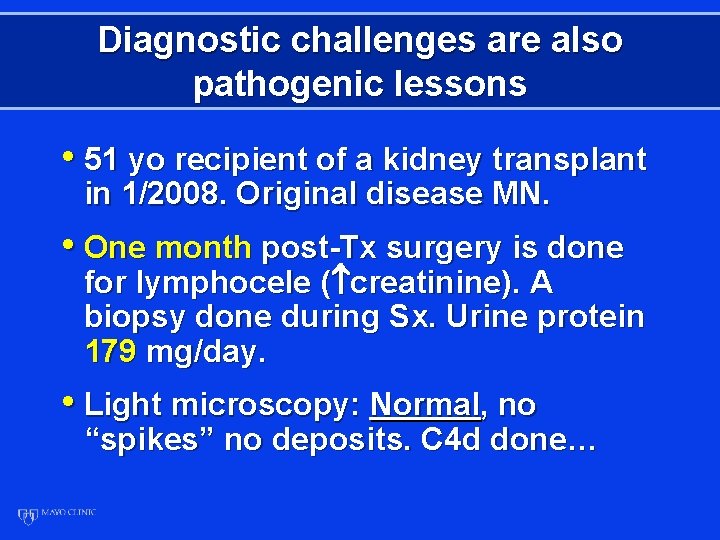
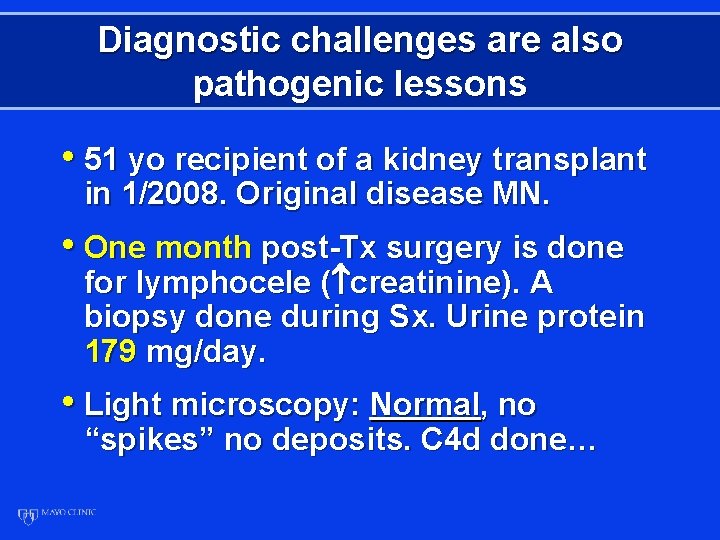
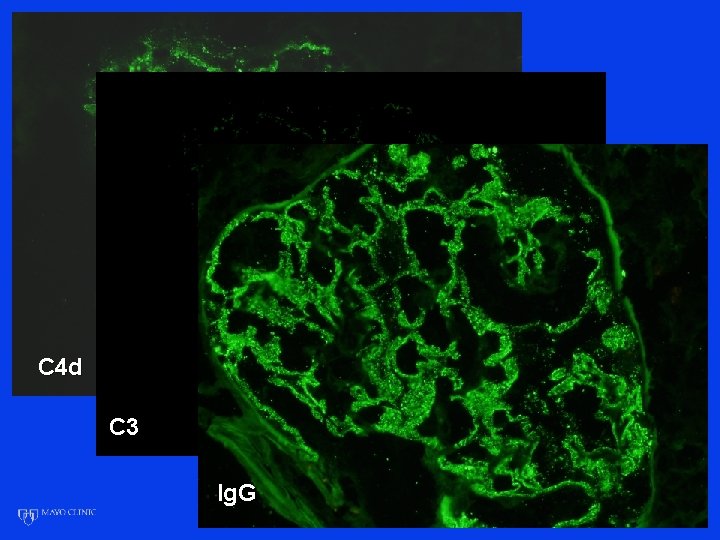
Diagnostic challenges are also pathogenic lessons • 51 yo recipient of a kidney transplant in 1/2008. Original disease MN. • One month post-Tx surgery is done for lymphocele ( creatinine). A biopsy done during Sx. Urine protein 179 mg/day. • Light microscopy: Normal, no “spikes” no deposits. C 4 d done…
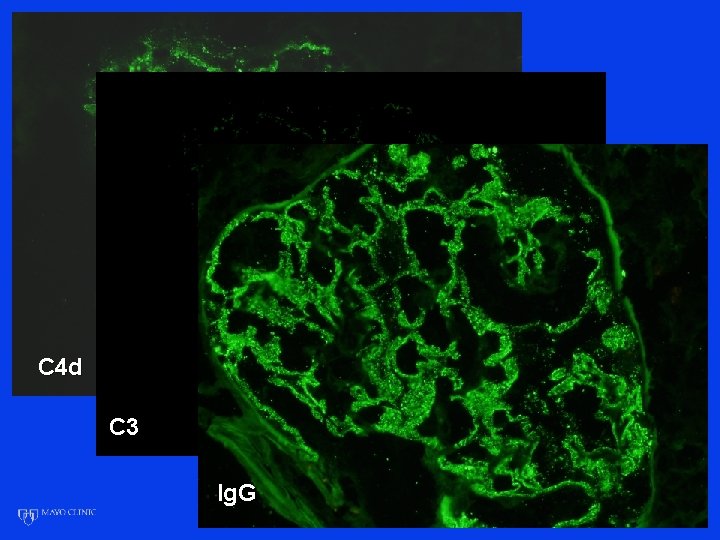
C 4 d C 3 Ig. G
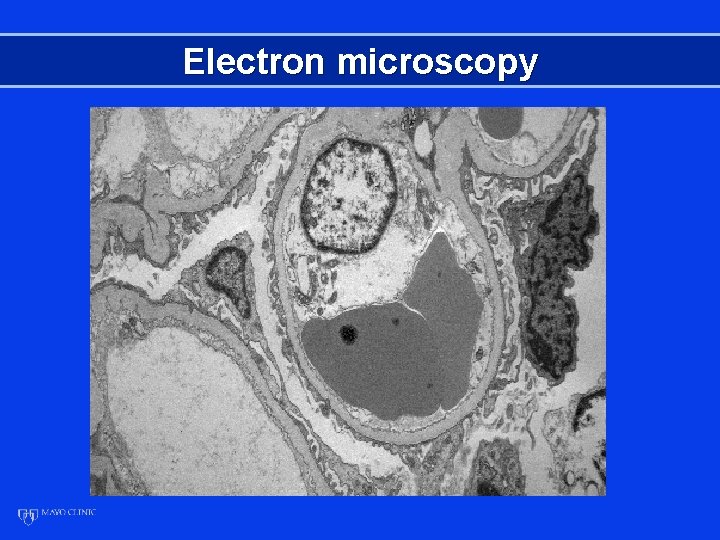
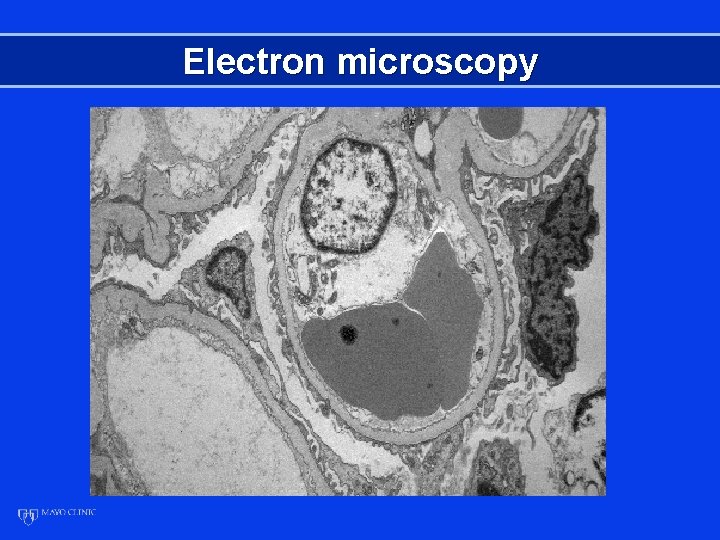
Electron microscopy
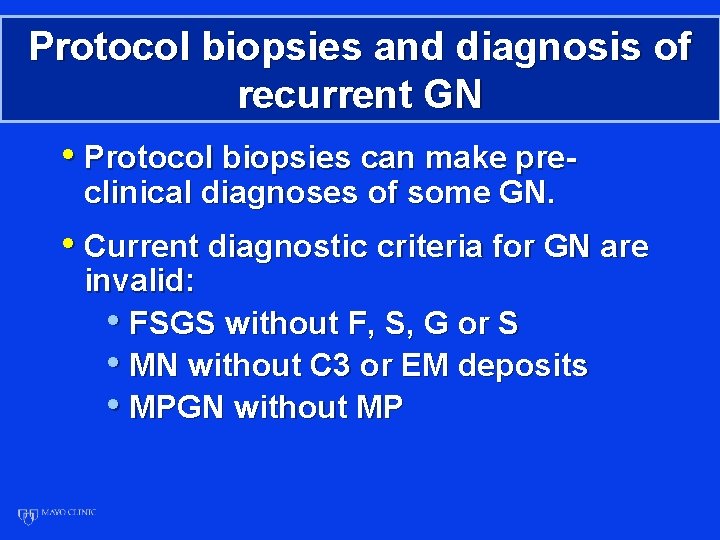
Protocol biopsies and diagnosis of recurrent GN • Protocol biopsies can make preclinical diagnoses of some GN. • Current diagnostic criteria for GN are invalid: • FSGS without F, S, G or S • MN without C 3 or EM deposits • MPGN without MP

Next question: Does a pre-clinical diagnosis lead to clinical disease? • 19 patients with MN diagnosed by protocol biopsy and followed, untreated for at least one year: • 2 (10. 5%) have maintained low levels of proteinuria. • 17 (89. 5%) have had progressive proteinuria • Repeat biopsies: MN in all (no spontaneous histologic remissions)
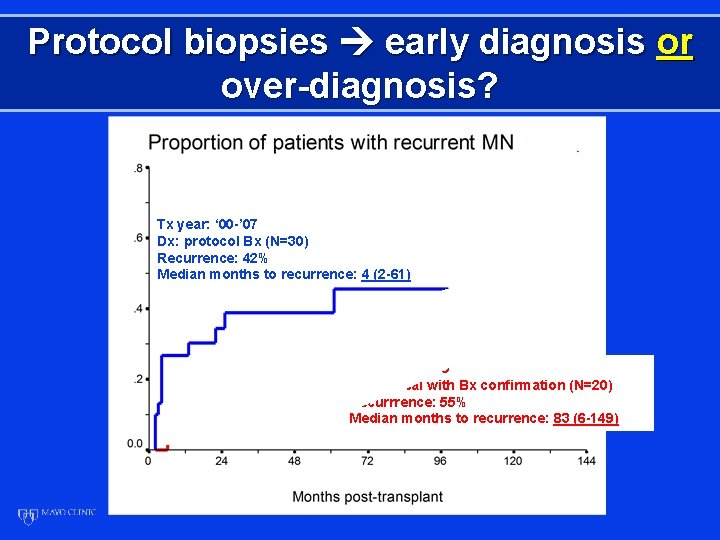
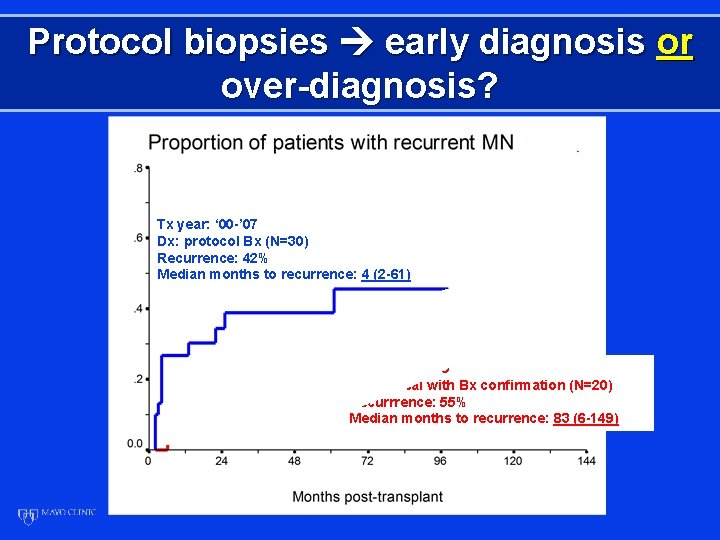
Protocol biopsies early diagnosis or over-diagnosis? Tx year: ‘ 00 -’ 07 Dx: protocol Bx (N=30) Recurrence: 42% Median months to recurrence: 4 (2 -61) Tx year: ‘ 90 -’ 99 Dx: clinical with Bx confirmation (N=20) Recurrrence: 55% Median months to recurrence: 83 (6 -149)
Postulated benefits of protocol biopsies in recurrent GN 1. Early, pre-clinical diagnosis 2. Pathogenic clues 3. Early histologic diagnosis may allow more effective treatment (preliminary studies suggest that we can/should start to explore this question)
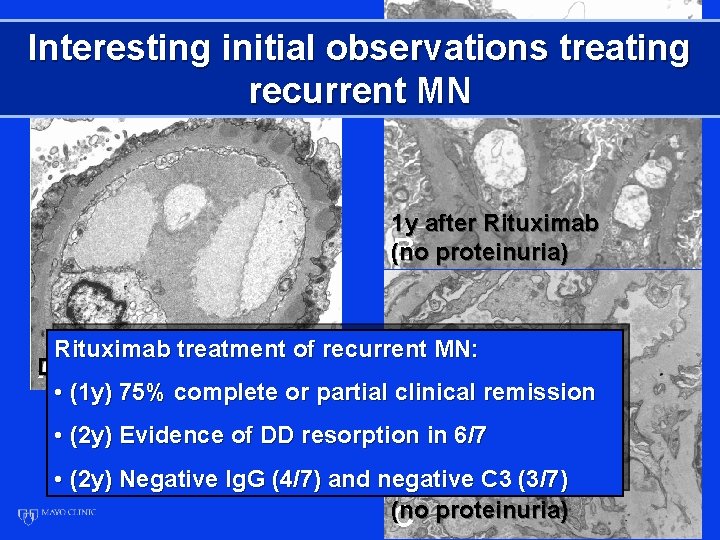
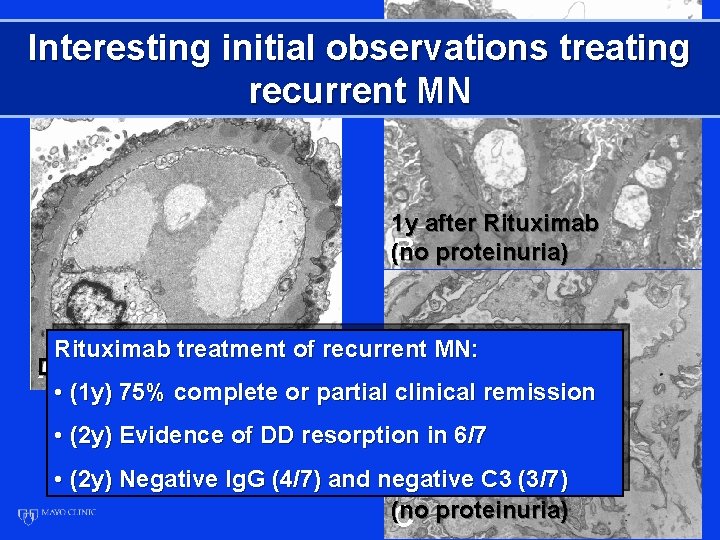
Interesting initial observations treating recurrent MN 1 y after Rituximab (no proteinuria) Rituximab treatment of recurrent MN: Diagnosis(4 mo post-Tx) • (1 y) 75% complete or partial clinical remission • (2 y) Evidence of DD resorption in 6/7 • (2 y) Negative Ig. G (4/7) and negative (3/7) 2 y after. C 3 Rituximab (no proteinuria)
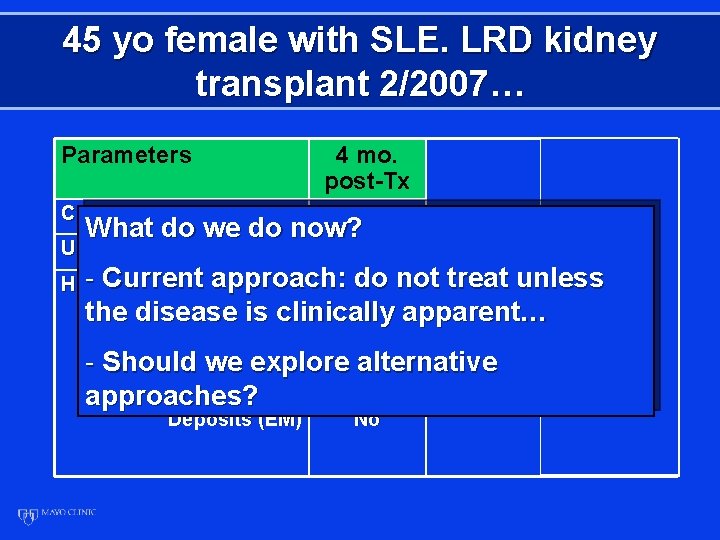
45 yo female with SLE. LRD kidney transplant 2/2007… Parameters Creatinine (GFR) 4 mo. post-Tx 12 mo. post-Tx 24 mo. post-Tx 1. 1 (57) 1. 0 (63) 132 90 165 What do we do now? U. Protein (mg/day) - Current Histology: approach: do not treat unless the disease is clinically Mesangial proliferation None apparent… Mild Moderate C 1 q (IF) 2+ - Should we explore. Trace alternative IGG (IF) Negative 3+ approaches? Deposits (EM) No Not done 3+ 3+ Mesangial paramesangi al

Recurrent disease • 20% of death-censored graft losses are due to recurrent disease (15% r. GN). • Studies using protocol biopsies suggest: • Need diagnostic criteria for early dis. • Need multicenter studies based on protocol biopsies to determine: • Histologic diagnosis clinical? • Effectiveness early Rx? • We finally have good questions and reasonable tools to try to answer them!


Recurrent disease after kidney transplantation-- it is time to unite to address this problem! A. Matas If we knew what we were doing it would not be called research A. Einstein

In addition, If we knew what we were doing it would not be called research A. Einstein
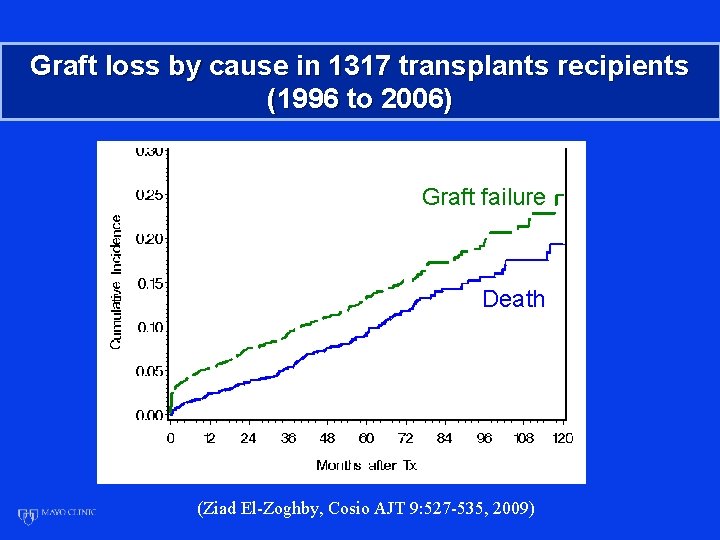
Graft loss by cause in 1317 transplants recipients (1996 to 2006) Graft failure Death (Ziad El-Zoghby, Cosio AJT 9: 527 -535, 2009)
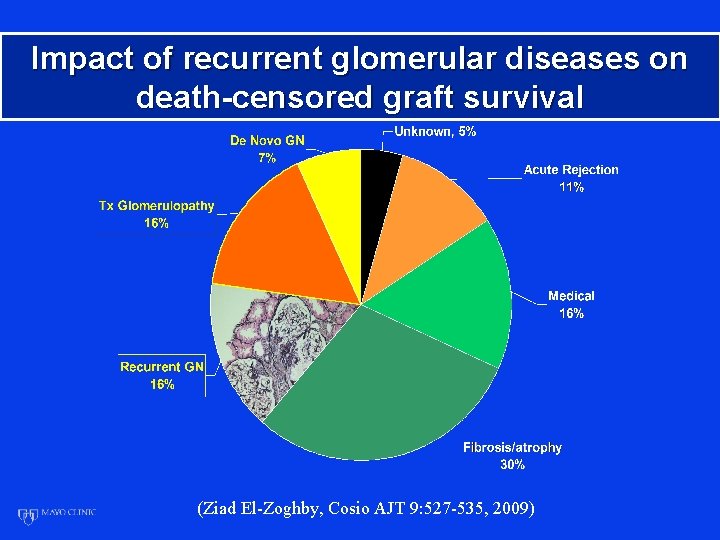
Impact of recurrent glomerular diseases on death-censored graft survival (Ziad El-Zoghby, Cosio AJT 9: 527 -535, 2009)
 Demineralized freeze-dried bone allograft
Demineralized freeze-dried bone allograft Autogenous vs allograft
Autogenous vs allograft Unit cost meaning
Unit cost meaning Bharathi viswanathan
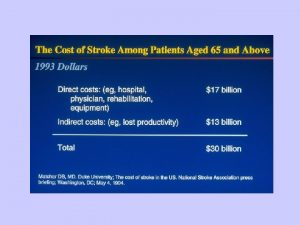
Bharathi viswanathan Recurrent stroke causes
Recurrent stroke causes Recurrent laryngeal nerve injury
Recurrent laryngeal nerve injury Bert question generation
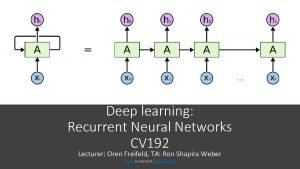
Bert question generation Visualizing and understanding recurrent networks
Visualizing and understanding recurrent networks Iliac nerve
Iliac nerve Arytenoid muscle function
Arytenoid muscle function 4th aortic arch derivatives
4th aortic arch derivatives Weber syndrome
Weber syndrome Jolls triangle thyroid
Jolls triangle thyroid Semons law
Semons law Pixel recurrent neural networks.
Pixel recurrent neural networks. Rolo tracking
Rolo tracking Andrew ng lstm
Andrew ng lstm A recurrent image in a literary work is the
A recurrent image in a literary work is the Extensions of recurrent neural network language model
Extensions of recurrent neural network language model Recurrent connection
Recurrent connection Visualizing and understanding recurrent networks
Visualizing and understanding recurrent networks Recurrent neural network based language model
Recurrent neural network based language model Recurrent strokes
Recurrent strokes Simple recurrent network
Simple recurrent network Part 135 recurrent training
Part 135 recurrent training Cs 7643 github
Cs 7643 github Disease of external nose
Disease of external nose Site:slidetodoc.com
Site:slidetodoc.com Five principles of hair design
Five principles of hair design Azure worker role
Azure worker role Krappmann symbolischer interaktionismus
Krappmann symbolischer interaktionismus Statuses and their related roles determine the structure
Statuses and their related roles determine the structure Fspos
Fspos